Abstract
Background:
The vast majority of studies emphasize the greater morbidity/mortality for elective spine surgery in morbidly obese patients.
Methods:
This review focuses on the increased morbidity/mortality of performing elective spinal operations in morbidly obese patients. There are two definitions of morbid obesity; a body mass index (BMI) of equal to or greater than 35 plus two major comorbid factors (e.g., hypertension, diabetes, etc.) or a BMI (morbidly obese III) of =≥40 kg/m2.
Results:
For patients undergoing spinal surgery, morbid obesity increases perioperative morbidity/mortality for various reasons. The quality of preoperative and intraoperative imaging is often compromised potentially leading to mistaken preoperative diagnoses, and wrong level surgery. Resultant major technical surgical limitations include poor/inadequate operative exposure, and the risk of suboptimal placement of instrumentation There is also increased exposure to major perioperative complications such as deep venous thrombosis, pulmonary embolism, infection, pneumonia, cardiac complications, blindness in the prone position, brachial and lumbar plexus injuries, increased anesthetic risks (e.g., even using awake intubation/awake positioning), and postoperative wound seromas/hematomas.
Conclusions:
Most of the spinal literature documents the marked increased perioperative morbidity/mortality for morbidly obese patients undergoing elective spine surgery. If elective surgery is warranted in these patients, the risks and timing of surgical intervention should include consideration of major preoperative weight loss strategies including bariatric procedures to optimize outcomes.
Keywords: Elective spine surgery, morbid obesity, morbidity, mortality, rates
INTRODUCTION
This review focuses on the increased morbidity/mortality for performing elective spine surgery in morbidly obese patients, but does not address emergency surgery. Here, we define morbid obesity as a BMI of >35 with two major comorbidities, or a BMI of >/=40 kg/m2 or greater. Our evaluation included the assessment of multiple perioperative factors and the attendant adverse events (AE)/complications that accompanied morbid obesity. Increased perioperative risks correlated with more prolonged anesthetic and operative times, greater estimated blood loss (EBL), poorer quality of preoperative, intraoperative (more difficulty correctly localizing the surgical levels), and postoperative diagnostic studies, more medical complications, and poorer surgical outcomes.
REVIEW DOES NOT INCLUDE ANALYSIS OF TRAUMATIC INJURIES IN MORBIDLY OBESE PATIENTS
This review did not focus on the greater morbidity/mortality associated with treating morbidly obese patients following traumatic spine injuries.[11,28] One study (2013) observed the “Best medical and surgical care may be compromised and outcome adversely affected in morbidly obese patients with spine trauma.”[28] Their 6 morbidly obese patients, who weighed over 265 pounds, and had BMIs of over 40 (range: 47.8–67.1), sustained high-speed injuries following motor vehicle accidents (MVA). Morbid obesity contributed to longer surgery, poorly fitting orthotics, suboptimal magnetic resonance (MR)/computed tomography (CT)/X-ray images including intraoperative radiographs risking wrong level surgery. There was also greater difficulty with operative positioning, technically more challenging surgery, more nursing problems, and higher risks for prophylaxis against deep venous thrombosis (DVT) and pulmonary embolism (PE). A case report (2104) discussed utilizing awake intubation and awake prone positioning to perform emergency lumbar surgery in a morbidly obese patient (BMI of 62 kg/m2) patient with a cauda equina syndrome attributed to an acute lumbar disc herniation.[11] They commented that anesthesia and the surgical procedure itself were complicated by the patients’ elevated BMI.
