Abstract
We performed a systematic review of the literature involving a number of databases to identify studies that included outcomes of surgical treatment of acetabular fractures in patients aged > 55 years. An initial search identified 1564 studies. After exclusion by two independent reviewers, 15 studies met the inclusion criteria. All studies were case series and the mean Coleman Methodology score for methodological quality assessment was 43.7 (standard deviation 12.3). There were 354 patients with acetabular fractures. Pooled analysis revealed a mean age of 71.6 years (55 to 96) and a mean follow-up of 43 months (20 to 188). Complex fractures were reported in 70.1% of patients.
Seven studies presented the results of open reduction and internal fixation (ORIF); in eight other studies a total hip arthroplasty (THA), alone or combined with different internal fixation techniques, was the chosen treatment. In the ORIF sub-group, conversion to THA was performed at a mean of 25.5 months with anatomical reduction in 11.6% and imperfect and poor reduction in 22.3%. In the THA sub-group, an acetabular ring or cage with a cemented acetabular component was used in four studies (52 patients) and a cementless acetabular component was implanted in five studies (78 patients). Six patients (4.9%) underwent revision at a mean of 39 months after the index procedure.
The analysis of intra-operative and post-operative parameters showed a statistical difference between the two sub-groups with regards to the mean operating time (236 mins ORIF vs 178 mins THA), the mean blood loss (707 mL ORIF vs 974 mL THA) and the mean mortality rate at one year (22.6% ORIF vs 8.8% THA).
Based on the current data available, acute THA (alone or in combination with internal fixation) may have a role in the treatment of older patients with complex acetabular fractures. Despite the wide heterogenecity of fracture types and patient co-morbidities, THA procedures were associated with lower rates of mortality and further surgery when compared with the ORIF procedures.
Cite this article: EFORT Open Rev 2017;2:97-103. DOI: 10.1302/2058-5241.2.160036
Keywords: Acute total hip arthroplasty, Open reduction internal fixation, Acetabular fracture
Introduction
As the elderly patient population continues to sustain a more active lifestyle, the incidence of pelvic and acetabular fractures in the elderly is on the rise. Epidemiological studies have demonstrated that the incidence of such fractures is expected to approximately double over the next 20 years in individuals aged > 60 years.1-3
Multiple subsets exist within the elderly population. These can be generally categorised by patient factors, injury factors or treatment factors.
Patient factors in the elderly include physiological age, degree of underlying osteoporosis, medical co-morbidities, pre-existing degenerative joint disease, pre-morbid activity level and baseline mental function.
Injury factors include the injury mechanism, fracture patterns and presence of associated injuries. Treatment factors include the chosen management pathway, the surgeon’s experience and the timing of treatment. Optimal management of the elderly patient with an acetabular fracture requires that each of these factors must be considered when formulating the treatment plan.
The goal of the treatment is to reconstitute the hip joint to provide a stable, painless construct capable of rapidly recovering its pre-injury level of function.4 Open reduction and internal fixation (ORIF) and total hip arthroplasty (THA) are both suitable for achieving these goals in properly selected patients.
To provide greater clarity about outcomes with different treatments for complex acetabular fractures in older patients, we carried out this systematic review of the literature to analyse the results of conventional ORIF and THA. Patients treated with percutaneous internal fixation were not included in this study.
Materials and methods
This systematic review included studies published in English, French, German, Spanish and Italian containing pooled results of the treatment of patients aged > 55 years who had sustained an acetabular fracture, or studies from which we could extract results based on the patient’s age.
Date limits were set between 2000 and 2015 to get a review of recent data. All experimental and observational studies, either retrospective, prospective or comparative, were included. Case reports, review articles, expert opinion and editorials were excluded from the review.
Searches were conducted in July 2015 using the following databases: Pubmed/MEDLINE, SCOPUS, Embase and Ovid. The following keywords were used: ‘acetabular’ OR ‘acetabulum’ AND ‘fracture’.
Two observers (MM, AC) independently screened all identified studies based on title and abstract for eligibility. In case of doubt, consensus was reached by discussion. Then the full text manuscripts of all studies, included after this first step, were again independently reviewed (MM, AC). Consensus in cases of doubt was reached by discussing the full text manuscripts.
The abstracts of all hits were reviewed, duplicates were eliminated and references were hand-screened for relevant citations. This left 15 studies5-19 available for data extraction. The first outcomes of interest were radiographic results, functional results and mortality. The secondary outcomes of interest were the rate of conversion surgery from ORIF to THA and complication rate in acute THA for the treatment of acetabular fractures.
