Abstract
Background:
Minimally invasive surgery (MIS) spine procedures were developed to limit operative time, the extent of dissection, and reduce perioperative morbidity. Here, we asked what are the “learning curves” for these MIS spine procedures?
Methods:
We reviewed studies in the literature that discussed the “learning curves” attributed to performing different MIS spine surgical procedures. Of interest, the majority were single-surgeon series.
Results:
Very few articles assessed the learning curves for different MIS spine procedures. One study reported no learning curve for open vs. MIS discectomy/laminotomy. Another study indicated that 20–30 cases were required for a surgeon to become proficient in performing a variety of MIS spine fusions [e.g., cervical MIS fusions, MIS anterior lumbar interbody fusions (ALIF), MIS transforaminal lumbar interbody fusions (TLIF), and MIS pedicle/screw placement in the thoracic/lumbar spine]. Several other studies specifically cited that, to become proficient in the performance of TLIF, surgeons had to have performed between 10, to 32, to 40, to 44 such cases.
Conclusions:
There is a very limited literature available that focuses on the “learning curves” associated with the performance of different types of MIS spine procedures. The number of cases required to satisfy the “learning curves” for different operations varied from 0 for MIS vs. open discectomy/laminotomy, to 20-30 for a variety of cervical-thoracic-lumbar procedures, and up to 44 cases for TLIF. Shouldn’t we ask whether better oversight measures and/or mentoring programs could limit the morbidity/AE occurring during these “learning curves” in the future?
Keywords: Adverse events, learning curve, minimally invasive spine surgery, minimizing, morbidity, mortality, under-reporting
INTRODUCTION
Minimally invasive spine surgery (MIS) theoretically limits operative time/dissection, and reduces perioperative morbidity and mortality. Here, we focused on the “learning curves,” defined as the number of cases required to become proficient (e.g., reduce operative time, estimated blood loss, morbidity/adverse events) for performing various MIS spinal procedures. As some studies documented comparable long-term outcomes for open vs. MIS spinal operations, how do we determine wheter (not if) the “learning curve’ is “worth it”?
MIS SPINE SURGERY ASSOCIATED WITH SIGNIFICANT ADVERSE EVENTS
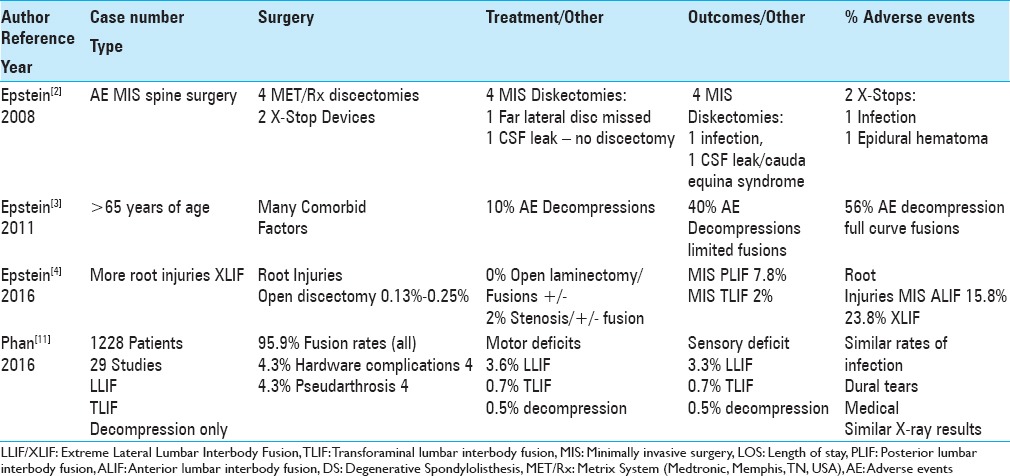
The adverse events (AE) attributed to MIS spine surgery need to be better recognized [Table 1].[2,3,4] In 2008, Epstein reported major complications of 4 MIS Met/RX diskectomies performed by other surgeons (MED/METRx, Medtronic, Memphis, TN, USA) and 2 major complications of MIS X-Stops devices (infection, hematoma) also performed by outside surgeons.[2] Epstein quoted another study in 2011 that observed AE increased with the greater complexity/extent of MIS spinal surgery performed in largely geriatric patients (e.g., 10% AE for decompression alone, 40% AE for decompression/limited fusions, and 56% AE for full curve fusions).[3] As of 2016, Epstein observed that the literature quoted higher frequencies of nerve root injuries occurring with MIS vs. open spine surgery.[4] Higher rates of nerve root injuries were reported during MIS fusions; posterior lumbar interbody fusions (PLIF 7.8%), transforaminal lumbar interbody fusions (TLIF 2%), anterior lumbar interbody fusions (ALIF 15.8%), and extreme lateral interbody fusions (XLIF 23.8%). Lower rates of nerve root injuries were confirmed in different reports for open procedures; from 0.13–0.25% for laminectomy/discectomy alone, 0–2% for laminectomy/stenosis with/without fusion, and up to 2% for laminectomy/stenosis/degenerative spondylolisthesis (DS) with/without fusion. Phan et al. in 2016 reviewed 29 studies involving 1228 patients, and defined higher incidences of motor/sensory deficits for patients undergoing MIS LLIF (lateral lumbar interbody fusions: motor 3.6%/sensory 3.3%) and TLIF (0.7%/0.7%), vs. open decompression alone for adult degenerative scoliosis (0.5%/0.5%) [Table 1].[11]
Table 1.