LIMITATIONS OF LARGE DATABASE ANALYSIS FOR MORBIDLY OBESE PATIENTS UNDERGOING SPINE SURGERY
Large database analyses for morbidly obese patients undergoing spine surgery often have major shortcomings. When Golinvaux et al. (2014) used the International Classification of Diseases Ninth Revision (ICD-9) codes to study morbidly obese patients undergoing spine surgery, 174 of 2075 patients were “morbidly obese” (BMI >40), but only 84 were correctly coded (278.01) [Table 1].[15] In addition, multiple major comorbid factors were not adequately recorded, and thus the authors warned; “it is important to realize that study outcomes can be skewed by data accuracy, and, thus, should not be blindly accepted simply by virtue of large sample sizes.”
Table 1.
More complications/adverse events (AE) for obese and morbidly obese having elective spine surgery
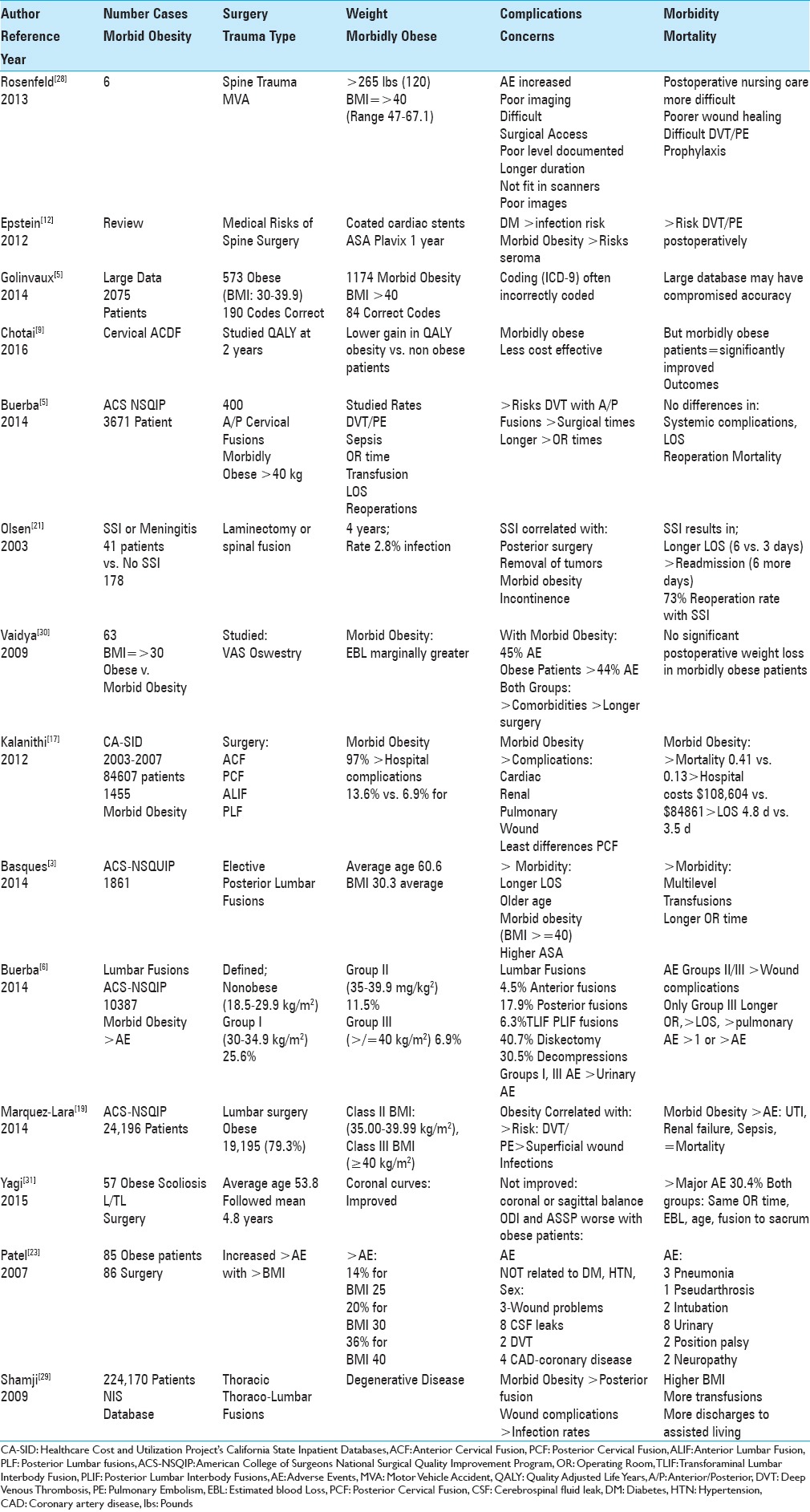
MORE MEDICAL RISK FACTORS WITH MORBID OBESITY
As spinal surgeons, we need to carefully assess whether our patients are “adequate medical” candidates for surgery [Table 1].[12] In 2012, Epstein looked at how major comorbidities impact the risks/complications/AE attributed to spine surgery. For example, surgery/anesthesia administered to a patient with a recent myocardial infarction (MI), within the last 6 months, may have a 40% mortality rate. Patients with stents (cardiac, carotid, peripheral vascular/other) placed in the last 6 months to 1 year, typically cannot stop antiplatelet therapy/anticoagulants due to a high risk of stent failure/thrombosis. Morbidly obese patients who are diabetic with large avascular fat pads between the muscle and overlying skin are also at much greater risk for postoperative infection, seroma, hematoma, poor wound healing, and wound dehiscence. Furthermore, those with chronic obstructive pulmonary disease or those who are active smokers are more likely to develop pneumonia, respiratory failure, and ventilator dependence.
Higher risks of deep venous thrombosis/pulmonary embolism in morbidly obese patients undergoing spine surgery
Morbid obesity increases the risks of perioperative/postoperative phlebitis, and pulmonary embolism [Table 1].[12,19] When Marquez-Lara et al. (2014) queried the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database, they identified 24196 patients undergoing lumbar surgery; 19195 were overweight/obese [Table 1].[19] Spine surgery in obese patients (Class 2: <40 kg/m2) correlated with increased risks of AE particularly including deep venous thrombosis (DVT)/pulmonary embolism (PE) and superficial wound infections, while morbid obesity (Class 3; BMI of ≥40 kg/m2) markedly increased the risks of urinary tract infections (UTI), acute renal failure, and sepsis, but not mortality.
Role for prophylactic inferior vena cava filters for spine surgery in morbidly obese patients
The spinal surgical literature supports the prophylactic placement of inferior vena cava (IVC) filters for morbid obesity (BMI >40), a history of DVT/PE, cancer, fusions, hypercoagulation syndromes, pulmonary/circulatory disorders, preoperative/postoperative immobility, staged procedures (five spinal levels), combined anterior-posterior surgery, iliocaval manipulation, age >80 years, and prolonged surgery (e.g., >261 min vs. >8 h). In 2015, two morbidly obese patients, ages 68 and 69 years of age, prophylactically had IVC filters placed by the author prior to multilevel L1-S1 lumbar laminectomies (note negative preoperative “surveillance” Doppler’s).[13] Both received intraoperative alternating compression stockings, and postoperative prophylactic low-dose subcutaneous heparin (5000 U q12 h) starting 48 h after surgery. Neither of these patients developed DVT or PE, and the filters were electively removed without incident 3 months later.
