Abstract
Purpose of Review
This review discusses the recent evidence for a selection of blood-based emerging risk factors, with particular reference to their relation with coronary heart disease and stroke.
Recent Findings
For lipid-related emerging risk factors, recent findings indicate that increasing high-density lipoprotein cholesterol is unlikely to reduce cardiovascular risk, whereas reducing triglyceride-rich lipoproteins and lipoprotein(a) may be beneficial. For inflammatory and hemostatic biomarkers, genetic studies suggest that IL-6 (a pro-inflammatory cytokine) and several coagulation factors are causal for cardiovascular disease, but such studies do not support a causal role for C-reactive protein and fibrinogen. Patients with chronic kidney disease are at high cardiovascular risk with some of this risk not mediated by blood pressure. Randomized evidence (trials or Mendelian) suggests homocysteine and uric acid are unlikely to be key causal mediators of chronic kidney disease-associated risk and sufficiently large trials of interventions which modify mineral bone disease biomarkers are unavailable. Despite not being causally related to cardiovascular disease, there is some evidence that cardiac biomarkers (e.g. troponin) may usefully improve cardiovascular risk scores.
Summary
Many blood-based factors are strongly associated with cardiovascular risk. Evidence is accumulating, mainly from genetic studies and clinical trials, on which of these associations are causal. Non-causal risk factors may still have value, however, when added to cardiovascular risk scores. Although much of the burden of vascular disease can be explained by ‘classic’ risk factors (e.g. smoking and blood pressure), studies of blood-based emerging factors have contributed importantly to our understanding of pathophysiological mechanisms of vascular disease, and new targets for potential therapies have been identified.
Keywords: Epidemiology, Atherosclerosis, Vascular disease, Coronary heart disease, Stroke, Risk factors
Introduction
Major risk factors for cardiovascular disease include, but are not limited to, cigarette smoking, blood pressure, blood lipids, diabetes mellitus and adiposity [1–5, 6•]. The causality of these ‘classic’ risk factors is well established and they are commonly used to assess absolute cardiovascular risk in the general population [7–9]. Over the last few decades, however, other risk factors (commonly blood-based biomarkers) have been identified with potentially important implications for cardiovascular disease prevention, either through improved risk prediction or for treating cardiovascular disease (Table 1) [6•, 10]. For many of these risk factors, their causal relevance to cardiovascular disease is not well established and research is ongoing. This review will discuss the recent evidence for a selection of blood-based emerging risk factors, with particular reference to their relation with major cardiovascular outcomes, namely coronary heart disease and stroke.
Table 1.
Emerging risk factors for atherosclerotic cardiovascular disease
| Lipid-related biomarkers |
| High-density lipoprotein cholesterol |
| Triglycerides |
| Lipoprotein(a) |
| Apolipoprotein A1 and B |
| Lipoprotein-associated phospholipase A2 |
| Inflammatory biomarkers |
| C-reactive protein |
| Interleukin (IL)-1, IL-6, IL-18 |
| Tumour necrosis factor-α |
| Matrix metalloproteinase-9 |
| Soluble CD40 ligand |
| Vascular and cellular adhesion molecule |
| Leukocyte count |
| Biomarkers of hemostasis and thrombosis |
| Fibrinogen |
| Coagulation factors II, V and VIII |
| von Willebrand factor antigen |
| Tissue plasminogen activator (t-PA) |
| Plasminogen activator inhibitor-1 |
| D-dimer |
| Cardiac-related biomarkers |
| High sensitivity troponin |
| B-type natriuretic peptide |
| Kidney-related biomarkers |
| Creatinine |
| Microalbuminuria |
| Cystatin C |
| Calcium |
| Phosphate/fibroblast growth factor 23 |
| Uric acid |
| Other factors |
| Homocysteine |
| Vitamin D |
| Metabolism-related (e.g. HbA1c) |
| Platelet-related factors (e.g. platelet volume) |
| Endothelial dysfunction (e.g. nitric oxide) |
| Environmental exposures (e.g. air pollution, radiation) |
| Other non-invasive measures of vascular disease (e.g. carotid plaque) |
Lipid-Related Biomarkers
Total cholesterol, low-density lipoprotein (LDL) cholesterol, high-density lipoprotein (HDL) cholesterol and non-HDL cholesterol (calculated as the difference between total cholesterol and HDL cholesterol) display robust log-linear associations with, and are considered classic predictors of, cardiovascular disease [4, 11]. All commonly used cardiovascular risk scores contain various combinations of these routinely measured lipids [8]. It has been demonstrated that the predictive capacities of apolipoprotein B100 and apolipoprotein A1 are very similar to non-HDL cholesterol and HDL cholesterol, respectively [4]. Robust data from monogenic conditions like familial hypercholesterolemia, randomized trials (most notably of statin therapy) and genetic studies have confirmed that LDL cholesterol is causally related to cardiovascular disease, and cardiovascular outcome trials of new powerful LDL cholesterol lowering therapies are starting to emerge [12–16]. Recent studies have also provided further insights into the relevance of HDL cholesterol, triglycerides, lipoprotein(a) and lipoprotein-associated phospholipase A2 to the development of cardiovascular disease.
HDL Cholesterol, Apolipoprotein A1 and Triglycerides
The inverse associations of HDL cholesterol and apolipoprotein A1 with cardiovascular disease have led to the development of various therapeutic approaches to increase their levels [11, 17, 18]. While some early fibrate trials (medicines which reduce triglyceride, modestly increase HDL cholesterol and reduce LDL cholesterol) suggested cardiovascular benefit, recent larger studies of HDL cholesterol-raising therapies have yielded little or no benefit [19, 20•]. Cholesterol-ester transfer protein (CETP) inhibitors are able to increase HDL cholesterol by 30–120%, though it should be noted that potent CETP inhibitors also modestly reduce LDL cholesterol. Despite evidence from genetic studies indicating that those with genetically determined lower CETP activity may be at lower cardiovascular risk [21], three major outcomes trials of CETP inhibitors have shown no benefit [22, 23]. Results for the final ongoing major trial are expected in 2017. Of the three agents which failed, dalcetrapib (a weak inhibitor of CETP) has offered the purest test of the ‘HDL hypothesis’ given that it increases HDL cholesterol by 30% but has no effect on LDL cholesterol levels. In the DalOUTCOMES trial conducted in 15,871 participants following a recent acute coronary syndrome, dalcetrapib had no effect on cardiovascular events compared to placebo over 2.6 years [23]. Recent analyses of genetic variants have suggested that higher genetically determined HDL cholesterol is not associated with lower cardiovascular risk [14•, 24], implying that therapeutic interventions designed solely to increase HDL cholesterol are unlikely to provide cardiovascular benefit. It has also been announced that the development of apolipoprotein A1 Milano, an HDL mimetic given by weekly intravenous infusion, has been halted due to failure to reduce coronary atherosclerosis as measured by intravascular ultrasound [25].
