Introduction
KEY TEACHING POINTS
|
We report a rare case presenting recurrent syncope in a 50-year-old woman due to idiopathic glossopharyngeal neuralgia (GN).
The patient presented at the emergency department for recurrent syncope, starting 1 week before presentation. All episodes of syncope started with a sharp stabbing pain sensation in the left anterior side of the throat, distributing to the ipsilateral side of the neck and ear, accompanied by heavy swallowing, rotating of the head to the right, generalized tonic seizure-like movements of both arms and legs with the urge to grab the left side of the neck with her hands, and eventually followed by syncope. Syncope lasted from a few seconds up to a minute. After the attack, the patient regained complete consciousness. No postictal symptoms, such as urine incontinency or tongue bite, had occurred. Furthermore, no cardiac symptoms, such as chest pain, palpitations, or vasovagal symptoms, occurred before syncope. Talking, turning of the head, emotional stress, palpitation of the neck, or even sleeping could initiate a new episode of syncope.
There was no history of trauma, unexplained syncope, and epileptic insults or a family history of acute unexplained death. In the year before the presentation, the patient had suffered from recurrent pain on the left side of the neck without syncope for several weeks in 2 different episodes. Complete remission had occurred without any form of medical intervention.
Physical examination revealed an anxious woman. Blood pressure was 125/80 mm Hg with a regular pulse rate of 80 beats/min. The general and cardiologic examination was considered normal. Direct flexible laryngoscopy as well as examination of ear and nose by an otolaryngologist showed no evidence of abnormality.
Neurological examination demonstrated trigger areas in the distribution of the glossopharyngeal nerve; palpation of the left side of the neck or performing the Weber and the Rinne tests (hearing tests) resulted in neck pain with subsequent bradycardia and asystole, during which patient temporarily lost consciousness. Both noninvasive and invasive monitoring showed a simultaneous decrease in the heart rate and blood pressure with the onset of pain (Figure 1).
Figure 1.
Continuous monitor lead electrocardiogram showing asystole followed by bradycardia and junctional escape during neuralgic pain.
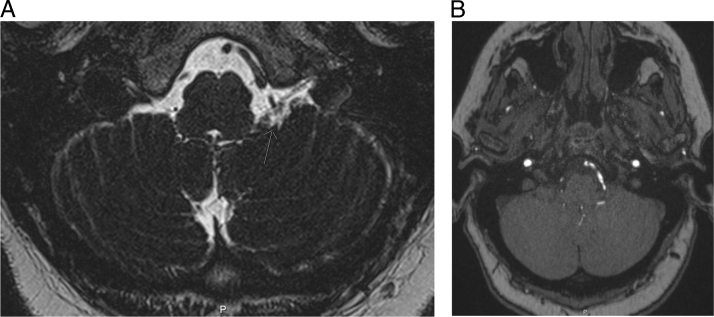
An additional investigation showed normal hematological and biochemical examinations. An electrocardiogram demonstrated a sinus rhythm of 83 beats/min, an intermediate heart axis, and normal conduction intervals (PQ interval 150 ms, QRS interval 94 ms, and corrected QT interval 430 ms). No signs of preexcitation, ischemia, or Brugada syndrome were seen on the electrocardiogram. A computed tomographic scan and a magnetic resonance image of the brain, neck, and heart showed no evidence of a tumor or malformation of the aorta, carotid artery, cervical vasculature, or the circle of Willis. Furthermore, the parotid and the submandibular gland and their relationship with brain nerves IX and X were considered normal. An additional magnetic resonance image addressing the anatomical relationship between cranial nerves and vessels demonstrated neurovascular compression of nerve IX by a thick posterior inferior cerebellar artery (PICA). (Figures 2A and 2B).
Figure 2.
A: MRI axial 3D T2 SPACE: the arrow points to the posterior inferior cerebellar artery that cross the glossopharyngeal nerve closely. B: MRI axial 3D TOF: the hyperintense line next to the brainstem is the thick posterior inferior cerebellar artery. 3D = 3-dimensional; MRI = magnetic resonance imaging; T2 SPACE = Sampling Perfection with Application optimized Contrasts using different flip angle Evolution; TOF =Time of Flight.
