Abstract
Objective
To describe the rates and causes for rehospitalization over 10 years following moderate-severe traumatic brain injury (TBI), and to characterize longitudinal trajectories of the probability of rehospitalization using Generalized Linear Mixed Models (GLMM) and Individual Growth Curve (IGC) models conditioned on factors that help explain individual variability in rehospitalization risk over time.
Design
Secondary analysis of data from a multicenter longitudinal cohort study.
Setting
Acute inpatient rehabilitation facilities and community follow-up.
Participants
Individuals aged 16 years and older with a primary diagnosis of TBI.
Main Outcome Measures
Rehospitalization (and reason for rehospitalization) as reported by participants or proxy during follow-up telephone interviews at 1, 2, 5, and 10 years post-injury.
Results
The greatest number of rehospitalizations occurred in the first year post-injury (27.8% of the sample), and the rates of rehospitalization remained largely stable (22.1–23.4%) at 2, 5 and 10 years. Reasons for rehospitalization varied over time: Orthopedic and reconstructive surgery rehospitalizations were most common in Year 1, while General Health Maintenance was most common by Year 2 with rates increasing at each follow-up. Longitudinal models indicate multiple demographic and injury-related factors are associated with the probability of rehospitalization over time.
Conclusion
These findings can inform the content and timing of interventions to improve health and longevity after TBI.
Keywords: Traumatic Brain Injury, Chronic health, Longitudinal outcomes, Rehospitalization
Readmission to an acute care hospital in the years following inpatient rehabilitation for traumatic brain injury (TBI) may create financial burden, disrupt community integration, and raise risk for secondary health complications. Acute care rehospitalization, especially for specific causes, is a commonly used metric of care quality and has increasingly been requested for public reporting. There has been enhanced pressure in recent years on many rehabilitation payers and providers to reduce rehospitalizations during and after inpatient rehabilitation.1,2 Rehospitalization data can also provide an indicator of post-acute and longer-term health concerns among survivors of TBI. TBI is increasingly recognized as a chronic health condition due to the longstanding and sometimes lifelong persistence of injury-related symptoms and associated health problems3,4 and shortened lifespan compared to the general population has been well documented.5–8 Further focused study of acute care rehospitalizations after TBI is necessary to determine the rates, reasons, and risk factors associated with rehospitalization many years after TBI. This information can help identify prevention opportunities and inform the development of chronic care management guidelines to improve health following TBI.
Several studies have examined causes of rehospitalization in prevalent TBI samples. For example, one study of individuals who received inpatient rehabilitation for TBI found that 28% were rehospitalized at least once in the first 9 months after discharge, and the most frequent reasons for rehospitalization were infection, neurologic issues, neurosurgical procedures, injury, psychiatric, and orthopedic issues.9 Another study followed 504 Veterans with TBI for more than 4 years post hospital discharge and asked caregivers specifically about medically treated injuries after the index TBI.10 In this cohort, unintentional injury prompted 32% of the sample to experience 228 emergency room visits or hospitalizations.10 Previous research conducted using the Traumatic Brain Injury Model System (TBIMS) National Data Base (NDB) has examined rehospitalization up to 5 years post-injury in a variety of sub-samples, suggesting rehospitalization rates of 20–23% in the first two years after discharge from inpatient rehabilitation.11–13 Across TBIMS studies, results suggest that orthopedic and reconstructive surgeries, followed by infection, general health issues, and neurological problems, are the most frequent reasons for acute care readmission in the first year following discharge.11–13
Beyond characterizing rates and reasons for rehospitalization after TBI in the post-acute period, some studies have endeavored to identify factors associated with rehospitalization risk. A retrospective database study in Canada of 29,269 individuals with TBI discharged from acute care hospitals from 2002 – 2010 and followed up to 3 years found that 35.5% were rehospitalized, and significant predictors included male sex, older age, history of a fall, more severe TBI, rural residence, and greater comorbid health and mental health conditions.14 Similarly, previous research has found that increasing age and severity of comorbid health conditions were associated with increased rehospitalization.15,16 In addition, history of seizures prior to injury or during acute care or rehabilitation and a history of previous brain injuries also increased the likelihood of rehospitalization.9 Being injured in a motor vehicular crash and high motor functioning at discharge were associated with reduced rehospitalization.9 Prior studies that used the TBIMS NDB to examine rehospitalizations up to 5 years post injury have not found significant relationships between demographic or injury characteristics associated with rehospitalization,11,12 with the exception of one study of individuals with disorders of consciousness in which inability to follow commands at the time of inpatient rehabilitation admission was associated with a two-fold increased rate of rehospitalization.13
Prior research on rehospitalization after TBI has focused on a limited period of time post-injury (a few months to 5 years) and these studies have provided cross-sectional descriptions of rehospitalization rates. The current study uses the TBIMS NDB to provide an updated and expanded characterization of rehospitalizations after inpatient rehabilitation for TBI up to 10 years post-injury. Beyond identifying predictors of rehospitalization at specific points in time, here we identify factors that impact risk for rehospitalization over time at the individual level. The objectives of this study are to: (1) describe the rates and causes for rehospitalization in the years following moderate-severe TBI, and (2) characterize factors associated with rehospitalization 1–10 years after injury by modeling the probability of rehospitalization at the individual level over time. We examine all hospital readmissions, which include admission to an acute care hospital setting as well as readmission to inpatient rehabilitation. To better understand the factors associated with rehospitalization over time, Generalized Linear Mixed Modeling (GLMM) and Individual Growth Curve (IGC) modeling are used to investigate individual-level longitudinal trajectories representing the probability of being rehospitalized in the years following discharge from acute TBI rehabilitation.17,18 Together, these analyses highlight common conditions that result in rehospitalization among TBI survivors, and also allow for identification of patient characteristics that are associated with risk for rehospitalization over time.
Methods
Data source and participants
The TBIMS NDB is a multicenter prospective longitudinal study of TBI outcomes funded by the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR, formerly NIDRR) within the Agency on Community Living in Health and Human Services. Further information about the database, measures, and study protocols can be found at www.tbindsc.org. Individuals are enrolled in the TBIMS NDB if they have sustained a TBI as defined by at least 1 of the following characteristics: Glasgow Coma Scale score <13 on emergency admission (not because of intubation, sedation, or intoxication), loss of consciousness >30 minutes (not because of sedation or intoxication), posttraumatic amnesia >24 hours, or trauma-related intracranial abnormality on neuroimaging. All TBIMS NDB participants are age 16 or older at the time of injury, receive medical care in a TBIMS-affiliated trauma center within 72 hours of injury, are transferred to an affiliated inpatient TBI rehabilitation program, and provide informed consent or consent by legal proxy to participate. Participants or their proxies complete a brief assessment protocol during inpatient rehabilitation and are followed prospectively (1, 2, and 5 years post-injury and every 5 years thereafter) with a standardized follow-up assessment protocol.
