Abstract
Waiting is a common phenomenon in the doctor's waiting room. The purpose of this audit is to assess patient waiting time and doctor consultation time in a primary healthcare clinic and to formulate strategies for improvement. This audit was conducted at a primary care clinic for 4 weeks using the universal sampling method. All patients who attended the clinic during this period was included in the study except for those who required more time to be seen such as those who were critically ill, aggressive or those who came for repeat medication or procedures only without needing to see the doctor. The time of arrival was captured using the queue management system (QMS) and then the patient was given a timing chit which had to be manually filled by the staff at every station. The waiting time for registration, pre-consultation, consultation, appointment, payment and pharmacy were recorded as well as consultation time. The data were entered into the statistical software SPSS version 17 for analysis. version 17. Results showed that more than half of the patients were registered within 15 minutes (53%) and the average total waiting time from registration to seeing a doctor was 41 minutes. Ninety-nine percentage of patients waited less than 30 minutes to get their medication. The average consultation time was 18.21 minutes. The problems identified in this audit were addressed and strategies formulated to improve the waiting and consultation time were carried out including increasing the number of staff at the registration counter, enforcing the staggered appointment system for follow-up patients and improving the queuing system for walk-in patients.
Keywords: Clinical audit, patient waiting time, consultation time, primary care, general practice
Introduction
“Patience is so valuable I'm willing to wait forever to achieve it. And while I wait, I may as well get busy being short-tempered.” This is a quote taken from “This Book Is Not For Sale” by Jarod Kintz,1 an appropriate saying for patients who spend a lot of time waiting to see a doctor. Many studies have shown an inverse relationship between waiting time and patient satisfaction.2–4 This has become a major concern for hospital administrators and policymakers because it is a measure of organisational efficiency.5 Waiting time as well as consultation time are the main factors that affect patient and consumer satisfaction.2,6–9
Patients are aware that they should wait to see a doctor; however, there is no known acceptable ‘waiting’ or ‘consultation’ time. Evidence shows that patients are less likely to be dissatisfied if their waiting time is within 30 minutes.4 Overseas studies have shown that patients are willing to wait an average of between 30 and 45 minutes to see a doctor.6,8 In Malaysia, the average waiting time in hospital outpatient departments is between 1 to 2 hours.10 The experience while waiting can also affect patient satisfaction and is influenced by other factors such as the condition and attractiveness of the waiting area.4,11,12 The availability of entertainment such as television, health information and reading materials may improve the anticipation of waiting.4,11,12 The presence of helpful and friendly staff is also important to improve the waiting experience.4,11,12
High number of patients, shortage of staff and aging equipment are among the factors contributing to a lengthy waiting time.6,12 A long and complicated registration or work process with unnecessary duplication of tests can prolong waiting time in clinics.6,13
Consultation length often varies from one country to another and is determined by both patient's and doctor's characteristics. Studies from abroad have shown that the average consultation time in a primary care setting ranges between 10 to 15 minutes.14,15 In general, studies have shown that patients prefer longer consultations.16 Doctors with longer consultations tend to prescribe less and offer more advice on lifestyle and other health-promoting activities.17 Consultation time increases to nearly twice as long when doctors explore psychosocial issues and this is associated with better recognition and handling of psychosocial problems.16–18
There is insufficient published data to support the acceptable waiting and consultation time in primary healthcare clinics in Malaysia. The purpose of this audit is to assess patient waiting time and doctor consultation time in a primary healthcare clinic and to formulate strategies to improve the clinic waiting time and consultation time.
Methods
This audit was conducted at a primary care clinic in Gombak District from 28 July 2015 until 24 August 2015. A four-week study period was perceived as sufficient for data collection to include clinics run by family medicine specialists (FMS), medical officers (MO) and a mixed sample of follow-up for non-communicable disease (NCD) patients and acute walk-in patients.
Clinic setting
The primary care clinic is situated in a large district of Gombak covering a total population of 682,996 people. It is situated in the ground floor with disabled access and parking provided and ready access to radiology, laboratory and referral services to other specialties. The primary care clinic has an average of 60 patient attendances per day. There is a staff located at the registration and appointment counter and another staff at the payment counter together with two nursing assistants and two nurses. There are seven consultation rooms with two FMS and five MO.
