Abstract
The aims of spinal deformity surgery are to achieve balance, relieve pain and prevent recurrence or worsening of the deformity.
The main types of osteotomies are the Smith-Petersen osteotomy (SPO), pedicle subtraction osteotomy (PSO), bone-disc-bone osteotomy (BDBO) and vertebral column resection (VCR), in order of increasing complexity.
SPO is a posterior column osteotomy in which the posterior ligaments and the facet joints are removed and correction is performed through the disc space. A mobile anterior disc is essential. SPO is best in patients with +6-8 cm C7 plumbline. The amount of correction is 9.3° to 10.7°/level (1°/mm bone).
PSO is a technique where the posterior elements and pedicles are removed. Then a triangular wedge through the pedicles is removed and the posterior spine is shortened using the anterior cortex as a hinge. The ideal candidates are patients with a severe sagittal imbalance. A single level osteotomy can produce 30° 40° of correction. A single level osteotomy may restore global sagittal balance by an average of 9 cm with an upper limit of 19 cm.
BDBO is an osteotomy done above and below a disc level. A BDBO provides correction rates in the range of 35° to 60°. The main indications are deformities with the disc space as the apex and severe sagittal plane deformities.
VCR is indicated for rigid multi-planar deformities, sharp angulated deformities, hemivertebra resections, resectable spinal tumours, post-traumatic deformities and spondyloptosis. The main indication for a VCR is fixed coronal plane deformity.
The type of osteotomy must be chosen mainly according to the aetiology, type and apex of the deformity. One may start with SPOs and may gradually advance to complex osteotomies.
Cite this article: EFORT Open Rev 2017;2:73-82.
DOI: 10.1302/2058-5241.2.160069
Introduction
Spinal deformity is a term to describe pathological curvatures of the spine in the sagittal and coronal planes. Deformity can occur in all age groups regardless of age or gender.
In older patients, pain and neurological symptoms are present, whereas in young patients, the main concern may be cosmetic.
In both patient groups, however, the aim of surgery is to achieve balance, relieve pain and prevent recurrence or worsening of the deformity.
With advances in new techniques/instrumentation and neuro-monitorisation supported with improved anaesthetic care, osteotomy techniques have evolved.
Spinal osteotomies are generally needed when the deformity is not correctable with the use of instrumentation alone or when facet or ligament releases are insufficient to gain enough flexibility.
Although osteotomies originally began as anteroposterior procedures, posterior-only procedures have gained wider acceptance in recent years. Osteotomy was a luxury in the past, applicable in only a few select spine centres. Nowadays even complex osteotomies can be performed on a daily basis in many centres thanks to increased numbers of courses and fellowships which have increased the level of competence of more spinal surgeons.
The main types of osteotomies are the Smith-Petersen osteotomy (SPO), pedicle subtraction osteotomy (PSO), bone-disc-bone osteotomy (BDBO) and vertebral column resection (VCR), in order of increasing complexity.
Below is a review of each osteotomy type with indications, limits and pitfalls.
Smith-Petersen osteotomy
The SPO is a posterior column osteotomy in which the posterior ligaments (supraspinous, intra-spinous ligaments and ligamentum flavum) and the facet joints are removed and correction is performed through the disc space. A mobile anterior disc is essential to benefit from this procedure. Both coronal and sagittal correction can be achieved. This procedure was first described by Smith- Petersen in 1945 (Figs 1 and 2).1 In 1984, Ponte described a very similar technique in Scheuermann’s kyphosis cases.2
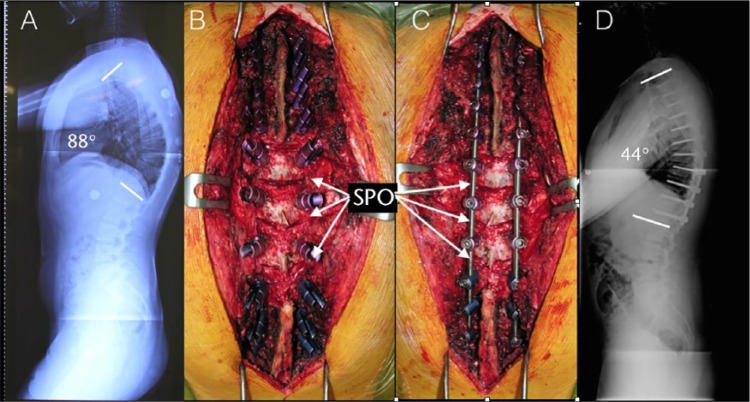
Fig. 1.
