Abstract
The bacterial factors associated with bacteremia by multidrug-resistant and extensively drug-resistant P. aeruginosa, including overexpression of efflux pumps, AmpC overproduction, and loss/alteration of the OprD porin in isolates that are non-Metallo-β-Lactamase producing were analyzed in a retrospective study. Molecular analyses included strain typing by Pulsed Field Gel Electrophoresis and identification of key genes via qualitative and quantitative PCR-based assays. Previous use of carbapenems and tracheostomy was independently associated with the development of bacteremia by extensively drug-resistant and multidrug-resistant strains of P. aeruginosa. A high consumption of antimicrobials was observed, and 75.0% of the isolates contained amplicons with the blaSPM-1 and blaVIM genes. Of the 47 non-Metallo-β-Lactamase isolates, none had another type of carbapenemase. However, the isolates exhibited high rates of hyperproduction of AmpC, loss of the OprD porin (71.4%) and the presence of MexABOprM (57.1%) and MexXY (64.3%). This study suggests that in non-Metallo-β-Lactamase isolates, the association of intrinsic resistance mechanisms could contributes to the expression of multidrug-resistant/extensively drug-resistant phenotypes.
Introduction
Pseudomonas aeruginosa, an opportunistic pathogen, is an major cause of health care associated infections [1,2], mainly in patients with impaired immune systems [1]. Today, high levels of resistance to several antimicrobial agents in P. aeruginosa clinical isolates have been reported as a worldwide problem [3–5]; however, this problem is more significant in Brazil due to a very high frequency of antibiotic use, particularly carbapenems and fluoroquinolones [6,7].
The carbapenems remain the primary antimicrobial used for treatment of severe infections caused by P. aeruginosa, however, the emergence and spread of resistance to these antibiotics may compromise their efficacy and are thus associated with high rates of mortality [8–11].
One of the most common resistance mechanisms to carbapenems in P. aeruginosa isolates is the loss or alteration of the outer membrane porin protein OprD [12], which regulates the entry of this class of antibiotics into the cell [13]. Other mechanisms include the upregulation of efflux pump systems, such as MexAB-OprM, MexEF-OprN, MexCD-OprJ and MexXY-OprM, the production of carbapenemase enzymes, including Metallo-β-lactamases (MBLs), especially the SPM-1 variant in Brazil, OXA-type carbapenemases and class A carbapenemases (e.g., GES and KPC types), and the overexpression of extended-spectrum chromosomally encoded AmpC cephalosporinase [12,14].
Many studies examining the mechanisms of carbapenem-resistance have involved controlled laboratory-derived strains; however, studies involving clinical isolates have not clearly defined the contributions of the MBL, AmpC cephalosporinase, alterations of the OprD porin or efflux systems to carbapenem-resistance [11,15]. In this report, we analyzed the mechanisms of carbapenem-resistance in clinical isolates of multidrug-resistant P. aeruginosa from blood samples. In addition, we evaluated the dissemination of high-risk clones in hospital settings.
Materials and methods
Patients and setting
The clinical microbiology laboratory database was reviewed, and 157 patients with nosocomial P. aeruginosa bacteremia from May 2009 to December 2012 at Uberlandia University Hospital (Brazil) were identified. Only the first episode of bacteremia was analyzed for those patients with more than one episode.
Study design and data collection
A retrospective observational cohort study was employed to identify the risk factors of multidrug-resistant (MDR) or extensively drug-resistant (XDR) Pseudomonas aeruginosa bacteremia. The demographic, clinical and epidemiological characteristics of the patients were obtained from individual medical records, following the model of the NHSN (National Healthcare Safety Network). For each patient studied, the following characteristics were recovered from their clinical records: age, gender, hospitalization time ≥ 30 days prior to infection, admission to the ICU, surgery, previous antibiotic use, invasive procedures such as mechanical ventilation, tracheostomy, urinary catheter, central venous catheter, surgical drain during the current hospitalization, enteral catheter or gastric nutrition, hemodialysis and parenteral nutrition.
Definitions and DDD for antibiotics
According to the Centers for Disease Control and Prevention [16], bacteremia can be defined as the presence of viable bacteria in the blood documented by a positive blood culture result. Bacteremia is considered as nosocomial if the infection occurred more than 48 hours after admission and if there was no clinical evidence of infection at the time of admission [17]. The MDR and XDR strains were defined according to Magiorakos and collaborators [18]. Previous antibiotic use was considered when the patient received therapy with any antibiotic for at least 72 hours during a period of 30 days prior to the microbiological infection diagnosis [19]. Antimicrobial consumption was expressed in a Defined Daily Dose (DDD) [20] per 1000 patient-days, and the data collection was conducted in the monthly electronic reports of antibiotic dispensing provided by the hospital pharmacy. The antimicrobial agents that were tracked included the following: cephalosporins (ceftriaxone and cefepime), carbapenems (imipenem and meropenem) and fluoroquinolones (ciprofloxacin and levofloxacin).
