Abstract
Myelin oligodendrocyte glycoprotein (MOG), a member of the immunoglobulin (Ig) superfamily, is a myelin protein solely expressed at the outermost surface of myelin sheaths and oligodendrocyte membranes. This makes MOG a potential target of cellular and humoral immune responses in inflammatory demyelinating diseases. Due to its late postnatal developmental expression, MOG is an important marker for oligodendrocyte maturation. Discovered about 30 years ago, it is one of the best-studied autoantigens for experimental autoimmune models for multiple sclerosis (MS). Human studies, however, have yielded controversial results on the role of MOG, especially MOG antibodies (Abs), as a biomarker in MS. But with improved detection methods using different expression systems to detect Abs in patients’ samples, this is meanwhile no longer the case. Using cell-based assays with recombinant full-length, conformationally intact MOG, several recent studies have revealed that MOG Abs can be found in a subset of predominantly pediatric patients with acute disseminated encephalomyelitis (ADEM), aquaporin-4 (AQP4) seronegative neuromyelitis optica spectrum disorders (NMOSD), monophasic or recurrent isolated optic neuritis (ON), or transverse myelitis, in atypical MS and in N-methyl-d-aspartate receptor-encephalitis with overlapping demyelinating syndromes. Whereas MOG Abs are only transiently observed in monophasic diseases such as ADEM and their decline is associated with a favorable outcome, they are persistent in multiphasic ADEM, NMOSD, recurrent ON, or myelitis. Due to distinct clinical features within these diseases it is controversially disputed to classify MOG Ab-positive cases as a new disease entity. Neuropathologically, the presence of MOG Abs is characterized by MS-typical demyelination and oligodendrocyte pathology associated with Abs and complement. However, it remains unclear whether MOG Abs are a mere inflammatory bystander effect or truly pathogenetic. This article provides deeper insight into recent developments, the clinical relevance of MOG Abs and their role in the immunpathogenesis of inflammatory demyelinating disorders.
Keywords: myelin oligodendrocyte glycoprotein, demyelination, autoantibodies, inflammation, MOG
Molecular Structure and Function of Myelin Oligodendrocyte Glycoprotein (MOG)
Myelin oligodendrocyte glycoprotein is a minor myelin component, with a length of 245 amino acids (AA) and a molecular weight of 26–28 kDa. It is only present in mammals and has a highly conserved nucleotide and AA structure within different species (1). The human MOG gene is located at chromosome 6 within the human leukocyte antigen (HLA) gene locus, whereas the mouse MOG gene is located on chromosome 17 within the major histocompatibility complex (MHC) gene locus (2). MOG is exclusively expressed in the central nervous system (CNS) on the surface of myelin sheaths and oligodendrocyte processes (1–3). MOG expression starts at the onset of myelination and is therefore a potential differentiation marker for oligodendrocyte maturation (4). The function of MOG is not yet fully understood, but its molecular structure and its extracellular immunoglobulin (Ig) domain indicate a possible function as a cell surface receptor or cell adhesion molecule (5). MOG belongs to the Ig superfamily, with a single extracellular immunoglobuline variable (IgV) domain, one transmembrane domain, one cytoplasmic loop, a membrane-associated region, and a cytoplasmic tail (6). Fifteen different alternatively spliced isoforms have been detected in humans. Full-length variants alpha 1 and beta 1 are found in fetal stages, whereas alternative variants are expressed in later postnatal stages (1, 6). It has been shown, that these isoforms are localized on the cell surface, in the endoplasmic reticulum, in the endocytic system, or can be found in a secreted form. The secreted form could have important effects triggering autoimmunity if released into the cerebrospinal fluid (CSF) and then drained into the periphery. The cytoplasmic tail of MOG determines the intracellular localization of the various splice forms and could play a role in intracellular signaling (6). The cross-linking of antibodies (Abs) reactive with the extracellular domain of MOG resulted in the activation of intracellular signaling cascades resulting in survival signals, changes of cytoskeletal stability, and cellular stress responses (7). MOG is highly homologous to butyrophilins which are expressed in mammary glands (8) and might cause autoimmunity by molecular mimicry (9). Furthermore, a sequence homology of MOG AA 35–55 (MOG35–55) to medium-sized neurofilament leads to the activation of MOG35–55 specific T cells (10).
Myelin oligodendrocyte glycoprotein has been implicated to be the cellular receptor for Rubella virus (11), as a ligand for DC-SIGN on antigen-expressing cells (12), and as a receptor for nerve growth factor (13). The interaction of DC-SIGN and MOG along with its correct glycosylation might keep myeloid antigen-presenting cells (APC) in an immature and tolerogenic state and thereby prevent autoimmunity (12). However, the inactivation of mouse MOG by gene targeting resulted in no clinical or histological abnormalities (14, 15).
Whereas the biological function of MOG is still not clear, its topology at the surface of myelin and oligodendrocytes and its special characteristics predict MOG to be a very important target of autoantibodies and cell-mediated immune responses in inflammatory demyelinating diseases. Initially, MOG was discovered as a dominant target of autoantibodies (they so called it M2 antigen) after immunization of guinea pigs with CNS tissue (16, 17). Numerous studies have then established an important role of MOG as autoantigen for T and B cell responses in experimental models and inflammatory demyelinating diseases.
Autoimmune Responses Against MOG in Animal Models
The first indications that humoral factors also contribute to demyelination have been described in 1947 by Kabat et al. who observed a demyelinating effect after immunization of rhesus monkeys with heterologous rabbit or homologous brain tissue (18). In 1968, it was noted that sera from guinea pigs sensitized with whole CNS preparations have a demyelinating effect in vitro (19). The first indication that MOG Abs might be pathogenic followed about 10 years later when it was observed that guinea pigs immunized with the M2 protein developed Abs with demyelinating activity in vitro (20, 21). Then, it was shown that the monoclonal MOG-specific Ab 8–18C5 induces demyelination in Lewis (LEW) rats with experimental autoimmune encephalomyelitis (EAE) (4, 22), that guinea pigs immunized with M2 show demyelinated lesions in their CNS, and that the M2 protein is identical to MOG (16). It soon became clear that MOG Abs may be pathogenic in a large number of additional species (Table 1) (23). Further characterizations of MOG revealed that this protein is found in the oligodendrocyte membrane with a large N-terminal extracellular IgG V-like domain (8) and that N-terminal domain (AA 1–125) is responsible for the formation of demyelinating Abs (23, 24). Studies in marmoset monkeys and mice clarified that pathogenic Abs recognize conformational epitopes on the extracellularly exposed MOG domain (25–27) and that strain specific differences in mounting such anti-conformational Ab responses correlate with exacerbation of diseases (28, 29). Epitopes for encephalitogenic T cells for many different strains of mice and for LEW rats are found on the extracellular domain of MOG (30–33), but also in its transmembrane region (34, 35) (Table 2).
Table 1.
The effects of myelin oligodendrocyte glycoprotein (MOG)-specific antibodies (Abs).
| Reference | Year | Findings |
|---|---|---|
| Trotter et al. (36) | 1986 | Myelin-specific Abs trigger macrophage-mediated demyelination |
| Linington and Lassmann (17) | 1987 | Ab-mediated demyelination in a chronic relapsing experimental autoimmune encephalomyelitis (EAE) in guinea pigs |
| Schluesener et al. (37) | 1887 | Monoclonal MOG Abs induced fatal relapses in a model of chronic relapsing-remitting EAE in SJL mice and enhanced acute EAE in Lewis (LEW) rats with increased inflammation and demyelination |
| Lassmann et al. (22) | 1988 | Demyelination occurs in a synergistic way between cellular (T cells) and humoral immune mechanisms |
| Linington et al. (4) | 1988 | MOG Abs augment demyelination in a myelin basic protein (MBP) T cell-mediated EAE model in LEW rats |
| Kerlero de Rosbo et al. (38) | 1990 | Monoclonal MOG Abs together with complement lead to demyelination and MBP loss in brain cells |
| Scolding and Compston (39) | 1991 | Abs mediate macrophage-dependent phagocytosis of oligodendrocytes in vitro |
| Vass et al. (40) | 1992 | MOG Ab-mediated demyelination is intensified by interferon-gamma |
| Linington et al. (41) | 1992 | Abs prevent tolarization effect of repeatedly induced MBP-T cell-mediated EAE and enhances demyelination |
| Piddlesden et al. (42) | 1993 | Ab-mediated demyelination is dependent on complement recruiting ability and independent on its epitope recognition |
| Genain et al. (43) | 1995 | MOG Abs facilitate demyelination in MOG-induced EAE in common marmosets |
| Johns et al. (44) | 1995 | MOG Abs lead to degradation of MBP and increased myelin protease activity |
| Ichikawa et al. (45) | 1996 | MOG35–55 encephalitogenic in LEW rats and a potential target for Ab-mediated demyelination |
| Menon et al. (46) | 1997 | Ab induced MBP loss and myelin destabilization by neutral proteases in human myelin |
| Van der Goes et al. (47) | 1999 | Abs to MOG play a crucial role for the phagocytosis of myelin by macrophages in vitro |
| Von Budingen et al. (25) | 2002 | Ab pathogenicity in marmosets is dependent on their ability to bind on conformational epitopes |
| Marta et al. (48) | 2003 | Ab cross-linking on oligodendrocyte cultures leads to the formation of lipid rafts and to a reconstitution of MOG |
| Bourquin et al. (28) | 2003 | Generation of pathogenic Abs to conformational MOG in H-2b mice is dependent on genes encoded within the major histocompatibility complex |
| Von Budingen et al. (49) | 2004 | EAE phenotype in marmosets correlates with the availability of conformational MOG Abs resulting in typical multiple sclerosis-like disease pattern. In addition Abs to MOG peptides lead to focal disease pattern in brain stem and spinal cord. MBP T cell-mediated EAE animals showed no demyelination when injected with MOG peptides. By contrast, conformational MOG Abs were more pathologic as controls |
| Marta et al. (26) | 2005 | Human but not rat MOG-induced B cell-dependent EAE in MOG primed C57BL/6 mice and Abs of hMOG immunized mice only lead to EAE formation in B cell-deficient mice. Pathogenic Abs react to conformational intact and glycosylated antigen only |
| Zhou et al. (50) | 2006 | Patient-derived MOG Abs enhance demyelination in rat EAE models |
| Urich et al. (51) | 2006 | Ab-mediated demyelination is FcR independent but completely relies on complement activation |
| Jagessar et al. (52) | 2008 | Increased Ab-dependent demyelination in marmosets immunized with murine myelin compared to myelin lacking MOG |
| Harrer et al. (53) | 2009 | Complement induced demyelination in a murine ex vivo model |
| Ohtani et al. (54) | 2011 | Ab titer against conformational MOG are directly associated with EAE activity and demyelination in EAE rats |
| Mader et al. (55) | 2011 | Human MOG Abs lead to complement activated cytotoxicity in HEK293A cells |
| de Graaf et al. (27) | 2012 | Correct refolding of MOG increases its pathogenicity by generating conformation-dependent MOG Abs |
| Dale et al. (56) | 2014 | Oligodendrocytes incubated with purified human MOG IgG lead to organizational disturbances of the thin filaments and microtubule cytoskeleton |
| Saadoun et al. (57) | 2014 | Patient-derived MOG IgG lead to complement-independent myelin changes and altered expression of axonal proteins, but did not trigger inflammation or cellular death |
| Flach et al. (58) | 2016 | MOG Abs boost EAE by activation of effector T cells |
| Kinzel et al. (59) | 2016 | MOG Abs are able to trigger spontaneous EAE in mice harboring endogenous MOG-specific T cells in the absence of B cells |
Table 2.
T cell responses against myelin oligodendrocyte glycoprotein (MOG) in experimental autoimmune encephalomyelitis (EAE) animal models.