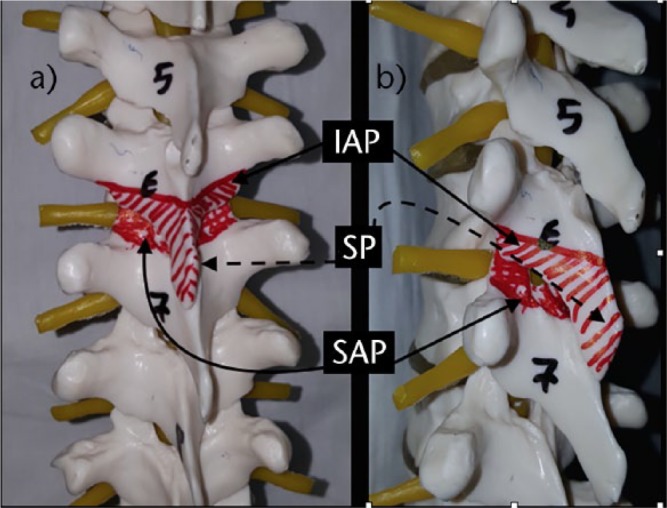
Smith-Petersen osteotomy. a) Spine from posterior view. The spinous process and facets of the upper vertebra are removed in addition to the superior facets of the inferior vertebra. The areas to be removed are painted in red. b) Spine from the lateral view. The areas to be resected are painted in red. the correction is based on the movement of the disc space. IAP, inferior articular process of the superior vertebra; SP, spinous process; SAP, superior articular process of the inferior vertebra.
Fig. 2.
Smith-Petersen osteotomies in a Scheuermann’s kyphosis patient. a) A 19-year-old male patient with Scheuermann’s kyphosis. Lateral radiograph. Thoracic kyphosis is 88°. b) Intra-operative view of T6-7, T7-8, T8-9, T9-10 Smith Petersen osteotomies. c) Intra-operative view after correction and stabilisation procedure. Note that the osteotomy sites were closed under compression. d) Lateral post-operative radiograph. The kyphosis angle is 44° after correction.
SPO, Smith-Petersen osteotomy.
Indications
SPO is indicated in both coronal and sagittal plane deformities.
When the surgeon is not familiar with the more extensile surgical procedures such as PSO, VCR or BDBO, the SPO is the least complicated procedure which can be applied by a surgeon.
Limits
Pitfalls
Epidural bleeding: profuse bleeding from the epidural space can occur during either ligamentectomy or facetectomy (especially during removal of the superior facet of the inferior vertebra). Packing with gelatin sponges usually solves this problem if bipolar cautery does not. Care must be taken not to pack in too much sponge to prevent cord compression.
Neural impingement: removal of facets and compression to correct kyphosis leads to a decrease in foraminal height. This may lead to nerve root impingement. A wide facetectomy can solve this problem if neurological abnormalities are seen on the neuromonitor.4
In some cases, if substantial correction is achieved with an extensive SPO opening anterior disc level (greater than 10 mm in height), it may be necessary to graft the disc space anteriorly.3
There are studies in the literature reporting coronal decompensation with SPO.6 A trapezoidal wedge-type resection or performing SPOs at neutral and stable vertebral segments have been suggested by the authors to prevent decompensation.6
Pedicle subtraction osteotomy
PSO is a technique where posterior elements and pedicles are removed, and a triangular wedge through the pedicles is removed either with a de-cancellation technique or an osteotome. The posterior spine is shortened by closing the osteotomy using the anterior cortex as a hinge (Fig. 3).
Fig. 3.
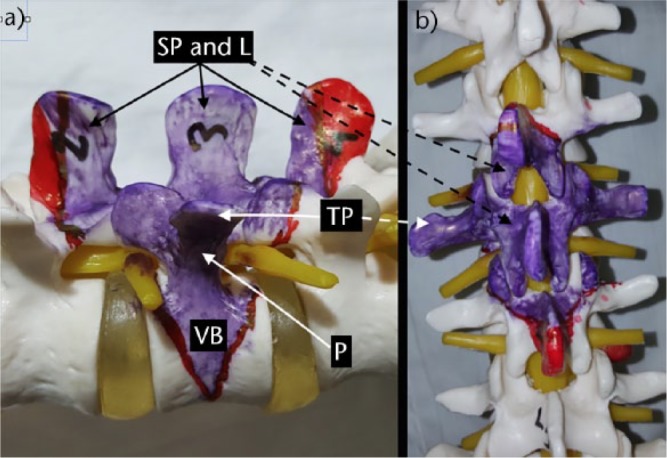
Pedicle subtraction osteotomy. a) An L3 pedicle subtraction osteotomy plan from the lateral view. Note that a wedge reaching to, but not crossing, the anterior cortex is to be removed. The parts of the laminae painted in red may be preserved if they do not interfere with closure of the osteotomy gap. b) While planning an osteotomy, laminectomy of the upper and lower vertebrae should be done to prevent buckling of the spinal cord after correction of the deformity. Again, the area painted in red may not be removed if enough decompression is done and these structures do not prevent closure of the osteotomy. SP, spinous process; L, lamina; TP, transverse process; VB, vertebral body; P, pedicle.
This was first described in 1985 first by Thomasen et al and Heining et al with small technical differences.7,8 Heining suggested resection of the vertebral body with the ‘eggshell’ technique, while Thomasen suggested removal of the bone using an osteotome (Fig. 4).8
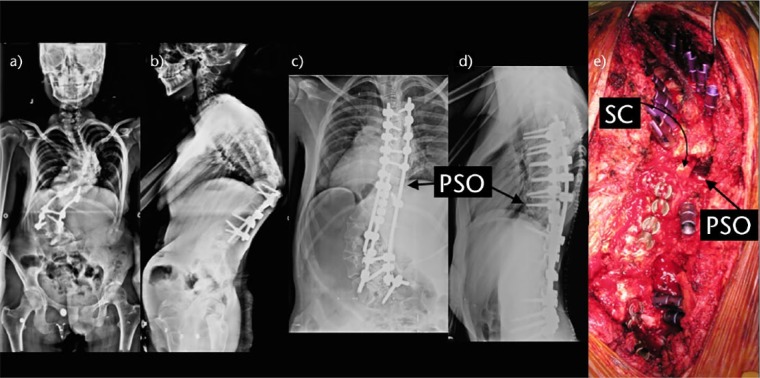
Fig. 4.
