Abstract
Hip arthroscopy is an evolving surgical technique that has recently increased in popularity.
Although femoroacetabular impingement was an important launch pad for this technique, extra-articular pathology has been described through hip endoscopy.
Good clinical results in the medium term will allow improvements in this technique and increase its indications.
Cite this article: EFORT Open Rev 2017;2:58-65. DOI: 10.1302/2058-5241.2.150041
Keywords: hip arthroscopy, femoro-acetabular impingement, labrum
Introduction
Hip arthroscopy has increased in popularity tremendously in the last five to ten years. In a recent cross-sectional study, an increase of 250% was observed with this surgical technique in the United States between 2007 and 2011. The annual frequency of hip arthroscopy was four cases per 10 000 orthopaedic patients in 2011.1 Although femoroacetabular impingement (FAI) is still the main indication for hip arthroscopy, the discovery of other intra-articular and extra-articular entities have increased its frequency. This paper will review the current state of different key points of this surgical technique.
Positioning and portals
Positioning during hip arthroscopy depends on the available system and the experience of the surgeon. Both positions, supine and lateral, offer advantages. The supine position is performed by a larger number of surgeons, because it is the simplest way to start performing hip arthroscopy.2 A classic fracture table can be used and the C-arm positioning is part of the operating room (OR) setup. For central compartment access, axial traction is necessary in abduction followed by adduction of the limb on the oversized perineal post. This forces the hip to dislocate distally and laterally. For peripheral compartment access, which is the first step with some surgeons, the hip is flexed in the range of 30° to 45°. This can be accompanied by removal of the central post to allow easier rotation of the hip while avoiding medial compression. In the lateral position, the advantage is the anatomical orientation for hip surgeons who perform hip replacement in the lateral position but this requires more preparation in the OR to adapt the traction system and the C-arm positioning. The post in both positions should be placed at a width of more than 10 cm to reduce the incidence of neuroapraxis and perineal injury.
The portals have varied according to surgeon’s technique (Fig. 1), whether they start with the peripheral compartment or the central compartment. Fluoroscopy is widely used to establish the first portal although anatomical references can be used to establish this portal without need for the radiographic C-arm.3 For central compartment access first, under traction, a capsulotomy is usually performed between the anterior (A) and anterolateral (AL) portals, parallel to the acetabular surface, to allow easy manoeuvrability inside the hip joint.4 Some surgeons continue this capsulotomy in a T-fashion along the axis of the neck, which allows a ‘bird’s-eye’ view of the hip joint. The posterolateral (PL) portal is not routinely performed but it facilitates the access to the posterior part of the hip down to the 10 o’clock position. The main iatrogenic injury with this portal is damage to the sciatic nerve but it can be very helpful for the removal of posterior loose bodies. The mid-anterior and proximal mid-anterior can be used while working on the peripheral compartment.
Fig. 1.
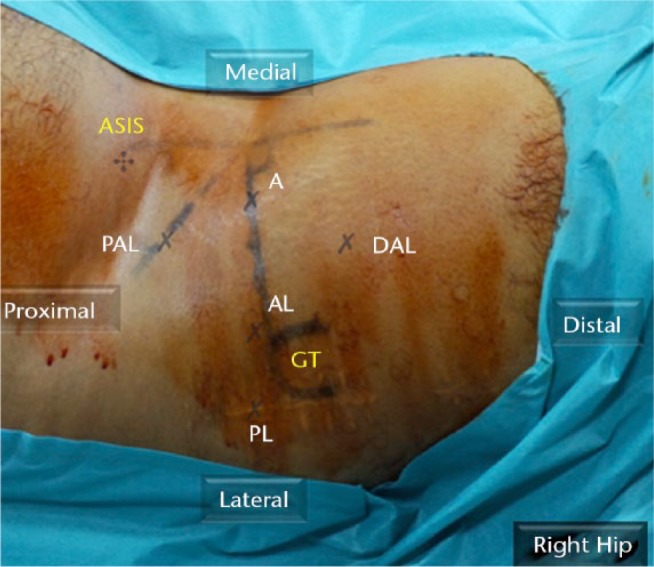
Arthroscopic portals (right hip). ASIS, antero superior iliac spine; GT, greater trochanter; A, anterior portal; AL, anterolateral portal; PL, posterolateral portal; DAL, distal anterolateral portal; PAL, proximal anterolateral portal.
For access to the peripheral compartment as a first approach,5 the proximal anterolateral (PAL) portal or proximal mid-anterior portal (PMAP) are the first portals. These portals should be used for the treatment of lesions at the head-neck junction or other pathologies in the peripheral compartment. A distal anterolateral portal (DAL) or mid-anterior portal (MAP) are useful for work on the lateral and anterolateral neck and are safer portals for anchor placement to avoid penetrating the acetabulum.
