Abstract
To evaluate hospitalization rates and causes among human immunodeficiency virus (HIV) patients in the late highly active antiretroviral therapy (HAART) era. Data during the years 2000 to 2012 were obtained from hospital/clinical charts. Hospitalizations were defined as a ≥24 hours hospital admission. Obstetric admissions were excluded. Causes of hospitalizations were defined as acquired immune deficiency syndrome (AIDS)-defining illnesses, AIDS-related diseases (HAART adverse events, metabolic complications and non-AIDS-defining tumors/infections), and non-HIV-related diseases. Hospitalization rates are presented as admissions per 100 patient years. The number of HIV patients (58% males) in our center increased from 521 in 2000 to 1169 in 2012. 1676 hospital admissions (in 557 patients) were observed during the years of the study. The mean number of admissions per hospitalized patient was 3 ± 3.39. Hospitalization rates of HIV patients declined significantly (18.4/100 in 2000, 9/100 patient years in 2012; P = .0001), but it was higher than the rates reported in the Israeli general population (X8.76 in 2000, X6.04 in 2012). Furthermore, hospitalizations for AIDS-defining illness declined (from 46.9% to 16.1%) whereas non-HIV-related hospitalizations increased (from 31.3% to 60.1%). Lower cluster of differentiation 4 (CD4) cell counts and older age, at the time of HIV diagnosis, were associated with higher rates of admissions (especially for AIDS-defining illnesses) and mortality. Hospitalization rates of HIV patients, especially for AIDS-defining illness, continue to decline in the late HAART era despite the increasing age of the patients, though it is still higher than that of the general population. Low CD4 cell counts and older age, at the time of HIV diagnosis, are associated with readmissions and mortality.
Keywords: age, AIDS-defining illness hospitalizations, CD4, HIV-related hospitalizations, hospital admission of HIV patients, viral load
1. Introduction
Highly active antiretroviral therapy (HAART) has been shown to reduce human immunodeficiency virus (HIV)/acquired immune deficiency syndrome (AIDS)-related morbidity and mortality.[1] Accordingly, previous studies reported a reduction in hospitalization rates by 20% to 40% in North America and Europe following the availability and the advanced usage of HAART in those continents.[2,3] However, as a result of their prolonged survival, HIV patients may suffer from a variety of medical problems (related and not related to HIV) such as adverse effects of prolonged exposure to HAART medications, coinfection with viral hepatitis (B and C), hypertension, diabetes mellitus, and cardiovascular diseases.[4] The latter medical problems may increase the morbidity of HIV patients and their need for hospitalizations. Indeed, after the first years of HAART availability, in the late HAART era, several studies reported that hospitalization rate of HIV patients started to increase, mainly for non-AIDS defining illnesses.[5] On the other hand, other studies did not report such a rise in hospitalization rate among HIV patients.[6,7] In Israel, HAART is available, free of charge, since 1997. The aim of the present study was to evaluate the rates of hospitalizations of HIV patients, their causes and trends over the years of the late HAART era (during the years 2000–2012) in a major HIV/AIDS center in Israel.
2. Patients and methods
2.1. Patients
The study is a retrospective cohort study of all patients with HIV/AIDS, who were treated in “Neve-Or” HIV/AIDS center (Kaplan Medical Center, Rehovot, Israel) during the years 2000 to 2012. Kaplan Medical Center is a secondary hospital, serving mainly urban population. The study was approved by the Kaplan Medical Center ethic committee. HIV was diagnosed by enzyme-linked immunosorbent assay and confirmed by Western Blot analysis. Cluster of differentiation 4 (CD4) cell counts were determined by fluorescence-activated cell sorting using fluorescein iisothiocyanate-conjugated monoclonal antibodies (IQ Products, Groningen, Netherlands).[8] HIV viral load (VL) was determined by the COBAS Ampliprep/COBAS AMPLICOR HIV-1 MONITOR Test, version 1.5 (CAP/CA; Roche Molecular Systems, Branchburg, NJ).[9] HIV-1 subtypes were determined by the REGA HIV-I subtyping tool (www.hivdb.sanford.edu/hiv). Viral load below 400 copies/mL was defined as lower detection limit (LDL). Immunocompetent patients were defined as patients with CD4 cell count above 500 cells/μL.
For each enrolled patient, we obtained all epidemiological (age, gender, mode of HIV acquisition) data. Most of our patients were immigrants from Ethiopia who acquired their HIV via heterosexual contacts. Males who have sex with males (MSMs) and intravenous drug users (IVDU) were mainly Israeli patients. Immunological (CD4 cell counts), virological (VL) and clinical data were obtained at diagnosis and every 1 to 3 month thereafter (according to the clinical status of the patients). Along the years of the study, the indications for treatment and the recommended regiments were changed several times. In our center, we treat our patients according to the European guidelines. In the first years of the study, standard HAART was based on nonnucleoside reverse transcriptase inhibitors and 2 nucleoside analog reverse transcriptase inhibitors. Later, Ritonavir boosted Protease inhibitor based regiment was the recommended treatment. In the last 3 years of the study, HAART based on integrase inhibitor became the standard treatment. In Israel, HAART was provided free of charge for all HIV patients according to the clinical guidelines since 1997.