| Reference | Year | Finding |
|---|---|---|
| Linington et al. (33) | 1993 | MOG peptide (MOG44–53) specific T cells induce atypical EAE in Lewis (LEW) rats |
| Amor et al. (30) | 1994 | Epitope MOG1–22, MOG43–57, and MOG134–148 induce clinically and pathological relevant EAE, however, mild effects in AB/H mice. Epitope MOG92–106 is highly encephalitogenic in SJL mice |
| Adelmann et al. (24) | 1995 | N-terminal domain (MOG1–125) leads to demyelination in LEW rats, T cells reactive to epitope MOG1–20 and MOG35–55 are only weakly encephalitogenic in EAE model |
| Kerlero de Rosbo et al. (31) | 1995 | Mild pathological signs were detected by inducing MOG35–55 in PL/J mice |
| Mendel et al. (32) | 1995 | MOG35–55 induces highly reproducible EAE in C57BL/6J and C3H.SW (H-2b) mice |
| Devaux et al. (60) | 1997 | Severe EAE with truncated human MOG (1–120) in SJL and (PLJ × SJL) F1 mice, encephalitogenic T cell proliferation against epitope MOG92–106 |
| Slavin et al. (61) | 1998 | Relapsing-remitting disease course in NOD/Lt mice (H-2g7) and chronic paralytic disease course in C57BL/6 mice after injection of MOG35–55 |
| Weissert et al. (62) | 1998 | Major histocompatibility complex (MHC) haplotype influences the degree of disease susceptibility, recruitment of MOG-specific immune cells, and pathology in MOG-induced EAE rats |
| Storch et al. (63) | 1998 | Immunization with MOG antigen in rats is able to mimic classical multiple sclerosis (MS) as well and variants such as optic neuritis (ON), Devic’s and Marburg’s disease |
| Encinas et al. (64) | 1999 | Active immunization with MOG35–55 induces relapsing-remitting EAE followed by a secondary progression in NOD mice |
| Raine et al. (65) | 1999 | MOG-induced EAE in marmosets lead to vesicular disruption and production of antigen-specific autoantibodies similar to MS |
| Abdul-Majid et al. (66) | 2000 | MOG79–96 is highly encephalitogenic in DBA/1 mice, including macrophage infiltration and demyelination |
| Kerlero de Rosbo et al. (67) | 2000 | rhMOG-EAE induced marmosets with different MHC background showed proliferative T cell responses against epitopes MOG4–20, MOG35–50, and MOG94–116 |
| Bourquin et al. (68) | 2000 | MOG-DNA vaccination lead to severe EAE |
| Brok et al. (69) | 2000 | Human MOG peptide MOG14–36 is highly encephalitogenic in marmosets (presented by a common class II Caja-DRB*W1201 molecule) |
| Weissert et al. (70) | 2001 | MOG91–114 immunization lead to clinical and histopathological EAE signs in LEW.1AV1 and LEW.1N rats |
| Bettelli et al. (71) | 2003 | Development of spontaneous ON in T cell receptor (MOG35–55) transgenic C57BL/6 mice |
| Delarasse et al. (14) | 2003 | MOG-deficient mice are resistant to rat MOG-induced EAE and developed a mild pathological phenotype after immunization of whole myelin. However, B- and T cell responses against the extracellular domain and peptides of MOG were not altered compared to wild-type mice, indicating MOG being resistant to the induction of immune tolerance |
| Sun et al. (72) | 2003 | CD8+ MOG-specific T cells recognize H-2Db dimers coupled with encephalitogenic peptide MOG40–54 |
| Smith et al. (73) | 2005 | Injection of full-length conformational MOG leads to chronic progressive EAE, but released MOG does not induce immunity during an ongoing disease in Biozzi ABH mice |
| Krishnamoorthy et al. (74) | 2006 | MOG35–55 leads to paralytic EAE and ON in a double-transgenic (IgHMOG and TCRMOG) C57BL/6 line |
| de Graaf et al. (75) | 2008 | In LEW.1N, LEW.1AV1, and dark agouti rats, MS-like pathology is mainly determined by presentation of MOG peptides on MHC class II molecules |
| Kap et al. (76) | 2008 | Cytotoxic T cells specific to epitope MOG34–56 trigger fast progression of rhMOG-induced EAE in marmosets |
| Matsumoto et al. (77) | 2009 | MOG91–108 is an encephalitogenic epitope able to induce mild T cell-mediated EAE but does not elicit Abs against the epitope or MOG in LEW.1AV1 rats |
| Pollinger et al. (78) | 2009 | Development of relapsing-remitting EAE in TCR (MOG92–106) transgenic SJL/J mice |
| Bettini et al. (79) | 2009 | CD8+ T cell dominant epitope MOG37–46 lead to mild form of EAE |
| York et al. (80) | 2010 | MOG-specific CD8+ T cells are able to ameliorate CD4+ driven EAE |
| Anderson et al. (81) | 2012 | CD4+ and CD8+ T cell driven EAE in transgenic MOG35–55 specific T cell mouse line (1C6) |
| de Graaf et al. (27) | 2012 | Correct refolding of MOG increases its encephalogenicity by enhancing its processing or/and presentation on MHC molecules |
| Jagessar et al. (82) | 2012 | MOG34–56 specific cytotoxic T cells are key regulators for gray and white matter demyelination in marmosets |
| Delarasse et al. (34) | 2013 | Transmembrane regions MOG113–127 and MOG120–134 and second hydrophobic domain MOG183–197 are found to be immunogenic and pathogenic in C57BL/6 (H-2b) |
| Ortega et al. (83) | 2013 | CD8+ cells reactive to MOG35–55 attenuate EAE severity in an adaptive CD4 T cell-mediated EAE model in C57BL/6 mice |
| Haanstra et al. (84) | 2013 | rhMOG (1–125) induces EAE in non-human primates |
| Shetty et al. (35) | 2014 | T cells directed to an encephalitogenic transmembrane domain (MOG110–132) induced clinical EAE, inflammation, and demyelination |
| Curtis et al. (85) | 2014 | Injection of rat immunoglobuline variable of MOG together with incomplete Freud’s adjuvant lead to atypical EAE in LEW rats and Macaca species |
| Herrera et al. (86) | 2014 | MOG35–55 induced EAE in C57BL/6 mice lead to lesions along the optic chiasm |
Immunizations of LEW rats with MOG activates MOG1–20- and MOG35–55- specific T cells which are only poorly encephalitogenic (24) and induces MOG-specific Abs which cause formation of focal small demyelinating lesions (24). In contrast to LEW rats are brown Norway and dark agouti rat strains highly susceptible to MOG-induced EAE (87). Different MHC haplotypes and non-MHC background genes modify the anti-MOG immune response (70, 75). This important information derived from EAE studies in MHC congenic LEW rats, i.e., in rats with different MHC class II alleles on the genetic background of LEW rats. Upon immunization with MOG, these animals either develop early onset acute lethal disease with extensive demyelinating plaques, chronic and/or relapsing types of disease, or do not show any evidence of clinical and histological disease, depending on the MHC class II haplotype present (62). Moreover, the MOG-induced T cell proliferation and interferon-gamma production, and the degree of MOG-specific B cell responses and Ab titers correlated with the severity of clinical disease (62). For further experiments, rats were selected which carried the most permissive MHC class II haplotype for the induction of MOG-specific autoimmune reactions, but differed in their non-MHC background genes. When these animals were sensitized with MOG, they mounted anti-MOG T cell and B cell responses, but showed differences in the maturation of these responses (62). Cumulatively, these data suggested that the MHC haplotype influences the degree of disease susceptibility, the clinical course, the recruitment of MOG-specific immunocompetent cells, and the CNS pathology, while non-MHC genes strongly influence the maturation of the anti-MOG response (62). A similar effect was also seen in human HLA DR4 transgenic mice which indicated that HLA DR shaped the anti-MOG response in both, humans and mice (88).
Further knowledge about the role of B cells in MOG-induced CNS inflammation derived from transgenic mice (Table 3). Mice were genetically engineered to express the heavy chain from the monoclonal anti-MOG Ab 8–18C5 described above, paired with endogenous Ig light chains (89). These animals had many MOG-reactive B cells in their immune repertoire and had titers of anti-MOG Abs in their circulation. And yet, they remained completely healthy until they were challenged with MOG. Then, they developed EAE with higher incidence, severity, and earlier onset compared to their non-transgenic counterparts (89). Further studies using B cell-deficient mice showed that B cells are required for EAE induction using the MOG protein, but are dispensable when the encephalitogenic MOG peptide is used for EAE induction (90–92). These studies also revealed that B cells are needed for the recovery from EAE, by the production of IL-10 and expression of CD40 (93). The role of B cells in promoting EAE was further confirmed by using transgenic mouse lines in which MHC class II products were knocked-out in B cells, or in which B cells were able to express MOG-specific B cell receptors on their surface, but were unable to secrete MOG-specific Abs (94). This and several other studies (see Table 3) revealed that B cells can act as APC, and that they can sufficiently promote pro-inflammatory T cell activation and spontaneous EAE onset (91, 94, 95). In another study, in which MOG-specific B cells and T cells were actively transferred into an intact immune repertoire of C57BL/6J mice, MOG-specific B cells were shown to aggravate CNS inflammation and EAE disease course. These results were further confirmed by using human MOG positive serum Abs, reproducing the same disease accelerating effects (58). Hence, both B cells and myelin-specific Abs can independently activate T cells and thus increase the risk of an autoimmune mediated inflammation of the CNS (59).
Table 3.
The role of B cells in experimental autoimmune encephalomyelitis (EAE) animal models.
| Reference | Year | Findings |
|---|---|---|
| Hjelmstrom et al. (92) | 1998 | B cell-independent demyelination in myelin oligodendrocyte glycoprotein (MOG)-induced EAE mice |
| Litzenburger et al. (89) | 1998 | MOG-specific B cells accelerate and exacerbate EAE, but are not able to induce spontaneous disease or demyelination without induced EAE |
| Stefferl et al. (87) | 1999 | Major histocompatibility complex (MHC) and MHC-linked effects can influence the antibody response and thereby disease severity in MOG-induced EAE |
| Lyons et al. (90) | 1999 | B-cell-deficient mice immunized with MOG35–55 induced EAE but not mice immunized with recombinant full-length MOG |
| Forsthuber et al. (88) | 2001 | MOG peptide 97–108 is the immunodominant human leukocyte antigen (HLA)-DR4-restricted T cell epitope in transgenic mice and is presented by human B cells expressing HLA-DR4 (DRB1*0401) |
| Lyons et al. (91) | 2002 | MOG-specific B cells and serum reconstitute the ability for inducing inflammatory EAE effects in B cell-deficient mice |
| Fillatreau et al. (93) | 2002 | IL-10 production of B cells regulate type 1 immunity and play a key role in EAE recovery |
| Svensson et al. (96) | 2002 | B cell-deficient mice with different genetic backgrounds (C57BL/10 and DBA/1) immunized with MOG1–125 showed decreased demyelination but inflammation was not affected |
| Bettelli et al. (97) | 2006 | TCRMOG × IgHMOG mice develop severe EAE, with inflammatory lesions in the spinal cord and optic nerves |
| Pollinger et al. (78) | 2009 | Transgenic mice expressing MOG92–106 specific T cells expand endogenous MOG-specific B cells, producing conformational, (epitope independent) Abs, and enhancing demyelinating EAE in a relapsing-remitting EAE model |
| Molnarfi et al. (94) | 2013 | MOG-specific B cells play a critical role in the EAE pathogenesis due to its function as an antigen-presenting cells |
| Parker Harp et al. (95) | 2015 | B cells directly interact with dendritic cells and enhance CD4 driven EAE severity in mice |
| Flach et al. (58) | 2016 | MOG-specific B cells accelerate MOG T cell driven EAE inflammation and disease severity |
Also spontaneous models of MOG-induced CNS disease were highly informative for deciphering the role of anti-MOG responses in autoimmune disease. These models were based on the transgenic expression in mice of MOG-specific T cell receptors, either alone (71, 78) or in combination with MOG-specific B cell receptors (74, 97) and gave striking results:
The overexpression of MOG-specific T cell receptors in transgenic C57/BL6 (71) or SJL (78) mice lead to spontaneous optic neuritis (ON) in more than 30% of all animals and rendered the animals hyper-susceptible to the induction of ON in response to sensitization with suboptimal amounts of MOG (71), or to a severe spontaneous relapsing-remitting EAE with episodes often altering between different CNS compartments in more than 60% of all male, and more than 80% of all females within 160 days after birth (78). In these animals, the transgenic T cells expanded MOG-specific B cells from the endogenous immune repertoire, which produced pathogenic autoantibodies binding to a conformational epitope on native MOG protein (78). Overexpression of MOG-specific T cell receptors in NOD mice led to MOG-specific CD4+ and CD8+ T cell responses at the same time (79). These animals revealed that CD8+ MOG-specific T cells may be weakly encephalitogenic (79) and are able to regulate and attenuate CD4+ driven immune responses by modulating APC functions and reducing CD4+ T cell responses (80, 83).
Mice genetically engineered to express MOG-specific receptors on T and B cells (74, 97) showed a class switch of MOG Abs to an IgG1 subtype, and spontaneously developed inflammatory demyelinating CNS disease (74, 97). Most interestingly, spontaneous development of disease in these animals crucially depended on the presence of commensal microbiota in the gut (98).
Although many seminal observations on MOG-reactive T and B cell responses derive from murine EAE models, it is important to know that in these animals, large lesions with myelin loss are mainly caused by axonal degeneration with secondary demyelination, while primary demyelination is sparse (99, 100). Therefore, it is necessary to also study MOG autoreactivity in the marmoset (Callithrix jacchus), in which MOG-induced EAE resembles human demyelinating diseases more closely (100–102). When these animals are immunized with the recombinant IgV domain of rat MOG, they developed lesions which were very similar to chronic multiple sclerosis (MS) plaques with mononuclear cell infiltrates, primary demyelination, and astrogliosis (103), even at the ultrastructural level (65). Moreover, some animals developed a progressive form of EAE, which was triggered by cytotoxic effector memory T cells and further promoted demyelination in the gray matter (76, 82). As seen before in mice and rats, the marmoset CD4+ T cell response against MOG may cover several different epitopes, only one of which is highly encephalitogenic (104).
Cumulatively, these animal models revealed that
autoimmune responses to MOG can be induced in many different species
the susceptibility to MOG is determined by MHC- and non-MHC genes
anti-MOG responses typically involve CD4+ T cells and complement-fixing Abs of the IgG1 subtype
the MOG-specific T cell repertoire contains T cells specific for several different T cell epitopes which vary between different species and substrains dependent on the MHC haplotype
not all MOG-specific T cells are encephalitogenic
MOG-specific B cells have Ab-dependent and Ab-independent effects on tissue damage
different types of anti-MOG Abs exist, but only those recognizing conformational epitopes on the extracellular domain of MOG are pathogenic
MOG-specific autoantibodies in the circulation specific for such conformational epitopes are harmless, unless these Abs gain access to the CNS via an opened blood-brain barrier in an inflammatory environment
MOG-specific Abs can cross-react with other proteins like butyrophilin
the extent of demyelination caused by anti-MOG Abs depends on MHC-dependent and MHC-independent factors.
Clinical Relevance of MOG Abs in Demyelinating Diseases
As outlined above, MOG is one of the best-studied autoantigens for experimental autoimmune models for MS. Attempts to translate these findings into the human disease have yielded controversial results, especially with regard to MOG Abs as a prognostic biomarker in MS (105, 106) [reviewed in Berger et al. (107)]. These results were caused by the use of inappropriate methods (e.g., immunoblotting, ELISA) and antigens (recombinant human MOG produced in Escherichia coli, MOG peptides) to determine disease-specific MOG Abs. However, with improved detection methods using correctly folded and glycosylated MOG protein expressed in mammalian cells for radioimmunoassays, flow cytometry, and immunofluorescence, MOG Abs were found in a subset of predominantly pediatric patients with acute disseminated encephalomyelitis (ADEM), aquaporin-4 (AQP4) seronegative neuromyelitis optica spectrum disorders (NMOSD), monophasic or recurrent isolated ON, or transverse myelitis (TM), in atypical MS, brainstem encephalitis, and N-methyl-d-aspartate receptor-encephalitis with overlapping demyelinating syndromes, but rarely in classical MS (50, 55, 56, 108–176). Since low-titer MOG Abs are often found in MS patients and controls, most of these studies have used either a “high-titer” cut-off or an IgG1 secondary Ab to increase specificity. Like many other autoantibodies, e.g., to AQP4, MOG Abs are therefore only present in rare diseases indicating widely established immunological tolerance to most autoantigens.