ANESTHETIC RISKS WITH MORBID OBESITY
Administering anesthesia is more complex in morbidly obese patients undergoing spine surgery. These patients may undergo awake nasotracheal/endotracheal fiberoptic intubation and awake positioning. Additionally using the 3-pin head holder maintains the neck in a neutral posture and avoids kinking the nasotracheal/endotracheal tube, avoids direct pressure on the face, limits neck rotation avoiding carotid and/or jugular compression, and avoids pressure on the eyes limiting the risk of blindness in the prone position (e.g., ischemic optic neuropathy (ION) (anterior (AION)/posterior (PION) by avoiding direct eye compression and increased venous/arterial pressure). Increased intraoperative risks for morbidly obese patients undergoing spinal procedures also include greater blood loss (attributed to increased intrathoracic pressure and greater back-bleeding from Batson's venous plexus), positioning-related brachial or lumbar plexus injury [e.g., even with intraoperative electromyography (EMG) monitoring], and sores/skin sloughing particularly for longer cases. In an analysis of 1861 patients undergoing elective posterior lumbar fusions, obtained from the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP), factors correlating with greater complications/AE with spine surgery included longer length of stay (LOS), older age, morbid obesity (body mass index ≥40 kg/m), higher American Society of Anesthesiologists (ASA) classification, longer and multilevel operations, and greater transfusion requirements [Table 1].[14] In a single case study, 3 major anesthetic risk factors for a 45-year-old female with morbid obesity (e.g., a body mass index of 47 kg/m2) undergoing acute lumbar discectomy/fusion for a cauda equina syndrome included morbid obesity, the prone position, and airway complications.[4]
NO INCREASED MORBIDITY FOR CERVICAL SPINE SURGERY IN MORBIDLY OBESE PATIENTS
Two studies documented no significant increase in morbidity/mortality for morbidly obese patients undergoing cervical spine surgery [Table 1].[5,9] Utilizing the ACS-NSQIP database, the authors (2014) retrospectively analyzed 30-day postoperative morbidity/mortality rates for morbidly obese patients undergoing anterior/posterior cervical fusions with Class II obesity (35–39.9 kg/m2), and Class III morbid obesity (BMI ≥40 kg/m2).[5] Morbidly obese patients exhibited a greater risk of DVT with anterior fusions, whereas posterior fusions correlated with longer surgical times. Of interest, there were no significant differences between obese and nonobese patients concerning lengths of hospital stay (LOS), reoperation rates, and mortality. The authors, therefore, concluded: “High BMI, regardless of obesity class, does not appear to be associated with increased complications after cervical fusion in the 30-day postoperative period.” Another study (2016) prospectively assessed outcomes for anterior cervical discectomy and fusion (ACDF) in morbidly obese patients.[9] Using the WHO Classification system for Class II (obesity) and Class III (morbid obesity) obesity, at 2 postoperative years, all patients exhibited significant improvement in pain in the Neck Disability Index, and quality of life (QALYs; EuroQol-5D; Short Form-12) scales. They also noted “…no significant difference in post-discharge health-care resource utilization, direct costs, indirect costs, and total costs between obese and non-obese patients…”
INCREASED MORBIDITY FOR LUMBAR SURGERY IN MORBIDLY OBESE PATIENTS
Three research studies specifically documented marked increases in perioperative morbidity for elective spine operations performed in morbidly obese patients [Table 1].[6,17,30] One study (2009) retrospectively evaluated 63 patients undergoing lumbar spinal fusion; more postoperative complications were observed for both morbidly obese (45%) and obese patients (44%) [Table 1].[30] They also exhibited more comorbid risk factors, required longer operative times, had more perioperative complications, and later demonstrated no significant weight loss. A second study (2012) retrospectively correlated morbid obesity with different types of spinal fusions, AE, and hospital charges [Table 1].[17] Using the Healthcare Cost and Utilization Project's California State Inpatient Databases (CA-SID), they assessed 4 types of fusions performed in nonobese and morbidly obese patients – anterior cervical fusion, posterior cervical fusion, anterior lumbar fusion, and posterior lumbar fusions. Out of 84607 admissions, there were 1455 morbidly obese patients who demonstrated a “97% higher in-hospital complication rate [13.6% vs. 6.9% (controls)]” largely attributed to cardiac, renal, pulmonary, and wound complications. Morbidly obese patients also incurred higher hospital costs ($108,604 vs. $84861), longer LOS (4.8 d vs. 3.5 d), and slightly higher mortality rates (0.41 vs. 0.13). In short they found: “Morbid obesity was the most significant predictor of complications in the anterior cervical and posterior lumbar fusion groups.”
A third study (2014) retrospectively examined the outcomes of lumbar fusions [anterior, posterior, transforaminal lumbar interbody fusions (TLIF)], for nonobese vs. obese (2 groups) vs. morbidly obese patients using the ACS-NSQIP database (2005 to 2010) [Table 1].[6] Of the 10387 patients undergoing lumbar surgery, 4.5% had anterior fusions, 17.9% had posterior fusions, 6.3% and TLIF/PLIF’s, 40.7% had discectomy, and 30.5% had decompressions. There were 25.6% of patients in the Obese I (30–34.9 kg/m2), 11.5% in the Obese II (35–39.9 kg/m2), and 6.9% in the Obese III (greater than or equal to 40 kg/m2) groups. Obese II and III patients had significantly more wound complications, but only morbidly Obese group III patients had significantly increased risks of more prolonged operating room time, more extended length of stay, greater pulmonary complications, and a higher risks of having one or more complications (all P < .05).