Study Design
The first part of the current study uses a cross sectional cohort design to describe the rates and most common reasons for rehospitalization among TBI survivors at four different points in time: 1, 2, 5, and 10 years post-injury. The second part of this study uses a longitudinal cohort design to describe the probability of rehospitalization over time using GLMM and IGC analysis (further discussion of these methods can be found in Kozlowski et al, 201319 and Pretz et al, 201420). The use of both cross-sectional and longitudinal approaches in this project allows us to evaluate rehospitalization after TBI in complementary ways: we first characterize the rates and reasons for rehospitalization at four distinct time points, and then evaluate the factors that explain variability in risk for rehospitalization at the individual level over time.
Variables
Outcome measure: Rehospitalization
Information is collected from participants with TBI and/or their informants regarding whether they were rehospitalized after discharge from inpatient rehabilitation, as well as the primary reason(s) for each rehospitalization. The variable includes all types of causes for any inpatient admission greater than 24 hours in any hospital, but does not include emergency department or urgent care visits. From 1989–2002 participants were asked annually whether they had been hospitalized in the past year, and starting in 2004 (when the TBIMS replaced annual follow-ups with its current follow-up protocol of 1, 2, 5, and every 5 years thereafter) participants were asked whether they had been hospitalized in the past year (not since the past study assessment, which in some cases may have been up to 5 years prior). Data collectors are trained in coding reasons for each reported rehospitalization into one of eight categories (Rehabilitation, Seizures, Neurologic (e.g., repeat TBI, headaches, shunt revision), Psychiatric (e.g., depression, suicidality, substance abuse), Infectious (e.g., infection, pneumonia, hepatitis C), Orthopedic and Reconstructive Surgery (e.g., surgical repair of fractured bone, cranioplasty, back surgery), General Health unrelated to TBI (e.g., heart attack, dehydration, bowel obstruction), and Other. When the reason for rehospitalization was not known it was coded as such.
Demographic variables and covariate selection
Information about participants and their injuries was collected per standard TBIMS protocol. We characterize the sample included in the cross-sectional and longitudinal analyses according to age at the time of injury, sex, education at injury, race, rehabilitation length of stay (RLOS), employment status, residence at time of inpatient discharge, primary payor source for inpatient rehabilitation, and the cognitive and motor subscales of Functional Independence Measure (FIM™)21 performance at inpatient rehabilitation discharge (see Table 1). The FIM™ is an 18-item measure of functional independence,21 and the current study uses data collected at rehabilitation discharge on both the 13-item FIM™ motor and 5-item FIM™ cognitive subscales. Each item in these subscales is scored using a rating scale that ranges from 1 (total assistance) to 7 (complete independence), yielding a score range of 13 to 91 for the motor FIM™ and 5 to 35 for the cognitive FIM. ™ The listed covariates were selected a priori based on previous literature and clinical experience suggesting associations between covariates and rehospitalization or change in rehospitalization likelihood over time. Due to sample size restrictions in longitudinal analyses we limited the number of covariates included.
Table 1.
Demographic characterization of cross-sectional sample by rehospitalization status at 1, 2, 5 and 10 years post-injury
| Year 1 | Year 2 | Year 5 | Year 10 | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hospitalized | Hospitalized | Hospitalized | Hospitalized | |||||||||||||
| Overall | Yes | No | p | Overall | Yes | No | p | Overall | Yes | No | p | Overall | Yes | No | p | |
| N | 7503 | 2084 | 5419 | 6656 | 1531 | 5125 | 5443 | 1198 | 4245 | 2598 | 607 | 1991 | ||||
| % | 27.8 | 72.2 | 23.0 | 73.0 | 22.0 | 78.0 | 23.4 | 76.6 | ||||||||
| Gender (%) | c | |||||||||||||||
| Female | 26.7 | 26.7 | 26.7 | 26.9 | 27.8 | 26.6 | 27.8 | 32.5 | 26.5 | 27.5 | 28.0 | 27.3 | ||||
| Male | 73.3 | 73.3 | 73.3 | 73.1 | 72.2 | 73.4 | 72.2 | 67.5 | 73.5 | 72.5 | 72.0 | 72.7 | ||||
| Race (%) | a | |||||||||||||||
| White | 69.9 | 69.5 | 70.0 | 70.6 | 71.3 | 70.4 | 71.1 | 69.6 | 71.5 | 68.5 | 66.9 | 69.0 | ||||
| Black | 16.5 | 17.1 | 16.3 | 16.6 | 16.7 | 16.5 | 18.0 | 20.5 | 17.4 | 20.9 | 23.7 | 20.1 | ||||
| Hispanic | 9.6 | 9.9 | 9.5 | 9.0 | 8.6 | 9.1 | 7.1 | 6.3 | 7.4 | 6.5 | 4.6 | 7.1 | ||||
| Other | 4.0 | 3.5 | 4.2 | 3.9 | 3.3 | 4.1 | 3.7 | 3.7 | 3.8 | 4.1 | 4.8 | 3.9 | ||||
| Pre-Injury Employment Status (%) | ||||||||||||||||
| Employed | 62.5 | 56.7 | 64.7 | c | 63.7 | 56.0 | 66.0 | c | 66.1 | 57.5 | 68.6 | c | 69.1 | 58.0 | 72.5 | c |
| Student | 6.6 | 6.1 | 6.8 | 7.2 | 4.9 | 8.0 | 7.6 | 6.7 | 7.9 | 9.4 | 9.6 | 9.4 | ||||
| Retired | 16.3 | 21.7 | 14.2 | 14.8 | 21.7 | 12.8 | 11.9 | 19.5 | 9.7 | 7.2 | 13.6 | 5.2 | ||||
| Not Employed | 14.6 | 15.5 | 14.3 | 14.2 | 17.4 | 13.3 | 14.4 | 16.3 | 13.8 | 14.3 | 18.8 | 12.9 | ||||
| Primary Payment Source (%) | c | c | c | c | ||||||||||||
| Other | 53.7 | 48.6 | 55.7 | 54.7 | 43.8 | 57.9 | 55.6 | 47.0 | 58.0 | 56.7 | 49.1 | 59.0 | ||||