Pedicle subtraction osteotomy in revision scoliosis surgery. a, b) Anteroposterior (AP) and lateral views of a 21-year-old female patient who had undergone a previously unsuccessful fusion operation. She presented with both a severe scoliosis and also decompensated kyphosis. The dotted white line represents the planned osteotomy. c, d) AP and lateral views after surgery. There was a significant correction of both coronal and sagittal balance. The osteotomy sites are shown with black arrows. e) Intra-operative view of an asymmetric T10 pedicle subtraction osteotomy and instrumentation. Spinal cord and osteotomy site are shown with black arrows. SC, spinal cord; PSO, pedicle subtraction osteotomy.
Indications
PSO can be used to correct deformities in both the coronal and the sagittal planes.9 It can even be used in patients with a previous 360° fusion of the spine.
There are various aetiologies of fixed sagittal plane deformity. These include ankylosing spondilytis, iatrogenic deformities like ‘flatback’ syndrome10 and kyphotic decompensation syndrome.11
Lumbar kyphosis may originate from congenital anomalies, trauma and metabolic or neoplastic disease with pathological fracture, spondylitis or from iatrogenic causes (Fig. 4).
The ideal candidates for PSO are patients with type 2 sagittal deformity and a substantial sagittal imbalance more than 12 cm (SVA > 12 cm) with a sharp, angular kyphosis, and those patients who have circumferential fusion over multiple segments, which would preclude performing SPOs. A PSO can also be done in areas of rotation and prior laminectomy, but this may lead to an increased complication rate and is technically demanding. If the patient has a type 1 coronal and type 2 sagittal imbalance, PSO can be performed asymmetrically with a more aggressive resection on one side, which categorises the osteotomy between a standard PSO and a VCR.3
PSO is most useful if done at the apex of the deformity. Although originally defined in the lumbar spine, the technique can be used in all regions of the spine above or below the conus including cervical and thoracic areas. While the posterior and middle columns shorten, this osteotomy does not lengthen the anterior column, does not create an anterior bone defect and provides a more stable correction.
A lumbar pedicle subtraction osteotomy may be used in patients both with open or fused disc spaces. However, in patients with open disc spaces, combined anteroposterior (AP) approaches or posteriorly based osteotomies such as SPO can be used.12,13
Normal sagittal alignment of the spine follows a vertical axis from the centre of C2, in front of T7, behind L3 and to the posterior margin of the sacrum.11 Forward displacement of C7 in relation to the pelvis may be caused by deformity in the cervical, thoracic or lumbar regions or fixed hip flexion.
The amount of correction from a single level PSO can be calculated using a 36-inch lateral standing whole spine radiograph. A template can be created using three segments above and below the level of planned osteotomy. The anterior column is intact and the posterior column is shortened in this technique; hence, the wedge including the pedicle can be cut off this template. Using this technique, the position of the spine after surgery can be estimated. The goal of this surgery is to place the centre of C7 over the posterosuperior aspect of S1 vertebral body so that a plumbline passes through both.
Key points in the surgical technique:
Positioning
The patient is positioned prone, typically on a four-poster frame. However, when the kyphosis is severe (the patient does not sit comfortably on a four-poster frame), then two separate posts may be used to position the patient (Fig. 5).
Fig. 5.

Patient positioning in a severe kyphosis patient. In severe kyphosis, instead of using a four-poster frame, two separate posts (P in the picture) can be used. In this case, one post was placed under the sternum and the other was placed under the pelvis. Please note that the operating table was also bent to comply with the global kyphosis of the patient. P.
Special care must be taken to prevent pressure on bony prominences like the pelvis, knees, toe tips, elbows and eyes.
Excessive pressure on the chin or forehead may lead to cervical fractures in completely fused spines of ankylosing spondylitis patients and this should be kept in mind while placing the patient.
Surgical approach
The approach is typical. After performing the exposure of the spine, anatomical landmarks should be identified. This is especially important in revision surgeries with a previous fusion.
Instrumentation
Instrumentation should be done before any osteotomy attempt. This should be followed by laminectomy. Standard pedicle screws are used at least three levels above and below the level of osteotomy. If there is a thick fusion mass, and the anatomical landmarks are obscure, then screws or hooks can be placed in the fusion mass.
The extent of laminectomy
This should be one level above and below the previously planned osteotomy level. This is important to prevent buckling of the spinal cord. Normally, for a one-level resection procedure, a posterior column laminectomy will result in a 5 to 6 cm exposure of the dura and neural elements. Buckling becomes a more severe problem, especially in cases where a previous laminectomy or laminotomy has been done and there is peridural fibrosis which prevents the gliding movement of the dura as the osteotomy gap is closed.
In addition to extending the laminectomy, laminar undercutting should be done to widen the spinal canal from within, again to prevent infolding of ligamentum flavum and bony surfaces.