Complications for minimally invasive vs. open spinal surgical procedures
MINIMAL TO STEEP LEARNING CURVES FOR MIS SPINE SURGERY
Several studies, most of which were single-surgeon series, identified “steep” learning curves for MIS spinal surgery [Table 2].[3,5,6,7,8,9,12,13] In 2003, Guyer et al. observed that learning curves for MIS spine surgery had to be better assessed.[3] Lau et al. in 2011, in a single-surgeon series, evaluated/compared the learning curve for 12 open TLIF vs. 10 MIS TLIF (e.g., for lumbar spondylolisthesis and lysis) over 1 postoperative year [Table 2].[7] Those undergoing MIS TLIF exhibited lower transfusion rates, fewer drains/shorter drainage periods, shorter time duration for bed rest, but “tended” to have higher complication rates that they attributed to the learning curve.[7]
Table 2.
Learning curve for minimally invasive spine procedures
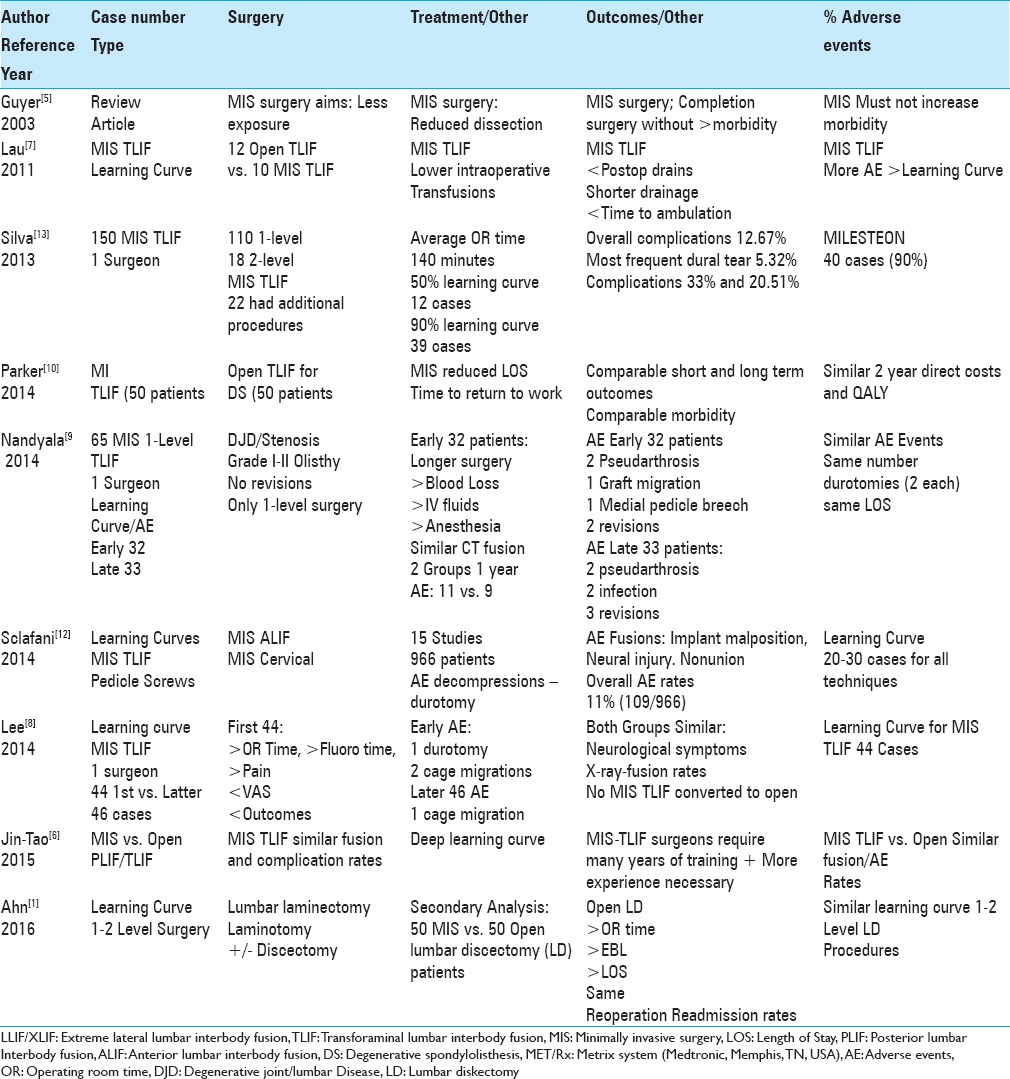
In 2013, Silva et al., in another single-surgeon series, noted MIS-TLIF correlated with “a steep learning curve.”[13] Procedures included; 110 one-level and 18 two-level MIS-TLIF. They observed a 50% learning curve by case 12 (defined by a complication rate of 33%), but a 90% learning curve by case 39 (defined by a complication rate 20.51%). They concluded that the learning curve for MIS TLIF was therefore, approximately 40 cases.