Bacterial isolates and clinical microbiology
A total of 157 consecutive non-duplicate P. aeruginosa isolates from patient blood were included in the study. Cultures were processed using a BACT/Alert (bioMérieux). Microbial identification and antimicrobial susceptibility test were performed on a VITEK II automated system (bioMérieux) for the following antimicrobials: aminoglycosides (gentamicin, amikacin), carbapenems (imipenem, meropenem), cephalosporins (ceftazidime, cefepime), fluoroquinolones (ciprofloxacin, levofloxacin), penicillins plus beta-lactamase inhibitors (piperacillin-tazobactam), monobactams (aztreonam) and polymyxins (colistin, polymyxin B). The isolates with intermediate susceptibility were considered as resistant. Quality control protocols were used according to the standards of the Clinical and Laboratory Standard Institute [21–23]. Fifty-six carbapenem-resistant P. aeruginosa isolates, confirmed by VITEK II system, were phenotypically screened for MBL production using a Double-Disc Synergy Test (DDST), as previously described [24]. The isolates that showed intermediate or resistant zones of inhibition for imipenem were tested for carbapenemase production with a Modified Hodge Test (MHT) according to CLSI recommendations and quality control [22–23]. The AmpC β-lactamase production was performed with an AmpC Disk Test that is based on the use of Tris-EDTA to permeabilize a bacterial cell and release β-lactamases into the external environment [25].
Molecular microbiology testing
The DNA extraction was performed by the technique of thermal lysis. A conventional multiplex PCR assay was performed for 56 isolates to detect five families of the MBL genes (blaIMP, blaVIM, blaSPM, blaGIM, blaSIM), using previous published primers [26]. The cycling conditions of this PCR were as follows: 94°C for 5 min, followed by 30 denaturation cycles at 94°C for 30 sec; annealing at 53°C for 45 sec; and extension at 72°C for 30 sec, followed by final extension at 72°C at 10 min. The strains were then submitted to a new conventional multiplex PCR that targets class D carbapenemases such as oxacillinase (blaOXA-51, blaOXA-23, blaOXA-40 and blaOXA-58) [27]. Additionally, the blaKPC gene was detected by conventional PCR using primers and cycling conditions previously described [27]. The amplified PCR products were visualized by electrophoresis on 1.5% agarose gels using the photo documentation System L-Pix EX (Loccus Biotechnology, Brazil).
Pulsed-field gel electrophoresis (PFGE)
Nine MBL-positive P. aeruginosa isolates (9/56) were typed by pulsed-field gel electrophoresis (PFGE) according to the protocols described by Galetti [28] with modifications, following digestion of intact genomic DNA with the restriction enzyme SpeI (Promega, Brazil). DNA fragments were separated on 1% (w/v) agarose gels in TBE 0.5% [Tris–borate–ethylene diamine tetra-acetic acid (EDTA)] buffer using a CHEF DRIII apparatus (Bio-Rad, USA) with 6 V/cm, pulsed from 5 s to 40 s, for 21 hours at 12°C. Gels were stained with ethidium bromide and photographed under ultraviolet light. Computer-assisted analysis was performed using BioNumerics 5.01 software (Applied Maths, Belgium). We were unable to determine the macrorestriction analysis profile of a single P. aeruginosa strain containing the blaSPM gene due to degradation of DNA. Comparison of the banding patterns was accomplished by the unweighted pair-group method with arithmetic averages (UPGMA) using the Dice similarity coefficient.
Relative quantification of mRNA by real time PCR (RT-PCR)
Semi-quantitative RT-PCR was performed for 14 MBL-negative isolates with VeriQuest Fast SYBR Green qPCR Master Mix (Affymetrix®) using specific primers for the chromosomal genes mexB, mexD, mexF, mexY, ampC and oprD, as previously described with some modifications [26]. The reaction was prepared in a final volume of 25 μL, containing 10 pmol of each primer and 2 μL of cDNA. Amplification was carried out in triplicate from cDNA preparations (Applied Biosystems, model 7300®). The relative transcript levels were calculated according to the ΔΔCt method, as previously described [29,30]. Briefly, the ΔΔCt method provides the relative gene expression levels by averaging cycle threshold (Ct) values from triplicate RT-PCR reactions for target and housekeeping genes. The range of expression levels obtained for the triplicates, which incorporates the standard deviation (SD) of the ΔΔCt value into the fold-difference, was used to calculate the confidence interval (CI) considering a confidence level of 95%. Additionally, in order to minimize the error and preserve the accuracy and robustness of this test, we have excluded and repeated those triplicate reactions whose average of Ct values presented an SD value higher than 0.20. The rpsL endogenous gene was used as the housekeeping gene and the wild-type P. aeruginosa PAO1 was used as the reference strain to determine the relative expression levels of the genes in the clinical isolates. The efflux systems MexAB-OprM, MexCD-OprJ, MexEF-OprN and MexXY-OprM were considered to be overexpressed when the transcriptional levels of mexB, mexD, mexE and mexY were at least two-, 100-, 100- and four-fold higher than those of the wild-type reference strain PAO1, respectively [26]. Reduced oprD expression and overexpression of ampC were considered relevant when their transcriptional levels were ≤ 70% and ≥ 10-fold, respectively, compared to the PAO1 reference strain [26].