Lumbar fusions in morbidly obese patients increase complication/AE, readmission/reoperation rates, and resource utilization
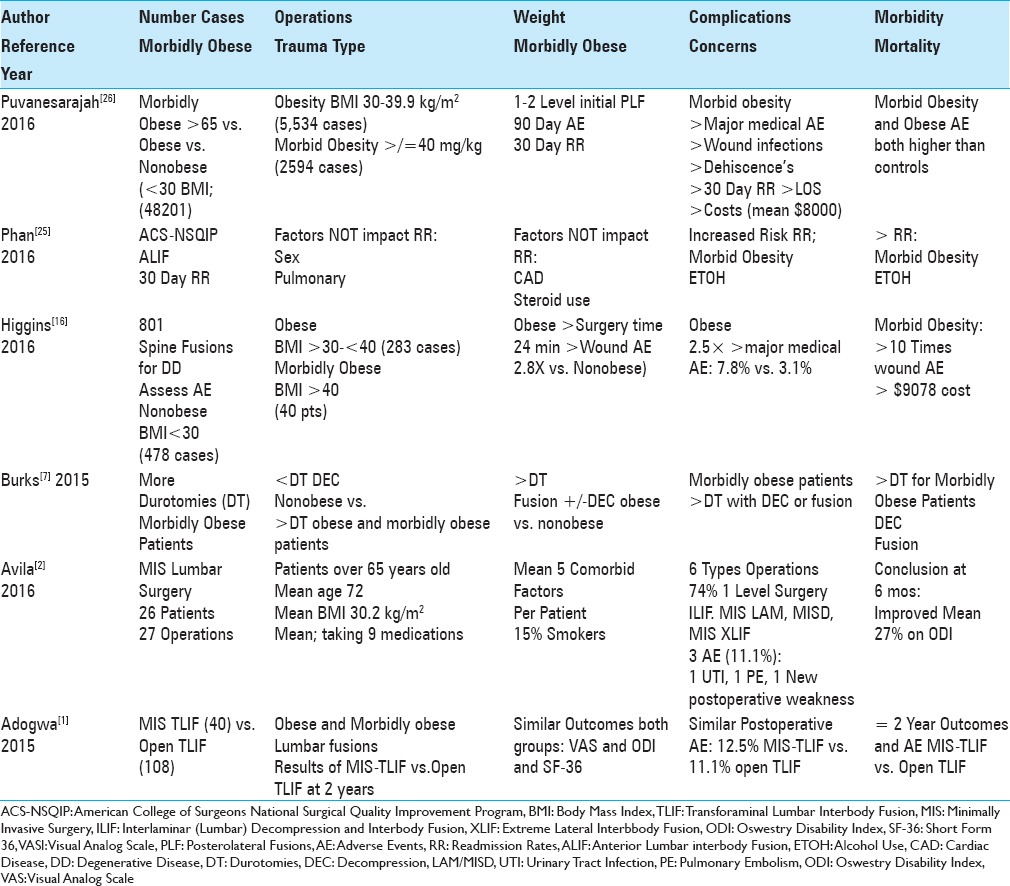
Morbidly obese patients undergoing lumbar fusions experienced increased complications/AE, readmission, reoperation, and resource utilization rates [Table 3].[16,26] One series (2016) evaluated the impact of morbid obesity (BMI ≥ 40 kg/m2 in 2594 patients) vs. obesity (BMI 30–39.9 in 5534 patients) vs. nonobesity (n = 48210) on 3-month complications, and 30-day readmission rates following 1–2 level posterolateral lumbar spinal fusions in patients over 65 years of age [Table 3].[26] Morbidly obese patients had higher rates of one major medical complication (e.g., wound infection and/or dehiscence) vs. obese patients, and demonstrated higher 30-day readmission rates, LOS, and in-hospital costs (more than $8000). A second study (2016) involving 801 patients undergoing instrumented spinal fusions addressing degenerative disease also correlated obesity with higher complication and resource utilization rates [Table 3].[16] They divided BMIs into three groups: (1) BMI <30 (nonobese, n = 478), (2) BMI ≥30 and <40 (obese, n = 283), and (3) BMI of ≥40 (morbidly obese, n = 40). Obesity led to longer anesthesia times (30 minutes), longer surgical times (24 minutes), 2.8 times more wound complications (4.2% vs. 1.5%), and 2.5 times more major medical complications (7.8% vs. 3.1). Morbid obesity, however, resulted in an even higher 10-fold rate of wound complications and greater ($9078) cost. Based on these findings, the authors “support (ed) a role for preoperative weight loss” for obese/morbidly obese patients under consideration for (elective) spine surgery.
Table 3.
Morbid obesity increases complication/AE and reoperation rates
Instrumented thoracolumbar/lumbar fusions in morbidly obese patients associated with more complications/AE
Several studies documented increased complication rates for morbidly obese patients undergoing thoracic/thoracolumbar/lumbar instrumented fusions [Table 1].[23,29,31] The first (2007) study evaluated the impact of obesity on morbidity/mortality in 84 patients undergoing 86 elective thoracic/thoracolumbar fusions (anterior, posterior, or combined anterior-posterior fusion). Significant complications proportionately increased with BMI: 14% for BMI of 25, 20% for BMI of 30, and 36% for BMI of 40, but did not increase with diabetes, hypertension, or sex. Morbid obesity also uniquely contributed to position-related palsies and other complications/AE; “wound infections (three cases), cerebrospinal fluid leakage (eight cases, one requiring reoperation), deep vein thrombosis (two cases), cardiac events (four cases), symptomatic pseudarthrosis (one case), pneumonia (three cases), prolonged intubation (two cases), urological issues (eight cases), positioning-related palsy (two cases), and neuropathic pain (two cases).” The second study (2009) also correlated higher BMI with higher morbidity/mortality rates for 244,170 patients from the Nationwide Inpatient Sample (NIS) database undergoing thoracolumbar/lumbar spine fusions for degenerative disease [Table 1].[29] Higher BMI's yielded more transfusions, more discharges to assisted living, more wound complications for those undergoing posterior procedures, and higher infection rates. Nevertheless, both groups (e.g., nonobese vs. obesity/morbid obesity) showed “...equivalent mortality (rates), length of stay, and other complication rates...” A third study (2015) examined the complications/AE in morbidly obese patients undergoing combined anterior/posterior thoracolumbar/lumbar spine fusions for scoliosis [Table 1].[31] The 57 patients averaged 53.8 years of age, and were followed up for an average of 4.8 years; ODI and Anterior Surgical Site Pain (ASSP) scores were “significantly worse in obese and overweight patients.” Although obesity correlated with poorer clinical outcomes and a higher 30.4% rate of major complications, both obese and nonobese groups demonstrated comparable operative times (OR), EBL, numbers of operated levels, incidence of osteopenia/osteoporosis, frequency of older age, kyphosis, and rates of fusion to the sacrum.
Morbid obesity increases infection rate for lumbar surgery
Olsen et al. (2003) determined that morbid obesity was a major risk factor contributing to surgical site infections (SSIs) following laminectomy and/or spinal fusion procedures [Table 1].[21] They evaluated 41 patients with SSI/meningitis vs. 178 uninfected (control) patients. SSI correlated not only with morbid obesity but also with postoperative incontinence, posterior surgery, removal of tumors, increased LOS (average 6 vs. 3 days on initial admission), and an additional average 6 day LOS for readmission/repeat surgery required in 73% of SSI patients.