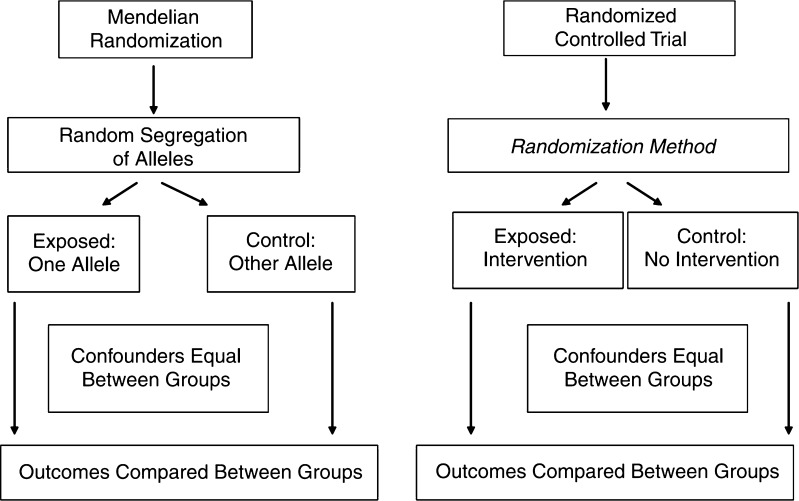
By contrast with HDL cholesterol, triglyceride levels are only weakly associated with, and do not improve prediction of, cardiovascular disease after adjustment for classic risk factors including HDL cholesterol [4]. However, recent Mendelian randomization studies (Fig. 1) have suggested that triglyceride-rich lipoproteins may be causally implicated in the development of cardiovascular disease. Lipoprotein lipase and apolipoprotein C3 are intimately involved in triglyceride metabolism. Genetic polymorphisms in both the LPL and APOC3 genes which result in higher triglyceride concentrations have been demonstrated to be associated with increased risk of myocardial infarction, while approaches combining data from multiple variants that affect triglyceride levels have yielded similar results [14•, 26–28]. An injectable antisense oligonucleotide to apolipoprotein C3 is currently under investigation in clinical trials to determine its effect on triglycerides, though not yet on cardiovascular disease risk [29].
Fig. 1.
Mendelian randomization and randomized controlled trial designs compared. Reproduced with permission from: Davey Smith G, Ebrahim S. Mendelian Randomization: Genetic Variants as Instruments for Strengthening Causal Inference in Observational Studies. In: Biosocial Surveys, National Research Council of the National Academy of Sciences, 2008. Courtesy of National Academies Press, Washington, D.C
Lipoprotein(a)
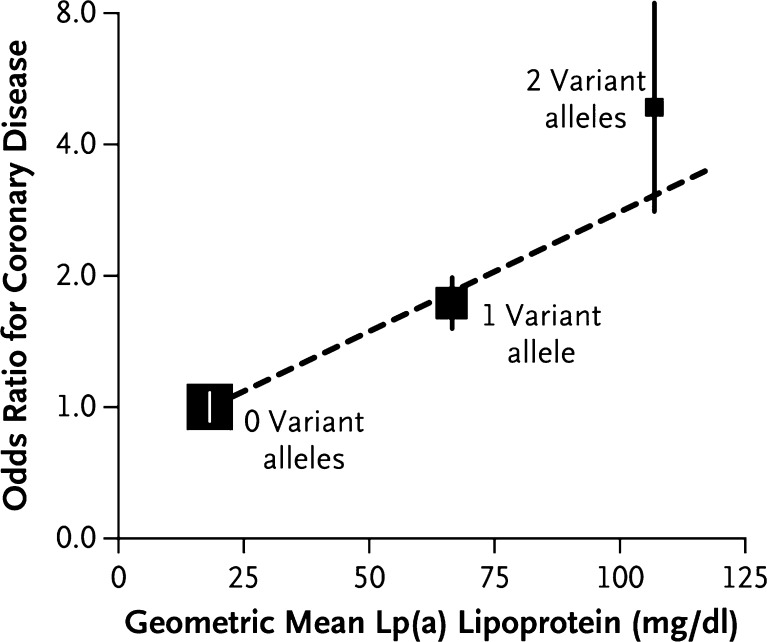
Lipoprotein(a) (Lp[a]) is a lipoprotein similar in structure to LDL but with the addition of apolipoprotein(a) which is covalently bound to the apolipoprotein B of the lipoprotein. The apolipoprotein(a) varies in size depending on the number of kringle repeats that it contains. Lp(a) levels are highly heritable and are considerably higher in black individuals than in whites [30, 31]. Levels of Lp(a) are positively associated with coronary heart disease in a curvilinear fashion with a clear increase above 1 μmol/L [31], a relationship largely unaffected by adjustment for classic cardiovascular risk factors. Lp(a) appears to have a weaker association with stroke. It is not clear whether Lp(a) meaningfully improves the prediction of cardiovascular events. However, studies of genetic polymorphisms in the LPA gene indicate that Lp(a) is causally implicated in the development of cardiovascular disease (Fig. 2) [32]. An injectable antisense oligonucleotide to apolipoprotein(a) has been developed and shown to reduce circulating Lp(a) by around 70% in early phase clinical trials [33•].
Fig. 2.
Association of the LPA Genotype Score with the Lp(a) Lipoprotein Level and the Risk of Coronary Disease in the PROCARDIS Cohort. The odds ratios (squares, with the size inversely proportional to the sampling variation) are for the association of the LPA genotype score (no variant alleles, one variant allele, or two variant alleles) with the risk of coronary disease, as measured with the use of ‘floating absolute risks’ which summarize the sampling variation for the three genotype scores without the selection of an arbitrary baseline genotype score. The vertical lines indicate 95% confidence intervals. Reproduced with permission from: Clarke R, Peden JF, Hopewell JC, et al. Genetic variants associated with Lp(a) lipoprotein level and coronary disease. N Engl J Med. 2009;361(26):2518–2528. Copyright © 2009 Massachusetts Medical Society. Reprinted with permission from Massachusetts Medical Society
Lipoprotein-Associated Phospholipase A2
Lipoprotein-associated phospholipase A2 (Lp-PLA2) is a mediator expressed in atherosclerotic plaque which increases the production of pro-inflammatory and pro-apoptotic mediators. A case-control analysis of 1740 participants in the WOSCOPS trial cohort demonstrated that those in the highest quintile of Lp-PLA2 mass were at double the risk of a coronary event compared to those in the lowest quintile [34]. Subsequent meta-analyses confirmed that Lp-PLA2, whether measured as mass or activity, is modestly associated with risk of coronary events [35]. However, genetic and clinical trial evidence has established that inhibition of this pathway is unlikely to provide cardiovascular benefit [36, 37]. For example, darapladib, an inhibitor of Lp-PLA2, failed to reduce cardiovascular events in the STABILITY trial of 15,828 patients with stable coronary heart disease over 3.7 years [37].
Inflammatory Biomarkers
Inflammatory processes play an important role in the pathogenesis of atherosclerotic vascular disease [38]. Yet, there is only limited evidence for the causal relevance of circulating inflammatory biomarkers on risk of vascular disease, and clinical trials of drugs specifically targeting inflammatory pathways are ongoing [39, 40].
C-reactive Protein
C-reactive protein (CRP) is an acute-phase reactant, synthesized primarily in the liver and released into the blood in response to tissue injury or infection. A large meta-analysis of individual participant data reported that 1-standard deviation (SD) higher loge CRP concentration was associated with 37% (95% CI 27–48%) higher risk of coronary heart disease and 27% (15–40%) higher risk of ischemic stroke, after adjusting for classic vascular risk factors [41]. However, a meta-analysis of Mendelian randomization studies found that genes encoding for CRP were not associated with risk of coronary heart disease (risk ratio for coronary heart disease 1.00 [95% CI 0.90–1.13] per 1-SD higher genetically raised loge CRP) [42]. In light of these findings, CRP is unlikely to be causally related to vascular disease, but it may still have some utility in improving the predictive ability of cardiovascular risk scores (although the added value appears small) [43].