2.2. Hospitalizations data collection
Hospitalizations were defined as a ≥24 hours admission to an inpatient hospital department. Obstetric admissions were excluded. Data were obtained from patients’ clinics and hospital charts (including hospital discharge). In patients with more than 1 hospital admission, each admission was evaluated separately. The main cause (diagnosis according to the International Statistical Classification of Diseases 9 [ICD9] system codes) for each hospital admission was characterized as AIDS-defining illness according to the Centers for Disease Control and Prevention criteria[10]; HIV related: medications adverse events, disorders related to HIV such as cytopenias (hemoglobin <10 g/dL, white blood cells <1500 cells/μL, platelets <50,000 cells/μL), tumors (non-AIDS defining), non-AIDS defining infections in immunocompromised hosts and metabolic disorders related to HIV such as renal disease, liver disease, heart disease, cerebrovascular accident, hyperglycemia, and osteoporotic fractures; non-HIV-related diseases: infections in immunocompetent hosts, elective surgical procedures, trauma, chronic lung disease exacerbations, and nonspecific chest pain. Each hospitalization (chart and ICD9 diagnosis) was evaluated separately by the same 2 investigators. In the case of disagreement, the issue was resolved following discussion with the principle investigator.
Hospitalization rate was calculated as the number of hospital admissions per 100 patient years for each year of the study. Hospitalization rates of the general population were obtained from the Israeli ministry of health report.[11]
2.3. Statistical analysis
Data are presented as average ± standard deviation. Student t test, Fisher Exact test, and Chi-square tests were used for statistical analysis. P ≤ .05 was considered statistically significant. For multiple comparisons, we used alpha adjustments. Backward stepwise logistic regression analysis was conducted to identify association between the independent variables (sex, age, way of HIV acquisition, CD4 and VL at the time of HIV diagnosis), and dependent variable (death).
2.4. Results
The number of HIV patients in our center increased from 521 in 2000 to 1169 patients in 2012, overall 10,884 patient years. As can be seen in Table 1, more than half (58%) of the cohort patients were males. The ratio of males to females did not change significantly along the years of the study. The average age of our entire cohort increased from 36.7 ± 17.1 years at 2000 to 47.06 ± 11.8 years at 2012. Most of the patients were heterosexual immigrants from Ethiopia (64%). Israeli MSMs were 15% of the cohort. In 10% of the patients, the mode of HIV acquisition was not defined. At the time of diagnosis, the VL of our patients was 279,285 ± 689,577 copies/mL (32% of the patients presented with VL above 100,000 copies/mL), and the average CD4 cell counts of was 285 ± 206 cells/μL (40% of the patients presented with CD4 cell counts below 200 cells/μL) (Table 1). The average VL as well as the average CD4 at the time of HIV diagnosis did not change significantly along the years of the study.
Table 1.
Demographic, clinical, immunological and virological characteristics of the entire Kaplan hospital HIV cohort and the 557 hospitalized patients.
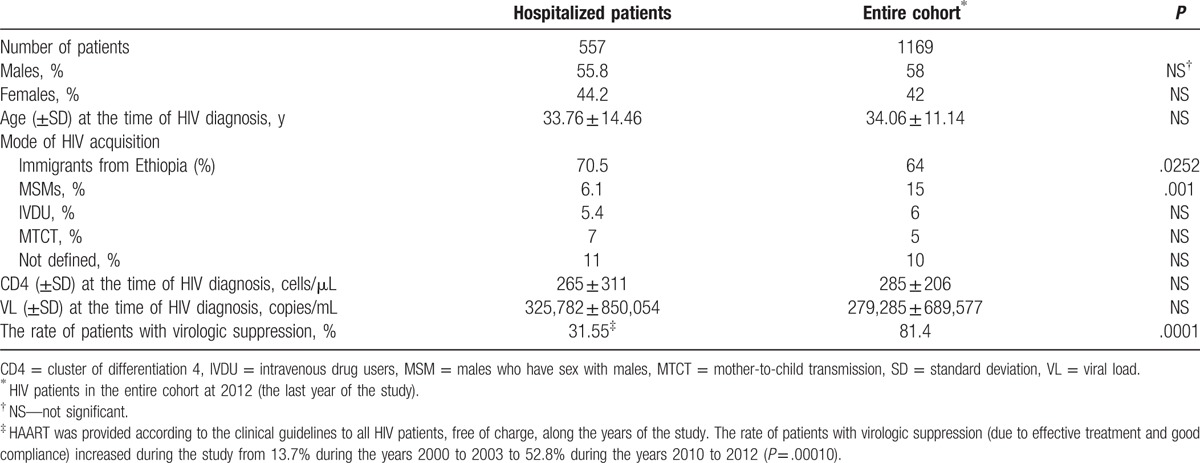
Five hundred fifty seven of our patients were hospitalized, at least once, during the years of the study. The total number of hospitalizations was 1676. The average age of the patients at the time of HIV diagnosis (34.4 ± 15.6 years for patients admitted at 2000 and 36.3 ± 17.7 years for patients admitted at 2012) was not significantly different from the average age of the entire cohort. As can be seen in Table 1, there were significantly more heterosexual immigrants from Ethiopia and less MSMs among the hospitalized patients as compared to the entire cohort.
Sixty three out of 557 hospitalized patients (11%) were newly diagnosed with HIV during their hospitalization. The rate of new HIV diagnosis during admissions did not change significantly during the years of the study.
The average age of the hospitalized patients at the time of admission was 41.6 ± 15.8 (range 0.3–85) years. The average age at the time of admission increased from 36.9 ± 16.8 years at 2000 to 45.1 ± 13.2 years at 2012. Most (75%) of the hospital admissions were in medical departments, 12.5% in surgical departments, 7.6% in the pediatric departments (patients ≤16 years of age), 3.9% in the department of gynecology, and 1% in the intensive care unit. The ratio of medical/surgical admissions did not change significantly along the years of the study. The average length of hospital admission was 7.5 ± 8.2 days without significant change during the years of the study.
