Abstract
Head injury is common and preventable. Assessment of the head injury patient includes airway, cervical spine protection, breathing, circulation, haemorrhage control and the Glasgow Coma Scale. Hypotension, hypoxia, hypocarbia and hypercarbia should be avoided by continuous monitoring of vital signs and hourly head chart to prevent secondary brain injury. This paper aims to assist primary healthcare providers to select the appropriate patient for transfer and imaging for further management of head injury.
Keywords: Head injury, Glasgow Coma Scale, referral, computed tomography, discharge advice
Introduction
Head injury is one of the commonest and probably the most preventable medical condition. Globally, road traffic accident is the commonest cause of head injury, besides accident at home, workplace and during a sports event. Head injury was the fifth (7.86%) commonest cause of hospitalisation in Malaysian public hospitals in 2014 with RTA being the commonest cause of injury-related hospitalisation. A high proportion of those with major trauma (86%) had injuries to the head and neck with an Abbreviated Injury Scale >3. In the World Health Organization's Global Status Report on Road Safety 2013, the road traffic fatality rate in Malaysia was higher than the global rate (25 versus 18 per 100,000 population). Many lives can be saved with good pre-hospital care and quick transportation to the hospital. Appropriate assessment, stabilisation and care of the trauma victim including referral and transportation are important to avoid secondary brain injury.
Definition
- To define head injury, criteria i and ii must be present with/without criteria iii:
- Mechanism—presence of external force*
- Physiological—alteration in physiology of the brain
- Anatomical—scalp and/or face and/ or skull and/or brain injury (internal and external)**
* The external forces may include any of the following events:
The head being struck by an object
The head striking an object
The brain undergoing an acceleration/ deceleration movement without direct external trauma to the head
A foreign body penetrating the brain
Forces generated from events such as blast or explosion, or other forces yet to be defined
** The anatomical or mechanical changes in the brain such as axonal injury, which may not be visualised in the computed tomography (CT) scan does not rule out such injury.
Classification of Head Injury
The severity of head injury can be classified according the presenting Glasgow Coma Scale (GCS) is the cumulative sum of the scale in each component score:
Mild head injury (MHI): GCS 13 to 15
Moderate head injury: GCS 9 to 12
Severe head injury: GCS 3 to 8
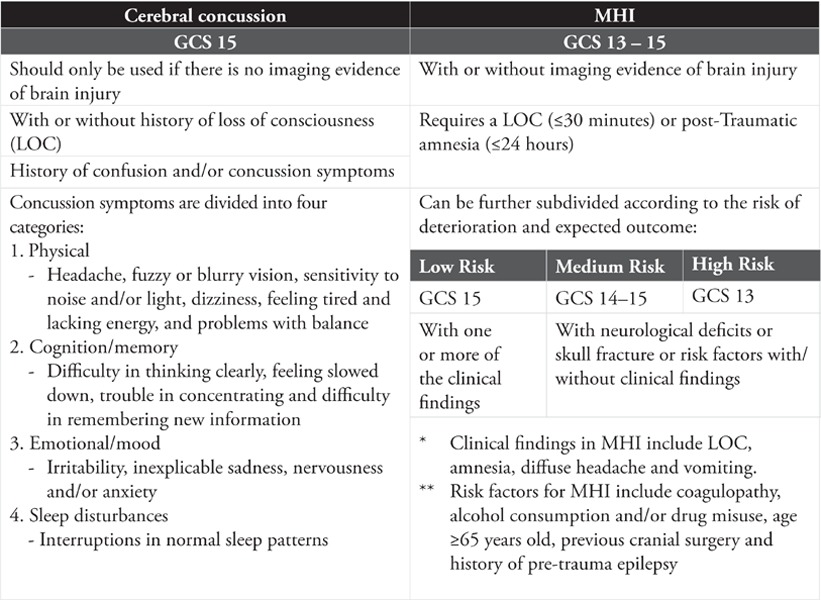
The MHI group can be subdivided into two types as shown in Table 1.
Table 1.
Types of MHI
Assessment
Assessment of the head injury patient should include airway, cervical spine protection, breathing, circulation, and haemorrhage control followed by the GCS.
The GCS score should be used in the assessment of all patients with head injury by trained healthcare providers. The patient's best eye, motor and verbal responses are assessed and categorised into mild, moderate and severe head injury. It is a reliable tool to monitor and detect deterioration in such patients. Alcohol intoxication, sedative medications, hypoxia and hypotension can influence the consciousness level. Therefore, any assessment of the GCS should be repeated after resuscitation from cardiopulmonary insult or recovery from intoxication and sedation.
The GCS is based on a 15-point scale used for estimating and categorising the severity of brain injury following a traumatic brain injury. The scale measures the best motor, verbal and eye opening response. Refer to Table 2.
Table 2.
GCS and score
| Component | Response | Score |
|---|---|---|
| Eye opening response | Spontaneous | 4 |
| To voice/sound | 3 | |
| To pressure/pain | 2 | |
| None | 1 | |
| Verbal response | Orientated | 5 |
| Confused | 4 | |
| Words | 3 | |
| Sounds | 2 | |
| None | 1 | |
| Motor response | Obeys commands | 6 |
| Localising | 5 | |
| Flexion withdrawal | 4 | |
| Abnormal flexion | 3 | |
| Extension | 2 | |
| None | 1 |
General Management
Oxygen supplementation should be given to prevent hypoxaemia [oxygen saturation (SpO2) < 90%].
An airway should be established in the following conditions:
Severe head injury (GCS < 8)
Inability to maintain an adequate airway
Hypoxaemia not corrected by supplemental oxygen
Manual in-line immobilisation should be performed during intubation.