Osteotomy
After completion of laminectomies, all or half of the transverse processes should be removed to gain access to the lateral aspect of the vertebral bodies. Then half of the inferior articular process of the upper vertebra and half of the superior articular process of the lower vertebra can be removed to help create a single foramen to accommodate two nerve roots after completion of the procedure. After defining the foramen above and below the pedicles to be excised, the nerve roots with their perineural fat tissue should be protected with a dural retractor. Then the pedicles on both sides can be removed using an osteotome or a burr.
The body can then be removed in a wedge-shaped fashion either using the ‘eggshell’ technique or using an osteotome. A transient rod is placed to prevent sudden collapsing of the spine during these manoeuvres. Classically, a unilateral rod is used; however, in severe angular kyphotic or kyphoscoliotic deformities, bilateral rods are recommended to prevent spinal subluxation. The posterior cortex is finally removed before closure of the osteotomy and after the osteotomy is completed including the lateral walls of the vertebral body. The nuts holding the transient rod are loosened and the osteotomy gap is closed by bending the operating table opposite the deformity.
Fixation
The rods should be angulated acutely at the level of osteotomy and should sit freely in the grooves of the screw heads. Otherwise, when there is a fused spine above and below the osteotomy line, as in ankylosing spondylitis or previous fusion cases, as the rod is not as acutely angulated as the spine, it does not sit into the grooves and pulls the screws just above and below the osteotomy line and causes loss of correction.
Limits
It is claimed that PSO increases regional lumbar lordosis by 30° and may be used to increase the lordosis up to 60°. It is accepted that depending on the level and extent of resection, a single-level osteotomy can lead to 30° to 40° of correction. Cho et al used PSO in 41 patients and reported an average correction of 31.7°.6
A single level osteotomy at L3 may restore global sagittal balance by an average of 9 cm with an upper limit of 19 cm. If more correction is needed, the osteotomy level can be changed to L4, or in some cases a two-level osteotomy may be planned.11 Kim et al reported an improvement of 11.2 ± 7.2 cm in the sagittal imbalance a correction of 0.48 ± 1.4 cm of the coronal plane in a series of 41 patients.14
In addition to the solution above, when the deformity is kyphotic more than 40° with a coronal imbalance (> 6 to 8 cm), it may be better to use a vertebral column resection instead.15
Pitfalls
Bleeding: up to 2 litres of blood may be lost during a PSO procedure. Cho et al6 compared three levels of SPO with single-level PSO in a series of 71 patients, and found that single-level PSO caused nearly twice as much bleeding than three levels of SPO. The surgeon should be familiar with haemostasis techniques; the use of thrombin-soaked collagen sponges, gelfoam, tranexamic acid, etc. should be kept in mind and these should be ready in the operating room.
Transient neurological deficits have been reported up to 20% of cases with PSO. These include radiculopathy, transient single root weakness and, rarely, cauda equina syndrome. Strict adherence to the abovementioned osteotomy technique, using neuro-monitorisation throughout the procedure, but especially during osteotomy closure, helps decrease these complications. Care must be taken to prevent vertebral translation at the osteotomy level at all costs. Buchowski et al16 showed an intra-operative or post-operative neurological deficit rate of 11.1% (12 of 108 patients), but only 2.8% of deficits were permanent over a ten-year period. Deficits were always unilateral and never proximal to the osteotomy, often did not correspond to the level of osteotomy and were not detected by neuro-monitoring. The incidence of neurological injury in the series of Yang et al17 and Ahn et al18 was 3.6% and 12%, respectively.
Pseudoarthrosis: this is a late complication. Anterior fusion is more likely as the osteotomy is through the cancellous bone. Posterior mid-line fusion is unlikely because of laminectomies. Posterolateral fusion must therefore be done after decorticating transverse processes appropriately. Kim et al15 reported their results in a series of 35 PSOs with five to eight years of follow-up. They observed no significant regional radiological changes between the post-operative second year and final follow-up. Pseudoarthrosis (nine at the thoracolumbar and one at the lumbosacral junction) was identified in ten (29 %) cases, five of which occurred within two years and the others between two and four years post-operatively. In order to avoid pseudarthrosis in a primary case where a PSO is performed, interbody arthrodesis above and below the osteotomy can be carried out. Interbody fusion can be done as either a transforaminal lumbar interbody fısion (TLIF) or an anterior lumbar interbody fusion (ALIF)procedure.19 Laminectomy sites may also be closed with a cortical strut allograft both to increase mid-line fusion and to prevent any dural complications if revision surgery is needed.19
Infection occurs in 4% to 7% of patients. The rate is related to the number of previous surgeries, to previous infection, to blood loss and to prolonged operative time. Underlying co-morbidities like insulin-dependent diabetes mellitus and chronic steroid use and the use of TNF alpha-blockers are also important risk factors for infection.
Bone-disc-bone osteotomy
BDBO is an osteotomy done both above and below a disc level and the resection includes the disc with its adjacent end-plate(s). A BDBO typically provides correction rates in the range of 35° to 60°.
Surgical technique
Pedicle screws are placed at least two levels below and three levels above the planned osteotomy level, followed by wide laminectomies of the vertebrae above and below the disc space planned to be resected. A wedge osteotomy including the disc end-plate(s) with or without the pedicle(s) is then performed and the wedge including the disc is removed. A titanium mesh cage can be placed anteriorly if lengthening of the anterior column is desired. Finally, the osteotomy site is closed bone-to-bone to decrease the risk of pseudoarthrosis (Fig. 6).