Interleukin
Interleukin(IL)-6 is a pro-inflammatory cytokine that acts high in the inflammatory pathways (an ‘upstream’ inflammatory biomarker) with effects that include stimulation of hepatic acute-phase reactants, such as CRP [44]. It has been found to be strongly associated with coronary heart disease risk: a meta-analysis of 17 studies (5730 cases and 19,038 controls) reported an odds ratio for coronary heart disease, adjusting for several classic vascular risk and correcting for within-person variability, of 1.83 (95% CI 1.56–2.14) per 1-SD increase in usual IL-6 values [45]. Furthermore, meta-analyses of Mendelian randomization studies of an IL-6 receptor variant (Asp358Ala), with effects consistent to IL-6 receptor blockade, have reported a decreased risk of coronary heart disease per allele, supporting the causal role of the IL-6 pathway in coronary heart disease [46•, 47•].
Other Pro-Inflammatory Cytokines
There is more limited evidence for the association of other pro-inflammatory cytokines with vascular disease. A recent large meta-analysis assessed the association between coronary heart disease risk and several other pro-inflammatory cytokines, including IL-18, matrix metalloproteinase-9, soluble CD40 ligand and tumour necrosis factor-α (TNF-α) [48]. Positive associations were described for IL-18 and TNF-α only, with relative risks of coronary heart disease per 1-SD higher levels of 1.13 (95% CI 1.05–1.20) and 1.17 (1.09–1.25), respectively. These associations have yet to be assessed reliably in Mendelian randomized studies. However, a Mendelian randomized analysis of the gene encoding a different cytokine, the IL-1 receptor antagonist, reported a per-allele odds ratio for coronary heart disease of 1.03 (95% CI 1.02–1.04) but no association with ischemic stroke (odds ratio 1.00 [0.98–1.02]) [49]. Trials are ongoing of drugs targeting the signalling pathways of IL-1, as well as those for IL-6 and TNF-α [39, 40, 50].
Biomarkers of Hemostasis and Thrombosis
Several circulating biomarkers of hemostasis and thrombosis are strongly associated with risk of vascular disease. Mendelian randomization studies support a causal role for a number of factors involved with coagulation pathways, consistent with the efficacy of anticoagulant drugs in reducing atherosclerotic vascular events [51].
Fibrinogen
The most extensively studied hemostatic biomarker is fibrinogen, the major circulating clotting factor by mass. A meta-analysis of prospective observational studies reported that, after adjusting for classic vascular risk factors, 1-g/L increase in usual plasma fibrinogen was associated with a 82% (95% CI 60–106%) higher risk of coronary heart disease and 82% (54–116%) higher risk of stroke [52]. Mendelian randomization studies, however, have not supported the causality of this association. A large meta-analysis of such studies reported a relative risk of coronary heart disease of 1.00 (95% CI 0.95–1.04) per higher-fibrinogen allele [51]. Inflammatory and hemostatic processes are interrelated and the strong observational associations of fibrinogen and vascular risk may, in part, reflect its regulation by pro-inflammatory cytokines, such as IL-6 [53]. As with CRP, however, fibrinogen may still be a useful adjunct to standard cardiovascular risk scores [43].
Tissue Plasminogen Activator, D-dimer and von Willebrand Factor
Several prospective studies have described associations of other hemostatic factors and vascular disease. In particular, increased circulating levels of tissue plasminogen activator (t-PA), D-dimer and von Willebrand factor (VWF) have been associated with increased coronary heart disease risk [54–57]. A meta-analysis of prospective population-based studies found relative risks for coronary heart disease per 1-SD higher baseline levels of 1.13 (95% CI 1.06–1.21) with t-PA, 1.23 (1.16–1.32) with D-dimer and 1.16 (1.10–1.22) for VWF [58]. However, there was strong potential for residual confounding in this meta-analysis and, as such, the relation with coronary heart disease is still uncertain. The largest single study in this meta-analysis, which adjusted for a more comprehensive set of potential confounders, reported somewhat shallower associations (relative risks per 1-SD higher baseline levels of 1.07 [95% CI 0.99–1.14] with t-PA, 1.06 [1.00–1.13] with D-dimer and 1.08 [1.02–1.15] for VWF) [58].
Other Hemostatic Factors
A genetic study of the effect of seven polymorphisms, all of which alter hemostatic pathways, reported strong associations with coronary heart disease risk for two genes both encoding for coagulant factors [59]. Per-allele relative risks for coronary heart disease of factor V (G1691A) and prothrombin (factor II; G20210A) were 1.17 (95% CI 1.08–1.28) and 1.31 (1.12–1.52), respectively. There was no evidence of an association with several platelet receptors (GP1a, GP1bα and GPIIIa) and the findings for genetic variants of plasminogen activator inhibitor-1 (PAI-1; a protein involved in fibrinolysis) were inconclusive as there was strong evidence of publication bias. There is limited evidence for the associations between other biomarkers of hemostasis and vascular disease [53].
Cardiac-Related Biomarkers
Troponin and natriuretic peptides are released into the circulation from cardiac tissue even under physiological conditions, suggesting that they may be attractive cardiovascular biomarkers. The increasing availability of high-sensitivity assays for troponin in routine biochemistry laboratories (where it is typically used for the diagnosis of myocardial infarction) alongside brain natriuretic peptide (especially N-terminal pro-b-type natriuretic peptide [NT-proBNP] which is usually measured when left ventricular failure is suspected), indicates that these assays could be easily incorporated into routine cardiovascular risk screening if they are demonstrated to predict risk effectively.
The Natriuretic Peptides Studies Collaboration combined data from 40 studies for 95,000 participants without cardiovascular disease at baseline. Those with NT-proBNP levels in the highest tertile were at double the risk of suffering a coronary event, stroke, or developing heart failure [60•]. Addition of NT-proBNP to a risk model with classical risk factors yielded modest improvements in cardiovascular risk prediction, similar in scale to that provided by HDL cholesterol and superior to CRP. Neprilysin inhibitors (e.g. sacubitril) are agents which inhibit the degradation of natriuretic peptides and other endogenous vasoactive peptides. The PARADIGM-HF trial, conducted in 8442 patients with heart failure, confirmed that neprilysin inhibition (when added to renin-angiotensin system blockade) reduces hospitalization and death due to heart failure but probably has little effect on the risk of stroke or myocardial infarction [61].
Data regarding the predictive capacity of high sensitivity troponin (both troponin-T and troponin-I) in those without cardiovascular disease are more limited than for NT-proBNP. In one major study, troponin-T levels were related to outcomes in 9698 participants without cardiovascular disease aged 54 to 74 years [62]. One third had measurable troponin-T. There was a graded increase in cardiovascular events at progressively higher levels of troponin-T compared to those with unmeasurable levels and the authors concluded that its predictive capacity was similar to that of NT-proBNP.
Chronic Kidney Disease and Kidney-Related Factors
Chronic kidney disease (CKD) is defined and staged by severity of reduced renal function, usually quantified using estimated glomerular filtration rate (eGFR) [63]. Its prevalence reaches 10% in populations where old age or diabetes are common [64]. CKD is independently associated with substantially increased risk of cardiovascular disease, with progressively more advanced CKD associated with progressively higher risk [65, 66].
