Abstract
Objective:
Sunken temporal fossa appears oftentimes in Asians and resembles bad fortune that people wish to change. Numerous techniques and materials have been applied clinically for augmenting the sunken temporal fossa with variable results. The microautologous fat transplantation (MAFT) technique proposed by Lin et al in 2006 has demonstrated favorable results in facial rejuvenation. In the present study, the authors applied the MAFT technique with an innovative instrument in sunken temporal fossa and reported its results.
Methods:
Microautologous fat transplantation was performed on 208 patients during the 4-year period starting in January 2010. Fat was harvested by liposuction, processed and refined by centrifugation at 1200 g for 3 minutes. Then purified fat was microtransplanted to the temporal fossa with the assistance of an instrument, MAFT-Gun. The patients were followed up regularly and photographs were taken for comparison.
Results:
On average, the MAFT procedure took 48 minutes to complete. The average delivered fat was 6.8 ± 0.2 mL/6.5 ± 0.3 mL for the right/left side. The average follow-up period was 18 months. No complication including skin necrosis, vascular compromise, nodulation, fibrosis, and asymmetry was noted. The patient-rated satisfaction 5-point Likert scale demonstrated that 81.3% of all patients had favorable results (38.5% very satisfied and 42.8% satisfied).
Conclusions:
The concept and technique of MAFT along with the micro- and precise controlling instrument enabled surgeons to perform fat grafting accurately and consistently. In comparison with other strategies for volume restoration, the MAFT procedure demonstrated the patients’ high satisfaction with the long-term results. Therefore, the potential of MAFT as an alternative strategy in sunken temporal fossa in Asians was emphasized.
Keywords: Fat graft, microautologous fat transplantation, sunken temporal fossa
Temple site of human is called “temporal” in medicine. Temporal hollowing (sunken or depression of temporal fossa) affects half of the people on the face shape contours to others feeling little face big head, giving a sarcastic sense. In Asian populations, temporal shaping can easily be overlooked, but the temporal shaping of coordination can bring significant people who had scar, birthmark, mole, and depression unhappy married lives and frustration.
A systematic review of the literature demonstrated that the technique for the correction of temporal hollowing seemed to be the use of nonbiologic materials since the 1970s.1–3 These materials have been used successfully but were associated with some complications. For the past 2 decades, there has been a growing experience with augmentation of the soft tissues of the temporal fossa using fillers.4,5 However, the high complications as allergic reaction (25%), filler material migration (12.5%), injection necrosis and embolism (25%), and foreign body granuloma (37.5%) were reported by Lee et al.6 The ideal strategy for volume restoration to temporal hollowing was not shown yet.
In 1893, German surgeon Neuber7 reported the first fat grafting. It has become a common procedure because of the ease of harvest, abundant volume, and no rejection reaction. However, survival and retention rates are unpredictable, and morbidities such as abscess, cyst formation, nodulation, or neurovascular injury have been reported.8 Structural fat grafting has received extensive attention and has demonstrated acceptable clinical outcomes.9 Lin et al proposed the concept of microautologous fat transplantation (MAFT) in 2006, and demonstrated its reliability in facial rejuvenation.10–15 In the present study, we applied the MAFT with new maneuver in the treatment of sunken temporal fossa and achieved favorable long-term result.
METHODS
Patient Demographics
Exclusive of any history of trauma or filler injection in the temporal area, consecutive 208 patients who underwent MAFT for the correction of the sunken temporal fossa between January 2010 and December 2014 were retrospectively analyzed. Photos were taken at each visit and compared pre- and postoperatively. Regular follow-up was conducted at an outpatient clinic at 1 month, 3 months, and 12 months (or longer where possible) after MAFT.
Preoperative Planning and Photography
All the patients were followed a standard operative procedure for preoperative photography after a signed consent. There were 7 basic photos taken including AP view, quarter views (right and left), profile views (right and left), chin-up view (waters view), and chin-down view (helicopter view). Before the operation, the surgical planning of sunken temporal fossa was outlined, as shown in Figure 1A to D.
FIGURE 1.
