INTRODUCTION
Genotype is increasingly recognized as an important factor influencing the likelihood for drug effectiveness or risk for adverse events. Genetic information is now included in US Food and Drug Administration‐approved labeling for over 130 drugs, and in some cases, the information is in the form of a boxed warning given the potentially serious implications of genotype on drug response. Based on the growing body of evidence supporting genetic contributions to drug response, the Clinical Pharmacogenetics Implementation Consortium (CPIC) was formed to provide consensus guidelines on interpretation and translation of genotype results into actionable prescribing decisions.1 Guidelines have been published for 18 drugs or drug classes as of late 2016. The Precision Medicine Initiative is expected to further drive discoveries in genomic medicine and their translation to patient care.2 In 2013, the National Institutes of Health (NIH)‐funded Implementing GeNomics In praTticE (IGNITE) network was established to support the development and investigation of genomic medicine practice models to enhance its implementation into routine clinical practice.3
One of the challenges hindering genomic implementation is the limited data on the outcomes and cost‐effectiveness of genotype‐guided drug therapy. The IGNITE network, consisting of institutions funded in the network and affiliate members, includes a number of institutions that have implemented pharmacogenetic testing to assist with prescribing decisions. This creates an opportunity for multiinstitutional collaboration to share data and create a real‐world patient population of sufficient size to examine the impact of implementing pharmacogenetic testing on important clinical outcomes. Herein, we describe the IGNITE Pharmacogenetics Working Group and the process for an initial collaboration to examine a use case, namely, outcomes with CYP2C19 genotype‐guided antiplatelet therapy following percutaneous coronary intervention (PCI). We also describe how this initial collaboration provides the infrastructure for ongoing and future collaborative work.
IGNITE PHARMACOGENETICS WORKING GROUP
The IGNITE Network and funded projects have been described.3 While not all funded projects are related to pharmacogenetics, all sites funded by the network and most affiliate members have implemented pharmacogenetic testing in some regard. Following establishment of the IGNITE Network in 2013, the Pharmacogenetics Working Group was formed in January 2015 with the goals of broadly engaging institutions (funded IGNITE sites and affiliate members) implementing pharmacogenetics into practice to: i) share and collectively disseminate data on implementation strategies, metrics, and patient‐related outcomes following the utilization of genotype‐guided therapy; and ii) examine healthcare costs with pharmacogenetic implementation at multiple institutions. The working group consists of the six NIH‐funded institutions within IGNITE, their collaborating institutions, and nine affiliate members (Figure 1). The group welcomes institutions that have established pharmacogenetic programs as well as those with newly implemented programs or in the process of implementation. Gene–drug pairs implemented at institutions within the interest group are listed in Table 1. Each institution agreed to share clinical implementation strategies with other institutions within the network for potential adoption. In this regard, newer programs may benefit from learning about and applying implementation strategies (i.e., genotyping procedures and clinical decision support) that have been successful at more established institutions. In addition, each site agreed to share patient‐level data as appropriate for collective examination of patient‐related outcomes with pharmacogenetic implementation. Institutions in the process of implementation (and without current data) are able to fully participate in conference calls and discussions, but have limited access to data from other institutions.
Figure 1.
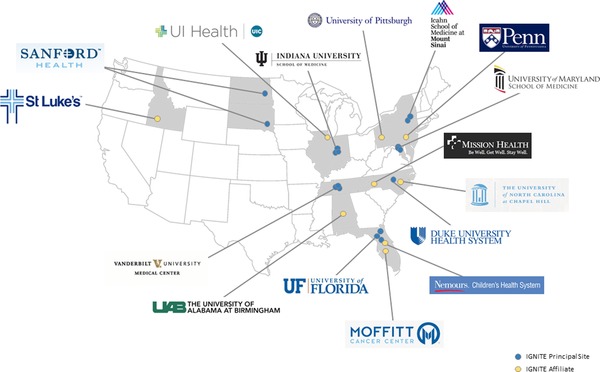
Institutions participating in the IGNITE Pharmacogenetics Working Group. Blue dots represent funded institutions within the IGNITE Network. Yellow dots represent affiliate members.