The main causes (diagnosis) for the 1676 hospital admissions of our patients along the entire study years were AIDS-defining illness in 449 hospitalizations (26.8%), HIV-related disease in 456 (27.2%), and non-HIV related in 771 (46%) hospitalizations. The main causes for AIDS-defining illnesses hospitalizations were non-Hodgkin lymphoma (Ly) (17.4%), pneumocystis jiroveci pneumonia (PCP) (15.9%), tuberculosis (TB) (14.8%), and recurrent pneumonia (14.6%), whereas the main causes of HIV-related diseases hospitalizations were infectious diseases (46.9%), gastrointestinal diseases (14.4%), cytopenia (anemia, leukopenia or thrombocytopenia) (11.5%), and drug reactions (7.1%). Non-HIV-related hospitalizations were because of infections in immunocompetent patients, elective surgical procedures, trauma, nonspecific chest pain, nonspecific abdominal pain, and exacerbations of chronic lung disease. There was no significant change in the ratio of surgical and medical adhesions along the years of the study.
As can be seen in Fig. 1, the hospitalization rate of our HIV patients declined dramatically (by 50%) during the study period (from 18.4 in 2000 to 9 hospitalizations per 100 patient years in 2012; P = .0001). However, it was still higher than the rate reported in the Israeli general population. During the years of the study, hospitalization rates of the general population (matched for gender, age, and calendar year) declined from 2.1/100 person years at 2000 to 1.49/100 person years at 2012 (29% reduction).[11] Thus, the reduction in hospitalization rates during the years of the study was greater in our patients (50% vs 29%). Nevertheless, the hospitalization rate of our HIV patients was much higher (X8.76 in 2000, X6.04 in 2012) than that of the general population.
Figure 1.
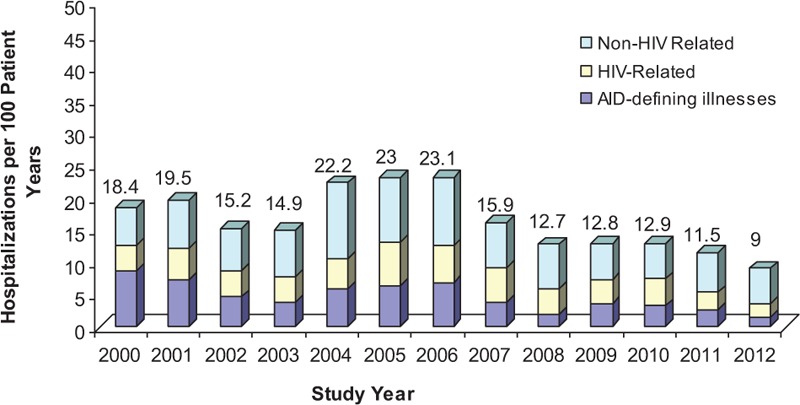
Hospitalization rates of human immunodeficiency virus (HIV) patients during the years 2000 to 2012. The hospitalization rates, defined as the number of hospital admissions per 100 patient years for each of the study years, declined significantly during the years of the study (from 18.4/100 patient years in 2000 to 9/100 patient years in 2012; P = .0001). Hospitalizations for acquired immune deficiency syndrome (AIDS)-defining illness declined (from 46.9% in 2000 to 16.1% in 2012; P = .0001), whereas non-HIV-related hospitalizations increased (from 31.3% in 2000 to 60.1% in 2012; P = .0001) along the study period. Hospitalizations due to HIV-related diseases remained stable (20%). AIDS-defining illnesses and HIV-related diseases as defined in Section 2.2.
In addition to the significant reduction in hospitalization rates of our HIV patients along the years of the study (Fig. 1), there was also a significant change in the causes for hospitalizations. Thus, during the years of the study hospitalizations for AIDS-defining illnesses declined significantly (P = .0001), whereas the non-HIV-related hospitalizations significantly increased (P = .0001). The rate of HIV-related hospitalizations was stable (Fig. 1). The reduction in hospitalizations for TB and PCP along the years of the study clearly demonstrated the decline of AIDS-defining illnesses as a major cause for hospitalization of HIV patients (Fig. 2).
Figure 2.
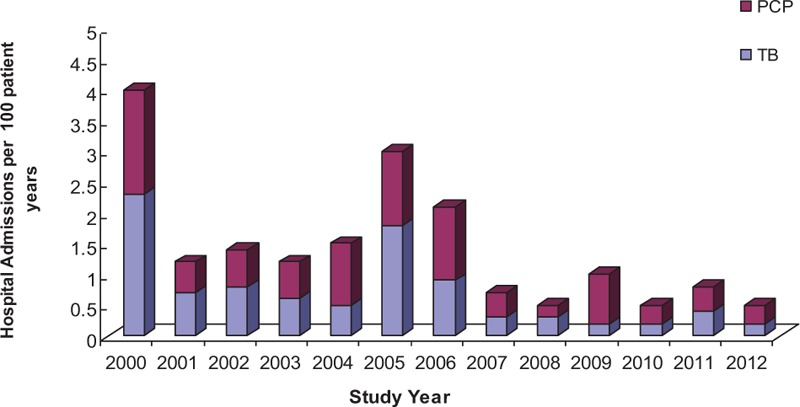
The rate of hospitalizations (per 100 patient years) due to tuberculosis (TB) and pneumocystis jiroveci pneumonia (PCP) along the years of the study (2000–2012). Hospitalizations due to TB declined from 2.3/100 patient years at 2000 to 0.2/100 patient years at 2012 (P = .0001). Concomitantly, hospitalizations for PCP declined from 1.7/100 patient years (2000) to 0.3/100 patient years at 2012 (P = .002).
