Abstract
The purpose of this study was to evaluate the efficacy of the Family Check-up (FCU), a parent-focused brief motivational intervention, in families where parents were concerned about one adolescent’s alcohol or marijuana use and the referred adolescent also had a sibling close in age. The primary goal of the FCU was to provide individualized feedback on specific parenting skills, including monitoring and supervision, limit setting, and alcohol-related communication. A total of 92 adolescents (37 female) between the ages of 12–19 years of age along with a sibling (48 female) between the ages of 11–21 years old, were randomized to the FCU or a psychoeducation (PE) comparison condition. Findings indicated that the FCU did not produce better effects on alcohol and other drug use outcomes than the PE condition, in either the adolescent or sibling. Brief interventions addressing parenting behaviors may not be sufficient to reduce alcohol use in adolescent drinkers not referred due to an alcohol-related incident. Future research might be conducted to explore whether brief parent interventions, such as those in the present study, could be useful as a preventive intervention for parents whose teens report low levels of substance use.
Keywords: Family Check-up, Psychoeducation, Underage drinking, Brief interventions, Adolescence
Graphical Abstract
1. Introduction
Multiple pathway, including developmentally normative experimentation (Masten, Faden, Zucker, & Spear, 2009), lead to alcohol use in adolescence but early and/or regular use have been associated with substance misuse in later adolescence (Chen, Storr, & Anthony, 2009; Lopez-Quintero et al., 2011). Over 26% of high school students report initiation of alcohol use and over 15% initiation of cannabis use by the 8th grade (Johnston, O’Malley, Miech, Bachman, & Schulenberg, 2016). By the time teens reach the 12th grade, 46.7% report having been drunk and 44.7% report cannabis use (Johnston et al., 2016). Youth who initiate alcohol and other drug (AOD) use early in adolescence are more likely to develop AOD diagnoses (SAMHSA, 2004). Furthermore, drinking to intoxication is highly associated with high-risk sexual behavior, high deviance, young adult arrests, and low educational attainment (McCambridge, McAlaney, & Rowe, 2011; Stueve & O’Donnell, 2005).
1.1. Parenting and AOD Use
Adolescent AOD use can be directly and indirectly influenced by parental modeling, punishment for experimentation, and advice about peer selection (Johnson & Johnson, 2001). Other parenting behavior associated with the onset and maintenance of adolescent AOD misuse includes poor parental monitoring, poor family communication, low warmth and support, high parental criticism/hostility, and parent-adolescent conflict (McMorris, Catalano, Kim, Toumbourou, & Hemphill, 2011; Ryan, Roman, & Okwany, 2015). A number of studies have also found that low levels of parental monitoring are related to early AOD use (Blustein et al., 2015; Chilcoat & Anthony, 1996; Ryan et al., 2015).
Positive parent-child affective quality and effective parenting processes, including parent and teen communication, appear to have important protective influences on youth AOD use (Chilcoat & Anthony, 1996). It is not just positive communication in general which deters adolescent AOD use but also the content, context, style, and timing of the communication about drinking that deters adolescent alcohol use (Jaccard & Turrisi, 1999). Several studies suggest that influencing how parents talk to their adolescents about their attitudes toward drinking should be included in interventions with parents, along with advice to parents about monitoring strategies (Zhang, Welte, & Wieczorek, 1997). Kosterman, Hawkins, Guo, Catalano, and Abbott (2000) found that strong parental norms against teenage drinking tended to reduce the risk of initiation in early adolescence and suggest the need to assess and improve not only parent management, but also relationship qualities, when addressing adolescent AOD use.
1.2. Siblings and Alcohol Use
Multiple studies have demonstrated that siblings show significant levels of similarity for alcohol use in adolescence (Kokkevi, Richardson, Florescu, Kuzman, & Stergar, 2007; Kothari, Sorenson, Bank, & Snyder, 2014; Poelen, Engels, Van Der Vorst, Scholte, & Vermulst, 2007). Siblings close in age show the most synchronous levels of substance use (Kothari et al., 2014; Scholte, Poelen, Willemsen, Boomsma, & Engels, 2008; Trim, Leuthe, & Chassin, 2006) and co-sibling drinking has been shown to be more predictive of alcohol use in adolescence than parental drinking (Kothari et al., 2014; Scholte et al., 2008; Whiteman, Jensen, & Maggs, 2013), and heavy drinking by a sibling has been shown to convey a risk of similar magnitude to peer heavy drinking (Kokkevi, Richardson, et al., 2007). Sibling collusion regarding deviant activities has also been shown to be related to AOD use (Stormshak, Comeau, & Shepard, 2004). Sibling drinking has emerged as a key predictor of heavy drinking in adolescence in several studies (Kokkevi, Arapaki, et al., 2007; Kokkevi, Richardson, et al., 2007; Kothari et al., 2014), suggesting it is an important target for family interventions.
1.3. The Family Check-Up
The Family Check-up (FCU; Dishion, Nelson, & Kavanagh, 2003) is based on Motivational Interviewing (MI) principles (Miller & Rollnick, 1991) with the goal of being designed to enhance parental recognition of adolescent risk behaviors and to provide support and guidance on how to reduce these behaviors. In one study (Dishion, Nelson, & Kavanagh, 2003), the FCU reduced the risk for future AOD use, among 6th grade students, three years later in the first year of high school; the prevention effect of the FCU was mediated by changes in parental monitoring. In another study (Spirito et al., 2011), parents of adolescents (ages 13–17) who were treated in an urban hospital emergency department for an alcohol-related event were randomized to receive either an individual adolescent motivational enhancement treatment (MET) or the individual MET plus the FCU. Both conditions resulted in a reduction in all drinking outcomes (i.e., frequency, quantity, and frequency of high volume drinking) at 3 months with a gradual increase in all drinking outcomes across the 6 and 12 month follow-up points. The FCU in combination with the MET was found to be superior to the individual MET in reducing the frequency of high-volume drinking at 3 months following the intervention, but not at 6 or 12 months follow-up.
1.4 Current Study
The purpose of the current study was to conduct a two-group randomized controlled trial to evaluate the efficacy of a sibling enhanced FCU, when focused on both an adolescent, whose parents were concerned about his/her alcohol or marijuana use, and a non-referred sibling close in age compared to Psychoeducation (PE). Individualized feedback was tailored to specific parenting skills that pertained to both the referred teen and sibling in the family. Based on our prior studies in which brief interventions had short term effects (Spirito et al, 2011), it was hypothesized that the FCU condition would result in both fewer drinking days and heavy drinking days than PE at 3 and 6 months, but not 12 months, for both the teen and sibling. In addition, based on the strong literature about the deterrent effects of parental monitoring on teen substance use, an a priori hypothesis stated that parental monitoring would result in fewer drinking days and heaving drinking days, for both teens and siblings, across all follow-up time points, regardless of treatment condition.
Material and Methods
1.1. Participants
Participants included 92 “target” adolescents who were enrolled because their parents were concerned about their alcohol or marijuana use (herein referred to as “teens”) and 92 siblings, one from each family (herein referred to as “siblings). Participants were recruited between January 2009 and May 2013 as part of a randomized controlled trial (see Table 1 for demographics). Eligibility criteria included: 1) between the ages of 12 and 19 years old; 2) living at home with a parent or legal guardian who is also willing to participate; 3) used alcohol or marijuana at least one time in the past 90 days; and 4) a sibling within 5 years of age of the target teen, living at home with the adolescent and participating parent(s), and between the ages of 11 and 21 years old. There were 7 adolescents, also included in these analyses, who reported during screening that they used alcohol or marijuana, but on the baseline assessment did not report any substance use.