Table 1.
Gene–drug pairs implemented into clinical practice at institutions participating in the IGNITE Pharmacogenetics Working Group
| Institution | Gene–drug pairs implemented |
|---|---|
| University of Floridaa | CYP2C19‐clopidogrel; CYP2D6‐codeine, tramadol; TPMT‐thiopurines; CYP2D6/CYP2C19‐SSRIs; CYP2C19‐PPIs; CYP2C19‐voriconazole (in development) |
| Vanderbilt Universitya | CYP2C19‐clopidogrel; SLCO1B1‐simvastatin; CYP2C9/VKORC1‐warfarin; CYP3A5‐tacrolimus; TPMT‐thiopurines |
| Indiana Universitya | CYP2C19‐clopidogrel, voriconazole, PPIs, citalopram; CYP2D6‐opioids, SSRIs, aripiprazole, atomoxetine; SLCO1B1‐simvastatin; CYP2C9/VKORC1/CYP4F2‐warfarin; CYP3A5‐tacrolimus; TPMT‐thiopurines; CYP2D6/CYP2C19‐TCAs; DPYD‐5‐fluorouracil, capecitabine, tegafur; G6PD‐rasburicase; ITPA‐thioguanine; CYP2B6‐efavirenz |
| Sanford Healtha | CYP2C19‐clopidogrel; CYP2C9/VKORC1‐warfarin; CYP2D6/CYP2C19‐SSRIs, TCAs; CYP2D6‐opioids; CYP3A5‐tacrolimus; SLCO1B1‐simvastatin; TPMT‐thiopurines; DPYD‐capecitabine, fluorouracil, tegafur |
| University of Marylandb | CYP2C19‐clopidogrel |
| Mount Sinaib | CYP2C19‐clopidogrel; CYP2C9/VKORC1‐warfarin; SLCO1B1‐simvastatin; CYP2D6‐codeine, tramadol; CYP2D6/CYP2C19‐TCAs (in development); CYP2D6/SSRIs (in development) |
| Duke Universityb | SLCO1B1‐statins |
| University of North Carolina at Chapel Hill | CYP2C19‐clopidogrel |
| Nemours Children's Health System | CYP2C19‐PPIs |
| University of Illinois at Chicago | CYP2C19‐clopidogrel; CYP2C9/VKORC1‐warfarin |
| Mission Health System | HLA‐B*1502‐carbamazepine |
| St. Luke's Mountain States Tumor Institute | DPYD‐fluorouracil, capecitabine; TPMT‐thiopurines |
| University of Pittsburgh | CYP2C19‐clopidogrel |
| University of Pennsylvania | CYP2C19‐clopidogrel |
| H. Lee Moffitt Cancer Center & Research Institute | CYP2C19‐voriconazole; CYP2D6‐opioids; TPMT‐thiopurines |
| University of Alabama, Birmingham | CYP2C19‐clopidogrel |
PPI, proton pump inhibitor; SSRI, selective serotonin reuptake inhibitor; TCA, tricyclic antidepressant.
Funded within IGNITE Network for pharmacogenetics implementation.
Funded within IGNITE for disease susceptibility genomic implementation, but also conducting pharmacogenetics implementation.
The working group is led by investigators at the University of Florida, and members communicate through twice‐monthly conference calls, in‐person meetings of the IGNITE Network, and additional teleconferences for data analysis and writing subgroups. Prior to participation in the working group, each institution signed a memorandum of understanding (MOU), adapted from the International Warfarin Pharmacogenetics Consortium, and outlining responsibilities of group members, requirements for access to compiled data, and authorship policies. The MOU is available through the SPARK toolbox on the IGNITE website (https://ignite-genomics.org/spark-toolbox/researchers/).