| Workers Compensation | 10.4 | 10.9 | 10.2 | 10.8 | 10.4 | 10.9 | 11.0 | 9.5 | 11.4 | 12.5 | 10.9 | 13.0 | ||||
| Medicare/Medicaid | 35.9 | 40.5 | 34.1 | 34.5 | 45.7 | 31.2 | 33.4 | 43.5 | 30.6 | 30.8 | 40.0 | 28.0 | ||||
| Education | c | b | a | |||||||||||||
| Greater than High School | 41.1 | 39.3 | 41.8 | 40.5 | 35.4 | 42.0 | 38.6 | 34.6 | 39.8 | 35.0 | 29.9 | 36.5 | ||||
| High School/GED | 35.8 | 37.4 | 35.2 | 35.9 | 37.3 | 35.5 | 34.9 | 35.3 | 34.7 | 34.8 | 38.4 | 33.7 | ||||
| Less than High School | 23.1 | 23.4 | 23.0 | 23.6 | 27.3 | 22.5 | 26.5 | 30.0 | 25.5 | 30.2 | 31.6 | 29.8 | ||||
| Residence at Discharge | c | c | c | c | ||||||||||||
| Private Residence | 82.8 | 74.9 | 85.8 | 83.8 | 77.0 | 85.9 | 86.0 | 81.9 | 87.2 | 88.2 | 82.7 | 89.9 | ||||
| Hospitals | 13.7 | 19.7 | 11.5 | 12.6 | 19.1 | 10.7 | 10.5 | 14.2 | 9.5 | 8.3 | 13.5 | 6.7 | ||||
| Other | 3.4 | 5.4 | 2.7 | 3.5 | 3.9 | 3.4 | 3.5 | 3.8 | 3.4 | 3.5 | 3.8 | 3.4 | ||||
| Age at Injury | 41.5 (19.5) | 44.5 (20.3) | 40.4 (19.0) | c | 40.3 (19.0) | 44.3 (20.0) | 39.1 (18.5) | c | 37.8 (17.4) | 42.2 (19.0) | 36.6 (16.8) | c | 34.3 (14.8) | 37.8 (16.2) | 33.3 (14.2) | c |
| Length of Stay Rehabilitation | 26.4 (25.3) | 30.5 (29.7) | 24.8 (23.1) | 26.5 (25.3) | 30.7 (31.4) | 25.3 (23.0) | 26.7 (25.4) | 27.6 (23.4) | 26.5 (25.9) | 26.3 (22.9) | 28.4 (26.7) | 25.7 (21.6) | ||||
| Discharge Cognitive FIM™ | 23.8 (6.7) | 22.6 (7.4) | 24.2 (6.4) | c | 23.8 (6.8) | 22.5 (7.4) | 24.3 (6.5) | c | 24.3 (6.7) | 23.6 (7.0) | 24.4 (6.6) | c | 24.8 (6.5) | 24.5 (6.7) | 24.9 (6.5) | c |
| Discharge Motor FIM™ | 65.8 (18.1) | 60.5 (19.7) | 67.8 (17.0) | c | 66.4 (18.3) | 61.1 (20.8) | 67.9 (17.2) | c | 68.4 (18.2) | 64.3 (19.5) | 69.6 (17.7) | c | 70.8 (17.9) | 68.2 (18.6) | 71.6 (17.6) | |
| Post Traumatic Amnesia | 23.3 (21.8) | 25.6 (24.3) | 22.5 (20.8) | c | 23.7 (21.8) | 25.5 (24.9) | 23.3 (20.8) | b | 24.0 (21.3) | 24.8 (22.2) | 23.7 (21.1) | 24.5 (21.1) | 24.8 (20.9) | 24.4 (21.1) | ||
Note. Proportions for categorical variables; means for continuous variables.
= p<= 0.05;
= p<= 0.01;
= p<= 0.001
Data Analysis
All data analyses were performed using SAS 9.4 or SPSS 19.0.22,23 First, we used descriptive statistics (percentages) to characterize the most common reasons for rehospitalization among TBI survivors at 1, 2, 5 and 10 years post-injury, and by calendar year between 2004–2014. Next, we employed a two-step process to illustrate the risk of being rehospitalized (for any reason, dichotomized as yes/no) longitudinally over time. The first step involved fitting a random intercept logistic generalized linear mixed model to generate logit based individual level temporal profiles. Only covariates that demonstrated a relationship with the outcome (p-value level of less than 0.05) were retained in the reduced model. A logit based profile was created for each individual in the database, and these profiles essentially serve as the data which are subsequently fit by way of random effects modeling i.e. IGC analysis in the second step. In the second step, we considered various unconditional models (models free of covariates) to determine which model optimally associates outcome (estimated logits) with time;24 we used AIC values to determine the best-fitting model which we then used to fit the data. We describe this longitudinal model by calculating estimates for the intercept, linear term, and quadratic term (i.e. growth parameters), and we explain variability across individuals by introducing covariates in a conditioned model and associations between the covariates and growth parameters were estimated. To enhance interpretably of the conditional model, all continuous covariates were centered about their respective means.19 The growth parameter estimates were transformed from logits to probabilities to enhance interpretability. To illustrate the complex relationships between growth parameters and covariates presented, we posted an interactive tool that encapsulates this information and reconfigures it into a user friendly visual format on the NDSC website (https://www.tbindsc.org/Researchers.aspx).
RESULTS
Description of Sample
The cross-sectional analyses reported below include all participants who were interviewed at each time point (1 year (n=7503), 2 years (n=6656), 5 years (n=5443), or 10 years (n=2598) post-injury) between 1/1/2004 and 10/1/2015). As seen in Table 1, individuals who are rehospitalized are more likely to be unemployed, on Medicare/Medicaid, and have lower education. Longitudinal analyses require at least three (not necessarily consecutive) three temporal measures to fit a model which, in combination with missing covariate values, reduces the number of participants in the longitudinal analyses to 2377. Accordingly, the samples included in the cross sectional and longitudinal analyses differ slightly in their composition. Participants included in the longitudinal models were younger (mean (standard deviation) 37.7 (17.0) versus 42.9 (20.1) years of age), performed higher on the FIM™ (67.6 (18.3) versus 65.3 (18.1)), and had longer duration of post-traumatic amnesia (PTA; 24.8 (23.0) versus 22.8 (21.3) days) compared to individuals who were included in cross-sectional analyses. The results of the longitudinal analyses are likely not representative of individuals who die soon after injury or who were recently added to the database.
