Abstract
Mutations of calreticulin (CALR) are detected in 25–30% of patients with essential thrombocythemia (ET) or primary myelofibrosis and cause frameshifts that result in proteins with a novel C-terminal. We demonstrate that CALR mutations activated signal transducer and activator of transcription 5 (STAT5) in 293T cells in the presence of thrombopoietin receptor (MPL). Human megakaryocytic CMK11-5 cells and erythroleukemic F-36P-MPL cells with knocked-in CALR mutations showed increased growth and acquisition of cytokine-independent growth, respectively, accompanied by STAT5 phosphorylation. Transgenic mice expressing a human CALR mutation with a 52 bp deletion (CALRdel52-transgenic mice (TG)) developed ET, with an increase in platelet count, but not hemoglobin level or white blood cell count, in association with an increase in bone marrow (BM) mature megakaryocytes. CALRdel52 BM cells did not drive away wild-type (WT) BM cells in in vivo competitive serial transplantation assays, suggesting that the self-renewal capacity of CALRdel52 hematopoietic stem cells (HSCs) was comparable to that of WT HSCs. Therapy with the Janus kinase (JAK) inhibitor ruxolitinib ameliorated the thrombocytosis in TG mice and attenuated the increase in number of BM megakaryocytes and HSCs. Taken together, our study provides a model showing that the C-terminal of mutant CALR activated JAK-STAT signaling specifically downstream of MPL and may have a central role in CALR-induced myeloproliferative neoplasms.
Introduction
There are three main diseases categorized as classical myeloproliferative neoplasms (MPNs), namely polycythemia vera, essential thrombocythemia (ET) and primary myelofibrosis (PMF). All are characterized by the autonomous growth of one or more lineages of hematopoietic cells.1 The discovery of the Janus kinase 2 (JAK2) valine 617 phenylalanine (V617F) mutation in MPNs shed light on the central mechanism of MPN development, now recognized as the autonomous activation of JAK-signal transducer and activator of transcription (STAT) signaling cascades.2, 3, 4, 5, 6 Consistent with this mechanism, mutations in JAK2 exon 12 and MPL were discovered in MPN patients, and these three kinds of mutations are thought to be the driver mutations in MPN.7, 8, 9 The JAK2 mutation has been observed in >95% of polycythemia vera patients and about half of ET and PMF patients have either JAK2 or MPL mutations. In 2013, calreticulin (CALR) mutations were reported in about two-thirds of JAK2-negative ET and PMF patients.10, 11 CALR mutations with a 52 bp deletion or a 5 bp insertion in exon 9, namely type 1 and type 2 mutations, respectively, occur in >80% of patients with CALR mutations and cause frameshifts that result in proteins with novel C-terminal domains.10 As CALR mutations have been exclusively observed with JAK2 or MPL mutations in MPN patients, the former are speculated to have a driver role in MPNs and recent studies have clarified a vital role for MPL and STAT5 activation in CALR mutation-induced MPN.12, 13, 14
In addition to providing insight regarding the ontogeny of MPN, the discovery of CALR mutations could divide ET or PMF patients into two phenotypic categories, one with JAK2 mutations and the other with CALR mutations. Compared with ET or PMF patients with JAK2 mutations, those with CALR mutations were shown to have lower hemoglobin (Hb) levels and lower numbers of granulocytes, but higher numbers of platelets.15, 16, 17, 18 The CALR mutation patients also had a lower incidence of thrombosis during their clinical course.
In this study, we generated human cell lines with knocked-in CALR mutations and transgenic mice expressing a human CALR type-1 mutant with a 52 bp deletion (CALRdel52-transgenic mice (TG)).
Materials and methods
Expression vector constructs, cell lines and cytokines, and other experimental details are described in the Supplementary Methods.
Luciferase assay
We transfected CALR wild type (WT), CALRdel52 mutant or CALRins5 mutant and either hCSF3R, hEPOR or hMPL, together with STAT3-LUC or STAT5-LUC vector, into 293T cells by calcium phosphate precipitation.19 Promoter activity was measured as luciferase activity 48 h after transfection. Luciferase activity was assayed using a Lumat LB9507 luminometer (Berthold, Wildbad, Germany). The results of the reporter assays represent average values for relative luciferase activity generated in three independent experiments.
CRISPR/Cas9 gene editing and cell proliferation assays
Plasmids coexpressing hCas9 and single-guide RNA were prepared by ligating oligonucleotides (5′-CACCGACAAGAAACGCAAAGAGGAGG-3′ and 5′-AAACCCTCCTCTTTGCGTTTCTTGTC-3′) for the target sequence of human CALR exon 9 (Supplementary Figure S1) into the BbsI site of pX330 (http://www.addgene.org/42230/). Ten micrograms of pX330 with the single-guide RNA sequence was introduced with a NEPA21 electroporator (Nepa Gene, Chiba, Japan) into 1 × 106 CMK11-5 cells and 1 × 106 F-36P-MPL cells. After limiting dilution cloning, CALR mutations were assessed (Supplementary Methods).
For the proliferation assay, cells were washed in phosphate-buffered saline and cultured at a density of 3 × 104 cells/ml with or without 10 ng/ml Granulocyte/macrophage-colony stimulating factor (GM-CSF). The cell number after Trypan blue dye staining was recorded on the indicated days. Cell growth activity was measured with the WST-8 assay kit (DOJIN, Kumamoto, Japan). After washing, cells were seeded on 96-well plates (3 × 103 cells/well) and then incubated in media containing the indicated concentration of thrombopoietin (TPO) for 72 h. STAT5 phosphorylation was assessed by the techniques in the Supplementary Methods.
Generation and analysis of transgenic mice
The pSP65-H2K-i-LTR vector20 was kindly provided by Dr Weissman (Stanford University School of Medicine, Stanford, CA, USA). We engineered the H2K-CALR transgenic construct by introducing the human CALRdel52 mutant cDNA into the NotI-subcloning site of the pSP65-H2K-i-LTR vector. The construct was isolated from vector sequences as an ApaLI/ApaLI fragment and purified. Transgenic mice were produced by standard oocyte injection using BDF1 mouse-derived fertilized eggs.21 All procedures were approved by the Local University of Miyazaki Ethics Committee.
The expression of human CALR mRNA was examined by real-time PCR. The expression of human and murine CALR protein was examined by western blotting (Supplementary Methods). To analyze the effect of ruxolitinib treatment, 24-week-old CALRdel52-TG mice were treated by oral gavage twice daily with 90 mg/kg ruxolitinib or vehicle for 4 weeks. Mice were randomized into groups with similar average platelet count. As a control for CALRdel52-TG treated with vehicle, we prepared WT mice treated with vehicle. As an another experiment we investigated the effect of ruxolitinib treatment to WT mice. Differential blood counts were assessed by retroorbital eye bleeds. Mice were killed and analyzed at the study end point. The investigators were blinded to the group allocation during histological examination.
Transplantation assays
We intravenously transplanted 5 × 106 bone marrow (BM) cells (B6-CD45.2) from either CALRdel52-TG or WT mice together with 2 × 105 WT BM cells (B6-CD45.1) into lethally irradiated (9.0 Gy), 8-week-old B6-CD45.1 mice. Transplanted recipients were sequentially analyzed in terms of complete blood cell counts and cell surface markers. In competitive serial transplantation assays, we mixed 1 × 106 of each of the BM cell types (B6-CD45.2) with 1 × 106 of WT BM cells (B6-CD45.1) and transplanted them into B6-CD45.1 mice. At 12 weeks after the first transplantations, second transplantations were carried out by transferring 1 × 106 BM cells from the first recipients.