A variety of modified portals have been described in the literature. Usually, more lateral portals give better access to the lateral and PL articular lesions. Nevertheless, more anterior portals give better access to the anterior articular pathology, but with higher risk of damage to the lateral femoral cutaneous nerve (LCNT). Distal portals are better used for anchor placement from the 1 o’clock to 3 o’clock positions.6 Medial portals have also been described to access the joint described as anterior, posterior and distal posterior to the adductor longus.7
Management of chondrolabral injury
Hip arthroscopy in young adults frequently reveals a chondrolabral lesion on the articular side. A systematic review study reported a prevalence of labral injury on MRI without intra-articular contrast in 68.1% of hips in an asymptomatic population.8 Fifteen years ago, labral treatment was limited to debridement or resection of this sort of lesion, but today it has progressed towards preservation or restoration of the anatomy and biomechanics as much as possible. Furthermore, revision hip arthroscopy is usually performed due to chondrolabral residual lesions.9 Labral vascularity, with a radial peri-acetabular distribution, explains the need for bony refreshment of the acetabular rim in order to achieve good revascularisation and secure re-fixation.10 Several in vitro and finite-element studies have shown the importance of labral structure in the stability and kinetics of the hip joint. Maintenance of the labral seal and increase of acetabular surface ensure hip stability while increasing contact area and normal pressure distribution. Current clinical studies also support acetabular labral preservation. A randomised clinical study compared resection with labral repair in patients with ‘pincer’ and combined FAI.11 The authors demonstrated better results for function, quality of life and subjective symptoms with labral repair. This study has stronger evidence than papers with historical series or retrospective analyses,12 but they all reported better results with labral repair. Interestingly, the results of labral repair alone are as good as labral re-fixation with acetabular rim resection.13 In cases where the acetabular labrum is irreparable, labral reconstructions are becoming an increasingly satisfactory option14 since there is no re-growth after labral resection.15 Different types of graft can be considered as viable graft options16,17 and some clinical series show promising results but with a lack of conclusive evidence.18,19
After labral lesions, articular cartilage lesions at the anterosuperior acetabular rim are the second most common pathology in patients undergoing hip arthroscopy. When cartilage lesions are left untreated, progression to more generalised degeneration will occur. The current standard of care for the treatment of small chondral defects is microfracture. However, this technique is recognised to be an incomplete solution to deal with these lesions.20,21 When there is a stable well-preserved delaminated flap, fibrin adhesive or chondral sutures have been used to stabilise and preserve the native cartilage.22,23 Unstable flaps and big cartilage defects can be treated with enhanced bone marrow stimulation techniques like BST Cargel,24 AMIC techniques25 or with chondrocyte cultures.26 These are promising techniques but there is still a lack of long-term results (Fig. 2).
Fig. 2.
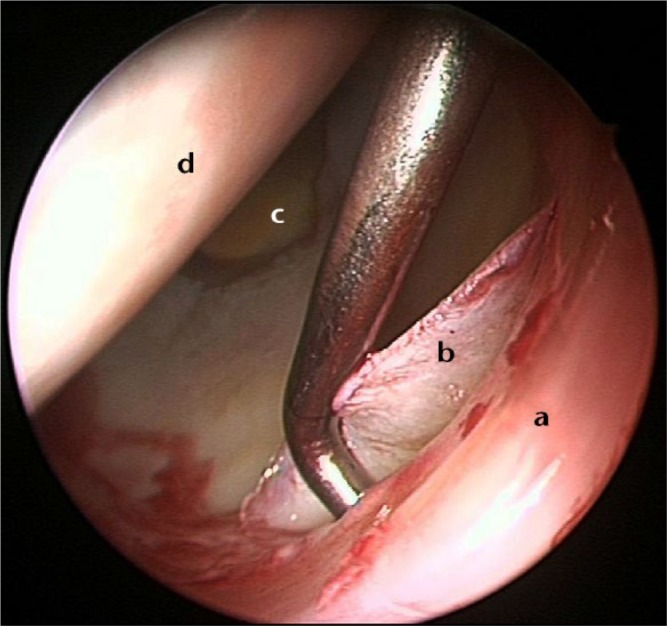
Arthroscopic view from the anterolateral portal (right hip). a) Labrum, b) chondrolabral delamination, c) cotyloid fossa, d) femoral head.
FAI management
The role of FAI as a cause of osteoarthritis of the hip has been related to ‘cam’ type impingement but there is still some concern about ‘pincer’ type impingement.27 Radiological findings of FAI in an asymptomatic population are around 20% and increase up to 60% to 80% in athletes.28 An interesting systematic review of an asymptomatic population established the prevalence of ‘cam’ deformity in 37% and ‘pincer’ deformity in 67%. The authors concluded that the physical examination findings should be carefully correlated with radiological findings.8 As the relationship between FAI and hip osteoarthritis is not clear, the current literature does not show any benefit with prophylactic surgical procedures in the asymptomatic population who have radiological signs of FAI.29
FAI is often related to sports activities that eventually need a hip arthroscopy. In a retrospective study of athletes undergoing hip arthroscopy for FAI, the most common sports related to FAI surgery were hockey, soccer and American football.30 Participating in cutting sports was associated with a younger age group at surgery than other sports. In football players, increasing the ‘alpha’ angle was the only independent predictor of groin pain;31 also, higher ‘alpha’ angles were associated with chondral delamination and labral injuries.32 Return to sport after FAI surgery was investigated in a systematic review of a cohort of 418 athletes, with a rate of return to the previous level of competition of 88%.33
‘Pincer’ deformity was poorly defined (four studies (15%); focal anterior overcoverage, acetabular retroversion, abnormal CEA or acetabular index, coxa profunda, acetabular protrusio, ischial spine sign, cross-over sign and posterior wall sign). Related to these findings, a retrospective study evaluated the progression of 96 asymptomatic hips with radiological signs of FAI. More than 82% remained free of osteoarthritis for a mean period of 18.5 years.34 There is no international consensus about the best parameter to define ‘pincer’ deformity. Different studies have mentioned radiological measures as main definers of the deformity. Although focal anterior overcoverage, acetabular retroversion, abnormal acetabular index, coxa profunda, acetabular protrusio, ischial spine sign, cross-over sign and posterior wall sign are widely described in different studies, their variability casts doubt on their routine use to guide surgical treatment.8,35-37 Correction of a ‘pincer’ type deformity should be performed with acetabular rim trimming. Excessive acetabular rim trimming should be avoided, since 1 mm rim trimming will decrease by approximately 2.4° of the CE angle. Therefore, acetabular rim resections greater than 4 to 5 mm could create an iatrogenic dysplastic hip.38,39 Currently, limited acetabuloplasty and labral re-fixation without detachment have demonstrated the same clinical outcomes as acetabuloplasty with labral detachment in the treatment of ‘pincer’ FAI.40-42
‘Cam’ deformity in FAI appears commonly at the anterosuperior head-neck junction and extends from the medial synovial fold to the anterolateral insertion of the retinacular vessels (Fig. 3). Playing some types of sports, such as football, more than three times a week by patients during skeletal growth was associated with a pathological alpha angle.43,44 Restoration of the normal head-neck shape should be our main goal but clinical outcome is more related to the pre-operative articular damage than the post-operative head-neck shape restoration.45 Rarely, extensive ‘cam’ resection could weaken the femoral neck and lead to a femoral neck fracture. Risk factors associated with this complication are violation of weight-bearing restrictions, female sex and age older than 50 years.46
Fig. 3.