Cross-sectional Analyses
We calculated the proportion of the sample that reported having been rehospitalized at each follow-up and found that 27.8% of participants were rehospitalized at year 1, 23.0% at year 2, 22.1% at year 5 and 23.4% at year 10.
Reasons for rehospitalization change slightly over time since injury. The data presented in Table 2 reflect the proportion of total rehospitalizations attributable to each reason category, not proportion of people rehospitalized; a single individual may have been rehospitalized more than once. Orthopedic and reconstructive surgeries account for the majority of (17.1%) of rehospitalizations in Year 1, which is unsurprising given that this category includes cranioplasty and other follow-up procedures to address concomitant injuries that are commonly addressed after acute and postacute TBI care needs have been addressed. The General Health category accounts for the largest proportion of rehospitalizations by Year 2 (18.7%) and this proportion increases in the later years post-injury (21.9% at Year 5 and 23.7% at Year 10). Seizures continue to be the 4th or 5th most common reason for rehospitalization in Years 2, 5, and 10. Psychiatric conditions are the only reason for rehospitalization that increases in absolute numbers after Year 1 and also accounts for a greater proportion of total rehospitalizations in Years 2, 5, and 10 compared to Year 1.
Table 2.
Reasons for Rehospitalizations at 1, 2, 5 and 10 year follow-up
| Year 1 | Year 2 | Year 5 | Year 10 | |
|---|---|---|---|---|
| Total number of rehospitalizations | 3,190 | 2,281 | 1,738 | 872 |
| Total number of people rehospitalized | 2084 | 1531 | 1198 | 607 |
| Reason | %(# subjects) | |||
| Orthopedic | 17.1% (458) | 15.3% (350) | 12.9% (199) | 11.8% (92) |
| Other | 16.1% (411) | 18.0% (329) | 22.3% (312) | 26.5% (187) |
| General Medical | 14.2% (367) | 18.7% (348) | 21.9% (308) | 23.7% (168) |
| Infection | 12.1% (294) | 11.0% (193) | 11.4% (161) | 10.4% (71) |
| Seizure | 11.6% (277) | 13.1% (228) | 12.1% (160) | 10.0% (67) |
| Rehabilitation | 10.4% (294) | 4.0% (81) | 2.9% (45) | 2.2% (14) |
| Neurological | 9.1% (245) | 6.5% (133) | 6.2% (96) | 3.9% (34) |
| Psychiatric | 6.0% (161) | 9.5% (176) | 7.4% (108) | 9.3% (69) |
| Unknown | 3.5% (34) | 3.8% (28) | 3.0% (19) | 2.2% (7) |
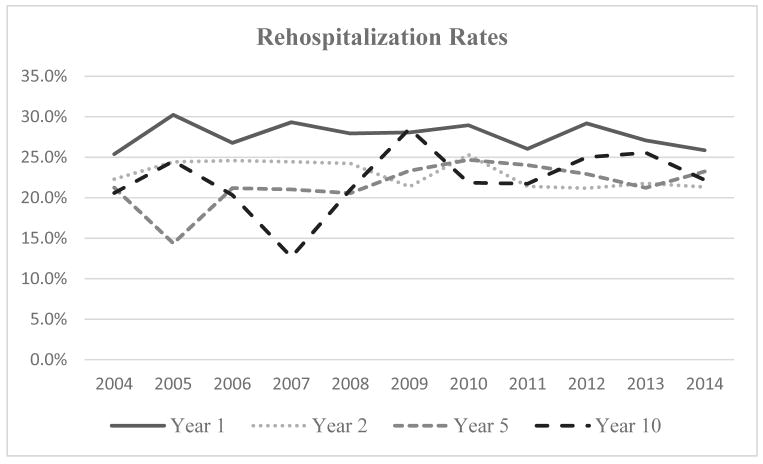
We also examined rates of rehospitalization by calendar year. Figure 1 displays rates of rehospitalization reported at follow-up between the years 2004–2014 by follow-up time point (1, 2, 5 and 10 years post-injury). Rates of rehospitalization have remained rather stable over this 10 year period.
Figure 1.
Percent of People Rehospitalized by Follow-up year and Year Interviewed.
Longitudinal Analyses
The first step in evaluating rehospitalization risk over time was to generate logit based individual level temporal profiles using a random intercept generalized linear mixed model. These profiles were estimated using a reduced model (presented in Table 3) which we built by removing covariates in which type III sums of squares analysis indicates a p-value level of less than 0.05.. As seen in Table 3, we adopted the customary approach of retaining the main effects in the model when the main effect was included in a significant interaction term.
Table 3.
Random Intercept Generalized Linear Mixed Model
| Covariate | F-Value | P-Value |
|---|---|---|
| Time | 6.34 | 0.0003 |
| Age at Injury | 26.13 | <.0001 |
| Race | 2.87 | 0.0350 |
| Gender | 2.05 | 0.1525 |
| Pre-Injury Employment Status | 4.67 | 0.0029 |
| Primary Payment Source | 12.30 | <.0001 |
| Residence at Discharge | 5.96 | 0.0026 |
| Cognitive FIM™ | 0.41 | 0.5227 |
| Motor FIM™ | 63.80 | <.0001 |
| Rehabilitation Length of Stay | 10.15 | 0.0015 |
| Education | 6.63 | 0.0013 |
| Time*Gender | 3.02 | 0.0287 |
| Time*Payer Source | 4.13 | 0.0004 |
| Time*Cognitive FIM™ | 6.80 | 0.0001 |
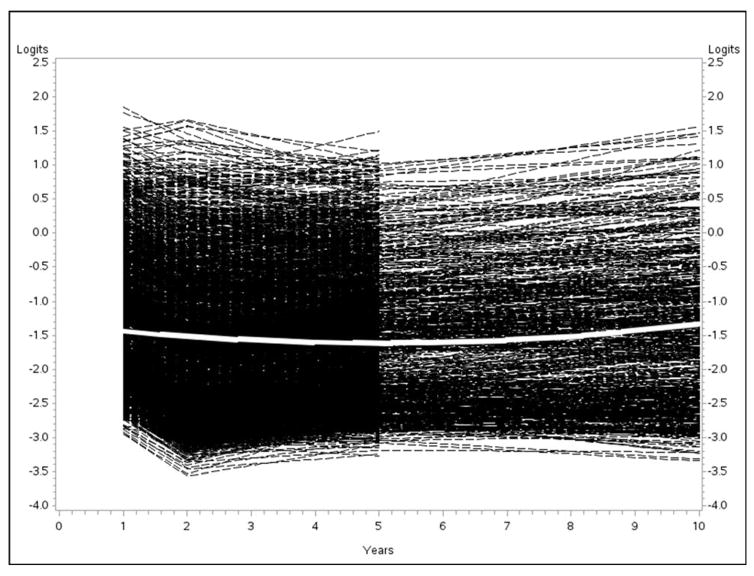
The logit based individual profiles are represented by black lines in Figure 2.