The spectrum of cardiovascular disease which manifests in people with CKD is wide and includes both arterial and cardiac disease. Common presentations of arterial disease in those with CKD include intimal atherosclerotic lesions [67], non-atheromatous non-calcified arterial stiffening [68], and heavy medial calcification [69] (see Wheeler et al. [70] for a comprehensive review). Correspondingly, people with CKD are at increased risk of coronary artery disease and structural heart disease [66, 71, 72]. CKD is also associated with increased stroke risk, and for large vessel stroke, there is some Mendelian randomization evidence that this association may be one of cause and effect. [73].
Every 30% decrement in eGFR is associated with about a 30% increase in risk of a cardiovascular event, so that a reduction in eGFR from 60 to 10 mL/min/1.73m2 is associated with about fourfold increased risk of cardiovascular disease [65]. The kidneys have a key role in modulating blood pressure which is a clear mechanism by which CKD causes increased risk of cardiovascular disease [74]. Each 10 mL/min/1.73m2 lower eGFR is associated with about a 5 mmHg higher systolic blood pressure [75], so a reduction in eGFR from 60 to 10 mL/min/1.73m2 would be expected to increase SBP by at least 20 mmHg, approximately doubling cardiovascular risk [2, 74]. The effect of CKD on blood pressure might therefore account for up to about one half of the association between CKD and cardiovascular disease.
A range of emerging risk factors which correlate with reduced renal function have been proposed to mediate the remaining CKD-associated cardiovascular risk which is not explained by blood pressure. However, the precise roles are not yet fully elucidated and quantified. For some, including homocysteine and uric acid, a body of evidence now suggests they are unlikely to be key causal mediators of arterial disease. Other risk factors remain potential candidates, including mediators of accelerated arterial calcification and certain lipid abnormalities. Details of the evidence supporting each of these mechanisms are provided below, with an emphasis on effects on coronary artery disease.
Homocysteinuria is a rare inherited disorder of metabolism which causes high blood homocysteine concentration and premature cardiovascular disease. Reduced renal function leads to moderately increased blood homocysteine concentrations and it is estimated that a 5 μmol/L increase in homocysteine is observed for each 10 mL/min/1.73m2 lower eGFR. Observational studies suggest such a change might increase coronary risk by about 20% [76]. However, Mendelian randomization experiments have been negative, and a meta-analysis of trials testing homocysteine lowering using folate supplementation found no evidence of benefit on major cardiovascular events [77, 78]. Moderate elevations of homocysteine therefore seem unlikely to be causally associated with coronary artery disease.
Blood uric acid concentration also increase as renal function falls, and positive associations between uric acid levels and coronary artery disease have been observed [79, 80]. Each 10 mL/min/1.73m2 lower eGFR is associated with about a 10–15 μmol/L increase in uric acid concentration, which is predicted to increase coronary risk by about 10% [79, 80]. However, again, Mendelian randomization experiments have cast doubt about whether such associations are causal, as once pleotropic pathways were taken into account, no clear association was observed [81].
Heavy arterial calcification is a particular feature of advanced CKD [69]. Both intimal and medial calcifications are common and associated with increased risk of cardiovascular disease, with perhaps the volume of intimal atheromatous coronary plaque calcification being more important than the density of calcification [69, 82]. A key emerging risk factor for arterial calcification is blood phosphate, the concentration of which increases as the capacity for its urinary excretion falls. High blood phosphate concentration can directly induce ossification of vascular smooth muscle cells and is associated with increased arterial calcification [83, 84]. For each 0.3 mmol/L increase in phosphate (which is the approximate effect of each 10 mL/min/1.73m2 lower eGFR), there is about a 30% increased risk of cardiovascular disease [85]. Phosphate lowering is achieved by dietary modification and phosphate binding medication [70, 86]. However, sufficiently large placebo-controlled trial have not been performed to confirm cardiovascular benefit from this practice. Trials comparing different binders are also complicated to interpret, as there are possible adverse cardiovascular effects of calcium-containing binders, and beneficial cardiovascular effects mediated through lipid lowering with some of the non-calcium containing binders [87]. Nevertheless, lowering phosphate is deeply embedded in nephrology practice.
Fibroblast growth factor-23 (FGF23) has recently emerged as another potential mediator of cardiovascular risk in CKD. It has particularly drawn interest as associations are consistently strong and FGF23 concentrations rise early in CKD mirroring the early rise in cardiovascular risk which is apparent with only modest reductions in renal function [88, 89]. FGF23 serves to increase phosphate excretion and does not appear to cause arterial calcification, observations which both suggest FGF23 is a protective homeostatic hormone (like natriuretic peptides) [90]. However, there is some mechanistic evidence that FGF23 may be directly cardiotoxic [91, 92]. Randomized experiments are therefore required to confirm whether consistently positive observational associations between FGF23 and risk of coronary artery disease represent confounding, or are causal.
Statin-based therapy is effective at lowering atherosclerotic risk in CKD, [93, 94] but LDL cholesterol (with the exception of nephrotic syndrome) is not generally raised in CKD [86, 87]. Instead, each 10 mL/min/1.73m2 lower eGFR is associated with a modest reduction in HDL cholesterol, perhaps as much as 0.1 mmol/L, which is associated with a 5–10% increased risk of coronary artery disease [4]. As discussed above, current evidence does not support HDL cholesterol being causally related to coronary disease. Perhaps more promisingly, reduced renal function is also associated with increased concentration of Lp(a) particles [95]. Mendelian randomization experiments predict Lp(a) to be causally associated with coronary artery disease, particularly the small Lp(a) isoforms [32]. Each 10 mL/min/1.73m2 lower eGFR is associated with a 0.2–0.3 μmol/L increase in Lp(a), which might increase coronary artery disease risk by about 10% [95]. Some uncertainty remains as the raised Lp(a) in CKD is mainly of the large isoform type, whose relevance to coronary artery disease risk is less well understood, but emerging Mendelian randomization evidence suggests that Lp(a) concentration may be associated with coronary risk independent of Lp(a) particle size [96].
Future Directions for Randomized Trials
Early stage clinical trials of drugs which lower lipoprotein(a) and triglycerides are in process, and the results to these studies will be influential in determining future trials of lipid-related factors [29, 33•]. In addition, novel mechanisms of reducing LDL cholesterol are being tested, including trials of PCSK9 inhibitors (monoclonal antibodies which target circulating PCSK9) [15, 16]. These antibodies have been found to dramatically lower LDL levels and, according to recently published results from the FOURIER trial, to reduce cardiovascular events in patients with clinically evident vascular disease [97]. With respect to inflammatory factors, there are a number of trials evaluating the effect of anti-inflammatory agents on cardiovascular outcomes, including low-dose methotrexate (a generic drug used to treat autoimmune conditions such as rheumatoid arthritis) and canakinumab (a human monoclonal antibody targeting the pro-inflammatory cytokine IL-1β) [39, 40, 50]. There is also a need for future trials of anti-inflammatory agents targeting specific cytokines for which there is strong evidence of causality, such as IL-6.
Limitations of Review
This review focuses on selected blood-based biomarkers and their relation to major vascular disease. There are other important blood-based biomarkers that it was not possible to cover in this review, some of which are listed in Table 1. In addition, we did not address metabolomic approaches to the simultaneous measurement of hundreds to thousands of small molecules that may yet lead to the identification of novel biomarkers. Furthermore, this review focuses on associations with coronary heart disease and stroke and did not address the relation of emerging risk factors with other major manifestations of vascular disease, notably abdominal aortic aneurysm and peripheral vascular disease. It was also outside the scope of this review to discuss non-blood-based emerging risk factors for vascular disease, such as radiation, coronary artery calcification, carotid intima-media thickness, carotid plaque and ankle-brachial index [10]. For a recent wide-ranging review of emerging risk factors for stroke see Hopewell and Clarke [6•].