Statistical analysis
Student’s t-test was used to compare continuous variables and X2 or Fisher’s exact test was used to compare categorical variables. Variables with P ≤ 0.05 in the univariate analysis were candidates for multivariate analysis. All P values were two-tailed, and P values of 0.05 were considered statistically significant.
Ethical considerations
The data and the samples analyzed in the present study were obtained in accordance with the standards and approved by the Federal University of Uberlandia Ethics Committee (UFU) through license number 00763112.7.0000.5152. For this study, samples were collected at the Microbiology Laboratory of the Clinical Hospital, with no contact with the patient and with the permission of the Hospital. This study was retrospective and there was no patient identification performed during data collection. Therefore, the ethics committee determined that informed consent was not required.
Results
A total of 157 non-repetitive patients with P. aeruginosa bacteremia at the university hospital were included in this study. The univariate analysis and independent risk factors associated with MDR and XDR P. aeruginosa bacteremia are summarized in Table 1. According to antimicrobial susceptibility testing results, MDR and XDR P. aeruginosa bacteremia occurred in 67 (42.7%) and 35 (22.3%) of the cases, respectively. Clinical and demographic data from these patients (MDR and XDR) were compared with a sensitive P. aeruginosa infections group (non-MDR) (Table 1). In the whole series, prior exposures to carbapenems and having a tracheostomy were associated with the development of bacteremia by MDR or XDR P. aeruginosa. Intensive Care Unit admission and length of stay ≥ 30 days prior to infection were other independent risk factors to MDR P. aeruginosa bacteremia.
Table 1. Univariate analysis and independent risk factors associated with multidrug-resistant and extensively drug-resistant P. aeruginosa bacteremia.
| Risk factor | XDR1 N = 35 (%) |
MDR2 N = 67 (%) |
Sensitive N = 90 (%) |
XDR | MDR |
||
|---|---|---|---|---|---|---|---|
| Univariate P4 (OR5) |
Multivariate P (OR) |
Univariate P (OR) |
Multivariate P (OR) |
||||
| Age–mean, years (range) | 56.06 (2–89) | 56.58 (2–89) | 49.09 (0–88) | 0.42 (-) | - | 0.10 (-) | - |
| Gender Male | 22 (62.9) | 44 (65.7) | 61 (67.8) | 0.75 (0.80) | - | 0.91 (0.91) | - |
| Gender Female | 13 (37.1) | 23 (34.3) | 29 (32.2) | 0.75 (1.24) | - | 0.91 (1.10) | - |
| Hospitalization time ≥ 30 days prior to infection | 17 (48.6) | 31 (46.6) | 32 (35.6) | 0.25 (1.71) | - | 0.02 (2.19)* | 0.05 (1.95)* |
| ICU3 admission | 17 (48.6) | 39 (58.2) | 35 (38.9) | 0.43 (1.48) | - | 0.02 (2.19)* | 0.02 (2.19)* |
| Surgery | 19 (54.3) | 34 (50.7) | 35 (38.9) | 0.17 (1.87) | - | 0.18 (1.62) | - |
| Previous antibiotic use | 31 (88.6) | 57 (85.1) | 67 (74.4) | 0.13 (2.66) | - | 0.01 (2.81)* | 0.57 (1.29) |
| Cephalosporin(3rd generation) | 13 (37.1) | 29 (43.3) | 39 (43.3) | 0.66 (0.77) | - | 0.87 (1.00) | - |
| Cefepime | 12 (34.3) | 26 (38.8) | 35 (38.9) | 0.78 (0.82) | - | 0.84 (1.00) | - |
| Carbapenems | 22 (62.9) | 39 (58.2) | 37 (41.1) | 0.04 (2.42)* | 0.001 (3.48)* | 0.05 (2.00)* | 0.02 (2.22)* |
| Fluoroquinolones | 7 (20.0 | 13 (19.4) | 7 (7.8) | 0.05 (2.96)* | 0.51 (0.71) | 0.05 (2.85)* | 0.43 (1.42) |
| Aminoglycosides | 4 (11.4) | 5 (7.5) | 7 (7.8) | 0.49 (1.53) | - | 0.81 (0.96) | - |
| Invasive | 33 (94.3) | 62 (92.5) | 77 (85.5) | 0.23 (2.79) | - | 0.23 (2.09) | - |
| Mechanical ventilation | 24 (68.6) | 45 (67.2) | 44 (48.9) | 0.04 (2.28)* | 0.61 (0.77) | 0.03 (2.14)* | 0.39 (1.42) |
| Tracheostomy | 22 (62.9) | 39 (58.2) | 31 (34.4) | 0.007 (3.22)* | 0.02 (2.97)* | 0.005 (2.55)* | 0.05 (2.19)* |
| Urinary catheter | 27 (77.1) | 49 (73.1) | 52 (57.8) | 0.07 (2.52) | - | 0.06 (1.99) | - |
| Catheter central line | 30 (85.7) | 54 (80.6) | 71 (78.9) | 0.53 (,61) | - | 0.95 (1.11) | - |
| Drain | 8 (22.8) | 10 (15.0) | 14 (15.6) | 0.07 (2.36) | - | 0.90 (0.95) | - |