Figure 2.
Individual Profiles Based on Logits and Unconditional Model Trajectory
In the next step, we used the individual profiles generated in the first step to fit a random effects (i.e., IGC) model. To do this we evaluated various unconditional models and determined that a quadrating model best fit the data, as indicated by AIC value.24 The estimates for the growth parameters for the quadratic model (intercept, linear term, and quadratic term) are reported in Table 4.
Table 4.
Growth Parameter Estimates for the Unconditional Model (n=2377)
| Growth Parameter | Estimate | P-Value | Lower 95% CI | Upper 95% CI |
|---|---|---|---|---|
| Intercept | −1.3399 | <.0001 | −1.3852 | −1.2973 |
| Linear Term (Time) | −0.1094 | <.0001 | −0.1176 | −0.1013 |
| Quadratic Term (Time*Time) | 0.01103 | <.0001 | 0.01023 | 0.01184 |
To illustrate the group mean trajectory, in Figure 2 we have overlaid upon the individual profiles (black dashed-lines) a white curve which represents the trajectory associated with these growth. It is clear that considerable variability exists around that group mean trajectory, and to explain some of this variability across individuals we built a conditioned model (see Table 5) which included the covariates listed above. We estimated the associations between the covariates and growth parameters; covariates covariates that demonstrated significant relationships with the growth parameters and that had significant interactions with time are displayed in Table 5.
Table 5.
Conditional model for Rehospitalization risk over time (Estimates Given in Logits) (n=2377)
| Parameter | Estimate | P-Value | Lower 95% CI | Upper 95% CI |
|---|---|---|---|---|
| Intercept | −1.4994 | <.0001 | −1.6017 | −1.3972 |
| Time | −0.01729 | 0.0092 | −0.03030 | −0.00428 |
| Age at Injury | 0.01024 | <.0001 | 0.007960 | 0.01253 |
| Race = Black | 0.05735 | 0.1763 | −0.02579 | 0.1405 |
| Race = Hispanic | −0.04730 | 0.4703 | −0.1757 | 0.08113 |
| Race = Other | −0.4587 | <.0001 | −0.6410 | −0.2763 |
| Race = White (Reference) | 0 | . | . | . |
| Gender = Male | 0.2475 | <.0001 | 0.1718 | 0.3233 |
| Gender = Female (Reference) | 0 | . | . | . |
| Pre-Injury Employment Status = Not Employed | 0.3315 | <.0001 | 0.2343 | 0.4287 |
| Pre-Injury Employment Status = Retired | 0.2056 | 0.0014 | 0.07984 | 0.3314 |
| Pre-Injury Employment Status = Student | −0.1407 | 0.0330 | −0.2700 | −0.01135 |
| Pre-Injury Employment Status = Employed (Reference) | 0 | . | . | . |
| Primary Payment Source = Medicare/Medicaid | 0.1696 | <.0001 | 0.08948 | 0.2497 |
| Primary Payment Source = Workers Compensation | 0.4995 | <.0001 | 0.3875 | 0.6116 |
| Primary Payment Source = Other (Reference) | 0 | . | . | . |
| Residence at Discharge = Hospital | 0.3102 | <.0001 | 0.2025 | 0.4178 |
| Residence at Discharge = Other | 0.2805 | 0.0072 | 0.07588 | 0.4852 |
| Residence at Discharge = Private Residence (Reference) | 0 | . | . | . |
| Cognitive FIM™ | −0.02760 | <.0001 | −0.03378 | −0.02142 |
| Motor FIM™ | −0.01686 | <.0001 | −0.01900 | −0.01472 |
| Rehabilitation Length of Stay | 0.003612 | <.0001 | 0.002380 | 0.004843 |
| Education = High School/GED | −0.2404 | <.0001 | −0.3252 | −0.1557 |
| Education = More than High School | −0.3532 | <.0001 | −0.4400 | −0.2664 |
| Education = Less than High School (Reference) | 0 | . | . | . |
| Time* Gender = Male | −0.1285 | <.0001 | −0.1425 | −0.1144 |
| Time* Gender = Female (Reference) | 0 | . | . | . |
| Time*Primary Payment Source = Medicare/Medicaid | 0.05590 | <.0001 | 0.04221 | 0.06959 |
| Time*Primary Payment Source = Workers Compensation | −0.1754 | <.0001 | −0.1958 | −0.1551 |
| Time*Primary Payment Source = Other (Reference) | 0 | . | . | . |
| Time* Cognitive FIM™ | 0.02114 | <.0001 | 0.02018 | 0.02211 |
| Time*Time | 0.005929 | <.0001 | 0.004653 | 0.007204 |
| Time*Time* Gender = Male | 0.006015 | <.0001 | 0.004635 | 0.007394 |
| Time*Time* Gender = Female (Reference) | 0 | . | . | . |
| Time*Time*Primary Payment Source = Medicare/Medicaid | −0.00087 | 0.2107 | −0.00224 | 0.000495 |
| Time*Time*Primary Payment Source = Workers Compensation | 0.01276 | <.0001 | 0.01083 | 0.01470 |
| Time*Time*Primary Payment Source = Other (Reference) | 0 | . | . | . |
| Time*Time* Cognitive FIM™ | −0.00194 | <.0001 | −0.00203 | −0.00184 |
The estimates in Table 5 are given in terms of logits, though these were subsequently transformed into probabilities to enhance interpretability. The growth parameters and covariate associations were able to be estimated with considerable accuracy, as reflected by the narrow width of the 95% confidence intervals.
Due to the complex system of relationships between growth parameters and covariates presented in Table 5, we created an interactive tool that encapsulates this information and reconfigures it into a user friendly visual format. The interactive tool generates individual-level trajectories based on both logits and probability of re-hospitalization for specified covariate values. The interactive tool is provided on the NDSC website (https://www.tbindsc.org/Researchers.aspx).