All patients with head injury are presumed to have cervical spine injury until proven otherwise, thus a cervical collar should be applied.
Isotonic crystalloid is the preferred choice of intravenous fluid.
Referral Criteria
Referral of patients with head injury to the nearest hospital should be considered if they have any of the following factors:
GCS of 15 but symptomatic such as LOC, amnesia, headache, vomiting or restlessness
Age >65 years old
Treated with antiplatelets or anticoagulants
GCS < 15 and/or declining GCS score
Alcohol intoxication and substance misuse
Focal temporal blow
Social issues such as transport, communication problem or no supervision by a responsible adult
An indication for head CT
Transfer
Hypotension, hypoxia, hypocarbia and hypercarbia and inadvertent cervical injury should be avoided before and during transfer to prevent secondary brain injury. Continuous monitoring of vital signs should be conducted during transfer. Effective communication should be established between the transfer team and receiving hospital.
Triaging
Triaging should follow a four-step algorithm based on physiologic abnormalities, anatomic injuries, mechanism of injuries, comorbidities and age.
Specific Management
Primary survey includes:
Airway patency and cervical spine protection
Breathing (to detect any intrathoracic injury)
Circulation and haemorrhage control
Disability including GCS, pupil size and reaction to light
Exposure including log roll
Secondary survey (head to toe examinations) includes signs of base of skull fracture such as periorbital ecchymosis (“Raccoon eyes”), retroauricular ecchymosis (“Battle's sign”), cerebrospinal fluid rhinorrhoea or otorrhea or seventh and eighth cranial nerves deficits.
Head chart that includes serial GCS, blood pressure, pulse rate and pupil size should be done at least hourly including while awaiting CT or transfer to another ward/ hospital.
Monitor for signs of intracranial hypertension such as decreased pupillary response to light, hypertension with bradycardia, posturing or respiratory abnormalities.
Imaging
Timely imaging expedites appropriate surgical and medical interventions. The following algorithm shows the criteria and timeliness of head CT.
A normal skull x-ray does not exclude intracranial haemorrhage and may miss a fracture.
Discharge Advice
All patients or their care givers should be given verbal and written discharge advice in the language that they understand. This must be documented. They should be asked to repeat the advice to ensure that they understand the content upon discharge.
Algorithm.
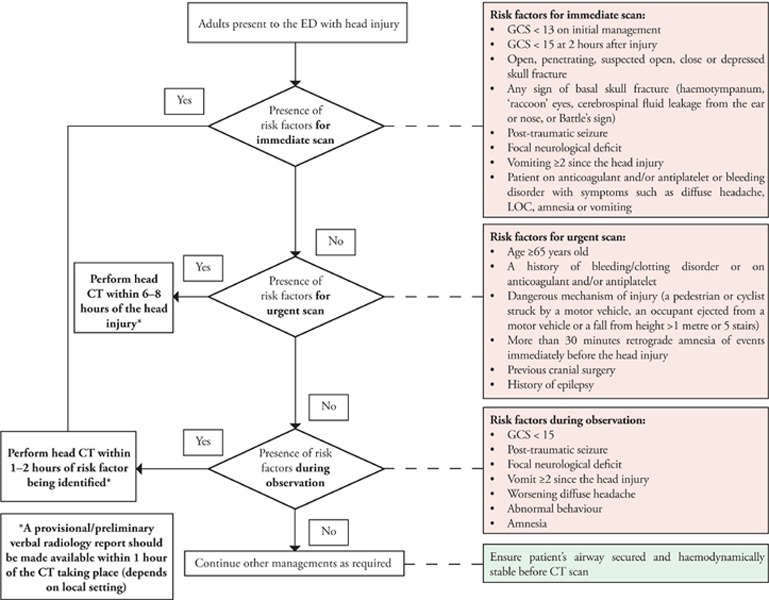
Selection of adults with head injury for head CT
Discharge advice for the patient
| DO | DON'T (until advised by your doctor) |
|---|---|
| ✓ Take paracetamol for headache | ✕ Take sleeping pills and anticoagulants/antiplatelets |
| ✓ Take your usual medications | ✕ Take alcohol |
| ✓ Mild exercise when you feel better | ✕ Play contact sport |
| ✓ Take rest or a few days off from work | ✕ Drive |
If any of the following alarming symptoms are present, the patient or the care giver should immediately contact the clinic or hospital for advice:
Fainting or sleepiness
Increasing confusion, inability to recognise people or place
Change in behaviour
Constant headache that is worsening
Vomiting
Inability to remember new events
Jerking or seizures, abnormal speech
Bleeding or fluids coming out of the ear
Inability to move any part of the body
Summary
In head injury, appropriate management of airway, breathing and circulation is important to prevent secondary brain injury. Knowledge and skill in the early management of head injury in adults and its proper implementation are vital to improve the quality of care. All healthcare providers have an important role to play in such management to ensure the best outcome for the patients.
Acknowledgement
Details of the evidence supporting the above statements can be found in Clinical Practice Guidelines on the Early Management of Head Injury in Adults 2015, available on the following website: Ministry of Health Malaysia: http://www.moh.gov.my and Academy of Medicine: http://www.acadmed.org.my. Corresponding organisation: CPG Secretariat, Health Technology Assessment Section, Medical Development Division, Ministry of Health Malaysia and contactable at htamalaysia@moh.gov.my.
Footnotes
Liew BS, Zainab K, Cecilia A, et al. Early management of head injury in adults in primary care. Malays Fam Physician. 2017;12(1);22–25.