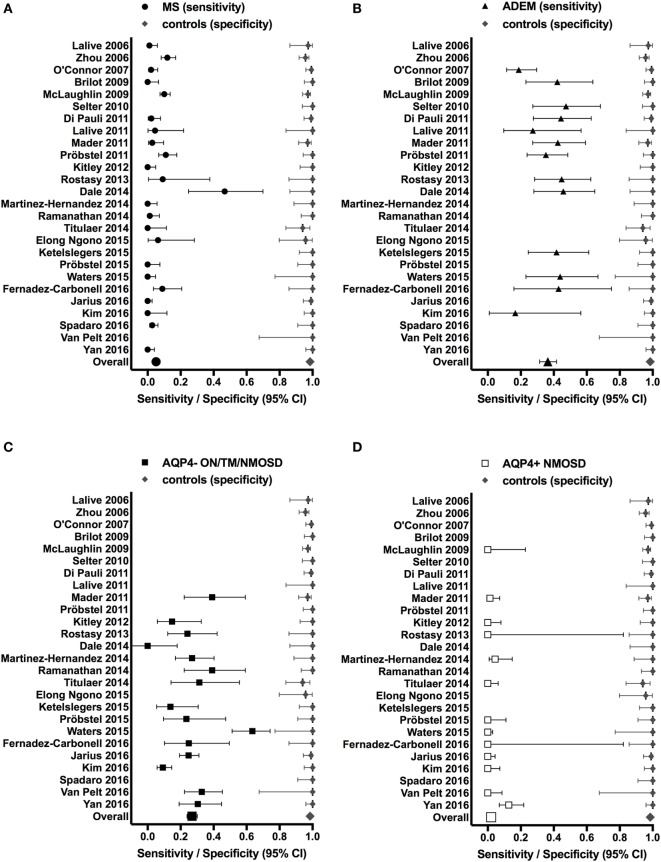
These findings, however, raise the important question whether MOG Abs are associated with a specific clinical phenotype like AQP4 Abs are associated with NMOSD (177). We have therefore reviewed the literature and compared all studies, which have analyzed the presence of MOG Abs in inflammatory demyelinating disorders (MS, ADEM, and AQP4 Ab seronegative and seropositive NMOSD) in comparison with a control group of patients with other neurological disorders or healthy controls. Results from these studies are shown in Table 4 and Figure 1. We have identified 26 studies which fulfilled these criteria (50, 55, 56, 109–116, 119, 121, 126, 130, 132, 134, 137, 141, 147, 148, 152, 156, 158, 165, 174). Only 13 of these studies included a control group with 50 or more individuals and only 5 studies included more than 100 controls (Table 4). Further, many patients and controls were repeatedly analyzed in some studies and therefore we decided not to include a statistical analysis of the reviewed publications. The specificity of these studies was calculated using the frequency of MOG Abs in other neurological disorders or healthy controls determined by the methods shown in Table 4. The overall specificity of these studies was 98.5% [95% confidence interval (CI) 97.8–99] and thus 1.5% (range 0–6%) of all controls were seropositive for MOG Abs (Table 4; Figure 1). The sensitivity of these studies was calculated using the frequency of MOG Abs in inflammatory demyelinating disorders determined by the methods shown in Table 4. The presence of MOG Abs in MS was analyzed in 23/26 studies and the overall sensitivity for MS was 5.1% (95% CI 4.2–6.1) and thus 5.1% (range 0–46.7%) of all MS patients were seropositive for MOG Abs. The highest frequency of MOG Abs within MS patients was found in pediatric MS patients and in one of the initial studies not using a high-titer cut-off. Therefore, it can be concluded that MOG Abs are rare in MS, particularly in adult MS, but are still found in a few patients in several studies. Since MOG Abs are associated with MS-like neuropathology (136, 149, 167, 172, 178, 179), they might play a role in pathophysiology in these patients and therefore the current practice to use MS as a negative control group for MOG Abs (141) should be regarded with caution. The presence of MOG Abs in ADEM was analyzed in 13/26 studies and the overall sensitivity for ADEM was 36.4% (95% CI 31.4–41.7; range 17.7–47.4%) and thus ADEM was the most frequent clinical presentation associated with MOG Abs. Again, the frequency of MOG Abs was highest in pediatric patients. Since the 26 studies used different clinical criteria for NMOSD, we reviewed the studies for the presence of MOG Abs in AQP4 seronegative patients with ON, TM, or NMOSD. The presence of MOG Abs in these conditions was analyzed in 15/26 studies and the overall sensitivity was 26.9% (95% CI 23.9–30.1; range 9.2–63.5%). Finally, the presence of MOG Abs in AQP4 seropositive NMOSD was analyzed in 13/26 studies and the overall sensitivity was 2% (95% CI 1.2–3.4; range 1.2–3.4%). Thus, the presence of MOG Abs in AQP4 Ab-positive NMOSD is in the range of the control group.
Table 4.
Studies reporting the presence of myelin oligodendrocyte glycoprotein (MOG) antibodies (Abs) in patients with inflammatory demyelinating disorders in comparison to a control group of patients with other neurological disorders and/or healthy controls.
| Reference | Method | Patients | Multiple sclerosis | Acute disseminated encephalomyelitis | Aquaporin-4 (AQP4)− optic neuritis/transverse myelitis/neuromyelitis optica spectrum disorders (NMOSD) | AQP4+ NMOSD | Controls |
|---|---|---|---|---|---|---|---|
| Lalive et al. (109) | FACS | ad | 1/92 (1%) | n.a. | n.a. | n.a. | 1/37 (3%) |
| Zhou et al. (50) | FACS | ad | 25/210 (12%) | n.a. | n.a. | n.a. | 8/187 (4%) |
| O’Connor et al. (110) | RIA | ad, ped | 3/140 (2%) | 13/69 (19%) | n.a. | n.a. | 1/133 (1%) |
| Brilot et al. (112) | FACS | ad, ped | 0/54 (0%) | 8/19 (42%) | n.a. | n.a | 0/73 (0%) |
| McLaughlin et al. (111) | FACS | ad, ped | 39/385 (10%) | n.a. | n.a. | 0/13 (0%) | 6/214 (3%) |
| Selter et al. (113) | FACS | ped | n.a. | 9/19 (47%) | n.a. | n.a. | 0/58 (0%) |
| Di Pauli et al. (115) | IF-HT | ad, ped | 2/89 (2%) | 12/27 (44%) | n.a. | n.a. | 1/105 (1%) |
| Lalive et al. 2011 (114) | FACS | ped | 1/22 (5%) | 3/11 (27%) | n.a. | n.a. | 0/20 (0%) |
| Mader et al. (55) | IF-HT | ad, ped | 2/71 (3%) | 14/33 (42%) | 9/23 (39%) | 1/75 (1%) | 3/101 (3%) |
| Probstel et al. (116) | FACS | ad, ped | 14/127 (11%) | 19/54 (35%) | n.a. | n.a. | 0/63 (0%) |
| Kitley et al. (119) | IF | ad | 0/75 (0%) | n.a. | 4/27 (15%) | 0/44 (0%) | 0/23 (0%) |
| Rostasy et al. (121) | IF-HT | ped | 1/11 (9%) | 13/29 (45%) | 7/29 (24%) | 0/2 (0%) | 0/23 (0%) |
| Dale et al. (56) | FACS | ped | 7/15 (47%) | 11/24 (46%) | 13/24 (54%) | n.a. | 0/24 (0%) |
| Martinez-Hernandez et al. (134) | IF-HT | ad | 0/64 (0%) | n.a. | 14/52 (27%) | 2/45 (4%) | 0/30 (0%) |
| Ramanathan et al. (130) | FACS | ad | 1/76 (1%) | n.a. | 9/23 (39%) | n.a. | 0/52 (0%) |
| Elong Ngono et al. (132) | IF-HT | ad | 1/16 (6%) | n.a. | n.a. | n.a. | 1/24 (4%) |
| Ketelslegers et al. (147) | FACS | ped | n.a. | 10/24 (42%) | 4/29 (14%) | n.a. | 0/44 (0%) |
| Probstel et al. (137) | FACS | ad | 0/48 (0%) | n.a. | 4/17 (24%) | 0/31 (0%) | 0/39 (0%) |
| Waters et al. (141) | IF-IgG1 | ad | 0/76 (0%) | 7/16 (44%) | 40/63 (64%) | 0/130 (0%) | 0/13 (0%) |
| Fernandez-Carbonell et al. (152) | FACS | ped | 4/45 (9%) | 3/7 (43%) | 4/14 (29%) | 0/2 (0%) | 0/23 (0%) |
| Jarius et al. (174) | IF-HT | ad, ped | 0/139 (0%) | n.a. | 50/202 (25%) | 0/83 (0%) | 1/98 (1%) |
| Kim et al. (148) | IF-IgG1 | ad | 0/29 (0%) | 1/6 (17%) | 15/163 (9%) | 0/49 (0%) | 0/72 (0%) |
| Spadaro et al. (165) | FACS | ad | 5/181 (3%) | n.a. | n.a. | n.a. | 0/39 (0%) |
| van Pelt et al. (158) | FACS | ad | n.a. | n.a. | 20/61 (33%) | 0/41 (0%) | 0/8 (0%) |
| Overall | 106/196 (5%) | 123/338 (36%) | 193/727 (27%) | 3/515 (1%) | 22/1527 (1%) |
The percentage of MOG Ab seropositivity was determined using the methods indicated in the table.
ad, adult; ped, pediatric; n.a., not analyzed; FACS, fluorescence-activated cell sorting; IF, immunofluorescence assay; IF-HT, immunofluorescence assay with high-titer cut-off; IF-IgG1, immunofluorescence assay for IgG1 Abs; RIA, radio immunoprecipitation assay.
Figure 1.
Studies reporting the presence of myelin oligodendrocyte glycoprotein (MOG) antibodies (Abs) in patients with inflammatory demyelinating disorders (A) MS; (B) ADEM; (C) AQP4− ON/TM/NMOSD; (D) AQP4+ NMOSD (sensitivity, left side of each graph) in comparison to a control group of patients with other neurological disorders and/or healthy controls (specificity, right side of each graph). Sensitivities and specificities are indicated by symbols with error bars (95% confidence intervals). Specificities were calculated using the frequency of MOG Abs in other neurological disorders or healthy controls determined by the methods shown in Table 4. Sensitivities were calculated using the frequency of MOG Abs in inflammatory demyelinating disorders determined by the methods shown in Table 4.
In conclusion, these studies revealed that MOG Abs are associated with heterogeneous clinical presentations and a younger age of onset in human inflammatory demyelinating diseases but a clear common clinical phenotype is missing.
The histopathology associated with MOG Abs has been described in few patients including NMOSD, atypical demyelination, CIS, and ADEM (136, 149, 167, 172, 178, 179) (Table 5). All cases showed demyelinating lesions with features of MS pattern II, with well-demarcated confluent plaques with loss of myelin, relative preservation of axons, well-preserved astrocytes, and numerous macrophages containing myelin debris. The inflammatory infiltrates were predominantly composed of perivascular and parenchymal T-cells and some perivascular B-cells. Moreover, the deposition of terminal complement complex C9neo was reported indicating complement-dependent cytotoxicity (136, 167). All lesions were characterized by well-preserved oligodendrocytes that were partly MOG-negative, most likely compatible with preoligodendrocytes. Demyelination associated with MOG Abs differs from AQP4 seropositive NMOSD that characteristically shows loss of astrocytes with deposition of IgG and terminal complement complex C9neo, inflammatory infiltrates including the presence of neutrophilic and eosinophilic granulocytes, and elevated glial fibrillary acidic protein levels in CSF (180).
Table 5.
Neuropathological findings in patients with myelin oligodendrocyte glycoprotein (MOG) antibody (Ab)-associated demyelination.
| Reference | Number of cases | Sex, age (years) | Clinical presentation | Findings |
|---|---|---|---|---|
| Konig et al. (178) | 1 | F, 49 | RRMS | Multiple sclerosis (MS) pattern II; oligodendrocytes in lesion preserved (CNPase+; MOG not determined) |
| Spadaro et al. (136) | 1 | F, 66 | Recurrent myelitis + brainstem involvement | MS pattern II; oligodendrocytes preserved (CNPase+; MOG−) |
| Di Pauli et al. (149) | 1 | M, 71 | Acute disseminated encephalomyelitis (ADEM)/acute MS | MOG and aquaporin-4 Ab positive; MS pattern II; oligodendrocytes preserved (CNPase+, MOG−) |
| Jarius et al. (172) | 1 | F, 63 | CIS | MS pattern II; oligodendrocytes preserved (CNPase+, MOG+) |
| Wang et al. (167) | 1 | F, 67 | Neuromyelitis optica spectrum disorders | Pattern classification not done; well-demarcated demyelinating lesion with preserved axons and astrocytes |
| Körtvélyessy et al. (179) | 2 | M, 49 | ADEM | Intrathecal MOG Ab synthesis; MS pattern II; one patient with overlapping features of pattern III (early MAG loss, apoptotic oligodendrocytes in addition to complement deposition) |
| M, 34 |
These similar immunopathological findings compatible with MS pattern II supports a humoral immune pathogenesis in patients with MOG Abs. Since the histopathological lesion type is independent from the clinical presentation the demyelinating lesions may be included under the term “MOG antibody syndrome.”