Conclusions
This review has discussed a range of blood-based cardiovascular risk factors that have emerged over the last few decades, with a particular focus on their relation with major vascular disease. For some risk factors, there is now strong evidence that their association with coronary heart disease and stroke is not causal. Non-causal risk factors may still have value, however, when added to cardiovascular risk scores and a number of cardiac-related biomarkers hold particular promise in this regard. For other risk factors (including triglyceride-rich lipoproteins, lipoprotein(a), IL-6 and several coagulation factors), there is increasing evidence of a causal role in the pathogenesis of major vascular disease. Although much of the burden of vascular disease can be explained by classic risk factors, studies of emerging risk factors have contributed importantly to our understanding of the pathophysiological mechanisms of vascular disease, and new targets for potential therapies (for both primary and secondary prevention) have been identified.
Abbreviations
- APOC3
Apolipoprotein C3 gene
- CETP
Cholesterol-ester transfer protein
- CI
Confidence interval
- CKD
Chronic kidney disease
- CRP
C-reactive protein
- eGFR
Estimated glomerular filtration rate
- FGF23
Fibroblast growth factor-23
- HDL
High-density lipoprotein
- IL
Interleukin
- Lp(a)/LPA
Lipoprotein(a)/Lp(a) gene
- Lp-PLA2
Lipoprotein-associated phospholipase A2
- LDL
Low-density lipoprotein
- LPL
lipoprotein lipase gene
- NT-proBNP
N-terminal pro-b-type natriuretic peptide
- SD
Standard deviation
- t-PA
Tissue plasminogen activator
- TNF-α
tumour necrosis factor-α
- VWF
von Willebrand factor
Compliance with Ethical Standards
Conflict of Interest
All authors are research staff at the Clinical Trial Service Unit and Epidemiological Studies Unit (‘CTSU’). CTSU is funded by the UK Medical Research Council (which supports an embedded MRC Unit [MRC Population Health Research Unit]) as well as by grants from the British Heart Foundation and from Cancer Research UK. The CTSU has a staff policy of not accepting honoraria or other payments from the pharmaceutical industry, except for reimbursement of costs to participate in scientific meetings.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards and international/national/institutional guidelines).
Footnotes
Ben Lacey, William G. Herrington and David Preiss would like to share first authorship; Sarah Lewington and Jane Armitage are joint contributors.
This article is part of the Topical Collection on Evidence Based Medicine
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Herrington W, Lacey B, Sherliker P, Armitage J, Lewington S. Epidemiology of atherosclerosis and the potential to reduce the global burden of atherothrombotic disease. Circ Res. 2016;118(4):535–546. doi: 10.1161/CIRCRESAHA.115.307611. [DOI] [PubMed] [Google Scholar]
- 2.Prospective Studies Collaboration Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360(9349):1903–1913. doi: 10.1016/S0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 3.Prospective Studies Collaboration Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373(9669):1083–1096. doi: 10.1016/S0140-6736(09)60318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Emerging Risk Factors Collaboration Major lipids, apolipoproteins, and risk of vascular disease. JAMA. 2009;302(18):1993–2000. doi: 10.1001/jama.2009.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Emerging Risk Factors Collaboration Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet. 2010;375(9733):2215–2222. doi: 10.1016/S0140-6736(10)60484-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hopewell JC, Clarke R. Emerging risk factors for stroke: what have we learned from Mendelian randomization studies? Stroke. 2016;47(6):1673–1678. doi: 10.1161/STROKEAHA.115.010646. [DOI] [PubMed] [Google Scholar]
- 7.DeFilippis AP, Young R, Carrubba CJ, et al. An analysis of calibration and discrimination among multiple cardiovascular risk scores in a modern multiethnic cohort. Ann Intern Med. 2015;162(4):266–275. doi: 10.7326/M14-1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Damen JA, Hooft L, Schuit E, et al. Prediction models for cardiovascular disease risk in the general population: systematic review. BMJ. 2016;353:i2416. doi: 10.1136/bmj.i2416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hajifathalian K, Ueda P, Lu Y, et al. A novel risk score to predict cardiovascular disease risk in national populations (Globorisk): a pooled analysis of prospective cohorts and health examination surveys. Lancet Diabetes Endocrinol. 2015;3(5):339–355. doi: 10.1016/S2213-8587(15)00081-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Helfand M, Buckley DI, Freeman M, et al. Emerging risk factors for coronary heart disease: a summary of systematic reviews conducted for the U.S. Preventive Services Task Force. Ann Intern Med. 2009;151(7):496–507. doi: 10.7326/0003-4819-151-7-200910060-00010. [DOI] [PubMed] [Google Scholar]
- 11.Prospective Studies Collaboration Blood cholesterol and vascular mortality by age, sex, and blood pressure: a meta-analysis of individual data from 61 prospective studies with 55,000 vascular deaths. Lancet. 2007;370(9602):1829–1839. doi: 10.1016/S0140-6736(07)61778-4. [DOI] [PubMed] [Google Scholar]
- 12.Jensen J, Blankenhorn DH, Kornerup V. Coronary disease in familial hypercholesterolemia. Circulation. 1967;36(1):77–82. doi: 10.1161/01.CIR.36.1.77. [DOI] [PubMed] [Google Scholar]
- 13.Cholesterol Treatment Trialists Collaboration Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010;376(9753):1670–1681. doi: 10.1016/S0140-6736(10)61350-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.White J, Swerdlow DI, Preiss D, et al. Association of lipid fractions with risks for coronary artery disease and diabetes. JAMA Cardiol. 2016;1(6):692–699. doi: 10.1001/jamacardio.2016.1884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sabatine MS, Giugliano RP, Keech A, et al. Rationale and design of the further cardiovascular OUtcomes research with PCSK9 inhibition in subjects with elevated risk trial. Am Heart J. 2016;173:94–101. doi: 10.1016/j.ahj.2015.11.015. [DOI] [PubMed] [Google Scholar]
- 16.Schwartz GG, Bessac L, Berdan LG, et al. Effect of alirocumab, a monoclonal antibody to PCSK9, on long-term cardiovascular outcomes following acute coronary syndromes: rationale and design of the ODYSSEY outcomes trial. Am Heart J. 2014;168(5):682–689. doi: 10.1016/j.ahj.2014.07.028. [DOI] [PubMed] [Google Scholar]
- 17.Parish S, Peto R, Palmer A, et al. The joint effects of apolipoprotein B, apolipoprotein A1, LDL cholesterol, and HDL cholesterol on risk: 3510 cases of acute myocardial infarction and 9805 controls. Eur Heart J. 2009;30(17):2137–2146. doi: 10.1093/eurheartj/ehp221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thompson A, Danesh J. Associations between apolipoprotein B, apolipoprotein AI, the apolipoprotein B/AI ratio and coronary heart disease: a literature-based meta-analysis of prospective studies. J Intern Med. 2006;259(5):481–492. doi: 10.1111/j.1365-2796.2006.01644.x. [DOI] [PubMed] [Google Scholar]