Table 1.
Demographics, Means and Standard Deviations of Study Variables
| Variable | TEEN (N=92) | SIBLING (N=92) | PARENT (N= 92) | |||
|---|---|---|---|---|---|---|
| FCU (N=47) | PE (N=45) | FCU (N=47) | PE (N=45) | FCU (N=47) | PE (N=45) | |
| Age | ||||||
| Mean (SD) | 15.85 (1.30) | 15.93 (1.37) | 14.83 (2.35) | 15.29 (2.15) | 43.3 (7.27) | 42.7 (6.81) |
| Gender | ||||||
| Female (%) | 46.8 | 33.3 | 63.8 | 40 | 87.2 | 93.3 |
| Male (%) | 53.2 | 66.7 | 36.2 | 60 | 12.8 | 6.7 |
| Race | ||||||
| White (%) | 44.7 | 35.6 | 42.6 | 42.2 | 53.2 | 48.9 |
| Black (%) | 2.1 | 15.6 | 6.4 | 24.4 | 8.5 | 20 |
| Native American (%) | 2.1 | 0 | 0 | 2.2 | 2.1 | 2.2 |
| Asian (%) | 2.1 | 2.2 | 2.1 | 2.2 | 2.1 | 0 |
| >1 race (%) | 21.3 | 15.6 | 14.9 | 4.4 | 4.3 | 8.9 |
| Ethnicity | ||||||
| Hispanic (%) | 27.7 | 31.1 | 34 | 24.4 | 29.8 | 20 |
| Parental Income | ||||||
| 0 to $25,999 | 36.4 | 45.5 | ||||
| $26,000 to $49,999 | 27.3 | 22.7 | ||||
| $50,000 or more | 36.4 | 31.8 | ||||
| Parental Marital Status | ||||||
| Single/Never Married | 21.7 | 35.6 | ||||
| Living Together/Married | 52.2 | 35.6 | ||||
| Divorced/Widowed | 26.1 | 28.9 | ||||
| Parental Highest Level of Education | ||||||
| Some school prior to HS | 2.2 | 2.3 | ||||
| HS/GED | 47.8 | 36.4 | ||||
| 2YR/4YR college | 45.7 | 54.5 | ||||
| >4YR college | 4.3 | 6.9 | ||||
Note: At the time this study was conducted, ethnicity and race were not assessed as separate categories.
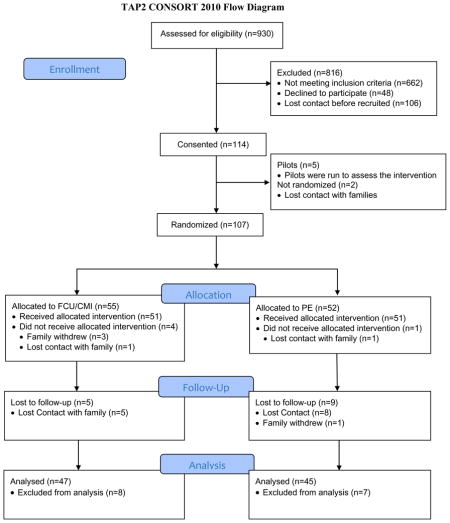
1.2.Procedure
Participants were recruited from the community, including local high schools, family court and truancy courts, as well as through advertisements or referrals from emergency departments or mental health agencies. After expressing interest in participating, potential participants were screened by research staff either in person or over the phone to determine eligibility. Because two related trials for adolescent AOD use were being conducted simultaneously, a large number of families (n = 930) received information. Of the 930 families, 29% met the eligibility criteria stated above and were therefore invited to participate in this trial. The consort diagram (Fig. 1) provides an outline of the procedures as well as participant enrollment/retention. All study procedures were approved by the university and hospital Institutional Review Boards. The proposed sample size (n = 150) was derived in order to have a sufficiently large sample, after follow-up attrition, to detect a medium effect size (Cohen, 1992). Recruitment challenges, specifically recruiting both teens and a sibling for the same study, precluded reaching the proposed target sample size.
Figure 1.
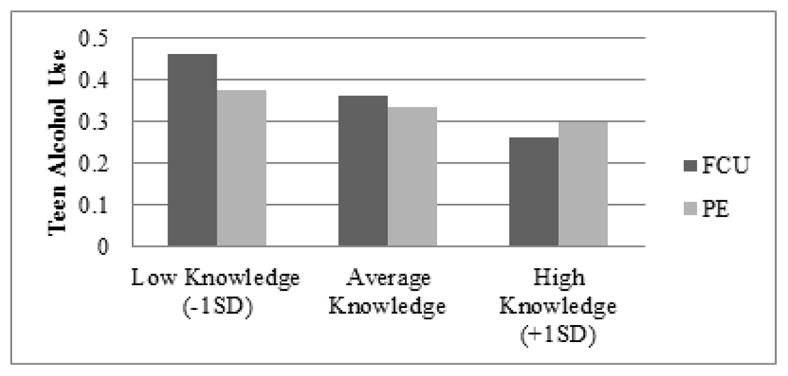
Parental Monitoring Knowledge by Teen Alcohol Use
Note: Teen alcohol use refers to average alcohol use across baseline and all 3 follow-up points using a log-transformed score.
The baseline assessment was approximately 45 minutes long. Adolescent and sibling assessments were each administered by a separate research assistant. Parent assessments were self-administered, unless the parent needed assistance. Upon completion of the assessments, a treatment provider randomized the family into the experimental or comparison condition (see below for further detail). Approximately two weeks following the baseline appointment, families returned to complete the intervention. Three follow-up visits were scheduled after the baseline appointment, at 3, 6, and 12 months. Research assistants conducting follow-up assessments were masked with respect to participant treatment condition assignment.
1.3. Intervention Conditions
Teens in both conditions received a computerized feedback program to satisfy referral sources and/or parents’ request for the target teen’s AOD use to be addressed individually. Depending on whether the adolescent identified a particular substance as more problematic than another, the teen received either the electronic-Check-Up to Go for High School Youth for alcohol use (e-CHUG; http://www.e-chug.com/hs/) or the electronic THC Online Knowledge Experience for marijuana use (e-TOKE; http://www.e-toke.com). Both e-CHUG and e-TOKE draw from MI (Miller & Rollnick, 2002), social norms feedback (Haines & Spear, 1996), and self-efficacy and peer modeling (Bandura, 1994) literature. e-CHUG and e-TOKE both begin with a series of questions on alcohol and marijuana use. The teen’s responses are used to create a personalized feedback report which included quantity, frequency, and pattern of use; amount of time spent under the influence of alcohol or marijuana compared to other activities; amount of income spent on alcohol or marijuana; normative comparisons; negative consequences of alcohol or marijuana use; and readiness and confidence to make a change.
In order to ensure that the two treatment conditions were balanced for alcohol use and externalizing problems, families were assigned to their condition using an urn randomization procedure (Stout, Wirtz, Carbonari, & Del Boca, 1994). Variables used in the urn included scores above or below the clinical cutoff on the externalizing subscale of the Child Behavior Checklist (CBCL; Achenbach & Rescorla, 2001; score greater than or equal to 64), and above or below the clinical cutoff on the Adolescent Drinking Index (ADI; Harrell & Wirtz, 1989; scores greater than or equal to 16). Different urns were generated for each combination of urn variables by the project coordinator and then placed in opaque envelopes and shuffled. The envelopes were opened at the completion of the baseline and the condition assignment was revealed.