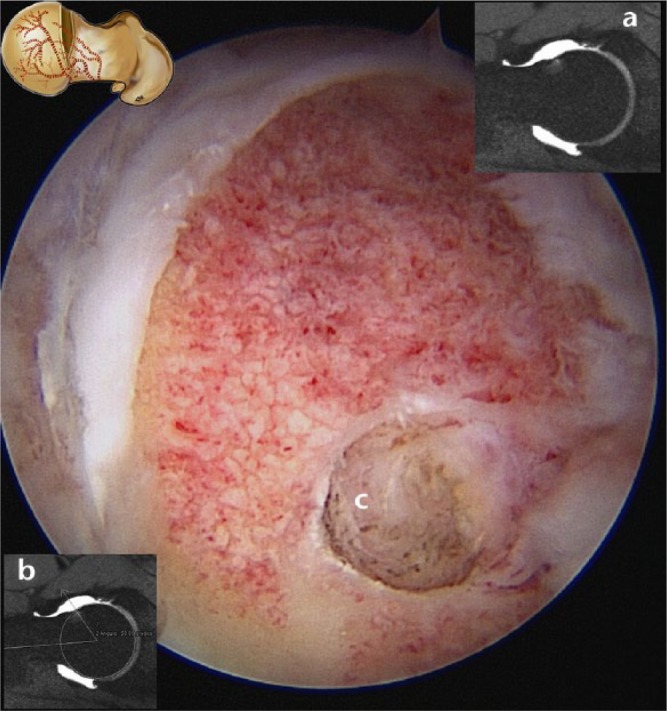
Arthroscopic view from the anterolateral portal (right hip). a) ArthroMRI with a ‘herniation pit’ at the head-neck junction, b) arthroMRI with pathological alpha angle (60°), c) intra-operative view of the ‘herniation pit’ at the head-neck junction after resection of ‘cam’ deformity.
Peripheral compartment pathology often requires extensive capsulotomy that should be anatomically closed at the end of the surgery to avoid iatrogenic instability.47 In recent cadaveric studies, authors demonstrated that larger size capsulotomies significantly increase joint instability and hip external rotation while proper repair restored the normal range of motion and capsule stability.48,49
Quality of life scores improved up to 76.6% at one year in non-arthritic patients who underwent hip arthroscopy for FAI. Curiously, 23.4% remained unchanged or became worse in the same period.50 Although joint space width is the main risk factor, there is a lack of consensus regarding how much joint space is the limit to indicate the need for arthroscopic treatment of FAI in symptomatic patients.51 Hip arthroscopy in patients with FAI and joint space greater than 2 mm is considered a cost-effective intervention.52 FAI arthroscopic treatment showed up to 80% of good or excellent clinical results at the mid-term.53 Even in patients older than 50 years, most patients revealed initial clinical improvement, but 43% underwent a total hip replacement (THR) when less than 2 mm was measured before hip arthroscopy.54,55
Non-articular hip arthroscopy
Based on the development of imaging techniques and further progress in hip arthroscopy instrumentation, extra-articular hip arthroscopy has greatly increased in numbers over the last five years.56 There are several extra-articular space pathologies that predispose to damage of soft tissues around the hip and, eventually, intra-articular structures.