The diagnosis of GN was made, and pregabalin 150 mg 3 times daily was initiated. Simultaneously, a temporary transvenous pacemaker was inserted because of the increasing frequency and length of syncopal episodes. This resulted in a reduction of the length of syncope (Figure 3). Therefore, a permanent demand dual-chamber pacemaker was implanted and no further episodes of syncope occurred.
Figure 3.
Continuous monitor lead electrocardiogram showing the effect of the pacemaker during an attack.
Although the frequency and intensity of the pain and the length of syncope were reduced by both interventions, the patient still experienced GN-related pain attacks and pregabalin was replaced by carbamazepine 200 mg (up to 5 times daily).
Eventually, lamotrigine 200 mg 2 times daily was added to the drug regimen. This regimen of carbamazepine and lamotrigine effectively suppressed both syncope and GN- related pain, and surgery was canceled.
GN
GN is a rare condition of craniofacial pain and represents 0.2%–1.3% of the cases with facial pain.1, 2 The incidence of GN is approximately 0.8 per 100,000 persons per year and occurs more frequently in male subjects with a mean age of 50.2 ± 14 years.1, 3, 4, 5, 6, 7, 8 The frequency of cardiac syncope in GN is 2%–20%.5, 9 The diagnostic criteria of GN according to the International Headache Society are listed in Table 1.10 However, the frequency of GN is underestimated because of difficulties in clinical diagnosis and unawareness of the disease.11
Table 1.
Diagnostic criteria of glossopharyngeal neuralgia according to the International Headache Society10
|
The pain in GN is characterized by paroxysmal lancinating pain and is usually confined to the unilateral somatosensory distribution of the glossopharyngeal or the auricular and pharyngeal branches of the vagus, such as the pharynx. It commonly radiates to the ear and subauricular area, as well as the lateral aspect of the throat and submandibular region.12, 13 The pain lasts from a few seconds to 5 minutes and is often precipitated or triggered by chewing, coughing, yawning, talking, and swallowing.14 Although trigger zones are rarely found in GN, syncope in our patient could be provoked by palpitation of the neck and by specific neurological examination. Accompanying symptoms include stridor, coughing, hoarseness, vomiting, sweating, and hypersalivation. GN must be differentiated from trigeminal neuralgia, which shares several characteristics with GN and can occur in a combined form in 10% of patients.15 Like trigeminal neuralgia, GN may go into spontaneous remission.5
“Idiopathic” cranial nerve neuralgias are attributed to a neurovascular nerve compression syndrome at the root entry zone of the respective cranial nerve.11 GN is generally caused by neurovascular compression of nerve IX by the PICA,11 which was first observed postmortem by Brihaye et al.16 However, several other mechanisms, besides intracranial vascular compression,16, 17, 18, 19, 20, 21 may cause GN and include Eagle syndrome,22 cerebellopontine angle or cranial base tumors,23 Chiari type I syndrome,24 pharyngeal tumors and abscesses,25, 26, 27 posterior fossa arteriovenous malformations, trauma,28 and multiple sclerosis.29 In our patient, these causes were excluded by neurovascular imaging.
Neurological syncope cascade
Syncope in GN related to neuralgic pain is most likely caused by activation of the dorsal motor nucleus of the vagus nerve by abnormally enhanced input from afferent or ischemic lesions of the glossopharyngeal nerve.30 The reflex arrhythmia could be explained from the fact that afferent nerve impulses from the glossopharyngeal nerve may reach the tractus solitarius of the brainstem and via collateral fibers reach the dorsal motor nucleus of the vagus nerve.31 One afferent branch of the glossopharyngeal nerve supplies the somatosensorial information to the nucleus ambiguus, while another afferent branch of the glossopharyngeal nerve, the carotid sinus nerve (Hering nerve), conducts impulses from the body of the carotid sinus to the nucleus dorsalis of the vagal nerve.32 It has been hypothesized that by artificial synapses in the glossopharyngeal nerve the impulses from the somsatosensorial branches stimulate the carotid sinus nerve and thereby the nucleus dorsalis. Activation of this abnormal loop during severe neuralgic pain would be responsible for bradycardia/asystole, with cerebral hypoperfusion, slowing of electroencephalographic activity, syncope, and convulsions in proportion to the duration of asystole.33 Individual differences in the susceptibility of the dorsal motor nucleus to the pain impulse may explain why not all cases are associated with syncope.