2.3.1. Family Check-Up condition
Families in the FCU condition completed self-report measures plus a one-hour video-taped family assessment task (FAsTask) at baseline. FAsTask observational data were used to provide feedback during the FCU feedback session. FAsTask videos were coded and an individualized feedback report was presented to parents during the FCU session. Parents met with a counselor about two weeks following the baseline assessment. At that session, they received feedback from the FAsTask and self-report measures completed about parental stress, substance use, and beliefs about substance use.
The primary goal of the FCU feedback session, which lasted from an hour to an hour and one-half, was used to educate parents about risk for AOD use among adolescents, support appropriate parenting, and motivate parents to change ineffective parenting. The counselor reviewed important steps in successful parenting, using a MI style, but emphasizing the parent’s own responsibility in deciding on their parenting strategies. If asked, counselors also provided advice on how to change parenting behavior (Miller, 1985; Miller & Sovereign, 1989). The counselor tailored the feedback to balance parental strengths and challenges while supporting parental self-efficacy and motivation to change.
The FCU used in this study was adapted for parents of adolescents with siblings. The risk for AOD use problems during adolescence, and specifically, for adolescents with a sibling who has already engaged in use, was first discussed. Next, the counselor reviewed a printed summary of the assessment findings and provided guidance in the following areas: parenting practices, e.g., communication, monitoring, and supervision; alcohol and drug expectations for teens; family context, such as parent AOD use and stress levels; and peer and sibling influence on AOD use. For example, the 5 W’s of monitoring (Who, What, Where, When, Why) were discussed as well as how to communicate with teens about drugs and alcohol. The final topic focused on encouraging teen strengths, e.g. school involvement. Parent motivation for change, change options, and specific steps for making positive changes in parenting were the final areas reviewed as well as potential barriers to change.
2.3.2 Psychoeducation (PE) condition
Participants in the PE condition completed the baseline assessment in the first session. At the second visit, informational material on AOD use was reviewed by the counselor including prevalence of teen substance use facts about abuse and dependence; negative consequences of AOD use on health and school; and high-risk situations for substance misuse and abuse. The session took approximately 60 minutes and ended with handouts on the topics reviewed in the session.
2.4 Training and supervision of counselors
Four masters level and one doctoral level counselor delivered both the FCU and PE conditions. The counselors received an 8 hour training in MI followed by training specific to the FCU protocol. The FCU protocol was reviewed, practiced by the counselor, and then role-played with doctoral-level supervisors. PE training consisted of a reviewing the PE materials and role-playing the PE session. Emphasis was placed on not letting MI/FCU techniques “drift” into the PE session. Once trained, counselors received weekly supervision and audiotape reviews.
2.5. Adherence and competency
A total of 18 out of 43 (42%) English-speaking FCU tapes were rated on 38 protocol-based components using a “no/yes” scale. Two coders rated all 18 tapes and interrater agreement on whether protocol components were administered was 89%. On average, 84% of the expected components of the FCU were administered. For competence ratings, the Motivational Interviewing Treatment Integrity Code Version 3.0 (MITI 3.0; Moyers, Martin, Manuel, Miller, & Ernst, 2010), with scores ranging from 1 = “Poor” to 5 = “Excellent,” was used. All MI competence scores, on average, were above the expected score of 3, with the exception of “support self-efficacy” which was slightly lower (See Table 2). Interrater reliability was very high, with an intraclass correlation of .85 across items.
Table 2.
Rater scores for Motivational Interviewing competence and MITI scores
| Item | (N = 18) M (SD) |
|---|---|
| Project/MI Competence Ratings | |
| Balance of strengths and challenges | 3.83 (0.49) |
| Provide examples from the videotaped assessment | 4.11 (0.50) |
| Responded appropriately to confusion | 3.38 (0.48) |
| Express empathy | 3.75 (0.52) |
| Develop discrepancy | 3.17 (0.49) |
| Roll with resistance a | 3.50 (0.71) |
| Support self-efficacy | 2.89 (0.50) |
| Open-ended questions | 4.00 (0.54) |
| Reflective listening | 3.92 (0.67) |
| Affirm | 3.75 (0.69) |
| Summarize | 3.09 (0.48) |
| Elicit change talk | 3.44 (0.51) |
| MITI Scores | |
| Evocation | 4.08 (0.43) |
| Collaboration | 4.00 (0.59) |
| Autonomy | 3.97 (0.44) |
| Direction | 4.06 (0.57) |
| Empathy | 4.11 (0.50) |
Note: Competence ratings were answered on a 5-point scale: 1 “Poor”, 3 “Good”, 5 “Excellent”. MITI = Motivational Interviewing Treatment Integrity Code Version 3.0 items were answered on a 5-point scale from 1 “low” to 5 “high”.
14 cases were rated on this item; for the rest resistance was not identified
With respect to the PE condition, 22 of 45 sessions were coded by two independent raters on adherence to protocol components as well as to detect whether there was drift with respect to the use of MI techniques in the PE session. On average, 97% of the expected elements of the PE session were delivered by the counselors. With respect to the use of MI techniques in the PE session, scores of 3 or above on the MITI 3.0 are the expectation in MI. The items on evocation and collaboration on the MITI 3.0 never exceeded a rating of 2. A rating of 3 was found on 4 of 22 interviews (18%) for the autonomy/support item and 3/22 (14%) for the empathy item. On the direction item, which is consistent with a PE approach as well MI, 11 of 22 (50%) of the items were rated 3 or above.
2.6.Booster Mailings and Contact Information Updates
In both the FCU and PE conditions, parents were mailed 8 booster brochures every 3–4 weeks over the 6-month follow-up period. The topics of these brochures included parental monitoring, communication, limit setting, problem solving, and managing parent stress.
2.7. Measures
All measures were administered at baseline, 3-, 6-, and 12-month follow-up.
Alcohol Use was assessed using the Adolescent Drinking Questionnaire (Jessor, Donovan, & Costa, 1989). Teens and siblings were each asked how often they drank alcohol in the past three months at each assessment. Heavy drinking days was assessed with the following question, “over the past three months, how many times did you drink five or more drinks (of beer, wine, or liquor) when you were drinking?” Answer options for both questions were: 1) every day, 2) 4–6 days a week, 3) 2–3 days a week, 4) once a week, 5) less than once a week but more than once a month, 6) once a month, 7) less than once a month, or 8) I did not drink alcohol in the past three months. Responses were recoded into measures of the number of drinking days and heavy drinking days per month, which were subsequently log transformed to normalize the distributions.
Marijuana Use was assessed by asking teens and siblings to record the number of days they used marijuana (Marijuana Days) in the prior three months. A second frequency score indicating the average number of times marijuana was used per day (Marijuana Daily Frequency) was also assessed. Scores were log transformed to normalize the distribution.
Number of Drugs Used was assessed by asking teens and siblings to respond yes/no as to whether, in the prior 3 months, they used marijuana (pot, has, hash oil, etc.), cocaine (crack, rock, freebase, etc.), designer drugs (ecstasy, MDMA, GHB, etc.), and other drugs not prescribed or used more often than prescribed or used to get high, including: stimulants (amphetamines, diet pills, Ritalin), sedatives (Valium, Xanax, Quaaludes), hallucinogens (mushrooms, LSD, PCP), opiates (opium, heroin, morphine), inhalants (paint, glue), cough syrup or cough medicine (Triple C, Robitussin, DXM), or “other”. The number of drug categories endorsed (maximum = 10) were summed into a score representing the number of drugs used.