CYP2C19‐clopidogrel project
The most common implementation among institutions was CYP2C19 genotyping to predict clopidogrel response and guide antiplatelet therapy after percutaneous coronary intervention (PCI). The CYP2C19 enzyme has a critical role in the biotransformation of clopidogrel to its pharmacologically active form. Approximately 30% of Whites and Blacks and 65% of Asians carry a nonfunctional CYP2C19 gene variant associated with reduced clopidogrel bioactivation and an increased risk of major adverse cardiovascular events in clopidogrel‐treated patients after PCI.4 The US Food and Drug Administration‐approved clopidogrel label includes a boxed warning regarding reduced clopidogrel effectiveness in poor metabolizers, who have two nonfunctional alleles. CPIC recommends alternative antiplatelet therapy after acute coronary syndrome and PCI in poor metabolizers as well as intermediate metabolizers, who have one nonfunctional allele.4
Institutions vary in their approaches to CYP2C19 implementation, including timing of genotyping (e.g., preemptively before antiplatelet therapy is needed or reactively in response to an order for clopidogrel) and how genotype‐based recommendations are communicated to prescribers (e.g., through automated clinical decision support or personal communication). However, all institutions are conducting genotyping in a Clinical Laboratory Improvement Amendments‐certified laboratory, with results entered into the electronic health record (EHR). In addition, all institutions recommend alternative therapy (e.g., prasugrel or ticagrelor) for patients with genotypes predicting the poor and/or intermediate metabolizer phenotypes.
A clinical trial examining outcomes with CYP2C19 genotype‐guided therapy after PCI is ongoing (Clinicaltrials.gov identifier NCT01742117) but not expected to be completed until 2020. Given the magnitude and expense of conducting traditional randomized controlled trials for every pharmacogenetically relevant drug–gene pair, other approaches are needed to generate the evidence base on outcomes with pharmacogenetic testing. As such, there was an interest among groups in collaborating to collect and share data on cardiovascular outcomes with implementation of CYP2C19 genotype‐guided therapy after PCI as our first demonstration project.
Each institution obtained approval from their respective Institutional Review Board (IRB) prior to data collection and sharing. A common data collection tool, adapted from the International Clopidogrel Pharmacogenomics Consortium, was developed to facilitate data collection and aggregation. Data were collected manually at each site, deidentified, and sent to UF for aggregation. The process for developing the tool included identifying all variables that would be ideally collected from the EHR to comprehensively assess outcomes among patients who underwent PCI and received CYP2C19 genotyping. The tool was pilot‐tested at several institutions to ensure that each data element was clearly defined and evaluate the feasibility of collecting different data elements of interest. The revised tool includes ∼60 variables, including patient characteristics, medical history, PCI indication, genotype results, antiplatelet therapy, and cardiovascular events within 12 months of PCI, and is freely available through the IGNITE website SPARK toolbox (https://ignite-genomics.org/spark-toolbox/researchers/). The tool can be modified and serve as a foundation to facilitate harmonized data collection on future projects.
Data from the initial working group collaboration, including 1,815 patients who underwent PCI and CYP2C19 genotyping across seven sites, were presented as a late‐breaking abstract at the 2016 American Heart Association Scientific Sessions.5 These data showed that among patients with a nonfunctional allele, the risk for major adverse cardiovascular events was significantly higher when clopidogrel vs. alternative antiplatelet therapy was prescribed.
ADDITIONAL COLLABORATIVE RESEARCH OPPORTUNITIES
The CYP2C19‐clopidogrel outcomes project serves as the initial example of a multiinstitution collaborative effort to examine outcomes with real‐world pharmacogenetic implementation. It also provides the platform for future studies, including those with other gene–drug pairs. This includes an ongoing project to compare implementation strategies for CYP2C19‐guided antiplatelet therapy across sites and assess how various strategies impact metrics. Further, because outcomes for multiple drugs are influenced by CYP2C19 genotype, IGNITE serves as a platform for standardizing our approach to pleiotropy, the principle that variation in one pharmacogene can impact outcome for more than one drug.6 In this regard, some of our member institutions provide automated decision support for selective serotonin reuptake inhibitors and other relevant drugs in patients who have had CYP2C19 initially genotyped for clopidogrel.6 Another important principle in pharmacogenetics is that biotransformation is robust, and the metabolism of one drug is often influenced by more than one gene. This makes the case for testing multiple genes, and many of our member institutions are therefore moving toward genotyping multiplexed panels of pharmacogenes. This provides the opportunity for groups to share data to examine the benefits of multiplex pharmacogenetics testing.