Following the family doctor concept, NCD or “follow-up” patients were given a specific appointment to see a named doctor who follows them up throughout their care. The walk-in patient who attended the clinic would be seen by any of the MO available. At the time of this audit, the clinic had not enforced the staggered appointment system and follow-up patients were still seen according to their arrival instead of their appointment time.
Sampling and recruitment
The study was conducted using a universal sampling method. All patients who attended the clinic during this study period were included in the study. The exclusion criteria included patients who were critically ill requiring referral or admission, psychiatric patients who were aggressive, those who came for repeat medications, investigations or procedures only without seeing a doctor, those who were involved in student teaching sessions and those who attended the primary care clinic as well as other specialist clinics. For example rehabilitation on the same day.
Training of staffs for the audit
A short briefing session among all staff was held prior to the audit to ensure proper time recording on the timing chit. An e-mail reminder and WhatsApp messages were sent to all MO and specialists prior and during the audit period. A reminder to use a pre-synchronised time on the Profdoc HIS system was given to staffs before and during the audit period.
Defining standards for acceptable waiting time practice
There have been various unpublished audit on waiting time done in primary care settings; however, the agreed and acceptable standards of practice were difficult to ascertain. The standard for this audit was defined according to the recommendation of the Malaysian Ministry of Health's patient charter, which stated that the waiting time for patients to be seen by the first provider in hospital outpatients and public health clinics should not exceed 30 minutes upon arrival with a standard of 80% target of achievement. It also stated that the dispensing of medication from the time the pharmacy received the patient's prescription should not exceed 30 minutes with a standard target of 95%.19,20
Process of data collection to determine the waiting and consultation time and statistical analysis
The process of recorded timing as demonstrated by Figure 1 started with the time the patient arrived and pushed the QMS button allowing the time to be captured in the QMS queuing slip. When the patient was called to the registration counter by the QMS number, he would then be given a timing chit containing his demographic details and time in and out to be filled by the dedicated staff at every station. The timing chit was stapled onto the patient's registration card and carried along to every station he attended. The pre-consultation waiting time was recorded by the nursing staffs in the vital signs assessment room. The consultation waiting time was recorded by the doctor (FMS or MO). The waiting time for appointment and payment was recorded at the registration and payment counter respectively. The completed timing chit was then kept by the staff at the payment counter and collected for data entry.
The timing for medication collection at the pharmacy was recorded by the electronic pharmacy record of the pharmacy information system. Data on demography and relevant clinical information were accessed via the electronic medical record system, which is
Profdoc HIS. All relevant data were recorded manually in audit proforma before being entered into the SPSS version 17.0 to be analysed. Descriptive analysis was conducted with independent T-test for significance and p value set at <0.01. The results of the audit were presented at a clinical meeting and recommended changes and improvements were made.
Figure 1.
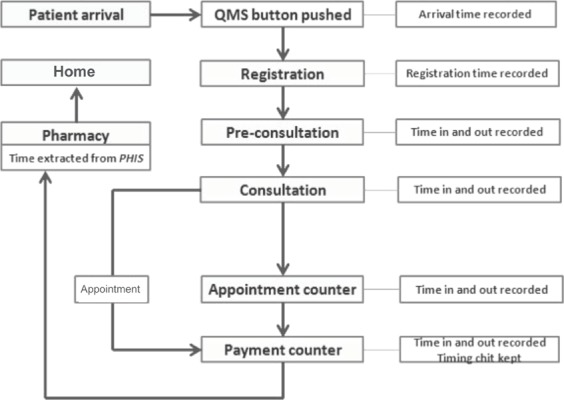
Flow chart showing patient's movement in the clinic from arrival to departure
Results
A total of 820 patients’ data who attended the clinic during this study period were collected and out of this, 64 fulfilled the exclusion criteria, therefore, a total of 756 patients were included in the study.
Table 1.