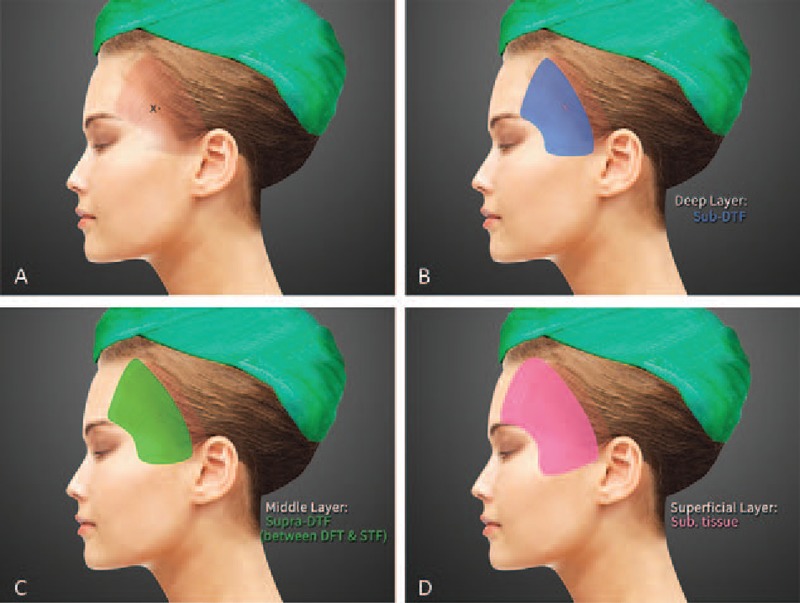
(A) The surgical planning of sunken temporal fossa is outlined as brown shadow. The X point is the insertion site made by #11 blade. (B) Deep layer is highlighted (in blue) to be bounded by temporal fusion line, lateral orbital rim, and zygomatic arch. (C) Middle layer in green (an areolar space between deep temporal fascia and superficial temporal fascia) is slight extended over the boundary of temporal fossa. (D) Superficial subcutaneous layer shown in pink is designed to act as a smooth tailoring over the boundary.
Anesthesiology Method
During the MAFT procedure, the patients were under total intravenous anesthesia. The fat-harvesting area, mostly in the lower abdomen (or thighs), was preinfiltrated with a tumescent solution prepared with the ratio of 10 mL of 2% lidocaine (20 mg/mL): 30 mL of Ringer lactate solution: 0.2 mL of epinephrine (1:1000). Appropriate local anesthesia was applied to the insertion sites of recipient, normally the pivot point in the temporal hair line (X point in Fig. 1A).
Microautologous Fat Transplantation Procedure
Harvesting of Fat
Approximately 15 to 20 minutes after tumescent infiltration, the fat was harvested using a blunt tip cannula (diameter, 2.5 mm or 3.0 mm, with 1 side hole). The lipoaspirate volume was suggested to be the same amount of tumescent solution preinfiltrated to ensure a high ratio of purified fat after processing by centrifugation. To minimize damage to the lipoaspirate, the plunger of a 10-mL syringe connected to the liposuction cannula was back pulled to approximately 2 to 3 mL to maintain the negative pressure between 270 and 330 mm Hg.10
Processing and Refinement of Fat
In accordance with the technique proposed by Coleman,9 a standard centrifugation of 3000 rpm (approximately 1200 g) was applied for 3 minutes to process and purify the lipoaspirated fat by using desktop centrifuge.
Transferring of Fat
The purified fat was carefully transferred into a 1 cc luer-slip syringe by using a transducer, and the fat prepared for transplantation after removing the blood content from the bottom layer and oil from the upper layer.
Transplantation of Fat
After the purified fat was transferred, the fat-filled syringe was loaded into a MAFT-GUN (Dermato Plastica Beauty Co, Ltd, Kaohsiung, Taiwan) (Fig. 2). The volume of the fat parcel injected by each triggering was set by adjusting a 6-graded dial (Fig. 2) for controlling the total injection frequency per 1 mL of fat graft. An 18-G blunt cannula was employed to inject the fat while withdrawing the MAFT-Gun. Each delivered fat parcel was set at 1/120 or 1/150 mL (each parcel volume 0.0083 or 0.0067 mL) and meticulously transplanted in 3 levels to the temporal fossa: the deeper layer, beneath the deep temporal fascia (DTF) (through temporalis muscle deep to temporal bone); middle layer, an areolar space between DTF to superficial temporal fascia (STF), and the superficial layer, subcutaneous layer (Figs. 1B–D and 3). The maneuver performed to transplant the fat graft was demonstrated in Supplemental Digital Content, Videos 1 and 2.
FIGURE 2.

The panorama of MAFT-GUN 3.0 (Dermato Plastica Beauty Co Ltd, Taiwan). The predetermined volume for each fat parcel is set at 0.0067 (1/150) mL (or 0.0083, 1/120 mL) by adjusting the 6-graded dial to 150 or 120.
FIGURE 3.
