Abstract
Background:
Advancement in surgical techniques and implants has improved the ability to manage radial head and olecranon fractures. However, trends in management of these fractures are largely unstudied.
Objective:
This purpose of this study is to evaluate management trends for these common fractures.
Methods:
A retrospective review of a comprehensive Humana database was performed using Pearl Diver supercomputer (Warsaw, IN, USA) for radial head and neck (RHNF) and olecranon fractures (OF) between 2007 and 2014. Treatment methods including open reduction internal fixation (ORIF), radial head arthroplasty (RHA), and non-operative treatment were reviewed. Total reported incidence of office visits and utilization of each treatment modality were investigated. Sub-analysis with stratification by age 15-74 and greater than 75-years was performed for OF.
Results:
A total of 10,609 OF and 20,400 RHNF were identified between 2007 and 2014. A significant trend increase in the annual incidence of RHNF (266 cases/year, p<0.001) and OF (133.9 cases/year, p=0.001) was observed. A significant trend increase in annual percent utilization of RHA (0.22% per year, p=0.011) and a significant trend decrease in the annual percent utilization of ORIF (-1.0% per year, p=0.004) and non-operative management (-0.53% per year, p=0.046) was observed for RHNF. A significant trend increase was observed in percent utilization (0.40% per year, p=0.022) for OF non-operative management, especially in patients over 75 years (66% per year, p=0.034).
Conclusion:
The percentage of patients being treated with RHA is increasing. Non-operative management of OF has increased, specifically in the patients who are over 75 years.
Keywords: Elbow fracture management, Non-operative management, Olecranon fracture, Open reduction internal fixation, Radial head arthroplasty, Radial head fracture, Radial neck fracture
INTRODUCTION
Fractures of the proximal ulna and radius are the most commonly observed elbow fractures [1-3]. While minimally-displaced, stable fractures are typically managed with non-operative treatment, those that are significantly displaced or comminuted are commonly treated with surgical intervention [4, 5].
Displaced fractures of the olecranon have historically been managed with variable methods of osteosynthesis [6-11]. However, there has been a more recent emphasis on non-operative treatment of displaced olecranon fractures (OF) in the elderly [12-14]. Displaced radial head fractures have historically been managed with osteosynthesis [15, 16] or radial head excision [17]. More recently, osteosynthesis has been suggested when the displaced fragments result in a loss of forearm rotation or are combined with ligamentous injuries [18]. Furthermore, those fractures that contain three or more fragments are often managed with radial head arthroplasty (RHA), as osteosysnthesis has been shown to result in high rates of unsatisfactory outcomes [19].
While the literature has helped to outline those fractures that might best be treated with surgery, and innovations in surgical technique and surgical implants have continued to improve, national trends have not been examined to determine the impact of these advances. The purpose of this study is to examine the national trends for management of two common elbow fractures-1) radial head and neck fractures (RHNF); 2) olecranon fractures – using the Humana claims database between 2007 and 2014. We hypothesize a gradual increase in patients being treated with RHA for RHNF and non-operative management for OF compared with ORIF for these fractures during this time period.
METHODS
A retrospective review of the entire Humana database for radial head and neck fractures as well as olecranon fractures in patients over 15 years old was conducted through the use of the Pearl Diver supercomputer (Warsaw, IN, USA). This software is a publicly available Health Insurance Portability and Accountability Act-compliant database that compiles the entire Humana files into a server. Data compiled within the Humana database are derived from a combination of Medicare/Medicare Advantage and private-payers yielding 18,620,198 patients from 2007-2014. Pearl Diver software provides access to the Humana registries with the use of Current Procedural Terminology (CPT; American Medical Association, Chicago, IL, USA) codes, as well as, International Classification of Disease Ninth Edition (ICD-9) codes.
A query of the Humana database was performed for OF using ICD-9 codes 813.01 (closed fracture of olecranon process), 813.11 (open fracture of olecranon process), 813.04 (other and unspecified closed fracture of proximal end of ulna, alone), and 813.14 (other and unspecified open fractures of the proximal end of ulna, alone). Open reduction with internal fixation and non-operative treatment of OF was identified via ICD-9 and CPT codes (Table 1). A sub-analysis stratification of OF by age was untaken; patients between the ages of 15-74 years (Group A) and greater than 75 years (Group B) were reviewed.