Demographic details of the patients in this study
| Variables | Frequency (n) (%) | Mean (SD) |
|---|---|---|
| All subjects, n (%) | 756 (100) | |
| Age | 48.8 (19.8) | |
| 0–12 years | 52 (6.9) | |
| 13–60 years | 463 (61.2) | |
| 61 years and above | 241 (31.9) | |
| Gender | ||
| Male | 312 (41.3) | |
| Female | 444 (58.7) | |
| Race | ||
| Malay | 594 (78.6) | |
| Chinese | 79 (10.4) | |
| Indian | 72 (9.5) | |
| Others | 11(1.5) | |
| Visit type | ||
| Walk-in | 327 (43.3) | |
| Follow-up | 429 (56.7) | |
| Payment | ||
| Pay | 244 (32.3) | |
| Guarantee letter | 512 (67.7) | |
| Patient type | ||
| No disability | 713 (94.3) | |
| Disabled (walking disability) | 42 (5.6) | |
| Disabled (blind, mute or deaf) | 1 (0.1) | |
| Doctor-in charge | ||
| Specialist | 83 (11) | |
| Medical officer | 673 (89) | |
| Stat procedures | ||
| No stat investigation | 593 (78.4) | |
| X-ray | 25 (3.3) | |
| Laboratory tests | 49 (6.5) | |
| ECG | 21 (2.8) | |
| Other | 37 (4.9) | |
| Multiple | 31 (4.1) |
In Table 2, the mean age of patients was 48.8 years with a standard deviation ± 19.8. The percentage of male patients were 41.3% and female patients were 58.7%. The majority were Malays followed by Chinese and Indians.
Table 2.
Definition of waiting and consultation time and the average patient waiting time for each clinic process and the percentage achievement according to the set criteria
| Waiting time | The definition of waiting or consultation time | Set target criteria | Average time (mins) | Percentage achievement to target criteria (%) |
|---|---|---|---|---|
| For registration | The time of arrival at the clinic to the time of registration at the registration counter | The documented waiting time should be <15 minutes | 17.20 | 53.44 |
| Pre-consultation | The time taken from registration at the registration counter to being assessed by the staff nurse at pre-consultation room | The documented waiting time should <30 minutes | 13.66 | 90.08 |
| Consultation | The time taken from completed assessment by the staff nurse to consultation by the MO or specialist in the consultation room | The documented waiting time should be <30 minutes | 24.05 | 72.35 |
| Pharmacy | The time taken from acknowledgement of medication prescription to dispensing medication | The documented waiting time should be <30 minutes | 0.68 | 99.80 |
| Total waiting time from registration to consultation | The time from registration to consultation by the MO or specialist in the consultation room | The documented total should be <90 minutes | 41.06 | 91.93 |
| Appointment counter | The time from completed consultation by the MO or specialist to being called at the appointment counter | The documented waiting time counter should be <15 minutes. (N = 756) | 11.60 | 73.65 |
| Payment counter | The time from completed consultation by the MO or specialist to acknowledgement at the payment counter | The documented waiting time should be <15 minutes. (N = 756) | 9.73 | 83.66 |
| Consultation time | The time taken for patient to enter the consultation room to the end of the consultation by the MO or specialist | The documented consultation time between the MO/ specialist and patient is between 10 and 20 minutes | 18.21 | 41.80 |
Figure 2 shows that the majority of patients (91.93%) waited for less than 90 minutes in total to see the doctor.
Figure 2.
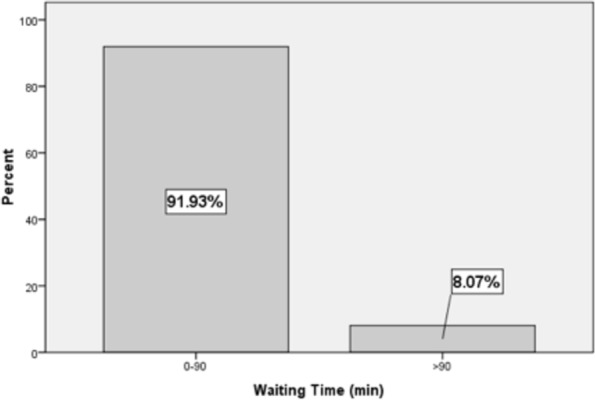
Total waiting time from registration counter to consultation with doctor (N = 756)
Figure 3 shows the consultation time with the doctor and that most patients (41.90%) spent between 11 and 20 minutes with the doctor and 19.05% spent between 21 and 30 minutes.
Figure 3.