Subsequently, in 2014, Nandyala et al., again in a single-surgeon study, evaluated the learning curve for the first 32 cases of MIS TLIF vs. the latter 33 MIS TLIF performed for disc disease/lumbar spinal stenosis with grade I or II spondylolisthesis.[9] Those in the first MIS TLIF group required significantly longer surgery with higher EBL; however, each group had comparable complication rates (e.g., 2 durotomies, and similar CT documented complications at one year; 11 vs. 9, respectively), with comparable LOS [Table 2]. They concluded that there should be “methods to minimize the complications associated with the learning curve.”
Lee et al. in 2014 assessed the learning curve for 90 one-level MIS TLIF performed by one surgeon.[8] Although the first 44 patients showed poorer VAS and neurogenic symptom scores vs. the latter 46 patients, both groups demonstrated comparable radiologic fusion, and complication/AE rates. They concluded that “the asymptote (the number of cases needed to approach the complication rate of standard surgical techniques) of the surgeon's learning curve for MIS TLIF was achieved at the 44th case.”
In 2015, Jin-Tao et al. summarized the findings of 14 studies (12-month follow-up) involving MIS TLIF vs. open PLIF/TLIF.[6] They concluded that MIS TLIF led to similar fusion and complication rates, however, higher revision/readmission rates were attributed to the deep learning curve. They observed that for MIS TLIF, surgeons require “many of training and experience is necessary. Otherwise, MIS TLIF may yield unsatisfactory results upon patients.”
Sclafani and Kim in 2014 also discussed the learning curves found in 14 studies involving 966 MIS procedures that included MIS TLIF, percutaneous pedicle screw insertion (thoracic/lumbar), MIS anterior lumbar interbody fusion, and MIS cervical fusions.[12] The most common complication/AE attributed to the “learning curve” for decompressions alone was durotomy, while for fusions, complications/AE included implant malposition, instrumented-related neural injury, and nonunion. Their total complication rate was 11% (109 of 966 cases). They concluded that the learning curve, largely based on operative time and complications, required 20 to 30 consecutive cases in each group. They also noted that “the field of MIS (spine surgery) would benefit from a standardization of study design and collected parameters in future learning curve investigations.”
NO LEARNING CURVE FOR MIS LUMBAR DISKECTOMY OR MIS TLIF
Two studies claimed no significant learning curves were associated with performing MIS vs. open lumbar discectomy, and MIS vs. open TLIF [Table 2].[1,10] Ahn et al. evaluated one-surgeon's leaning curve for performing 50 MIS vs. 50 open lumbar discectomy (LD patients); MIS procedures were shorter, involved less blood loss, and shorter LOS. However, both groups demonstrated comparable 30-day readmission rates/AE.[1] Parker et al. found comparable safety/efficacy and cost effectiveness of 50 MIS-TLIF vs. 50 open procedures for degenerative spondylolisthesis [Table 1].[10] Although MIS reduced the length of stay (LOS) and time to return to work, both offered comparable outcomes/quality-adjusted life year QALY, AE, readmission rates, and 2-year health care costs.