Epitope Recognition and Species Specificity of Human MOG Abs
As MOG Ab binding has been shown to be dependent on the correct folding and glycosylation pattern of their antigen, studies were directed toward the binding motifs/epitopes of these Abs with the aim to identify specific binding patterns for diseases. Mayer and colleagues (122) performed epitope recognition studies of MOG Abs from several demyelinating diseases and seven distinct binding patterns were found. However, no clinical correlation between the binding patterns and different disease entities could be shown. Furthermore, these Abs were directed against only a single epitope or multiple epitopes and an association between glycosylation and an increased binding capacity could not be detected. The most frequent epitopes were found in the CC′-loop and FG-loop of the extracellular IgV domain of correctly folded human MOG protein. Within the CC′-loop, AA P42 was essential for binding and therefore human MOG Abs did not bind either to rodent MOG, which has a serine at position 42, or to mutated human MOG P42S (122). These findings were confirmed and extended by Sepulveda et al. (166) who demonstrated that only a subset of human MOG Abs is also reactive to rodent MOG epitopes as analyzed by cell-based assays and tissue immunohistochemistry and this reactivity to rodent MOG did not correlate with a specific clinical phenotype. Finally, it has been already demonstrated that species differences of MOG lead to the activation of different pathogenic mechanisms in EAE induced with rodent or human MOG35–55 or recombinant MOG (26, 92, 181).
MOG Abs: Epiphenomenon or Indicative for Disease Phenotype
The animal experiments described above clearly indicated that murine MOG Abs can be pathogenic. Furthermore, pathologic similarities to ADEM have been shown in transgenic MOG-IgG mice infected with several neurotrophic encephalitogenic viruses, exacerbating virus-induced CNS inflammation. These similarities were indicated by clinical defined extensive perivascular infiltrates (mixed inflammatory cell population, e.g., lymphocytes, neutrophils, NK cells, and blood born macrophages) and perivenous demyelination (182, 183).
By contrast, only four studies aimed to investigate the pathogenic role of human MOG Abs in vivo. Whereas several studies indicated that human MOG Abs can activate complement and cellular-dependent cytotoxicity (50, 55, 112) in vitro, these mechanisms were not observed after transfer of human MOG Abs to rodents in vivo: the injection of concentrated serum samples from MOG Ab-positive patients into LEW rats with EAE did not increase the clinical score of the disease, but led to a minor increase in demyelination and axonal loss (50). Intrathecal injection of purified human MOG IgG caused reversible brain edema and myelin loss with very little complement deposition at the lesion site (57).
A different pathogenic mechanism for MOG Abs was proposed in two recent studies (58, 59). In the first study (58), it was demonstrated that MOG-specific B cells and their products (MOG Abs) activate MOG-specific effector T cells via CNS resident APC. A similar effect was demonstrated for peripheral APC in the second study (59). Both studies emphasize an important role for Ab-mediated antigen opsonization and accumulation in Fc receptor expressing APCs and subsequent increased antigen presentation and activation of specific T cells.
Are MOG Abs a Primary or a Secondary Immune Response?
The findings discussed in the previous chapter raise the important question whether human MOG Abs are pathogenic themselves or just a epiphenomenal bystander or a secondary immune reaction due to previous demyelination (184). An example for a secondary immune response was shown in a study using a transgenic myelin-specific T cell mice model, which developed spontaneous EAE (98). In this model, an interaction between MOG-specific T and B cells is necessary for inflammatory demyelination, resulting in the activation of native B cells by dendritic cells presenting MOG peptides in the cervical lymph nodes (78). In a gut germ free environment, autoreactive T cell activation failed, and therefore the signal cascade for producing autoantibodies producing B cells was significantly reduced, but increased after microbial re-colonization. One potential mechanism mediating the onset of spontaneous EAE is molecular mimicry, activating encephalitogenic T cells, with subsequent inflammation of the CNS and second, it leads to an activation of native MOG-specific B cells recruited to the CNS tissue via locally produced MOG material or drained into the CNS along peripheral lymph nodes.
But even if MOG Abs would only be a secondary immune reaction they still could be clinically relevant biomarkers such as seen in diabetes type I, an autoimmune disease affecting insulin producing β-cells in the pancreas. Four autoantibodies to insulin (185), glutamic acid decarboxylase (186), Islet antigen-2 (187), and zinc transporter 8 (188) have been identified as highly specific biomarkers to predict this disease. There is more than an 80% probability of developing diabetes in children and adolescents, if 2/4 autoantibodies are detected [reviewed in Bonifacio (189)]. However, these autoantibodies are not pathogenic itself, but rather indicate a disturbed immune activity or an underlying T cell-mediated autoimmune process (190). Similarly, it could be that human MOG Abs play only a minor role in the pathophysiology of inflammatory demyelination, but are highly specific markers for affected patients.
Conclusion
In the past years, autoantibodies emerged as important biomarkers in neurological autoimmune diseases. One of the best examples for these biomarkers is AQP4 Abs as diagnostic marker for NMOSD. Numerous studies have now established a possible similar role for MOG Abs that are associated with a very heterogeneous age-dependent clinical presentation and MS-like neuropathology. The exact pathologic effect of human MOG Abs is still unclear and needs to be critically investigated in order to clarify the immunopathological role of these Abs.
Author Contributions
PP prepared the main body of the manuscript and tables. MB and TB participated in the preparation of the manuscript. RH participated in the preparation of the manuscript and prepared tables and figures. MR supervised the work and participated in the preparation of the manuscript and figures and tables. All authors approved the final version of the manuscript.
Conflict of Interest Statement
The Neurological Research Laboratory (Medical University of Innsbruck and Tirol Kliniken) receives payments for antibody assays (AQP4- and anti-neuronal antibodies) and for MOG and AQP4 antibody validation experiments organized by Euroimmun (Germany).
Acknowledgments
The authors are grateful to A. Navarro for proof-reading and comments on the manuscript.
Funding
PP and MR are supported by a research grant from the Fonds zur Förderung der wissenschaftlichen Forschung, Austria (FWF graduate program W1206 SPIN).
Abbreviations
AA, amino acids; Ab, antibody; ADEM, acute disseminated encephalomyelitis; AQP4, aquaporin-4; BN, brown Norway; CNS, central nervous system; CSF, cerebrospinal fluid; DA, dark agouti; EAE, experimental autoimmune encephalomyelitis; HLA, human leukocyte antigen; Ig, immunoglobulin; MBP, myelin basic protein; MHC, major histocompatibility complex; MOG, myelin oligodendrocyte glycoprotein; MS, multiple sclerosis; NMOSD, neuromyelitis optica spectrum disorders; ON, optic neuritis; TM, transverse myelitis.
References
- 1.Delarasse C, Della Gaspera B, Lu CW, Lachapelle F, Gelot A, Rodriguez D, et al. Complex alternative splicing of the myelin oligodendrocyte glycoprotein gene is unique to human and non-human primates. J Neurochem (2006) 98(6):1707–17. 10.1111/j.1471-4159.2006.04053.x [DOI] [PubMed] [Google Scholar]
- 2.Pham-Dinh D, Mattei MG, Nussbaum JL, Roussel G, Pontarotti P, Roeckel N, et al. Myelin/oligodendrocyte glycoprotein is a member of a subset of the immunoglobulin superfamily encoded within the major histocompatibility complex. Proc Natl Acad Sci U S A (1993) 90(17):7990–4. 10.1073/pnas.90.17.7990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brunner C, Lassmann H, Waehneldt TV, Matthieu JM, Linington C. Differential ultrastructural localization of myelin basic protein, myelin/oligodendroglial glycoprotein, and 2′,3′-cyclic nucleotide 3′-phosphodiesterase in the CNS of adult rats. J Neurochem (1989) 52(1):296–304. 10.1111/j.1471-4159.1989.tb10930.x [DOI] [PubMed] [Google Scholar]
- 4.Linington C, Bradl M, Lassmann H, Brunner C, Vass K. Augmentation of demyelination in rat acute allergic encephalomyelitis by circulating mouse monoclonal antibodies directed against a myelin/oligodendrocyte glycoprotein. Am J Pathol (1988) 130(3):443–54. [PMC free article] [PubMed] [Google Scholar]
- 5.Martini R, Schachner M. Immunoelectron microscopic localization of neural cell adhesion molecules (L1, N-CAM, and MAG) and their shared carbohydrate epitope and myelin basic protein in developing sciatic nerve. J Cell Biol (1986) 103(6 Pt 1):2439–48. 10.1083/jcb.103.6.2439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boyle LH, Traherne JA, Plotnek G, Ward R, Trowsdale J. Splice variation in the cytoplasmic domains of myelin oligodendrocyte glycoprotein affects its cellular localisation and transport. J Neurochem (2007) 102(6):1853–62. 10.1111/j.1471-4159.2007.04687.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marta CB, Montano MB, Taylor CM, Taylor AL, Bansal R, Pfeiffer SE. Signaling cascades activated upon antibody cross-linking of myelin oligodendrocyte glycoprotein: potential implications for multiple sclerosis. J Biol Chem (2005) 280(10):8985–93. 10.1074/jbc.M413174200 [DOI] [PubMed] [Google Scholar]
- 8.Gardinier MV, Amiguet P, Linington C, Matthieu JM. Myelin/oligodendrocyte glycoprotein is a unique member of the immunoglobulin superfamily. J Neurosci Res (1992) 33(1):177–87. 10.1002/jnr.490330123 [DOI] [PubMed] [Google Scholar]
- 9.Guggenmos J, Schubart AS, Ogg S, Andersson M, Olsson T, Mather IH, et al. Antibody cross-reactivity between myelin oligodendrocyte glycoprotein and the milk protein butyrophilin in multiple sclerosis. J Immunol (2004) 172(1):661–8. 10.4049/jimmunol.172.1.661 [DOI] [PubMed] [Google Scholar]
- 10.Krishnamoorthy G, Saxena A, Mars LT, Domingues HS, Mentele R, Ben-Nun A, et al. Myelin-specific T cells also recognize neuronal autoantigen in a transgenic mouse model of multiple sclerosis. Nat Med (2009) 15(6):626–32. 10.1038/nm.1975 [DOI] [PubMed] [Google Scholar]
- 11.Cong H, Jiang Y, Tien P. Identification of the myelin oligodendrocyte glycoprotein as a cellular receptor for rubella virus. J Virol (2011) 85(21):11038–47. 10.1128/JVI.05398-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Garcia-Vallejo JJ, Ilarregui JM, Kalay H, Chamorro S, Koning N, Unger WW, et al. CNS myelin induces regulatory functions of DC-SIGN-expressing, antigen-presenting cells via cognate interaction with MOG. J Exp Med (2014) 211(7):1465–83. 10.1084/jem.20122192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.von Budingen HC, Mei F, Greenfield A, Jahn S, Shen YA, Reid HH, et al. The myelin oligodendrocyte glycoprotein directly binds nerve growth factor to modulate central axon circuitry. J Cell Biol (2015) 210(6):891–8. 10.1083/jcb.201504106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Delarasse C, Daubas P, Mars LT, Vizler C, Litzenburger T, Iglesias A, et al. Myelin/oligodendrocyte glycoprotein-deficient (MOG-deficient) mice reveal lack of immune tolerance to MOG in wild-type mice. J Clin Invest (2003) 112(4):544–53. 10.1172/JCI15861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Linares D, Mana P, Goodyear M, Chow AM, Clavarino C, Huntington ND, et al. The magnitude and encephalogenic potential of autoimmune response to MOG is enhanced in MOG deficient mice. J Autoimmun (2003) 21(4):339–51. 10.1016/j.jaut.2003.09.001 [DOI] [PubMed] [Google Scholar]
- 16.Lebar R, Baudrimont M, Vincent C. Chronic experimental autoimmune encephalomyelitis in the Guinea pig. Presence of anti-M2 antibodies in central nervous system tissue and the possible role of M2 autoantigen in the induction of the disease. J Autoimmun (1989) 2(2):115–32. 10.1016/0896-8411(89)90149-2 [DOI] [PubMed] [Google Scholar]