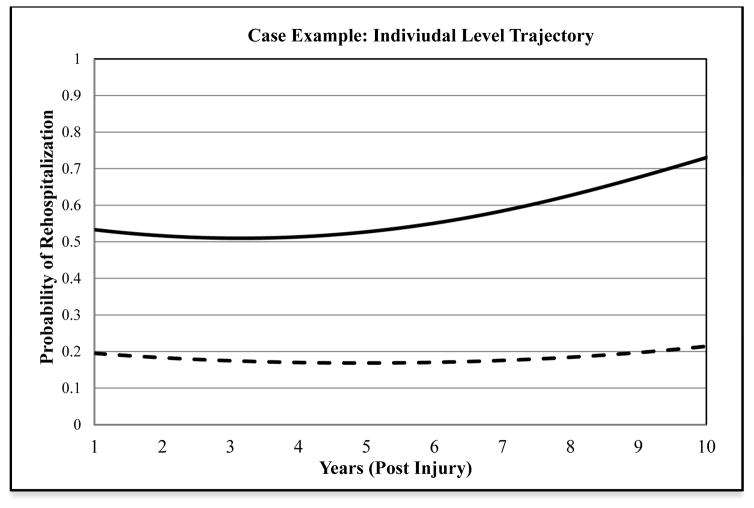
To illustrate the impact of demographic and injury information on risk (probability) for rehospitalization over time, a case example is provided. In Figure 3, the average trajectory of risk for the longitudinal sample is contrasted with the risk trajectory for individuals who were Black Hispanic female, aged 70 years, unemployed prior to injury, received insurance coverage through Medicare or Medicaid, were discharged to an institutional setting (as opposed to home) after inpatient rehabilitation, had a Cognitive FIM score of 16 and Motor FIM score of 35 at rehabilitation discharge, and whose rehabilitation length of stay lasted 40 days. As seen in Figure 3, individuals with this combination of characteristics differ markedly in rehospitalization risk from the group mean. Their risk for rehospitalization is higher at the intercept, and risk increases over time with most marked increase in risk starting at around 5 years post-injury. This example illustrates only one of countless trajectories of individual level change with regard to probability of re-hospitalization. We encourage readers to enter any plausible combination of covariate values into the interactive tool to investigate how individual and injury characteristics produce different trajectories of risk over time.
Figure 3.
Sample individual-level trajectory of rehospitalization risk compared to group mean.
Note. The black line trajectory demonstrates individual-level probability of rehospitalization for individuals in the NDB with the following characteristics: Black, female, age 70 years, high school education, unemployed prior to injury, receives Medicare or Medicaid, and were discharged after 40 days of inpatient rehabilitation to an institutional setting with Cognitive FIM = 16 and Motor FIM = 35. The dashed line represents the average trajectory for the full longitudinal sample.
DISCUSSION
The current study examined rehospitalization cross-sectionally and over time for individuals in the TBIMS NDB for up to 10 years after discharge from inpatient rehabilitation. Rates of rehospitalization have been examined previously11–13 in subsamples of the TBIMS NDB, and the current study builds on that literature by including a longer duration of follow-up and incorporating GLMM and IGC models to evaluate factors the impact risk for rehospitalization at the individual level over time. Results suggest that rates of rehospitalization are highest in the first year after injury (27.8%), with many of those hospitalizations being attributable to orthopedic causes possibly related to the injury itself. Rates of rehospitalization, on average, remain quite consistent (22–23.4%) across the next 3 time points (2, 5, and 10 years post injury), but a large proportion of these rehospitalizations are attributed to general health reasons and “Other,” possibly reflecting an increase in comorbid health issues and overall disease burden in the later years after TBI. This notion is consistent with recent literature that suggests TBI is best conceptualized for some survivors as an evolving disease process in which the injury initiates or exacerbates other health conditions.3,4 Similarly, the current study found that psychiatric rehospitalizations actually increase over time, which is consistent with the finding that psychiatric and mood disorders can develop in the post-acute period after TBI and persist at rates that well exceed those seen in the general population.25
Analyses of rehospitalization rates by calendar year indicate there has been no major change in rates of rehospitalization for any follow-up time point over the past 10 years. Over this period of time, a variety of changes in the health care landscape have occurred, including the reauthorization of the TBI Act in 2000,26 recommendations from the Institute of Medicine (2009) that full access to the entire spectrum of care be available to patients,27 and the passing of the Patient Protection and Affordable Care Act of 2010,28 each of which would theoretically enhance TBI survivors’ ability to access follow-up medical care. On the other hand, Data from the Uniform Data System for Medical Rehabilitation indicate that inpatient rehabilitation length of stay has decreased steadily between the years of 1999–2008,29 and a recent study found that shorter inpatient length of stay was associated with a decrease in the level of functioning at rehabilitation discharge and at one year post injury30 which may result in greater long-term care needs. Full consideration of the factors that may impact rates of rehospitalization over a particular time period falls outside the scope of this project, but the lack of change over this 10 year period certainly suggests that there remains room for improvement in long-term health management provided to TBI survivors.
The longitudinal analyses conducted here provide a nuanced understanding of the interaction of demographic and injury variables on individual level probabilities of rehospitalization over time. When examined individually, certain factors (older age at the time of injury, being unemployed, lower educational attainment, and receiving Medicare/Medicaid) are associated with higher rates of rehospitalization at most follow-up time points. These associations, while useful in broadly identifying high risk groups, do not allow for characterization of individual-level risk dynamically over time. Patients and their families are most interested in knowing detailed information about prognosis and long-term outcomes that are relevant to their loved one.31 As demonstrated here, the interactive tool - can create individual-level trajectories of rehospitalization risk that describe data gathered through the TBIMS from individuals with a particular constellation of demographic and injury characteristics. Also consistent with the current study’s goal of describing all rehospitalizations more comprehensively than has been possible in previous efforts, it should be noted that the longitudinal models presented here include rehospitalizations for rehabilitation. Overall the number of rehospitalizations for rehabilitation was low at each time point, and excluding rehabilitation rehospitalizations from longitudinal analyses did not significantly impact the estimates of fixed effects in the conditional model presented above (sensitivity analyses not presented here). Given that rehospitalization for inpatient rehabilitation could reflect functional improvement (such as individuals who are readmitted for intensive rehabilitation after emerging from prolonged disorders of consciousness13 or functional deterioration (debility following acute illness or clinical frailty) that requires intervention, it is difficult to interpret rehabilitation rehospitalizations with the data available. No prior studies specifically focused on readmission to inpatient rehabilitation after the initial inpatient rehabilitation stay.