Progenitor cell assays
Progenitor cells in BM and spleen cells were determined by fluorescence-activated cell sorter analysis (Supplementary Methods). Colony-replating assays were performed as described previously22 and 50000 BM cells were plated in methylcellulose (M3434 StemCell Technologies Inc., Vancouver, BC, Canada). After culture for 1 week, colonies were counted and single-cell suspensions of colonies (5 × 104 cells) were replated. Every 1 week, replating was repeated in the same way.
Statistical analysis
Results are presented as means±s.e.m. To assess the statistical significance between the two groups, the two-tailed Student's t-test was used. To assess statistical significance among groups, Tukey's multiple comparison test with one-way analysis of variance was used. For the comparison of the hematological values between CALRdel52-TG and WT mice, analysis of variance with repeated measures was used. The paired data between pre-treatment and post-treatment were analyzed with a paired two-tailed t-test. Statistical analysis of the survival were performed with the log-rank test.
Results
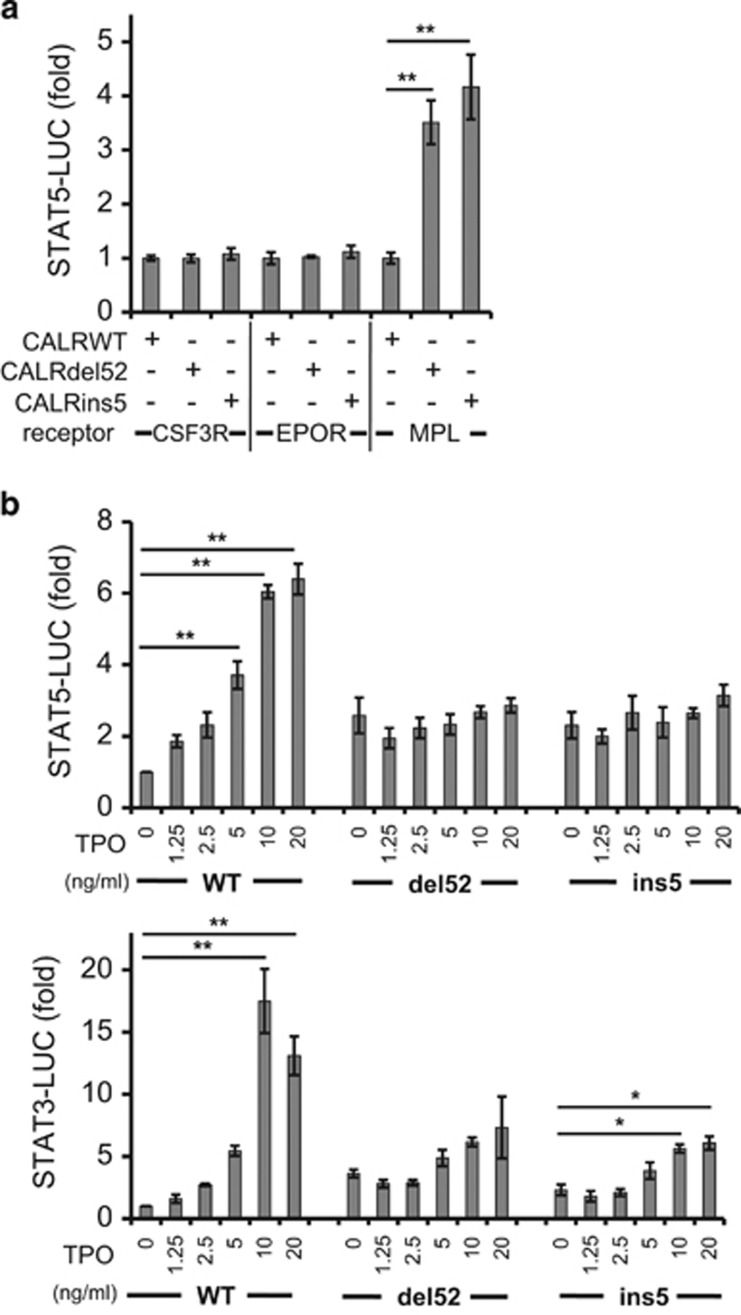
CALR mutants augmented the transcriptional activity of STAT5 in the presence of MPL, but not of CSF3R or EPOR
Compared with JAK2V617F-positive ET or PMF patients, CALR mutation-positive ET or PMF patients had lower Hb levels and reduced numbers of granulocytes in peripheral blood, and had higher numbers of platelets.15, 16, 17, 18 JAK2 activation by erythropoietin (EPO), granulocyte-colony stimulating factor or TPO stimulation-induced erythropoiesis, granulopoiesis and thrombopoiesis, respectively,23 and thus constitutive JAK2 activation by JAK2V617F, induces pancytosis in MPN patients. We hypothesized that CALR mutations would specifically activate MPL downstream signaling cascades, but would have no influence on CSF3R or EPOR downstream signaling cascades. To verify this, we transiently transfected 293T cells with two kinds of vectors and measured the luciferase activity; the first vector was either the CALRdel52 mutant or CALRins5 mutant, and the second was either CSF3R, EPOR or MPL, together with STAT5-LUC (Figure 1a). Only in the presence of MPL, both types of CALR mutants augmented STAT5 transcriptional activity and neither CSF3R nor EPOR influenced STAT5 activation in collaboration with the CALR mutants. The situation was the same for STAT3 activation and only the presence of MPL, but not CSF3R or EPOR, augmented STAT3 transcriptional activity.
Figure 1.
CALR mutants specifically activate MPL and lead to cell growth augmentation. (a) 293T cells were transiently transfected with STAT5-LUC and CALR WT, CALRdel52 mutant or CALRins5 mutant in the presence of granulocyte-colony stimulating factor (G-CSF) receptor (CSF3R), erythropoietin receptor (EPOR) or thrombopoietin receptor (MPL). The vertical axis number is the fold induction when compared with that of WT CALR. Only in the presence of MPL, both type of CALR mutants augmented STAT5 activity. *P<0.05 and **P<0.01 vs CALR WT. (b) STAT5 (upper panel) and STAT3 (lower panel) transcriptional activity was assessed by the luciferase assay in 293T cells transiently expressing CALR WT, CALRdel52 mutant or CALRins5 mutant, together with MPL and either STAT5-LUC or STAT3-LUC. Twenty-four hours after transfection, cells were stimulated with several concentrations (0, 1.25, 2.5, 5, 10 and 20 ng/ml) of TPO. STAT5 and STAT3 transcriptional activity is enhanced by TPO stimulation in 293T cells in the presence of WT CALR. In contrast, TPO stimulation shows little effect on STAT5 transcriptional activity in the presence of CALRdel52 or CALRins5. *P<0.05 and **P<0.01 vs cells without TPO stimulation. The average values for relative luciferase activity generated in three independent experiment is shown. Data are presented as means±s.e.m. Tukey's multiple comparison test with one-way analysis of variance was used.
TPO stimulation activated the JAK-STAT signaling cascade. We then examined whether CALR mutation conferred TPO hypersensitivity to MPL-expressing cells. In the presence of WT CALR, STAT5 and STAT3, transcriptional activity was enhanced by TPO stimulation in 293T cells transiently expressing MPL. In contrast, TPO stimulation had little effect on STAT5 transcriptional activity in the presence of CALRdel52 or CALRins5, although the baseline STAT5 transcriptional activity without TPO stimulation in the presence of CALRdel52 or CALRins5 was much greater than that in the presence of WT CALR (P=0.033 for CALRdel52, P=0.022 for CALRins5). As for the STAT3 transcriptional activity, TPO stimulation enhanced it in the presence of CALRins5, but to a much lesser degree than in the presence of WT CALR (Figure 1b).