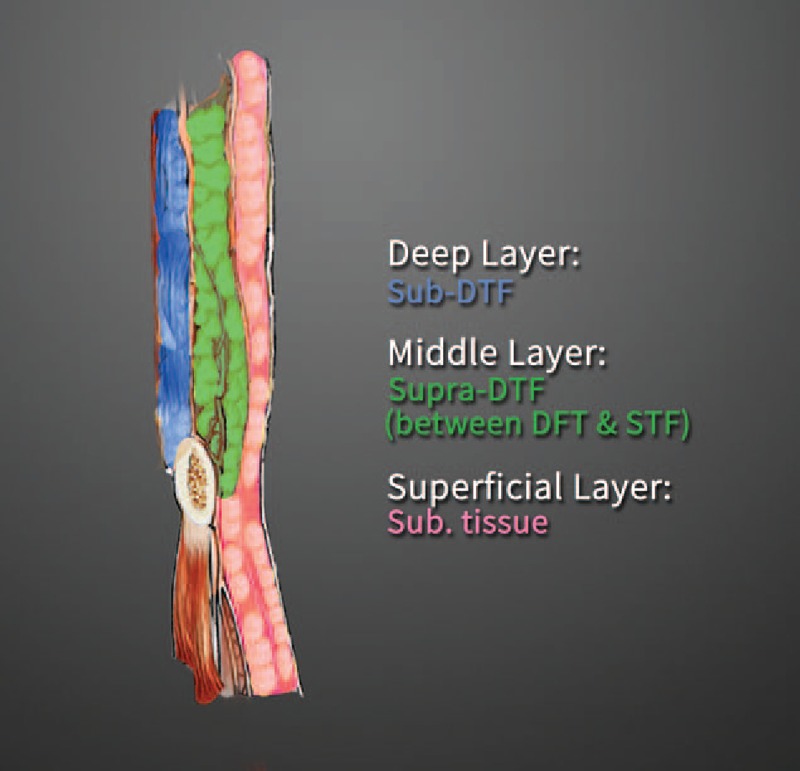
The coronal section of temporal fossa is shown to illustrate the deeper layer (blue), middle layer (green), and superficial layer (pink) with the transplantation of micro-fat parcels at size of 1/120 mL (0.0083) or 1/150 mL (0.0067).
Regular postoperative care and oral antibiotic and nonsteroid antiinflammatory drugs were administered for 3 days when necessary. No massaging was performed following the MAFT procedure. A gentle lymphatic-drain massage was encouraged 7 days after surgery.
Patient-rated satisfaction using a typical Likert scale “very unsatisfied, unsatisfied, neutral, satisfied, very satisfied” was obtained during patient's final visit (at 6 months after last MAFT) anonymously conducted by office staff (Table 1).
TABLE 1.
Patient Satisfaction Score With Microautologous Fat Transplantation for Sunken Temporal Fossa (n = 208)
| n = 208 | Very Unsatisfied (%) | Unsatisfied (%) | Neutral (%) | Satisfied (%) | Very Satisfied (%) | |
| One session | 168 | 0 | 5 (3.0) | 33 (19.6) | 85 (50.6) | 45 (26.8) |
| Two sessions | 40 | 0 | 0 | 1 (2.5) | 4 (10.0) | 35 (87.5) |
| 208 | 0 | 5 (2.4) | 34 (16.3) | 89 (42.8) | 80 (38.5) |
RESULTS
The mean age of the 208 patients was 43.3 years (range, 26–60 years). The entire MAFT procedure (from harvesting to transplantation) took an average of 48 minutes to complete. On average, the fat volume delivered in this study was 6.8 ± 0.2 and 6.5 ± 0.3 mL on the right and left sides respectively. All the patients were monitored for an average of 18 months (ranging from 10 to 52 months). No major complications (eg, infection, skin necrosis, nodulation, fibrosis, asymmetry, or vascular insults) were recorded. Patient-rated satisfaction scores (Table 1) obtained during their final visit showed that 26.8% (45/168) very satisfied, 50.6% satisfied (85/168), and 19.6% (33/168) with the outcome after 1 MAFT session. There were 40 patients (19.2%, 40/208) who requested a second session of MAFT (touchup) to further augmentation and contouring. The scores in the 2 session groups were 87.5% (35/40) very satisfied, 10% satisfied (4/40), and 2.5% (1/40) neutral. Five patients after MAFT for sunken temporal fossa were illustrated in Figures 4 to 7.
FIGURE 4.
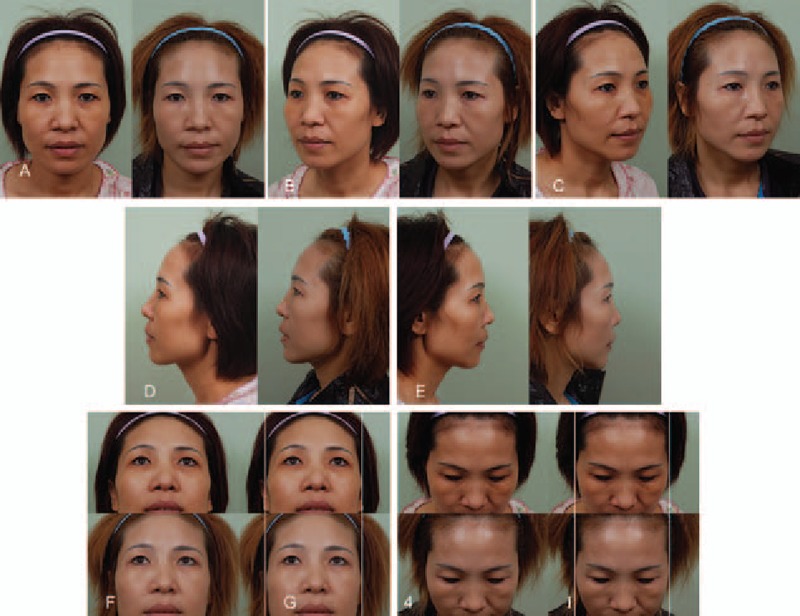
(Patient 1) This 42-year-old woman presented for augmentation with fat grafting to increase the hollowing appearance of her temporal fossa. Microautologous fat transplantation was performed to place a 3.0 mL/3.5 mL (right/left side) fat graft (Pre-op in A, B, C, D, and E, left). Six months after a single MAFT session, the volume restoration of the hollowing temple area was maintained as fullness (Post-op in A, B, C, D, and E, right). Chin-up, chin-down, and close-up views showed the improved contouring (Pre-op in F, G, H, and I upper; Post-op, lower). MAFT, microautologous fat transplantation.