Sources of Parental Knowledge, also referred to as the Parental Monitoring Questionnaire (Stattin & Kerr, 2000), was used to assess parental monitoring knowledge and practices. There are four subscales: a parent monitoring knowledge subscale (α’s > .72), and three specific source subscales: parental solicitation (α’s > .72), parental control (α’s > .89), and teen disclosure (α’s > .22). The parent monitoring knowledge subscale was highly correlated with each specific source scale for teens and siblings (r’s between .48 and .84) and specific subscales were also highly interrelated for teens and siblings (r’s between .41 and .71). In order to reduce the number of analyses, we only used the parental monitoring knowledge subscale, for both teens and siblings.
2.7. Analytic Strategy
A series of t-tests and chi-square analyses were conducted as preliminary analyses to determine any differences between conditions at baseline on socio-demographics (i.e., age, sex, race, ethnicity) and study outcome variables (i.e., alcohol use or marijuana use). Attrition analyses, examining differences on baseline measures for those who did and did not complete the 12-month follow-up point, were conducted with Kruskal –Wallis tests. All tests were conducted separately for teens and siblings. We hypothesized that: (1) there would be a reduction in AOD use outcomes over time, (2) there would be a difference in that treatment effect based on treatment condition, and (3) there would be a difference in the treatment effect based on parent monitoring. In order to test these hypotheses, we conducted a hierarchical linear model that included time (in months) since baseline (linear slope), treatment condition, a condition*time interaction, parental monitoring, as well as two-way interactions for parental monitoring, treatment condition, and time. Exploratory three-way interactions were also conducted. We included three covariates, sibling age, teen age, and the siblings’ scores on the alcohol and marijuana outcome variables, when conducting for teen analyses (or teens’ score on the alcohol and marijuana outcome variables when conducting sibling analyses). Time and parental monitoring were included at level 1 as they were measured repeatedly. We included a random effect on time, as it was expected that there would be individual differences in AOD changes over time, but we did not include a random effect on monitoring, as this was not of primary interest here. Treatment condition and the covariates were included at level 2.
3. Results
There were no differences between the two groups at baseline on age, sex, race, ethnicity, alcohol use, or marijuana use. In the PE condition, 9 out of 52 participants were lost to follow-up (17%): 8 were unable to be contacted and 1 family withdrew from the study. In the FCU condition, 5 out of 55 participants were unable to be contacted and were lost to follow-up (9%). Attrition analyses examining differences between baseline and 12-month follow-up on age, sex, race, ethnicity, alcohol and marijuana use were all non-significant for both teens and siblings. Because there were no differences between conditions in AOD use at baseline or follow-up, Table 3 presents percentage of alcohol and marijuana use, as well as the means and standards deviations on the parental monitoring subscale of the PMQ for the entire sample. Outcome analyses for teen and sibling alcohol, marijuana, and other drug use are presented below.
Table 3.
Teen and Sibling Descriptive Statistics for Study Variables at Baseline and 3, 6, and 12 month Follow-up
| Assessment: | Baseline | 3 month follow-up | 6 month follow-up | 1 year follow-up | ||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| Alcohol Use Frequency | ||||||||
| Teen | N | (%) | N | (%) | N | (%) | N | (%) |
| Every Day | 0 | (0%) | 0 | (0.0%) | 1 | (1.1%) | 0 | (0.0%) |
| 4–6 days/week | 2 | (1.8%) | 1 | (1.1%) | 1 | (1.1%) | 0 | (0.0%) |
| 2–3 days/week | 8 | (7.3%) | 6 | (6.7%) | 9 | (10.1%) | 10 | (11.8%) |
| Once per week | 12 | (11.0%) | 11 | (12.4%) | 9 | (10.1%) | 4 | (4.7%) |
| Less than once per week | 21 | (19.3%) | 12 | (13.5%) | 19 | (21.3%) | 19 | (22.4%) |
| Once per month | 13 | (11.9%) | 11 | (12.4%) | 4 | (4.5%) | 13 | (15.3%) |
| Less than Once per month | 30 | (27.5%) | 22 | (24.7%) | 17 | (19.1%) | 10 | (11.8%) |
| none | 23 | (21.1%) | 26 | (29.2%) | 29 | (32.6%) | 29 | (34.1%) |
| Sibling | ||||||||
| Every Day | 0 | (0.0%) | 0 | (0.0%) | 0 | (0.0%) | 0 | (0.0%) |
| 4–6 days/week | 1 | (1.0%) | 0 | (0.0%) | 1 | (1.2%) | 0 | (0.0%) |
| 2–3 days/week | 3 | (3.0%) | 5 | (6.1%) | 7 | (8.6%) | 7 | (9.2%) |
| Once per week | 9 | (9.1%) | 4 | (4.9%) | 7 | (8.6%) | 4 | (5.3%) |
| Less than once per week | 14 | (14.1%) | 10 | (12.2%) | 9 | (11.1%) | 10 | (13.2%) |
| Once per month | 8 | (8.1%) | 5 | (6.1%) | 4 | (4.9%) | 5 | (6.6%) |
| Less than Once per month | 12 | (12.1%) | 7 | (8.5%) | 13 | (16.0%) | 7 | (9.2%) |
| none | 52 | (52.5%) | 51 | (62.2%) | 40 | (49.4%) | 43 | (56.6%) |
| Marijuana Use (yes) | ||||||||
| Teen | 69 | (67.7%) | 56 | (62.9%) | 59 | (66.3%) | 51 | (60.0%) |
| Sibling | 39 | (42.4%) | 32 | (39.0%) | 32 | (39.5%) | 31 | (40.8%) |
| Parental Monitoring | M | (SD) | M | (SD) | M | (SD) | M | (SD) |
| Teen | 3.37 | (.83) | 3.60 | (.81) | 3.26 | (.90) | 3.15 | (1.00) |
| Sibling | 3.76 | (1.02) | 3.86 | (0.91) | 3.71 | (.91) | 3.54 | (1.05) |
Note. N’s vary with missing data. All substance use was assessed ‘over the past 3 months’. Parental monitoring was assessed using the Parent Monitoring Knowledge subscale of the Parental Monitoring Questionnaire
3.1. Teen Alcohol
Parameter estimates for frequency of teen alcohol use are presented in Table 4, column 2. There was no effect of treatment condition on the number of drinks teens reported (per month). Alcohol use did not change over time, and there was no treatment condition by time interaction. There was no main effect of parental monitoring or parental monitoring by time interaction. There was a significant interaction of parental monitoring by treatment condition. Analysis of simple slopes suggested that the effect of monitoring was more pronounced for the FCU group than the PE group (see Figure 1). The three-way interaction of treatment condition, time, and parental monitoring was not significant. Older teens used alcohol more frequently.
Table 4.