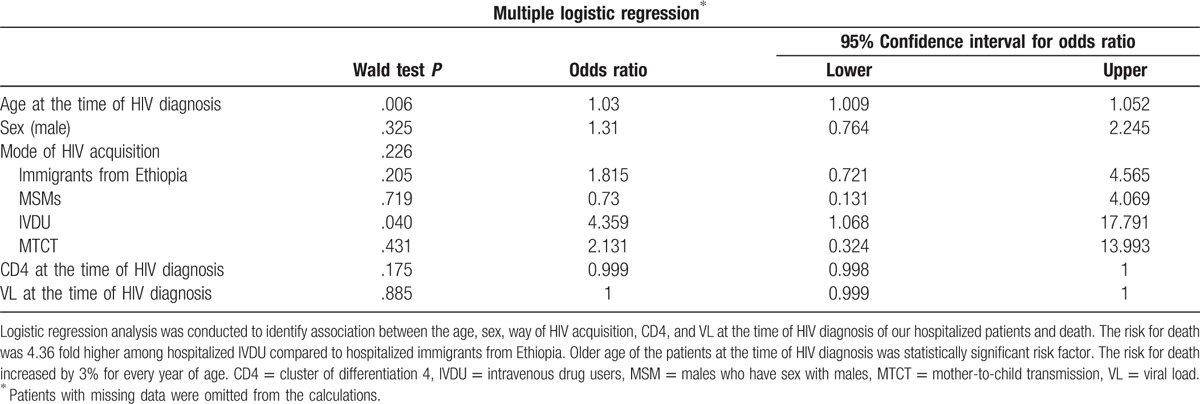
One hundred sixteen (20.8%) of our hospitalized patients died during the years of the study. The causes of death were AIDS-defining Illnesses in 44.8%, HIV-related diseases in 41.3%, and other reasons (trauma and suicide) in 13.8% of the patients. The average age, at the time of HIV diagnosis of the patients who died was significantly higher than that of the patients who did not die (38.7 ± 15.07 vs 32.12 ± 14.01 years, P = .0001). The mortality rate of patients who were presented with low CD4 cell counts (<200 cells/μL) was 25.7%, compared to 15.3% in patients with initial CD4 cell counts between 201 and 350 cells/μL and 13.5% in patients with high (>350 cells/μL) CD4 cells count at the time of diagnosis (P = .006 comparing CD4 201–350 cells/μL to CD4 > 350 cells/μL; significant after alpha adjustment). The mean CD4 cell counts, at the time of HIV diagnosis, were significantly lower in the patients who died during the study as compared to the patients who did not 212.2 ± 222.13 vs 298.3 ± 327.26 cells/μL; P = .0076). Apart from CD4 cell counts and the age of the patients at the time of diagnosis, more hospitalized males (as compared to females) died during the years of the study (P = .0045). The mortality was also higher among IVDU (P = .0368). As can be seen in Table 2, following logistic regression analysis, only the age of the patients at the time of diagnosis was a significant risk factor for death among our hospitalized patients (P = .0001).
Table 2.
Statistical analysis of HIV infected hospitalized patients mortality.
The 557 hospitalized patients were admitted 1676 times during the period of the study. Thus, the mean number of hospital admissions per hospitalized patient was 3 ± 3.39 (range 1–24). Readmissions were more common among male patients (3.19 ± 3.77 vs 2.77 ± 2.83; admissions per hospitalized males and females, respectively; P = .001). As can be seen in Fig. 3, 350 (63%) of the hospitalized patients were admitted 1 to 2 times, 139 (25%) were admitted 3 to 5 times, and 68 patients were admitted 6 times or more during the years of the study. The mortality rate was significantly higher in patients who were admitted more than twice during the years of the study (mortality rate of 14.3%, 27.3%, and 41.2% mortality rate for patients with 1–2, 3–5, and ≥6 hospital admissions; respectively) (Fig. 3). Moreover, the number of admissions per patient was significantly related to the CD4 cell counts of the patients at the time of HIV diagnosis. Thus, the mean number of hospital admissions per patient with low CD4 cells counts (<200 cells/μL), at the time of HIV diagnosis, was higher (3.58 ± 3.91) than that of patients with higher CD4 cell counts (>200 cells/μL) (2.81 ± 3.20; P = .0019). In addition, hospitalizations due to AIDS-defining illnesses were significantly more common (32.4%) among patients with low CD4 (<200 cells/μL) at the time of HIV diagnosis as compared to patients who were presented with CD4 cell counts of 200 to 350 cells/μL (20.3%; P = .0004), or with CD4 cell counts above 350 cells/μL (21.9%; P = .0001 compared to patients with CD4 < 200 cells/μL; significant after alpha adjustment).
Figure 3.