Data extraction
Data were extracted by two observers (MM, PM) who used a pre-set standardised data extraction form.
The treatment offered for the fractures was the comparator, and the information extracted included the number of patients, mean age, mean follow-up, type of treatment, classification of fracture, mean operating time, mean blood loss, secondary procedure, complications, functional and radiographic results.
The extracted data were entered onto a spreadsheet (Excel; Microsoft Corp., Redmond, Washington) as raw numbers where possible, plus any summary measures such as standard deviations (sd), 95% confidence intervals (CIs) and ranges.
Quality assessment
All studies were case series and represent level IV evidence. The quality of the studies was assessed using the Coleman Methodology Score (CMS),20 which assesses methodology using ten criteria, giving a total score between 0 and 100. A score of 100 indicates that the study largely avoids chances of bias and confounding factors. The mean CMS was 43.7 (21 to 60; sd 12.3).
Statistical analysis
This was conducted using SPSS version 21.0 software (IBM, Armonk, New York). Analysis of the data was performed by using proportions and frequencies for categorical variables, means along with sd, and ranges for continuous variables. For univariate analysis, means were weighted for sample size and statistical comparison between the different treatment modalities performed, using the Student’s t-test for parametric scale variables in independent groups and the Mann-Whitney U test for non-parametric scale variables and ordinal variables in independent groups. In bivariate analysis, adjusted risks (odds ratios (OR)) were presented with 95% CIs. Values of p < 0.05 were considered to be statistically significant.
Results
Description of the studies
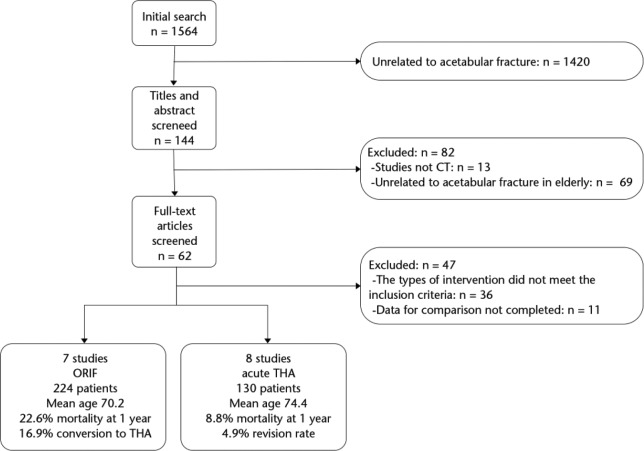
Studies from initial searches to final inclusion or exclusion are displayed in the flowchart (Fig. 1). This systematic review includes a total of 15 studies, published between 2003 and 2014, written in English, French and German. The characteristics of the included studies are shown in Table 1. A total of 13 studies5,7-16,18,19 are retrospective and two6,17 are prospective. According to the Letournel and Judet fracture classification system,21 elementary patterns were reported in 29.9% of cases while complex patterns were reported in 70.1% of the patients. In the ORIF sub-group the most common types reported were both columns (BC) (28.1%), anterior column posterior hemitransverse (ACPHT) (26.8%) and anterior column (AC) (11.6%). In this sub-group, the authors reported femoral head injury in 8.5% of the cases associated with different fractures types.
Fig. 1.
Flowchart of trials selection process (ORIF, open reduction and internal fixation; THA, total hip arthroplasty).
Table 1.