| Gastric/enteral tube | 24 (68.6) | 50 (74.6) | 59 (65.6) | 0.91 (1.15) | - | 0.29 (1.55) | - |
| Haemodialysis | 13 (37.1) | 21 (31.3) | 18 (20.0) | 0.07 (2.36) | - | 0.14 (1.83) | - |
| Parenteral nutrition | 4 (11.4) | 9 (13.4) | 16 (17.8) | 0.55 (0.60) | — | 0.60 (0.72) | - |
1XDR, Extensively resistant
2MDR, Multidrug-resistant
3ICU, Intensive care unit
4P Value
5OR, Odds Ratio
*P ≤ 0.05 is statistically significant
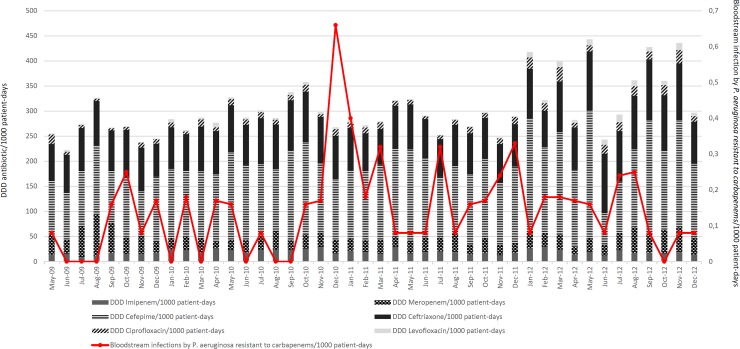
The relationship between the defined daily dose of an antimicrobial per 1000 patient-days and the number of patients with carbapenem-resistant P. aeruginosa per 1000 patient-days are shown in Fig 1. Consumption of antimicrobials was high, and an increase in use was observed at the end of the study period, particularly for ceftriaxone, cefepime and meropenem. There was no positive correlation between the increase of carbapenem-resistant P. aeruginosa isolates and antimicrobial consumption.
Fig 1. Endemic level of carbapenem resistant P. aeruginosa bacteremia per 1000 patient-days from March 2009 to December 2012.
All carbapenem-resistant P. aeruginosa isolates determined to contain MBL genes by PCR were subjected to molecular typing analysis. All these isolates were DDST positive. The genetic similarity among the strains was determined by PFGE and included the nine strains positive for the blaSPM (six strains) and blaVIM genes (three strains). It was impossible to determine the macro-restriction profile of one blaSPM-positive isolate due to degradation of the DNA sample. The genetic similarity dendrogram was generated from the macro-restriction profile, and the data from the P. aeruginosa with MBL genes are summarized in Table 2. In total, six different P. aeruginosa genotypic profiles were observed, differentiated from each other by a similarity factor above 80%. Two profiles corresponded to isolates containing the blaSPM gene (profiles A and B) and another three profiles included the blaVIM isolates (profiles C, D and E). The only A clone presented three subtypes (A1, A2 and A3) (S1 Fig, available in the Supporting Information). There was spread of clone A, as well as polyclonal dissemination of the blaVIM isolates at the Hospital (Table 2). The antimicrobial susceptibility testing showed that all P. aeruginosa isolates analyzed by PFGE showed an MDR or XDR profile. The isolates from clone A exhibited the same resistance profile and were all classified as XDR, while pulsotype B was classified as MDR.
Table 2. Phenotypic and genotypic profile of resistance, hospital unit and the date of isolation of P. aeruginosa samples characterized by PFGE.
| DDST1 | bla Gene | Pulsotype PFGE2 |
Hospital Units | Date | MDR3/XDR4 |
|---|---|---|---|---|---|
| + | VIM | E | Medical clinical | 06/07/2011 | XDR |
| + | VIM | D | Surgery unit | 31/01/2011 | XDR |
| + | VIM | C | Medical clinical | 17/11/2010 | MDR |
| + | SPM | B | Surgery unit | 26/03/2011 | MDR |
| + | SPM | A3 | Surgery unit | 07/08/2012 | XDR |
| + | SPM | A2 | Surgery unit | 06/09/2011 | XDR |
| + | SPM | A1 | Adult ICU5 | 30/03/2012 | XDR |
| + | SPM | A1 | Adult ICU | 10/09/2011 | XDR |
1Double Disk Synergistic Test
2PFGE; Pulsed-Field Gel Electrophoresis
3MDR, Multidrug-resistant
4XDR, Extensively-resistant
5ICU, Intensive Care Unit; + Positive test
Of the 56 carbapenem-resistant isolates, 47 did not show MBL production. Of this 47, 13 exhibited the MDR profile and 34 exhibited XDR profile and all 47 were included in the phenotypic and genotypic tests to search for other resistance mechanisms (Table 3). The Hodge test showed the presence of carbapenemase activity in just one isolate, which showed MDR/XDR profile, but the blaOXA and blaKPC genes were not detected by PCR in any isolate analyzed. The frequency of phenotypic production of the AmpC cephalosporin through the D-Test was common among isolates resistant to carbapenems (76.6%). However, the frequency of AmpC activity decreased in MDR strains (64.7%) and dropped further in XDR strains (38.4%).