Parameter Estimates and Model Fitting Results for Frequency of Teen and Sibling Alcohol Use
| Teen Alcohol | Sibling Alcohol | Teen Heavy Alcohol | Sibling Heavy Alcohol | |
|---|---|---|---|---|
| Fixed Effects | ||||
| Intercept | .35* (.04) | .20* (.03) | .26* (.05) | .12* (.03) |
| Treatment Condition | .03 (.06) | .06 (.05) | −.01 (.06) | .06 (.05) |
| Time | −.003 (.004) | .004 (.004) | −.002 (.004) | .003 (.004) |
| Time * Condition | <.0001 (.006) | −.005 (.005) | −.0002 (.01) | .003 (.005) |
| Parental Monitoring | −.02 (.04) | −.003 (.03) | −.05 (.04) | −.03 (.03) |
| Time * Monitoring | −.003 (.005) | −.008* (.004) | −.01 (.005) | −.008* (.003) |
| Condition * Monitoring | −.13* (.05) | −.05* (.04) | −.08 (.05) | −.07 (.04) |
| Time * Condition * Monitoring | .01† (.007) | .01* (.005) | .01* (.006) | .01* (.005) |
| Covariates | ||||
| Other Sib scorea | .17* (.06) | .16* (.05) | .08 (.07) | .07† (.04) |
| Teen Age | .04* (.02) | −.01 (.02) | .03 (.02) | −.01 (.02) |
| Sibling Age | −.004 (.01) | .07* (.01) | .01 (.01) | .05* (.02) |
| Random effects | ||||
| Intercept | .04* (.01) | .03* (.01) | .06* (.01) | .02* (.008) |
| Assessment | <.0001 (<.0001) | <.0001 (<.0001) | <.0001 (<.0001) | <.0001 (<.0001) |
| Residual | .05* (.005) | .04* (.004) | .05* (.005) | .04* (.004) |
| Model fit | ||||
| −2 Res Log Likelihood | 143.1 | 58.3 | 157.7 | 27.1 |
| AIC | 149.1 | 64.3 | 163.7 | 33.1 |
for Teen Alcohol, other sib score = sibling alcohol score; for Sibling Alcohol, other sib score = Teen Alcohol; for Teen Marijuana, other sib score = sibling marijuana score; for Sibling Marijuana, other sib score = Teen Marijuana.
p < .05;
p < .10.
Monitoring = Parental Monitoring subscale of the Parental Monitoring Questionnaire
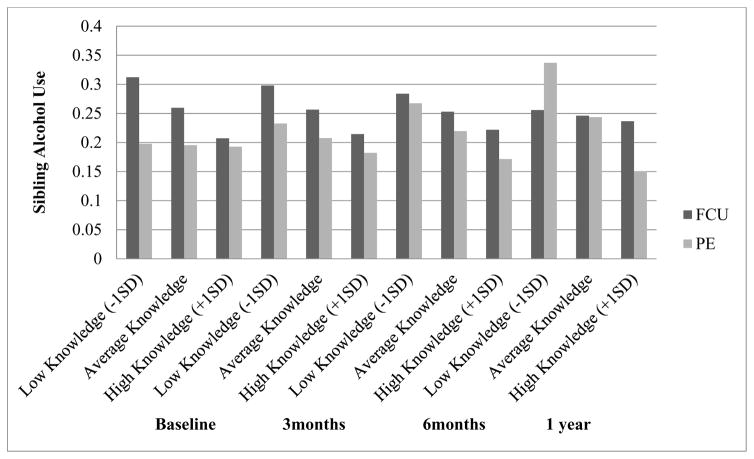
3.2 Sibling Alcohol
Parameter estimates for frequency of sibling alcohol use are presented in Table 4, column 3. There was no effect of treatment condition on the number of drinks siblings reported having per month. Siblings’ alcohol use did not change over time, and there was no treatment condition by time interaction. There was no main effect of parental monitoring, or parental monitoring by treatment condition interaction. There was a significant interaction of parental monitoring and time; however, this two-way interaction was qualified by a significant three-way interaction, parental monitoring, time, and treatment. Analysis of simple slopes suggested that monitoring only had a significant effect among siblings of PE participants at the 1-year follow-up. The effect of monitoring became more pronounced over time for the PE group, but less pronounced over time for the FCU group (See Figure 2). Teen alcohol use was associated with sibling alcohol use and alcohol use increased with the age of the sibling.
Figure 2.
Parental Monitoring Knowledge by Sibling Alcohol Use
Note: Sibling alcohol use refers to average alcohol use across baseline and all 3 follow-up points using a log-transformed score.
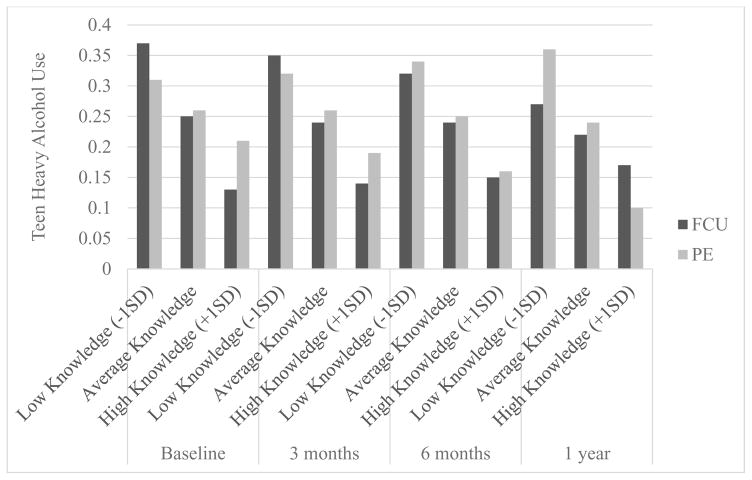
3.3. Teen Heavy Drinking
Parameter estimates for frequency of teen heavy drinking are presented in Table 4, column 4. There was no effect of treatment condition on the number of heavy drinking days teens reported (per month). Heavy alcohol use did not change over time, and there was no treatment condition by time interaction. There was no main effect of parental monitoring or parental monitoring by time or by treatment condition interaction. There was, however, a significant interaction of parental monitoring by treatment condition by time. Analysis of simple slopes suggested that the effect of monitoring became more pronounced over time for the PE group, but less pronounced over time for the FCU group (see Figure 3).
Figure 3.
Parental Monitoring Knowledge by Teen Heavy Alcohol Use
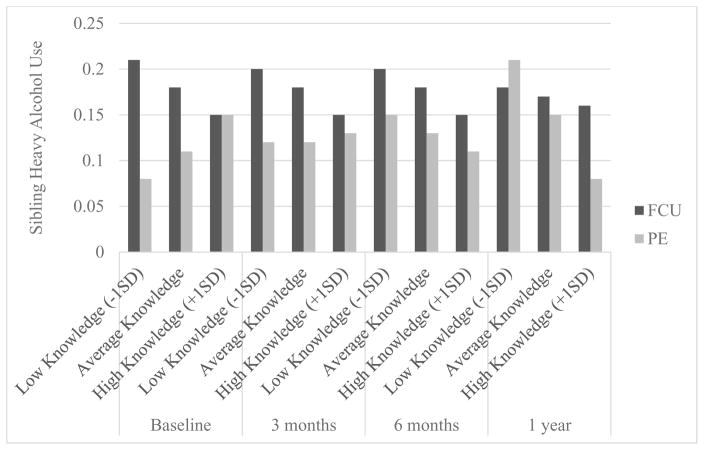
3.4 Sibling Heavy Drinking
Parameter estimates for frequency of sibling heavy drinking are presented in Table 4, column 5. There was no effect of treatment condition on the number of heavy drinking days siblings reported per month. Sibling heavy drinking did not change over time, and there was no treatment condition by time interaction. There was no main effect of parental monitoring, or parental monitoring by treatment condition interaction. There was a significant interaction of parental monitoring and time; however, this two-way interaction was qualified by a significant three-way interaction, parental monitoring, time, and treatment. Analysis of simple slopes suggested that the effect of monitoring was opposite of expected directions in the PE group initially, but began being effective and became more pronounced over time in the PE group, whereas the effect of monitoring was more constant, and perhaps became less pronounced over time for the FCU group (see Figure 4).
Figure 4.
Parental Monitoring Knowledge by Sibling Heavy Alcohol Use
3.5. Teen Marijuana and Other Drug Use
Parameter estimates for teen marijuana use are presented in Table 5, column 2. There was no effect of treatment condition on the number of days (per month) teens reported using marijuana. Marijuana use did not change over time, and there was no treatment condition by time interaction. There was no main effect of parental monitoring, or any two- and three-way interactions of parental monitoring with treatment condition and time. None of the covariates significantly predicted teens’ marijuana use. Sibling alcohol use was associated with teen marijuana use.