CONCLUSION
The spine literature documents different learning curves (e.g., complications/AE) for performing various types of MIS spinal surgical procedures.[1,5,6,7,8,9,12,13] Two studies stipulated there were no learning curves necessary to perform MIS vs. open discectomy/laminotomy.[1,10] Another study found that an average of 20–30 cases were warranted to satisfy learning curves for TLIF, MIS Pedicle Screws, MIS ALIF, and MIS cervical surgery.[12] Several other studies described learning curves for MIS TLIF requiring from 10 to 44 cases [Table 2].[7,8,9,13] Shouldn’t we ask whether better oversight measures and/or mentoring programs would/should limit the morbidity/AE occurring during these “learning curves” in the future?
Footnotes
REFERENCES
- 1.Ahn J, Iqbal A, Manning BT, Leblang S, Bohl DD, Mayo BC, et al. Minimally invasive lumbar decompression-the surgical learning curve. Spine J. 2016;16:909–16. doi: 10.1016/j.spinee.2015.07.455. [DOI] [PubMed] [Google Scholar]
- 2.Epstein NE. How often is minimally invasive minimally effective: What are the complication rates for minimally invasive surgery? Surg Neurol. 2008;70:386–8. doi: 10.1016/j.surneu.2007.08.013. [DOI] [PubMed] [Google Scholar]
- 3.Epstein NE. Spine surgery in geriatric patients: Sometimes unnecessary, too much, or too little. Surg Neurol Int. 2011;2:188. doi: 10.4103/2152-7806.91408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Epstein NE. More nerve root injuries occur with minimally invasive lumbar surgery, especially extreme lateral interbody fusion: A review. Surg Neurol Int. 2016;7(Suppl 3):S83–95. doi: 10.4103/2152-7806.174895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guyer RD, Foley KT, Phillips FM, Ball PA. Minimally invasive fusion: Summary statement. Spine. 2003;28(15 Suppl):S44. doi: 10.1097/01.BRS.0000076897.87487.6D. [DOI] [PubMed] [Google Scholar]
- 6.Jin-Tao Q, Yu T, Mei W, Xu-Dong T, Tian-Jian Z, Guo-Hua S, et al. Comparison of MIS vs. open PLIF/TLIF with regard to clinical improvement, fusion rate, and incidence of major complication: A meta-analysis. Eur Spine J. 2015;24:1058–65. doi: 10.1007/s00586-015-3890-5. [DOI] [PubMed] [Google Scholar]
- 7.Lau D, Lee JG, Han SJ, Lu DC, Chou D. Complications and perioperative factors associated with learning the technique of minimally invasive transforaminal lumbar interbody fusion (TLIF) J Clin Neurosci. 2011;18:624–7. doi: 10.1016/j.jocn.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 8.Lee KH, Yeo W, Soeharno H, Yue WM. Learning curve of a complex surgical technique: Minimally invasive transforaminal lumbar interbody fusion (MIS TLIF) J Spinal Disord Tech. 2014;27:E234–40. doi: 10.1097/BSD.0000000000000089. [DOI] [PubMed] [Google Scholar]
- 9.Nandyala SV, Fineberg SJ, Pelton M, Singh K. Minimally invasive transforaminal lumbar interbody fusion: One surgeon's learning curve. Spine J. 2014;14:1460–5. doi: 10.1016/j.spinee.2013.08.045. [DOI] [PubMed] [Google Scholar]
- 10.Parker SL, Mendenhall SK, Shau DN, Zuckerman SL, Godil SS, Cheng JS, et al. Minimally invasive versus open transforaminal lumbar interbody fusion for degenerative spondylolisthesis: Comparative effectiveness and cost-utility analysis. World Neurosurg. 2014;82:230–8. doi: 10.1016/j.wneu.2013.01.041. [DOI] [PubMed] [Google Scholar]
- 11.Phan K, Huo YR, Hogan JA, Xu J, Dunn A, Cho SK, et al. Minimally invasive surgery in adult degenerative scoliosis: A systematic review and meta-analysis of decompression, anterior/lateral and posterior lumbar approaches. J Spine Surg. 2016;2:89–104. doi: 10.21037/jss.2016.06.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sclafani JA, Kim CW. Complications associated with the initial learning curve of minimally invasive spine surgery: A systematic review. Clin Orthop Relat Res. 2014;472:1711–7. doi: 10.1007/s11999-014-3495-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Silva PS, Pereira P, Monteiro P, Silva PA, Vaz R. Learning curve and complications of minimally invasive transforaminal lumbar interbody fusion. Neurosurg Focus. 2013;35:E7. doi: 10.3171/2013.5.FOCUS13157. [DOI] [PubMed] [Google Scholar]