Fig. 6.
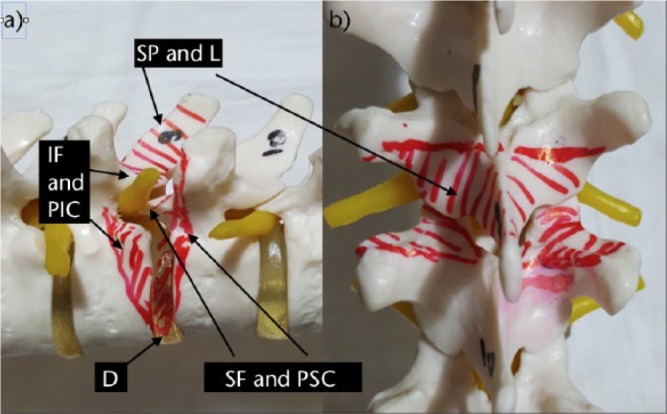
Bone-disc-bone osteotomy. a) Spine from the lateral view. Upper end-plate of T10 and lower end-plate of T9 were included in the area to be resected. Resection should also include the disc space. Closure of the osteotomy allows bone-to-bone contact and direct bone healing. b) Spine from the posterior view. Lower facets and spinous process of the upper vertebra and upper facets of the lower vertebra should be removed to gain access to the area to be resected. SP, spinous process; L, lamina; IF, inferior facet; SF, superior facet; PIC, postero-inferior corner; PSC, posterosuperior corner; D, disc.
The advantages of BDBO compared with PSO include: correction of the deformity at its apex (CORA), especially when the apex is at the disc space; comparable correction rates; potential decrease in pseudoarthrosis rate due to disc removal; and better stability in type 1 osteotomies since there are four pedicle screws close to the osteotomy site (there are three types of BDBO).19,20
Indications
The main indications are deformities with the disc space as the apex or centre of the rotational axis (CORA) and severe sagittal plane deformities that necessitate correction rates exceeding those that a simple PSO can provide.
Limits
Although Ozturk et al suggested that the major advantage of BDBO compared with posterior-only VCR (PVCR) is applicability at the lumbar spine without sacrificing the nerve roots while providing correction rates closer to PVCR, we are not sure if this is accountable as we do not need to sacrifice nerve roots while doing PVCR.20
In a series of 12 patients with kyphosis and kyphoscoliosis deformity, Ozturk et al reported an average correction of 38° in the sagittal plane without any neurological injury or pseudoarthrosis during a two-year follow-up after BDBO.20 Domanic et al21 reported an average correction of 49° with BDBO in a group of patients who had severe rigid kyphotic deformities.
A BDBO may be impossible or hard to apply in ankylosing spondilitis patients when the anterior annulus is calcified or ossified. Aetiology must be kept in mind when selecting the type of osteotomy.
Pitfalls
Although not reported before, a BDBO may theoretically be complicated with damage to the vascular structures especially when an anterior lengthening is done through the disc space.
In BDBO type 2 or 3, the abovementioned advantage of four pedicle screws close to the osteotomy site is not present. In that case, the number of instrumented levels may be increased.
As in all new techniques, this technique too should be worked on before it is possible to achieve the claimed degrees of correction.
Vertebral column resection
The use of a vertebrectomy procedure has been practised for some time, with the first description in 1922 by MacLennan,22 who described a posterior apical resection followed by post-operative casting for the treatment of severe scoliosis. Following that, several authors recorded their experiences with vertebrectomies, most commonly for the surgical treatment of congenital scoliosis.23-30 Performing a circumferential VCR approach for severe, rigid spinal deformity was first described by Bradford in the late 1980s (Fig. 7).31 He was the first to describe the use of a circumferential vertebral column resection coupled with concave rib osteotomies, convex thoracoplasty and segmental spinal instrumentation with fusion in 13 patients with severe structural spinal deformities. The patients underwent a level 1 to 7 (average three levels) vertebrectomy. Scoliosis patients had a pre-operative curve averaging 117°, correcting to an average 55°. Kyphosis patients had a pre-operative curve averaging 112°, correcting to an average 56°. The average estimated blood loss was 5800 cc, and the average operative time was 10.5 hours for these combined procedures.
Fig. 7.
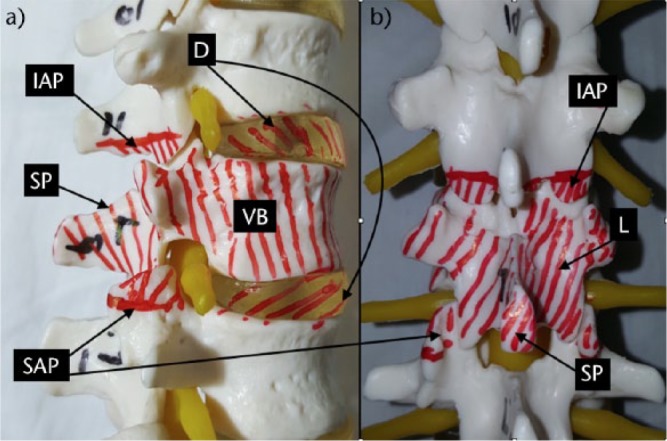
Vertebral column resection. a) Lateral view. Lower facets of the upper and upper facets of the lower vertebrae should be removed to allow removal of the laminae and pedicles of the vertebra to be resected. Discs should also be resected and this should be followed by end-plate preparation for a successful fusion. b) AP view of the anatomical structures to be resected during a PVCR operation. IAP, inferior articular process; D, disc; SP, spinous process; SAP, superior articular process; VB, vertebral body; L, lamina.