Table 5.
Parameter Estimates and Model Fitting Results for Frequency of Teen and Sibling Marijuana and Other Drug Use
| Teen Marijuana Days | Sibling Marijuana Days | Teen Marijuana Daily Frequency | Sibling Marijuana Daily Frequency | Teen Number of Drugs Used | Sibling Number of Drugs Used | |
|---|---|---|---|---|---|---|
| Fixed Effects | ||||||
| Intercept | .81* (.10) | .47* (.08) | .43* (.10) | .36* (.07) | .77* (.10) | .48* (.06) |
| Treatment Condition | .01 (.14) | −.02 (.11) | .02 (.13) | −.06 (.09) | .05 (.14) | −.06 (.09) |
| Time | .005 (.01) | .0003 (.007) | .001 (.01) | −.01 (.01) | −.01 (.01) | −.01 (.01) |
| Time * Condition | −.002 (.01) | .003 (.009) | −.001 (.01) | .01 (.01) | −.01 (.01) | .01 (.01) |
| Parental Monitoring | −.11 (.07) | −.18* (.06) | .01 (.07) | −.17* (.06) | −.11 (.08) | −.20* (.05) |
| Time * Monitoring | −.01 (.01) | −.002 (.006) | −.01 (.01) | −.01 (.01) | .002 (.01) | −.01 (.01) |
| Condition * Monitoring | .02 (.11) | .10 (.08) | −.13 (.10) | .15† (.08) | .04 (.11) | .07 (.07) |
| Time * Condition * Monitoring | .02 (.01) | −.002 (.008) | .01 (.01) | −.0004 (.009) | .004 (.01) | .01 (.01) |
| Covariates | ||||||
| Other Sib scorea | .13† (.07) | .09* (.04) | .36* (.08) | .24* (.06) | .04 (.07) | .02 (.04) |
| Teen Age | .05 (.05) | −.02 (.04) | .03 (.04) | −.04 (.03) | .05 (.05) | .001 (.03) |
| Sibling Age | .05 (.03) | .11* (.03) | .02 (.03) | .08* (.02) | .05 (.03) | .07* (.02) |
| Random effects | ||||||
| Intercept | .34* (.07) | .23* (.04) | .19* (.05) | .09* (.03) | .35* (.07) | .11* (.03) |
| Assessment | .001* (.001) | .0002 (.0003) | <.0001 (<.0001) | .0001 (.0003) | .002* (.001) | .001* (.0004) |
| Residual | .15* (.02) | .09* (.01) | .07* (.01) | .05* (.01) | .15* (.02) | .10* (.01) |
| Model fit | ||||||
| −2 Res Log Likelihood | 582.7 | 413.3 | 225.7 | 150.9 | 585.6 | 422.9 |
| AIC | 590.7 | 421.3 | 231.7 | 158.9 | 593.6 | 430.9 |
Teen Marijuana, other sib score = sibling marijuana score; for Sibling Marijuana, other sib score = Teen Marijuana.
p < .05;
p < .10.
Monitoring = Parental Monitoring subscale of the Parental Monitoring Questionnaire
Identical findings were evident when the number of times marijuana was used per day (Table 5, column 4) and when number of drugs used (Table 5, column 6) was substituted for days of marijuana use per month
3.6. Sibling Marijuana and Other Drug Use
Parameter estimates for sibling marijuana use are presented in Table 5, column 3. There was no effect of treatment condition on the number of days siblings reported using marijuana across the month. Sibling marijuana use did not change over time, and there was no treatment condition by time interaction. Lower parental monitoring was associated with more sibling marijuana use. There were no interactions between parental monitoring, time, and treatment condition. Teen marijuana use was associated with sibling marijuana use. Marijuana use increased with the age of the sibling.
With the exception of the finding that lower parental monitoring was associated with more sibling marijuana use, identical findings were evident when the number of times marijuana was used per day was substituted for days per month (Table 5, column 5). Identical findings were evident when the number of drugs used was substituted for days per month (Table 5, column 7).
4. Discussion
The present study examined if a brief MET geared towards parents concerned about an adolescent’s alcohol or marijuana use would have a greater effect on AOD use of the teen, as well as a sibling close in age, compared to a PE condition. The clinical premise driving this study was that intervening with parents regarding one teen would have associated positive effects on a sibling close in age to the teen. This primary hypothesis was not supported. The FCU did not produce better results than a PE comparison condition. Our PE program was comprehensive and engaging and a number of parents commented on how valuable the PE intervention was to them. In addition, both conditions were delivered by the same counselors who received weekly supervision regarding adherence to each condition. However, more disappointingly, neither the FCU nor PE program was found to significantly reduce alcohol or marijuana use in the identified teens. The effects on sibling AOD use were also limited in both conditions.
Previous studies conducted by our group of these brief METs, whether with the teen alone (Spirito et al, 2004) or the teen and a parent (Spirito et al, 2011) have found significant reductions in use, especially the first 3 months, followed by a gradual rise in use. A similar pattern was found in this sample but the effects were not statistically significant. Our previous study (Spirito et al, 2011) also found a significantly greater reduction in heavy drinking days at 3 months for the FCU condition relative to an individual MI, but that was not the case in this study. The limited findings reported here are similar to findings of other studies. A recent review of brief interventions conducted in schools, for example, found that while they outperformed assessment only control conditions, they did not produce significant effects when compared to information-only interventions (Carney, Myers, Louw, & Okwundu, 2016).
The limited intervention findings in this study may have been due to the fact that adolescents in the current study were recruited from numerous sources and were not required to have an alcohol-related negative event to be eligible for the study, e.g., ED admission due to intoxication. One recruitment strategy was for study staff to go into local high schools and conduct presentations about myths and facts of AOD use. After the presentations, staff presented the study to adolescents and those who were interested were individually screened. Although we found this to be the best method for recruiting, only a limited number of parents, when contacted about the study, were interested in participating in the study. In such recruitment circumstances,, a brief MET focused on motivating parents to change their behaviors may not have been sufficient to affect AOD use in the adolescent. In addition, the brief computerized individual adolescent interventions may have had limited effects with this population; all our previous MET interventions were face-to-face. Also, since this study recruited adolescents who reported alcohol and/or marijuana use in the prior 3 months, at baseline, some youth did not use alcohol and some did not use marijuana, which made it more difficult to detect a reduction in use of either substance.
The somewhat unique recruitment challenges of the study might account, in part, for the limited findings, especially with siblings. Parents interested in the study needed to have both a teen and sibling to participate in the study. Anecdotally, a number of parents who initially expressed interest said they could get one, but not the other teen, to participate, so they never enrolled in the study. Consequently, a very heterogeneous group of siblings, some older than the referred teen and some reporting significant AOD use, comprised our sample. If the entire group of siblings had been younger than the identified teen and/or experimenting or not reporting any use, interpretation of the findings would have been more straightforward. Almost half of the siblings reported alcohol use at least monthly. In families where more than one sibling is using substances, brief interventions may not be sufficient.
Another possibility for the limited intervention findings was due to the low rates of substance use, particularly alcohol, at baseline, as well as follow-up in the sample. However, the overall rate of teen alcohol use decreased over 6 months of follow-up and then was stable in both conditions at the 12 month follow-up. Sibling alcohol use remained fairly stable. Marijuana use also remained fairly stable for the teens and their siblings. These findings suggest there may have been a preventative effect of both interventions on teen use, particularly alcohol use. That is, whereas national survey data typically indicates that adolescent alcohol and marijuana use increase among adolescents as they age (Miech, Johnston, O’Malley, Bachman, & Schulenberg, 2016), the intervention conditions may have dampened the uptake of or increase in substance use over the year follow-up period.