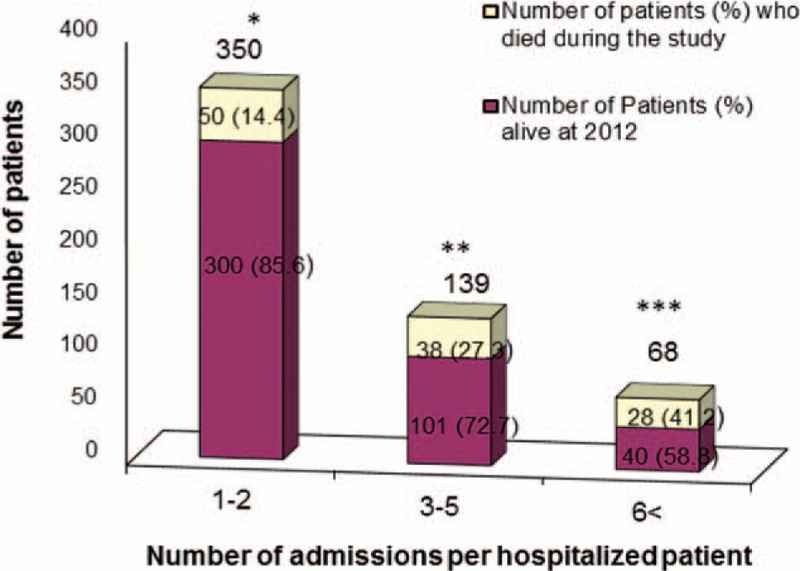
Mortality rate according to the number of hospital admissions per hospitalized patient. A total of 350 patients were hospitalized 1 to 2 times, 139 patients were admitted 3 to 5 times, and 68 patients were admitted 6 or more times during the years of the study. The mortality rates increased significantly with the number of hospital admissions. Thus, the number of patients who died during the study was 50 (14.3%), 38 (27.3%), 28 (41.2%) in patients with 1–2, 3–5, ≥6 hospital admissions, respectively. ∗P = .0001 mortality rate for patients with 1 to 2 hospital admissions versus mortality rate for patients with ≥6 hospital admissions, significant after alpha adjustment. ∗∗P = .001 mortality rates for patients with 1 to 2 hospital admissions versus mortality rate for patients with 3 to 5 hospital admissions, significant after alpha adjustment. ∗∗∗P = .056 mortality rate for patients with 3 to 5 versus comparing mortality rate for patients with ≥6 hospital admissions.
The CD4 cell counts at the time of hospital admissions were also associated with the rate and causes of hospitalization. More than half (58.4%) of the hospitalizations occurred in patients with CD4 cell counts below 200 cells/μL. CD4 cells counts above 350 cells/μL (at the time of admission) were observed in only 25% of the hospitalized HIV patients. Moreover, hospitalizations due to AIDS-defining illnesses were observed in 43.8% of the patients who were admitted with low CD4 cell counts (<200 cells/μL) compared to 13.3% in patients admitted with CD4 cell counts of 200 to 350 cells/μL (P = .0001) and 9.3% in patients admitted with high CD4 cell counts (>350 cells/μL; P = .0001) (Fig. 4) (significant after alpha adjustment).
Figure 4.
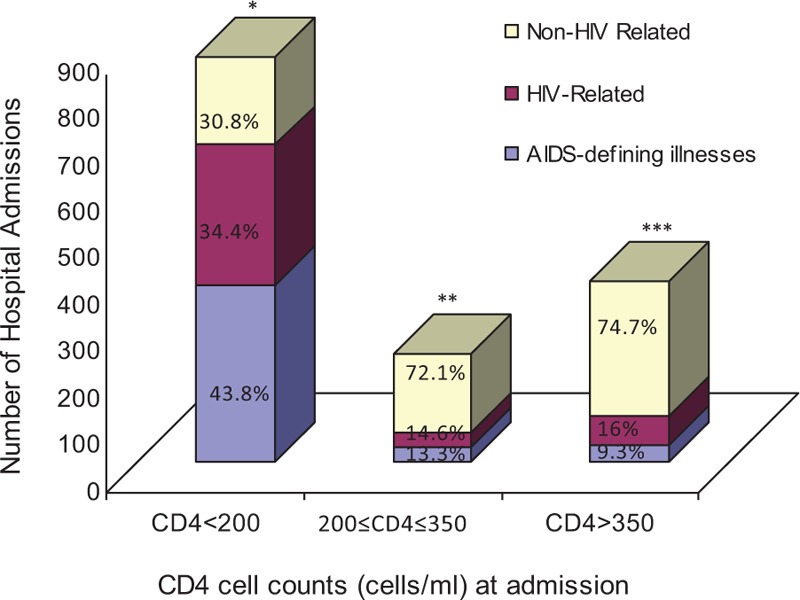
Number of hospital admissions and their causes as related to the cluster of differentiation 4 (CD4) cell counts at the time of hospitalization. Higher rates of hospitalizations due to acquired immune deficiency syndrome (AIDS)-defining illnesses and human immunodeficiency virus (HIV)-related diseases were observed in patients with low CD4 cells count (<200 cells/μL) at the time hospital admission (43.8%, 34.4%; for AIDS-defining illness and HIV-related diseases, respectively) compared to patients who were admitted with CD4 cell counts 201 to 350 cells/μL, (13.3%, 14.6% for AIDS-defining illness and HIV-related diseases, respectively) or with CD4 > 350 cells/μL (9.3%, 16% for AIDS-defining illness and HIV-related diseases, respectively). In contrast, non-HIV-related admissions were more common in patients with higher CD4 cell counts at the time of admission (30.8%, 72.1%, 74.7% for patients with CD4 cells count of <200 cells/μL, 201–350 cells/μL, >350 cells/μL; respectively). ∗P = .0001 comparing AIDS-defining illness in patients with CD4 < 200 cells/μL, versus CD4 201 to 350 cells/μL, significant after alpha adjustment. ∗∗P = .109 comparing AIDS-defining illness in patients with CD4 201 to 350 cells/μL versus CD4 > 350 cells/μL. ∗∗∗P = .001 comparing AIDS-defining illness in patients with CD4 < 200 cells/μL, versus CD4 > 350 cells/μL, significant after alpha adjustment.