Bradford and Tribus23 later reported on 24 patients with rigid coronal decompensation who underwent a circumferential VCR. The average pre-operative scoliosis was 103°, corrected by 52%. Importantly, coronal and sagittal imbalances were corrected to an average of 82% and 87%, respectively. However, there was an average operative time of over 12 hours, an average blood loss of 5500 mL and 31 overall complications.
In 1997, Boachie-Adjei15 further expanded on Bradford’s original case series and reported 16 patients undergoing circumferential VCR. Excellent deformity correction and rebalancing of the trunk was reported with few serious complications.
Suk was the first investigator to promote a PVCR. He believed that there was a reduction in the total operating time and the amount of blood loss through this one-stage posterior-only procedure. In 2005, he presented a series of 16 patients (average age 29 years) who underwent a PVCR having a minimum two-year follow-up.32 His indication for this procedure was scoliosis of more than 80° with flexibility less than 25%. There was an average of 1.3 vertebrae removed, 15 in the thoracic spine and six in the lumbar spine. The mean pre-operative scoliosis of 109° was corrected to 46° (59% correction). However, complications were encountered in four patients, including one with complete permanent paralysis. He recommended this as an effective alternative for severe rigid scoliosis but cautioned that it was a highly technical procedure and should only be performed by an experienced surgical team. It is important to note that he did not use any form of motor tract monitoring during the surgeries, only Somato-sensory evoked potentialsmonitoring.
Lenke reported on 43 consecutive patients undergoing PVCR for severe paediatric and adult spinal deformity. The indications for the procedure were divided into four main groups: severe scoliosis; global kyphosis; angular kyphosis; and kyphoscoliosis. The severe scoliosis cases had a correction rate of 69%, 54% for the global kyphosis cases, 63% for the angular kyphosis cases and 55% for the combined kyphoscoliosis cases.33
Indications
VCR is indicated for rigid multi-planar deformities, sharp angulated deformities, hemivertebra resections, resectable spinal tumours, post-traumatic deformities and spondyloptosis. The main indication for a vertebral column resection is fixed coronal plane deformity. In these patients, a posteriorly based pedicle subtraction osteotomy or AP procedure is not enough to solve the problem.
In order to achieve balance, the spine must not only be shortened but also translated. This requires resection of the vertebral body. Clinical indications are pain, progression of deformity, neurological and/or functional deficit and cosmesis (Figs 7 and 8).
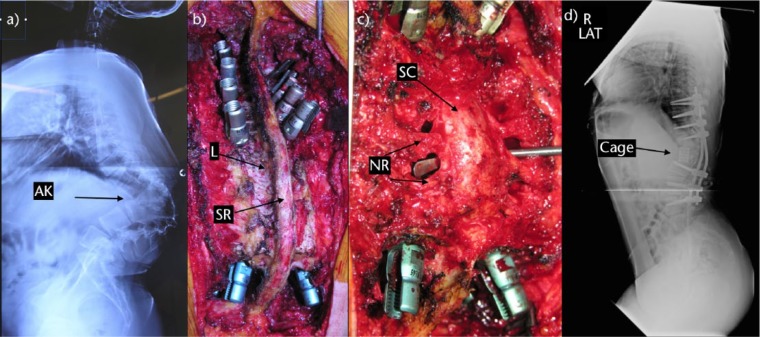
Fig. 8.
a) A 33-year-old woman with congenital kyphosis. b) Intra-operative view of the kyphotic region. c) Intra-operative view of three levels. Vertebral column resection including T11, T12 and L1. d) Post-operative lateral view. AK, apex of kyphosis; L, lamina; SP, spinous process; NR, nerve root; SC, spinal cord.
The most common cause of fixed coronal deformity is post-surgically treated idiopathic scoliosis. Congenital scoliosis or other post-surgical deformities may also lead to fixed coronal deformity.
Vertebral resection is not necessary if the shoulders of the patient are level despite coronal deformity or if coronal balance is complicated by angulation of the shoulders into the convexity of the deformity.
Depending on the familiarity of the surgeon with various techniques, a VCR can be done as an AP procedure or a posterior-only procedure.
Hamzaoglu et al34 reported an average correction rate of 62% in the coronal plane and 72% in the sagittal plane in their series of 102 severe adult deformity patients. Suk et al35 reported a correction of 61.9° in the coronal plane and 45.2° in the sagittal plane in their series of 70 patients. In a series of 35 children, Lenke et al36 noted major curve improvements as 51% in scoliosis cases, 55% in global kyphosis cases, 58% in angular kyphosis cases, 54% in kyphoscoliosis cases and 60% in congenital scoliosis cases after PVCR. The same authors reported another series of PVCR including a slightly larger number of adults and children with severe deformity. Correction rates were 69% for scoliosis, 54% for global kyphosis, 63% for angular kyphosis and 56% for kyphoscoliosis.34-36
Limits
Intra-spinal pathologies
Region to be resected: thoracic, thoracolumbar and lumbar regions require different anterior approaches.