Treatment
Both medical and surgical treatments have been used to treat GN.34
Carbamazepine is considered as a first-line treatment and is thought to be useful in controlling GN-related pain by the inhibitory effect on the brain stem reflex activity.35 Furthermore, it possibly prevents bradycardia.36, 37 Other medical treatments have been reported and include gabapentin, lamotrigine, and pregabalin.38, 39, 40, 41 Both pregabalin and gabapentin induce a decreasing release of excitatory neurotransmitters by acting on the α2δ subunit of calcium channels.41 Bradyarrhythmic complications of GN are treated with anticholinergic medications or with a β2-adrenoceptor agonist, such as atropine, isoprenaline, or with temporary pacing.
The need for on-demand dual-chamber pacemakers in the long-term treatment of GN remains controversial.31, 42 In 1971, a temporary transvenous cardiac pacemaker was inserted for the first time to prevent GN-related syncope.43
However, pacing might prevent or only reduces the length of syncope and does not affect GN-related pain. Furthermore, pacing may not be effective in preventing GN-related syncope in patients who have important vasodepressor response.44, 45, 46 A permanent demand pacemaker, combined with medical treatment, should be considered depending on the frequency of syncope and the vasodepressive response before addressing surgical intervention.44
Neurovascular surgery
Microvascular decompression is a second-line treatment in idiopathic GN and is reserved only for those who have failed medical treatment and have dual-chamber pacemakers.14, 47 During this surgery, dissection of the vessel will take place according to the trigeminal nerve decompression suggested by Jannetta and coworkers,47 followed by placing a Teflon interpositum. The rationale behind surgery is that GN is caused by direct compression of the root entry zone of the glossopharyngeal nerve, most often by the PICA, and vascular decompression could resolve this.11 In 1977, Laha et al were the first to report good results of microvascular decompression for GN.18 Gaul et al11 demonstrated that 16 of the 18 patients were completely pain free after microsurgical decompression for GN and no longer needed any anticonvulsant or other pain medication. Furthermore, studies have shown excellent long-term results.8, 48
References
- 1.Chawla J.C., Falconer M.A. Glossopharyngeal and vagal neuralgia. Br Med J. 1967;3:529–531. doi: 10.1136/bmj.3.5564.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fraioli B., Esposito V., Ferrante L., Trubiani L., Lunardi P. Microsurgical treatment of glossopharyngeal neuralgia: case reports. Neurosurgery. 1989;25:630–632. doi: 10.1097/00006123-198910000-00018. [DOI] [PubMed] [Google Scholar]
- 3.Manzoni G.C., Torelli P. Epidemiology of typical and atypical craniofacial neuralgias. Neurol Sci. 2005;26:s65–s67. doi: 10.1007/s10072-005-0410-0. [DOI] [PubMed] [Google Scholar]
- 4.Katusic S., Williams D.B., Beard C.M., Bergstralh E., Kurland L.T. Incidence and clinical features of glossopharyngeal neuralgia, Rochester, Minnesota, 1945-1984. Neuroepidemiology. 1991;10:266–275. doi: 10.1159/000110283. [DOI] [PubMed] [Google Scholar]