In addition, VL at the time of admission was also associated with the rate and causes of hospitalization. More than half (67.1%) of the hospitalizations occurred in patients with detectable VL in their sera (>400 copies/mL). On the other hand, undetectable VL (<400 copies/mL) at the time of admission was observed in only 32.9% of the patients. Moreover, hospitalizations due to AIDS-defining illnesses were observed in 35.5% of the patients who were admitted with detectable VL as compared to 12.13% in patients admitted with undetectable VL (P = .0001). Along the years of the study, the rate of hospitalized patients with LDL viral load increased significantly from an average of 13.7% during the years 2000 to 2003 to an average of 52.8% during the years 2010 to 2012 (P = .00010).
3. Discussion
The main findings of the present study are that the rate of hospitalizations of HIV patients in the late HAART era (2000–2012) continued to decrease from 18.4 (in 2000) to 9 (in 2012) per 100 patient years, though it was still higher than the rate reported for the general Israeli population (X6.04 in 2012). Furthermore during the years of the study, hospitalizations for AIDS-defining illnesses declined, whereas non-HIV-related hospitalizations increased.
The expansion of access to antiretroviral medications in the early HAART era has led to a substantial decrease in HIV-related mortality and morbidity (including hospitalization rates).[1,3] Trends in HIV patient's hospitalization rates during the late HAART era are not yet defined. Some studies reported an increasing rate of hospitalizations due to the aging of HIV patients, long-term HAART toxicity, and the development of chronic diseases (e.g., heart, lung, and liver disorders).[5,12–14] Hospitalization rates may be a sensitive indicator, better than mortality, for antiretroviral treatment efficacy.[5] In addition, hospitalizations are an important component of healthcare costs of HIV patients.[15] Thus, it is indeed an important clinical outcome in HIV medicine.[14] Our large cohort study (1169 patients; 10,884 patient years; 2000–2012) analyzed 1676 hospitalizations of HIV patients in a major HIV center in Israel during the late HAART era. We included in our study all patients diagnosed with HIV, regardless to their engagement to care or HAART adherence. Thus, our results demonstrate the true hospitalization rates of the entire HIV population.[11,16,17]
The hospitalization rate of our HIV patients declined by 50% during the years of the study (from 18.4 in 2000 to 9 in 2012 per 100 patient years; Fig. 1). This decline was observed despite the ageing (about 10 years) of our cohort patients. Similar trend was observed by other studies.[4,6,13,18] Consistent decline of hospitalization rates was observed since 2007 (Fig. 1) which most probably resulted from the scale up of HAART implantation.[4] The hospitalizations rates observed in our study were similar to those reported for HIV patients in studies from Italy and the Unites States[14,17] but were much higher (X8.76 in 2000, X6.04 in 2012) than the rates reported by the Israeli ministry of health for gender and age-matched general population.[11] We did not find any gender differences in hospitalization rates, though in other studies[5,12] the hospitalization rates of females with HIV were higher than that of the males. It should be noted that, in our cohort, the rate of hospitalizations was relatively high in heterosexual immigrants from Ethiopia (males and females) and lower in the MSMs group of patients. This is most probably due to differences in linkage to care and HAART adherence between these 2 groups of patients.[7,12,19]
The reduction in hospitalization rates originated mainly from the improvement of HIV care including HAART availability, adherence to treatment, and the usage of better (higher efficacy with lower short and long-term toxicity) antiretroviral drugs. Indeed, the rate of hospitalized patients who achieved virological suppression (LDL) increased from an average of 13.7% during the years 2000 to 2003 to an average of 52.8% during the years 2010 to 2012. Higher hospitalization rates, including AIDS-defining hospitalization rates, were observed in patients with lower CD4 at the time of HIV diagnosis. However, the fact that that the average CD4 cell counts (in the entire cohort) did not change significantly along the years of the study indicates that earlier diagnosis (with better immunological status) was not the major cause for the reduction rate of hospitalizations. Moreover, the fact that new HIV diagnosis during hospitalization did not decrease along the years of the study and also suggest that earlier HIV diagnosis was not the main reason for hospitalization risk reduction in our study. The rise in cardiovascular, malignancy, and metabolic disorders appeared to have a lower than expected influence on hospitalization rates.[20,21] Future study of our cohort, 10 to 15 years ahead, is needed in order to evaluate the effects of the latter disorders on hospitalization rates among ageing HIV patients.
The average length of hospital stay in our study was 7.5 ± 8.2 days without a significant change during the years. This is similar to the report from United Kingdom.[17] In contrast, longer hospital stay was reported in Italy (16 days)[17] and in Portugal (10 days in 2010).[13] The length of stay in the latter 2 studies most probably reflects different hospitalization policies in Italy and Portugal as compared to policies used in Israel and the United Kingdom.[22]
About a quarter (26.8%) of all hospital admissions were due to AIDS-defining illnesses.[10] As was reported by others,[7,13,16,17,23] the main causes for AIDS-defining illnesses hospitalizations were: Ly, PCP, TB, and recurrent pneumonia. Another quarter of hospitalizations were due to HIV-related diseases (mainly non-AIDS-related infections). Studies from Barcelona,[16] United Kingdom, and Italy[17] reported similar percentage of hospitalizations due to AIDS-defining illnesses. Higher percentages of hospital admissions due to AIDS-defining illnesses were noted in south Brazil (40%)[23] and in a worldwide meta-analysis (46%).[18] This difference is probably the result of differences in the availability of HIV care in different countries.