Table 3. Characterization of resistance mechanisms in carbapenem-resistant P. aeruginosa isolates, both multidrug-resistant and extensively drug-resistant.
| Phenotype | Total |
Resistance Mechanisms | |||||
|---|---|---|---|---|---|---|---|
| Carbapenemase | AmpC cephalosporinase | Loss of OprD | Efflux pump | ||||
| Hodge-test/ Positive (%) | PCR1/ Positive (%) | D-Test/ Positive (%) | qRT-PCR2*/ Positive (%) | qRT-PCR*/ Positive (%) | qRT-PCR*/ Positive (%) [system] | ||
| Carbapenem resistant | 47 | 47/1 (2.1%) | 47/0 (-) | 47/36 (76.6) | 14/10 (71.4) | 14/10 (71.4) | 14/8 (57.1) [ABM+] 14/9 (64.3) [XY+] |
| MDR3 | 34 (72.3) | 34/1 (2.9) | 34/0 (-) | 34/22 (64.7) | 10/6 (60.0) | 10/6 (60.0) | 10/7 (70.0) [ABM+] 10/9 (90.0) [XY+] |
| XDR4 | 13 (27.7) | 13/1 (7.7) | 13/0 (-) | 13/5 (38.5) | 4/2 (50.0) | 4/3 (75.0) | 4/3 (75.0) [ABM+] 4/4 (100.0) [XY+] |
1PCR, Polymerase Chain Reaction
2qRT-PCR, quantitative Real Time-Polymerase Chain Reaction
3MDR, Multidrug-resistant profile
4XDR, Extensively drug-resistant profile
*Only 14 of the 47 isolates resistant to carbapenems were tested for qRT-PCR (10 MDR and 4 XDR).
Of 47 non-MBL carbapenem-resistant isolates, 14 were included in the qRT-PCR test for efflux pump overexpression, overproduction of AmpC and loss/reduction OprD porin (Table 4). The frequency of isolates with AmpC overproduction and loss of OprD porin was 71.4% (10/14) for both, and MexABOprM and MexXY pumps were 57.1% (8/14) and 64.3% (9/14), respectively. Most isolates with the MDR/XDR profile showed an association with three or more resistance mechanisms, and the presence of AmpC overproduction and loss of OprD porin predominated among non-MDR/XDR isolates that were only resistant to carbapenems (N = 4).
Table 4. Characterization of efflux pumps overexpression, overproduction of AmpC and loss/reduction OprD in P. aeruginosa isolates.
| Isolates | Overproduction of AmpC | Overexpression of efflux pumps |
Loss OprD |
Resistance profile (MDR1/XDR2) | ||||
|---|---|---|---|---|---|---|---|---|
| D-Test3 | AmpC | ABM | XY | EFN | CDJ | OprD | ||
| 1 | - | + | - | + | - | - | + | CAZ4, PPTAZ5, IMI6, CIP8, LEV9, GEN10, AZT11 (MDR) |
| 2 | + | + | - | + | - | - | - | CPM12, IMI, MER7, CIP, GEN, AMK13, AZT (MDR) |
| 3 | + | - | + | + | - | - | + | CAZ, CPM, PPTAZ, IMI, MER, CIP, LEV, GEN, AMK, AZT (XDR) |
| 4 | + | - | + | - | - | - | + | CPM, IMI, MER, CIP, GEN, AMK, AZT (MDR) |
| 5 | + | + | + | + | - | - | + | CAZ, CPM, PPTAZ, IMI, MER, CIP, LEV, GEN, AZT (XDR) |
| 6 | + | + | + | + | - | - | + | CAZ, IMI, MER, CIP, LEV, GEN, AZT (MDR) |
| 7 | - | + | + | + | - | - | - | CAZ, CPM, IMI, MER, CIP, LEV, GEN, AMK (MDR) |
| 8 | + | + | + | - | - | - | + | IMP, MER (-) |
| 9 | + | + | - | - | - | - | + | IMP (-) |
| 10 | + | - | - | + | - | - | + | CAZ, CPM, IMI, MER, CIP, LEV, GEN, AMK, AZT (XDR) |
| 11 | - | - | + | + | - | - | - | CAZ, CPM, IMI, MER (MDR) |
| 12 | + | + | - | - | - | - | + | IMI (-) |
| 13 | + | + | - | - | - | - | + | IMI, MER (-) |
| 14 | + | + | + | + | - | - | - | CAZ, CPM, PPTAZ, IMI, MER, CIP, LEV, GEN (XDR) |
|
Total N (%) |
11 (78,0) | 10 (71,4) | 8 (57,1) | 9 (64,3) | 0 (-) | 0 (-) | 10 (71,4) | - |
1MDR, Multidrug-resistant
2XDR, Extensively-resistant
3Phenotypic test for overproduction of AmpC
4Ceftazidime
5Piperacillin-tazobactam
6Imipenem
7Meropenem
8Ciprofloxacin
9Levofloxacin
10Gentamicin
11Aztreonam
12Cefepime
13Amicacin.