Table 1.
Codes used for the query of Humana database.
| Procedure | Code |
|---|---|
| ORIF of Olecranon Fracture | |
| Open treatment of olecranon process with or without internal or external fixation | CPT 24685 |
| ORIF of Radial Head and Neck Fractures | |
| Open treatment of radial head or neck fracture with or without internal fixation or radial head excision | CPT 24665 |
| ORIF of Olecranon Fracture OR Radial Head and Neck Fracture* | |
| Internal fixation of bone without fracture reduction, radius and ulna | ICD-9: 78.53 |
| Open reduction of fracture with internal fixation, radius and ulna | ICD-9: 79.32 |
| Open reduction of separated epiphysis, radius and ulna | ICD-9: 79.52 |
| Non- operative Management of Olecranon Fracture | |
| Closed treatment of olecranon process; without manipulation | CPT 24670 |
| Closed treatment of olecranon process; with manipulation | CPT 24675 |
| Radial Head Arthroplasty | |
| Arthroplasty radial head; with implant | CPT 24366 |
| Open treatment of radial head or neck fracture with or without internal fixation or radial head excision; with radial head prosthetic replacement | CPT 24666 |
| Other repair of elbow | ICD-9: 81.85 |
| Non- operative Management of Radial Head and Neck Fractures | |
| Closed treatment of radial head or neck fracture; without manipulation | CPT 24650 |
| Closed treatment of radial head or neck fracture; with manipulation | CPT 24655 |
| CPT, Current Procedural Terminology (American Medical Association, Chicago, IL, USA); ICD-9, International Classification of Diseases, Ninth Edition. *These codes were used in the query of both ORIF for Olecranon fractures and ORIF of radial head and neck fractures. | |
RHNF were queried via the Humana database using ICD-9 codes 813.05 (closed fracture of head of radius), 813.15 (open fracture of neck of radius), 813.06 (closed fracture of neck of radius), 813.16 (open fracture of neck of radius), 813.07 (other and unspecified closed fracture of proximal end of radius, alone) and 813.17 (other and unspecified open fracture of proximal end of radius, alone). Radial head arthroplasty (RHA), ORIF, and non-operative treatment of RHNF were identified using ICD-9 and CPT codes (Table 1).
The incidence of reported OF and RHNF was examined and trend changes for each fracture type were reported. Utilization of non-operative management as well as surgical procedures (ORIF and radial head arthroplasty) was examined to define trend changes. The percent utilization of each treatment modality was also examined to detect any change trends in treatment selections for each fracture type.
Statistical analysis was mainly descriptive to define the incidence of each procedure throughout the study period. Linear regression models were analyzed to examine any trends in incidence of fracture type, incidence of treatment modalities chosen, as well as percent utilization for these treatment modalities using a 95% confidence interval. A p-value of <0.05 was selected to be significant. Moreover, correlational analysis using the Pearson method was used to observe any relationships between trends in incidence and concomitant trends in treatment modalities. These same correlational analyses were carried out for stratified age groups. Statistical analysis was performed with Prism 6 software (GraphPad Software, La Jolla, CA, USA).
RESULTS
A total of 20,400 RHNF were identified in the Humana population between 2007 and 2014 (Table 2). A significant trend increase in annual reported incidence of RHNF was observed (Fig. 1); R2= 0.88; p<0.001; 95% CI [169.2, 363.2]) at a rate of 266 cases per year. A total of 1,028 RHNF were managed with a RHA with a significant trend increase in the annual percentage of RHNF managed with RHA at a rate of 0.22% per year (Fig. 2); R2= 0.68; p=0.011; 95% CI [0.07, 0.36]). A total of 5,612 RHNF were treated with ORIF with a significant decrease trend in the annual percentage of RHNF fractures managed with ORIF at a rate of -1.0% per year (R2= 0.78; p=0.004; 95% CI [-1.53, -0.46]). A total of 5,887 RHNF were managed non-operatively with a significant decrease trend observed in annual percentage of RHNF managed without surgery at a rate of -0.53% per year (R2= 0.51; p=0.046; 95% CI [-1.06, -0.01]).