More durotomies in morbidly obese patients undergoing lumbar surgery
Burks et al. (2015) observed that durotomies (dural tears (DT)) typically occurred in from 0.5% to 2.6% (large database population) of patients undergoing spinal procedures, but were more frequent in obese or morbidly obese patients having decompression and/or fusions [Table 3].[7]
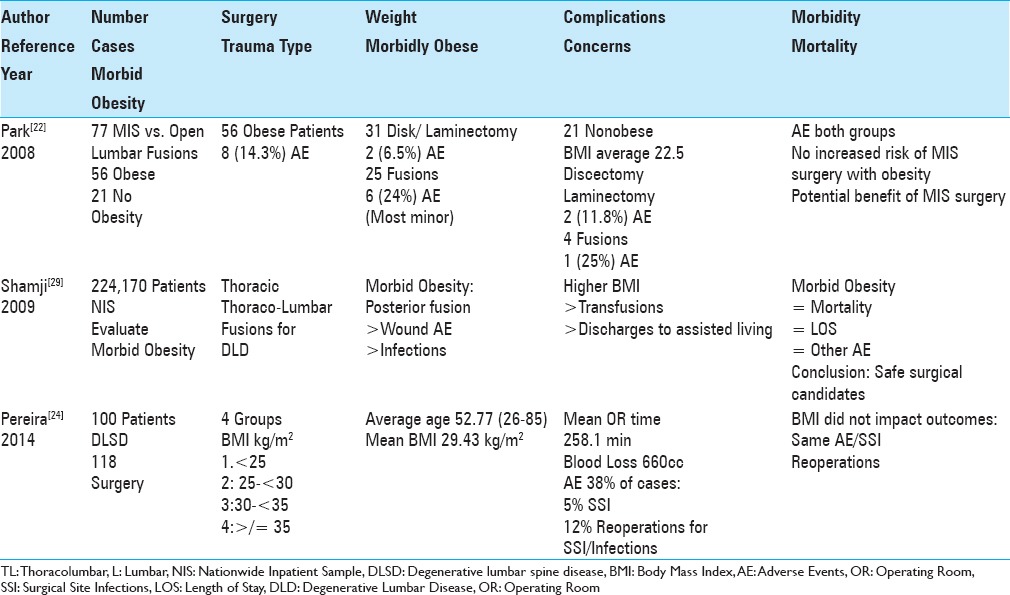
MORBID OBESITY DOES NOT INCREASE MORBIDITY FOR OPEN VS. MIS SPINE SURGERY
Morbid obesity had no negative impact on complications/AE or outcomes of MIS vs. open lumbar spine surgery [Table 2].[1,2,22,24] When Park et al. (2008) evaluated the impact of obesity on AE in 77 patients undergoing MIS vs. open lumbar spine surgery, 56 had average BMIs of 31.0 kg/m2 (range of BMI 25.1–43.8 kg/m2) vs. 21 nonobese patients (<25 kg/m2) [Table 2].[22] For 31 of 56 obese patients undergoing discectomy/laminotomy, there were two (6.5%) AEs, while in the fusion group, there were six (24%) AEs. Twenty-one nonobese patients demonstrated similar frequencies of AE: 2 (11.8%) of 17 undergoing discectomy/laminotomy had AE and 1 of 4 (25%) having fusions exhibited AE. They concluded there were no statistically significant differences in complication rates between obese and nonobese groups, “...which may reflect a potential benefit of the MIS approach.” Pereira et al. (2014) next evaluated whether obesity impacted outcomes for 118 open procedures performed in 100 obese patients averaging 52.77 years of age undergoing 1–4 level surgery for degenerative lumbar spine disease (DLSD) [Table 2].[24] There were four groups: BMI <25, BMI 25–30, BMI >30–35, and BMI >35 (average BMI 29.43 kg/m2) [Table 2]. The frequency of SSI was 5%, and correlated with initially more extensive surgery, more complications, and a 12% higher reoperation rate. Despite this, the authors concluded: “BMI is not a complicating factor for the outcome of patients undergoing surgery for DLSD in terms of SSI, surgical complications, and re-operation rates.” Adogwa et al. (2015) asked whether MIS-TLIF (40 patients) vs. open-TLIF (108 patients) were better for treating degenerative disc disease or spondylolisthesis in morbidly obese patients [Table 3].[1] Both groups demonstrated comparable outcomes at 2 postoperative years (e.g., on the VAS (back/leg pain), ODI, and SF-36 physical score/mental scales), with similar complication rates (e.g., 12.5% MIS-TLIF vs. 11.11% open TLIF).
Table 2.
No increase in complications/adverse events (AE) for patients who are obese/morbid obese having spine surgery
Avila et al. (2016) retrospectively evaluated the outcomes/complications for one surgeon performing 27 MIS lumbar procedures in 26 patients over the age of 65 with multiple comorbidities, and an average BMI of 30.2 kg/m2 [Table 3].[2] The study included 6 different operations typically performed at one level (74%); interlaminar decompression and fusion (ILIF), MIS laminectomy, microdiscectomy, and MIS lateral fusion (XLIF). There were only 3 (11.1%) complications; 1 urinary tract infection (UTI), 1 pulmonary embolism (PE), and 1 new postoperative neurological deficit. Six months postoperatively, patients demonstrated a 27% incidence of improvement on the Oswestry Disability Index (ODI) scale. They concluded MIS spine surgery was an effective means for treating obese patients requiring spinal operations.
ANTERIOR LUMBAR INTERBODY FUSIONS IN MORBIDLY OBESE PATIENTS INCREASES COMPLICATION/AE RATES
Phan et al. (2016), utilizing National Surgical Quality Improvement Program (ACS NSQIP), evaluated the 30-day readmissions after anterior lumbar interbody fusions (ALIF) [Table 3].[25] The highest unplanned 30-day readmission rates correlated with morbid obesity and alcohol abuse, but not with sex, pulmonary disease comorbidity, cardiac disease, comorbidity, and steroid use.