Antero-inferior iliac spine (AIIS) syndrome was described as an impingement between a prominent AIIS and the femoral neck or acetabular labrum (Fig. 4). Arthroscopic sub-spine decompression of 1 to 1.5 cm of the proximal AIIS, associated with the surgical treatment of other FAI findings, should be the elective treatment option.57
Psoas impingement (PI) explains labral tears at the 1 o’clock to 2 o’clock positions for a right hip or the 10 o’clock to 11 o’clock positions for the left hip.58 Patients have impingement between the psoas tendon and the anterior labrum (Fig. 5). Arthroscopic psoas tenotomy is the ‘goal standard’ treatment of this entity. Some authors recommend being cautious in performing psoas tendon tenotomy with borderline dysplasia, in order to avoid anterior instability.59
Most patients with internal snapping hip complain about a ‘sound’ at the medial area of the groin when they move from flexion and external rotation to extension and internal rotation of the hip. It is commonly asymptomatic and typically present in sports that require repetitive hip flexion such as ballet. The patient only rarely experiences severe pain and conservative treatment should be the ‘gold standard’. When conservative options fail, arthroscopic tenotomy of the psoas tendon can relieve the symptoms. Arthroscopic psoas tenotomy can be performed at different levels along the tendon and it has demonstrated better recovery than open surgery.60 Endoscopic iliopsoas tendon release at the level of the lesser trochanter and arthroscopic tenotomy from the central compartment are the two most popular options. Clinical results of both techniques are comparable and selection of one over the other only depends on the surgeon’s preference.61
External ‘snapping’ hip is a cause of trochanteric pain due to the friction between the iliotibial band and the trochanter. If conservative management fails, arthroscopic surgical release or lengthening of the iliotibial band is a good option. This technique also provides good access to the abductor tendons when damage is suspected.62
Gluteus medius and minimus tears can be a common cause of greater trochanteric pain syndrome (GTPS). Patients are usually female with trochanteric bursitis and partial abductor tears.63 Open or arthroscopic repair provides good clinical results (Fig. 6). Open surgery seems to have higher post-operative complications64,65 but takes less operative time for full thickness tears.66
- Deep gluteal syndrome (DGS) is an underdiagnosed entity characterised by pain and dysaesthesia in the buttock area, posterior thigh and radicular pain due to a non-discogenic sciatic nerve entrapment in the subgluteal space. Multiple pathologies have been incorporated into the term ‘piriformis syndrome’, a term related to the presence of fibrous bands, obturator internus syndrome, ischiofemoral pathology, hamstring conditions and gluteal disorders. Clinical assessment of patients with DGS is difficult since the symptoms are imprecise and may be confused with other lumbar and intra- or extra-articular hip diseases. It is usually characterised by a set of symptoms occurring in isolation or in combination.67 Intolerance of sitting for more than 20 to 30 minutes, limping, disturbed or loss of sensation in the affected extremity and pain at night getting better during the day are other symptoms reported by patients. The concept of fibrous bands playing a role in causing symptoms related to sciatic nerve mobility and entrapment represents a radical change in the current diagnosis of and therapeutic approach to DGS. Recently, a new pathological classification of these bands has been published:68
- Type 1: compressive or bridge-type bands limiting the movement of the sciatic nerve from anterior to posterior (type 1A) or from posterior to anterior (type 1B).
- Type 2: adhesive or ‘horse-strap’ bands, which bind strongly to the sciatic nerve structure, anchoring it in a single direction. They can be attached to the sciatic nerve laterally (type 2A) or medially (type 2B).
Fig. 4.

Three-dimensional CT reconstruction in sub-spine impingement: a) antero-inferior iliac spine (AIIS), b) femoral neck impingement area against AIIS.
Fig. 5.
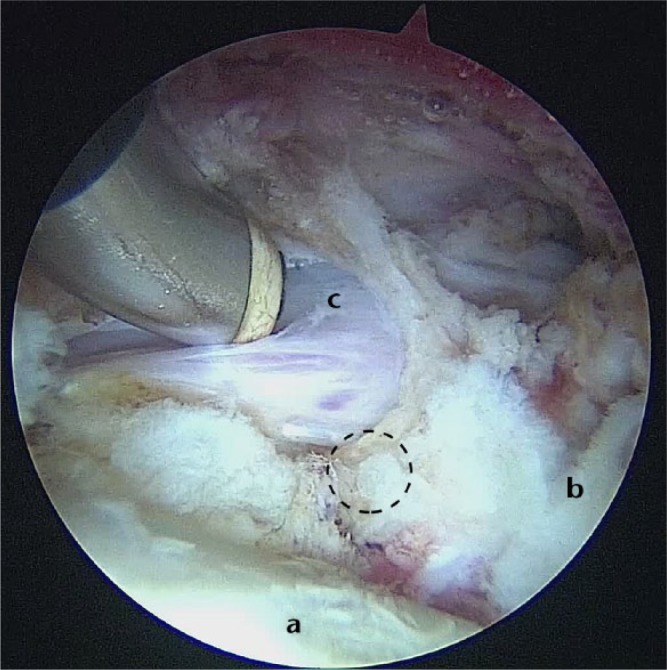
Left hip arthroscopic view. Psoas impingement (circle in dotted line): a) femoral head, b) capsule-labral recess, c) psoas tendon.
Fig. 6.
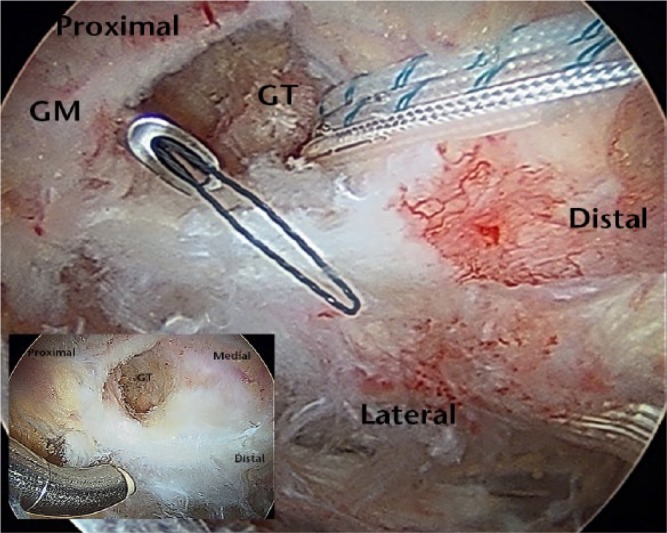
Right hip (peritrochanteric endoscopic view). Gluteus medius (GM) tear (lower left corner image). Repair of GM with anchors to the greater trochanter (GT).