Characteristics of the studies included in the systematic review
| n | Study | Year | Periods | Design | Surgical treatment | Patients (n) | Mean age (yrs) | Follow-up (mths) |
|---|---|---|---|---|---|---|---|---|
| 1 | Archdeacon et al13 | 2013 | 2000-2009 | Retrospective | ORIF | 38 | 80 | 34 |
| 2 | Bastian et al14 | 2013 | 2005-2009 | Retrospective | ORIF | 17 | 72 | 35 |
| 3 | Jeffcoat et al12 | 2012 | 1992-2006 | Retrospective | ORIF | 41 | 67 | 63 |
| 4 | Kinik and Armangil7 | 2004 | 1996-2001 | Retrospective | ORIF | 9 | 64.1 | 44 |
| 5 | Laflamme et al11 | 2011 | 2006-2010 | Retrospective | ORIF | 21 | 64.3 | 50 |
| 6 | Li and Tang18 | 2014 | 2000-2008 | Retrospective | ORIF | 52 | 69.9 | 29 |
| 7 | O’Toole et al19 | 2014 | 2001-2006 | Retrospective | ORIF | 46 | 69 | 51 |
| 8 | Boraiah et al9 | 2009 | 1997-2007 | Retrospective | IF + THA | 18 | 72 | 46.8 |
| 9 | Borens et al6 | 2004 | 1998-2000 | Prospective | IF + THA | 15 | 81 | 36 |
| 10 | Chakravarty et al16 | 2014 | 2005-2011 | Retrospective | IF + THA | 19 | 77 | 22 |
| 11 | Cochu et al8 | 2007 | 1981-2001 | Retrospective | THA | 16 | 76.1 | 38.4 |
| 12 | Enocson and Blomfeldt17 | 2014 | 2001-2008 | Prospective | THA | 15 | 75 | 48 |
| 13 | Herscovici et al10 | 2010 | 1995-2005 | Retrospective | IF + THA | 22 | 75.3 | 29.4 |
| 14 | Tidermark et al5 | 2003 | 1993-1999 | Retrospective | THA | 10 | 73 | 38 |
| 15 | Malhotra et al15 | 2013 | 2000-2005 | Retrospective | IF + THA | 15 | 64.5 | 81.5 |
ORIF, open reduction and internal fixation; THA, total hip arthroplasty; IF, internal fixation
In the THA sub-group the most common types reported were ACPHT (21.5%) and transverse posterior wall (TVPW) (14.6%). Femoral head injury was recorded in 14.6% of the fractures (Table 2).
Table 2.
Classification of fractures patterns in the selected studies
| Study | Elementary | Complex | PW | AW | AC | PC | TV | BC | ACPHT | PCPW | T-type | TVPW | IQP | AWAC | PW +FI | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Archdeacon et al13 | 7 | 31 | 7 | 9 | 22 | |||||||||||
| Bastian et al14 | 4 | 13 | 3 | 1 | 5 | 7 | 1 | |||||||||
| Jeffcoat et al12 | 1 | 40 | 1 | 19 | 20 | 1 | ||||||||||
| Kinik and Armangil7 | 3 | 6 | 1 | 2 | 2 | 2 | 1 | 1 | ||||||||
| Laflamme et al11 | 6 | 15 | 6 | 6 | 6 | 3 | ||||||||||
| Li and Tang18 | 22 | 30 | 4 | 8 | 5 | 1 | 4 | 15 | 1 | 1 | 6 | 4 | 1 | 1 | 1 | |
| O’Toole et al19 | 23 | 23 | 17 | 4 | 1 | 1 | 7 | 2 | 7 | 3 | 4 | |||||
| Boraiah et al9 | 2 | 16 | 1 | 1 | 1 | 1 | 1 | 2 | 11 | |||||||
| Borens et al6 | 2 | 13 | 2 | 1 | 2 | 8 | 2 | |||||||||
| Chakravarty et al16 | 4 | 15 | 1 | 3 | 4 | 5 | 2 | 3 | 1 | |||||||
| Cochu et al8 | 8 | 8 | 1 | 3 | 4 | 1 | 4 | 1 | 1 | 1 | ||||||
| Enocson and Blomfeldt17 | 11 | 4 | 10 | 1 | 4 | |||||||||||
| Herscovici et al10 | 0 | 22 | 6 | 7 | 9 | |||||||||||
| Malhotra et al15 | 8 | 7 | 3 | 3 | 2 | 2 | 3 | 2 | ||||||||
| Tidermark et al5 | 5 | 5 | 5 | 5 | ||||||||||||
| Total | 106 | 248 | 27 | 8 | 40 | 5 | 26 | 76 | 88 | 16 | 26 | 27 | 1 | 2 | 12 | 354 |
| Incidence (%) | 29.9 | 70.1 | 7.6 | 2.3 | 11.3 | 1.4 | 7.3 | 21.5 | 24.9 | 4.5 | 7.3 | 7.6 | 0.3 | 0.6 | 3.4 | |
| Total ORIF | 58 | 166 | 22 | 8 | 26 | 2 | 8 | 63 | 60 | 9 | 15 | 8 | 1 | 1 | 1 | 224 |
| Incidence (%) | 25.9 | 74.1 | 9.8 | 3.6 | 11.6 | 0.9 | 3.6 | 28.1 | 26.8 | 4.0 | 6.7 | 3.6 | 0.4 | 0.4 | 0.4 | |
| Total acute THA | 40 | 90 | 5 | 0 | 14 | 3 | 18 | 13 | 28 | 7 | 11 | 19 | 0 | 1 | 11 | 130 |
| Incidence (%) | 30.8 | 69.2 | 3.8 | 0.0 | 10.8 | 2.3 | 13.8 | 10.0 | 21.5 | 5.4 | 8.5 | 14.6 | 0.0 | 0.8 | 8.5 |