Study results did confirm some well-established findings from the literature. Specifically, teen alcohol and marijuana use were associated with sibling alcohol and marijuana use, respectively (Kothari et al., 2014; Whiteman et al., 2013). Age was related to both alcohol and marijuana use; older teens and older siblings reported more use than younger teens and siblings (Johnston et al., 2016; Kothari et al., 2014). Age was related to other drug use for siblings, but not teens. Parental monitoring was associated with lower sibling marijuana use and number of drugs used (Blustein et al., 2015), but not teen marijuana use or number of drugs used.
Parental monitoring findings were contradictory. On the one hand, greater parental monitoring knowledge was associated with less teen alcohol use in the FCU, but not the PE, condition. However, there was no difference in alcohol use between the FCU and PE conditions at any given point on the parental monitoring knowledge spectrum, i.e., low, medium, or high parental monitoring knowledge. That is, treatment condition moderated the effect on parental monitoring knowledge, but parental monitoring knowledge did not lead to lower teen alcohol use in FCU compared to PE. This may have been related to the unexpected finding that parental monitoring of teen heavy alcohol use was more pronounced in the PE condition than the FCU condition over time.
On the other hand, parental monitoring knowledge was related to lower alcohol use among siblings of PE, but not FCU, participants, at the 1-year follow-up. As noted above, this finding might have been related to the fact that parental monitoring of sibling heavy alcohol use was more pronounced in the PE condition than the FCU condition over time. Also, the heterogeneous presentations of the siblings in the study, i.e. some demonstrating significant AOD use and others not reporting any use at all, may have influenced this finding. For some parents, preventing AOD use onset was the main goal for the sibling, while for others intervening on current AOD use was indicated. For the siblings who were not using at baseline, high levels of parental monitoring knowledge may have reduced use at the 12 month follow-up period. Why this was the case for the siblings in the PE, but not the FCU, condition, is unclear.
There are several limitations in this study which should be taken into consideration when interpreting its findings. First, these results are based on data from a sample of teens and siblings with a wide range of AOD use. Therefore, these results may not be generalizable to specific subpopulations, such as those with heavy AOD use. Second, all of the data in this study were obtained through self-report, which may have had an effect on the validity of the results. Asking adolescents to recall and report their AOD use in the prior 90 days is likely less than completely accurate, due to problems with memory, recall, fear of negative reaction from the assessor, and worries about confidentiality (Lewis-Esquerre et al., 2005; Siegel, Aten, & Roghmann, 1998; Waldron, Slesnick, Brody, Turner, & Peterson, 2001). Third, the difficulty in recruiting families with a teen who had a substance use event, as well as a sibling similar in age to the recruited teen, may have contributed to lower than expected baseline substance use. This factor may have reduced the size of any treatment effect and/or the ability to detect a small effect size between conditions or over time.
5. Conclusion
A brief parent motivational intervention, the FCU, was not effective in reducing AOD use, compared to a PE condition, in a heterogeneous sample of adolescents whose parents were concerned about their teen’s alcohol or marijuana use. The effects on sibling AOD use was also very limited in both conditions. The findings raise the possibility that a more intensive intervention may be necessary to affect change in AOD use with adolescents not referred for counseling due to an alcohol-related problem or event. Future research might be conducted to explore whether brief parent interventions, such as those in the present study, could be useful as a preventive intervention for those parents with teens who have low baseline substance use.
Highlights.
A brief parent motivational intervention was compared to psychoeducation
A heterogeneous sample of adolescents reporting alcohol misuse was examined
An identified, referred teen and a sibling close in age were studied
Neither the brief motivational intervention or psychoeducation condition were effective in reducing alcohol and other drug use
Acknowledgments
Sources of Funding: National Institute on Alcohol Abuse and Alcoholism (AA-017659)
ClinicalTrials. Gov Identifier: NCT00925340
Abbreviations
- AOD
alcohol and other drugs
- MI
Motivational Interviewing
- FCU
Family Check-Up
- MET
Motivational Enhancement Treatment
- PE
Psychoeducation
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, and Families; 2001. [Google Scholar]
- Bandura A. Regulative function of perceived self-efficacy. In: Rumsey MG, Walker CB, Harris JH, editors. Personnel selection and classification. Hillsdale, NJ, England: Lawrence Erlbaum Associates, Inc; 1994. pp. 261–271. [Google Scholar]
- Blustein EC, Munn-Chernoff MA, Grant JD, Sartor CE, Waldron M, Bucholz KK, … Heath AC. The Association of Low Parental Monitoring With Early Substance Use in European American and African American Adolescent Girls. J Stud Alcohol Drugs. 2015;76(6):852–861. doi: 10.15288/jsad.2015.76.852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carney T, Myers B, Louw J, Okwundu C. Brief school-based interventions and behavioroural outcomes for substance-using adolescents. Cochrane Database of Systematic Reviews. 2016:1. doi: 10.1002/14651858.CD008969.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen CY, Storr CL, Anthony JC. Early-onset drug use and risk for drug dependence problems. Addict Behav. 2009;34(3):319–322. doi: 10.1016/j.addbeh.2008.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chilcoat HD, Anthony JC. Impact of parent monitoring on initiation of drug use through late childhood. J Am Acad Child Adolesc Psychiatry. 1996;35(1):91–100. doi: 10.1097/00004583-199601000-00017. [DOI] [PubMed] [Google Scholar]
- Cohen J. A power primer. Psychol Bull. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Dishion TJ, Nelson SE, Kavanagh K. The family check-up with high-risk young adolescents: Preventing early-onset substance use by parent monitoring. Behav Ther. 2003;34(4):553–571. [Google Scholar]
- Haines M, Spear SF. Changing the perception of the norm: A strategy to decrease binge drinking among college students. J Am Coll Health. 1996;45(3):134–140. doi: 10.1080/07448481.1996.9936873. [DOI] [PubMed] [Google Scholar]
- Harrell AV, Wirtz PW. Screening for adolescent problem drinking: Validation of a multidimensional instrument for case identification. Psychol Assessment. 1989;1(1):61–63. [Google Scholar]
- Jaccard J, Turrisi R. Parent-based intervention strategies to reduce adolescent alcohol-impaired driving. J Stud Alcohol Drugs. 1999;13:84–93. doi: 10.15288/jsas.1999.s13.84. [DOI] [PubMed] [Google Scholar]
- Jessor R, Donovan JE, Costa FM. Health Behavior Questionnaire. Boulder, CO: University of Colorado; 1989. [Google Scholar]
- Johnson P, Johnson H. Reaffirming the power of parental influence on adolescent smoking and drinking decisions. Adolesc Fam Health. 2001;2(1):37–43. [Google Scholar]
- Johnston LD, O’Malley PM, Miech RA, Bachman JG, Schulenberg JE. Monitoring the Future national survey results on drug use, 1975–2015: Overview, key findings on adolescent drug use. Ann Arbor: Institute for Social Research, The University of Michigan; 2016. [Google Scholar]