Fig. 7.
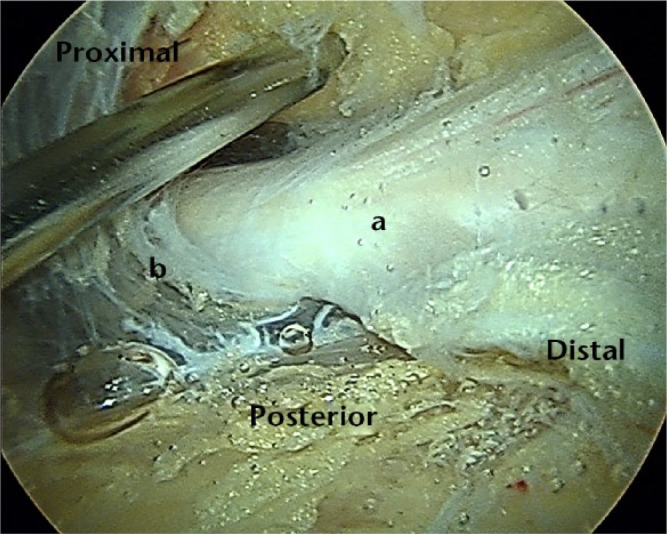
Right hip. Deep gluteal space (endoscopic view). a) Sciatic nerve close to the b) ischial tunnel.
Hip instability
Although the hip joint is very stable because of its bone shape, the capsule and labrum also play an important role in hip stability. Any damage in the labrum and capsule can develop in an unstable joint. Traumatic instability is associated with sports (skiing, rugby, biking, football and soccer). Athletes with pure posterior dislocation commonly return to sport at three months. Atraumatic instability is usually associated with hip dysplasia and connective tissue disorders, such as Marfan’s or Ehlers-Danlos syndromes. Idiopathic instability is commonly described. Treatment options include thermal capsulorrhaphy and arthroscopic capsular plication.70,71 Ligamentum teres disruption is commonly described in arthroscopic surgical reports.72 It has been related to the tearing of the ligamentum which gives stability in limiting internal rotation during sports such as martial arts, ballet, soccer, golf and kicking in American football.73 When compared with ligamentum teres reconstruction, patients treated with arthroscopic debridement achieve better clinical scores.74
In conclusion, hip arthroscopy is currently increasing its indications and new entities are appearing as a result of the increase in knowledge of hip pathology. In future, long-term clinical results after the treatment of these new hip pathologies will demonstrate whether hip arthroscopic techniques are a trend or a real advance.
Footnotes
ICMJE Conflict of Interest Statement: OMP reports receiving personal fees from DePuy, Smith & Nephew and Sanofi and non-financial report from Arthrex outside of this work.
PD reports receiving a grant from Smith & Nephew related to this paper. MTP reports that he is a consultant for Smith & Nephew.
RNV reports receiving personal fees and non-financial support from Smith & Nephew outside of this work.
Funding
The author or one or more of the authors have received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Sing DC, Feeley BT, Tay B, Vail TP, Zhang AL. Age-related trends in hip arthroscopy: a large cross-sectional analysis. Arthroscopy 2015;31:2307-2313. [DOI] [PubMed] [Google Scholar]
- 2. Pollard TC, Khan T, Price AJ, et al. Simulated hip arthroscopy skills: learning curves with the lateral and supine patient positions: a randomized trial. J Bone Joint Surg [Am] 2012;94-A:e68. [DOI] [PubMed] [Google Scholar]
- 3. Masoud MA, Said HG. Intra-articular hip injection using anatomic surface landmarks. Arthrosc Tech 2013;2:e147-e149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Telleria JJ, Lindsey DP, Giori NJ, Safran MR. An anatomic arthroscopic description of the hip capsular ligaments for the hip arthroscopist. Arthroscopy 2011;27:628-636. [DOI] [PubMed] [Google Scholar]
- 5. Dienst M, Seil R, Kohn DM. Safe arthroscopic access to the central compartment of the hip. Arthroscopy 2005;21:1510-1514. [DOI] [PubMed] [Google Scholar]
- 6. Byrd JW. Femoroacetabular impingement in athletes: current concepts. Am J Sports Med 2014;42:737-751. [DOI] [PubMed] [Google Scholar]
- 7. Polesello GC, Omine Fernandes AE, de Oliveira LP, Tavares Linhares JP, Queiroz MC. Medial hip arthroscopy portals: an anatomic study. Arthroscopy 2014;30:55-59. [DOI] [PubMed] [Google Scholar]
- 8. Frank JM, Harris JD, Erickson BJ, et al. Prevalence of femoroacetabular impingement imaging findings in asymptomatic volunteers: a systematic review. Arthroscopy 2015;31:1199-1204 [DOI] [PubMed] [Google Scholar]
- 9. Sardana V, Philippon MJ, de Sa D, et al. Revision hip arthroscopy indications and outcomes: a systematic review. Arthroscopy 2015;31:2047-2055 [DOI] [PubMed] [Google Scholar]
- 10. Kalhor M, Horowitz K, Beck M, Nazparvar B, Ganz R. Vascular supply to the acetabular labrum. J Bone Joint Surg [Am] 2010;92-A:2570-2575. [DOI] [PubMed] [Google Scholar]
- 11. Krych AJ, Thompson M, Knutson Z, Scoon J, Coleman SH. Arthroscopic labral repair versus selective labral debridement in female patients with femoroacetabular impingement: a prospective randomized study. Arthroscopy 2013;29:46-53. [DOI] [PubMed] [Google Scholar]
- 12. Schilders E, Dimitrakopoulou A, Bismil Q, Marchant P, Cooke C. Arthroscopic treatment of labral tears in femoroacetabular impingement: a comparative study of refixation and resection with a minimum two-year follow-up. J Bone Joint Surg [Br] 2011;93-B:1027-1032. [DOI] [PubMed] [Google Scholar]