Along with the significant reduction in hospitalizations rates, a clear shift in the causes for hospitalizations was observed. Thus, during the years of the study, hospitalizations for AIDS-defining illnesses declined (from 46.9% to 16.1%), whereas the non-HIV-related hospitalizations increased (from 31.3% to 60.1%) (Fig. 1). The significant reduction in hospitalizations for TB and PCP clearly demonstrates the decline of AIDS-defining illnesses as a major cause for hospitalization in our HIV patients (Fig. 2). Similar reduction in hospitalizations due to AIDS-defining illnesses in the late HAART era was observed in Brazil, France, and the United States.[2,4–6,18,24,25] The rate of hospitalizations for PCP in 2000 in our study (1.7/100 patient years) was lower than the rate reported in the United States (3.9/100 person years)[24] but higher than the EUROSIDA report (0.3/100 person years).[25] This reflects differences in HIV care, HAART availability and adherence to treatment as well as the immunological status (CD4 cell counts) of the patients at the time of HIV diagnosis and during the follow-up period in different parts of the world.
As was also shown by others,[2,5–7,14,26,27] the status of the immune system of HIV patients has a significant effect on hospitalizations. Thus, patients with low CD4 cell counts at the time of HIV diagnosis had a higher rate of hospitalizations. Moreover, a relatively high portion of admissions of the later patients was due to AIDS-defining illnesses, whereas most (74.7%) admissions of patients with CD4 cell counts above 350 cells/μL were due to non-HIV-related diseases (Fig. 4). The mean number of hospital admissions per patient along the years of the study was 3 ± 3.39 (range 1–24). Sixty eight of our patients (5.8% of the entire cohort; 12% of hospitalized patients) were hospitalized 6 or more times. Readmissions were associated with impaired immunological status (low CD4 cell counts) and with high rate of mortality (Fig. 3). Similar to other studies, we evaluated the immune system function by CD4 cell counts. It should be noted that recent studies had suggested that CD4/CD8 ratio, rather than CD4 cell counts alone, may be used as a better marker for the function of the immune system and morbidity in HIV patients.[28,29]
One hundred sixteen (20.8%) of our patients died during the years of the study. As was previously shown by us and by others[1,27,30] older age at the time of diagnosis was an independent risk factor for death. Not surprisingly, as was also reported by others,[23] mortality was higher among patients who were hospitalized 3 or more times during the years of the study (Fig. 3).
In our study, 63 patients (5.3% of the entire HIV cohort; 11.3% of the hospitalized patients) were newly diagnosed with HIV at the time of hospital admission. Other studies report even higher rate (up to 33%) of new HIV diagnosis at the time of admission.[18] This highlights the mandatory need for a more effective community-based HIV testing programs in order to decrease HIV-related mortality and morbidity.
The present study has several limitations. First, it is a single center retrospective cohort study. Other AIDS centers with different types of patients (e.g., more MSMs or IVDU) may reveal different trends of hospitalizations. Moreover, patients in AIDS centers who do not have good access to HAART will demonstrate, most likely, higher rates of hospitalizations including AIDS-defining illnesses. Second, other HIV/AIDS medical centers may have different admission criteria, with higher or lower thresholds for hospitalization of HIV patients. This, indeed, will change the absolute rate of HIV hospitalizations but should not affect the hospitalization trends (decrease in hospitalization rates and change in their causes in the late HAART era). Third, our study did not include psychiatric hospitalizations that were shown to be important in other studies.[4,13] In addition, one cannot exclude the possibility that we missed some hospitalizations of our patients in remote hospitals. The latter is quite unlikely since we obtained hospitalization data not only from hospital charts, but also from our clinic charts. In any case, we used the same data collection system throughout the study; thus, the decrease in hospitalizations rate is valid. Moreover, we present here a large cohort of patients with a relatively long follow-up period (10,884 patient years) and 1676 hospitalizations that support the validity of our results.
To conclude, the hospitalization rates, especially those due to AIDS-defining illnesses of HIV patients, decreased significantly in the late HAART era. However, the rate is still higher than that of the general population. Patients with low CD4 cell counts, older patients, and those with recurrent hospitalizations should be followed more intensively to enforce their linkage to medical care and HAART adherence.
Footnotes
Abbreviations: AIDS = acquired immune deficiency syndrome, CD4 = cluster of differentiation 4, HAART = highly active antiretroviral therapy, HIV = human immunodeficiency virus, ICD9 = International Statistical Classification of Diseases 9, IVDU = intravenous drug user, Ly = lymphoma, MSM = male who have sex with male, PCP = pneumocystis jiroveci pneumonia, TB = tuberculosis, VL = viral load.