Table 2.
Annual RHNF incidence and management among the Humana population between 2007 and 2014.
| Year | RHNF | RHA | % Use of RHA | ORIF | % Use of ORIF | Non-op Tx | % Use of Non-op Tx |
|---|---|---|---|---|---|---|---|
| 2007 | 1,773 | 77 | 4.34% | 545 | 30.74% | 550 | 31.02% |
| 2008 | 2,020 | 88 | 4.36% | 584 | 28.91% | 574 | 28.42% |
| 2009 | 2,122 | 102 | 4.81% | 676 | 31.86% | 673 | 31.72% |
| 2010 | 2,319 | 93 | 4.01% | 671 | 28.93% | 684 | 29.50% |
| 2011 | 2,462 | 129 | 5.24% | 704 | 28.59% | 737 | 29.94% |
| 2012 | 2,631 | 141 | 5.36% | 723 | 27.48% | 771 | 29.30% |
| 2013 | 3,156 | 182 | 5.77% | 785 | 24.87% | 885 | 28.04% |
| 2014 | 3,917 | 216 | 5.51% | 924 | 23.59% | 1,013 | 25.86% |
| Totals | 20,400 | 1,028 | 5,612 | 5,887 | |||
|
Trend p-value |
<0.001 | <0.001 | 0.011 | <0.001 | 0.004 | <0.001 | 0.046 |
Fig. (1).
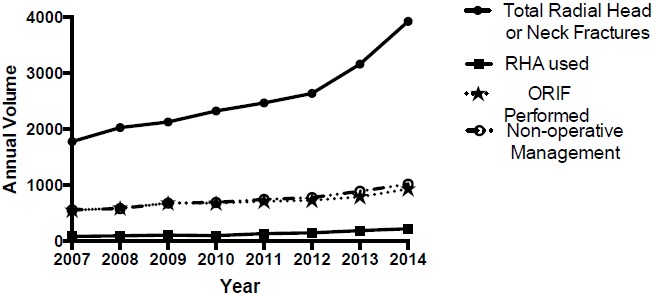
Radial head & neck fractures and management.
Fig. (2).
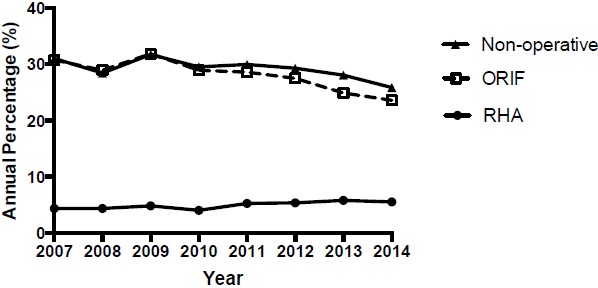
Management of radial head and neck fracture.
A total of 10,609 OF were identified in the Humana population between 2007 and 2014 (Table 3). A significant trend increase in the annual incidence of olecranon fractures (Fig. 3); R2= 0.86; p=0.001; 95% CI [78.88, 188.9]) was observed at a rate of 133.9 fractures per year. A total of 8,146 OF were managed with ORIF with no significant trend change in the annual percentage of OF treated with ORIF (R2= 0.12; p=0.392; 95% CI [-2.28, 1.03]). A total of 1,225 OF were managed non-operatively with significant trend increase observed in the annual percentage of OF treated without surgery at a rate of 0.40% per year (Fig. 4); R2= 0.61; p=0.022; 95% CI [0.08, 0.72]).
Table 3.
Annual OF incidence and management among the Humana population between 2007 and 2014.
| Year | Incidence of OF | ORIF | % Use of ORIF | Non-op Tx | % Use of Non-op Tx |
|---|---|---|---|---|---|
| 2007 | 948 | 726 | 76.58% | 98 | 10.34% |
| 2008 | 1,030 | 787 | 76.41% | 102 | 9.90% |
| 2009 | 1,098 | 910 | 82.88% | 112 | 10.20% |
| 2010 | 1,261 | 968 | 76.76% | 144 | 11.42% |
| 2011 | 1,312 | 1,040 | 79.27% | 148 | 11.28% |
| 2012 | 1,287 | 1,070 | 83.14% | 169 | 13.13% |
| 2013 | 1,649 | 1,227 | 74.41% | 218 | 13.22% |
| 2014 | 2,024 | 1,418 | 70.06% | 234 | 11.56% |
| Totals | 10,609 | 8,146 | 1,225 | ||
| Annual trend p-value | 0.001 | <0.001 | 0.392 | <0.001 | 0.022 |
Fig. (3).