- 13. Byrd JW, Jones KS. Primary repair of the acetabular labrum: outcomes with 2 years’ follow-up. Arthroscopy 2014;30:588-592. [DOI] [PubMed] [Google Scholar]
- 14. Lee S, Wuerz TH, Shewman E, et al. Labral reconstruction with iliotibial band autografts and semitendinosus allografts improves hip joint contact area and contact pressure: an in vitro analysis. Am J Sports Med 2015;43:98-104. [DOI] [PubMed] [Google Scholar]
- 15. Miozzari HH, Celia M, Clark JM, et al. No regeneration of the human acetabular labrum after excision to bone. Clin Orthop Relat Res 2015;473:1349-1357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ferro FP, Philippon MJ, Rasmussen MT, et al. Tensile properties of the human acetabular labrum and hip labral reconstruction grafts. Am J Sports Med 2015;43:1222-1227. [DOI] [PubMed] [Google Scholar]
- 17. Tey M, Erquicia JI, Pelfort X, et al. Allogenic labral transplantation in hip instability following arthroscopic labrectomy. Hip Int 2011;21:260-262. [DOI] [PubMed] [Google Scholar]
- 18. Ayeni OR, Alradwan H, de Sa D, Philippon MJ. The hip labrum reconstruction: indications and outcomes–a systematic review. Knee Surg Sports Traumatol Arthrosc 2014;22:737-743. [DOI] [PubMed] [Google Scholar]
- 19. Domb BG, El Bitar YF, Stake CE, et al. Arthroscopic labral reconstruction is superior to segmental resection for irreparable labral tears in the hip: a matched-pair controlled study with minimum 2-year follow-up. Am J Sports Med 2014;42:122-130. [DOI] [PubMed] [Google Scholar]
- 20. Karthikeyan S, Roberts S, Griffin D. Microfracture for acetabular chondral defects in patients with femoroacetabular impingement: results at second-look arthroscopic surgery. Am J Sports Med 2012;40:2725-2730. [DOI] [PubMed] [Google Scholar]
- 21. Domb BG, Gupta A, Dunne KF, et al. Microfracture in the hip: results of a matched-cohort controlled study with 2-year follow-up. Am J Sports Med 2015;43:1865-1874. [DOI] [PubMed] [Google Scholar]
- 22. Stafford GH, Bunn JR, Villar RN. Arthroscopic repair of delaminated acetabular articular cartilage using fibrin adhesive. Results at one to three years. Hip Int 2011;21:744-750. [DOI] [PubMed] [Google Scholar]
- 23. Sekiya JK, Martin RL, Lesniak BP. Arthroscopic repair of delaminated acetabular articular cartilage in femoroacetabular impingement. Orthopedics 2009. September;32(9). [DOI] [PubMed] [Google Scholar]
- 24. Tey M, Mas J, Pelfort X, Monllau JC. Arthroscopic treatment of hip chondral defects with bone marrow stimulation and BST-CarGel. Arthrosc Tech 2015;4:e29-e33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Mancini D, Fontana A. Five-year results of arthroscopic techniques for the treatment of acetabular chondral lesions in femoroacetabular impingement. Int Orthop 2014;38:2057-2064. [DOI] [PubMed] [Google Scholar]
- 26. Korsmeier K, Claßen T, Kamminga M, et al. Arthroscopic three-dimensional autologous chondrocyte transplantation using spheroids for the treatment of full-thickness cartilage defects of the hip joint. Knee Surg Sports Traumatol Arthrosc 2016;24:2032-2037. [DOI] [PubMed] [Google Scholar]
- 27. Audenaert EA, Peeters I, Van Onsem S, Pattyn C. Can we predict the natural course of femoroacetabular impingement? Acta Orthop Belg 2011;77:188-196. [PubMed] [Google Scholar]
- 28. Laborie LB, Lehmann TG, Engesæter IØ, et al. Prevalence of radiographic findings thought to be associated with femoroacetabular impingement in a population-based cohort of 2081 healthy young adults. Radiology 2011;260:494-502. [DOI] [PubMed] [Google Scholar]
- 29. Collins JA, Ward JP, Youm T. Is prophylactic surgery for femoroacetabular impingement indicated? A systematic review. Am J Sports Med 2014;42:3009-3015. [DOI] [PubMed] [Google Scholar]
- 30. Nawabi DH, Bedi A, Tibor LM, Magennis E, Kelly BT. The demographic characteristics of high-level and recreational athletes undergoing hip arthroscopy for femoroacetabular impingement: a sports-specific analysis. Arthroscopy 2014;30:398-405. [DOI] [PubMed] [Google Scholar]
- 31. Larson CM, Sikka RS, Sardelli MC, et al. Increasing alpha angle is predictive of athletic-related “hip” and “groin” pain in collegiate National Football League prospects. Arthroscopy 2013;29:405-410. [DOI] [PubMed] [Google Scholar]
- 32. Johnston TL, Schenker ML, Briggs KK, Philippon MJ. Relationship between offset angle alpha and hip chondral injury in femoroacetabular impingement. Arthroscopy 2008;24:669-675. [DOI] [PubMed] [Google Scholar]