AmpC, Overproduction of AmpC; ABM, Overexpression of MexABOprM; XY, Overexpression of MexXY; EFN, Overexpression of MexEFOprN; CDJ, Overexpression of MexCDOprJ; OprD, Loss/alteration of OprD porin.
+ or–(positive or negative).
Discussion
Pseudomonas aeruginosa is considered one of the most problematic pathogens among gram-negative bacteria that cause hospital infections, especially due to its extraordinary ability to acquire resistance genes [31,32]. In this study, we found that high rates of carbapenem-resistance, MDR and XDR profiles existed in P. aeruginosa clinical isoltes. A multicenter study in Latin America reported significant rates of reduced susceptibility to meropenem: 53.8% among the isolates from Argentina, 46.7% in Brazil, 33.3% in Chile and 28.8% of isolates from Mexico [8]. In Brazil, surveillance studies and independent research groups in the south and center of the country have reported an increasing trend in imipenem resistance rates for the years 2001, 2004 and 2009, at frequencies of approximately 30.2%, 58.9% and 82.7%, respectively [3,33,34]. In these cases, the use of antibiotic therapy was restricted to therapy with alternative drugs considered problematic due to their high toxicity, such as polymyxins (polymyxin B and colistin), that are often not commercially available in Brazil [35,36]. All isolates in our study were sensitive to polymyxin; however, the presence of clinical isolates with reduced susceptibility to this antimicrobial agent class has been reported in the literature [37,38].
Usually, the antibiotic use is high in developing countries, particularly in intensive care units [39,40]. This high consumption of antimicrobials results in a higher incidence of multidrug-resistant and extensively drug-resistant bacteria [41], combined with greater dissemination of these microorganisms [42]; this is explained, in part, by the lack of resources and failure to implement control practices and prevention [41]. The data from this study have verified most of the risk factors mentioned in the literature as those related to the acquisition of bacteremia by P. aeruginosa resistant to antimicrobials, including the over use of antimicrobials, lengthy hospital stays, admission to an intensive care unit, presence of invasive procedures, especially intravenous devices and mechanical ventilation, as well as a secondary source of infection, especially the lungs [43,44].
As previously mentioned, it is known that both the prior use of antimicrobials, as well as their use during hospitalization, are related to the increase in infections by resistant isolates [45,46]. Samonis et al. [47] demonstrated that the prior use of fluoroquinolones was independently associated with infection by extensively drug-resistant P. aeruginosa isolates. In this study, the use of broad-spectrum cephalosporins was predominant among the prescribed antibiotics, with large variations in the observed period. However, the use of carbapenems, including imipenem and meropenem, was also high. Additionally, in general, the antibiotics use in the Uberlandia University Hospital (UFU-HC) was much higher as compared to other countries [48], but without significant relationship with increased incidence of P. aeruginosa resistant to carbapenems in this study.
P. aeruginosa has a wide variety of intrinsic and acquired resistance mechanisms to different antimicrobials [2,13]. The carbapenem-resistance often results from the production of carbapenemases, particularly those that hydrolyze carbapenem, such as metallo-β-lactamases [2,4,5,49]. The prevalence of P. aeruginosa resistant to carbapenems phenotypically through production of MBL in Brazilian studies achieves rates above 50% in different geographic regions, and the SPM-1 enzyme is the most prevalent among the resistant isolates in the country [28,33]. However, other MBLs, including the VIM and IMP types, have also been identified in P. aeruginosa isolates in Brazil [26,37,49]. An important change in the epidemiology of P. aeruginosa has been observed in the UFU-HC, in which only producers SPM-1 were found from 2005 to 2011 [50] to the present, where our results indicate the emergence and spread of VIM.
When we evaluated the clonal relationship between strains containing the blaSPM and blaVIM genes, we observed high similarity (greater than 80%) among isolates containing blaSPM; this was not observed for those containing the blaVIM gene. The presence of a multidrug-resistant P. aeruginosa clone persisting for long periods in different hospital units reinforces the idea of resistance genes dissemination among hospitalized patients, emphasizing the need to improve prevention and control strategies of infection [51–53].
