Abstract
Purpose
To describe the indications, visual acuity outcomes and graft survival after penetrating keratoplasty in Addis Ababa, Ethiopia.
Methods
The medical records of patients who had penetrating keratoplasty (PKP) at Menelik II Hospital between September 2000 and September 2013 were retrospectively reviewed. The pre-specified outcomes were graft survival, visual acuity, and complication rates.
Results
A total of 321 patients underwent penetrating keratoplasty during the study period and were included in the analysis. The indications for surgery were trachoma or leukoma in 141 (44%), keratoconus (KCN) in 45 (14%), corneal dystrophy in 46 (14%), pseudophakic or aphakic bullous keratopathy in 28 (9%), trauma in 27 (8%), prior graft failure in 18 (6%), active ulcer, burn or perforation 9 (3%), and other 7 (2%). Graft survival was 80% overall at 2 years but varied considerably depending on indication for surgery. Uncorrected visual acuity improved from baseline mean logMAR 2.09 (SD 0.67) to mean logMAR of 1.53 (SD 1.03) at 2 years. A number of factors affected visual acuity outcomes. Patients were not routinely refracted, and only 18% (N = 60) of patients had access to corrective spectacles or contact lenses post-operatively. Complication rates were high with infectious keratitis being the most common.
Conclusions
Penetrating keratoplasty is becoming a viable treatment for corneal opacity in developing countries. However, the high burden of disease and lack of corrective lenses remain significant obstacles to overcome.
Keywords: Penetrating Keratoplasty, Graft Failure, Ethiopia, Cornea
Introduction
Although corneal opacity is a common cause of visual loss in developing countries, access to sight restoring corneal transplantation remains challenging for many patients.1 In resource poor settings management of penetrating keratoplasty is complicated by a lack of supportive infrastructure such as eye banks and adequately equipped operating rooms. There may also be limited access to trained corneal surgeons and follow up care, and little opportunity for corrective lenses for visual rehabilitation.2,3
The World Health Organization estimates that corneal blindness is the second leading cause of blindness among all age groups in Ethiopia and the leading cause of visual impairment among children and adolescents in that country.4 In order to meet this need, an eye bank has been operating in the country since 2003 - one of the only eye banks in Africa. While a growing number of cornea fellowship-trained ophthalmologists are practicing throughout the country, most transplants are performed at the university hospital, Menelik II Eye Hospital in Addis Ababa. Given the challenges of implementing corneal transplantation in the developing world, we sought to document the outcomes of patients receiving corneal transplants at this hospital in order to guide surgeons throughout Africa as corneal transplantation becomes more available on the continent. Here, we describe the indications for surgery, visual acuity outcomes as well as graft survival in patients undergoing penetrating keratoplasty in Addis Ababa, Ethiopia.
Methods
The medical records of patients who underwent penetrating keratoplasty (PKP) at Menelik II Eye Hospital in Addis Ethiopia were retrospectively reviewed. All corneal transplants were performed by one of two experienced cornea-trained Ethiopian surgeons under local anesthesia with retrobulbar block. In most cases, the donor graft was oversized by 0.25–0.5 mm compared with the recipient and a 16-bite interrupted suture technique was used. Post-operative care including timing of removal of graft sutures and tapering of topical antibiotics and steroids were at the discretion of the treating physician.
Data were collected including demographic information such as patient’s age, sex, baseline visual acuity, the surgical indication and other ocular co-morbid conditions. The primary study outcome was graft survival, defined as irreversible loss of graft clarity. Secondary outcomes included uncorrected visual acuity, and complications rates such as development of secondary ocular hypertension or glaucoma, infectious keratitis, graft rejection, endophthalmitis and the need for subsequent surgery. Visual acuity was uncorrected unless the patient had access to spectacles and no pinhole visual acuity was available. Ocular hypertension or glaucoma was defined as either a measured intraocular pressure greater than 25 or an observed increase in the cup-disc ratio.
IRB approval for this study was obtained at the University of California, San Francisco and the Menelik II Hospital in Addis Ababa, Ethiopia. Informed consent was obtained from all study participants, and the study conformed to the Declaration of Helsinki. Graft survival curves were produced using the Kaplan Meier method. The log-rank test was used to evaluate differences in survival based on indication for surgery comparing graft survival in keratoconus (KCN) to all of the other indications. Cox proportional hazards models were used to assess the time to each complication by indication for surgery. An alpha of <0.05 was considered to be statistically significant. All data were analyzed with Stata 14.0.
Results
A total of 332 patients underwent penetrating keratoplasty (PKP) between September of 2000 and September of 2013. The study population consisted of 173 men (52%) and 159 women (48%) and had a mean age of 33 (SD 19). Mean baseline uncorrected visual acuity was logMAR 2.09 (SD 0.67, approximate snellen 20/2400). The vast majority of transplants were performed for optical rather than therapeutic indications (N = 330; 99%) and half of those undergoing PKP could not pay for the services (N = 167, 50%). Table 1 outlines the indication for surgery which was trachoma or post-infectious corneal opacity in 141 (44%), keratoconus (KCN) in 45 (14%), corneal dystrophy in 46 (14%), pseudophakic or aphakic bullous keratopathy in 28 (9%), trauma in 27 (8%), prior graft failure in 18 (6%), active ulcer, burn or perforation in 9 (3%), and another indication in 8 (2%).
Table 1.
Indication for Penetrating Keratoplasty in Ethiopia at Menelik II Hospital
| Indication for Surgery | N = 321 | % |
|---|---|---|
| Leukoma/Trachoma | 141 | 44 |
| Corneal Dystrophy | 46 | 14 |
| Keratoconus | 45 | 14 |
| Pseudophakic/Aphakic Bullous Keratopathy | 28 | 9 |
| Trauma | 27 | 8 |
| Prior Graft Failure | 18 | 6 |
| Active Ulcer/Burn/Perforation | 9 | 3 |
| Other | 7 | 2 |
Donor tissue for transplantation came from the Ethiopian eye bank in 92% (N = 307) of cases. The remaining donor tissue (N = 27) was donated from the United States, Poland, Czech Republic and Paraguay. The most common cause of death among Ethiopian donors was trauma (N = 255; 83%) while it was cardiovascular disease among imported tissue (N = 13; 52%). The mean donor age for Ethiopian tissue was quite young at 29 years (SD 9) while the mean age of imported tissue was 58 years (SD 12). Ethiopian tissue had a mean death to preservation time of 4.8 hours (SD 1.8) and death to implantation time of 6.9 days (SD 3.2); the corresponding numbers for imported tissue were 9.9 hours (SD 5.8) and 12 days (SD 3.1). Optisol was the most common storage media (N = 328; 99%).
The mean endothelial cell count of imported tissue was 2708 (SD 489) as measured by the specular microscope at each respective institution. The mean endothelial cell count of donor grafts as measured by specular microscopy at the Ethiopian Eye Bank was 3,539 cells/mm2 (SD 637). The Ethiopian endothelial cell counts appeared to be remarkably high and although the donors were very young which could account for this, it was thought that measurement error was also possible.
The average donor graft diameter was 8mm (range 7mm to 8.75), and the majority of grafts were performed with an interrupted versus running suture technique (N = 328; 99%). Eighty-four patients (25%) had concurrent extra-capsular cataract extraction at the time of keratoplasty, an additional 8 had intraocular lens (IOL) exchange and one patient had IOL explantation. The most common intra-operative complication was vitreous loss, which occurred 6% of the time (N = 20).
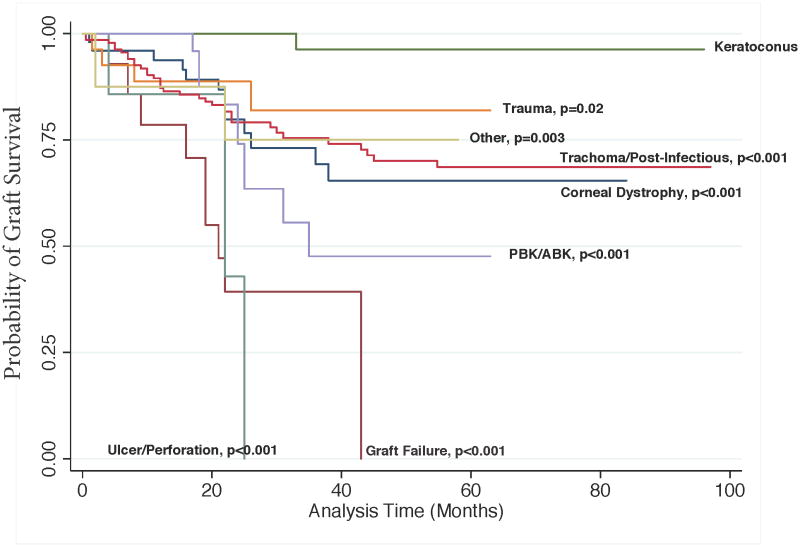
Mean follow-up time for all study participants was 37 months (SD 21). There was at least six-month follow-up available for 96% (N = 319) and two years data were available for 76% (N = 252). By 5 years follow up data was available for 26% (N = 85) and at 10 years post-operatively data were available for 1% (N = 3). Figure 1 demonstrates the Kaplan-Meyer curves for graft survival by indication for surgery. Graft survival including all available follow up for all patients was 71% (N = 235). Graft survival at 6 months was 95% (N = 315), 89% at 1 year (N =297), and 80% at 2 years (N =266). Study participants who had PKP for keratoconus had a mean follow up time of 46 months (SD 21). Their two-year graft survival rate was 100% with follow up data available for 89% of study participants (N = 40). Compared with keratoconus all other indications had statistically significantly decreased 2-year graft survival including corneal dystrophy (78%, P < 0.001), prior graft failure (56%, P < 0.001), trauma (94%; P = 0.02), active ulcer/burn/perforation (86%; P < 0.001) trachoma/post-infectious corneal opacity (78%; P < 0.001) pseudophakic/aphakic bullous keratopathy (83%; P = 0.004) and all other indications (75%; P < 0.001).
Figure 1. Graft Survival by Indication.
Kaplan-Meyer curves showing graft survival at last follow-up by indication for surgery. Logrank P values reflect a comparison of the Kaplan-Meyer curve for keratoconus versus each of the other indications for surgery.
Abbreviations: PBK/ABK, pseudophakic bullous keratopathy/aphakic bullous keratopathy
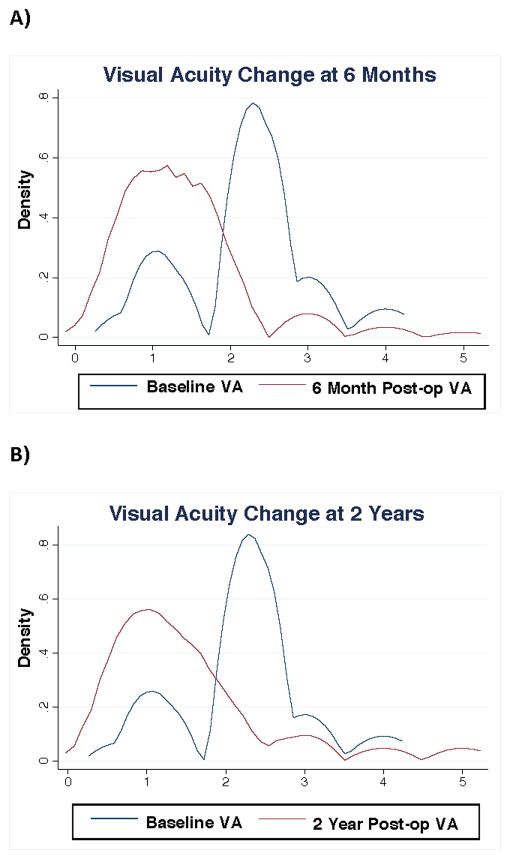
Figure 2 demonstrates the change in uncorrected visual acuity from baseline to six months and two years in logMAR for patients with follow-up of that duration. Mean uncorrected visual acuity at baseline was logMAR 2.2 (SD 0.78; ~Snellen 20/3200) and improved to logMAR 1.39 (SD 0.83; ~Snellen of 20/490) at 6 months, although it had declined somewhat to logMAR 1.53 (SD 1.04; ~Snellen of 20/670) at 2 years. A number of factors affected visual acuity outcomes. Patients were not routinely refracted, and only 18% (N = 60) of patients had access to corrective spectacles. Of those with access to spectacles post-operatively visual acuity was better with logMAR 1.07 (SD 0.46; ~Snellen of 20/230) at 6 months and logMAR 1.28 (SD 0.98; ~Snellen 20/380) at 2 years. Visual acuity outcomes were also improved among KCN patients who had mean baseline visual acuity of logMAR 1.96 (SD 0.60; ~Snellen of 20/1800) that improved dramatically at 6-months post-operatively with mean visual acuity of logMAR 0.92 (SD 0.48; ~Snellen 20/160) and remained stable at 2 years with mean logMAR 0.91 (SD 0.35; ~Snellen 20/160). Although over 53% (N = 168) of grafts were determined to have poor vision despite a clear graft and thought to have vision-limiting corneal astigmatism, none of these patients had access to rigid contact lenses. A small number of patients were also thought to have vision limiting ocular co-morbid conditions including amblyopia 8% (N = 27), end-stage glaucoma in 3% (N = 9), retinal pathology in 2% (N = 7), and other etiologies in 1% (N =3).
Figure 2. Visual Acuity Change from A) Baseline to 6 Months and B) Baseline to 2 Years Post-Operatively.
Kernel density plots showing visual acuity change from baseline to 6 months and from baseline to 2 years in LogMAR including only study participants with follow up of that duration. Of note, lower numbers on the logMAR scale represent an improvement in visual acuity.
The most common post-operative complications included infectious keratitis in 32% (N =101), secondary glaucoma in 30% (N = 95), endothelial rejection in 26% (N = 83), and endophthalmitis in 7% (N = 21). Patients who had an episode of endothelial rejection had a 3.84-fold increase in subsequent graft failure rate (95% CI 2.44–6.04; P < 0.001). There was no observed increased risk of graft failure among study participants who developed secondary glaucoma (HR 1.06, 95% CI 0.66 to 1.71, P = 0.80). Compared with imported tissue those receiving Ethiopian prepared tissue had 0.62 decreased odds of graft failure but this was not a statistically significant difference (95% CI 0.26 to 1.45; P = 0.27).
Complications varied somewhat by indication for keratoplasty. As expected, prior graft failure conferred a greater risk of endothelial rejection compared with keratoconus (P <0.001). Active ulcer, perforation or corneal burn conferred a higher risk of infectious keratitis (P = 0.04) and endophthalmitis (P <0.001) compared with study participants undergoing corneal transplant for keratoconus. All indications of surgery had similar rates of secondary glaucoma.
Discussion
In this study of penetrating keratoplasty outcomes in Ethiopia, we found that indication for surgery was a statistically significant predictor of graft survival. Indication for surgery has been shown to be an important determinant of graft survival both in the US5 and internationally.2,6–8 Since patients undergoing penetrating keratoplasty for keratoconus (KCN) have an excellent prognosis it has been suggested that graft survival in KCN can be used as a comparison between different centers and countries.9 Graft survival of KCN in our series was excellent and quite comparable to other series.9,10 Grafts performed for other indications in Ethiopia had lower survival than KCN which is likely due to the fact that most of them were performed for high-risk indications.
Graft survival was improved among study participants receiving Ethiopian tissue compared with donor tissue imported from other countries, although this difference was not statistically significant. The corneal donor study has demonstrated that donor age is a factor in graft survival, therefore, these results are probably related to the young age of donors in our series.11 The elevated endothelial cell counts among Ethiopian donors in our study are assumed to be erroneous possibly due to measurement error at the eye bank.
The most common complications in our series were related to suture abscess and corneal ulceration. As expected these complications were more common in high-risk grafts and those performed for therapeutic indications. Not surprisingly, study participants who had one such complication had a statistically significant increased risk of graft failure. Strategies to reduce infectious complications such as early suture removal, prolonged topical antibiotics and close follow up may reduce these complications in the future.
Limitations to this study include those common to all retrospective studies. Given the fact that our study was located in a resource poor setting there were some missing data in chart reviews, and patients had inconsistent follow ups or were lost to follow up altogether. However, 96% of our study participants had at least 6 months of follow-up and problems such as intermittent follow up or different follow up times are commonly managed with survival analysis, as it was in our study. Visual acuity outcomes in our study were imperfect because we did not have best corrected visual acuity for most of our study participants due to a lack of access to glasses or contact lenses. Although this is a significant limitation it is representative of real-life outcomes of corneal transplantation in resource poor settings. The question of how to allocate resources such as spectacles versus corneal transplant to best improve vision-related quality-of-life in Ethiopia requires further study. A larger prospective study of corneal transplant outcomes in a setting such as Ethiopia will also be needed in order to confirm the findings in this study.
Corneal transplantation appears to be a viable treatment to address the high burden of corneal blindness in Ethiopia. Overall there was post-operative visual acuity improvement after corneal transplant in our series which resulted in ambulatory vision or better for many of our patients. There is room for improvement in visual rehabilitation after transplant at our center as demonstrated by the low number of transplant recipients who had access to spectacles post-operatively and the lack of availability of contact lenses. This should be an important focus of corneal transplant management to improve upon in the future.
Acknowledgments
Funding: This work was funded in part by unrestricted grants from the ALTA foundation (JRN), the Research to Prevent Blindness, and an individual NIH grant K23025025 (JRN).
None of the authors have any conflicts of interest to declare. This work was funded in part by unrestricted grants from the ALTA foundation (JRN), the Research to Prevent Blindness, and an individual NIH grant K23025025 (JRN). Dr. Jennifer Rose-Nussbaumer and Dr. Jeremy Keenan had full access to all the data and take responsibility for the integrity of the data and the accuracy of the data analysis.
Dr. Rose-Nussbaumer, Dr. Keenan, Dr. Menen and Dr. Yonas contributed to writing of the manuscript. Dr. Menen, Dr. Yonas, Dr. Keenan and Dr. Holsclaw contributed to study design and implementation. Dr. Indaram, and Nicole Stoller contributed to study implementation and editing of the manuscript.
Footnotes
Disclosures: The authors have no financial disclosures or conflicts of interest
References
- 1.Whitcher JP, Srinivasan M, Upadhyay MP. Corneal blindness: a global perspective. Bulletin of the World Health Organization. 2001;79:214–221. [PMC free article] [PubMed] [Google Scholar]
- 2.Tilahun Y, Shimelash D. The outcome of corneal transplantation versus indications in a tertiary eye care center in Ethiopia. Ethiopian medical journal. 2010;48:35–39. [PubMed] [Google Scholar]
- 3.Yorston D, Wood M, Foster A. Penetrating keratoplasty in Africa: graft survival and visual outcome. The British journal of ophthalmology. 1996;80:890–894. doi: 10.1136/bjo.80.10.890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pascolini D, Mariotti SP. Global estimates of visual impairment: 2010. The British journal of ophthalmology May. 2012;96:614–618. doi: 10.1136/bjophthalmol-2011-300539. [DOI] [PubMed] [Google Scholar]
- 5.Writing Committee for the Cornea Donor Study Research G. Sugar A, Gal RL, et al. Factors associated with corneal graft survival in the cornea donor study. JAMA ophthalmology Mar. 2015;133:246–254. doi: 10.1001/jamaophthalmol.2014.3923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dandona L, Naduvilath TJ, Janarthanan M, et al. Survival analysis and visual outcome in a large series of corneal transplants in India. The British journal of ophthalmology Sep. 1997;81:726–731. doi: 10.1136/bjo.81.9.726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wagoner MD, Gonnah el S, Al-Towerki AE King Khaled Eye Specialist Hospital Cornea Transplant Study G. Outcome of primary adult penetrating keratoplasty in a Saudi Arabian population. Cornea Sep. 2009;28:882–890. doi: 10.1097/ICO.0b013e31819b00d8. [DOI] [PubMed] [Google Scholar]
- 8.Tabin GC, Gurung R, Paudyal G, et al. Penetrating keratoplasty in Nepal. Cornea Aug. 2004;23:589–596. doi: 10.1097/01.ico.0000121712.36593.0d. [DOI] [PubMed] [Google Scholar]
- 9.Tan DT, Janardhanan P, Zhou H, et al. Penetrating keratoplasty in Asian eyes: the Singapore Corneal Transplant Study. Ophthalmology Jun. 2008;115:975–982. e971. doi: 10.1016/j.ophtha.2007.08.049. [DOI] [PubMed] [Google Scholar]
- 10.Williams KA, Roder D, Esterman A, et al. Factors predictive of corneal graft survival. Report from the Australian Corneal Graft Registry. Ophthalmology. 1992 Mar;99:403–414. doi: 10.1016/s0161-6420(92)31960-8. [DOI] [PubMed] [Google Scholar]
- 11.Writing Committee for the Cornea Donor Study Research G. Mannis MJ, Holland EJ, et al. The effect of donor age on penetrating keratoplasty for endothelial disease: graft survival after 10 years in the Cornea Donor Study. Ophthalmology Dec. 2013;120:2419–2427. doi: 10.1016/j.ophtha.2013.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]