Pitfalls
Placement of the cord: because of vertebral rotation at the apex, especially when doing an anterior corporectomy, even if the canal is identified using the location of the pedicles, the location and direction of the cord is difficult to identify.
All bone anterior to the posterior longitudinal ligament (PLL) must be resected to prevent buckling of the PLL and subsequent anterior compression of the spinal cord.
Neurological deficit: a wide laminectomy should be done including the lower part of the lamina of the upper vertebra and the upper part of the lamina of the lower vertebra. The most common cause is spinal subluxation. This is followed by over-shortening of the anterior column and buckling of the spinal cord. Preventing over-shortening and if a deficit occurs, supporting and lengthening the anterior column by a cage or changing the cage with a longer one, may solve the problem. Maintaining a haemoglobin level > 10 and mean arterial blood pressure of 75 to 80 mmHg is essential.
Neurologic complications may also result from subluxation of the spinal column, dural buckling and compression of the spinal cord by residual bone or soft tissues in the canal after correction. Suk et al35 reported a 34.3% overall rate of complications and a 17.1% rate of neurological complications. Lenke et al36 reported a similar 40% overall rate of complications and a 11.4% rate of neurological complications. Hamzaoglu et al34 reported an overall complication rate of 7.84% including transient nerve palsies in 1.96% of patients.
Spinal instability before reduction: to prevent this, a temporary rod will solve the problem.
Kyphotic deformities carry a higher risk of neurological deficits. Strict and vigilant care is needed.
The demand for more cosmetic outcomes necessitates more degrees of correction. As a result, osteotomies are an integral part of deformity treatment in today’s spinal surgery. All orthopaedic surgeons dealing with spine surgery should gain familiarity with these techniques.
The type of osteotomy must be chosen according to the aetiology, type and apex of the deformity, the experience of the surgeon, the availability of blood and bleeding control agents, and the availability of intensive care. Inexperienced surgeons may start with SPOs and may gradually advance to more complex types of osteotomies.
Footnotes
ICMJE Conflict of Interest Statement: None
Funding
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Smith-Petersen MN, Larson EB, AuFranc OE. Osteotomy of the spine for correction of flexion deformity in rheumatoid arthritis. J Bone Joint Surg [Am] 1945;27-A:1-11. [PubMed] [Google Scholar]
- 2. Ponte A, Vero B, Siccardi GL. Surgical treatment of Scheuermann’s kyphosis. In: Winter RB, ed. Progress in spinal pathology: kyphosis. Bologna: Aulo Gaggi, 1984:75-80. [Google Scholar]
- 3. Bridwell KH. Decision making regarding Smith-Petersen vs. pedicle subtraction osteotomy vs. vertebral column resection for spinal deformity. Spine (Phila Pa 1976) 2006;31:S171-S178. [DOI] [PubMed] [Google Scholar]
- 4. Dorward IG, Lenke LG. Osteotomies in the posterior-only treatment of complex adult spinal deformity: a comparative review. Neurosurg Focus 2010;28:E4. [DOI] [PubMed] [Google Scholar]
- 5. Lafage V, Schwab F, Patel A, Hawkinson N, Farcy JP. Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine (Phila Pa 1976) 2009;34:E599-E606. [DOI] [PubMed] [Google Scholar]
- 6. Cho KJ, Bridwell KH, Lenke LG, Berra A, Baldus C. Comparison of Smith-Petersen versus pedicle subtraction osteotomy for the correction of fixed sagittal imbalance. Spine (Phila Pa 1976) 2005;30:2030-2037. [DOI] [PubMed] [Google Scholar]
- 7. Thomasen E. Vertebral osteotomy for correction of kyphosis in ankylosing spondylitis. Clin Orthop Relat Res 1985;194:142-152. [PubMed] [Google Scholar]
- 8. Heining CA. Eggshell procedure. In: Luque ER, ed. Segmental spinal instrumentation. Thorofare, NJ: Slack, 1984:221-230. [Google Scholar]
- 9. Berven SH, Deviren V, Smith JA, et al. Management of fixed sagittal plane deformity: results of the transpedicular wedge resection osteotomy. Spine (Phila Pa 1976) 2001;26:2036-2043. [DOI] [PubMed] [Google Scholar]
- 10. Doherty J. Complications of fusion in lumbar scoliosis. Proceedings of the Scoliosis Research Society. J Bone Joint Surg [Am] 1973;55-A:438. [Google Scholar]
- 11. Farcy JP, Schwab FJ. Management of flatback and related kyphotic decompensation syndromes. Spine (Phila Pa 1976) 1997;22:2452-2457. [DOI] [PubMed] [Google Scholar]