- 5.Rushton J.G., Stevens J.C., Miller R.H. Glossopharyngeal (vagoglossopharyngeal) neuralgia: a study of 217 cases. Arch Neurol. 1981;38:201–205. doi: 10.1001/archneur.1981.00510040027002. [DOI] [PubMed] [Google Scholar]
- 6.Koopman J.S.H.A., Dieleman J.P., Huygen F.J., de Mos M., Martin C.G.M., Sturkenboom M.C.J.M. Incidence of facial pain in the general population. Pain. 2009;147:122–127. doi: 10.1016/j.pain.2009.08.023. [DOI] [PubMed] [Google Scholar]
- 7.Pearce J.M.S. Glossopharyngeal neuralgia. Eur Neurol. 2006;55:49–52. doi: 10.1159/000091429. [DOI] [PubMed] [Google Scholar]
- 8.Patel A., Kassam A., Horowitz M., Chang Y.-F. Microvascular decompression in the management of glossopharyngeal neuralgia: analysis of 217 cases. Neurosurgery. 2002;50:705–710. doi: 10.1097/00006123-200204000-00004. discussion 710–711. [DOI] [PubMed] [Google Scholar]
- 9.Varrasi C., Strigaro G., Prandi P., Comi C., Mula M., Monaco F., Cantello R.M. Complex pattern of convulsive syncope in glossopharyngeal neuralgia: video/EEG report and short review. Epilepsy Behav. 2011;20:407–409. doi: 10.1016/j.yebeh.2010.12.017. [DOI] [PubMed] [Google Scholar]
- 10.Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition (beta version) Cephalalgia. 2013;33:629–808. doi: 10.1177/0333102413485658. [DOI] [PubMed] [Google Scholar]
- 11.Gaul C., Hastreiter P., Duncker A., Naraghi R. Diagnosis and neurosurgical treatment of glossopharyngeal neuralgia: clinical findings and 3-D visualization of neurovascular compression in 19 consecutive patients. J Headache Pain. 2011;12:527–534. doi: 10.1007/s10194-011-0349-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Svien H.J., Hill N.C., Daly D.D. Partial glossopharyngeal neuralgia associated with syncope. J Neurosurg. 1957;14:452–457. doi: 10.3171/jns.1957.14.4.0452. [DOI] [PubMed] [Google Scholar]
- 13.Taha J.M., Tew J.M. Long-term results of surgical treatment of idiopathic neuralgias of the glossopharyngeal and vagal nerves. Neurosurgery. 1995;36:926–930. doi: 10.1227/00006123-199505000-00006. discussion 930–931. [DOI] [PubMed] [Google Scholar]
- 14.Jamshidi A., Masroor M.A. Glossopharyngeal neuralgia with cardiac syncope: treatment with a permanent cardiac pacemaker and carbamazepine. Arch Intern Med. 1976;136:843–845. [PubMed] [Google Scholar]
- 15.Rozen T.D. Trigeminal neuralgia and glossopharyngeal neuralgia. Neurol Clin. 2004;22:185–206. doi: 10.1016/S0733-8619(03)00094-X. [DOI] [PubMed] [Google Scholar]
- 16.Brihaye J., Perier O., Smulders J., Franken L. Glossopharyngeal neuralgia caused by compression of the nerve by an atheromatous vertebral artery. J Neurosurg. 1956;13:299–302. doi: 10.3171/jns.1956.13.3.0299. [DOI] [PubMed] [Google Scholar]
- 17.Jannetta P.J. Cranial nerve vascular compression syndromes (other than tic douloureux and hemifacial spasm) Clin Neurosurg. 1981;28:445–456. doi: 10.1093/neurosurgery/28.cn_suppl_1.445. [DOI] [PubMed] [Google Scholar]
- 18.Laha R.K., Jannetta P.J. Glossopharyngeal neuralgia. J Neurosurg. 1977;47:316–320. doi: 10.3171/jns.1977.47.3.0316. [DOI] [PubMed] [Google Scholar]
- 19.Morales F., Albert P., Alberca R., de Valle B., Narros A. Glossopharyngeal and vagal neuralgia secondary to vascular compression of the nerves. Surg Neurol. 1977;8:431–433. [PubMed] [Google Scholar]