The IGNITE Pharmacogenetics Working Group also provides the infrastructure to examine economic outcomes with practical implementation of pharmacogenetics, and an economic analysis of CYP2C19‐guided antiplatelet therapy is underway. Cost‐effectiveness analysis can impact decisions by providers to adopt pharmacogenetic testing, by payers to reimburse for such companion diagnostics, and by regulatory agencies when deciding on what guidance to issue regarding such technology. These decisions, in turn, impact the likelihood that high‐value pharmacogenetic testing will be implemented outside of research settings. Additional sensitivity analysis can be used to explore the impact of apparent unexplained variation in costs and outcomes, and to identify priorities for future research, while complementary decision analytic models can be used to explore heterogeneity of costs and effects across time, patient groups, and clinical settings. Thus, the coordination of analyses across sites provides an opportunity not only to provide statistically more precise estimates for use in economic modeling, but also to better understand how results generalize across different implementation strategies for dissemination of pharmacogenetics test results in real‐world settings.
SUMMARY
In summary, we have created a multiinstitution infrastructure of academic and community healthcare institutions with a shared interest in advancing the practice of pharmacogenetics. Recognizing the paucity of data on clinical utility of genotype‐guided therapy, the working group aims to provide data on important clinical and economic outcomes with pharmacogenetic implementation, with the ultimate goal of providing evidence to support reimbursement for testing and broader clinical implementation of pharmacogenetics.
Acknowledgments
Work supported by the National Institutes of Health (NIH) grants U01 HG007269 (LHC, KWW, AE, JAJ), U01 HG007775 (LJJ), U01 HG007253 (JFP, RAW), and U01 HG007762 (TCS, VMP, AMH), as part of the NIH IGNITE network. Additional support provided by NIH U01 GM074492 and U01 HL105198 (both part of the NIH Pharmacogenomics Research Network), and by substantial institutional support from the University of Florida and its Clinical Translational Science Institute (UL1 TR000064 and UL1 TR001427) for LHC, EA, KWW, and JAJ; NIH U01 HL105198, and support from the University of Maryland Medical Center and University of Maryland School of Medicine Program for Personalized and Genomic Medicine for ALB and LJBJ; NIH K23 GM112014 and the University of Illinois at Chicago Offices of the Vice President for Health Affairs and Vice Chancellor for Research for JDD; American Society of Health System Pharmacists, NIH UL1TR0000005, and by an Anonymous Donor for PEE; Penn Center for Precision Medicine at the Perelman School of Medicine at the University of Pennsylvania for ST; NIH R01HL092173, 1K24HL133373, University of Alabama, Birmingham Health Service Foundations' General Endowment Fund, and NIH UL1TR000165 for NAL; R01 GM088076 for TCS; Indiana University Health – Indiana University School of Medicine Strategic Research Initiative for VMP.
Conflict of Interest
The authors declared no conflict of interest.
References
- 1. Relling, M.V. & Klein, T.E. CPIC: Clinical pharmacogenetics implementation consortium of the pharmacogenomics research network. Clin. Pharmacol. Ther. 89, 464–467 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Collins, F.S. & Varmus, H. A new initiative on precision medicine. N. Engl. J. Med. 372, 793–795 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Weitzel, K.W. et al The IGNITE network: a model for genomic medicine implementation and research. BMC. Med. Genomics. 9, 1 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Scott, S.A. et al Clinical pharmacogenetics implementation consortium guidelines for CYP2C19 genotype and clopidogrel therapy: 2013 update. Clin. Pharmacol. Ther. 94, 317–323 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cavallari L.H. et al Prospective clinical implementation of CYP2C19‐genotype guided antiplatelet therapy after PCI: a multi‐site investigation of MACE outcomes in a real‐world setting. Circulation. 134, e711–e712 (2016). [Google Scholar]
- 6. Oberg, V. , Differding, J. , Fisher, M. , Hines, L. & Wilke, R.A. Navigating pleiotropy in precision medicine: pharmacogenes from trauma to behavioral health. Pharmacogenomics. 17, 499–505 (2016). [DOI] [PubMed] [Google Scholar]