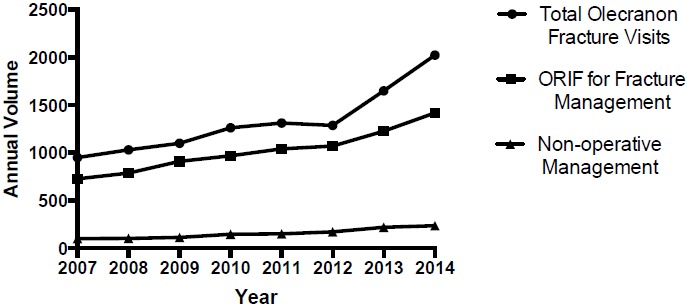
Annual olecranon fractures & management.
Fig. (4).
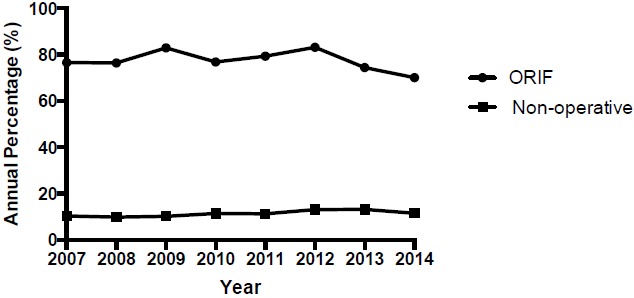
Management of olecranon fractures.
Stratification of olecranon fracture management by age demonstrated differences. Group A (15-74 years) showed a significant trend increase in annual incidence of OF at a rate of 70.92 fractures per year (R2= 0.78; p=0.004; 95% CI [32.99, 108.8]), utilization of ORIF at a rate of 50.56 cases per year (R2= 0.87; p<0.001; 95% CI [31.06, 70.06]), and utilization of non-operative management, at a rate of 10.29 cases per year (R2= 0.85; p=0.001; 95% CI [5.92, 14.65]), of olecranon fractures. These increases in management had a significantly strong correlation to the increase in total olecranon fractures for both ORIF (r=0.959; p<0.001) and non-operative management (r=0.954; p<0.001). There were no significant trends observed in percentage of olecranon fractures treated with ORIF (R2= 0.01; p=0.835; 95% CI [-2.26, 1.90]) and the percentage managed non-operatively (R2= 0.34; p=0.126; 95% CI [-0.11, 0.67]). In Group B (≥75 years), a significant trend increase in annual incidence of OF at a rate of 69.29 fractures per year (R2= 0.93; p<0.001; 95% CI [50.86, 87.71]), utilization of ORIF at a rate of 49.42 cases per year (R2= 0.95; p<0.001; 95% CI [38.54, 60.29]), and utilization of non-operative management at a rate of 11.35 cases per year (R2=0.93; p<0.001; 95% CI [8.27, 14.42]) of OF was seen. Significantly strong correlations were observed between annual incidence of OF and utilization of ORIF (r=0.985; p<0.001) and utilization of non-operative treatment (r=0.945; p<0.001). No significant trend in percentage of OF managed with ORIF (R2= 0.27; p=0.190; 95% CI [-3.30, 0.81]) was seen. However, there was an increase in the annual percentage of OF treated non-operatively at a rate of 0.66% per year (R2= 0.56; p=0.034; 95% CI [0.07, 1.25]).
DISCUSSION
Results of this study show a recent shift in the management of both olecranon and radial head and neck fractures among the Humana population. A significantly increased percentage of patients are being treated with non-operative management for olecranon fractures and radial head arthroplasty is now used more frequently for radial head and neck fractures. Furthermore, in the over-75-year-old patient population, non-operative management of olecranon fractures is increasing.