- 19.Keech A, Simes RJ, Barter P, et al. Effects of long-term fenofibrate therapy on cardiovascular events in 9795 people with type 2 diabetes mellitus (the FIELD study): randomised controlled trial. Lancet. 2005;366(9500):1849–1861. doi: 10.1016/S0140-6736(05)67667-2. [DOI] [PubMed] [Google Scholar]
- 20.HPS2-THRIVE Collaborative Group Effects of extended-release niacin with laropiprant in high-risk patients. N Engl J Med. 2014;371(3):203–212. doi: 10.1056/NEJMoa1300955. [DOI] [PubMed] [Google Scholar]
- 21.Johannsen TH, Frikke-Schmidt R, Schou J, Nordestgaard BG, Tybjaerg-Hansen A. Genetic inhibition of CETP, ischemic vascular disease and mortality, and possible adverse effects. J Am Coll Cardiol. 2012;60(20):2041–2048. doi: 10.1016/j.jacc.2012.07.045. [DOI] [PubMed] [Google Scholar]
- 22.Barter PJ, Caulfield M, Eriksson M, et al. Effects of torcetrapib in patients at high risk for coronary events. N Engl J Med. 2007;357(21):2109–2122. doi: 10.1056/NEJMoa0706628. [DOI] [PubMed] [Google Scholar]
- 23.Schwartz GG, Olsson AG, Abt M, et al. Effects of dalcetrapib in patients with a recent acute coronary syndrome. N Engl J Med. 2012;367(22):2089–2099. doi: 10.1056/NEJMoa1206797. [DOI] [PubMed] [Google Scholar]
- 24.Voight BF, Peloso GM, Orho-Melander M, et al. Plasma HDL cholesterol and risk of myocardial infarction: a mendelian randomisation study. Lancet. 2012;380(9841):572–580. doi: 10.1016/S0140-6736(12)60312-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nicholls SJ, Nissen SE, Ballantyne C, et al. Impact of infusion of apoA-Milano HDL mimetic on regression of coronary atherosclerosis in acute coronary syndrome patients: MILANO-PILOT study. New Orleans: American Heart Association 2016 Scientific Sessions; 2016. [Google Scholar]
- 26.Triglyceride Coronary Disease Genetics Consortium and Emerging Risk Factors Collaboration Triglyceride-mediated pathways and coronary disease: collaborative analysis of 101 studies. Lancet. 2010;375(9726):1634–1639. doi: 10.1016/S0140-6736(10)60545-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jorgensen AB, Frikke-Schmidt R, Nordestgaard BG, Tybjaerg-Hansen A. Loss-of-function mutations in APOC3 and risk of ischemic vascular disease. N Engl J Med. 2014;371(1):32–41. doi: 10.1056/NEJMoa1308027. [DOI] [PubMed] [Google Scholar]
- 28.Do R, Willer CJ, Schmidt EM, et al. Common variants associated with plasma triglycerides and risk for coronary artery disease. Nat Genet. 2013;45(11):1345–1352. doi: 10.1038/ng.2795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gaudet D, Alexander VJ, Baker BF, et al. Antisense inhibition of apolipoprotein C-III in patients with hypertriglyceridemia. N Engl J Med. 2015;373(5):438–447. doi: 10.1056/NEJMoa1400283. [DOI] [PubMed] [Google Scholar]
- 30.Boomsma DI, Kaptein A, Kempen HJ, Gevers Leuven JA, Princen HM. Lipoprotein(a): relation to other risk factors and genetic heritability. Results from a Dutch parent-twin study. Atherosclerosis. 1993;99(1):23–33. doi: 10.1016/0021-9150(93)90047-X. [DOI] [PubMed] [Google Scholar]
- 31.Emerging Risk Factors Collaboration Lipoprotein(a) concentration and the risk of coronary heart disease, stroke, and nonvascular mortality. JAMA. 2009;302(4):412–423. doi: 10.1001/jama.2009.1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Clarke R, Peden JF, Hopewell JC, et al. Genetic variants associated with Lp(a) lipoprotein level and coronary disease. N Engl J Med. 2009;361(26):2518–2528. doi: 10.1056/NEJMoa0902604. [DOI] [PubMed] [Google Scholar]
- 33.Viney NJ, van Capelleveen JC, Geary RS, et al. Antisense oligonucleotides targeting apolipoprotein(a) in people with raised lipoprotein(a): two randomised, double-blind, placebo-controlled, dose-ranging trials. Lancet. 2016;388(10057):2239–2253. doi: 10.1016/S0140-6736(16)31009-1. [DOI] [PubMed] [Google Scholar]
- 34.Packard CJ, O’Reilly DS, Caslake MJ, et al. Lipoprotein-associated phospholipase A2 as an independent predictor of coronary heart disease. West of Scotland Coronary Prevention Study Group. N Engl J Med. 2000;343(16):1148–1155. doi: 10.1056/NEJM200010193431603. [DOI] [PubMed] [Google Scholar]
- 35.Lp-PLA2 Studies Collaboration. Lipoprotein-associated phospholipase A(2) and risk of coronary disease, stroke, and mortality: collaborative analysis of 32 prospective studies. Lancet. 2010;375(9725):1536–44. [DOI] [PMC free article] [PubMed]
- 36.Casas JP, Ninio E, Panayiotou A, et al. PLA2G7 genotype, lipoprotein-associated phospholipase A2 activity, and coronary heart disease risk in 10 494 cases and 15 624 controls of European Ancestry. Circulation. 2010;121(21):2284–2293. doi: 10.1161/CIRCULATIONAHA.109.923383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Investigators STABILITY. Darapladib for preventing ischemic events in stable coronary heart disease. N Engl J Med. 2014;370(18):1702–1711. doi: 10.1056/NEJMoa1315878. [DOI] [PubMed] [Google Scholar]
- 38.Libby P, Ridker PM, Hansson GK. Progress and challenges in translating the biology of atherosclerosis. Nature. 2011;473(7347):317–325. doi: 10.1038/nature10146. [DOI] [PubMed] [Google Scholar]
- 39.Ridker PM, Thuren T, Zalewski A, Libby P. Interleukin-1beta inhibition and the prevention of recurrent cardiovascular events: rationale and design of the Canakinumab Anti-inflammatory Thrombosis Outcomes Study (CANTOS) Am Heart J. 2011;162(4):597–605. doi: 10.1016/j.ahj.2011.06.012. [DOI] [PubMed] [Google Scholar]
- 40.Everett BM, Pradhan AD, Solomon DH, et al. Rationale and design of the cardiovascular inflammation reduction trial: a test of the inflammatory hypothesis of atherothrombosis. Am Heart J. 2013;166(2):199–207. doi: 10.1016/j.ahj.2013.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Emerging Risk Factors Collaboration C-reactive protein concentration and risk of coronary heart disease, stroke, and mortality: an individual participant meta-analysis. Lancet. 2010;375(9709):132–140. doi: 10.1016/S0140-6736(09)61717-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.C Reactive Protein Coronary Heart Disease Genetics Collaboration Association between C reactive protein and coronary heart disease: mendelian randomisation analysis based on individual participant data. BMJ. 2011;342:d548. doi: 10.1136/bmj.d548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Emerging Risk Factors Collaboration C-reactive protein, fibrinogen, and cardiovascular disease prediction. N Engl J Med. 2012;367(14):1310–1320. doi: 10.1056/NEJMoa1107477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ridker PM. Targeting inflammatory pathways for the treatment of cardiovascular disease. Eur Heart J. 2014;35(9):540–543. doi: 10.1093/eurheartj/eht398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Danesh J, Kaptoge S, Mann AG, et al. Long-term interleukin-6 levels and subsequent risk of coronary heart disease: two new prospective studies and a systematic review. PLoS Med. 2008;5(4):e78. doi: 10.1371/journal.pmed.0050078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Interleukin-6 Receptor Mendelian Randomisation Analysis (IL6R MR) Consortium The interleukin-6 receptor as a target for prevention of coronary heart disease: a mendelian randomisation analysis. Lancet. 