PW, posterior wall; AW, anterior wall; AC, anterior column; PC, posterior column; TV, transverse; BC, both columns; ACPHT, anterior column posterior hemitransverse; PCPW, posterior column posterior wall; TVPW, transverse posterior wall; IQP, isolated quadrilateral plate; AWAC, anterior wall anterior column; FI, femoral injury; ORIF, open reduction and internal fixation; THA, total hip arthroplasty
In the ORIF sub-group, all seven studies7,11-14,18,19 used conventional ORIF with cortical screws and reconstruction plates placed on the pelvic brim. Different surgical approaches were used: Kocher-Langenbeck (32%) for PW or posterior column (PC) fractures and the ileo-inguinal approach (29.2%) for isolated AC or ACPHT fractures. A combined approach of Stoppa and a lateral window of the ileo-inguinal approach (12.3%) was used for AC fractures with displacement of the quadrilateral plate (QP), combined Kocher-Langenbeck and ileo-inguinal (12.3%) for BC or T-shaped fractures.
Five studies6,9,10,15,16 presented the results of a combined procedure of internal fixation (IF) and THA; three studies5,8,17 evaluated the results of THA alone. The surgical approaches most commonly used were a posterior approach in 76.9% and lateral approach in 23.1% of the cases. Various techniques were described among this sub-group: Chakravarty et al16 obtained a previous stabilisation of the acetabular fracture with one or two cannulated screws, whereas in the Borens et al series,6 a cable fixation was used to obtain fracture reduction. In three studies,9,10,15 standard ORIF prior THA implantation was used. Cochu et al8 and Malhotra et al15 used different types of reinforcement rings to fix the acetabular component to the ilium. In Enocson and Blomfeldt’s17 and Tidermark et al’s5 series a Burch–Schneider antiprotrusio cage (Zimmer, Warsaw, Indiana) was adjusted and fixed to the pelvis using two to five screws in the intact part of the ileum. The femoral head was morsellised and used as autograft for acetabular reconstruction in 73% of the patients. In all, 60% of the acetabular components were cementless. The femoral stem was cemented in 58% of the cases.
Demographics
The mean age of the 354 patients treated in the studies was 71.6 years (55 to 96) at the time of surgery and 70% were male. In all, 54% presented a low energy trauma, 34.9% road traffic accidents and 10.4% a fall from higher than standing height.
Intra-operative parameters
In the ORIF sub-group the mean operating time of 236.6 mins (167 to 280) was reported in 127 patients and a mean blood loss of 707 mL (500 to 1400) was reported in 106 patients. On the other hand, in the THA sub-group a mean operating time of 178.4 mins (135 to 235) was reported in 112 patients and a mean blood loss of 974 mL (700 to 1163) was reported in 81 patients. The mean operating time was significantly longer (p < 0.001) in the ORIF sub-group than in the THA sub-group. Conversely, the mean blood loss was significantly higher (p < 0.001) in the THA sub-group than in the ORIF sub-group.
Complications
The mortality rate at one year reported in three ORIF studies (128 patients) was 22.6% (95% CI 16.3 to 30.6), while in the five THA studies (80 patients) the rate reported was 8.8% (95% CI 4.3 to 17). The Student’s t-test demonstrated a significant difference in mortality rate between the two sub-groups (p = 0.018).
The mean incidence of non-fatal complications was 32.02% (95% CI 25.6 to 39.2) in the ORIF studies and 30.3% (95% CI 21.8 to 40.5) in the IF + THA studies. No statistical difference was found between the two sub-groups regarding non-fatal complications (p = 0.703). In the THA sub-group, the rate of hip dislocation was 4.8%, while it was 8.9% in the THA + IF subgroup.