PROS AND CONS OF BARIATRIC SURGERY IN MORBIDLY OBESE PATIENTS
Bariatric surgery and weight loss reduces back pain in morbidly obese patients
Several authors documented substantial weight reduction, reduced chronic back pain, and a reduced need for spine surgery 6 months following bariatric procedures in morbidly obese patients.[8,18] Khoueir et al. (2009) found improvement in chronic axial low back pain in 58 morbidly obese patients (defined as 50–100% above their ideal body weight and/or BMI >40) who lost a lot of weight 6 months following bariatric surgery; there was a 44% decrease in axial back pain (VAS), while mean physical health scores increased by 58% (Short Form-36: SF-36), and there was a significant 24% decrease in ODI scores [Table 4].[18] Cakir et al. (2015) similarly found weight loss 6 months after laparoscopic sleeve gastrectomy (LSG) also substantially relieved back pain (head, neck, shoulder, low back, knee) for 39 (average age 37.9) morbidly obese females; their average preoperative BMI was 46.49 kg/m2, and postoperative BMI was 32.33 kg/m2 [Table 4].[8]
Table 4.
Trial of bariatric surgery/weight loss prior to spine surgery and impact of osteoporosis
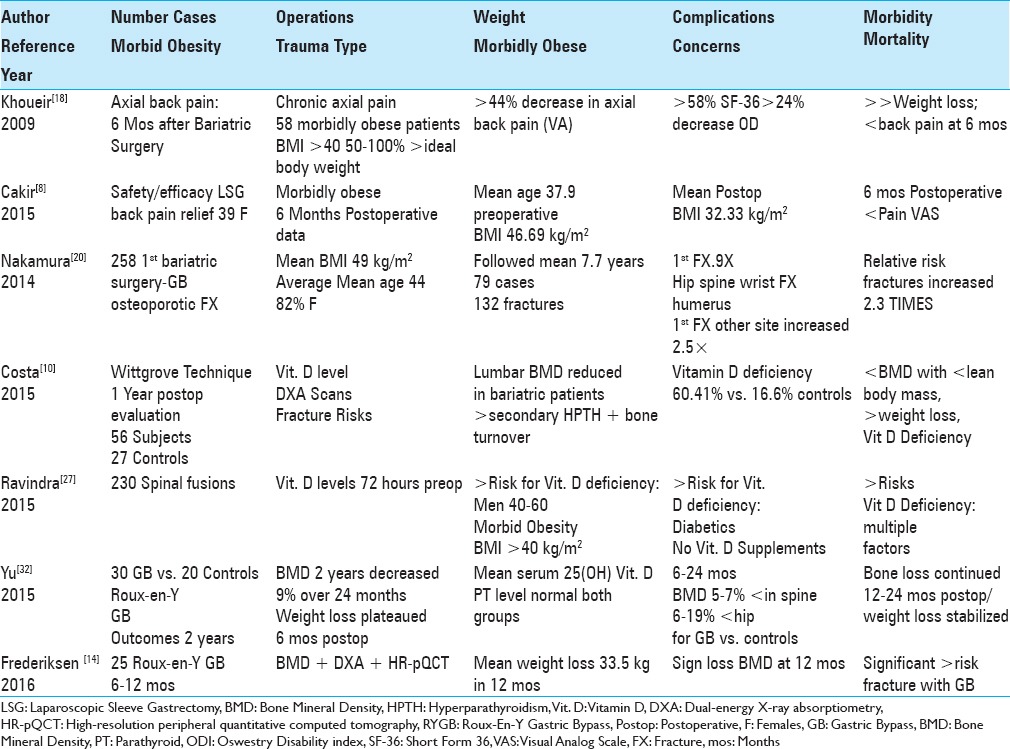
Bariatric surgery in morbidly obese patients results in osteoporosis, reduced bone mineral density (BMD), vitamin D deficiency, and increases fracture risk
Three studies demonstrated that bariatric surgery results in a greater risk of osteoporosis, reduced bone mineral density (BMD), Vitamin D deficiency, and an increased risk of spinal fractures [Table 4].[10,20,27] Nakamura et al. (2014) evaluated fracture risks utilizing standardized incidence (SIRs) and hazard ratios (HR) in 258 patients undergoing initial bariatric procedures (gastric bypass 94%) [Table 4].[20] Their average BMI was 49.0 ± 8.4 kg/m2, their mean age was 44, and 82% (212) were females; they were followed up for an average of 7.7 years. When they observed 132 fractures in 79 patients they concluded; the “Relative risk for any fracture was increased 2.3-fold and was elevated for a first fracture involving the hip, spine, wrist, or humerus or at any other site.” Costa et al. (2015) documented bariatric surgery (Wittgrove technique evaluated at 1 year) in 56 patients vs. 27 controls contributed to reduced BMD, greater vitamin D deficiency, increased bone turnover [dual energy X-ray absorptiometry (DXA)], and an increased risk for bone fractures [Table 4].[10] Lumbar BMD was reduced for bariatric patients (e.g., also correlated with reduced lean body mass and greater weight loss), while 60.41% also showed Vitamin D deficiency vs. 16.6% for control patients. They, therefore, recommended that patients undergoing bariatric surgery should immediately undergo Vitamin D supplementation. Ravindra et al. (2015) similarly documented decreased BMD/osteoporosis/osteomalacia, and vitamin D deficiency increasing the risk of fractures for 230 patients undergoing elective instrumented spinal procedures (degenerative spinal spondylosis or spinal instability) [Table 4].[27] All patients had serum 25-OH (Hydroxy) vitamin D levels drawn within less than <72 hours of surgery. For these patients, 89 9 (38.9%) had laboratory confirmed Vitamin D Insufficiency, there were more males age 40-60 who were osteopenic/osteoporotic vs. females. Additionallly, lower 25-OH levels correlated with morbid obesity, diabetes, or the lack of utiliation of vitamin D supplementation.