- 20.Resnick D.K., Jannetta P.J., Bissonnette D., Jho H.D., Lanzino G. Microvascular decompression for glossopharyngeal neuralgia. Neurosurgery. 1995;36:64–68. doi: 10.1227/00006123-199501000-00008. discussion 68–69. [DOI] [PubMed] [Google Scholar]
- 21.Tsuboi M., Suzuki K., Nagao S., Nishimoto A. Glossopharyngeal neuralgia with cardiac syncope: a case successfully treated by microvascular decompression. Surg Neurol. 1985;24:279–283. doi: 10.1016/0090-3019(85)90039-4. [DOI] [PubMed] [Google Scholar]
- 22.Graf C.J. Glossopharyngeal neuralgia and ossification of the stylohyoid ligament. J Neurosurg. 1959;16:448–453. doi: 10.3171/jns.1959.16.4.0448. [DOI] [PubMed] [Google Scholar]
- 23.Orton C.I. Glossopharyngeal neuralgia: its diagnosis and treatment. Br J Oral Surg. 1972;9:228–232. doi: 10.1016/s0007-117x(71)80038-0. [DOI] [PubMed] [Google Scholar]
- 24.Aguiar P.H., Tella O.I., Pereira C.U., Godinho F., Simm R. Chiari type I presenting as left glossopharyngeal neuralgia with cardiac syncope. Neurosurg Rev. 2002;25:99–102. doi: 10.1007/s101430100178. [DOI] [PubMed] [Google Scholar]
- 25.Dykman T.R., Montgomery E.B., Gerstenberger P.D., Zeiger H.E., Clutter W.E., Cryer P.E. Glossopharyngeal neuralgia with syncope secondary to tumor: treatment and pathophysiology. Am J Med. 1981;71:165–170. doi: 10.1016/0002-9343(81)90287-4. [DOI] [PubMed] [Google Scholar]
- 26.Giorgi C., Broggi G. Surgical treatment of glossopharyngeal neuralgia and pain from cancer of the nasopharynx: a 20-year experience. J Neurosurg. 1984;61:952–955. doi: 10.3171/jns.1984.61.5.0952. [DOI] [PubMed] [Google Scholar]
- 27.Sobol S.M., Wood B.G., Conoyer J.M. Glossopharyngeal neuralgia-asystole syndrome secondary to parapharyngeal space lesions. Otolaryngol Head Neck Surg. 1982;90:16–19. doi: 10.1177/019459988209000104. [DOI] [PubMed] [Google Scholar]
- 28.Waga S., Kojima T. Glossopharyngeal neuralgia of traumatic origin. Surg Neurol. 1982;17:77–79. doi: 10.1016/0090-3019(82)90051-9. [DOI] [PubMed] [Google Scholar]
- 29.Kahana E., Leibowitz U., Alter M. Brainstem and cranial nerve involvement in multiple sclerosis. Acta Neurol Scand. 1973;49:269–279. doi: 10.1111/j.1600-0404.1973.tb01299.x. [DOI] [PubMed] [Google Scholar]
- 30.Karnosh L.J., Gardner W.J., Stowell A. Glossopharyngeal neuralgia physiological consideration of the role of ninth and tenth cranial nerves: report of cases. Trans Am Neurol Assoc. 1947;72:205–207. [Google Scholar]
- 31.Giza E., Kyriakou P., Liasides C., Dimakopoulou A. Glossopharyngeal neuralgia with cardiac syncope: an idiopathic case treated with carbamazepine and duloxetine. Eur J Neurol. 2008;15:e38–e39. doi: 10.1111/j.1468-1331.2008.02097.x. [DOI] [PubMed] [Google Scholar]
- 32.Ozveren M.F., Türe U., Ozek M.M., Pamir M.N. Anatomic landmarks of the glossopharyngeal nerve: a microsurgical anatomic study. Neurosurgery. 2003;52:1400–1410. doi: 10.1227/01.neu.0000064807.62571.02. discussion 1410. [DOI] [PubMed] [Google Scholar]
- 33.Kazemi B., Akbarzadeh F. Syncopal storm caused by glossopharyngeal neuralgia. Am J Emerg Med. 2012;30(2101):e5–e7. doi: 10.1016/j.ajem.2012.03.003. [DOI] [PubMed] [Google Scholar]
- 34.Ferrante L., Artico M., Nardacci B., Fraioli B., Cosentino F., Fortuna A. Glossopharyngeal neuralgia with cardiac syncope. Neurosurgery. 1995;36:58–63. doi: 10.1227/00006123-199501000-00007. discussion 63. [DOI] [PubMed] [Google Scholar]