FIGURE 7.
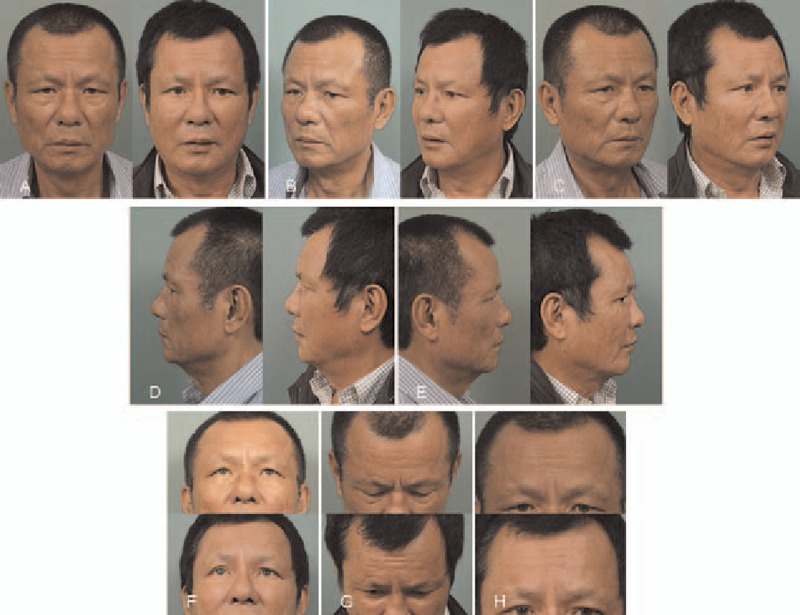
(Patient 4) This 66-year-old male presented for fat grafting to augment his temporal hollowness and improve the unevenness. Microautologous fat transplantation was performed to place a 4.0 mL/4.0 mL (right/left side) fat graft (Pre-op in A, B, and C, left). Four years and 4 months after a single MAFT session, the full and smooth appearance and volume restoration of the temple area were maintained (Post-op in A, B, and C, right). The improved appearance of engorged temporal vessels, unevenness were illustrated with rejuvenating effect of skin (Pre-op in D and E, left; post-op in right). Chin-up, chin-down, and closed-up views showed the recontouring for his temporal fossa (Pre-op in F, G, and H, left; post-op in right).
FIGURE 5.
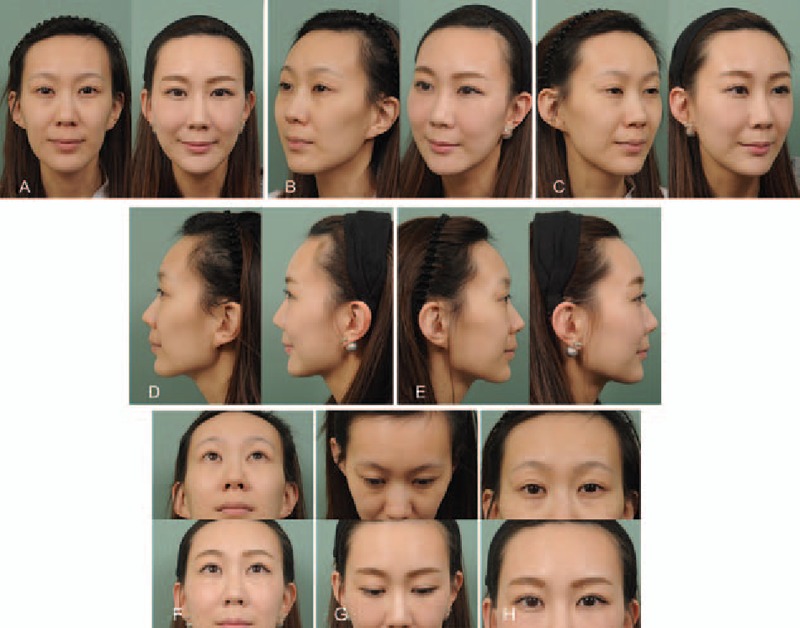
(Patient 2) This 31-year-old woman presented for augmentation temporoplasty with fat grafting to increase the hollowing appearance of her temporal fossa. Microautologous fat transplantation was performed to place an 8.0 mL/8.0 mL (right/left side) fat graft (Pre-op in A, B, C, D, and E, left). Six months after a single MAFT session, the fullness and volume restoration of the hollowing temple area were maintained (Post-op in A, B, C, D, and E, right). Chin-up, chin-down, and close-up views showed the improved contouring (Pre-op in F, G, and H, upper. Post-op, lower). MAFT, microautologous fat transplantation.