The current study shows that the incidence of radial head fractures is increasing. Treatment options for these fractures have included non-operative therapy, radial head resection, ORIF, and RHA. Non-operative treatment has historically been recommended for stable, nondisplaced fractures [20, 21]. Radial head resection has been utilized since at least the early 1900s [22] and, with the advent of the Mason classification, was initially recommended for displaced or comminuted fractures [21]. ORIF was later recommended as treatment for comminuted radial head fractures as it was found to have satisfactory outcomes and avoided many of the complications of radial head resection [15, 16]. Management with radial head prostheses were initially recommended for radial head fractures previously treated with radial head excision that resulted in a grossly unstable elbow [23].
Recent findings have re-shaped the management of radial head fractures Table 4. Radial head resection has mostly fallen out of favor due to the recognition of the radial head as a secondary stabilizer of the elbow and poor outcomes and instability often associated with the procedure [24]. Mason type II fractures have been successfully treated without surgery [20, 25] and ORIF of fractures with 3 or more fragments have been shown to have worse outcomes [19]. Several randomized control trials have shown the superiority of RHA compared to ORIF in terms of post-operative complications and outcome scores for Mason type III and IV fractures [26, 27]. These findings have likely contributed to the trend increase in utilization of RHA (p<0.001) observed in the current study, and likely contributed to the decreasing trends in utilization of ORIF (p=0.004) and non-operative management (p=0.046) for radial head and neck fractures. Additional factors that may have contributed to these trends include the shorter operative time with RHA, improvement of radial head implant technology and surgical techniques, and the increased technical challenge posed by ORIF in comminuted fractures.
Table 4.
Summary of study findings that reshaped the management of radial head fractures.
| Method of treatment discussed | Authors | Population | Summary of key findings |
|---|---|---|---|
| Radial head resection | Hall et al. [24] | Case series: 42 patients evaluated for elbow or forearm problems after radial head resection. | 7 patients (17%) were diagnosed with posterolateral rotational instability of the elbow. |
| Non-operative | Akesson et al. [20] | 49 patients treated non-operatively for Mason type-IIa radial head fractures. 6 patients had delayed radial head excision for poor outcome. | 40 of the 49 patients (82%) had no subjective complaints after non-operative treatment. Injured elbows had significantly lower ROM and higher degenerative changes compared to non-injured elbows but this was thought to be clinically insignificant by the authors. |
| Herbertsson et al. [25] | Retrospective study: 100 patients treated non-operatively, with radial head resection, or with ORIF for Mason type-II or III radial head and neck fractures. Mean follow-up was 19 years. | 77 of the 100 patients had no symptoms at follow-up. Mean ROM deficits were minor (2 degree flexion, 3 degree extension, and 3 degree supination deficits). 19 patients had primary radial head excision while 9 patients had a secondary procedure performed due to residual pain. | |
| ORIF | Ring et al. [19] | Retrospective study: 56 patients treated with ORIF for intra-articular radial head fracture. | 14 out of 15 patients with Mason Type-3 comminuted radial head fractures with at least 3 articular fragments had unsatisfactory results (based on failure of fixation or nonunion requiring radial head excision, a fair or poor result with the system of Broberg and Morrey, or recovery of < 100 degrees of forearm rotation). |
| RHA | Yan et al. [27] | RCT: 39 patients with Mason type-3 radial head fractures and associated terrible triad injuries of the elbow | RHA group had a significant shorter surgery duration, fewer post-surgical complications, and better clinical outcomes compared to the ORIF group. |
| Chen et al. [26] | RCT: 45 patients with unstable, multi-fragmented fractures of the radial head treated with either ORIF or RHA | Better outcome scores and lower complication rates among the RHA group compared to the ORIF group. |
Trends in the management of olecranon fractures were found to have changes as well. While no significant change was noted in the percent utilization of ORIF, there were trend increases observed in the percent utilization of non-operative management. This was specifically noted for patients over the age of 75, where the percentage of non-operative treatment was found to have increased. Treatment options for olecranon fractures have historically consisted of non-operative therapy and various methods of fracture fixation including k-wires, tension-band, intra-medullary screw, intra-medullary nail, and plate fixation [7-11]. Complications were found to be linked to fixation methods and thus fragment excision with repair of the triceps insertion was considered as an alternative treatment [6, 28]. Improvements in limiting these complications led to resurgence in the use of ORIF [29]. However, relatively recent articles suggest non-operative treatment as an option for low-demand elderly patients [12-14], thus re-shaping the management of olecranon fractures in this age group (Table 5). Veras Del Monte et al. reviewed non-operative management in 12 elderly patients and reported good short-term clinical outcomes with 92% excellent patient satisfaction and 67% of patients reporting no pain. No patients reported limitations in their daily activities [14]. In a retrospective review of 43 patients with a mean age of 76 years, Duckworth et al. reported 72% of patients had excellent or good short-term outcomes, with 23 patients available for long-term follow up and an overall patient satisfaction rating of 91% [12]. These findings have likely contributed to the significant trend increase in the percent utilization of non-operative treatment of olecranon fractures in patients aged over 75 years observed in the current study.