Two-year changes in BMD after Roux-en-Y gastric bypass surgery
Two studies showed decreases in BMD following Roux-en-Y gastric bypasses.[14,32] Yu et al. (2015) evaluated bone density (quantitative computed tomography (QCT)) and DXA absorptiometry at 0, 12, and 24 months after Roux-en-Y gastric bypass surgery [Table 4].[32] At 24 months, BMD was 5–7% lower in the spine and 6–10% lower at the hip for bypass vs. control patients. Notably, “Substantial bone loss continued even if the weight loss stabilized from 12–24 months after surgery, (and) the potential for adverse effects on skeletal integrity remained an important concern.” Frederiksen et al. (2016) evaluated (prospective/cohort study) the 6–12 month impact of Roux-en-Y gastric bypass surgery on bone loss (DMB dual-energy X-ray absorptiometry (DXA)) and high-resolution peripheral quantitative computed tomography (HR-pQCT)) for 25 morbidly obese (15 females, 10 males) patients [Table 4].[14] Patients lost an average of 33.5 ± 12.1 kg (25.8 ± 8.5 %) in 12 months. Significant changes increased the risk of fracture for patients undergoing bariatric surgery, but they “only observed bone structural changes in the weight-bearing bone, which indicates that mechanical un-loading is (was) the primary mediator.”
CONCLUSION
The majority of studies involving morbidly obese patients undergoing lumbar spinal surgery demonstrated increased perioperative morbidity. The greater complication/AE Rates included more prolonged operative times, longer anesthesia time, greater intraoperative blood loss, more postoperative wound complications, higher infection rate, longer LOS, poorer outcomes, more durotomies, and more medical complications (e.g., DVT/PE, UTI, respiratory complications) among others. Interestingly, morbid obesity did not negatively impact the outcomes of cervical spine surgery, particularly if performed anteriorly. Although bariatric procedures prior to spine surgery typically results in marked weight loss and potential reduction of perioperative morbidity, the procedures themselves increase the perioperative risks attributed to more severe osteoporosis, reduced BMD, greater Vitamin D Deficiency, and greater susceptibility to fracture.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
REFERENCES
- 1.Adogwa O, Carr K, Thompson P, Hoang K, Darlington T, Perez E, et al. A prospective, multi-institutional comparative effectiveness study of lumbar spine surgery in morbidly obese patients: Does minimally invasive transforaminal lumbar interbody fusion result in superior outcomes? World Neurosurg. 2015;83:860–6. doi: 10.1016/j.wneu.2014.12.034. [DOI] [PubMed] [Google Scholar]
- 2.Avila MJ, Walter CM, Baaj AA. Outcomes and Complications of Minimally Invasive Surgery of the Lumbar Spine in the Elderly. Cureus. 2016;8:e519. doi: 10.7759/cureus.519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Basques BA, Fu MC, Buerba RA, Bohl DD, Golinvaux NS, Grauer JN. Using the ACS-NSQIP to identify factors affecting hospital length of stay after elective posterior lumbar fusion. Spine. 2014;39:497–502. doi: 10.1097/BRS.0000000000000184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baxi V, Budhakar S. Anesthesia management of a morbidly obese patient in prone position for lumbar spine surgery. Craniovertebr Junction Spine. 2010;1:55–7. doi: 10.4103/0974-8237.65483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Buerba RA, Fu MC, Grauer JN. Anterior and posterior cervical fusion in patients with high body mass index are not associated with greater complications. Spine J. 2014;14:1643–53. doi: 10.1016/j.spinee.2013.09.054. [DOI] [PubMed] [Google Scholar]
- 6.Buerba RA, Fu MC, Gruskay JA, Long WD, 3rd, Grauer JN. Obese Class III patients at significantly greater risk of multiple complications after lumbar surgery: An analysis of 10,387 patients in the ACS NSQIP database. Spine J. 2014;14:2008–18. doi: 10.1016/j.spinee.2013.11.047. [DOI] [PubMed] [Google Scholar]
- 7.Burks CA, Werner BC, Yang S, Shimer AL. Obesity is associated with an increased rate of incidental durotomy in lumbar spine surgery. Spine. 2015;40:500–4. doi: 10.1097/BRS.0000000000000784. [DOI] [PubMed] [Google Scholar]
- 8.Çakır T, Oruç MT, Aslaner A, Duygun F, Yardımcı EC, Mayir B, et al. The effects of laparoscopic sleeve gastrectomy on head, neck, shoulder, low back and knee pain of female patients. Int J Clin Exp Med. 2015;8:2668–73. [PMC free article] [PubMed] [Google Scholar]
- 9.Chotai S, Sielatycki JA, Parker SL, Sivaganesan A, Kay HL, Stonko DP1, et al. Effect of obesity on cost per quality-adjusted life years gained following anterior cervical discectomy and fusion in elective degenerative pathology. Spine J. 2016;9430:30281–9. doi: 10.1016/j.spinee.2016.06.023. [DOI] [PubMed] [Google Scholar]
- 10.Costa TL, Paganotto M, Radominski RB, Kulak CM, Borba V. Calcium metabolism, vitamin D and bone mineral density after bariatric surgery. Osteoporos Int. 2015;26:757–64. doi: 10.1007/s00198-014-2962-4. [DOI] [PubMed] [Google Scholar]
- 11.Douglass J, Fraser J, Andrzejowski J. Awake intubation and awake prone positioning of a morbidly obese patient for lumbar spine surgery. Anaesthesia. 2014;69:166–9. doi: 10.1111/anae.12387. [DOI] [PubMed] [Google Scholar]