- 17.Linington C, Lassmann H. Antibody responses in chronic relapsing experimental allergic encephalomyelitis: correlation of serum demyelinating activity with antibody titre to the myelin/oligodendrocyte glycoprotein (MOG). J Neuroimmunol (1987) 17(1):61–9. 10.1016/0165-5728(87)90031-2 [DOI] [PubMed] [Google Scholar]
- 18.Kabat EA, Wolf A, Bezer AE. The rapid production of acute disseminated encephalomyelitis in rhesus monkeys by injection of heterologous and homologous brain tissue with adjuvants. J Exp Med (1947) 85(1):117–30. 10.1084/jem.85.1.117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Seil FJ, Falk GA, Kies MW, Alvord EC., Jr The in vitro demyelinating activity of sera from Guinea pigs sensitized with whole CNS and with purified encephalitogen. Exp Neurol (1968) 22(4):545–55. 10.1016/0014-4886(68)90148-9 [DOI] [PubMed] [Google Scholar]
- 20.Lebar R, Boutry JM, Vincent C, Robineaux R, Voisin GA. Studies on autoimmune encephalomyelitis in the Guinea pig. II. An in vitro investigation on the nature, properties, and specificity of the serum-demyelinating factor. J Immunol (1976) 116(5):1439–46. [PubMed] [Google Scholar]
- 21.Lebar R, Vincent C, Fischer-le Boubennec E. Studies on autoimmune encephalomyelitis in the Guinea pig – III. A comparative study of two autoantigens of central nervous system myelin. J Neurochem (1979) 32(5):1451–60. 10.1111/j.1471-4159.1979.tb11084.x [DOI] [PubMed] [Google Scholar]
- 22.Lassmann H, Brunner C, Bradl M, Linington C. Experimental allergic encephalomyelitis: the balance between encephalitogenic T lymphocytes and demyelinating antibodies determines size and structure of demyelinated lesions. Acta Neuropathol (1988) 75(6):566–76. 10.1007/BF00686201 [DOI] [PubMed] [Google Scholar]
- 23.Bradl M, Linington C. Animal models of demyelination. Brain Pathol (1996) 6(3):303–11. 10.1111/j.1750-3639.1996.tb00857.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Adelmann M, Wood J, Benzel I, Fiori P, Lassmann H, Matthieu JM, et al. The N-terminal domain of the myelin oligodendrocyte glycoprotein (MOG) induces acute demyelinating experimental autoimmune encephalomyelitis in the Lewis rat. J Neuroimmunol (1995) 63(1):17–27. 10.1016/0165-5728(95)00124-7 [DOI] [PubMed] [Google Scholar]
- 25.von Budingen HC, Hauser SL, Fuhrmann A, Nabavi CB, Lee JI, Genain CP. Molecular characterization of antibody specificities against myelin/oligodendrocyte glycoprotein in autoimmune demyelination. Proc Natl Acad Sci U S A (2002) 99(12):8207–12. 10.1073/pnas.122092499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Marta CB, Oliver AR, Sweet RA, Pfeiffer SE, Ruddle NH. Pathogenic myelin oligodendrocyte glycoprotein antibodies recognize glycosylated epitopes and perturb oligodendrocyte physiology. Proc Natl Acad Sci U S A (2005) 102(39):13992–7. 10.1073/pnas.0504979102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.de Graaf KL, Albert M, Weissert R. Autoantigen conformation influences both B- and T-cell responses and encephalitogenicity. J Biol Chem (2012) 287(21):17206–13. 10.1074/jbc.M111.304246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bourquin C, Schubart A, Tobollik S, Mather I, Ogg S, Liblau R, et al. Selective unresponsiveness to conformational B cell epitopes of the myelin oligodendrocyte glycoprotein in H-2b mice. J Immunol (2003) 171(1):455–61. 10.4049/jimmunol.171.1.455 [DOI] [PubMed] [Google Scholar]
- 29.Berer K, Wekerle H, Krishnamoorthy G. B cells in spontaneous autoimmune diseases of the central nervous system. Mol Immunol (2011) 48(11):1332–7. 10.1016/j.molimm.2010.10.025 [DOI] [PubMed] [Google Scholar]
- 30.Amor S, Groome N, Linington C, Morris MM, Dornmair K, Gardinier MV, et al. Identification of epitopes of myelin oligodendrocyte glycoprotein for the induction of experimental allergic encephalomyelitis in SJL and Biozzi AB/H mice. J Immunol (1994) 153(10):4349–56. [PubMed] [Google Scholar]
- 31.Kerlero de Rosbo N, Mendel I, Ben-Nun A. Chronic relapsing experimental autoimmune encephalomyelitis with a delayed onset and an atypical clinical course, induced in PL/J mice by myelin oligodendrocyte glycoprotein (MOG)-derived peptide: preliminary analysis of MOG T cell epitopes. Eur J Immunol (1995) 25(4):985–93. 10.1002/eji.1830250419 [DOI] [PubMed] [Google Scholar]
- 32.Mendel I, Kerlero de Rosbo N, Ben-Nun A. A myelin oligodendrocyte glycoprotein peptide induces typical chronic experimental autoimmune encephalomyelitis in H-2b mice: fine specificity and T cell receptor V beta expression of encephalitogenic T cells. Eur J Immunol (1995) 25(7):1951–9. 10.1002/eji.1830250723 [DOI] [PubMed] [Google Scholar]
- 33.Linington C, Berger T, Perry L, Weerth S, Hinze-Selch D, Zhang Y, et al. T cells specific for the myelin oligodendrocyte glycoprotein mediate an unusual autoimmune inflammatory response in the central nervous system. Eur J Immunol (1993) 23(6):1364–72. 10.1002/eji.1830230627 [DOI] [PubMed] [Google Scholar]
- 34.Delarasse C, Smith P, Baker D, Amor S. Novel pathogenic epitopes of myelin oligodendrocyte glycoprotein induce experimental autoimmune encephalomyelitis in C57BL/6 mice. Immunology (2013) 140(4):456–64. 10.1111/imm.12155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shetty A, Gupta SG, Varrin-Doyer M, Weber MS, Prod’homme T, Molnarfi N, et al. Immunodominant T-cell epitopes of MOG reside in its transmembrane and cytoplasmic domains in EAE. Neurol Neuroimmunol Neuroinflamm (2014) 1(2):e22. 10.1212/NXI.0000000000000022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Trotter J, DeJong LJ, Smith ME. Opsonization with antimyelin antibody increases the uptake and intracellular metabolism of myelin in inflammatory macrophages. J Neurochem (1986) 47(3):779–89. 10.1111/j.1471-4159.1986.tb00679.x [DOI] [PubMed] [Google Scholar]
- 37.Schluesener HJ, Sobel RA, Linington C, Weiner HL. A monoclonal antibody against a myelin oligodendrocyte glycoprotein induces relapses and demyelination in central nervous system autoimmune disease. J Immunol (1987) 139(12):4016–21. [PubMed] [Google Scholar]
- 38.Kerlero de Rosbo N, Honegger P, Lassmann H, Matthieu JM. Demyelination induced in aggregating brain cell cultures by a monoclonal antibody against myelin/oligodendrocyte glycoprotein. J Neurochem (1990) 55(2):583–7. 10.1111/j.1471-4159.1990.tb04173.x [DOI] [PubMed] [Google Scholar]
- 39.Scolding NJ, Compston DA. Oligodendrocyte-macrophage interactions in vitro triggered by specific antibodies. Immunology (1991) 72(1):127–32. [PMC free article] [PubMed] [Google Scholar]
- 40.Vass K, Heininger K, Schafer B, Linington C, Lassmann H. Interferon-gamma potentiates antibody-mediated demyelination in vivo. Ann Neurol (1992) 32(2):198–206. 10.1002/ana.410320212 [DOI] [PubMed] [Google Scholar]
- 41.Linington C, Engelhardt B, Kapocs G, Lassman H. Induction of persistently demyelinated lesions in the rat following the repeated adoptive transfer of encephalitogenic T cells and demyelinating antibody. J Neuroimmunol (1992) 40(2–3):219–24. 10.1016/0165-5728(92)90136-9 [DOI] [PubMed] [Google Scholar]
- 42.Piddlesden SJ, Lassmann H, Zimprich F, Morgan BP, Linington C. The demyelinating potential of antibodies to myelin oligodendrocyte glycoprotein is related to their ability to fix complement. Am J Pathol (1993) 143(2):555–64. [PMC free article] [PubMed] [Google Scholar]
- 43.Genain CP, Nguyen MH, Letvin NL, Pearl R, Davis RL, Adelman M, et al. Antibody facilitation of multiple sclerosis-like lesions in a nonhuman primate. J Clin Invest (1995) 96(6):2966–74. 10.1172/JCI118368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Johns TG, Kerlero de Rosbo N, Menon KK, Abo S, Gonzales MF, Bernard CC. Myelin oligodendrocyte glycoprotein induces a demyelinating encephalomyelitis resembling multiple sclerosis. J Immunol (1995) 154(10):5536–41. [PubMed] [Google Scholar]
- 45.Ichikawa M, Johns TG, Adelmann M, Bernard CC. Antibody response in Lewis rats injected with myelin oligodendrocyte glycoprotein derived peptides. Int Immunol (1996) 8(11):1667–74. 10.1093/intimm/8.11.1667 [DOI] [PubMed] [Google Scholar]
- 46.Menon KK, Piddlesden SJ, Bernard CC. Demyelinating antibodies to myelin oligodendrocyte glycoprotein and galactocerebroside induce degradation of myelin basic protein in isolated human myelin. J Neurochem (1997) 69(1):214–22. 10.1046/j.1471-4159.1997.69010214.x [DOI] [PubMed] [Google Scholar]
- 47.Van der Goes A, Kortekaas M, Hoekstra K, Dijkstra CD, Amor S. The role of anti-myelin (auto)-antibodies in the phagocytosis of myelin by macrophages. J Neuroimmunol (1999) 101(1):61–7. 10.1016/S0165-5728(99)00133-2 [DOI] [PubMed] [Google Scholar]
- 48.Marta CB, Taylor CM, Coetzee T, Kim T, Winkler S, Bansal R, et al. Antibody cross-linking of myelin oligodendrocyte glycoprotein leads to its rapid repartitioning into detergent-insoluble fractions, and altered protein phosphorylation and cell morphology. J Neurosci (2003) 23(13):5461–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.von Budingen HC, Hauser SL, Ouallet JC, Tanuma N, Menge T, Genain CP. Frontline: epitope recognition on the myelin/oligodendrocyte glycoprotein differentially influences disease phenotype and antibody effector functions in autoimmune demyelination. Eur J Immunol (2004) 34(8):2072–83. 10.1002/eji.200425050 [DOI] [PubMed] [Google Scholar]
- 50.Zhou D, Srivastava R, Nessler S, Grummel V, Sommer N, Bruck W, et al. Identification of a pathogenic antibody response to native myelin oligodendrocyte glycoprotein in multiple sclerosis. Proc Natl Acad Sci U S A (2006) 103(50):19057–62. 10.1073/pnas.0607242103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Urich E, Gutcher I, Prinz M, Becher B. Autoantibody-mediated demyelination depends on complement activation but not activatory Fc-receptors. Proc Natl Acad Sci U S A (2006) 103(49):18697–702. 10.1073/pnas.0607283103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jagessar SA, Smith PA, Blezer E, Delarasse C, Pham-Dinh D, Laman JD, et al. Autoimmunity against myelin oligodendrocyte glycoprotein is dispensable for the initiation although essential for the progression of chronic encephalomyelitis in common marmosets. J Neuropathol Exp Neurol (2008) 67(4):326–40. 10.1097/NEN.0b013e31816a6851 [DOI] [PubMed] [Google Scholar]
- 53.Harrer MD, von Budingen HC, Stoppini L, Alliod C, Pouly S, Fischer K, et al. Live imaging of remyelination after antibody-mediated demyelination in an ex-vivo model for immune mediated CNS damage. Exp Neurol (2009) 216(2):431–8. 10.1016/j.expneurol.2008.12.027 [DOI] [PubMed] [Google Scholar]
- 54.Ohtani S, Kohyama K, Matsumoto Y. Autoantibodies recognizing native MOG are closely associated with active demyelination but not with neuroinflammation in chronic EAE. Neuropathology (2011) 31(2):101–11. 10.1111/j.1440-1789.2010.01131.x [DOI] [PubMed] [Google Scholar]
- 55.Mader S, Gredler V, Schanda K, Rostasy K, Dujmovic I, Pfaller K, et al. Complement activating antibodies to myelin oligodendrocyte glycoprotein in neuromyelitis optica and related disorders. J Neuroinflammation (2011) 8:184. 10.1186/1742-2094-8-184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dale RC, Tantsis EM, Merheb V, Kumaran RY, Sinmaz N, Pathmanandavel K, et al. Antibodies to MOG have a demyelination phenotype and affect oligodendrocyte cytoskeleton. Neurol Neuroimmunol Neuroinflamm (2014) 1(1):e12. 10.1212/NXI.0000000000000012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Saadoun S, Waters P, Owens GP, Bennett JL, Vincent A, Papadopoulos MC. Neuromyelitis optica MOG-IgG causes reversible lesions in mouse brain. Acta Neuropathol Commun (2014) 2:35. 10.1186/2051-5960-2-35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Flach AC, Litke T, Strauss J, Haberl M, Gomez CC, Reindl M, et al. Autoantibody-boosted T-cell reactivation in the target organ triggers manifestation of autoimmune CNS disease. Proc Natl Acad Sci U S A (2016) 113(12):3323–8. 10.1073/pnas.1519608113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kinzel S, Lehmann-Horn K, Torke S, Hausler D, Winkler A, Stadelmann C, et al. Myelin-reactive antibodies initiate T cell-mediated CNS autoimmune disease by opsonization of endogenous antigen. Acta Neuropathol (2016) 132(1):43–58. 10.1007/s00401-016-1559-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Devaux B, Enderlin F, Wallner B, Smilek DE. Induction of EAE in mice with recombinant human MOG, and treatment of EAE with a MOG peptide. J Neuroimmunol (1997) 75(1–2):169–73. 10.1016/S0165-5728(97)00019-2 [DOI] [PubMed] [Google Scholar]