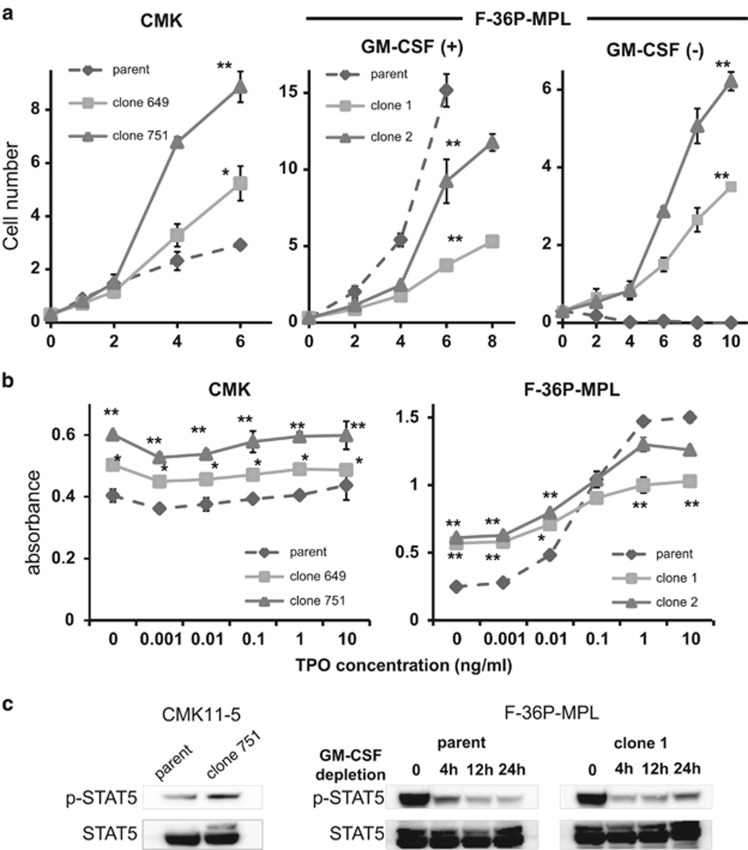
CALR mutation knock-in cells increased cell growth or acquired cytokine-independent growth
As CALR mutants augmented STAT5 activity in the presence of MPL in 293T cells, we next evaluated the influence of CALR mutation on cell growth. For this experiment, we used two human cell lines: the megakaryocytic leukemia-derived cell line CMK11-5, which expresses endogenous MPL on the cell surface,24 and F-36P-MPL, which was generated by exogenous stable expression of MPL in the human erythroid leukemic cell line F-36P.25 In both cell lines we knocked in a CALR mutation with the CRISPR-Cas9 system and obtained several clones with CALR mutations that generated the common novel C-terminus peptide observed in CALR-mutated MPN patients (Supplementary Figure S1 and Supplementary Results). Both CMK11-5 clone 751 with CALRdel4/del17 and clone 649 with CALRdel25 showed increased cell proliferation compared with parent CMK11-5 cells (Figure 2a). The growth of F-36P-MPL was dependent on GM-CSF and neither F-36P-MPL clone 1 with CALRdel1/ins1 nor clone 2 with CALRdel1/ins1 showed a growth advantage compared with parent F-36P-MPL in the presence of GM-CSF. After GM-CSF depletion, parent F-36P-MPL cells did not grow; however, both F-36P-MPL clones 1 and 2 acquired cytokine-independent growth. We next examined whether these clones with CALR mutations were hypersensitive to TPO. Neither mutant nor parent CMK11-5 cells responded to TPO (Figure 2b). Both mutant and parent F-36P-MPL cells showed TPO concentration-dependent growth; however, we observed no TPO hypersensitivity in F-36P-MPL clones 1 or 2.
Figure 2.
The effect of CALR mutations on the growth and the response to TPO in human cell line cells expressing MPL. (a) CALR mutation was introduced with the CRISPR-Cas9 system into CMK11-5 cells and F-36P-MPL cells. CMK11-5 clone 751 with CALRdel4/del17, CMK11-5 clone 649 with CALRdel25 and parent CMK11-5 cells (left), as well as F-36P-MPL clone 1 with CALRdel1/ins1, F-36P-MPL clone 2 with CALRdel1/ins1 and parent F-36P-MPL cells (middle, left), were grown in the absence (left and right) or the presence (middle) of GM-CSF. Cell numbers (average of triplicate±s.e.m.) were counted on the indicated days. Both CMK11-5 clones 751 and 649 show increased cell proliferation compared with parent CMK11-5 cells. The growth of F-36P-MPL clones 1 and 2 is less than that of parent F-36P-MPL cells in the presence of 10 ng/ml GM-CSF; however, F-36P-MPL clones 1 and 2 show growth in the absence of GM-CSF. (b) WST-8 assay at various TPO concentrations. CMK11-5 clones 751 and 649, and parent CMK11-5 cells show no response to TPO. In contrast, F-36P-MPL clones 1 and 2, and parent F-36P-MPL demonstrate a response to TPO, and F-36P-MPL clones 1 and 2 show no hypersensitivity to TPO. One representative experiment is shown. Data are presented as means±s.e.m. Tukey's multiple comparison test with one-way analysis of variance was used. *P<0.05 and **P<0.01vs parent cells. (c) STAT5 phosphorylation. CMK 11-5 clone 751 shows augmented STAT5 phosphorylation compared with parent CMK11-5 cells (left). F-36P-MPL is a cytokine-dependent cell line and STAT5 is phosphorylated in the presence of GM-CSF. Its phosphorylation disappears after withdrawal of GM-CSF (middle). The phosphorylation of STAT5, which transiently decreased after withdrawal of GM-CSF, was re-observed 24 h after GM-CSF depletion in F-36P-MPL clone 1 (right).
CMK 11-5 clone 751 demonstrated augmented STAT5 phosphorylation compared with parent CMK11-5 cells. The growth of parent F-36P-MPL was cytokine dependent and STAT5 was phosphorylated in the presence of GM-CSF, but this phosphorylation disappeared after withdrawal of GM-CSF. In contrast, the phosphorylation of STAT5, which transiently decreased after GM-CSF depletion, reoccurred in F-36P-MPL clone 1 at 24 h after GM-CSF depletion (Figure 2c). These observations suggested that the acquisition of cytokine independence in F-36P-MPL clone 1 was due to activation of the JAK-STAT signaling cascade induced by CALR mutations.
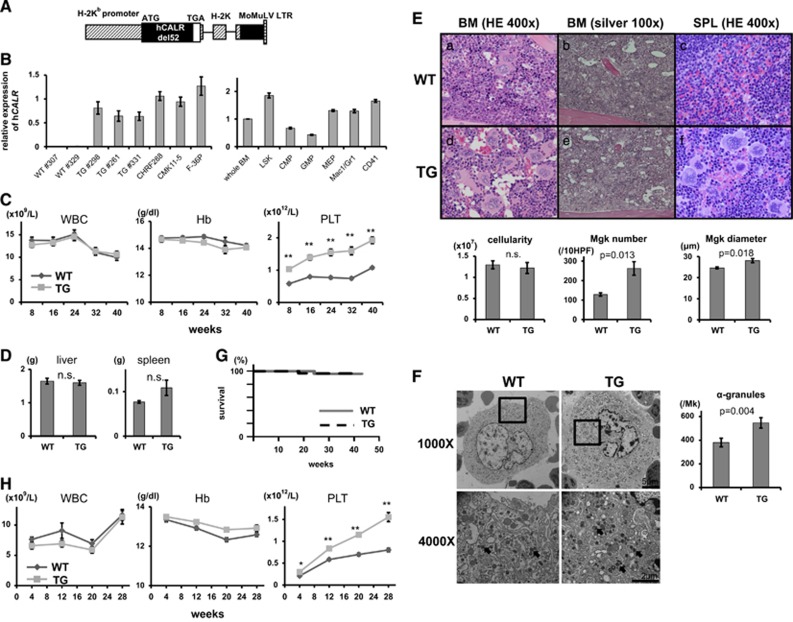
CALR mutant mice developed ET
We next evaluated the role of CALR mutations in vivo. Human CALRdel52 mutant was expressed under the murine H-2Kb promoter and generated CALRdel52-TG mice (Figure 3A). Two copies of transgenes were integrated in opposite directions in intron 5 of Tmigd3 on chromosome 3 (Supplementary Figure S2). Real-time PCR analysis showed that the level of expression of human CALRdel52 mRNA in BM cells from CALRdel52-TG was 0.64-fold smaller than the average of three human cell lines. Most CALR-mutated MPN patients have CALR mutations in one allele and the expression of mutant CALR in BM cells from CALRdel52-TG was ~1.3-fold of that in cells from MPN patients. Compared with the level of CALRdel52 expression in whole BM cells, that in LSK (Lin−Sca-1+c-Kit+), erythromegakaryocyte progenitors and CD41+ BM cells was higher, whereas that in common myeloid progenitors, granulocyte–macrophage progenitors and Mac1/Gr1+ BM cells was lower (Figure 3B).
Figure 3.
CALR mutant mice develop ET. (A) A transgenic construct was generated by introducing human CALRdel52 mutant cDNA into the pSP65-H2K-i-LTR vector. (B) The level of expression of human CALRdel52 mRNA in different lineage cells. Left: the average expression level of CALR mRNA in two human megakaryocytic leukemia cell lines (CHRF288 and CMK11-5) is set at 1. The level of expression of human CALRdel52 mRNA in BM cells from CALRdel52-TG is 0.64-fold smaller than the average expression of CALR mRNA in three human megakaryocytic cell lines. Right: the expression level of CALRdel52 in whole BM cells is set at 1. Compared with the expression of CALRdel52 in BM cells, that in LSKs, erythromegakaryocyte progenitors (MEP) and CD41+ BM cells is higher, whereas that in common myeloid progenitor (CMP), granulocyte–macrophage progenitor (GMP) and Mac1/Gra1+ BM cells is lower. (C) The average complete blood cell count in CALRdel52-TG mice every 8 weeks after birth (n=30). Compared with WT mice (n=29), TG mice show thrombocytosis at 8 weeks and later. There is no difference in WBC count or Hb level between WT and TG mice. **P<0.01 vs WT mice. (D) Liver and spleen weights from 9- to 13-week-old mice. CALRdel52-TG mice (n=10) do not show hepatosplenomegaly compared with WT mice (n=9). (E) Histological analysis of 24-week-old CALRdel52-TG mice. BM and spleen stained with hematoxylin and eosin (HE) (a, c, d and f); BM with Gomori silver stain (b and e). CALRdel52-TG mice show increased numbers of megakaryocytes in BM and spleen (d and f). There is no fibrosis in BM (e). Lower left panel: the nucleated cells in one femur and one tibia from TG (n=10) or WT mice (n=9) were counted. There is no difference in cellularity between the two groups. Lower center panel: the number of megakaryocytes per 10 HPF in BM was higher in TG (n=5) than in WT mice (n=5). Lower right panel: sizes of megakaryocytes in BM. In each mouse, the diameters of 100 megakaryocytes were measured. Megakaryocytes in TG mice (n=5) are significantly larger than those in WT mice (n=5). P-values are shown. (F) Left panel: electron microscopic appearance of mature megakaryocytes found in WT and TG BM (magnification × 1000 in upper, × 4000 in lower). α-Granules and nuclear lobes are well developed in megakaryocytes in TG. Right panel: the numbers of α-granules were counted in 50 randomly selected megakaryocytes from each of three WT mice and three TG mice. P-values are shown. (G) Kaplan–Meier plot of WT and TG mice. (H) 5 × 106 BM cells from either TG or WT mice together with 2 × 105 WT BM cells were transplanted into irradiated WT mice. Recipient mice transplanted with TG BM cells (n=12) exhibit thrombocytosis, but like recipients transplanted with WT BM cells they do not show erythrocytosis or leukocytosis (n=12). *P<0.05 and **P<0.01 vs WT mice. All data are presented as means±s.e.m. To assess the statistical significance between the two groups, the two-tailed Student's t-test was used (D–F). For the comparison of the hematological values between CALRdel52-TG and WT mice, analysis of variance with repeated measures was used (C and H). Statistical analyses of the survival were performed with the log-rank test (G).
CALRdel52-TG exhibited thrombocytosis, with platelet counts as high as 2 × 1012/l. Leukocyte number and differentiation, and the proportion of granulocytes and T and B lymphocytes, were comparable between WT and CALRdel52-TG mice (Supplementary Figure S3). CALR mutation had no impact on Hb level, liver weight or spleen weight (Figures 3C and D). CALRdel52-TG and WT mice exhibited similar cellularity in hematoxylin and eosin-stained BM samples, as well as a comparable number of nucleated cells in one femur and one tibia, which represents the cellularity of BM (Figure 3E). There was a striking difference in the number of megakaryocytes, which was twofold higher in the BM from CALRdel52-TG mice than in WT mice. The CALRdel52-TG megakaryocytes were also more mature, with larger diameter, and contained a much higher number of α-granules compared with WT cells (Figure 3F). These observations showed that CALRdel52-TG developed human ET-like disease. CALRdel52-TG did not develop myelofibrosis (MF) during 12 months of observation after birth (Supplementary Figure S2D). The survival of CALRdel52-TG mice was comparable to that of WT mice (Figure 3G). Next, we transplanted 5 × 106 BM cells from either CALRdel52-TG or WT mice (B6-CD45.2), together with 2 × 105 WT BM cells (B6-CD45.1) into lethally irradiated B6-CD45.1 mice. Mice transplanted with TG BM cells exhibited thrombocytosis but did not show erythrocytosis or leukocytosis (Figure 3H).
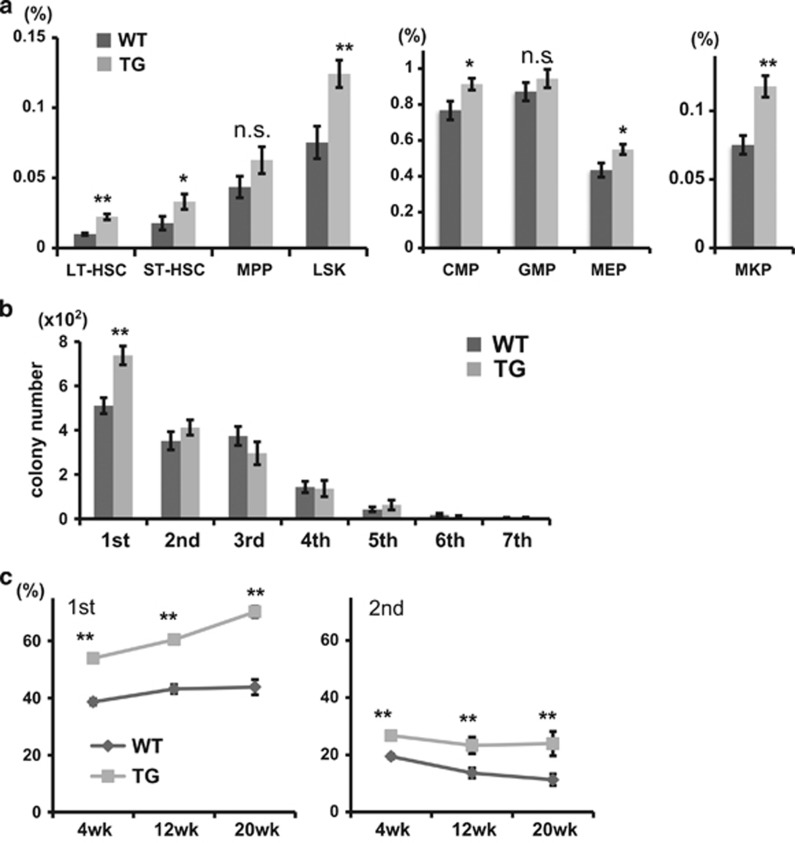
To characterize in detail the impact of MPNs induced by the CALRdel52 mutant, we evaluated the frequencies of hematopoietic stem cells (HSCs) and progenitors in the BM (Figure 4a). The frequency of both long-term HSCs and short-term HSCs in the BM was higher in CALRdel52-TG mice compared with that in WT mice. The frequencies of progenitors (common myeloid progenitor, erythromegakaryocyte progenitor and megakaryocyte progenitors) were also greater in the BM from CALRdel52-TG mice than from WT mice. To identify the qualitative differences among HSCs with the CALRdel52 mutation, we performed colony-replating assays of BM cells from CALRdel52-TG mice and WT mice. The number of primary colonies generated from TG BM cells was greater than those from WT BM cells, but there was no difference in secondary or successive colonies. TG BM cells did not have sequential colony-replating capacity (Figure 4b).
Figure 4.
The influence of CALR mutation on hematopoietic stem/progenitor cells. (a) The proportion of HSCs and progenitors. Compared with WT mice (n=9), CALRdel52-TG mice (n=10) show increased frequencies of long-term (LT)-HSC, short-term (ST)-HSC, LSK, common myeloid progenitor (CMP), erythromegakaryocyte progenitors (MEP) and megakaryocyte progenitor (MKP). *P<0.05 and **P<0.01 vs WT mice. (b) Enumeration of colonies and serial replating capacity of 5 × 104 BM cells from WT (n=9) or TG (n=10) mice. Compared with the BM cells from WT mice, those from TG mice generated larger numbers of colonies in vitro. TG BM cells did not have enhanced sequential colony-replating capacity. **P<0.01 vs WT mice. (c) Serial transplantation assays. WT or CALRdel52 BM cells (B6-CD45.2) together with competitor WT BM cells (B6-CD45.1) were transplanted in a 1:1 ratio into lethally irradiated recipients (B6-CD45.1) and then recipient 1 × 106 BM cells were transplanted into a second set of lethally irradiated recipients (B6-CD45.1). The chimerism of donor-derived CD45.2+ cells in peripheral blood after the first and the second transplantations at the indicated time points is shown. **P<0.01 vs WT cells. All data are presented as means±s.e.m. The two-tailed Student's t-test was used (a and b). For the comparison of the chimerism, analysis of variance with repeated measures was used (c).
We next examined whether CALRdel52 conferred any clonal advantage. We transplanted WT or CALRdel52 BM cells (B6-CD45.2) together with competitor WT BM cells (B6-CD45.1) in a 1:1 ratio into lethally irradiated recipients (B6-CD45.1) and then continued serial transplantations (Figure 4c). The transplanted CALRdel52 cells exhibited higher peripheral blood chimerism in the first and second recipients. However, the proportion of CALRdel52 and WT cells in the secondary recipient mice was constant and CALRdel52 cells did not drive WT cells away. Given the higher frequency of HSC in the BM from CALRdel52-TG, these observations might suggest that CALRdel52 BM cells exhibited a growth advantage comparable to WT BM cells.
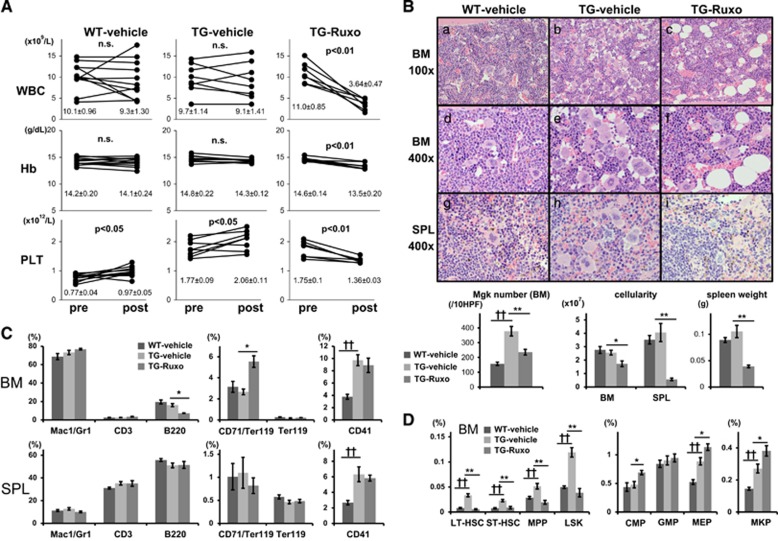
Ruxolitinib, the first-in-class JAK1/2 inhibitor, is now the primary therapeutic option for higher-risk MF patients who are not candidates for transplantation.26 We next examined whether or not ruxolitinib treatment ameliorated thrombocytosis in CALRdel52-TG mice. Either 90 mg/kg bid of ruxolitinib or vehicle was administrated to TG mice for 4 weeks. As shown in Figure 5A, TG mice treated with vehicle showed a mean 16% increase in platelet count during the 4-week treatment period, probably due to the disease progression. Ruxolitinib treatment attenuated the increase in the number of platelets in TG mice by a mean of 22%, but the overall count was still higher than that in WT mice. Ruxolitinib treatment also decreased white blood cell count and Hb level in TG mice. The decline in the white blood cell count was particularly prominent. In TG mice treated with ruxolitinib, it was reduced to 33% of the value in TG control mice and reached as low as 3.6 × 109/l. The ruxolitinib dosage level in this experiment also affected WT mice (Supplementary Figure S3). Hb level and white blood cell count were decreased to 89% and 65% of the pre-treatment values, respectively, although platelet count was slightly increased by ruxolitinib.
Figure 5.
Ruxolitinib ameliorates thrombocytosis in CALR mutation-induced ET. (A) Differential blood counts in WT mice treated with vehicle (WT-vehicle; n=11) for 4 weeks and in CALRdel52-TG mice treated with either vehicle (TG-vehicle; n=8) or 90 mg/kg bid ruxolitinib for 4 weeks (TG-Ruxo) (n=7). CALRdel52-TG demonstrate thrombocytosis, which is partially resolved by ruxolitinib therapy. Ruxolitinib also decreased white blood cell counts in TG mice. The paired data between pre- and post-treatment were analyzed with a paired two-tailed t-test. P-values are shown. (B) Upper panel: histological changes in CALRdel52-TG mice following ruxolitinib treatment for 4 weeks. BM were stained with hematoxylin and eosin (HE). TG mice treated with vehicle exhibit megakaryocyte proliferation in both BM and spleen (b, e and h). TG mice treated with ruxolitinib show a marked reduction of megakaryocytes in these organs (c, f and i). Lower left panel: the number of megakaryocytes is decreased by ruxolitinib therapy in TG mice. Lower center panel: the absolute numbers of nucleated cells in BM (one femur and one tibia) and spleen. Compared with vehicle-treated mice, TG treated with ruxolitinib show decreased nucleated cells in BM and spleen. Lower right panel: spleen weights are decreased by treatment with ruxolitinib but not vehicle. ††P<0.01 vs WT mice. *P<0.05 and **P<0.01 vs TG-vehicle mice. (C) The proportion of myeloid cells (Mac1/Gr1), T cells (CD3), B cells (B220), erythroid cells (CD71/Ter119 and Ter119) and megakaryocytes (CD41) in the BM and spleen. Ruxolitinib treatment in TG mice had little effect on the frequency of these cells, with the exception of B220 B cells and CD71/Ter119 erythroid cells. ††P<0.01 vs WT mice. *P<0.05 and **P<0.01 vs TG-vehicle mice. (D) The proportions of HSCs and progenitors in BM. TG treated with ruxolitinib show decreased HSC, MPP and LSK frequencies compared with TG mice treated with vehicle. ††P<0.01 vs WT mice. *P<0.05 and **P<0.01 vs TG-vehicle mice. All data are presented as means±s.e.m.
Hematoxylin and eosin-stained BM sections showed that ruxolitinib reduced the megakaryocyte number in CALRdel52-TG mice (Figure 5B). Ruxolitinib therapy seemed to have little effect on the proportion of each cell lineage in CALRdel52-TG BM, except for B220-positive cells and CD71/Ter119 double-positive cells (Figure 5C), and the number of nucleated cells from one femur and one tibia in ruxolitinib-treated mice fell to two-thirds of that in vehicle treated mice (Figure 5B). The cytoreductive effect was more prominent in the spleen, where the cell number in CALRdel52-TG mice that were treated with ruxolitinib fell to 15% of the number in TG mice treated with vehicle (Figure 5B). Consequently, in an estimation of the absolute number of cells in the body calculated based on the sum of cell numbers from two femurs, two tibias and the spleen,27 ruxolitinib treatment decreased the number of CD41-positive cells to about half of the number following vehicle treatment. It also decreased Mac1/Gr1- and B220-positive cell numbers to about one-half and one-fifth, respectively, compared with vehicle treatment.
As for the effect of ruxolitinib on HSC and progenitor cells, the proportions of HSC, MPP and LSK cells decreased, those of common myeloid progenitor, erythromegakaryocyte progenitor and megakaryocyte progenitor cells increased, and that of granulocyte–macrophage progenitor cells showed no change in CALRdel52-TG mice after 4 weeks of ruxolitinib therapy (Figure 5D and Supplementary Figure S4). Consequently, in an estimation of the absolute number of cells in the body, CALRdel52-TG mice treated by ruxolitinib showed drastically decreased numbers of HSC, MPP and LSK cells, with HSC counts of <10% of those in vehicle-treated TG mice; however, ruxolitinib had little impact on the numbers of common myeloid progenitor, erythromegakaryocyte progenitor and megakaryocyte progenitor cells.
Discussion
We showed that CALRdel52 and CALRins5 augmented STAT5 transcriptional activity in 293T cells transiently expressing MPL, and when CALR mutations were introduced into human megakaryoblastic and erythroleukemic cell lines to form the common novel C-terminus peptide observed in CALR-mutated MPN patients, these cell lines demonstrated increased growth or acquired cytokine-impendent cell growth. They did not show hypersensitivity to TPO. These observations may indicate that the effect of CALR mutations is the cytokine-independent activation of the JAK-STAT signaling cascade, which induces increased cell growth in cytokine-independent cells or confers cytokine-independent growth in cytokine-dependent cells.
CALRdel52-TG mice developed ET. This indicates that the CALRdel52 mutation is sufficient to augment megakaryocytic cell growth and cause ET, and CALR mutations, such as the JAK2 mutation, has a driver role in MPN. In contrast to transgenic mice expressing JAK2V617F (JAK2VF-TG),28 CALRdel52-TG mice did not show erythrocytosis or granulocytosis. This is consistent with many reports in which ET patients with a CALR mutation had lower Hb levels and/or leukocyte counts compared with ET patients with a JAK2V617F mutation.15, 16, 17, 18 In a mouse model, Marty et al.14 reported that recipient mice transplanted with BM cells that had been transduced with retroviruses expressing a human CALR mutation-induced thrombocytosis, but not erythrocytosis or leukocytosis. Both JAK2 and CALR mutations have a driver role in MPN and their effects on cell growth were assessed by the competitive serial transplantation assay. Just similar to JAK2-mutated BM cells, BM cells with a CALR mutation exhibited a growth advantage compared with WT cells in the first recipients. In the secondary recipients, BM cells with a JAK2 mutation demonstrated exhaustion,29 whereas BM cells with a CALR mutation exhibited almost the same growth as WT BM cells. As neither mutation had a growth advantage over WT cells in secondary recipients, other mutations in addition to that of CALR or JAK2 may be required for the development of MPN.
We previously reported that survival of JAK2VF-TG mice was inferior to that of WT mice.22 In contrast, in this study CALRdel52-TG mice showed similar survival to WT mice. In ET or PMF patients, the incidence of clinical episodes of thrombosis was lower in patients with CALR mutations than those with the JAK2 mutation.15, 16, 17, 18 This difference in the incidence of thrombotic events may influence the survival of patients with different mutations. Although the direct effect of either mutation may directly change platelet function, the difference in the incidence of thrombosis might be due to variations in leukocyte numbers between JAK2VF-TG mice and CALRdel52-TG mice. In MPN patients, leukocytosis has an adverse effect on thrombosis; the risk of thrombosis is elevated up to 1.7-fold when white blood cell counts exceed 15 000/μl.30, 31 In addition, the younger age at onset in patients with CALR mutations might contribute to their lower incidence of thrombosis.
ET is characterized by increased numbers of large, mature megakaryocytes in the BM, in addition to sustained thrombocytosis. In CALRdel52-TG mice, the number of megakaryocytes in the BM was approximately double that in WT mice, and their size and the number of α-granules they contained were also increased in TG mice. Megakaryocytes invaded the spleen in CALRdel52-TG mice, although the spleen weight was comparable in WT mice. As mentioned, although CALRdel52-TG developed ET, they did not demonstrate MF during the 12 months of observation after birth. This contrasts with the results of retrovirally transduced bone marrow transplantation model reported by Marty et al.,14 in which BM fibrosis occurred 6 months after transplantation. This discrepancy might be caused by different levels of expression of mutant CALR; the expression of CALRdel52 in our TG model was near physiological levels, in contrast to the overexpression of retroviral transgenes in general.
We showed that the presence of MPL was necessary for the augmentation of STAT5 activity by the CALR mutant in 293T cells. STAT5 activation only in megakaryocytes, which express MPL, may contribute to these megakaryocyte- and platelet-specific features in CALRdel52-TG mice. STAT5 activity was not enhanced by the presence of CSF3R or EPOR, and this observation was consistent with that recently reported by Chachoua et al.12 HSCs were reported to express MPL and TPO stimulation increased their number in vitro and in vivo.32, 33 The augmentation of STAT5 activation by the CALR mutant in cells with MPL might explain why the proportion of HSCs in the BM was higher in CALRdel52-TG mice than in WT mice.
Ruxolitinib is a JAK inhibitor that ameliorates splenomegaly and constitutional symptoms associated with MF.34, 35 It was effective in JAK2V617F-negative MF patients, although to a slightly lesser extent than in patients who were JAK2V617F positive.34 Ruxolitinib is suspected to be effective in the roughly two-thirds of JAK2V617F-negative MF patients who have CALR mutations. In fact, COMFORT-II, an exploratory, retrospective analysis of CALR-mutated patients, found that 20% of MF patients with CALR mutation, who received ruxolitinib, achieved a ⩾35% reduction in spleen volume at week 48 compared with baseline and there were no significant differences in spleen response rates between CALR mutation-positive patients and the overall COMFORT-II population treated with ruxolitinib.36 In line with these clinical observations, ruxolitinib therapy attenuated the increased numbers of peripheral blood platelets and BM megakaryocytes in CALRdel52-TG mice. The effect of ruxolitinib on mice with CALR mutations also supports the idea that sustained thrombocytosis with increased numbers of megakaryocytes was mediated by JAK-STAT activation. Ruxolitinib also decreased the numbers of peripheral blood leukocytes, in particular B lymphocytes, in both CALRdel52-TG and WT mice. Grade 3 or 4 lymphopenia, in addition to anemia and thrombocytopenia, was one of the most common hematologic abnormalities in clinical studies in which the effect of ruxolitinib was compared with the best available therapy.37, 38 In these studies, lymphopenia occurred at similar rates in the ruxolitinib and best-available therapy groups. Together, these findings suggest that the ruxolitinib-induced leukopenia observed in CALRdel52-TG may not be due to the ruxolitinib effect on a pathway activated by the CALR mutation, but may instead be a sign of toxicity.
Recent studies, in addition to our observations here, revealed a vital role for MPL and STAT5 activation in CALR mutation-induced MPN. Chachoua et al.12 reported that asparagine (N) 117 and N178 at N-glycosylated sites of MPL, and tyrosine (Y) 109 and aspartic acid (D) 135 of glycan-binding sites of CALR, were required for the augmentation of STAT5 activation by cooperation between CALR mutants and MPL. Araki et al.13 showed that a CALR mutant, but not WT CALR, could bind to MPL. They showed that CALR binds to MPL via its N-domain (amino acids 1–197), and that the P-domain (amino acids 198–307), which is preserved in both WT and mutant CALR, interfered with this binding. Thus, perhaps WT CALR does not bind to MPL but CALR mutants are able to do so by removing this interference. In addition, Elf et al.39 reported that the C-terminus of the CALRdel52 protein, which is necessary for interactions between that protein and MPL, showed a positive electrostatic charge that was required for CALRdel52-induced MPN in mice.
In summary, CALR mutation induced autonomous cell growth and caused ET in mice. MPL was essential for CALR mutation-induced STAT5 activation in 293T cells. Ruxolitinib therapy attenuated the increased numbers of peripheral blood platelets and BM megakaryocytes, and ameliorated CALR mutation-induced ET.
Acknowledgments
We thank M Matsushita, T Shinmori and S Saito for their technical assistance. This work was supported by Grants-in-Aid for Young Scientists (B; 26860738 and 15K19554) and for Scientific Research (C; 26461408 and 15K09480) from the Japan Society for the Promotion of Science, and by Research Grants from Takeda Science Foundation.
Author contributions
K Shide, TK and TY performed research. K Shide and AH performed CRISPR/Cas9 gene editing. TK and AS performed pathological examinations using transmission electron microscopy. MS, NI, A Kamiunten, KA, KN, TH, YK, HS, A Kitanaka, HA, TM, HI, YT, MS, SH, SY and KN analyzed and interpreted data. K Shide, TK and K Shimoda conceived the research, guided its design, analysis and interpretation, and wrote the manuscript.
Footnotes
Supplementary Information accompanies this paper on the Leukemia website (http://www.nature.com/leu)
The authors declare no conflict of interest.
Supplementary Material
References
- Swerdlow SH (ed). Myeloproliferative neoplasms. In: WHO Classificationof Tumors of Haematopoietic and Lymphoid Tissues. IARC Press: Lyon, 2008, pp 40–50.
- Kralovics R, Passamonti F, Buser AS, Teo SS, Tiedt R, Passweg JR et al. A gain-of-function mutation of JAK2 in myeloproliferative disorders. N Engl J Med 2005; 352: 1779–1790. [DOI] [PubMed] [Google Scholar]
- James C, Ugo V, Le Couédic J-P, Staerk J, Delhommeau F, Lacout C et al. A unique clonal JAK2 mutation leading to constitutive signalling causes polycythaemia vera. Nature 2005; 434: 1144–1148. [DOI] [PubMed] [Google Scholar]
- Baxter EJ, Scott LM, Campbell PJ, East C, Fourouclas N, Swanton S et al. Acquired mutation of the tyrosine kinase JAK2 in human myeloproliferative disorders. Lancet 2005; 365: 1054–1061. [DOI] [PubMed] [Google Scholar]
- Levine RL, Wadleigh M, Cools J, Ebert BL, Wernig G, Huntly BJ et al. Activating mutation in the tyrosine kinase JAK2 in polycythemia vera, essential thrombocythemia, and myeloid metaplasia with myelofibrosis. Cancer Cell 2005; 7: 387–397. [DOI] [PubMed] [Google Scholar]
- Rampal R, Al-Shahrour F, Abdel-Wahab O, Patel JP, Brunel JP, Mermel CH et al. Integrated genomic analysis illustrates the central role of JAK-STAT pathway activation in myeloproliferative neoplasm pathogenesis. Blood 2014; 123: e123–e133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott LM, Tong W, Levine RL, Scott MA, Beer PA, Stratton MR et al. JAK2 exon 12 mutations in polycythemia vera and idiopathic erythrocytosis. N Engl J Med 2007; 356: 459–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pardanani AD, Levine RL, Lasho T, Pikman Y, Mesa RA, Wadleigh M et al. MPL515 mutations in myeloproliferative and other myeloid disorders: a study of 1182 patients. Blood 2006; 108: 3472–3476. [DOI] [PubMed] [Google Scholar]
- Pikman Y, Lee BH, Mercher T, McDowell E, Ebert BL, Gozo M et al. MPLW515L is a novel somatic activating mutation in myelofibrosis with myeloid metaplasia. PLoS Med 2006; 3: e270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klampfl T, Gisslinger H, Harutyunyan AS, Nivarthi H, Rumi E, Milosevic JD et al. Somatic mutations of calreticulin in myeloproliferative neoplasms. New Engl J Med 2013; 369: 2379–2390. [DOI] [PubMed] [Google Scholar]
- Nangalia J, Massie CE, Baxter EJ, Nice FL, Gundem G, Wedge DC et al. Somatic CALR mutations in myeloproliferative neoplasms with nonmutated JAK2. N Engl J Med 2013; 369: 2391–2405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chachoua I, Pecquet C, El-Khoury M, Nivarthi H, Albu R-I, Marty C et al. Thrombopoietin receptor activation by myeloproliferative neoplasm associated calreticulin mutants. Blood 2016; 127: 1325–1335. [DOI] [PubMed] [Google Scholar]