- 33. Alradwan H, Philippon MJ, Farrokhyar F, et al. Return to preinjury activity levels after surgical management of femoroacetabular impingement in athletes. Arthroscopy 2012:28:1567-1576. [DOI] [PubMed] [Google Scholar]
- 34. Hartofilakidis G, Bardakos NV, Babis GC, Georgiades G. An examination of the association between different morphotypes of femoroacetabular impingement in asymptomatic subjects and the development of osteoarthritis of the hip. J Bone Joint Surg [Br] 2011;93-B:580-586. [DOI] [PubMed] [Google Scholar]
- 35. Diesel CV, Ribeiro TA, Coussirat C, et al. Coxa profunda in the diagnosis of pincer-type femoroacetabular impingement and its prevalence in asymptomatic subjects. Bone Joint J 2015;97-B:478-483. [DOI] [PubMed] [Google Scholar]
- 36. Zaltz I, Kelly BT, Hetsroni I, Bedi A. The crossover sign overestimates acetabular retroversion. Clin Orthop Relat Res 2013;471:2463-2470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Diaz-Ledezma C, Novack T, Marin-Peña O, Parvizi J. The relevance of the radiological signs of acetabular retroversion among patients with femoroacetabular impingement. Bone Joint J 2013;95-B:893-899. [DOI] [PubMed] [Google Scholar]
- 38. Philippon MJ, Wolff AB, Briggs KK, Zehms CT, Kuppersmith DA. Acetabular rim reduction for the treatment of femoroacetabular impingement correlates with preoperative and postoperative center-edge angle. Arthroscopy 2010;26:757-761. [DOI] [PubMed] [Google Scholar]
- 39. Bhatia S, Lee S, Shewman E, et al. Effects of acetabular rim trimming on hip joint contact pressure: how much is too much? Am J Sports Med 2015;43:2138-2145. [DOI] [PubMed] [Google Scholar]
- 40. Redmond JM, El Bitar YF, Gupta A, et al. Arthroscopic acetabuloplasty and labral refixation without labral detachment. Am J Sports Med 2015;43:105-112. [DOI] [PubMed] [Google Scholar]
- 41. Ilizaliturri VM, Jr, Joachin P, Acuna M. Description and mid-term results of the ‘over the top’ technique for the treatment of the pincer deformity in femoroacetabular impingement. J Hip Preserv Surg 2015;2:369-373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Crawford EA, Welton KL, Kweon C, et al. Arthroscopic treatment of pincer-type impingement of the hip. JBJS Rev 2015;3:e4. [DOI] [PubMed] [Google Scholar]
- 43. Tak I, Weir A, Langhout R, et al. The relationship between the frequency of football practice during skeletal growth and the presence of a cam deformity in adult elite football players. Br J Sports Med 2015;49:630-634. [DOI] [PubMed] [Google Scholar]
- 44. Packer JD, Safran MR. The etiology of primary femoroacetabular impingement: genetics or acquired deformity? J Hip Preserv Surg 2015;2:249-257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Beaulé PE, Le Duff MJ, Zaragoza E. Quality of life following femoral head-neck osteochondroplasty for femoroacetabular impingement. J Bone Joint Surg [Am] 2007;89-A:773-779. [DOI] [PubMed] [Google Scholar]
- 46. Merz MK, Christoforetti JJ, Domb BG. Femoral neck fracture after arthroscopic femoroplasty of the hip. Orthopedics 2015;38:e696-e700. [DOI] [PubMed] [Google Scholar]
- 47. Bedi A, Galano G, Walsh C, Kelly BT. Capsular management during hip arthroscopy: from femoroacetabular impingement to instability. Arthroscopy 2011;27:1720-1731. [DOI] [PubMed] [Google Scholar]
- 48. Wuerz TH, Song SH, Grzybowski JS, et al. Biomechanical evaluation of capsulotomy and capsular repair in the hip: restoring stability. Orthop J Sports Med 2015;3:2325967115S00134. [Google Scholar]
- 49. Abrams GD, Hart MA, Takami K, et al. Biomechanical evaluation of capsulotomy, capsulectomy, and capsular repair on hip rotation. Arthroscopy 2015;31:1511-1517. [DOI] [PubMed] [Google Scholar]
- 50. Malviya A, Stafford GH, Villar RN. Impact of arthroscopy of the hip for femoroacetabular impingement on quality of life at a mean follow-up of 3.2 years. J Bone Joint Surg [Br] 2012;94-B:466-470. [DOI] [PubMed] [Google Scholar]
- 51. Cooper AP, Basheer SZ, Maheshwari R, Regan L, Madan SS. Outcomes of hip arthroscopy. A prospective analysis and comparison between patients under 25 and over 25 years of age. Br J Sports Med 2013;47:234-238. [DOI] [PubMed] [Google Scholar]
- 52. Shearer DW, Kramer J, Bozic KJ, Feeley BT. Is hip arthroscopy cost-effective for femoroacetabular impingement? Clin Orthop Relat Res 2012;470:1079-1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Byrd JW, Jones KS. Arthroscopic management of femoroacetabular impingement: minimum 2-year follow-up. Arthroscopy 2011;27:1379-1388. [DOI] [PubMed] [Google Scholar]