- 12. Smith-Petersen Carroll B. Larson, Otto E. Aufranc. Osteotomy of the spine for correction of flexion deformity in rheumatoid arthritis. J Bone Joint Surg [Am] 1945;27-A:1-11. [PubMed] [Google Scholar]
- 13. Berven SH, Deviren V, Smith JA, Hu SH, Bradford DS. Management of fixed sagittal plane deformity: outcome of combined anterior and posterior surgery. Spine (Phila Pa 1976) 2003;28:1710-1715. [DOI] [PubMed] [Google Scholar]
- 14. Kim YJ, Bridwell KH, Lenke LG, Cheh G, Baldus C. Results of lumbar pedicle subtraction osteotomies for fixed sagittal imbalance: a minimum 5-year follow-up study. Spine (Phila Pa 1976) 2007;32:2189-2197. [DOI] [PubMed] [Google Scholar]
- 15. Boachie-Adjei O, Bradford DS. Vertebral column resection and arthrodesis for complex spinal deformities. J Spinal Disord 1991;4:193-202. [DOI] [PubMed] [Google Scholar]
- 16. Buchowski JM, Bridwell KH, Lenke LG, et al. Neurologic complications of lumbar pedicle subtraction osteotomy: a 10-year assessment. Spine (Phila Pa 1976) 2007;32:2245-2252. [DOI] [PubMed] [Google Scholar]
- 17. Yang BP, Ondra SL, Chen LA, et al. Clinical and radiographic outcomes of thoracic and lumbar pedicle subtraction osteotomy for fixed sagittal imbalance. J Neurosurg Spine 2006;5:9-17. [DOI] [PubMed] [Google Scholar]
- 18. Ahn UM, Ahn NU, Buchowski JM, et al. Functional outcome and radiographic correction after spinal osteotomy. Spine (Phila Pa 1976) 2002;27:1303-1311. [DOI] [PubMed] [Google Scholar]
- 19. Enercan M, Ozturk C, Kahraman S, et al. Osteotomies/spinal column resections in adult deformity. Eur Spine J 2013;22:S254-S264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ozturk C, Alanay A, Ganiyusufoglu K, et al. Short-term X-ray results of posterior vertebral column resection in severe congenital kyphosis, scoliosis, and kyphoscoliosis. Spine (Phila Pa 1976) 2012;37:1054-1057. [DOI] [PubMed] [Google Scholar]
- 21. Domanic U, Talu U, Dikici F, Hamzaoglu A. Surgical correction of kyphosis: posterior total wedge resection osteotomy in 32 patients. Acta Orthop Scand 2004;75:449-455. [DOI] [PubMed] [Google Scholar]
- 22. MacLennan A. Scoliosis. BMJ 1922;2:864-866. [Google Scholar]
- 23. Bradford DS, Tribus CB. Vertebral column resection for the treatment of rigid coronal decompensation. Spine (Phila Pa 1976) 1997;22:1590-1599. [DOI] [PubMed] [Google Scholar]
- 24. Dick J, Boachie-Adjei O, Wilson M. One-stage versus two-stage anterior and posterior spinal reconstruction in adults. Comparison of outcomes including nutritional status, complications rates, hospital costs, and other factors. Spine (Phila Pa 1976) 1992;17:S310-S316. [DOI] [PubMed] [Google Scholar]
- 25. Herbert JJ. Vertebral osteotomy; technique, indications and results. J Bone Joint Surg [Am] 1948;30-A:680-689. [PubMed] [Google Scholar]
- 26. Johnson JR, Holt RT. Combined use of anterior and posterior surgery for adult scoliosis. Orthop Clin North Am 1988;19:361-370. [PubMed] [Google Scholar]
- 27. Leatherman KD. Resection of vertebral bodies. J Bone Joint Surg [Am] 1969;51-A:206. [Google Scholar]
- 28. Thomasen E. Vertebral osteotomy for correction of kyphosis in ankylosing spondylitis. Clin Orthop Relat Res 1985;194:142-152. [PubMed] [Google Scholar]
- 29. Tokunaga M, Minami S, Kitahara H, et al. Vertebral decancellation for severe scoliosis. Spine (Phila Pa 1976) 2000;25:469-474. [DOI] [PubMed] [Google Scholar]
- 30. Wiles P. Resection of dorsal vertebrae in congenital scoliosis. J Bone Joint Surg [Am] 1951;33-A:151-154. [PubMed] [Google Scholar]
- 31. Bradford DS. Vertebral column resection. Orthop Trans 1987;11:502. [Google Scholar]
- 32. Suk SI, Kim JH, Kim WJ, et al. Posterior vertebral column resection for severe spinal deformities. Spine (Phila Pa 1976) 2002;27:2374-2382. [DOI] [PubMed] [Google Scholar]
- 33. Lenke LG, Sides BA, Koester LA, Hensley M, Blanke KM. Vertebral column resection for the treatment of severe spinal deformity. Clin Orthop Relat Res 2010;468:687-699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hamzaoglu A, Alanay A, Ozturk C, et al. Posterior vertebral column resection in severe spinal deformities: a total of 102 cases. Spine (Phila Pa 1976) 2011;36:E340-E344. [DOI] [PubMed] [Google Scholar]
- 35. Suk SI, Chung ER, Kim JH, et al. Posterior vertebral column resection for severe rigid scoliosis. Spine (Phila Pa 1976) 2005;30:1682-1687. [DOI] [PubMed] [Google Scholar]
- 36. Lenke LG, O’Leary PT, Bridwell KH, et al. Posterior vertebral column resection for severe pediatric deformity: minimum two-year follow-up of thirty-five consecutive patients. Spine (Phila Pa 1976) 2009;34:2213-2221. [DOI] [PubMed] [Google Scholar]