FIGURE 6.

(Patient 3) This 39-year-old woman presented for fat grafting to restore her temporal hollowness. Microautologous fat transplantation was performed to place an 8.0 mL/8.0 mL (right/left side) fat graft (Pre-op in A, B, and C, left). Six months after a single MAFT session, the fullness and volume restoration of the hollowing temple area were maintained (Post-op in A, B, and C, right). The improved appearance of engorged temporal vessels and rejuvenating effect of skin were illustrated in close-up profile view (Pre-op in D and E, left; post-op in right). Chin-up, chin-down, and closed-up views showed the recontouring for her sunken temporal fossa (Pre-op in F, G, and H, upper; post-op in lower).
DISCUSSION
Numerous autologous grafts (bone graft, fat graft) and synthetic implants are available and applied clinically for augmenting and recontouring the temporal hollowing.1–3 The most common synthetic implant materials, such as silicone prosthesis, polyethylene implant, Mersilene mesh, bone cement, are reliable and achieve acceptable results in selective patients; however, their long-term feasibility has not been demonstrated. Potential complications, such as infection, deviation, incompatibility, and skeletonization, remain a challenging to surgeons.1–3 Though popular recently, fillers such as hyaluronic acid are not appreciated in all patients because of the expense, necessity of repeating, and possibility of allergy.4–6 Autologous tissues, such as bone, dermal graft, and fat graft, are preferable because of their biocompatibility and effectiveness in certain patients.3 However, in fat grafting, the dissatisfaction resulting from unpredictable absorption rate, potential morbidities, and a lack of long-term evidence remained unresolved.
When describing the structure fat graft technique, Coleman addressed that in specific areas, such as the periorbital area (thinner skin), each delivered fat parcel should be 1/30 to 1/50 mL (0.020–0.033 mL) to avoid potential central necrosis and subsequent complications.9,16 Based on the theory by Dr Carpaneda, only 40% of the tissue survives at the area of 1.5 ± 0.5 mm from the grafted margin.17 The favorable injection frequency of 1 mL of fat graft should be between 30 and 240 was demonstrated as the central dogma of microautologous fat transplantation and advocated by Lin et al10 (Table 2 and Fig. 8). The contention of MAFT postulated by Lin et al10 in 2006 emphasized that each of the delivered parcel should be less than 1/100 mL (<0.01 mL) (ie, a parcel in spherical shape with radius around 1.3 mm = 1300 μm owns the volume of 0.01 mL) to avoid the potential morbidities of fat grafting resulting from central necrosis. These precise, miniature, and consistent 0.01 mL parcels (a spherical with 1300 μm in radius) were further proven by Yoshimura et al using molecular biology and immunohistology to retain the radius approximately as the outer survival zone (100–300 μm thick) and middle regenerative zone (600–1200 μm thick) to avoid the grave necrotic zone.18,19 Based on oxygen diffusion and perfusion, Khouri et al pointed out further that the fat injections larger than 0.16 cm in radius will have an area of central necrosis (in this situation the volume of such spherical parcel is 17.16 mm3 which renders the total injection frequency of injecting 1 mL should be at least 58).19 The innovative patent instrument, MAFT-GUN, possesses its precise controlling mechanism that allows accurate and consistent deliver fat parcel from 1/60,1/90, 1/120, 1/150, 1/180, and 1/240 mL, provides surgeon with a tool to control the volume of parcels and avoid the central necrosis and subsequent complications (Table 2).8 Clinical results with MAFT have demonstrated its feasibility and importance in controlling the parcel size to achieve favorable outcomes.10–15 In other words, the accurate and consistent controlling of fat parcel volume might be crucial to avoid the occasional dislodgement of larger parcels resulting in nodulation and skin irregularity after fat grafting.17–20
TABLE 2.
Injecting Frequency of 1 mL Fat Grafting at the Size of 1.0, 1.5, and 2.0 mm in Radius of a Spherical Is 240, 70, and 30 Respectively
| Global Radius (mm) | Global Volume (mm)3 | Injection Frequency for per 1 cc (1000 mm3) of Fat Grafting |
| r = 1.0 | 4.2 | 240 |
| r = 1.5 | 14.1 | 70 |
| r = 2.0 | 33.5 | 30 |
FIGURE 8.