Table 5.
Summary of study findings that reshaped the management of olecranon fractures in elderly patients.
| Authors | Population | Summary of key findings |
|---|---|---|
| Veras Del Monte et al. [14] | Retrospective study: 12 elderly patients (mean age 81.8 years) treated non-operatively for displaced olecranon fractures. | 92% of patients had excellent satisfaction and 67% of patients reported no pain. |
| Duckworth et al. [12] | Trauma database study: 43 older patients (mean age 76 years) treated non-operatively for olecranon fractures. | Short-term follow-up (mean 4 months): 72% of patients had excellent or good outcomes. Long-term follow-up (mean 6 years): Overall patient satisfaction rating of 91%. |
| Gallucci et al. [13] | Retrospective study: 28 elderly patients (mean age 82 years) treated non-operatively for displaced olecranon fractures. | Median VAS pain score was 1.1 out of 10 and the mean satisfaction score was 9 out of 10. Non-union occurred in 85% of patients but the authors thought this to be irrelevant to final outcomes. |
This study is not without limitations. First, the analysis is limited to the Humana database. Selection bias may exist as the Humana patient population may not be representative of the entire country. Additionally, the accuracy of the data is contingent on proper coding practices. More than one indication for common elbow fracture might have been coded (i.e., olecranon fracture and radial head fracture) and there may be overlap in treatment modality (ICD-9 79.32 is ORIF of radius and ulna). In addition, the use of ICD-9 codes allows for less specificity of fracture type or treatment. The major strength of this study relates to the completeness of the data. The PearlDiver database represents complete data for the entire Humana private-payer population.
CONCLUSION
A shift in management trends for radial head and neck fractures and olecranon fractures among the Humana population has been found in recent years. The percentage of patients being treated with RHA for radial head and neck fractures is increasing. Additionally, non-operative management of olecranon fractures has increased in recent years; more so amongst patients aged 75 years or older.
ACKNOWLEDGEMENTS
Matthew Motisi, DO: designed research study, wrote/reviewed paper
Jennifer Kurowicki, MD: performed data extraction, wrote/reviewed paper
Derek D. Berglund, MD: performed literature review, wrote/reviewed paper
Jacob J. Triplet, DO: performed literature review, wrote/reviewed paper
Shanell Disla, BS, CCRP: wrote/reviewed paper
Timothy Niedzielak, BS: performed data analysis, wrote/reviewed paper
Jonathan C. Levy, MD: wrote/reviewed paper
LIST OF ABBREVIATIONS
- OF
= Olecranon fractures
- ORIF
= Open reduction and internal fixation
- RHA
= Radial head arthroplasty
- RHNF
= Radial head and neck fractures
CONFLICT OF INTEREST
Jonathan C. Levy, MD is a paid consultant for DJO Orthopaedics and Globus Medical, and he receives royalties from DJO Orthopaedics and Innomed.
No funding was obtained for this study.
Timothy Niedzielak, BS has no financial benefits.
Matthew Motisi, DO has no financial benefits.
Jennifer Kurowicki, MD has no financial benefits.
Derek D. Berglund has no financial benefits.
Jacob J. Triplet, DO has no financial benefits.
Shanell Disla, BS, CCRP has no financial benefits.