2012;379(9822):1214–1224. doi: 10.1016/S0140-6736(12)60110-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.IL6R Genetics Consortium Emerging Risk Factors Collaboration Interleukin-6 receptor pathways in coronary heart disease: a collaborative meta-analysis of 82 studies. Lancet. 2012;379(9822):1205–1213. doi: 10.1016/S0140-6736(11)61931-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kaptoge S, Seshasai SR, Gao P, et al. Inflammatory cytokines and risk of coronary heart disease: new prospective study and updated meta-analysis. Eur Heart J. 2014;35(9):578–589. doi: 10.1093/eurheartj/eht367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Interleukin 1 Genetics Consortium Cardiometabolic effects of genetic upregulation of the interleukin 1 receptor antagonist: a Mendelian randomisation analysis. Lancet Diabetes Endocrinol. 2015;3(4):243–253. doi: 10.1016/S2213-8587(15)00034-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ridker PM, Howard CP, Walter V, et al. Effects of interleukin-1beta inhibition with canakinumab on hemoglobin A1c, lipids, C-reactive protein, interleukin-6, and fibrinogen: a phase IIb randomized, placebo-controlled trial. Circulation. 2012;126(23):2739–2748. doi: 10.1161/CIRCULATIONAHA.112.122556. [DOI] [PubMed] [Google Scholar]
- 51.Keavney B, Danesh J, Parish S, et al. Fibrinogen and coronary heart disease: test of causality by ‘Mendelian randomization’. Int J Epidemiol. 2006;35(4):935–943. doi: 10.1093/ije/dyl114. [DOI] [PubMed] [Google Scholar]
- 52.Fibrinogen Studies Collaboration Plasma fibrinogen level and the risk of major cardiovascular diseases and nonvascular mortality: an individual participant meta-analysis. JAMA. 2005;294(14):1799–1809. doi: 10.1001/jama.294.14.1799. [DOI] [PubMed] [Google Scholar]
- 53.Lowe G, Rumley A. The relevance of coagulation in cardiovascular disease: what do the biomarkers tell us? Thromb Haemost. 2014;112(5):860–867. doi: 10.1160/TH14-03-0199. [DOI] [PubMed] [Google Scholar]
- 54.Danesh J, Whincup P, Walker M, et al. Fibrin D-dimer and coronary heart disease: prospective study and meta-analysis. Circulation. 2001;103(19):2323–2327. doi: 10.1161/01.CIR.103.19.2323. [DOI] [PubMed] [Google Scholar]
- 55.Whincup PH, Danesh J, Walker M, et al. von Willebrand factor and coronary heart disease: prospective study and meta-analysis. Eur Heart J. 2002;23(22):1764–1770. doi: 10.1053/euhj.2001.3237. [DOI] [PubMed] [Google Scholar]
- 56.Lowe GD, Danesh J, Lewington S, et al. Tissue plasminogen activator antigen and coronary heart disease. Prospective study and meta-analysis. Eur Heart J. 2004;25(3):252–259. doi: 10.1016/j.ehj.2003.11.004. [DOI] [PubMed] [Google Scholar]
- 57.Wannamethee SG, Whincup PH, Shaper AG, Rumley A, Lennon L, Lowe GD. Circulating inflammatory and hemostatic biomarkers are associated with risk of myocardial infarction and coronary death, but not angina pectoris, in older men. J Thromb Haemost. 2009;7(10):1605–1611. doi: 10.1111/j.1538-7836.2009.03574.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Willeit P, Thompson A, Aspelund T, et al. Hemostatic factors and risk of coronary heart disease in general populations: new prospective study and updated meta-analyses. PLoS One. 2013;8(2):e55175. doi: 10.1371/journal.pone.0055175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ye Z, Liu EH, Higgins JP, et al. Seven haemostatic gene polymorphisms in coronary disease: meta-analysis of 66,155 cases and 91,307 controls. Lancet. 2006;367(9511):651–658. doi: 10.1016/S0140-6736(06)68263-9. [DOI] [PubMed] [Google Scholar]
- 60.Natriuretic Peptides Studies Collaboration Natriuretic peptides and integrated risk assessment for cardiovascular disease: an individual-participant-data meta-analysis. Lancet Diabetes Endocrinol. 2016;4(10):840–849. doi: 10.1016/S2213-8587(16)30196-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.McMurray JJ, Packer M, Desai AS, et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014;371(11):993–1004. doi: 10.1056/NEJMoa1409077. [DOI] [PubMed] [Google Scholar]
- 62.Saunders JT, Nambi V, de Lemos JA, et al. Cardiac troponin T measured by a highly sensitive assay predicts coronary heart disease, heart failure, and mortality in the atherosclerosis risk in communities study. Circulation. 2011;123(13):1367–1376. doi: 10.1161/CIRCULATIONAHA.110.005264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.KDIGO CKD Working Group KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;3:1–150. doi: 10.1038/kisup.2012.73. [DOI] [PubMed] [Google Scholar]
- 64.Levey AS, Coresh J. Chronic kidney disease. Lancet. 2012;379(9811):165–180. doi: 10.1016/S0140-6736(11)60178-5. [DOI] [PubMed] [Google Scholar]
- 65.Mafham M, Emberson J, Landray MJ, Wen CP, Baigent C. Estimated glomerular filtration rate and the risk of major vascular events and all-cause mortality: a meta-analysis. PLoS One. 2011;6(10):e25920. doi: 10.1371/journal.pone.0025920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tonelli M, Muntner P, Lloyd A, et al. Risk of coronary events in people with chronic kidney disease compared with those with diabetes: a population-level cohort study. Lancet. 2012;380(9844):807–814. doi: 10.1016/S0140-6736(12)60572-8. [DOI] [PubMed] [Google Scholar]
- 67.Kono K, Fujii H, Nakai K, et al. Composition and plaque patterns of coronary culprit lesions and clinical characteristics of patients with chronic kidney disease. Kidney Int. 2012;82(3):344–351. doi: 10.1038/ki.2012.118. [DOI] [PubMed] [Google Scholar]
- 68.Schwarz U, Buzello M, Ritz E, et al. Morphology of coronary atherosclerotic lesions in patients with end-stage renal failure. Nephrology, dialysis, transplantation : official publication of the European Dialysis and Transplant Association - European Renal Association. 2000;15(2):218–223. doi: 10.1093/ndt/15.2.218. [DOI] [PubMed] [Google Scholar]
- 69.London GM, Guérin AP, Marchais SJ, Métivier F, Pannier B, Adda H. Arterial media calcification in end-stage renal disease: impact on all-cause and cardiovascular mortality. Nephrology, dialysis, transplantation : official publication of the European Dialysis and Transplant Association - European Renal Association. 2003;18(9):1731–1740. doi: 10.1093/ndt/gfg414. [DOI] [PubMed] [Google Scholar]
- 70.Wheeler DC, Haynes R, Landray MJ, Baigent C. Chapter 56: cardiovascular aspects of kidney disease. In: Taal MW, Chertow GM, Marsden P, Skorecki K, ASL Y, Brenner BM, editors. Brenner and Rector’s the kidney. Philadelphia: Elsevier Saunders; 2012. [Google Scholar]