The current study has limitations that should be considered. The TBIMS NDB includes data collected on individuals who received care at specialized centers for TBI rehabilitation, and thus, the findings presented here may not generalize to all TBI survivors. Rehospitalization data were based on self-report from people with TBI or their proxy, and may be subject to recall bias. The broad coding scheme used to categorize reasons for rehospitalization precludes more detailed analyses of factors surrounding rehospitalizations such as whether a given hospitalization is elective, planned, preventative, or corrective. Within a given reason category, some rehospitalizations may represent improvement or progress (e.g., removal of hardware) and others may represent decline or deterioration (e.g., hip fracture resulting from a fall 5 years after the initial TBI). It is important to note that this study examined rehospitalization during a specific interview year, and does not represent cumulative rehospitalization of 10 years following TBI. With respect to the longitudinal analyses presented here, it is worth noting that the analytic methods require a “double estimation” process in which a set of temporal logits is estimated per individual using a generalized linear mixed model, and then patterns in the logits are evaluated by way of IGC analysis. Such an estimation process introduces additional error, though error remains relatively small due to the large study sample. Moreover, the transformation from logits to probabilities requires a transformation from an infinite scale (logits) to a bounded scale (0 to 1 for probabilities), and thus trajectories on the logit scale will not directly mirror trajectories conformed to probabilities. Due to the descriptive focus of the study, comparison between trajectories should be made based on clinical relevance alone; in other words, the study is not inferential in nature. Study trajectories are mathematical representations based on the associations between identified covariates and the growth parameters and are representative of the data at hand. Caution is warranted in using these models to inform prognosis for individual patients. Additional factors that may impact rehospitalization risk such as overall medical disease burden, family support, access to health care, health self-management skills, and cognitive functioning are not included in the current models, so it is important to note that individuals with a TBI may not be constrained to their corresponding trajectory.
Conclusions
Individuals who survive a moderate-severe TBI can experience a wide range of long-term health and functional outcomes, and rehospitalization provides a proxy indicator of medical need after rehabilitation discharge. Rehospitalization is particularly common in the first year after injury, as the early post-acute period is often characterized by high care needs resulting from complications of TBI in addition to ongoing medical intervention for concomitant extracranial injuries. Decreasing length of hospital stays heightens the need for intensive discharge care planning. In the current study, rates of rehospitalizations for general health maintenance increased across the follow-up period, suggesting a role for a chronic disease management model in improving long-term health care for TBI survivors. Longitudinal models presented here indicate multiple demographic and injury-related factors impact the probability of rehospitalization over time, and across these diverse individual-level longitudinal trajectories, a pattern emerges in which risk for rehospitalization begins to increase around 5 years post-injury. These findings suggest that long-term health management interventions are needed after TBI and the content and timing of these efforts can be informed by the descriptive trajectories of TBIMS NDB participants such as those presented here.
Acknowledgments
Source of Funding
This work was funded by Grants from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR) to the Traumatic Brain Injury Model Systems National Data and Statistical Center (Grant Number is 90DP0010-01-00), the New York TBI Model System (Grant Number 90DP0038-02-00), Indiana University/Rehabilitation Hospital of Indiana TBI Model System (Grant Number 90DP0036-01-00), University of Washington Traumatic Brain Injury Model System (Grant Number 90DP0031-01-00), Spaulding – Harvard TBI Model System (Grant Number 2012P002490), University of Alabama at Birmingham Traumatic Brain Injury Care System (Grant Number 90DP0044-01-00), and by a grant from the National Institutes of Health, National Institute of Child Health and Development (Grant Number K01HD074651–01A1).
Footnotes
Conflicts of Interest
We certify that no party having a direct interest in the results of the research supporting this article has or will confer a benefit on us or on any organization with which we are associated AND we certify that all financial and material support for this research are clearly identified in the title page of the manuscript.
References
- 1.Centers for Medicare & Medicaid Services. Specifications for the All-Cause Unplanned Readmission Measure for 30 Days Post Discharge from Inpatient Rehabilitation Facilities. Washington, DC: Centers for Medicare & Medicaid Services; 2013. [Google Scholar]
- 2.Ottenbacher KJ, Karmarkar A, Graham JE, et al. Thirty-day hospital readmission following discharge from postacute rehabilitation in fee-for-service Medicare patients. JAMA. 2014;311(6):604–614. doi: 10.1001/jama.2014.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Masel BE. The chronic consequences of neurotrauma. J Neurotrauma. 2015;32(23):1833. doi: 10.1089/neu.2015.29004.bm. [DOI] [PubMed] [Google Scholar]
- 4.Masel BE, DeWitt DS. Traumatic brain injury: a disease process, not an event. J Neurotrauma. 2010;27(8):1529–1540. doi: 10.1089/neu.2010.1358. [DOI] [PubMed] [Google Scholar]
- 5.Harrison-Felix C, Whiteneck G, Devivo MJ, Hammond FM, Jha A. Causes of death following 1 year postinjury among individuals with traumatic brain injury. J Head Trauma Rehabil. 2006;21(1):22–33. doi: 10.1097/00001199-200601000-00003. [DOI] [PubMed] [Google Scholar]
- 6.McMillan TM, Teasdale GM. Death rate is increased for at least 7 years after head injury: a prospective study. Brain. 2007;130(Pt 10):2520–2527. doi: 10.1093/brain/awm185. [DOI] [PubMed] [Google Scholar]