The carbapenem resistance mechanisms were investigated in greater detail in those isolates negative for MBL production, but no gene related to other carbapenemases was detected, and a positive result for MBL production was only observed through the Hodge test. These results suggest that in the absence of an efficient carbapenemase, other resistance mechanisms exist in these isolates, including overproduction of AmpC cephalosporinase, changes in permeability of the outer membrane through loss/reduction of the OprD porin and overexpression of efflux pumps.
Of all the efflux pumps already described in P. aeruginosa, MexABOprM, MexCDOprJ, and MexXY MexEFOprN are among the best-characterized systems, and they are associated with a variety of antibiotics resistance in clinical isolates [13,14]. In addition, they are known to be associated with multidrug-resistance, since one system can act on multiple substrates [54,55]. In the present study, all the isolates that tested positive in qRT-PCR and were characterized with overexpression of efflux pumps also exhibited some another type of associated resistance mechanism. In addition, it became apparent that the MDR phenotype, and/or especially the XDR phenotype, was present between the isolates that showed association of three or more resistance mechanisms, except the presence of MBL.
According to previous studies in Brazil, the efflux pumps most commonly found in clinical isolates of P. aeruginosa include MexABOprM and MexXY systems, which are constitutively expressed and play an important role in carbapenem-resistance and cover a wider range of antimicrobial resistance than the MexCDOprJ and MexEFOprN pumps [55,56]. In this study, no increased expression of mexD and mexF genes was observed among the isolates investigated, and the frequency of MexABOprM and MexXY overexpression was high. A recent study conducted on clinical isolates of multidrug-resistant P. aeruginosa from hospitals in Thailand revealed that 92.06% of those isolates overexpress the MexABOprM system and 63.49% overexpress the MexXY system [57]. In Brazil, another study evaluating this overexpression in clinical isolates of P. aeruginosa recovered from blood noted the presence of MexABOprM and MexXY expression in 27.1% and 50.8% of the isolates, respectively [26].
According to the literature, one of the most consistent findings for resistance to carbapenems, particularly imipenem, has been the impermeability of the membrane due to loss of the OprD porin [13,58–62], and several groups have reported rates of this type of mechanism exceeding 80% among clinical isolates of P. aeruginosa [26]. Here, we also noted significant rate reduction in the expression of the oprD gene. Moreover, the association between multidrug-resistance via loss of OprD in P. aeruginosa clinical isolates has been reported in literature, mainly as a synergistic effect with other resistance mechanisms [63]. In addiction, through this survey, this association has been well-characterized, as isolates with MDR/XDR and OprD porin loss also had concomitant overexpression of efflux pumps and hyperproduction of AmpC.
In conclusion, a high rate of resistance and multidrug-resistance among Pseudomonas aeruginosa isolates suggest some level of SPM-1 transmission that reinforces the importance of greater rigor in the prevention and control of infection in healthcare settings. Our results further confirm previous reports showing a high incidence of carbapenem-resistant P. aeruginosa in Brazilian hospitals and that this is associated with the abusive and indiscriminate use of antibiotics, indicating that it is also necessary to revise the antimicrobial use policies. Regarding the resistance mechanisms, our results showed that, in the absence of an effective carbapenemase, resistance to carbapenems in P. aeruginosa can be explained by overexpression of MexABOprM and MexXY systems, AmpC overproduction and loss of the OprD porin, that when presented in association with other factors can contribute to expression of MDR/XDR phenotypes.
Supporting information
A similarity coefficient of 80% was chosen for cluster definition. 1Metallo-β-lactamase.
(TIF)
(DOCX)
(DOCX)
Acknowledgments
We thank FAPEMIG (Fundação de Amparo à Pesquisa de Minas Gerais), CNPq (Conselho Nacional de Desenvolvimento Científico e Tecnológico) and CAPES (Coordenação de Aperfeiçoamento de Pessoal de Nível Superior) for the financial support and scholarships.
Data Availability
Data is available on figshare at 10.6084/m9.figshare.4286534.
Funding Statement
We thank FAPEMIG (Fundação de Amparo à Pesquisa de Minas Gerais), CNPq (Conselho Nacional de Desenvolvimento Científico e Tecnológico) and CAPES (Coordenação de Aperfeiçoamento de Pessoal de Nível Superior) for the financial support and scholarships.