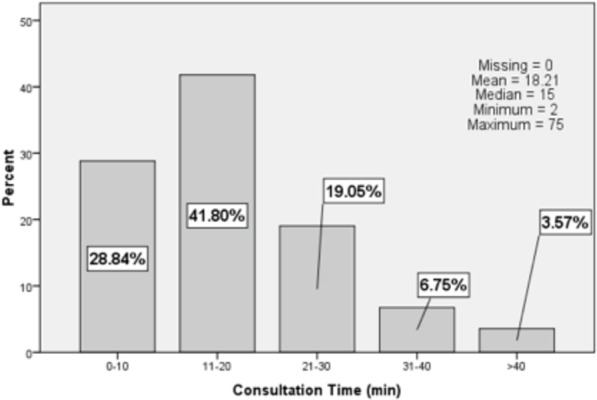
Bar chart of doctor consultation time (time patient spends with the doctor in the consulting room) (N = 756)
Figure 4 shows the mean consultation time for diagnoses categorised by systems and it was found that the longest consultation was for patients consulting for psychiatry problems followed by oncology. Independent T-test showed significant results (p < 0.001) for psychiatry versus non-psychiatry and oncology versus non-oncology (p < 0.005). The shortest consultation time was for paediatrics and haematological cases.
Figure 4.
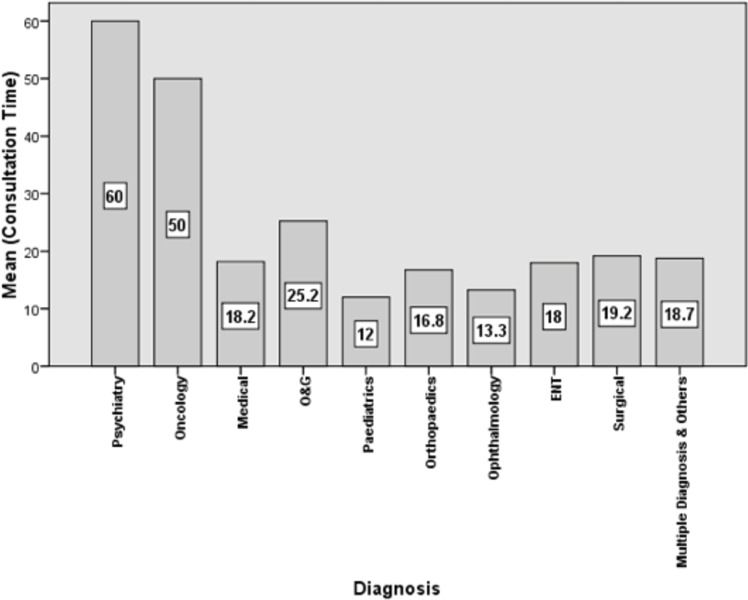
Bar chart of the mean consultation time according to different systemic diagnosis
Discussion
The positive outcome from this study was that the clinic achieved the target adopted from the Ministry of Health patient charter. A 2011 study of outpatient waiting time in 21 hospitals in Malaysia found that the average waiting time to see the doctor was 60 minutes.10 A study in Kedah found that patients who waited less than 2 hours were more satisfied with the outpatient service compared to those who waited for more than 2 hours.2 In comparison, this clinic achieved a good average total waiting time of 41 minutes to see the doctor and 92% of patients achieved the target of waiting to see the doctor within or less than 90 minutes.
There were several problems identified from this study that needed to be rectified. A high percentage of patients were still waiting an unnecessarily long time to be registered and to see the doctor. Registration should be a quick and simple process. We identified that the long waiting time is due to long queues caused by the registration counter being manned by one clerical staff who is also in charge of giving appointments to patients. Lack of staffing is a known contributor to lengthy waiting time in hospital outpatients and public health clinics.12 A recommendation was made to increase the number of registration staff to two members to cope with the tasks.