- 7.Ventura T, Harrison-Felix C, Carlson N, et al. Mortality after discharge from acute care hospitalization with traumatic brain injury: a population-based study. Arch Phys Med Rehabil. 2010;91(1):20–29. doi: 10.1016/j.apmr.2009.08.151. [DOI] [PubMed] [Google Scholar]
- 8.Selassie AW, McCarthy ML, Ferguson PL, Tian J, Langlois JA. Risk of posthospitalization mortality among persons with traumatic brain injury, South Carolina 1999–2001. J Head Trauma Rehabil. 2005;20(3):257–269. doi: 10.1097/00001199-200505000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Hammond FM, Horn SD, Smout RJ, et al. Rehospitalization during 9 months after inpatient rehabilitation for traumatic brain injury. Arch Phys Med Rehabil. 2015;96(8 suppl):S330–S339. doi: 10.1016/j.apmr.2014.09.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carlson KF, Meis LA, Jensen AC, et al. Caregiver reports of subsequent injuries among veterans with traumatic brain injury after discharge from inpatient polytrauma rehabilitation programs. J Head Trauma Rehabil. 2012;27(1):14–25. doi: 10.1097/HTR.0b013e318236bd86. [DOI] [PubMed] [Google Scholar]
- 11.Cifu DX, Kreutzer JS, Marwitz JH, et al. Etiology and incidence of rehospitalization after traumatic brain injury: a multicenter analysis. Arch Phys Med Rehabil. 1999;80(1):85–90. doi: 10.1016/s0003-9993(99)90312-x. [DOI] [PubMed] [Google Scholar]
- 12.Marwitz JH, Cifu DX, Englander J, High WM., Jr A multi-center analysis of rehospitalizations five years after brain injury. J Head Trauma Rehabil. 2001;16(4):307–317. doi: 10.1097/00001199-200108000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Nakase-Richardson R, Tran J, Cifu D, et al. Do rehospitalization rates differ among injury severity levels in the NIDRR Traumatic Brain Injury Model Systems program? Arch Phys Med Rehabil. 2013;94(10):1884–1890. doi: 10.1016/j.apmr.2012.11.054. [DOI] [PubMed] [Google Scholar]
- 14.Saverino C, Swaine B, Jaglal S, et al. Rehospitalization after traumatic brain injury: a population-based study. Arch Phys Med Rehabil. 2016;97(2 suppl):S19–S25. doi: 10.1016/j.apmr.2015.04.016. [DOI] [PubMed] [Google Scholar]
- 15.Boaz TL, Becker MA, Andel R, McCutchan N. Rehospitalization risk factors for psychiatric treatment among elderly Medicaid beneficiaries following hospitalization for a physical health condition. Aging Ment Health. 2015:1–7. doi: 10.1080/13607863.2015.1104532. [DOI] [PubMed] [Google Scholar]
- 16.Davydow DS, Zivin K, Katon WJ, et al. Neuropsychiatric disorders and potentially preventable hospitalizations in a prospective cohort study of older Americans. J Gen Intern Med. 2014;29(10):1362–1371. doi: 10.1007/s11606-014-2916-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cuthbert JP, Pretz CR, Bushnik T, et al. Ten-year employment patterns of working age individuals after moderate to severe traumatic brain injury: a National Institute on Disability and Rehabilitation Research Traumatic Brain Injury Model Systems study. Arch Phys Med Rehabil. 2015;96(12):2128–2136. doi: 10.1016/j.apmr.2015.07.020. [DOI] [PubMed] [Google Scholar]
- 18.Pretz CR. Combining Generalized Linear Mixed Modeling and Random Effects Modeling to provide a comprehensive understanding of individual level change in probability of outcome over time. Paper presented at: Joint Statistical Meetings; 2015; Seattle, WA. [Google Scholar]
- 19.Kozlowski AJ, Pretz CR, Dams-O’Connor K, Kreider S, Whiteneck G. An introduction to applying individual growth curve models to evaluate change in rehabilitation: a National Institute on Disability and Rehabilitation Research Traumatic Brain Injury Model Systems report. Arch Phys Med Rehabil. 2013;94(3):589–596. doi: 10.1016/j.apmr.2012.08.199. [DOI] [PubMed] [Google Scholar]
- 20.Pretz CR, Ketchum JM, Cuthbert JP. An introduction to analyzing dichotomous outcomes in a longitudinal setting: a NIDRR traumatic brain injury model systems communication. J Head Trauma Rehabil. 2014;29(5):E65–71. doi: 10.1097/HTR.0000000000000025. [DOI] [PubMed] [Google Scholar]
- 21.Granger CV, Deutsch A, Russell C, Black T, Ottenbacher KJ. Modifications of the FIM instrument under the inpatient rehabilitation facility prospective payment system. Am J Phys Med Rehabil. 2007;86(11):883–892. doi: 10.1097/PHM.0b013e318152058a. [DOI] [PubMed] [Google Scholar]
- 22.SAS [computer program]. Version 9.4. Cary, NC: SAS Institute Inc; 2013. [Google Scholar]
- 23.IBM SPSS Statistics for Windows [computer program]. Version 19.0. Armonk, NY: IBM Corp; 2010. [Google Scholar]
- 24.Pretz CR, Kozlowski AJ, Dams-O’Connor K, et al. Descriptive modeling of longitudinal outcome measures in traumatic brain injury: a National Institute on Disability and Rehabilitation Research Traumatic Brain Injury Model Systems study. Arch Phys Med Rehabil. 2013;94(3):579–588. doi: 10.1016/j.apmr.2012.08.197. [DOI] [PubMed] [Google Scholar]
- 25.Zgaljardic DJ, Seale GS, Schaefer LA, Temple RO, Foreman J, Elliott TR. Psychiatric disease and post-acute traumatic brain injury. J Neurotrauma. 2015;32(23):1911–1925. doi: 10.1089/neu.2014.3569. [DOI] [PubMed] [Google Scholar]
- 26.Title XIII of the Children’s Health Act of 2000: The Traumatic Brain Injury Act Amendments, Pub L No. 106–310, 114 Stat. 1101 (2000).
- 27.Institute of Medicine. Gulf War and Health: Volume 7: Long-Term Consequences of Traumatic Brain Injury. Washington, DC: The National Academies Press; 2009. [PubMed] [Google Scholar]
- 28.Patient Protection and Affordable Care Act, 42 USC §18001 et seq. (2010).
- 29.Granger CV, Markello SJ, Graham JE, Deutsch A, Reistetter TA, Ottenbacher KJ. The uniform data system for medical rehabilitation: report of patients with lower limb joint replacement discharged from rehabilitation programs in 2000–2007. Am J Phys Med Rehabil. 2010;89(10):781–794. doi: 10.1097/PHM.0b013e3181f1c83a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ashley J, Kreber L, Seneca P, et al. Recovery trajectories following traumatic brain injury. Poster presented at: Second Annual Santa Clara Valley Brain Injury Conference; 2012; San Jose, CA. [Google Scholar]
- 31.Biester RC, Krych D, Schmidt MJ, et al. Individuals with traumatic brain injury and their significant others’ perceptions of information given about the nature and possible consequences of brain injury: analysis of a national survey. Prof Case Manag. 2016;21(1):22–33. doi: 10.1097/NCM.0000000000000121. [DOI] [PubMed] [Google Scholar]