- 71.Park M, Hsu CY, Li Y, et al. Associations between kidney function and subclinical cardiac abnormalities in CKD. Journal of the American Society of Nephrology : JASN. 2012;23(10):1725–1734. doi: 10.1681/ASN.2012020145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Foley RN, Parfrey PS, Kent GM, Harnett JD, Murray DC, Barre PE. Long-term evolution of cardiomyopathy in dialysis patients. Kidney Int. 1998;54(5):1720–1725. doi: 10.1046/j.1523-1755.1998.00154.x. [DOI] [PubMed] [Google Scholar]
- 73.Holliday EG, Traylor M, Malik R, et al. Polygenic overlap between kidney function and large artery atherosclerotic stroke. Stroke. 2014;45(12):3508–3513. doi: 10.1161/STROKEAHA.114.006609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Blood Pressure Lowering Treatment Trialists Collaboration Blood pressure lowering and major cardiovascular events in people with and without chronic kidney disease: meta-analysis of randomised controlled trials. BMJ. 2013;347:f5680. doi: 10.1136/bmj.f5680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Boudville N, Prasad GV, Knoll G, et al. Meta-analysis: risk for hypertension in living kidney donors. Ann Intern Med. 2006;145(3):185–196. doi: 10.7326/0003-4819-145-3-200608010-00006. [DOI] [PubMed] [Google Scholar]
- 76.Homocysteine Studies Collaboration Homocysteine and risk of ischemic heart disease and stroke: a meta-analysis. JAMA. 2002;288(16):2015–2022. doi: 10.1001/jama.288.16.2015. [DOI] [PubMed] [Google Scholar]
- 77.Clarke R, Bennett DA, Parish S, et al. Homocysteine and coronary heart disease: meta-analysis of MTHFR case-control studies, avoiding publication bias. PLoS Med. 2012;9(2):e1001177. doi: 10.1371/journal.pmed.1001177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Clarke R, Halsey J, Lewington S, et al. Effects of lowering homocysteine levels with B vitamins on cardiovascular disease, cancer, and cause-specific mortality: meta-analysis of 8 randomized trials involving 37 485 individuals. Arch Intern Med. 2010;170(18):1622–1631. doi: 10.1001/archinternmed.2010.348. [DOI] [PubMed] [Google Scholar]
- 79.Chen Z, Ding Z, Fu C, Yu C, Ma G. Correlation between serum uric acid and renal function in patients with stable coronary artery disease and type 2 diabetes. Journal of clinical medicine research. 2014;6(6):443–450. doi: 10.14740/jocmr1909w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Fang J, Alderman MH. Serum uric acid and cardiovascular mortality the NHANES I epidemiologic follow-up study, 1971-1992. National Health and Nutrition Examination Survey. JAMA. 2000;283(18):2404–2410. doi: 10.1001/jama.283.18.2404. [DOI] [PubMed] [Google Scholar]
- 81.White J, Sofat R, Hemani G, et al. Plasma urate concentration and risk of coronary heart disease: a Mendelian randomisation analysis. Lancet Diabetes Endocrinol. 2016;4(4):327–336. doi: 10.1016/S2213-8587(15)00386-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Criqui MH, Denenberg JO, Ix JH, et al. Calcium density of coronary artery plaque and risk of incident cardiovascular events. JAMA. 2014;311(3):271–278. doi: 10.1001/jama.2013.282535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Johnson RC, Leopold JA, Loscalzo J. Vascular calcification: pathobiological mechanisms and clinical implications. Circ Res. 2006;99(10):1044–1059. doi: 10.1161/01.RES.0000249379.55535.21. [DOI] [PubMed] [Google Scholar]
- 84.Ix JH, De Boer IH, Peralta CA, et al. Serum phosphorus concentrations and arterial stiffness among individuals with normal kidney function to moderate kidney disease in MESA. Clinical journal of the American Society of Nephrology : CJASN. 2009;4(3):609–615. doi: 10.2215/CJN.04100808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Palmer SC, Hayen A, Macaskill P, et al. Serum levels of phosphorus, parathyroid hormone, and calcium and risks of death and cardiovascular disease in individuals with chronic kidney disease: a systematic review and meta-analysis. JAMA. 2011;305(11):1119–1127. doi: 10.1001/jama.2011.308. [DOI] [PubMed] [Google Scholar]
- 86.Block GA, Wheeler DC, Persky MS, et al. Effects of phosphate binders in moderate CKD. Journal of the American Society of Nephrology : JASN. 2012;23(8):1407–1415. doi: 10.1681/ASN.2012030223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Navaneethan SD, Palmer SC, Craig JC, Elder GJ, Strippoli GF. Benefits and harms of phosphate binders in CKD: a systematic review of randomized controlled trials. American journal of kidney diseases : the official journal of the National Kidney Foundation. 2009;54(4):619–637. doi: 10.1053/j.ajkd.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 88.Isakova T, Wahl P, Vargas GS, et al. Fibroblast growth factor 23 is elevated before parathyroid hormone and phosphate in chronic kidney disease. Kidney Int. 2011;79(12):1370–1378. doi: 10.1038/ki.2011.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351(13):1296–1305. doi: 10.1056/NEJMoa041031. [DOI] [PubMed] [Google Scholar]
- 90.Scialla JJ, Lau WL, Reilly MP, et al. Fibroblast growth factor 23 is not associated with and does not induce arterial calcification. Kidney Int. 2013;83(6):1159–1168. doi: 10.1038/ki.2013.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Leifheit-Nestler M, Grosse Siemer R, Flasbart K, et al. Induction of cardiac FGF23/FGFR4 expression is associated with left ventricular hypertrophy in patients with chronic kidney disease. Nephrology, dialysis, transplantation : official publication of the European Dialysis and Transplant Association - European Renal Association. 2016;31(7):1088–1099. doi: 10.1093/ndt/gfv421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Gutierrez OM. Connecting the dots on fibroblast growth factor 23 and left ventricular hypertrophy. Nephrology, dialysis, transplantation : official publication of the European Dialysis and Transplant Association - European Renal Association. 2016;31(7):1031–1033. doi: 10.1093/ndt/gfv445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Baigent C, Landray MJ, Reith C, et al. The effects of lowering LDL cholesterol with simvastatin plus ezetimibe in patients with chronic kidney disease (study of heart and renal protection): a randomised placebo-controlled trial. Lancet. 2011;377(9784):2181–2192. doi: 10.1016/S0140-6736(11)60739-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Cholesterol Treatment Trialists Collaboration. Impact of renal function on the effects of LDL cholesterol lowering with statin-based regimens: a meta-analysis of individual participant data from 28 randomised trials. Lancet Diabetes Endocrinol. 2016;4(10):829–39 [DOI] [PubMed]
- 95.Kronenberg F. Causes and consequences of lipoprotein(a) abnormalities in kidney disease. Clin Exp Nephrol. 2014;18(2):234–237. doi: 10.1007/s10157-013-0875-8. [DOI] [PubMed] [Google Scholar]
- 96.Saleheen D, Haycock PC, Zhao W, et al. Apolipoprotein(a) isoform size, lipoprotein(a) concentration, and coronary artery disease: a mendelian randomisation analysis. Lancet Diabetes Endocrinol. 2017. doi:10.1056/NEJMoa1615664. [DOI] [PMC free article] [PubMed]
- 97.Sabatine MS, Giugliano RP, Keech AC, et al. FOURIER steering committee and investigators: evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med. 2017. doi:10.1016/S2213-8587(17)30088-8.