Another contributing factor was the tendency for patients to arrive earlier than their given appointment, hence arriving at the same time in large numbers. A recommendation was made to enforce the staggered appointment system for follow-up patients and improve the clinic patient scheduling system. A study showed that early arrivals were common despite warnings and reminders to arrive at the scheduled time.6 Scheduling is important to ensure a smooth clinic process and to reduce waiting times. A study of scheduled model found that patients who were given an appointment time and arrived at the appropriate time had shorter waiting time than those who walked in without an appointment.21 Applying a more effective scheduling system may also improve waiting time such as scheduling appointments according to expected consultation time.22
Scheduling should reflect the needs of the clinic and the type of patients attending the clinic to attain the best waiting time results.23
With regards to the consultation time, the study found that the average consultation time was 18.21 minutes and 41.8% of patients saw the doctor for 10–20 minutes. In comparison, a study in Malaysia found that the average consultation time in outpatients was 15 minutes.10 There are no guidelines on the best consultation length but studies have found that patients prefer to have more time with the doctor.16,18 Also patients are willing to wait longer if they get to see a familiar doctor.24,25 Continuity of care with the same doctor is important to patients especially when it comes to conditions dealing with uncertainty or routine checks for chronic diseases.24 Patients are usually willing to see any doctor for minor acute complaints.24 There are benefits to slower and longer consultation. Doctors who consult less than 7 minutes were found to be more likely to miss psychosocial issues in patients.26 Slower and longer consultation is associated with doctors being more likely to to identify psychosocial problems, explore presenting complaints more accurately, prescribe less and offer more preventative advice.26
Limitation
The use of manual recording due to incomplete recording by the electronic system might have introduced bias to data collection due to recollection error by the person who filled in the timing chit. This error was reduced by using the QMS system and synchronised clocks on the computer Profdoc HIS system. All staffs were briefed and reminded with regards to the audit and this may have introduced bias by staff trying to achieve targets. The data collection duration was short and a longer audit can be conducted to minimise the Hawthorne effect. Also, completion of the audit cycle, by implementing the recommended changes and re-auditing, is needed.
Conclusion
The clinic needs to improve its waiting time and to make the recommended changes to improve its services to patients. There is also a need to conduct further research to assess patient satisfaction on the clinic services including identification of patient's needs and to improve the quality of waiting by having distractions and facilities for patient comfort.
Acknowledgement
The authors would like to acknowledge all the doctors, nurses and staffs in the primary care clinic who participated in this audit.
Footnotes
Azraii AB, Kamaruddin KN, Ariffin F. An assessment of patient waiting and consultation time in a primary healthcare clinic. Malays Fam Physician. 2017;12(1);14–21.
References
- 1.Kintz J. This Book Is Not for Sale. Ebook; 2011. [Google Scholar]
- 2.Hassali MA, Alrasheedy AA, Ab Razak BA. et al. Assessment of general public satisfaction with public healthcare services in Kedah, Malaysia. [Accessed Jan 11;2017 ];AMJ. 2014 7(1):35–44. doi: 10.4066/AMJ.2014.1936. http//dx.doi.org/10.4066/AMJ.2014.1936 Available at: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Manaf NHA, Phang SN. Patient satisfaction as an indicator of service quality in Malaysian public hospitals. [Accessed Jan 11;2017 ];Asian J Qual. 2009 10(1):77–87. http://dx.doi.org/10.1108/15982680980000628 Available at: [Google Scholar]
- 4.McKinnon K, Crofts PD, Rhiannon E. et al. The outpatient experience: results of a patient feedback survey. Int J Health Care Qual Assur Inc Leadersh Health Serv. 2006;11(5):156–60. doi: 10.1108/09526869810230858. http://dx.doi.org/10.1108/09526869610230858 Available at: [DOI] [PubMed] [Google Scholar]
- 5.Kujala J, Lillrang P, Kronström V. Time-based management of patient processes. [Accessed Jan 11;2017 ];J Health Organ Manag. 2006 20(6):512–24. doi: 10.1108/14777260610702262. http://dx.doi.org/10.1108/14777260610702262 Available at: [DOI] [PubMed] [Google Scholar]
- 6.Barlow GL. Auditing hospital queuing. [Accessed Jan 11;2017 ];Managerial Auditing J. 2002 17(7):397–403. http://dx.doi.org/10.1108/02686900210437507 Available at: [Google Scholar]
- 7.Manaf NHA. Quality management in Malaysian public health care. [Accessed Jan 11;2017 ];Int J Health Care Qual Assur Inc Leadersh Health Serv. 2005 18(3):204–16. doi: 10.1108/09526860510594767. http://dx.doi.org/10.1108/09526860510594767 Available at: [DOI] [PubMed] [Google Scholar]
- 8.Bielen F, Demoulin N. Waiting time influence on the satisfaction-loyalty relationship in services. [Accessed Jan 11;2017 ];Manag Serv Qual: An Int J. 2007 17(2):174–93. http://dx.doi.org/10.1108/09604520710735182 Available at: [Google Scholar]
- 9.Lexshimi RG, Zaleha MI, Shamsul AS. et al. Patient satisfaction on waiting time and duration of consultation at orthopaedic clinic, Universiti Kebangsaan Malaysia Medical centre. Med & Health. 2009;4(1):35–46. [Google Scholar]
- 10.Pillay DI, Ghazali RJ, Manaf NH. Hospital waiting time: the forgotten premise of healthcare service delivery? [Accessed Jan 11;2017 ];Int J Health Care Qual Assur. 2011 24(7):506–22. doi: 10.1108/09526861111160553. http://dx.doi.org/10.1108/09526861111160553 Available at: [DOI] [PubMed] [Google Scholar]
- 11.Feddock CA, Hoellein AR, Griffith CH III. et al. Can physicians improve patient satisfaction with long waiting times? Eval & Health Prof. 2005;28(1):40–52. doi: 10.1177/0163278704273084. [DOI] [PubMed] [Google Scholar]
- 12.Oche MO, Adamu H. Determinants of patient waiting time in the general outpatient department of a tertiary health institution in North Western Nigeria. Annals Med Health Sci Res. 2013;3(4):588–92. doi: 10.4103/2141-9248.122123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Garber AM. Corporate treatment for ills of academic medicine. New England J Med. 2004;351(16):1601–3. doi: 10.1056/NEJMp048215. [DOI] [PubMed] [Google Scholar]
- 14.Cape J. Consultation length, patient-estimated consultation length, and satisfaction with the consultation. British J Gen Pract. 2002;52:1004–6. [PMC free article] [PubMed] [Google Scholar]
- 15.Britt H, Valenti L, Miller G. Time for care. Length of general practice consultations in Australia. Aust Fam Physician. 2002;31(9):876–80. [PubMed] [Google Scholar]
- 16.Deveugele M, Derese A, Brink-Muinen AVD. et al. Consultation length in general practice: cross sectional study in six European countries. BMJ. 2002;325:472. doi: 10.1136/bmj.325.7362.472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Freeman GK, Horder JP, Howie JGR. et al. Evolving general practice consultation in Britain: issues of length and context. BMJ. 2002;324:880–2. doi: 10.1136/bmj.324.7342.880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ogden J, Bavalia K, Bull M. et al. I want more time with my doctor: a quantitative study of time and the consultation. Fam Pract. 2004;21:479–83. doi: 10.1093/fampra/cmh502. [DOI] [PubMed] [Google Scholar]
- 19. [Accessed Jan 11;2017 ];Pekililing Ketua Pengarah Kesihatan Malaysia Bil 2/2008, Pemantauan Waktu Menunggu Dalam Tempoh 30 Minit Di Jabatan Pesakit Luar Hospital Dan Klinik Kesihatan. 2016 Mar; www.moh.gov.my/english.php/database_stores/store__view_page/10/158 [Cited. ]. Available at:
- 20. [Accessed Jan 11;2017 ];Piagam Pelanggan Kementerian Kesihatan Malaysia (KKM) 2015. 2016 Mar; www.moh.gov.my/index.php/pages/view/200 [Cited. ]. Available at:
- 21.Su S, Shih C-L. Managing a mixed registration-type appointment system in outpatient clinics. Inter J Med Inform. 2003;70:31–40. doi: 10.1016/s1386-5056(03)00008-x. [DOI] [PubMed] [Google Scholar]
- 22.Tang SH, Pah PS, Manohara A. et al. Use of simulation to solve outpatient clinic problems: a review of the literature. South African J Ind Eng. 2013;24(3):27–42. [Google Scholar]
- 23.Klassen KJ, Rohleder TR. Scheduling outpatient appointments in a dynamic environment. J Oper Manage. 1996;14:83–101. [Google Scholar]
- 24.Turner D, Tarrant C, Windridge K. et al. Do patients value continuity of care in general practice? An investigation using stated preference discrete choice experiments. J Health Serv Res Policy. 2007;12(3):132–7. doi: 10.1258/135581907781543021. [DOI] [PubMed] [Google Scholar]
- 25.Bower P, Roland M, Campbell J. et al. Setting standards based on patient's views on access and continuity: secondary analysis of data from the general practice assessment survey. BMJ. 2003;326(258):1–5. doi: 10.1136/bmj.326.7383.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wilson A, Childs S. The relationship between consultation length, process and outcomes in general practice: a systematic review. Br J Gen Pract. 2002;52:1012–20. [PMC free article] [PubMed] [Google Scholar]