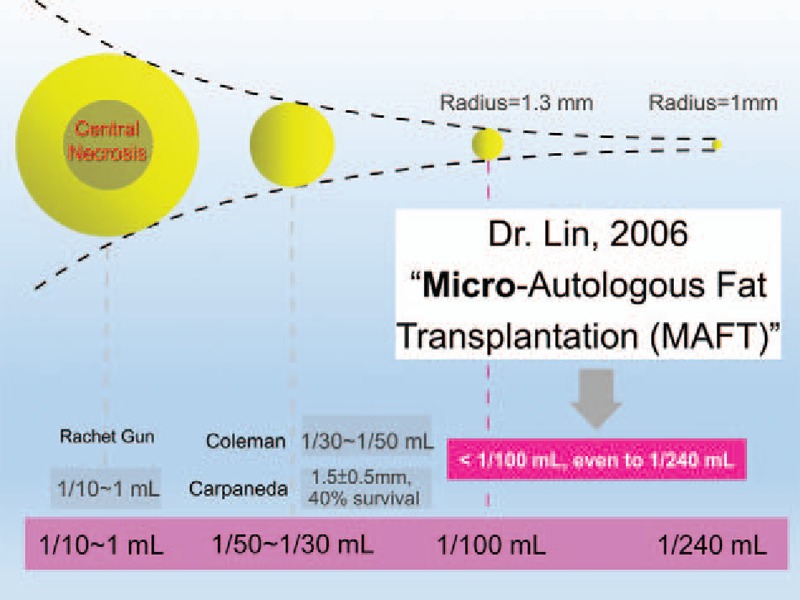
The evolution of the parcel size (volume) is from 1/10 mL Rachet Gun (even l mL by manual or larger Rachet Gun) to 1/50 to 1/30th proposed by Dr Coleman and theory of Dr Carpaneda to the microautologous fat transplantation concept (microautologous fat transplantation) advocated by Dr Lin et al in 2006. The MAFT emphasizes each delivered fat parcel is better to be <1/100 mL (0.010 mL) which renders the real radius of such parcel is 1.3 mm in spherical. MAFT, microautologous fat transplantation.
Anatomically, there are several structures to be defined in temporal region.21,22 However, while applying the technique of MAFT, we usually partition the soft tissues where fat grating should be transplanted into 3 levels (deeper layer, middle layer, and superficial layer) using the DTF and STF as a demarcation.
Deeper layer (ie, retro-DTF to temporal bone, in-between temporalis muscle), the fat parcels (volume was predetermined at 1/120 or 1/150 mL while the 6-grade dial is turned to 120 or 150) might have a well-vascularized recipient site, temporalis muscle to graft.
Middle layer (an areolar space between DTF and STF), this layer was a relative avascular areolar layer allowing the blunt cannula to go smoothly within the boundary of temporal region; temporal fusion line, lateral orbital rim, and zygomatic arch.
Superficial layer (subcutaneous layer), meanwhile, in this layer all parcels were transplanted in subcutaneous tissue where temporal vessels insults should be carefully avoided.
Technique of Microautologous Fat Transplantation Maneuver (Animation and DVD)
Parcels in Deeper Layer (Retro-Deep Temporal Fascia, In-Between Temporalis Muscle)
First, make sure the blunt tip of injection cannula inserts vertically through a 2 mm wound cut by #11 blade. Then keep pressure on the tip of cannula and swing around to make a penetrating hole through DTF. Slant and advance the MAFT-GUN, then go into the temporalis muscle along with gentle telecentric movement of the cannula (away from insertion point) and this maneuver could be easily and safely advanced for around 3 cm in length. Limitation of the advanced tracts will be encountered in temporal fusion line, lateral orbital rim, and zygomatic arch where the DTF was firmly adhered (animation and DVD). Fat parcels were delivered out of the side hole while surgeons withdrew the MAFT-GUN. In a fan-shaped manner, numerous parcels (1/120 or 1/150 mL) could be microtransplanted consistently by triggering the MAFT-GUN. Oftentimes, 2 to 3 mL (sometimes more in individual variable) of fat will be grafted in this deeper layer.
Parcels in Middle Layer (Areolar Space Between Deep Temporal Fascia and Superficial Temporal Fascia)
Once the cannula tip goes through the incision but is not kept vertically, an areolar space between DTF and STF will be liable to enter. Advancement of cannula tip was performed on the top of DTF, so there might be more advancement even over the boundary of temporal region (ie, going over the temporal fusion line, lateral orbital rim, and zygomatic arch). Another 2 to 3 mL (or more) of fat will be easily transplanted in this layer.
Parcels in Superficial Layer (Subcutaneous Layer)
Moreover, while inserting the cannula more superficially at the moment of entering the insertion, the tip of cannula will go freely without resistance and extend over the temporal region easily. This smooth maneuver served as a tailoring effect to make the boundary and subcutaneous vessels invisible. Caution was specially taken to avoid violent movement and unintentional vascular injury. Therefore, in this wider area (compared with deeper and middle layers), it was easy to microtransplant more parcels. Oftentimes the total delivered volume for this superficial layer was about 1.5-fold as deeper or middle layer.
Secondary Touchup
In some patients (40/208, 19%), the ones who had relative thinness of temporal area or those who wished to have more fullness rendered it difficult for placing more parcels or to reach fullness appearance in 1 session. Usually, a secondary touch-up MAFT was performed 4 to 6 months after the first session that is appreciated should patients request.