- 54. Philippon MJ, Schroder Souza BG, Briggs KK. Hip arthroscopy for femoroacetabular impingement in patients aged 50 years or older. Arthroscopy 2012;28:59-65. [DOI] [PubMed] [Google Scholar]
- 55. Marín-Peña Ó. Femoroacetabular impingement. New York: Springer, 2012. [Google Scholar]
- 56. Martin HD. Evolving concepts in extra-articular hip pathology. J Hip Preserv Surg 2015;2:91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Hapa O, Bedi A, Gursan O, et al. Anatomic footprint of the direct head of the rectus femoris origin: cadaveric study and clinical series of hips after arthroscopic anterior inferior iliac spine/subspine decompression. Arthroscopy 2013;29:1932-1940. [DOI] [PubMed] [Google Scholar]
- 58. de Sa D, Alradwan H, Cargnelli S, et al. Extra-articular hip impingement: a systematic review examining operative treatment of psoas, subspine, ischiofemoral, and greater trochanteric/pelvic impingement. Arthroscopy 2014;30:1026-1041. [DOI] [PubMed] [Google Scholar]
- 59. Fabricant PD, Bedi A, De La, Torre K, Kelly BT. Clinical outcomes after arthroscopic psoas lengthening: the effect of femoral version. Arthroscopy 2012;28:965-971. [DOI] [PubMed] [Google Scholar]
- 60. Khan M, Adamich J, Simunovic N, et al. Surgical management of internal snapping hip syndrome: a systematic review evaluating open and arthroscopic approaches. Arthroscopy 2013;29:942-948. [DOI] [PubMed] [Google Scholar]
- 61. Ilizaliturri VM, Jr, Buganza-Tepole M, Olivos-Meza A, Acuna M, Acosta-Rodriguez E. Central compartment release versus lesser trochanter release of the iliopsoas tendon for the treatment of internal snapping hip: a comparative study. Arthroscopy 2014;30:790-795. [DOI] [PubMed] [Google Scholar]
- 62. Ilizaliturri VM, Jr, Camacho-Galindo J. Endoscopic treatment of snapping hips, iliotibial band, and iliopsoas tendon. Sports Med Arthrosc 2010;18:120-127. [DOI] [PubMed] [Google Scholar]
- 63. Lindner D, Shohat N, Botser I, Agar G, Domb BG. Clinical presentation and imaging results of patients with symptomatic gluteus medius tears. J Hip Preserv Surg 2015;2:310-315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Alpaugh K, Chilelli BJ, Xu S, Martin SD. Outcomes after primary open or endoscopic abductor tendon repair in the hip: a systematic review of the literature. Arthroscopy 2015;31:530-540. [DOI] [PubMed] [Google Scholar]
- 65. Chandrasekaran S, Lodhia P, Gui C, et al. Outcomes of open versus endoscopic repair of abductor muscle tears of the hip: a systematic review. Arthroscopy 2015;31:2057-2067. [DOI] [PubMed] [Google Scholar]
- 66. Nawabi DH, Wentzel C, Ranawat AS, Bedi A, Kelly BT. A comparison of open and endoscopic repair of full-thickness tears of the gluteus medius tendon at a minimum of 2 years follow-up. Orthop J Sports Med 2015;3:2325967115S00088. [Google Scholar]
- 67. Martin HD, Reddy M, Gómez-Hoyos J. Deep gluteal syndrome. J Hip Preserv Surg 2015;2:99-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Hernando MF, Cerezal L, Pérez-Carro L, Abascal F, Canga A. Deep gluteal syndrome: anatomy, imaging, and management of sciatic nerve entrapments in the subgluteal space. Skeletal Radiol 2015;44:919-934. [DOI] [PubMed] [Google Scholar]
- 69. Martin HD, Shears SA, Johnson JC, Smathers AM, Palmer IJ. The endoscopic treatment of sciatic nerve entrapment/deep gluteal syndrome. Arthroscopy 2011;27:172-181. [DOI] [PubMed] [Google Scholar]
- 70. Smith MV, Sekiya JK. Hip instability. Sports Med Arthrosc. 2010;18:108-112. [DOI] [PubMed] [Google Scholar]
- 71. Domb BG, Stake CE, Lindner D, El-Bitar Y, Jackson TJ. Arthroscopic capsular plication and labral preservation in borderline hip dysplasia: two-year clinical outcomes of a surgical approach to a challenging problem. Am J Sports Med 2013;41:2591-2598. [DOI] [PubMed] [Google Scholar]
- 72. Botser IB, Martin DE, Stout CE, Domb BG. Tears of the ligamentum teres: prevalence in hip arthroscopy using 2 classification systems. Am J Sports Med 2011;39:117S-125S. [DOI] [PubMed] [Google Scholar]
- 73. Martin HD, Hatem MA, Kivlan BR, Martin RL. Function of the ligamentum teres in limiting hip rotation: a cadaveric study. Arthroscopy 2014;30:1085-1091. [DOI] [PubMed] [Google Scholar]
- 74. de SA D, Phillips M, Philippon MJ, et al. Ligamentum teres injuries of the hip: a systematic review examining surgical indications, treatment options, and outcomes. Arthroscopy 2014;30:1634-1641. [DOI] [PubMed] [Google Scholar]