Functional outcomes
Functional outcomes were evaluated with a mean follow-up of 43 months (22 to 81.5). In the ORIF sub-group, all the studies except one used the Modified Merle d’Aubigné-Postel score22 with a mean value of 16.05 (9 to 18); the Harris Hip Score (HHS)23 was used in three studies (90 patients) with a mean value of 85.8 (23 to 100). In the acute THA sub-group (96 patients), all the studies except two6,16 used the HHS as the outcome measure. The mean score was 82.5 (42 to 100). The Mann-Whitney U test demonstrated no statistical difference (p = 0.79) in HHS between the two sub-groups.
Radiological outcome
All the studies in the ORIF treatment sub-group used the Matta criteria24 to assess radiological outcomes. Anatomical reduction was achieved in 50% of the patients, imperfect reduction in 35.7% and poor reduction in 14.3%.
Laflamme et al11 noticed how the presence of a ‘Gull sign’21 resulted in lower initial quality of reduction and it was correlated with a higher conversion rate to THA.
Li and Tang18 reported excellent or good clinical outcomes in 100% of the patients (18/18) whose hips did not have any radiographic negative prognostic signs. By contrast, they had fair or poor clinical outcomes in 6/15 (40%) patients with quadrilateral plate fracture, 6/12 (50%) with ‘Gull sign’, 7/22 (32%) with posterior dislocation of the hip and 7/10 (70%) with femoral head injury.18
O’Toole et al19 noticed how the failure rate in elderly patients with posterior wall fracture was double compared with patients without a posterior wall fracture while the anatomical reduction of the fractures was not related to a lower incidence of THA conversion rate.
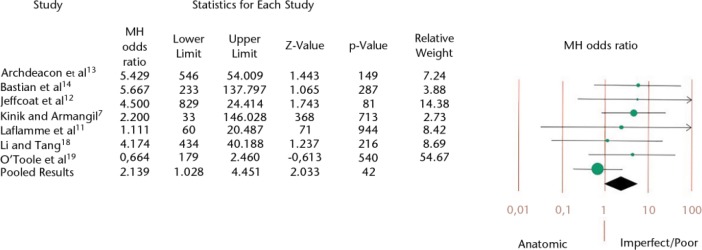
In the ORIF sub-group, the overall mean THA conversion rate of fractures with anatomical reduction was 11.6% (13 hips) while it was 22.3% (25 hips) in those with imperfect and poor reduction. The mean time from the ORIF procedure to the conversion to THA was reported in five studies and was 27.7 months (14 to 43.6). Pooled analysis shows that imperfect and poor reductions are related to a higher risk of delayed THA (Fig. 2).
Fig. 2.
Forest plot of relative risk with confidence interval for open reduction and internal fixation to total hip arthroplasty conversion rate correlated to reduction quality (Mantel-Haenszel (MH) odds ratio = 2.139: 95% confidence interval 1.028 to 4.451; p = 0.042).
In the THA sub-group, the mean follow-up was 39 months (22 to 81.5) with an incidence of component revision of 4.9% (95% CI 2.2 to 10.2). Three patients underwent revisions of both components as results of recurrent dislocations, and two patients required isolated acetabular revision for aseptic loosening. One patient required revision surgery for fracture of the zirconia femoral head.
No deep infections were reported. Heterotopic ossification of various grades25 was diagnosed in 23.1% of the cases. The pooled results of all patients stratified by form of treatment are shown in Table 3.
Table 3.