- Araki M, Yang Y, Masubuchi N, Hironaka Y, Takei H, Morishita S et al. Activation of the thrombopoietin receptor by mutant calreticulin in CALR-mutant myeloproliferative neoplasms. Blood 2016; 127: 1307–1316. [DOI] [PubMed] [Google Scholar]
- Marty C, Pecquet C, Nivarthi H, El-Khoury M, Chachoua I, Tulliez M et al. Calreticulin mutants in mice induce an MPL-dependent thrombocytosis with frequent progression to myelofibrosis. Blood 2016; 127: 1317–1324. [DOI] [PubMed] [Google Scholar]
- Rotunno G, Mannarelli C, Guglielmelli P, Pacilli A, Pancrazzi A, Pieri L et al. Impact of calreticulin mutations on clinical and hematological phenotype and outcome in essential thrombocythemia. Blood 2014; 123: 1552–1555. [DOI] [PubMed] [Google Scholar]
- Rumi E, Pietra D, Ferretti V, Klampfl T, Harutyunyan AS, Milosevic JD et al. JAK2 or CALR mutation status defines subtypes of essential thrombocythemia with substantially different clinical course and outcomes. Blood 2014; 123: 1544–1551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rumi E, Pietra D, Pascutto C, Guglielmelli P, Martinez-Trillos A, Casetti I et al. Clinical effect of driver mutations of JAK2, CALR, or MPL in primary myelofibrosis. Blood 2014; 124: 1062–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tefferi A, Lasho TL, Finke CM, Knudson RA, Ketterling R, Hanson CH et al. CALR vs JAK2 vs MPL mutated or triple-negative myelofibrosis: clinical, cytogenetic and molecular comparisons. Leukemia 2014; 28: 1472–1477. [DOI] [PubMed] [Google Scholar]
- Numata A, Shimoda K, Kamezaki K, Haro T, Kakumitsu H, Shide K et al. Signal transducers and activators of transcription 3 augments the transcriptional activity of CCAAT/enhancer-binding protein alpha in granulocyte colony-stimulating factor signaling pathway. J Biol Chem 2005; 280: 12621–12629. [DOI] [PubMed] [Google Scholar]
- Domen J, Gandy KL, Weissman IL. Systemic overexpression of BCL-2 in the hematopoietic system protects transgenic mice from the consequences of lethal irradiation. Blood 1998; 91: 2272–2282. [PubMed] [Google Scholar]
- Kakumitsu H, Kamezaki K, Shimoda K, Karube K, Haro T, Numata A et al. Transgenic mice overexpressing murine thrombopoietin develop myelofibrosis and osteosclerosis. Leuk Res 2005; 29: 761–769. [DOI] [PubMed] [Google Scholar]
- Shide K, Shimoda HK, Kumano T, Karube K, Kameda T, Takenaka K et al. Development of ET, primary myelofibrosis and PV in mice expressing JAK2 V617F. Leukemia 2008; 22: 87–95. [DOI] [PubMed] [Google Scholar]
- Ihle JN, Nosaka T, Thierfelder W, Quelle FW, Shimoda K. Jaks and Stats in cytokine signaling. Stem Cells 1997; 15 (Suppl 1): 105–111, discussion 112. [DOI] [PubMed] [Google Scholar]
- Nagano T, Ohga S, Kishimoto Y, Kimura T, Yasunaga K, Adachi M et al. Ultrastructural analysis of platelet-like particles from a human megakaryocytic leukemia cell line (CMK 11-5). Int J Hematol 1992; 56: 67–78. [PubMed] [Google Scholar]
- Chiba S, Takaku F, Tange T, Shibuya K, Misawa C, Sasaki K et al. Establishment and erythroid differentiation of a cytokine-dependent human leukemic cell line F-36: a parental line requiring granulocyte-macrophage colony-stimulating factor or interleukin-3, and a subline requiring erythropoietin. Blood 1991; 78: 2261–2268. [PubMed] [Google Scholar]
- Reilly JT, McMullin MF, Beer PA, Butt N, Conneally E, Duncombe AS et al. Use of JAK inhibitors in the management of myelofibrosis: a revision of the British Committee for Standards in Haematology Guidelines for Investigation and Management of Myelofibrosis 2012. Br J Haematol 2014; 167: 418–420. [DOI] [PubMed] [Google Scholar]
- Boggs DR. The total marrow mass of the mouse: a simplified method of measurement. Am J Hematol 1984; 16: 277–286. [DOI] [PubMed] [Google Scholar]
- Tiedt R, Hao-Shen H, Sobas MA, Looser R, Dirnhofer S, Schwaller J et al. Ratio of mutant JAK2-V617F to wild-type Jak2 determines the MPD phenotypes in transgenic mice. Blood 2008; 111: 3931–3940. [DOI] [PubMed] [Google Scholar]
- Kameda T, Shide K, Yamaji T, Kamiunten A, Sekine M, Taniguchi Y et al. Loss of TET2 has dual roles in murine myeloproliferative neoplasms: disease sustainer and disease accelerator. Blood 2015; 125: 304–315. [DOI] [PubMed] [Google Scholar]
- Alvarez-Larran A, Pereira A, Cervantes F, Arellano-Rodrigo E, Hernandez-Boluda JC, Ferrer-Marin F et al. Assessment and prognostic value of the European LeukemiaNet criteria for clinicohematologic response, resistance, and intolerance to hydroxyurea in polycythemia vera. Blood 2012; 119: 1363–1369. [DOI] [PubMed] [Google Scholar]
- Landolfi R, Di Gennaro L, Barbui T, De Stefano V, Finazzi G, Marfisi R et al. Leukocytosis as a major thrombotic risk factor in patients with polycythemia vera. Blood 2007; 109: 2446–2452. [DOI] [PubMed] [Google Scholar]
- Kaushansky K. Mpl and the hematopoietic stem cell. Leukemia 2002; 16: 738–739. [DOI] [PubMed] [Google Scholar]
- Solar GP, Kerr WG, Zeigler FC, Hess D, Donahue C, de Sauvage FJ et al. Role of c-mpl in early hematopoiesis. Blood 1998; 92: 4–10. [PubMed] [Google Scholar]
- Verstovsek S, Mesa RA, Gotlib J, Levy RS, Gupta V, DiPersio JF et al. A double-blind, placebo-controlled trial of ruxolitinib for myelofibrosis. N Engl J Med 2012; 366: 799–807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison C, Kiladjian JJ, Al-Ali HK, Gisslinger H, Waltzman R, Stalbovskaya V et al. JAK inhibition with ruxolitinib versus best available therapy for myelofibrosis. N Engl J Med 2012; 366: 787–798. [DOI] [PubMed] [Google Scholar]
- Guglielmelli P, Rotunno G, Bogani C, Mannarelli C, Giunti L, Provenzano A et al. Ruxolitinib is an effective treatment for CALR-positive patients with myelofibrosis. Br J Haematol 2016; 173: 938–940. [DOI] [PubMed] [Google Scholar]
- Kantarjian HM, Silver RT, Komrokji RS, Mesa RA, Tacke R, Harrison CN. Ruxolitinib for myelofibrosis—an update of its clinical effects. Clin Lymph Myeloma Leuk 2013; 13: 638–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vannucchi AM, Kiladjian JJ, Griesshammer M, Masszi T, Durrant S, Passamonti F et al. Ruxolitinib versus standard therapy for the treatment of polycythemia vera. N Engl J Med 2015; 372: 426–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elf S, Abdelfattah NS, Chen E, Perales-Patón J, Rosen EA, Ko A et al. Mutant calreticulin requires both its mutant c-terminus and the thrombopoietin receptor for oncogenic transformation. Cancer Discov 2016; 6: 368–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.