Anatomically, there are 3 levels where the fat parcel should be microtransplanted. With the illustration of dyes (deeper layer: blue, middle layer: green and superficial layer: pink), surgeons would be familiar with the right planes to be grafted (Fig. 9A, B).
FIGURE 9.
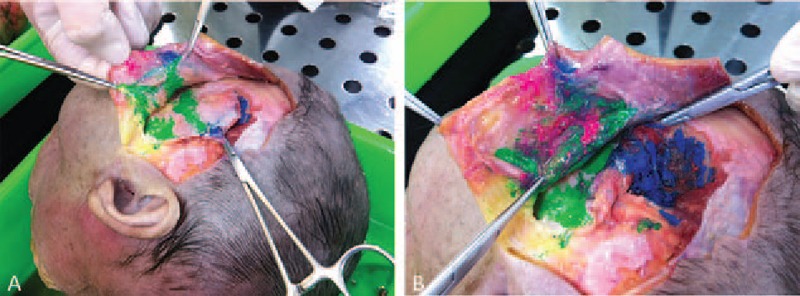
(A) Three dye colors are injected in different layers (blue in deep, green in middle, and pint in superficial layer) shown in cadaver dissection. (B) Close-up view demonstrated that blue dye will be in deep layer where the temporalis muscle is transplanted, green dye is shown in the space between deep temporal fascia and superficial temporal fascia and the pink is distributed in subcutaneous layer.
By using the innovative instrument, MAFT-GUN, surgeons can accurately deliver each parcel for sunken temporal fossa at 1/120 mL (0.0083 mL) or 1/150 mL (0.0067 mL) (the actual range of each parcel by MAFT-GUN might be flexibly set at 1/60, 1/90, 1/120, /1/150, 1/180, and 1/240 mL) to avoid complications related closely to central necrosis and its subsequent morbidities such as abscess, cyst formation, nodulation, severe fibrosis, or calcification.8 The diameter of 18 G blunt tip cannula that is 1.2 mm in diameter further makes the procedure safe by preventing the penetration into frontal or parietal branch of superficial temporal artery (the evidence-based medicine showed the average size of frontal/parietal branch of superficial temporal artery is 1.4 ± 0.4 mm/1.4 ± 0.5 mm or 1.8 ± 0.3/1.5 ± 0.2 mm).23,24 The possibility of severe vascular insults such as central retinal artery occlusion or brain infarction caused by fat parcels was highly decreased. However, meticulous performance without violating maneuver and appropriate anesthesia to keep patient calm and stable were also crucial during the MAFT procedure.
For patients who underwent 1 session of MAFT but wished to have more fullness, secondary touchup might be considered 4 to 6 months after the first procedure. The estimated fat retention rate in this study was approximately >50% with 1 session MAFT, and the long-term outcome (up to 4 years and 4 months) was reliable, as anticipated (Fig. 7). Therefore, 2 sessions of MAFT or even more might be necessary and informed preoperatively for those who requested more fullness or in patients whose temporal hollowing is severe. Because of the increased thickness by fat grafting after the first session, in the second session of MAFT, more volume of fat might be transplanted to ensure good results.
CONCLUSION
Various strategies can be employed to restore the fullness of the sunken temporal fossa in Asian patients. Implants or fillers do not appear to be feasible and preferable for all patients. Although not all patients with sunken temporal fossa can be solved with fat grafting in 1 session, MAFT plays an alternative strategy for the restoration of the volume in the correction of temporal hollowness.
In conclusion, this study developed a simple and reliable procedure based on the MAFT technique for the correction of sunken temporal fossa in Asians. Favorable outcomes (77.4%) were obtained for candidates with 1 session of MAFT (26.8%, very satisfied and 50.6%, satisfied). The advantages of MAFT in such clinical candidates not only include the recontouring of the temporal fossa, but also improving the skin texture with sustainable long-term effectiveness, further confirming that this strategy is a reliable alternative.
Supplementary Material
Supplementary Material
Footnotes
S-SL, Y-HH are cofirst authors.
This paper has been presented partially at 4th ISPRES, December 4 to 6, 2015, Beijing, China, and 18th IMCAS, January 28 to 31, 2016, Paris, France.
Dr T-ML owns the patent rights of MAFT-Gun, and is the scientific adviser of Dermato Plastica Beauty Co, which is the manufacturer of the MAFTGun device.
The authors report no conflicts of interest.