KM-G and IA have contributed equally to the article.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Mocroft A, Ledergerber B, Katlama C, et al. Decline in the AIDS and death rates in the EuroSIDA study: an observational study. Lancet 2003;362:22–9. [DOI] [PubMed] [Google Scholar]
- [2].Buchacz K, Baker RK, Moorman AC, et al. Rates of hospitalizations and associated diagnoses in a large multisite cohort of HIV patients in the United States, 1994–2005. AIDS 2008;22:1345–54. [DOI] [PubMed] [Google Scholar]
- [3].Mocroft A, Barry S, Sabin CA, et al. The changing pattern of admissions to a London hospital of patients with HIV: 1988–1997. Royal Free Centre for HIV Medicine. AIDS 1999;13:1255–61. [DOI] [PubMed] [Google Scholar]
- [4].Berry SA, Fleishman JA, Moore RD, et al. Trends in reasons for hospitalization in a Multisite United States Cohort of Persons Living with HIV, 2001–2008. J Acquir Immune Def Syndr 2012;59:368–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Krenz HB, Dean S, Gill MJ. Longitudinal assessment (1995–2003) of hospitalizations of HIV-infected patients within a geographical population in Canada. HIV Med 2006;7:457–66. [DOI] [PubMed] [Google Scholar]
- [6].Luz PM, Bruyand M, Ribeiro S, et al. AIDS and non-AIDS severe morbidity associated with hospitalizations among HIV-infected patients in two regions with universal access to care and antiretroviral therapy, France and Brazil, 2000–2008: hospital-based cohort studies. BMC Infect Dis 2014;14:278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Bachhuber MA, Southern WN. Hospitalization rates of people living with HIV in the United States, 2009. Public Health Rep 2014;129:178–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].http://aidsinfo.nih.gov/guidelines/html/1/adult-and-adolescenttreatmentguidelines/0.AIDSinfo [April 8, 2015]. [Google Scholar]
- [9].Ferrara GB, Strelkauskas AJ, Longo A, et al. Markers of human T cell subsets identified by alloantisera. J Immunol 1979;123:1272–7. [PubMed] [Google Scholar]
- [10].Schneider E, Whitmore S, Glynn KM, et al. Centers for Disease Control and Prevention (CDC). Revised surveillance case definitions for HIV infection among adults, adolescents, and children aged < 18 months and for HIV infection and AIDS among children aged 18 months to <–13 years—United States, 2008. MMWR Recomm Rep 2008;57:1–2. [PubMed] [Google Scholar]
- [11].Haklai Z, Meron J, Aburba M, et al. Hospitalization in internal medicine departments in Israel 2000–2012. Jerusalem, Israel: Ministry of Health. Information Health Division; 2013. [Google Scholar]
- [12].Fleishman JA, Yehia BR, Moore RD, et al. Disparities in receipt of antiretroviral therapy among HIV-infected adults (2002–2008). Med Care 2012;50:419–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Catumbela E, Freitas A, Lopes F, et al. HIV disease burden, cost, and length of stay in Portuguese hospitals from 2000 to 2010: a cross-sectional study. BMC Health Ser Res 2015;15:144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Crum-Ciaflone N, Granditis G, Echoles S, et al. Trends and causes of hospitalizations among HIV-infected persons during the late HAART era: what is the impact of CD4 count and HAART use? J Acquir Immune Defic Syndr 2010;54:248–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Schackman BR, Gebo KA, Walensky RP, et al. The lifetime cost of current human immunodeficiency virus care in the United States. Med Care 2006;44:990–7. [DOI] [PubMed] [Google Scholar]
- [16].Vallecillo G, Moyal S, Torrens M, et al. Antiretroviral therapy (ART) use, human immunodeficiency virus (HIV-1) RNA suppression, and medical causes of hospitalization among HIV-infected intravenous drug users in the late ART era. Open Forum Infect Dis 2014;1:ofu010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Cenderello G, Tittle V, Pasa A, et al. Inpatient admissions of patients living with HIV in two European centres (UK and Italy); comparisons and contrasts. J Infect 2015;70:690–4. [DOI] [PubMed] [Google Scholar]
- [18].Ford N, Shubber Z, Meintjes G, et al. Causes of hospital admission among people living with HIV worldwide: a systematic review and meta-analysis. Lancet HIV 2015;2:e438–44. [DOI] [PubMed] [Google Scholar]
- [19].Elbirt D, Asher I, Broda K, et al. Israeli-migrants from sub-Saharan Africa (Ethiopia) and HIV: medical and social issues—the experience of one major HIV center. Int Public Health J 2010;2:329–37. [Google Scholar]
- [20].Palella FJ, Phair JP. Cardiovascular disease in HIV infection. Curr Opin HIV AIDS 2011;6:266–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Walker Harris V, Brown TT. Bone loss in the HIV-infected patient: evidence, clinical implications, and treatment strategies. J Infect Dis 2012;205(suppl 3):S391–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Health Care Utilisation: Hospital average length of stay by diagnostic categories (http://stats.oecd.org/index.aspx?queryid=30165). [Google Scholar]
- [23].Guerro AC, Andretta IB, Bello SL, et al. Causes of hospital admission of AIDS patients in southern Brazil 2007–2012. Rev Soc Bras Med Trop 2014;47:632–6. [DOI] [PubMed] [Google Scholar]
- [24].Morris A, Lundgren JD, Masur H, et al. Current epidemiology of Pneumocystis pneumonia. Emerg Infect Dis 2004;10:1713–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Llibre JM, Revollo B, Vanegas S, et al. Pneumocystis jirovecii pneumonia in HIV-1-infected patients in the late-HAART era in developed countries. Scand J Infect Dis 2013;45:635–44. [DOI] [PubMed] [Google Scholar]
- [26].Berry SA, Manabe YC, Moore RD, et al. Hospitalization risk following initiation of highly active antiretroviral therapy. HIV Med 2010;11:289–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Bray S, Gedeon J, Hadi A, et al. Predictive value of CD4 cell count nadir on long-term mortality in HIV-positive patients in Uganda. HIV AIDS 2012;4:135–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Mussini C, Lorenzini P, Cozzi-Lepri A, et al. CD4/CD8 ratio normalisation and non-AIDS-related events in individuals with HIV who achieve viral load suppression with antiretroviral therapy: an observational cohort study. Lancet HIV 2015;2:e98–106. [DOI] [PubMed] [Google Scholar]
- [29].Hema MN, Ferry T, Dupon M, et al. Low CD4/CD8 ratio is associated with non AIDS-defining cancers in patients on antiretroviral therapy: ANRS CO8 (Aproco/Copilote) Prospective Cohort Study. PLoS One 2016;11:e0161594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Asher I, Mahlab-Guri K, Elbirt D, et al. Characteristics and outcome of patients diagnosed with HIV at older age. Medicine 2016;95:e2327. [DOI] [PMC free article] [PubMed] [Google Scholar]