REFERENCES
- 1.Duckworth A.D., Clement N.D., Jenkins P.J., Aitken S.A., Court-Brown C.M., McQueen M.M. The epidemiology of radial head and neck fractures. J. Hand Surg. Am. 2012;37(1):112–119. doi: 10.1016/j.jhsa.2011.09.034. [DOI] [PubMed] [Google Scholar]
- 2.Kaas L., van Riet R.P., Vroemen J.P., Eygendaal D. The epidemiology of radial head fractures. J. Shoulder Elbow Surg. 2010;19(4):520–523. doi: 10.1016/j.jse.2009.10.015. [DOI] [PubMed] [Google Scholar]
- 3.Duckworth A.D., Clement N.D., Aitken S.A., Court-Brown C.M., McQueen M.M. The epidemiology of fractures of the proximal ulna. Injury. 2012;43(3):343–346. doi: 10.1016/j.injury.2011.10.017. [DOI] [PubMed] [Google Scholar]
- 4.Burkhart K.J., Wegmann K., Müller L.P., Gohlke F.E. Fractures of the radial head. Hand Clin. 2015;31(4):533–546. doi: 10.1016/j.hcl.2015.06.003. [DOI] [PubMed] [Google Scholar]
- 5.Veillette C.J., Steinmann S.P. Olecranon fractures. Orthop. Clin. North Am. 2008;39(2):229–236. doi: 10.1016/j.ocl.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 6.Adler S., Fay G.F., Macausland W.R. Treatment of olecranon fractures. Indications for excision of the olecranon fragment and repair of the triceps tendon. J. Trauma Inj. Infect. Crit. Care. 1962;2:597–602. doi: 10.1097/00005373-196211000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Flinterman H.J., Doornberg J.N., Guitton T.G., Ring D., Goslings J.C., Kloen P. Long-term outcome of displaced, transverse, noncomminuted olecranon fractures. Clin. Orthop. Relat. Res. 2014;472(6):1955–1961. doi: 10.1007/s11999-014-3481-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bailey C.S., MacDermid J., Patterson S.D., King G.J. Outcome of plate fixation of olecranon fractures. J. Orthop. Trauma. 2001;15(8):542–548. doi: 10.1097/00005131-200111000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Holdsworth B.J., Mossad M.M. Elbow function following tension band fixation of displaced fractures of the olecranon. Injury. 1984;16(3):182–187. doi: 10.1016/0020-1383(84)90156-6. [DOI] [PubMed] [Google Scholar]
- 10.Argintar E., Cohen M., Eglseder A., Edwards S. Clinical results of olecranon fractures treated with multiplanar locked intramedullary nailing. J. Orthop. Trauma. 2013;27(3):140–144. doi: 10.1097/BOT.0b013e318261906e. [DOI] [PubMed] [Google Scholar]
- 11.Johnson R.P., Roetker A., Schwab J.P. Olecranon fractures treated with AO screw and tension bands. Orthopedics. 1986;9(1):66–68. doi: 10.3928/0147-7447-19860101-11. [DOI] [PubMed] [Google Scholar]
- 12.Duckworth A.D., Bugler K.E., Clement N.D., Court-Brown C.M., McQueen M.M. Nonoperative management of displaced olecranon fractures in low-demand elderly patients. J. Bone Joint Surg. Am. 2014;96(1):67–72. doi: 10.2106/JBJS.L.01137. [DOI] [PubMed] [Google Scholar]
- 13.Gallucci G.L., Piuzzi N.S., Slullitel P.A., Boretto J.G., Alfie V.A., Donndorff A., De Carli P. Non-surgical functional treatment for displaced olecranon fractures in the elderly. Bone Joint J. 2014;96-B(4):530–534. doi: 10.1302/0301-620X.96B4.33339. [DOI] [PubMed] [Google Scholar]
- 14.Veras Del Monte L., Sirera Vercher M., Busquets Net R., Castellanos Robles J., Carrera Calderer L., Mir Bullo X. Conservative treatment of displaced fractures of the olecranon in the elderly. Injury. 1999;30(2):105–110. doi: 10.1016/S0020-1383(98)00223-X. [DOI] [PubMed] [Google Scholar]