Pooled analysis of outcome measures by type of surgical treatment
| All patients (15 studies)5-19 |
ORIF (7 studies)7,11-14,18,19 |
Acute THA (8 studies)5,6,8-10,15-17 |
||||
|---|---|---|---|---|---|---|
| Patients (n) | Mean (95% CI) | Patients (n) | Mean (95% CI) | Patients (n) | Mean (95% CI) | |
| Age (yrs) | 354 | 71.6 (71.0 to 72.2) | 224 | 70.2 (69.5 to 70.9) | 130 | 74.4 (73.6 to 75.2) |
| Gender (Male %) | 276 | 70.3 (64.6 to 75.4) | 179 | 73.7 (66.8 to 79.6) | 97 | 63.9 (54 to 72.8) |
| Follow-up (mths) | 318 | 43 (41.3 to 44.7) | 195 | 44.3 (42.2 to 45.2) | 123 | 39 (34.8 to 43.2) |
| Operation time (mins) | 239 | 209.3 (207.6 to 216) | 127 | 236.6 (228.8 to 245.2) | 112 | 178.4 (170.5 to 186.3) |
| Blood loss (mL) | 187 | 822.6 (781.4 to 863.8) | 106 | 707 (632.4 to 781.6) | 81 | 974 (929.5 to 1018.5) |
| Mortality at one yr (%) | 208 | 17.3 (12.8 to 23) | 128 | 22.6 (16.3 to 30.6) | 80 | 8.8 (4.3 to 17) |
| Non-fatal complication rate (%) | 267 | 31.5 (26.2 to 37.3) | 178 | 32.02 (25.6 to 39.2) | 89 | 30.3 (21.8 to 40.5) |
| Harris Hip Score | 186 | 84.1 (83.2 to 85) | 90 | 85.8 (85.4 to 86.2) | 96 | 82.5 (81 to 84) |
| Satisfactory results (%) | 192 | 74.5 (67.9 to 80.1) | 161 | 72.7 (65.3 to 79) | 31 | 83.9 (67.4 to 92.9) |
| THA conversion rate (%) | 195 | 16.96 (12.6 to 22.4) | ||||
| Time to failure (mths) | 39 | 27.7 (23.9 to 31.6) | ||||
| Revision procedure (%) | 123 | 4.9 (2.2 to 10.2) | ||||
CI, confidence interval; ORIF, open reduction and internal fixation; THA, total hip arthroplasty; IF, internal fixation
Discussion
In this study, we isolated a sub-group of older patients with complex acetabular fracture in an attempt to define the outcome of surgical treatment stratified by treatment modality.
Elderly patients with acetabular fractures show broad heterogeneity and therefore treatment has to be highly individualised. As described in previous studies,1-3 pooled analysis of patients who underwent operative treatment for acetatabular fractures showed an overall male prevalence of 70%. The mechanism of injury was more frequently related to a fall (54%) than to a road traffic accident (34.9%). Complex fractures were reported in 70.1% of the cases. The incidence of ACPHT (24.9%) fractures and BC (21.5%) fractures was substantially higher than that previously reported for acetabular fractures at all ages.26,27
Femoral head injury was reported in 10.7% of the cases; this incidence rate was also higher than previously reported in the literature.26,27
The likelihood of obtaining an anatomical reduction with ORIF was only 50% which compares unfavourably with 74%28 and 75%27 in two recently published series on young patients.
The rate of ORIF conversion to THA in this study was 17% at a mean of 27.7 months, which is far higher than the 8.5% quoted in the literature on the treatment of acetabular fractures in all age groups.26
In our review, the analysis of intra-operative parameters showed statistical differences (p < 0.001) between the two sub-groups; the mean operating time was shorter in the THA sub-group (236.6 mins ORIF vs 178.4 mins THA); and the mean blood loss was lower in the ORIF sub-group (707 mL ORIF vs 974 mL THA).
In the ORIF sub-group, mean mortality rate at one year was 22%, higher than the 3% detected in younger patients (mean age 38.6; sd 4.6) treated with ORIF.26
In the THA sub-group, the mean mortality rate of 8.8% at one year was significantly lower (p = 0.018) compared with the ORIF sub-group.
The mortality benefit associated with the THA procedure in elderly patients might be explained by the early weight-bearing (on average six weeks after THA), as it is with proximal femoral fracture.29
On the other hand, the rate of peri-operative non-fatal complications in both sub-groups was more than 30%, similar to the one in patients with femoral neck fractures in the same age group.30
Among all the studies, there was a wide heterogeneity of functional scores, and this made comparison of the clinical outcomes difficult. In the ORIF sub-groups, the mean Merle D’Aubigné-Postel score was 16 points which is comparable with the mean 16.8 points reported in a review by Giannoudis et al26 which analysed the clinical results in young patients.
The analysis of the functional results assessed with the HHS demonstrated a mean of 74.5% satisfactory results but no statistical difference (p = 0.79) between the ORIF sub-group (85.8 points) and the THA sub-group (82.5 points).
According to the outcomes reported in this review, the acute THA (alone or in combination with internal fixation) may have a definite role in the treatment of elderly patients with complex acetabular fractures. In this group of patients, THA was associated with a shorter operating time, lower rates of mortality and delayed surgery.
The main concern when performing a THA for an acute acetabular fracture is acetabular component fixation. In the THA sub-group, an acetabular ring or cage with a cemented acetabular component was used in four studies (52 patients) and a cementless acetabular component was implanted in five studies (78 patients). Six cases (4.6%) of acetabular component revisions were reported at a mean of 39 months’ follow-up.