References
- 1.Alhazmi A. Pseudomonas aeruginosa–Pathogenesis and Pathogenic Mechanisms. International Journal of Biology 2015; 7. [Google Scholar]
- 2.Breidenstein EBM, de la Fuente-Núñez C, Hancock REW. Pseudomonas aeruginosa: all roads lead to resistance. Trends in Microbiol. 2011; 19: 419–426. [DOI] [PubMed] [Google Scholar]
- 3.Sader HS, Gales AC, Pfaller MA, Mendes RE, Zoccoli C, Barth A, Jones RN. Pathogen frequency and resistance patterns in Brazilian hospitals: summary of results from three years of the SENTRY Antimicrobial Surveillance Program. Braz J Infect Dis. 2001; 5: 200–214. [DOI] [PubMed] [Google Scholar]
- 4.Van der Bij AK, Van Mansfeld R, Peirano G, Goessens WH, Severin JA, Pitout JD, Willems R, Van Westreenen M. First outbreak of VIM-2 metallo-b-lactamase-producing Pseudomonas aeruginosa in The Netherlands: microbiology, epidemiology and clinical outcomes. Int J Antimicrob Agents 2011; 37: 513–518. doi: 10.1016/j.ijantimicag.2011.02.010 [DOI] [PubMed] [Google Scholar]
- 5.Van der Bij AK, Van der Zwan D, Peirano G, Severin JA, Pitout JD, Van Westreenen M, Goessens WH. MBL-PA Surveillance Study Group (2012). Metallo-b-lactamase-producing Pseudomonas aeruginosa in the Netherlands: the nationwide emergence of a single sequence type. Clin Microbiol Infect. 2012; 18: E369–E372. doi: 10.1111/j.1469-0691.2012.03969.x [DOI] [PubMed] [Google Scholar]
- 6.Moreira MR, Guimarães MP, Rodrigues AAA, Gontijo-Filho PP. Antimicrobial use, incidence, etiology and resistance patterns in bacteria causing ventilator-associated pneumonia in a clinical-surgical intensive care unit. Rev Soc Bras Med Trop. 2013; 46: 39–44. [DOI] [PubMed] [Google Scholar]
- 7.Porto JP, Santos RO, Gontijo-Filho PP, Ribas RM. Active surveillance to determine the impact of methicillin resistance on mortality in patients with bacteremia and influences of the use of antibiotics on the development of MRSA infection. Rev Soc Bras Med Trop. 2013; 46: 713–718. doi: 10.1590/0037-8682-0199-2013 [DOI] [PubMed] [Google Scholar]
- 8.Gales AC, Castanheira M, Jones RN, Sader HS. Antimicrobial resistance among gram-negative bacilli isolated from latin America: results from SENTRY antimicrobial Suveillance Program (Latin America, 2008–2010). Diagnostic Microbiology and Infections Diseases 2012; 73: 354–360. [DOI] [PubMed] [Google Scholar]
- 9.Gales AC, Menezes LC, Silbert S, Sader HS. Dissemination in distinct Brazilian regions of an epidemic carbapenem-resistant Pseudomonas aeruginosa producing SPM metallo-β-lactamases. Journal of Antimicrobial Chemotherapy 2003; 52: 699–702. doi: 10.1093/jac/dkg416 [DOI] [PubMed] [Google Scholar]
- 10.Liu Q, Li X, Li W, Du X, He J, Tao C, Feng Y. Influence of carbapenem resistance on mortality of patients with Pseudomonas aeruginosa infection: a meta-analysis. Scientific Reports 2015; 5: 11715 doi: 10.1038/srep11715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Quale J, Bratu S, Gupta J, Landman D. Interplay of Efflux System, ampC, and oprD Expression in Carbapenem Resistance of Pseudomonas aeruginosa Clinical Isolates. Antimicrobial Agents and Chemotherapy 2006; 50: 1633–1641. doi: 10.1128/AAC.50.5.1633-1641.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pai H, Kim J, Kim J, Lee JH, Choe KW, Gotoh N. Carbapenem Resistance Mechanisms in Pseudomonas aeruginosa Clinical Isolates. Antimicrobial Agents and Chemotherapy 2001; 480–484. doi: 10.1128/AAC.45.2.480-484.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lister PD, Wolter DJ, Hanson ND. Bacterial-resistant Pseudomonas aeruginosa: clinical impact and complex regulation of chromosomally encoded resistance mechanisms. Clinical Microbiology Reviews 2009; 22: 582–610. doi: 10.1128/CMR.00040-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nikaido H, Pages JM. Broad-specificity efflux pumps and their role in multidrug resistance of Gram-negative bactéria. FEMS Microbiology Review 2012; 36: 340–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Santos KV, Carvalho MAR, Martins WA, Andrade HM, Veloso LC, Coutinho SC, Bahia JL, Andrade JPL, Apolônio ACM, Diniz CG, Nicoli JR, Farias LM. Phenotypic Changes in a Laboratory-derived Ertapenem-resistant Escherichia coli strain. Journal of Chemotherapy 2011; 23: 135–139. doi: 10.1179/joc.2011.23.3.135 [DOI] [PubMed] [Google Scholar]
- 16.CDC. Centers for Disease Control and Prevention. Guidelines for the prevention of intravascular catheter–related infections. Mortality and Morbidity Weekly Reports 2002; 51: 1–36. [PubMed] [Google Scholar]
- 17.Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM. CDC definitions for nosocomial infections. In: Olmsted, R.N. (Eds.), APIC Infections Control and Applied Epidemiology: Principles and Practice. