Abstract
Purpose
Present a novel case of ocular argyrosis mimicking conjunctival melanoma.
Methods
A 48-year-old male career jewelry manufacturer presented with raised pigmented lesions in the inferior fornixes of both eyes. Brown-black colored, follicle-like, masses were observed in both fornixes.
Results
An incisional biopsy confirmed the presence of silver and the diagnosis of ocular argyrosis.
Conclusion
Despite its limited negative health effects, ocular arygrosis should be considered in the differential diagnosis of conjunctival pigmented lesions due to the potential for misidentification of neoplastic growth.
Keywords: Argyrosis, Silver, Conjunctival, mimicking melanoma, simulating melanoma
Introduction
Throughout history, naturally occurring silver has been used for various applications. The inherent physical properties of silver, such as malleability, luster, corrosion and oxidation resistance, high electrical conductivity, and ductility serve to make it both a useful and precious metal. Human exposure to silver in certain forms, and for prolonged periods, can have clinically detectable effects. Argyria is a condition caused by generalized embedding of silver granule deposits into skin and mucous membranes.1 Ocular argyrosis, however, is a specific form of argyria in which silver deposits accumulate in the region of the eye.2
Case Report
A 48-year-old male noted irritation and progressive pigmentation in his eyes over a period of twelve months. His medical history is unremarkable excluding diet-controlled hypercholesterolemia; no instances of personal or familial cancer exist. He was referred for unusual raised pigmented lesions in the inferior fornixes of both eyes. Upon examination, skin and eyelids showed no abnormal discoloration and vision was 20/20 in both eyes. Yet, as depicted in Figure 1A and 1B, prominent brown-black colored follicle-like masses were observed in both fornixes. There were no intrinsic cysts, feeder vessels, or abnormal pigmentation of the bulbar conjunctiva noted. On further questioning, the patient’s occupation was found to be jewelry manufacturing; he used an automated cutting machine that produced significant aerosolized material. An incisional biopsy was performed. Routine light microscopic examination identified abundant granular deposits, later found to be silver particles, around the basement membranes of vascular and adnexal structures, Figure 1C and 1D. A significant reactive lymphoid infiltrate was noted; its origin is possibly related to the metallic particles or another environmental stimulus. A negative Steiner stain discounted some known occult infectious etiologies that, in appearance, mimic this disease. We were unable to conduct a rhodamine stain at the time. Discrete black globular structures in the substantia propia showed orange-red birefringence on polaroscopic examination. The authors suspect that these structures are composed of gold, a material possessing anisotropic features when exposed to polarized light.3 Backscattered electron imaging identified these dense particles that were found by energy dispersive x-ray analysis to represent predominantly silver (17/20 particles) associated with sulfur, gold (2/20 particles) and iron (1/20 particles), Figure 2. The final interpretation was of ocular argyrosis with a small amount of chrysiasis. The area healed well and no clinically visible residual infiltrate was seen. The patient was advised of the condition and instructed to use measures to limit continued exposure.
Figure 1. Photographs of Inferior Fornices and Histopathology.
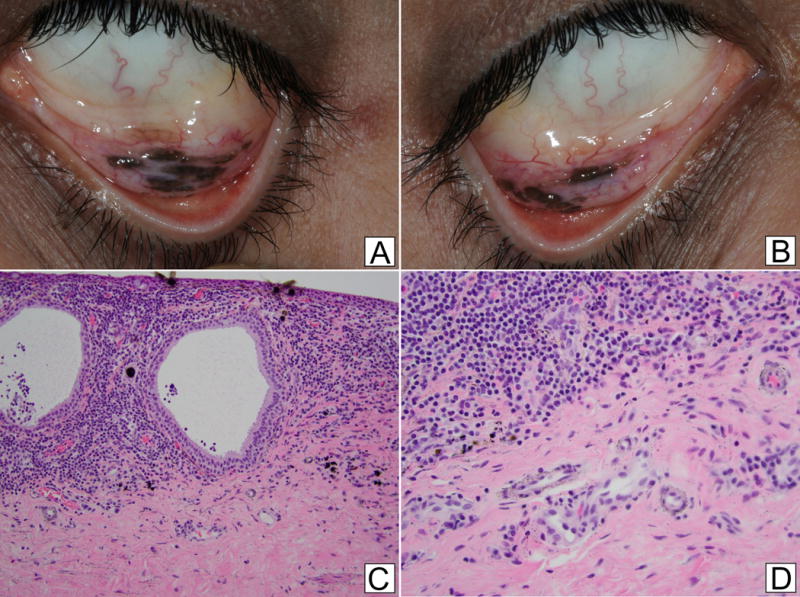
a.b. External photographs of the left (a) and right (b) inferior fornices showing elevated pigmented lesions with surrounding hypervascularity
c. A dense lichenoid lymphocytic infiltrate surrounds cystic invaginations of the mucosa, consistent with reactive lymphoid hyperplasia. Within surrounding submucosa, small rounded black deposits are noted (Hematoxylin and Eosin, 200×)
d. Higher power view shows fine to coarse black granules of silver embedded within the submucosa. A few rounded larger elements are also noted. (Hematoxylin and Eosin, 400×)
Figure 2. Backscatter Electron Imaging and Energy Dispersive X-Ray Analysis.
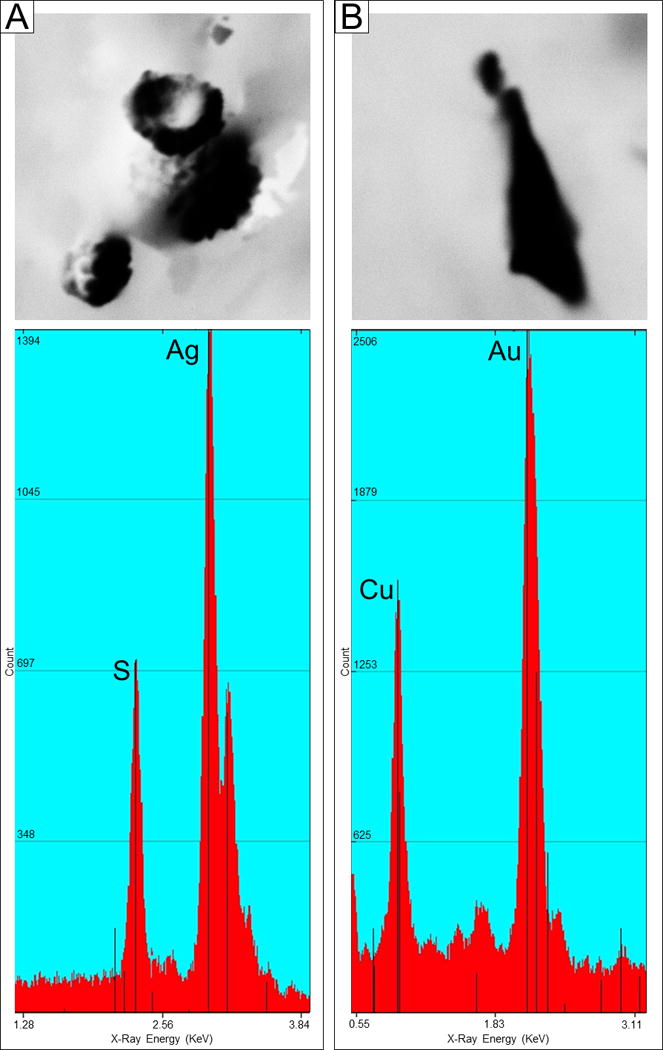
a. Backscattered electron imaging (BEI), 2700×, irregularly shaped AgS particles; Spectrum showing peaks for Ag and S
b. BEI, 7000×, irregularly shaped AuCu particle; Spectrum showing peaks for Au and Cu
Discussion
Previous research has shown that chronic exposure to silver-containing compounds is a risk factor for argyrosis development.4 Some types of exposure hazards include, but are not limited to, working with silver compounds in an occupational setting (silverware industry, photographic and x-ray film manufacturing, jewelry processing, etc.), consistently self-applying professional-grade eyelash tint, or chronic use of ocular silver protein drops (Argyrol).5,6,7,8,9
Clinical symptoms of argyrosis chiefly present in the form of discoloration localized to sites of silver absorption and deposition.9 Small particles can erode through, and remain in, mucous membranes subepithelially causing visible discoloration. In certain instances, clinical symptoms of argyrosis can be mistaken for other conditions including primary acquired melanosis or even melanoma.10 It should be noted that ocular argyrosis is mainly a cosmetic problem; it does not cause vision loss.5 Nevertheless, this disease can be mistaken for a neoplastic process and should be included in the differential diagnosis of conjunctival pigmented lesions.
Acknowledgments
Melinda Swift for X-Ray energy spectrum data (Pathology and Laboratory Services, Duke University Health System, Durham NC)
Funding: NIH NIDA Core Center of Excellence P30 Grant
Footnotes
The authors have no pertinent conflict of interest or financial disclosures.
References
- 1.Stafeeva K, Erlanger M, Velez-Montoya R, et al. Ocular argyrosis secondary to long-term ingestion of silver nitrate salts. Clin Ophthalmol. 2000;6:2033–2036. doi: 10.2147/OPTH.S37898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Calvery H, Lightbody H, Rones B. Effects of some silver salts on the eye. Arch Ophthalmol. 1941;25:839–847. [Google Scholar]
- 3.Al-Talib R, Wright H, Theaker J. Orange‐red birefringence of gold particles in paraffin wax embedded sections. Histopathol. 1994;24:176–178. doi: 10.1111/j.1365-2559.1994.tb01300.x. [DOI] [PubMed] [Google Scholar]
- 4.Kubba A, Kubba R, Batrani M, et al. Argyria an unrecognized cause of cutaneous pigmentation in Indian patients: A case series and review of the literature. Indian J Dermatol Ve. 2013;79:805–811. doi: 10.4103/0378-6323.120735. [DOI] [PubMed] [Google Scholar]
- 5.Hanna C, Fraunfelder F, Sanchez J. Ultrastructural study of argyrosis of the cornea and conjunctiva. Arch Ophthalmol. 1974;92:18–22. doi: 10.1001/archopht.1974.01010010022006. [DOI] [PubMed] [Google Scholar]
- 6.Jensen S. Argyrosis of conjunctiva in studio photographer. Acta Ophthalmol. 1962;40:544–547. doi: 10.1111/j.1755-3768.1962.tb07828.x. [DOI] [PubMed] [Google Scholar]
- 7.Gallardo M, Randleman J, Price K, Johnson D, et al. Ocular argyrosis after long-term self-application of eyelash tint. Am J Ophthamol. 2006;141:198–200. doi: 10.1016/j.ajo.2005.07.054. [DOI] [PubMed] [Google Scholar]
- 8.Spencer W, Garron L, Contreras F, Hayes T, et al. Endogenous and exogenous ocular and systemic silver deposition. T Ophthal Soc UK. 1980;100:171–178. [PubMed] [Google Scholar]
- 9.Pala G, Fronterré A, Scafa F, et al. Ocular argyrosis in a silver craftsman. J Occup Health. 2008;50:521–524. doi: 10.1539/joh.n8001. [DOI] [PubMed] [Google Scholar]
- 10.Zografos L, Uffer S, Chamot L. Unilateral conjunctival-corneal argyrosis simulating conjunctival melanoma. Arch Ophthalmol. 2003;121:1483–1487. doi: 10.1001/archopht.121.10.1483. [DOI] [PubMed] [Google Scholar]