Several limitations were recognised in this review. All the studies identified for analysis were case series and therefore lacked a control group. Publication bias is an inherent risk in this type of review, and it might be reflected in only 15 studies included. The cumulative sample size was not very large because most trials included relatively few acetabular fractures. This was especially true for the sub-group analyses (ORIF and IF + THA). The absence of a significant difference in functional results between the two sub-groups may be the result of heterogeneity in the evaluation and the follow-up when the different forms of treatment were compared.
This systematic review of ORIF/IF + THA treatments for acetabular fractures has confirmed that older patients have worse outcomes than younger patients.
Open reduction and internal fixation remains the treatment of choice for displaced acetabular fractures but there is a recognised subset of patients where an acute hip arthroplasty could be considered as a valid treatment option. This may be due to patient factors (increasing age, osteoporosis) or fracture patterns (complex fracture with dome comminution, femoral head injury) which are considered as poor prognostic factors for treatment by ORIF.3
THA performed in an acute setting after an acetabular fracture yields good clinical results, but this procedure can be substantially more complex in comparison with primary THA.
It is difficult to define guidelines for the surgical treatment of acetabular fractures in elderly patients with no direct comparison of any type of treatment. The evidence on outcomes presented in this review may help orthopaedic surgeons in their decision-making. More studies and better-designed trials are needed in order to improve the evidence and to draw stronger conclusions about the role of acute THA in the treatment of complex acetabular fractures.
Footnotes
ICMJE Conflict of interest statement: None.
Funding Statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Kannus P, Palvanen M, Niemi S, Parkkari J, Järvinen M. Epidemiology of osteoporotic pelvic fractures in elderly people in Finland: sharp increase in 1970-1997 and alarming projections for the new millennium. Osteoporos Int 2000;11:443-448. [DOI] [PubMed] [Google Scholar]
- 2. Laird A, Keating JF. Acetabular fractures: a 16-year prospective epidemiological study. J Bone Joint Surg [Br] 2005;87-B:969-973. [DOI] [PubMed] [Google Scholar]
- 3. Ferguson TA, Patel R, Bhandari M, Matta JM. Fractures of the acetabulum in patients aged 60 years and older: an epidemiological and radiological study. J Bone Joint Surg [Br] 2010;92-B:250-257. [DOI] [PubMed] [Google Scholar]
- 4. Pagenkopf E, Grose A, Partal G, Helfet DL. Acetabular fractures in the elderly: treatment recommendations. HSS J 2006;2:161-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tidermark J, Blomfeldt R, Ponzer S, Söderqvist A, Törnkvist H. Primary total hip arthroplasty with a Burch-Schneider antiprotrusion cage and autologous bone grafting for acetabular fractures in elderly patients. J Orthop Trauma 2003;17:193-197. [DOI] [PubMed] [Google Scholar]
- 6. Borens O, Wettstein M, Garofalo R, et al. Die Behandlung von Acetabulumfrakturen bei geriatrischen Patienten mittels modifizierter Kabelcerclage und primärer Hüfttotalprothese. Erste Ergebnisse. Unfallchirurg 2004;107:1050-1056. (In German) [DOI] [PubMed] [Google Scholar]
- 7. Kinik H, Armangil M. Extensile triradiate approach in the management of combined acetabular fractures. Arch Orthop Trauma Surg 2004;124:476-482. [DOI] [PubMed] [Google Scholar]
- 8. Cochu G, Mabit C, Gougam T, et al. L’arthroplastie totale de hanche dans le traitement des fractures récentes de l’acétabulum du sujet âgé. Rev Chir Orthop Repar Appar Mot 2007;93:818-827. (In French) [DOI] [PubMed] [Google Scholar]
- 9. Boraiah S, Ragsdale M, Achor T, Zelicof S, Asprinio DE. Open reduction internal fixation and primary total hip arthroplasty of selected acetabular fractures. J Orthop Trauma 2009;23:243-248. [DOI] [PubMed] [Google Scholar]