- 12.Epstein NE. How much medicine do spine surgeons need to know to better select and care for patients? Surg Neurol Int. 2012;3(Suppl 5):S329–49. doi: 10.4103/2152-7806.103866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Epstein NE. Prophylactic inferior vena cava filter placement prior to lumbar surgery in morbidly obese patients: Two-case study and literature review. Surg Neurol Int. 2015;6(Suppl 19):S469–74. doi: 10.4103/2152-7806.166877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Frederiksen KD, Hanson S, Hansen S, Brixen K, Gram J, Jørgensen NR, et al. Bone Structural Changes and Estimated Strength After Gastric Bypass Surgery Evaluated by HR-pQCT. Calcif Tissue Int. 2016;98:253–62. doi: 10.1007/s00223-015-0091-5. [DOI] [PubMed] [Google Scholar]
- 15.Golinvaux NS, Bohl DD, Basques BA, Fu MC, Gardner EC, Grauer JN. Limitations of administrative databases in spine research: A study in obesity. Spine J. 2014;14:2923–8. doi: 10.1016/j.spinee.2014.04.025. [DOI] [PubMed] [Google Scholar]
- 16.Higgins DM, Mallory GW, Planchard RF, Puffer RC, Ali M, Gates MJ, et al. Understanding the Impact of Obesity on Short-term Outcomes and In-hospital Costs After Instrumented Spinal Fusion. Neurosurgery. 2016;78:127–32. doi: 10.1227/NEU.0000000000001018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kalanithi PA, Arrigo R, Boakye M. Morbid obesity increases cost and complication rates in spinal arthrodesis. Spine. 2012;37:982–8. doi: 10.1097/BRS.0b013e31823bbeef. [DOI] [PubMed] [Google Scholar]
- 18.Khoueir P, Black MH, Crookes PF, Kaufman HS, Katkhouda N, Wang MY. Prospective assessment of axial back pain symptoms before and after bariatric weight reduction surgery. Spine J. 2009;9:454–63. doi: 10.1016/j.spinee.2009.02.003. [DOI] [PubMed] [Google Scholar]
- 19.Marquez-Lara A, Nandyala SV, Sankaranarayanan S, Noureldin M, Singh K. Body mass index as a predictor of complications and mortality after lumbar spine surgery. Spine. 2014;39:798–804. doi: 10.1097/BRS.0000000000000232. [DOI] [PubMed] [Google Scholar]
- 20.Nakamura KM, Haglind EG, Clowes JA, Achenbach SJ, Atkinson EJ, Melton LJ, 3rd, et al. Fracture risk following bariatric surgery: A population-based study. Osteoporos Int. 2014;25:151–8. doi: 10.1007/s00198-013-2463-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Olsen MA, Mayfield J, Lauryssen C, Polish LB, Jones M, Vest J, et al. Risk factors for surgical site infection in spinal surgery. J Neurosurg. 2003;98:149–55. [PubMed] [Google Scholar]
- 22.Park P, Upadhyaya C, Garton HJ, Foley KT. The impact of minimally invasive spine surgery on perioperative complications in overweight or obese patients. Neurosurgery. 2008;62:693–9. doi: 10.1227/01.neu.0000317318.33365.f1. [DOI] [PubMed] [Google Scholar]
- 23.Patel N, Bagan B, Vadera S, Maltenfort MG, Deutsch H, Vaccaro AR, et al. Obesity and spine surgery: Relation to perioperative complications. J Neurosurg Spine. 2007;6:291–7. doi: 10.3171/spi.2007.6.4.1. [DOI] [PubMed] [Google Scholar]
- 24.Pereira BJ, de Holanda CV, Ribeiro CA, de Moura SM, Galvão PE, Quidute BS, et al. Impact of body mass index in spinal surgery for degenerative lumbar spine disease. Clin Neurol Neurosurg. 2014;127:112–5. doi: 10.1016/j.clineuro.2014.09.016. [DOI] [PubMed] [Google Scholar]
- 25.Phan K, Lee NJ, Kothari P, Kim JS, Cho SK. Risk Factors for Readmissions Following Anterior Lumbar Interbody Fusion. Spine. 2016 doi: 10.1097/BRS.0000000000001677. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 26.Puvanesarajah V, Cancienne JM, Pehlivan H, Jain A, Shimer AL, Singla A, et al. Morbid Obesity and Lumbar Fusion in Patients over 65 Years of Age: Complications, Readmissions, Costs, and Length of Stay. Spine. 2017;42:122–7. doi: 10.1097/BRS.0000000000001692. [DOI] [PubMed] [Google Scholar]
- 27.Ravindra VM, Godzik J, Guan J, Dailey AT, Schmidt MH, Bisson EF, et al. Prevalence of Vitamin D Deficiency in Patients Undergoing Elective Spine Surgery: A Cross-Sectional Analysis. World Neurosurg. 2015;83:1114–9. doi: 10.1016/j.wneu.2014.12.031. [DOI] [PubMed] [Google Scholar]
- 28.Rosenfeld HE, Limb R, Chan P, Fitzgerald M, Bradley WP, Rosenfeld JV. Challenges in the surgical management of spine trauma in the morbidly obese patient: A case series. Neurosurg Spine. 2013;19:101–9. doi: 10.3171/2013.4.SPINE12876. [DOI] [PubMed] [Google Scholar]
- 29.Shamji MF, Parker S, Cook C, Pietrobon R, Brown C, Isaacs RE. Impact of body habitus on perioperative morbidity associated with fusion of the thoracolumbar and lumbar spine. Neurosurgery. 2009;65:490–8. doi: 10.1227/01.NEU.0000350863.69524.8E. [DOI] [PubMed] [Google Scholar]
- 30.Vaidya R, Carp J, Bartol S, Ouellette N, Lee S, Sethi A. Lumbar spine fusion in obese and morbidly obese patients. Spine. 2009;34:495–500. doi: 10.1097/BRS.0b013e318198c5f2. [DOI] [PubMed] [Google Scholar]
- 31.Yagi M, Patel R, Boachie-Adjei O. Complications and Unfavorable Clinical Outcomes in Obese and Overweight Patients Treated for Adult Lumbar or Thoracolumbar Scoliosis With Combined Anterior/Posterior Surgery. J Spinal Disord Tech. 2015;28:E368–76. doi: 10.1097/BSD.0b013e3182999526. [DOI] [PubMed] [Google Scholar]
- 32.Yu EW, Bouxsein ML, Putman MS, Monis EL, Roy AE, Pratt JS, et al. Two-year changes in bone density after Roux-en-Y gastric bypass surgery. J Clin Endocrinol Metab. 2015;100:1452–9. doi: 10.1210/jc.2014-4341. [DOI] [PMC free article] [PubMed] [Google Scholar]