- 61.Slavin A, Ewing C, Liu J, Ichikawa M, Slavin J, Bernard CC. Induction of a multiple sclerosis-like disease in mice with an immunodominant epitope of myelin oligodendrocyte glycoprotein. Autoimmunity (1998) 28(2):109–20. 10.3109/08916939809003872 [DOI] [PubMed] [Google Scholar]
- 62.Weissert R, Wallstrom E, Storch MK, Stefferl A, Lorentzen J, Lassmann H, et al. MHC haplotype-dependent regulation of MOG-induced EAE in rats. J Clin Invest (1998) 102(6):1265–73. 10.1172/JCI3022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Storch MK, Stefferl A, Brehm U, Weissert R, Wallstrom E, Kerschensteiner M, et al. Autoimmunity to myelin oligodendrocyte glycoprotein in rats mimics the spectrum of multiple sclerosis pathology. Brain Pathol (1998) 8(4):681–94. 10.1111/j.1750-3639.1998.tb00194.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Encinas JA, Wicker LS, Peterson LB, Mukasa A, Teuscher C, Sobel R, et al. QTL influencing autoimmune diabetes and encephalomyelitis map to a 0.15-cM region containing Il2. Nat Genet (1999) 21(2):158–60. 10.1038/5941 [DOI] [PubMed] [Google Scholar]
- 65.Raine CS, Cannella B, Hauser SL, Genain CP. Demyelination in primate autoimmune encephalomyelitis and acute multiple sclerosis lesions: a case for antigen-specific antibody mediation. Ann Neurol (1999) 46(2):144–60. [DOI] [PubMed] [Google Scholar]
- 66.Abdul-Majid KB, Jirholt J, Stadelmann C, Stefferl A, Kjellen P, Wallstrom E, et al. Screening of several H-2 congenic mouse strains identified H-2(q) mice as highly susceptible to MOG-induced EAE with minimal adjuvant requirement. J Neuroimmunol (2000) 111(1–2):23–33. 10.1016/S0165-5728(00)00360-X [DOI] [PubMed] [Google Scholar]
- 67.Kerlero de Rosbo N, Brok HP, Bauer J, Kaye JF, ‘t Hart BA, Ben-Nun A. Rhesus monkeys are highly susceptible to experimental autoimmune encephalomyelitis induced by myelin oligodendrocyte glycoprotein: characterisation of immunodominant T- and B-cell epitopes. J Neuroimmunol (2000) 110(1–2):83–96. 10.1016/S0165-5728(00)00306-4 [DOI] [PubMed] [Google Scholar]
- 68.Bourquin C, Iglesias A, Berger T, Wekerle H, Linington C. Myelin oligodendrocyte glycoprotein-DNA vaccination induces antibody-mediated autoaggression in experimental autoimmune encephalomyelitis. Eur J Immunol (2000) 30(12):3663–71. [DOI] [PubMed] [Google Scholar]
- 69.Brok HP, Uccelli A, Kerlero De Rosbo N, Bontrop RE, Roccatagliata L, de Groot NG, et al. Myelin/oligodendrocyte glycoprotein-induced autoimmune encephalomyelitis in common marmosets: the encephalitogenic T cell epitope pMOG24-36 is presented by a monomorphic MHC class II molecule. J Immunol (2000) 165(2):1093–101. 10.4049/jimmunol.165.2.1093 [DOI] [PubMed] [Google Scholar]
- 70.Weissert R, de Graaf KL, Storch MK, Barth S, Linington C, Lassmann H, et al. MHC class II-regulated central nervous system autoaggression and T cell responses in peripheral lymphoid tissues are dissociated in myelin oligodendrocyte glycoprotein-induced experimental autoimmune encephalomyelitis. J Immunol (2001) 166(12):7588–99. 10.4049/jimmunol.166.12.7588 [DOI] [PubMed] [Google Scholar]
- 71.Bettelli E, Pagany M, Weiner HL, Linington C, Sobel RA, Kuchroo VK. Myelin oligodendrocyte glycoprotein-specific T cell receptor transgenic mice develop spontaneous autoimmune optic neuritis. J Exp Med (2003) 197(9):1073–81. 10.1084/jem.20021603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sun D, Zhang Y, Wei B, Peiper SC, Shao H, Kaplan HJ. Encephalitogenic activity of truncated myelin oligodendrocyte glycoprotein (MOG) peptides and their recognition by CD8+ MOG-specific T cells on oligomeric MHC class I molecules. Int Immunol (2003) 15(2):261–8. 10.1093/intimm/dxg023 [DOI] [PubMed] [Google Scholar]
- 73.Smith PA, Heijmans N, Ouwerling B, Breij EC, Evans N, van Noort JM, et al. Native myelin oligodendrocyte glycoprotein promotes severe chronic neurological disease and demyelination in Biozzi ABH mice. Eur J Immunol (2005) 35(4):1311–9. 10.1002/eji.200425842 [DOI] [PubMed] [Google Scholar]
- 74.Krishnamoorthy G, Lassmann H, Wekerle H, Holz A. Spontaneous opticospinal encephalomyelitis in a double-transgenic mouse model of autoimmune T cell/B cell cooperation. J Clin Invest (2006) 116(9):2385–92. 10.1172/JCI28330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.de Graaf KL, Barth S, Herrmann MM, Storch MK, Wiesmuller KH, Weissert R. Characterization of the encephalitogenic immune response in a model of multiple sclerosis. Eur J Immunol (2008) 38(1):299–308. 10.1002/eji.200737475 [DOI] [PubMed] [Google Scholar]
- 76.Kap YS, Smith P, Jagessar SA, Remarque E, Blezer E, Strijkers GJ, et al. Fast progression of recombinant human myelin/oligodendrocyte glycoprotein (MOG)-induced experimental autoimmune encephalomyelitis in marmosets is associated with the activation of MOG34-56-specific cytotoxic T cells. J Immunol (2008) 180(3):1326–37. 10.4049/jimmunol.180.3.1326 [DOI] [PubMed] [Google Scholar]
- 77.Matsumoto Y, Park IK, Hiraki K, Ohtani S, Kohyama K. Role of pathogenic T cells and autoantibodies in relapse and progression of myelin oligodendrocyte glycoprotein-induced autoimmune encephalomyelitis in LEW.1AV1 rats. Immunology (2009) 128(1 Suppl):e250–61. 10.1111/j.1365-2567.2008.02955.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Pollinger B, Krishnamoorthy G, Berer K, Lassmann H, Bosl MR, Dunn R, et al. Spontaneous relapsing-remitting EAE in the SJL/J mouse: MOG-reactive transgenic T cells recruit endogenous MOG-specific B cells. J Exp Med (2009) 206(6):1303–16. 10.1084/jem.20090299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Bettini M, Rosenthal K, Evavold BD. Pathogenic MOG-reactive CD8+ T cells require MOG-reactive CD4+ T cells for sustained CNS inflammation during chronic EAE. J Neuroimmunol (2009) 213(1–2):60–8. 10.1016/j.jneuroim.2009.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.York NR, Mendoza JP, Ortega SB, Benagh A, Tyler AF, Firan M, et al. Immune regulatory CNS-reactive CD8+T cells in experimental autoimmune encephalomyelitis. J Autoimmun (2010) 35(1):33–44. 10.1016/j.jaut.2010.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Anderson AC, Chandwaskar R, Lee DH, Sullivan JM, Solomon A, Rodriguez-Manzanet R, et al. A transgenic model of central nervous system autoimmunity mediated by CD4+ and CD8+ T and B cells. J Immunol (2012) 188(5):2084–92. 10.4049/jimmunol.1102186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Jagessar SA, Heijmans N, Blezer EL, Bauer J, Blokhuis JH, Wubben JA, et al. Unravelling the T-cell-mediated autoimmune attack on CNS myelin in a new primate EAE model induced with MOG34-56 peptide in incomplete adjuvant. Eur J Immunol (2012) 42(1):217–27. 10.1002/eji.201141863 [DOI] [PubMed] [Google Scholar]
- 83.Ortega SB, Kashi VP, Tyler AF, Cunnusamy K, Mendoza JP, Karandikar NJ. The disease-ameliorating function of autoregulatory CD8 T cells is mediated by targeting of encephalitogenic CD4 T cells in experimental autoimmune encephalomyelitis. J Immunol (2013) 191(1):117–26. 10.4049/jimmunol.1300452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Haanstra KG, Jagessar SA, Bauchet AL, Doussau M, Fovet CM, Heijmans N, et al. Induction of experimental autoimmune encephalomyelitis with recombinant human myelin oligodendrocyte glycoprotein in incomplete Freund’s adjuvant in three non-human primate species. J Neuroimmune Pharmacol (2013) 8(5):1251–64. 10.1007/s11481-013-9487-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Curtis AD, II, Taslim N, Reece SP, Grebenciucova E, Ray RH, Rosenbaum MD, et al. The extracellular domain of myelin oligodendrocyte glycoprotein elicits atypical experimental autoimmune encephalomyelitis in rat and macaque species. PLoS One (2014) 9(10):e110048. 10.1371/journal.pone.0110048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Herrera SL, Palmer VL, Whittaker H, Smith BC, Kim A, Schellenberg AE, et al. Damage to the optic chiasm in myelin oligodendrocyte glycoprotein-experimental autoimmune encephalomyelitis mice. Magn Reson Insights (2014) 7:23–31. 10.4137/MRI.S19750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Stefferl A, Brehm U, Storch M, Lambracht-Washington D, Bourquin C, Wonigeit K, et al. Myelin oligodendrocyte glycoprotein induces experimental autoimmune encephalomyelitis in the “resistant” brown Norway rat: disease susceptibility is determined by MHC and MHC-linked effects on the B cell response. J Immunol (1999) 163(1):40–9. [PubMed] [Google Scholar]
- 88.Forsthuber TG, Shive CL, Wienhold W, de Graaf K, Spack EG, Sublett R, et al. T cell epitopes of human myelin oligodendrocyte glycoprotein identified in HLA-DR4 (DRB1*0401) transgenic mice are encephalitogenic and are presented by human B cells. J Immunol (2001) 167(12):7119–25. 10.4049/jimmunol.167.12.7119 [DOI] [PubMed] [Google Scholar]
- 89.Litzenburger T, Fassler R, Bauer J, Lassmann H, Linington C, Wekerle H, et al. B lymphocytes producing demyelinating autoantibodies: development and function in gene-targeted transgenic mice. J Exp Med (1998) 188(1):169–80. 10.1084/jem.188.1.169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Lyons JA, San M, Happ MP, Cross AH. B cells are critical to induction of experimental allergic encephalomyelitis by protein but not by a short encephalitogenic peptide. Eur J Immunol (1999) 29(11):3432–9. [DOI] [PubMed] [Google Scholar]
- 91.Lyons JA, Ramsbottom MJ, Cross AH. Critical role of antigen-specific antibody in experimental autoimmune encephalomyelitis induced by recombinant myelin oligodendrocyte glycoprotein. Eur J Immunol (2002) 32(7):1905–13. [DOI] [PubMed] [Google Scholar]
- 92.Hjelmstrom P, Juedes AE, Fjell J, Ruddle NH. B-cell-deficient mice develop experimental allergic encephalomyelitis with demyelination after myelin oligodendrocyte glycoprotein sensitization. J Immunol (1998) 161(9):4480–3. [PubMed] [Google Scholar]
- 93.Fillatreau S, Sweenie CH, McGeachy MJ, Gray D, Anderton SM. B cells regulate autoimmunity by provision of IL-10. Nat Immunol (2002) 3(10):944–50. 10.1038/ni833 [DOI] [PubMed] [Google Scholar]
- 94.Molnarfi N, Schulze-Topphoff U, Weber MS, Patarroyo JC, Prod’homme T, Varrin-Doyer M, et al. MHC class II-dependent B cell APC function is required for induction of CNS autoimmunity independent of myelin-specific antibodies. J Exp Med (2013) 210(13):2921–37. 10.1084/jem.20130699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Parker Harp CR, Archambault AS, Sim J, Ferris ST, Mikesell RJ, Koni PA, et al. B cell antigen presentation is sufficient to drive neuroinflammation in an animal model of multiple sclerosis. J Immunol (2015) 194(11):5077–84. 10.4049/jimmunol.1402236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Svensson L, Abdul-Majid KB, Bauer J, Lassmann H, Harris RA, Holmdahl R. A comparative analysis of B cell-mediated myelin oligodendrocyte glycoprotein-experimental autoimmune encephalomyelitis pathogenesis in B cell-deficient mice reveals an effect on demyelination. Eur J Immunol (2002) 32(7):1939–46. [DOI] [PubMed] [Google Scholar]
- 97.Bettelli E, Baeten D, Jager A, Sobel RA, Kuchroo VK. Myelin oligodendrocyte glycoprotein-specific T and B cells cooperate to induce a Devic-like disease in mice. J Clin Invest (2006) 116(9):2393–402. 10.1172/JCI28334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Berer K, Mues M, Koutrolos M, Rasbi ZA, Boziki M, Johner C, et al. Commensal microbiota and myelin autoantigen cooperate to trigger autoimmune demyelination. Nature (2011) 479(7374):538–41. 10.1038/nature10554 [DOI] [PubMed] [Google Scholar]
- 99.Lassmann H, Bradl M. Multiple sclerosis: experimental models and reality. Acta Neuropathol (2017) 133(2):223–44. 10.1007/s00401-016-1631-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Hoftberger R, Leisser M, Bauer J, Lassmann H. Autoimmune encephalitis in humans: how closely does it reflect multiple sclerosis? Acta Neuropathol Commun (2015) 3(1):80. 10.1186/s40478-015-0260-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.‘t Hart BA, Gran B, Weissert R. EAE: imperfect but useful models of multiple sclerosis. Trends Mol Med (2011) 17(3):119–25. 10.1016/j.molmed.2010.11.006 [DOI] [PubMed] [Google Scholar]
- 102.‘t Hart BA, van Kooyk Y, Geurts JJ, Gran B. The primate autoimmune encephalomyelitis model; a bridge between mouse and man. Ann Clin Transl Neurol (2015) 2(5):581–93. 10.1002/acn3.194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Massacesi L, Genain CP, Lee-Parritz D, Letvin NL, Canfield D, Hauser SL. Active and passively induced experimental autoimmune encephalomyelitis in common marmosets: a new model for multiple sclerosis. Ann Neurol (1995) 37(4):519–30. 10.1002/ana.410370415 [DOI] [PubMed] [Google Scholar]