- 10. Herscovici D, Jr, Lindvall E, Bolhofner B, Scaduto JM. The combined hip procedure: open reduction internal fixation combined with total hip arthroplasty for the management of acetabular fractures in the elderly. J Orthop Trauma 2010;24:291-296. [DOI] [PubMed] [Google Scholar]
- 11. Laflamme GY, Hebert-Davies J, Rouleau D, Benoit B, Leduc S. Internal fixation of osteopenic acetabular fractures involving the quadrilateral plate. Injury 2011;42:1130-1134. [DOI] [PubMed] [Google Scholar]
- 12. Jeffcoat DM, Carroll EA, Huber FG, et al. Operative treatment of acetabular fractures in an older population through a limited ilioinguinal approach. J Orthop Trauma 2012;26:284-289. [DOI] [PubMed] [Google Scholar]
- 13. Archdeacon MT, Kazemi N, Collinge C, Budde B, Schnell S. Treatment of protrusio fractures of the acetabulum in patients 70 years and older. J Orthop Trauma 2013;27:256-261. [DOI] [PubMed] [Google Scholar]
- 14. Bastian JD, Tannast M, Siebenrock KA, Keel MJ. Mid-term results in relation to age and analysis of predictive factors after fixation of acetabular fractures using the modified Stoppa approach. Injury 2013;44:1793-1798. [DOI] [PubMed] [Google Scholar]
- 15. Malhotra R, Singh DP, Jain V, Kumar V, Singh R. Acute total hip arthroplasty in acetabular fractures in the elderly using the Octopus System: mid term to long term follow-up. J Arthroplasty 2013;28:1005-1009. [DOI] [PubMed] [Google Scholar]
- 16. Chakravarty R, Toossi N, Katsman A, et al. Percutaneous column fixation and total hip arthroplasty for the treatment of acute acetabular fracture in the elderly. J Arthroplasty 2014;29:817-821. [DOI] [PubMed] [Google Scholar]
- 17. Enocson A, Blomfeldt R. Acetabular fractures in the elderly treated with a primary Burch-Schneider reinforcement ring, autologous bone graft, and a total hip arthroplasty: a prospective study with a 4-year follow-up. J Orthop Trauma 2014;28:330-337. [DOI] [PubMed] [Google Scholar]
- 18. Li YL, Tang YY. Displaced acetabular fractures in the elderly: results after open reduction and internal fixation. Injury 2014;45:1908-1913. [DOI] [PubMed] [Google Scholar]
- 19. O’Toole RV, Hui E, Chandra A, Nascone JW. How often does open reduction and internal fixation of geriatric acetabular fractures lead to hip arthroplasty? J Orthop Trauma 2014;28:148-153. [DOI] [PubMed] [Google Scholar]
- 20. Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD. Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scand J Med Sci Sports 2000;10:2-11. [DOI] [PubMed] [Google Scholar]
- 21. Anglen JO, Burd TA, Hendricks KJ, Harrison P. The “Gull Sign”: a harbinger of failure for internal fixation of geriatric acetabular fractures. J Orthop Trauma 2003;17:625-634. [DOI] [PubMed] [Google Scholar]
- 22. d’Aubigne RM, Postel M. Functional results of hip arthroplasty with acrylic porsthesis. J Bone Joint Surg [Am] 1954;36-A:451-475. [PubMed] [Google Scholar]
- 23. Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg [Am] 1969;51-A:737-755. [PubMed] [Google Scholar]
- 24. Matta JM. Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg [Am] 1996;78-A:1632-1645. [PubMed] [Google Scholar]
- 25. Brooker AF, Bowerman JW, Robinson RA, Riley LH., Jr. Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg [Am] 1973;55-A:1629-1632. [PubMed] [Google Scholar]
- 26. Giannoudis PV, Grotz MR, Papakostidis C, Dinopoulos H. Operative treatment of displaced fractures of the acetabulum. A meta-analysis. J Bone Joint Surg [Br] 2005;87-B:2-9. [PubMed] [Google Scholar]
- 27. Briffa N, Pearce R, Hill AM, Bircher M. Outcomes of acetabular fracture fixation with ten years’ follow-up. J Bone Joint Surg [Br] 2011;93-B:229-236. [DOI] [PubMed] [Google Scholar]
- 28. Tannast M, Najibi S, Matta JM. Two to twenty-year survivorship of the hip in 810 patients with operatively treated acetabular fractures. J Bone Joint Surg [Am] 2012;94-A:1559-1567. [DOI] [PubMed] [Google Scholar]
- 29. Gary JL, Paryavi E, Gibbons SD, et al. Effect of surgical treatment on mortality after acetabular fracture in the elderly: a multicenter study of 454 patients. J Orthop Trauma 2015;29:202-208. [DOI] [PubMed] [Google Scholar]
- 30. Roche JJ, Wenn RT, Sahota O, Moran CG. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ 2005;331:1374. [DOI] [PMC free article] [PubMed] [Google Scholar]