REFERENCES
- 1.Brown BL, Neel HB, 3rd, Kern EB. Implants of supramid, proplast, plasti-pore, and silastic. Arch Otolaryngol 1979; 105:605–609. [DOI] [PubMed] [Google Scholar]
- 2.Holmes RE, Hagler HK. Porous hydroxyapatite as a bone graft substitute in cranial reconstruction: a histometric study. Plast Reconstr Surg 1988; 81:662–671. [DOI] [PubMed] [Google Scholar]
- 3.Falconer DT, Phillips JG. Reconstruction of the defect at the donor site of the temporalis muscle flap. Br J Oral Maxillofac Surg 1991; 29:16–18. [DOI] [PubMed] [Google Scholar]
- 4.Sykes JM. Applied anatomy of the temporal region and forehead for injectable fillers. J Drugs Dermatol 2009; 8 (10 suppl):s24–s27. [PubMed] [Google Scholar]
- 5.Chundury RV, Weber AC, McBride J, et al. Microanatomical location of hyaluronic acid gel following injection of the temporal hollows. Ophthal Plast Reconstr Surg 2015; 31:418–420. [DOI] [PubMed] [Google Scholar]
- 6.Lee SK, Kim SM, Cho SH, et al. Adverse reactions to injectable soft tissue fillers: memorable cases and their clinico-pathological overview. J Cosmet Laser Ther 2015; 17:102–108. [DOI] [PubMed] [Google Scholar]
- 7.Neuber F. Fat transplantation [in German]. Bericht über die Verhandlungen Deutschen Gesellschaft Chirurgie Zbl Chir 1893; 22:66. [Google Scholar]
- 8.Khawaja HA, Hernández-Pérez E. Fat transfer review: controversies, complications, their prevention, and treatment. Int J Cosmetic Surg Aesthet Dermatol 2002; 4:131–138. [Google Scholar]
- 9.Coleman SR. Structural fat grafting. Aesthet Surg J 1998; 18:386–388. [DOI] [PubMed] [Google Scholar]
- 10.Lin TM, Lin SD, Lai CS, et al. The treatment of nasolabial fold with free fat graft: preliminary concept of Micro-Autologous Fat Transplantation (MAFT) in 2nd Academic Congress of Taiwan Cosmetic Association, Taipei, 2007 [Google Scholar]
- 11.Chou C K, Lin T M, Chou C, et al. Influential factors in autologous fat transplantation—focusing on the lumen size of injection needle and the injecting volume. J IPRAS 2013; 9:25–27. [Google Scholar]
- 12.Lin TM, Lin TY, Chou CK, et al. Application of microautologous fat transplantation in the correction of sunken upper eyelid. Plast Reconstr Surg Glob Open 2014; 2:e259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lin TM. Pu LLQ, Chen YR, Li QF, et al. Total facial rejuvenation with micro-autologous fat transplantation (MAFT). Aesthetic Plastic Surgery in Asians: Principles and Techniques 1st ed.St. Louis, MO: CRC Press; 2015. 127–146. [Google Scholar]
- 14.Lin TM, Lin TY, Huang YH, et al. Fat grafting for recontouring sunken upper eyelids with multiple folds in Asians-novel mechanism for neoformation of double eyelid crease. Ann Plast Surg 2016; 76:371–375. [DOI] [PubMed] [Google Scholar]
- 15.Kao WP, Lin YN, Lin TY, et al. Microautologous fat transplantation for primary augmentation rhinoplasty: long-term monitoring of 198 Asian patients. Aesthet Surg J 2016; 36:648–656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Coleman SR. Structural fat grafting: more than a permanent filler. Plast Reconstr Surg 2006; 118 (3 suppl):108S–120S. [DOI] [PubMed] [Google Scholar]
- 17.Carpaneda CA, Ribeiro MT. Percentage of graft viability versus injected volume in adipose autotransplants. Aesthet Plast Surg 1994; 18:17–19. [DOI] [PubMed] [Google Scholar]
- 18.Kato H, Mineda K, Eto H, et al. Degeneration, regeneration, and cicatrization after fat grafting: dynamic total tissue remodeling during the first 3 months. Plast Reconstr Surg 2014; 133:303e–313e. [DOI] [PubMed] [Google Scholar]
- 19.Eto H, Kato H, Suga H, et al. The fate of adipocytes after nonvasularized fat grafting: evidence of early death and replacement of adipocytes. Plast Reconstr Surg 2012; 129:1081–1092. [DOI] [PubMed] [Google Scholar]
- 20.Khouri RK, Jr, Khouri RE, Lujan-Hernandez JR, et al. Diffusion and perfusion: the keys to fat grafting. Plast Reconstr Surg Glob Open 2014; 2:e220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ramirez OM. Three-dimensional endoscopic midface enhancement: a personal quest for the ideal cheek rejuvenation. Plast Reconstr Surg 2002; 109:329–340. [DOI] [PubMed] [Google Scholar]
- 22.O’Brien JX, Ashton MW, Rozen WM, et al. New perspectives on the surgical anatomy and nomenclature of the temporal region: literature review and dissection study. Plast Reconstr Surg 2013; 131:510–522. [DOI] [PubMed] [Google Scholar]
- 23.Kim BS, Jung YJ, Chang CH, et al. The anatomy of the superficial temporal artery in adult Koreans using 3-dimensional computed tomographic angiogram: clinical research. J Cerebrovasc Endovasc Neurosurg 2013; 15:145–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kuruoglu E, Cokluk C, Marangoz AH, et al. The evaluation of three-dimensional anatomy of the superficial temporal artery using the volume rendering technique. Turk Neurosurg 2015; 25:285–288. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