- 104.Genain CP, Hauser SL. Experimental allergic encephalomyelitis in the New World monkey Callithrix jacchus. Immunol Rev (2001) 183:159–72. 10.1034/j.1600-065x.2001.1830113.x [DOI] [PubMed] [Google Scholar]
- 105.Berger T, Rubner P, Schautzer F, Egg R, Ulmer H, Mayringer I, et al. Antimyelin antibodies as a predictor of clinically definite multiple sclerosis after a first demyelinating event. N Engl J Med (2003) 349(2):139–45. 10.1056/NEJMoa022328 [DOI] [PubMed] [Google Scholar]
- 106.Kuhle J, Pohl C, Mehling M, Edan G, Freedman MS, Hartung HP, et al. Lack of association between antimyelin antibodies and progression to multiple sclerosis. N Engl J Med (2007) 356(4):371–8. 10.1056/NEJMoa063602 [DOI] [PubMed] [Google Scholar]
- 107.Berger T, Reindl M. Antibody biomarkers in CNS demyelinating diseases – a long and winding road. Eur J Neurol (2015) 22(8):1162–8. 10.1111/ene.12759 [DOI] [PubMed] [Google Scholar]
- 108.Pache F, Zimmermann H, Mikolajczak J, Schumacher S, Lacheta A, Oertel FC, et al. MOG-IgG in NMO and related disorders: a multicenter study of 50 patients. Part 4: afferent visual system damage after optic neuritis in MOG-IgG-seropositive versus AQP4-IgG-seropositive patients. J Neuroinflammation (2016) 13(1):282. 10.1186/s12974-016-0720-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Lalive PH, Menge T, Delarasse C, Della Gaspera B, Pham-Dinh D, Villoslada P, et al. Antibodies to native myelin oligodendrocyte glycoprotein are serologic markers of early inflammation in multiple sclerosis. Proc Natl Acad Sci U S A (2006) 103(7):2280–5. 10.1073/pnas.0510672103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.O’Connor KC, McLaughlin KA, De Jager PL, Chitnis T, Bettelli E, Xu C, et al. Self-antigen tetramers discriminate between myelin autoantibodies to native or denatured protein. Nat Med (2007) 13(2):211–7. 10.1038/nm1488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.McLaughlin KA, Chitnis T, Newcombe J, Franz B, Kennedy J, McArdel S, et al. Age-dependent B cell autoimmunity to a myelin surface antigen in pediatric multiple sclerosis. J Immunol (2009) 183(6):4067–76. 10.4049/jimmunol.0801888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Brilot F, Dale RC, Selter RC, Grummel V, Kalluri SR, Aslam M, et al. Antibodies to native myelin oligodendrocyte glycoprotein in children with inflammatory demyelinating central nervous system disease. Ann Neurol (2009) 66(6):833–42. 10.1002/ana.21916 [DOI] [PubMed] [Google Scholar]
- 113.Selter RC, Brilot F, Grummel V, Kraus V, Cepok S, Dale RC, et al. Antibody responses to EBV and native MOG in pediatric inflammatory demyelinating CNS diseases. Neurology (2010) 74(21):1711–5. 10.1212/WNL.0b013e3181e04096 [DOI] [PubMed] [Google Scholar]
- 114.Lalive PH, Hausler MG, Maurey H, Mikaeloff Y, Tardieu M, Wiendl H, et al. Highly reactive anti-myelin oligodendrocyte glycoprotein antibodies differentiate demyelinating diseases from viral encephalitis in children. Mult Scler (2011) 17(3):297–302. 10.1177/1352458510389220 [DOI] [PubMed] [Google Scholar]
- 115.Di Pauli F, Mader S, Rostasy K, Schanda K, Bajer-Kornek B, Ehling R, et al. Temporal dynamics of anti-MOG antibodies in CNS demyelinating diseases. Clin Immunol (2011) 138(3):247–54. 10.1016/j.clim.2010.11.013 [DOI] [PubMed] [Google Scholar]
- 116.Probstel AK, Dornmair K, Bittner R, Sperl P, Jenne D, Magalhaes S, et al. Antibodies to MOG are transient in childhood acute disseminated encephalomyelitis. Neurology (2011) 77(6):580–8. 10.1212/WNL.0b013e318228c0b1 [DOI] [PubMed] [Google Scholar]
- 117.Kezuka T, Usui Y, Yamakawa N, Matsunaga Y, Matsuda R, Masuda M, et al. Relationship between NMO-antibody and anti-MOG antibody in optic neuritis. J Neuroophthalmol (2012) 32(2):107–10. 10.1097/WNO.0b013e31823c9b6c [DOI] [PubMed] [Google Scholar]
- 118.Rostasy K, Mader S, Schanda K, Huppke P, Gartner J, Kraus V, et al. Anti-myelin oligodendrocyte glycoprotein antibodies in pediatric patients with optic neuritis. Arch Neurol (2012) 69(6):752–6. 10.1001/archneurol.2011.2956 [DOI] [PubMed] [Google Scholar]
- 119.Kitley J, Woodhall M, Waters P, Leite MI, Devenney E, Craig J, et al. Myelin-oligodendrocyte glycoprotein antibodies in adults with a neuromyelitis optica phenotype. Neurology (2012) 79(12):1273–7. 10.1212/WNL.0b013e31826aac4e [DOI] [PubMed] [Google Scholar]
- 120.Huppke P, Rostasy K, Karenfort M, Huppke B, Seidl R, Leiz S, et al. Acute disseminated encephalomyelitis followed by recurrent or monophasic optic neuritis in pediatric patients. Mult Scler (2013) 19(7):941–6. 10.1177/1352458512466317 [DOI] [PubMed] [Google Scholar]
- 121.Rostasy K, Mader S, Hennes EM, Schanda K, Gredler V, Guenther A, et al. Persisting myelin oligodendrocyte glycoprotein antibodies in aquaporin-4 antibody negative pediatric neuromyelitis optica. Mult Scler (2013) 19(8):1052–9. 10.1177/1352458512470310 [DOI] [PubMed] [Google Scholar]
- 122.Mayer MC, Breithaupt C, Reindl M, Schanda K, Rostasy K, Berger T, et al. Distinction and temporal stability of conformational epitopes on myelin oligodendrocyte glycoprotein recognized by patients with different inflammatory central nervous system diseases. J Immunol (2013) 191(7):3594–604. 10.4049/jimmunol.1301296 [DOI] [PubMed] [Google Scholar]
- 123.Woodhall M, Coban A, Waters P, Ekizoglu E, Kurtuncu M, Shugaiv E, et al. Glycine receptor and myelin oligodendrocyte glycoprotein antibodies in Turkish patients with neuromyelitis optica. J Neurol Sci (2013) 335(1–2):221–3. 10.1016/j.jns.2013.08.034 [DOI] [PubMed] [Google Scholar]
- 124.Sato DK, Callegaro D, Lana-Peixoto MA, Waters PJ, de Haidar Jorge FM, Takahashi T, et al. Distinction between MOG antibody-positive and AQP4 antibody-positive NMO spectrum disorders. Neurology (2014) 82(6):474–81. 10.1212/WNL.0000000000000101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Kitley J, Waters P, Woodhall M, Leite MI, Murchison A, George J, et al. Neuromyelitis optica spectrum disorders with aquaporin-4 and myelin-oligodendrocyte glycoprotein antibodies: a comparative study. JAMA Neurol (2014) 71(3):276–83. 10.1001/jamaneurol.2013.5857 [DOI] [PubMed] [Google Scholar]
- 126.Titulaer MJ, Hoftberger R, Iizuka T, Leypoldt F, McCracken L, Cellucci T, et al. Overlapping demyelinating syndromes and anti-N-methyl-d-aspartate receptor encephalitis. Ann Neurol (2014) 75(3):411–28. 10.1002/ana.24117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Hacohen Y, Absoud M, Woodhall M, Cummins C, De Goede CG, Hemingway C, et al. Autoantibody biomarkers in childhood-acquired demyelinating syndromes: results from a national surveillance cohort. J Neurol Neurosurg Psychiatry (2014) 85(4):456–61. 10.1136/jnnp-2013-306411 [DOI] [PubMed] [Google Scholar]
- 128.Tanaka M, Tanaka K. Anti-MOG antibodies in adult patients with demyelinating disorders of the central nervous system. J Neuroimmunol (2014) 270(1–2):98–9. 10.1016/j.jneuroim.2014.03.001 [DOI] [PubMed] [Google Scholar]
- 129.Miyauchi A, Monden Y, Watanabe M, Sugie H, Morita M, Kezuka T, et al. Persistent presence of the anti-myelin oligodendrocyte glycoprotein autoantibody in a pediatric case of acute disseminated encephalomyelitis followed by optic neuritis. Neuropediatrics (2014) 45(3):196–9. 10.1055/s-0034-1371179 [DOI] [PubMed] [Google Scholar]
- 130.Ramanathan S, Reddel SW, Henderson A, Parratt JD, Barnett M, Gatt PN, et al. Antibodies to myelin oligodendrocyte glycoprotein in bilateral and recurrent optic neuritis. Neurol Neuroimmunol Neuroinflamm (2014) 1(4):e40. 10.1212/NXI.0000000000000040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Amano H, Miyamoto N, Shimura H, Sato DK, Fujihara K, Ueno S, et al. Influenza-associated MOG antibody-positive longitudinally extensive transverse myelitis: a case report. BMC Neurol (2014) 14:224. 10.1186/s12883-014-0224-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Elong Ngono A, Lepetit M, Reindl M, Garcia A, Guillot F, Genty A, et al. Decreased frequency of circulating myelin oligodendrocyte glycoprotein B lymphocytes in patients with relapsing-remitting multiple sclerosis. J Immunol Res (2015) 2015:673503. 10.1155/2015/673503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Tsuburaya RS, Miki N, Tanaka K, Kageyama T, Irahara K, Mukaida S, et al. Anti-myelin oligodendrocyte glycoprotein (MOG) antibodies in a Japanese boy with recurrent optic neuritis. Brain Dev (2015) 37(1):145–8. 10.1016/j.braindev.2014.02.002 [DOI] [PubMed] [Google Scholar]
- 134.Martinez-Hernandez E, Sepulveda M, Rostasy K, Hoftberger R, Graus F, Harvey RJ, et al. Antibodies to aquaporin 4, myelin-oligodendrocyte glycoprotein, and the glycine receptor alpha1 subunit in patients with isolated optic neuritis. JAMA Neurol (2015) 72(2):187–93. 10.1001/jamaneurol.2014.3602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Baumann M, Sahin K, Lechner C, Hennes EM, Schanda K, Mader S, et al. Clinical and neuroradiological differences of paediatric acute disseminating encephalomyelitis with and without antibodies to the myelin oligodendrocyte glycoprotein. J Neurol Neurosurg Psychiatry (2015) 86(3):265–72. 10.1136/jnnp-2014-308346 [DOI] [PubMed] [Google Scholar]
- 136.Spadaro M, Gerdes LA, Mayer MC, Ertl-Wagner B, Laurent S, Krumbholz M, et al. Histopathology and clinical course of MOG-antibody-associated encephalomyelitis. Ann Clin Transl Neurol (2015) 2(3):295–301. 10.1002/acn3.164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Probstel AK, Rudolf G, Dornmair K, Collongues N, Chanson JB, Sanderson NS, et al. Anti-MOG antibodies are present in a subgroup of patients with a neuromyelitis optica phenotype. J Neuroinflammation (2015) 12:46. 10.1186/s12974-015-0256-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Hacohen Y, Absoud M, Deiva K, Hemingway C, Nytrova P, Woodhall M, et al. Myelin oligodendrocyte glycoprotein antibodies are associated with a non-MS course in children. Neurol Neuroimmunol Neuroinflamm (2015) 2(2):e81. 10.1212/NXI.0000000000000081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Symmonds M, Waters PJ, Kuker W, Leite MI, Schulz UG. Anti-MOG antibodies with longitudinally extensive transverse myelitis preceded by CLIPPERS. Neurology (2015) 84(11):1177–9. 10.1212/WNL.0000000000001370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Morris KA, Waters P, Woodhall MR, Kuker W, Vincent A, Leite MI, et al. A 41-year-old woman with acute weakness and encephalopathy associated with MOG antibodies. Neurol Neuroimmunol Neuroinflamm (2015) 2(3):e88. 10.1212/NXI.0000000000000088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Waters P, Woodhall M, O’Connor KC, Reindl M, Lang B, Sato DK, et al. MOG cell-based assay detects non-MS patients with inflammatory neurologic disease. Neurol Neuroimmunol Neuroinflamm (2015) 2(3):e89. 10.1212/NXI.0000000000000089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Ikeda K, Kiyota N, Kuroda H, Sato DK, Nishiyama S, Takahashi T, et al. Severe demyelination but no astrocytopathy in clinically definite neuromyelitis optica with anti-myelin-oligodendrocyte glycoprotein antibody. Mult Scler (2015) 21(5):656–9. 10.1177/1352458514551455 [DOI] [PubMed] [Google Scholar]
- 143.Nakajima H, Motomura M, Tanaka K, Fujikawa A, Nakata R, Maeda Y, et al. Antibodies to myelin oligodendrocyte glycoprotein in idiopathic optic neuritis. BMJ Open (2015) 5(4):e007766. 10.1136/bmjopen-2015-007766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Hyun JW, Kim SH, Huh SY, Kim W, Yun J, Joung A, et al. Idiopathic aquaporin-4 antibody negative longitudinally extensive transverse myelitis. Mult Scler (2015) 21(6):710–7. 10.1177/1352458514551454 [DOI] [PubMed] [Google Scholar]
- 145.Hoftberger R, Sepulveda M, Armangue T, Blanco Y, Rostasy K, Cobo Calvo A, et al. Antibodies to MOG and AQP4 in adults with neuromyelitis optica and suspected limited forms of the disease. Mult Scler (2015) 21(7):866–74. 10.1177/1352458514555785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Chalmoukou K, Alexopoulos H, Akrivou S, Stathopoulos P, Reindl M, Dalakas MC. Anti-MOG antibodies are frequently associated with steroid-sensitive recurrent optic neuritis. Neurol Neuroimmunol Neuroinflamm (2015) 2(4):e131. 10.1212/NXI.0000000000000131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Ketelslegers IA, Van Pelt DE, Bryde S, Neuteboom RF, Catsman-Berrevoets CE, Hamann D, et al. Anti-MOG antibodies plead against MS diagnosis in an acquired demyelinating syndromes cohort. Mult Scler (2015) 21(12):1513–20. 10.1177/1352458514566666 [DOI] [PubMed] [Google Scholar]