- Kokkevi AE, Arapaki AA, Richardson C, Florescu S, Kuzman M, Stergar E. Further investigation of psychological and environmental correlates of substance use in adolescence in six European countries. Drug Alcohol Depend. 2007;88(2–3):308–312. doi: 10.1016/j.drugalcdep.2006.10.004. [DOI] [PubMed] [Google Scholar]
- Kokkevi AE, Richardson C, Florescu S, Kuzman M, Stergar E. Psychosocial correlates of substance use in adolescence: a cross-national study in six European countries. Drug Alcohol Depend. 2007;86(1):67–74. doi: 10.1016/j.drugalcdep.2006.05.018. [DOI] [PubMed] [Google Scholar]
- Kosterman R, Hawkins JD, Guo J, Catalano RF, Abbott RD. The dynamics of alcohol and marijuana initiation: Patterns and predictors of first use in adolescence. Am J Public Health. 2000;90(3):360–366. doi: 10.2105/ajph.90.3.360. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10705852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kothari BH, Sorenson P, Bank L, Snyder J. Alcohol and Substance Use in Adolescence and Young Adulthood: The Role of Siblings. J Fam Soc Work. 2014;17(4):324–343. doi: 10.1080/10522158.2014.924457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis-Esquerre JM, Colby SM, O’Leary Tevyaw T, Eaton CA, Kahler CW, Monti PM. Validation of the timeline follow-back in the assessment of adolescent smoking. Drug Alcohol Depend. 2005;79:33–43. doi: 10.1016/j.drugalcdep.2004.12.007. [DOI] [PubMed] [Google Scholar]
- Lopez-Quintero C, Perez de los Cobos J, Hasin DS, Okuda M, Wang S, Grant BF, Blanco C. Probability and predictors of transition from first use to dependence on nicotine, alcohol, cannabis, and cocaine: results of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Drug Alcohol Depend. 2011;115(1–2):120–130. doi: 10.1016/j.drugalcdep.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masten AS, Faden VB, Zucker RA, Spear LP. A Developmental Perspective on Underage Alcohol Use. Alcohol Research & Health. 2009;32(1):3–15. [PMC free article] [PubMed] [Google Scholar]
- McCambridge J, McAlaney J, Rowe R. Adult consequences of late adolescent alcohol consumption: a systematic review of cohort studies. PLoS Med. 2011;8(2):e1000413. doi: 10.1371/journal.pmed.1000413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMorris BJ, Catalano RF, Kim MJ, Toumbourou JW, Hemphill SA. Influence of family factors and supervised alcohol use on adolescent alcohol use and harms: similarities between youth in different alcohol policy contexts. J Stud Alcohol Drugs. 2011;72(3):418–428. doi: 10.15288/jsad.2011.72.418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miech R, Johnston L, O’Malley P, Bachman J, Schulenberg J. Monitoring the Future national survey results on drug use, 1975 – 2015: Volume 1, Secondary school students. Ann Arbor: Institute for Social Research, U of Michigan; 2016. [Google Scholar]
- Miller WR. Motivation for treatment: A review with special emphasis on alcoholism. Psychol Bull. 1985;98(1):84–107. doi: 10.1037/0033-2909.98.1.84. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people to change addictive behavior. New York: Guilford Press; 1991. [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2. New York: Guilford Press; 2002. [Google Scholar]
- Miller WR, Sovereign RG. The check-up: A model for early intervention in addictive behaviors. In: Loberg T, Miller WR, Nathan PE, Marlatt GA, editors. Addictive behaviors: Prevention and early intervention. Amsterdam: Swits & Zeitlinger; 1989. pp. 219–231. [Google Scholar]
- Moyers TB, Martin T, Manuel JK, Miller WR, Ernst D. Motivational Interviewing Treatment Integrity (MITI 3.1.1) Center on Alcoholism, Substance Abuse and Addictions: University of New Mexico; 2010. [Google Scholar]
- Poelen EA, Engels RC, Van Der Vorst H, Scholte RH, Vermulst AA. Best friends and alcohol consumption in adolescence: a within-family analysis. Drug Alcohol Depend. 2007;88(2–3):163–173. doi: 10.1016/j.drugalcdep.2006.10.008. [DOI] [PubMed] [Google Scholar]
- Ryan J, Roman NV, Okwany A. The effects of parental monitoring and communication on adolescent substance use and risky activity: A systematic review. TOFAMSJ. 2015;7:12–27. [Google Scholar]
- Scholte RH, Poelen EA, Willemsen G, Boomsma DI, Engels RC. Relative risks of adolescent and young adult alcohol use: the role of drinking fathers, mothers, siblings, and friends. Addict Behav. 2008;33(1):1–14. doi: 10.1016/j.addbeh.2007.04.015. [DOI] [PubMed] [Google Scholar]
- Siegel DM, Aten MJ, Roghmann KJ. Self-reported honesty among middle and high school students responding to a sexual behavior questionnaire. J Adolesc Health. 1998;23(1):20–28. doi: 10.1016/s1054-139x(97)00274-7. [DOI] [PubMed] [Google Scholar]
- Spirito A, Monti P, Barnett N, Colby S, Sindelar H, Rohsenow D, Lewander W, Myers M. A randomized clinical trial of a brief motivational intervention for alcohol positive adolescents treated in an Emergency Department. J Pediatr. 2004;145:396–402. doi: 10.1016/j.jpeds.2004.04.057. [DOI] [PubMed] [Google Scholar]
- Spirito A, Sindelar-Manning H, Colby SM, Barnett NP, Lewander W, Rohsenow DJ, Monti PM. Individual and family motivational interventions for alcohol-positive adolescents treated in an emergency department: Results of a randomized clinical trial. Arch Pediatr Adolesc Med. 2011;165(3):269–274. doi: 10.1001/archpediatrics.2010.296. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/21383276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stattin H, Kerr M. Parental monitoring: A reinterpretation. Child Dev. 2000;71(4):1072–1085. doi: 10.1111/1467-8624.00210. [DOI] [PubMed] [Google Scholar]
- Stormshak EA, Comeau CA, Shepard SA. The relative contribution of sibling deviance and peer deviance in the prediction of substance use across middle childhood. J Abnorm Child Psychol. 2004;32(6):635–649. doi: 10.1023/b:jacp.0000047212.49463.c7. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/15648530. [DOI] [PubMed] [Google Scholar]
- Stout RL, Wirtz PW, Carbonari JP, Del Boca FK. Ensuring balanced distribution of prognostic factors in treatment outcome research. J Stud Alcohol Drugs. 1994;12:70–75. doi: 10.15288/jsas.1994.s12.70. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/7723001. [DOI] [PubMed] [Google Scholar]
- Stueve A, O’Donnell LN. Early alcohol initiation and subsequent sexual and alcohol risk behaviors among urban youths. Am J Public Health. 2005;95(5):887–893. doi: 10.2105/ajph.2003.026567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trim RS, Leuthe E, Chassin L. Sibling influence on alcohol use in a young adult, high-risk sample. J Stud Alcohol. 2006;67(3):391–398. doi: 10.15288/jsa.2006.67.391. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/16608148. [DOI] [PubMed] [Google Scholar]
- Waldron HB, Slesnick N, Brody JL, Turner CW, Peterson TR. Treatment outcomes for adolescent substance abuse at 4-and 7-month assessments. J Consult Clin Psych. 2001;69(5):802–813. Retrieved from <Go to ISI>://000171572400007. [PubMed] [Google Scholar]
- Whiteman SD, Jensen AC, Maggs JL. Similarities in Adolescent Siblings’ Substance Use: Testing Competing Pathways of Influence. J Stud Alcohol Drugs. 2013;74(1):104–113. doi: 10.15288/jsad.2013.74.104. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3517254/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang LN, Welte JW, Wieczorek WF. Peer and parental influences on male adolescent drinking. Subst Use Misuse. 1997;32(14):2121–2136. doi: 10.3109/10826089709035624. Retrieved from <Go to ISI>://000071198000009. [DOI] [PubMed] [Google Scholar]