- 15.Geel C.W., Palmer A.K., Ruedi T., Leutenegger A.F. Internal fixation of proximal radial head fractures. J. Orthop. Trauma. 1990;4(3):270–274. doi: 10.1097/00005131-199004030-00006. [DOI] [PubMed] [Google Scholar]
- 16.Sanders R.A., French H.G. Open reduction and internal fixation of comminuted radial head fractures. Am. J. Sports Med. 1986;14(2):130–135. doi: 10.1177/036354658601400206. [DOI] [PubMed] [Google Scholar]
- 17.Broberg M.A., Morrey B.F. Results of delayed excision of the radial head after fracture. J. Bone Joint Surg. Am. 1986;68(5):669–674. doi: 10.2106/00004623-198668050-00005. [DOI] [PubMed] [Google Scholar]
- 18.Pike J.M., Athwal G.S., Faber K.J., King G.J. Radial head fracturesan update. J. Hand Surg. Am. 2009;34(3):557–565. doi: 10.1016/j.jhsa.2008.12.024. [DOI] [PubMed] [Google Scholar]
- 19.Ring D., Quintero J., Jupiter J.B. Open reduction and internal fixation of fractures of the radial head. J. Bone Joint Surg. Am. 2002;84-A(10):1811–1815. doi: 10.2106/00004623-200210000-00011. [DOI] [PubMed] [Google Scholar]
- 20.Akesson T., Herbertsson P., Josefsson P.O., Hasserius R., Besjakov J., Karlsson M.K. Primary nonoperative treatment of moderately displaced two-part fractures of the radial head. J. Bone Joint Surg. Am. 2006;88(9):1909–1914. doi: 10.2106/JBJS.E.01052. [DOI] [PubMed] [Google Scholar]
- 21.Mason M.L. Some observations on fractures of the head of the radius with a review of one hundred cases. Br. J. Surg. 1954;42(172):123–132. doi: 10.1002/bjs.18004217203. [DOI] [PubMed] [Google Scholar]
- 22.Hammond R., III Fracture of the head and neck of the radius. Ann. Surg. 1910;52(2):207–214. doi: 10.1097/00000658-191008000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Harrington I.J., Tountas A.A. Replacement of the radial head in the treatment of unstable elbow fractures. Injury. 1981;12(5):405–412. doi: 10.1016/0020-1383(81)90012-7. [DOI] [PubMed] [Google Scholar]
- 24.Hall J.A., McKee M.D. Posterolateral rotatory instability of the elbow following radial head resection. J. Bone Joint Surg. Am. 2005;87(7):1571–1579. doi: 10.2106/JBJS.D.02829. [DOI] [PubMed] [Google Scholar]
- 25.Herbertsson P., Josefsson P.O., Hasserius R., Karlsson C., Besjakov J., Karlsson M., Long-Term Follow-Up Study Uncomplicated Mason type-II and III fractures of the radial head and neck in adults. A long-term follow-up study. J. Bone Joint Surg. Am. 2004;86-A(3):569–574. doi: 10.2106/00004623-200403000-00016. [DOI] [PubMed] [Google Scholar]
- 26.Chen X., Wang S.C., Cao L.H., Yang G.Q., Li M., Su J.C. Comparison between radial head replacement and open reduction and internal fixation in clinical treatment of unstable, multi-fragmented radial head fractures. Int. Orthop. 2011;35(7):1071–1076. doi: 10.1007/s00264-010-1107-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yan M., Ni J., Song D., Ding M., Liu T., Huang J. Radial head replacement or repair for the terrible triad of the elbow: which procedure is better? ANZ J. Surg. 2015;85(9):644–648. doi: 10.1111/ans.13060. [DOI] [PubMed] [Google Scholar]
- 28.Macko D., Szabo R.M. Complications of tension-band wiring of olecranon fractures. J. Bone Joint Surg. Am. 1985;67(9):1396–1401. doi: 10.2106/00004623-198567090-00015. [DOI] [PubMed] [Google Scholar]
- 29.Gartsman G.M., Sculco T.P., Otis J.C. Operative treatment of olecranon fractures. Excision or open reduction with internal fixation. J. Bone Joint Surg. Am. 1981;63(5):718–721. doi: 10.2106/00004623-198163050-00005. [DOI] [PubMed] [Google Scholar]