- 148.Kim SM, Woodhall MR, Kim JS, Kim SJ, Park KS, Vincent A, et al. Antibodies to MOG in adults with inflammatory demyelinating disease of the CNS. Neurol Neuroimmunol Neuroinflamm (2015) 2(6):e163. 10.1212/NXI.0000000000000163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Di Pauli F, Hoftberger R, Reindl M, Beer R, Rhomberg P, Schanda K, et al. Fulminant demyelinating encephalomyelitis: insights from antibody studies and neuropathology. Neurol Neuroimmunol Neuroinflamm (2015) 2(6):e175. 10.1212/NXI.0000000000000175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Numa S, Kasai T, Kondo T, Kushimura Y, Kimura A, Takahashi H, et al. An adult case of anti-myelin oligodendrocyte glycoprotein (MOG) antibody-associated multiphasic acute disseminated encephalomyelitis at 33-year intervals. Intern Med (2016) 55(6):699–702. 10.2169/internalmedicine.55.5727 [DOI] [PubMed] [Google Scholar]
- 151.Adachi T, Yasui K, Takahashi T, Fujihara K, Watanabe Y, Nakashima K. Anti-myelin oligodendrocyte glycoprotein antibodies in a patient with recurrent optic neuritis involving the cerebral white matter and brainstem. Intern Med (2016) 55(10):1351–4. 10.2169/internalmedicine.55.6122 [DOI] [PubMed] [Google Scholar]
- 152.Fernandez-Carbonell C, Vargas-Lowy D, Musallam A, Healy B, McLaughlin K, Wucherpfennig KW, et al. Clinical and MRI phenotype of children with MOG antibodies. Mult Scler (2016) 22(2):174–84. 10.1177/1352458515587751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Piccolo L, Woodhall M, Tackley G, Jurynczyk M, Kong Y, Domingos J, et al. Isolated new onset ‘atypical’ optic neuritis in the NMO clinic: serum antibodies, prognoses and diagnoses at follow-up. J Neurol (2016) 263(2):370–9. 10.1007/s00415-015-7983-1 [DOI] [PubMed] [Google Scholar]
- 154.Baumann M, Hennes EM, Schanda K, Karenfort M, Kornek B, Seidl R, et al. Children with multiphasic disseminated encephalomyelitis and antibodies to the myelin oligodendrocyte glycoprotein (MOG): extending the spectrum of MOG antibody positive diseases. Mult Scler (2016) 22(14):1821–9. 10.1177/1352458516631038 [DOI] [PubMed] [Google Scholar]
- 155.Kakalacheva K, Regenass S, Wiesmayr S, Azzi T, Berger C, Dale RC, et al. Infectious mononucleosis triggers generation of IgG auto-antibodies against native myelin oligodendrocyte glycoprotein. Viruses (2016) 8(2):E51. 10.3390/v8020051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Yan Y, Li Y, Fu Y, Yang L, Su L, Shi K, et al. Autoantibody to MOG suggests two distinct clinical subtypes of NMOSD. Sci China Life Sci (2016) 59(12):1270–81. 10.1007/s11427-015-4997-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Cobo-Calvo A, Sepulveda M, Bernard-Valnet R, Ruiz A, Brassat D, Martinez-Yelamos S, et al. Antibodies to myelin oligodendrocyte glycoprotein in aquaporin 4 antibody seronegative longitudinally extensive transverse myelitis: clinical and prognostic implications. Mult Scler (2016) 22(3):312–9. 10.1177/1352458515591071 [DOI] [PubMed] [Google Scholar]
- 158.van Pelt ED, Wong YY, Ketelslegers IA, Hamann D, Hintzen RQ. Neuromyelitis optica spectrum disorders: comparison of clinical and magnetic resonance imaging characteristics of AQP4-IgG versus MOG-IgG seropositive cases in the Netherlands. Eur J Neurol (2016) 23(3):580–7. 10.1111/ene.12898 [DOI] [PubMed] [Google Scholar]
- 159.Ramanathan S, Prelog K, Barnes EH, Tantsis EM, Reddel SW, Henderson AP, et al. Radiological differentiation of optic neuritis with myelin oligodendrocyte glycoprotein antibodies, aquaporin-4 antibodies, and multiple sclerosis. Mult Scler (2016) 22(4):470–82. 10.1177/1352458515593406 [DOI] [PubMed] [Google Scholar]
- 160.Akaishi T, Sato DK, Nakashima I, Takeshita T, Takahashi T, Doi H, et al. MRI and retinal abnormalities in isolated optic neuritis with myelin oligodendrocyte glycoprotein and aquaporin-4 antibodies: a comparative study. J Neurol Neurosurg Psychiatry (2016) 87(4):446–8. 10.1136/jnnp-2014-310206 [DOI] [PubMed] [Google Scholar]
- 161.Sepulveda M, Armangue T, Sola-Valls N, Arrambide G, Meca-Lallana JE, Oreja-Guevara C, et al. Neuromyelitis optica spectrum disorders: comparison according to the phenotype and serostatus. Neurol Neuroimmunol Neuroinflamm (2016) 3(3):e225. 10.1212/NXI.0000000000000225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Akaishi T, Nakashima I, Takeshita T, Mugikura S, Sato DK, Takahashi T, et al. Lesion length of optic neuritis impacts visual prognosis in neuromyelitis optica. J Neuroimmunol (2016) 293:28–33. 10.1016/j.jneuroim.2016.02.004 [DOI] [PubMed] [Google Scholar]
- 163.Polat I, Yis U, Karaoglu P, Ayanoglu M, Ozturk T, Guleryuz H, et al. Myelin oligodendrocyte glycoprotein antibody persistency in a steroid-dependent ADEM case. Pediatrics (2016) 137(5):e20151958. 10.1542/peds.2015-1958 [DOI] [PubMed] [Google Scholar]
- 164.Siritho S, Sato DK, Kaneko K, Fujihara K, Prayoonwiwat N. The clinical spectrum associated with myelin oligodendrocyte glycoprotein antibodies (anti-MOG-Ab) in Thai patients. Mult Scler (2016) 22(7):964–8. 10.1177/1352458515614093 [DOI] [PubMed] [Google Scholar]
- 165.Spadaro M, Gerdes LA, Krumbholz M, Ertl-Wagner B, Thaler FS, Schuh E, et al. Autoantibodies to MOG in a distinct subgroup of adult multiple sclerosis. Neurol Neuroimmunol Neuroinflamm (2016) 3(5):e257. 10.1212/NXI.0000000000000257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Sepulveda M, Armangue T, Martinez-Hernandez E, Arrambide G, Sola-Valls N, Sabater L, et al. Clinical spectrum associated with MOG autoimmunity in adults: significance of sharing rodent MOG epitopes. J Neurol (2016) 263(7):1349–60. 10.1007/s00415-016-8147-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Wang JJ, Jaunmuktane Z, Mummery C, Brandner S, Leary S, Trip SA. Inflammatory demyelination without astrocyte loss in MOG antibody-positive NMOSD. Neurology (2016) 87(2):229–31. 10.1212/WNL.0000000000002844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Thulasirajah S, Pohl D, Davila-Acosta J, Venkateswaran S. Myelin oligodendrocyte glycoprotein-associated pediatric central nervous system demyelination: clinical course, neuroimaging findings, and response to therapy. Neuropediatrics (2016) 47(4):245–52. 10.1055/s-0036-1583184 [DOI] [PubMed] [Google Scholar]
- 169.Lechner C, Baumann M, Hennes EM, Schanda K, Marquard K, Karenfort M, et al. Antibodies to MOG and AQP4 in children with neuromyelitis optica and limited forms of the disease. J Neurol Neurosurg Psychiatry (2016) 87:897–905. 10.1136/jnnp-2015-311743 [DOI] [PubMed] [Google Scholar]
- 170.Hacohen Y, Nishimoto Y, Fukami Y, Lang B, Waters P, Lim MJ, et al. Paediatric brainstem encephalitis associated with glial and neuronal autoantibodies. Dev Med Child Neurol (2016) 58(8):836–41. 10.1111/dmcn.13090 [DOI] [PubMed] [Google Scholar]
- 171.Azumagawa K, Nomura S, Shigeri Y, Jones LS, Sato DK, Nakashima I, et al. Post-vaccination MDEM associated with MOG antibody in a subclinical Chlamydia infected boy. Brain Dev (2016) 38(7):690–3. 10.1016/j.braindev.2016.02.004 [DOI] [PubMed] [Google Scholar]
- 172.Jarius S, Metz I, Konig FB, Ruprecht K, Reindl M, Paul F, et al. Screening for MOG-IgG and 27 other anti-glial and anti-neuronal autoantibodies in ‘pattern II multiple sclerosis’ and brain biopsy findings in a MOG-IgG-positive case. Mult Scler (2016) 22(12):1541–9. 10.1177/1352458515622986 [DOI] [PubMed] [Google Scholar]
- 173.Kaneko K, Sato DK, Nakashima I, Nishiyama S, Tanaka S, Marignier R, et al. Myelin injury without astrocytopathy in neuroinflammatory disorders with MOG antibodies. J Neurol Neurosurg Psychiatry (2016) 87(11):1257–9. 10.1136/jnnp-2015-312676 [DOI] [PubMed] [Google Scholar]
- 174.Jarius S, Ruprecht K, Kleiter I, Borisow N, Asgari N, Pitarokoili K, et al. MOG-IgG in NMO and related disorders: a multicenter study of 50 patients. Part 1: frequency, syndrome specificity, influence of disease activity, long-term course, association with AQP4-IgG, and origin. J Neuroinflammation (2016) 13(1):279. 10.1186/s12974-016-0719-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Jarius S, Ruprecht K, Kleiter I, Borisow N, Asgari N, Pitarokoili K, et al. MOG-IgG in NMO and related disorders: a multicenter study of 50 patients. Part 2: epidemiology, clinical presentation, radiological and laboratory features, treatment responses, and long-term outcome. J Neuroinflammation (2016) 13(1):280. 10.1186/s12974-016-0718-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Jarius S, Kleiter I, Ruprecht K, Asgari N, Pitarokoili K, Borisow N, et al. MOG-IgG in NMO and related disorders: a multicenter study of 50 patients. Part 3: brainstem involvement – frequency, presentation and outcome. J Neuroinflammation (2016) 13(1):281. 10.1186/s12974-016-0717-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Lennon VA, Wingerchuk DM, Kryzer TJ, Pittock SJ, Lucchinetti CF, Fujihara K, et al. A serum autoantibody marker of neuromyelitis optica: distinction from multiple sclerosis. Lancet (2004) 364(9451):2106–12. 10.1016/S0140-6736(04)17551-X [DOI] [PubMed] [Google Scholar]
- 178.Konig FB, Wildemann B, Nessler S, Zhou D, Hemmer B, Metz I, et al. Persistence of immunopathological and radiological traits in multiple sclerosis. Arch Neurol (2008) 65(11):1527–32. 10.1001/archneur.65.11.1527 [DOI] [PubMed] [Google Scholar]
- 179.Körtvélyessy P, Breu M, Pawlitzki M, Metz I, Heinze H-J, Matzke M, et al. ADEM-like presentation, anti-MOG antibodies, and MS pathology: TWO case reports. Neurol Neuroimmunol Neuroinflamm (2017) 4(3):e335. 10.1212/NXI.0000000000000335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Misu T, Hoftberger R, Fujihara K, Wimmer I, Takai Y, Nishiyama S, et al. Presence of six different lesion types suggests diverse mechanisms of tissue injury in neuromyelitis optica. Acta Neuropathol (2013) 125(6):815–27. 10.1007/s00401-013-1116-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Oliver AR, Lyon GM, Ruddle NH. Rat and human myelin oligodendrocyte glycoproteins induce experimental autoimmune encephalomyelitis by different mechanisms in C57BL/6 mice. J Immunol (2003) 171(1):462–8. 10.4049/jimmunol.171.9.4934 [DOI] [PubMed] [Google Scholar]
- 182.Burrer R, Buchmeier MJ, Wolfe T, Ting JP, Feuer R, Iglesias A, et al. Exacerbated pathology of viral encephalitis in mice with central nervous system-specific autoantibodies. Am J Pathol (2007) 170(2):557–66. 10.2353/ajpath.2007.060893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Young NP, Weinshenker BG, Parisi JE, Scheithauer B, Giannini C, Roemer SF, et al. Perivenous demyelination: association with clinically defined acute disseminated encephalomyelitis and comparison with pathologically confirmed multiple sclerosis. Brain (2010) 133(Pt 2):333–48. 10.1093/brain/awp321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Reindl M, Di Pauli F, Rostasy K, Berger T. The spectrum of MOG autoantibody-associated demyelinating diseases. Nat Rev Neurol (2013) 9(8):455–61. 10.1038/nrneurol.2013.118 [DOI] [PubMed] [Google Scholar]
- 185.Palmer JP, Asplin CM, Clemons P, Lyen K, Tatpati O, Raghu PK, et al. Insulin antibodies in insulin-dependent diabetics before insulin treatment. Science (1983) 222(4630):1337–9. 10.1126/science.6362005 [DOI] [PubMed] [Google Scholar]
- 186.Baekkeskov S, Aanstoot HJ, Christgau S, Reetz A, Solimena M, Cascalho M, et al. Identification of the 64K autoantigen in insulin-dependent diabetes as the GABA-synthesizing enzyme glutamic acid decarboxylase. Nature (1990) 347(6289):151–6. 10.1038/347151a0 [DOI] [PubMed] [Google Scholar]
- 187.Rabin DU, Pleasic SM, Shapiro JA, Yoo-Warren H, Oles J, Hicks JM, et al. Islet cell antigen 512 is a diabetes-specific islet autoantigen related to protein tyrosine phosphatases. J Immunol (1994) 152(6):3183–8. [PubMed] [Google Scholar]
- 188.Wenzlau JM, Juhl K, Yu L, Moua O, Sarkar SA, Gottlieb P, et al. The cation efflux transporter ZnT8 (Slc30A8) is a major autoantigen in human type 1 diabetes. Proc Natl Acad Sci U S A (2007) 104(43):17040–5. 10.1073/pnas.0705894104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Bonifacio E. Predicting type 1 diabetes using biomarkers. Diabetes Care (2015) 38(6):989–96. 10.2337/dc15-0101 [DOI] [PubMed] [Google Scholar]
- 190.Pihoker C, Gilliam LK, Hampe CS, Lernmark A. Autoantibodies in diabetes. Diabetes (2005) 54(Suppl 2):S52–61. 10.2337/diabetes.54.suppl_2.S52 [DOI] [PubMed] [Google Scholar]