- 35.Evans R.W., Torelli P., Manzoni G.C. Glossopharyngeal neuralgia. Headache. 2006;46:1200–1202. doi: 10.1111/j.1526-4610.2006.00513.x. [DOI] [PubMed] [Google Scholar]
- 36.Jacobson R.R., Russell R.W. Glossopharyngeal neuralgia with cardiac arrhythmia: a rare but treatable cause of syncope. Br Med J. 1979;1:379–380. doi: 10.1136/bmj.1.6160.379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kim S.S., Lal R., Ruffy R. Bradycardic and vasodepressor syncope secondary to glossopharyngeal neuralgia from hypopharyngeal tumor. Am Heart J. 1985;109:1101–1102. doi: 10.1016/0002-8703(85)90255-8. [DOI] [PubMed] [Google Scholar]
- 38.Moretti R., Torre P., Antonello R.M., Bava A., Cazzato G. Gabapentin treatment of glossopharyngeal neuralgia: a follow-up of four years of a single case. Eur J Pain Lond Engl. 2002;6:403–407. doi: 10.1016/s1090-3801(02)00026-5. [DOI] [PubMed] [Google Scholar]
- 39.Titlic M., Jukic I., Tonkic A., Grani P., Jukic J. Use of lamotrigine in glossopharyngeal neuralgia: a case report. Headache. 2006;46:167–169. doi: 10.1111/j.1526-4610.2006.00316_2.x. [DOI] [PubMed] [Google Scholar]
- 40.Kitchener J.M., Guido M., Specchio L.M. Glossopharyngeal neuralgia responding to pregabalin. Headache. 2006;46:1307–1308. doi: 10.1111/j.1526-4610.2006.00543_3.x. [DOI] [PubMed] [Google Scholar]
- 41.Savica R., Laganà A., Calabrò R.S., Casella C., Musolino R. Vagoglossopharyngeal neuralgia: a rare case of syncope responding to pregabalin. Cephalalgia. 2007;27:566–567. doi: 10.1111/j.1468-2982.2007.01304.x. [DOI] [PubMed] [Google Scholar]
- 42.Ozenci M., Karaoguz R., Conkbayir C., Altin T., Kanpolat Y. Glossopharyngeal neuralgia with cardiac syncope treated by glossopharyngeal rhizotomy and microvascular decompression. Europace. 2003;5:149–152. doi: 10.1053/eupc.2002.0298. [DOI] [PubMed] [Google Scholar]
- 43.Khero B.A., Mullins C.B. Cardiac syncope due to glossopharyngeal neuralgia: treatment with a transvenous pacemaker. Arch Intern Med. 1971;128:806–808. [PubMed] [Google Scholar]
- 44.Johnston R.T., Redding V.J. Glossopharyngeal neuralgia associated with cardiac syncope: long term treatment with permanent pacing and carbamazepine. Br Heart J. 1990;64:403–405. doi: 10.1136/hrt.64.6.403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Weinstein R.E., Herec D., Friedman J.H. Hypotension due to glossopharyngeal neuralgia. Arch Neurol. 1986;43:90–92. doi: 10.1001/archneur.1986.00520010084029. [DOI] [PubMed] [Google Scholar]
- 46.Cicogna R., Bonomi F.G., Curnis A., Mascioli G., Bollati A., Visioli O., Rossi L. Parapharyngeal space lesions syncope-syndrome: a newly proposed reflexogenic cardiovascular syndrome. Eur Heart J. 1993;14:1476–1483. doi: 10.1093/eurheartj/14.11.1476. [DOI] [PubMed] [Google Scholar]
- 47.McLaughlin M.R., Jannetta P.J., Clyde B.L., Subach B.R., Comey C.H., Resnick D.K. Microvascular decompression of cranial nerves: lessons learned after 4400 operations. J Neurosurg. 1999;90:1–8. doi: 10.3171/jns.1999.90.1.0001. [DOI] [PubMed] [Google Scholar]
- 48.Sampson J.H., Grossi P.M., Asaoka K., Fukushima T. Microvascular decompression for glossopharyngeal neuralgia: long-term effectiveness and complication avoidance. Neurosurgery. 2004;54:884–889. doi: 10.1227/01.neu.0000114142.98655.cc. discussion 889–890. [DOI] [PubMed] [Google Scholar]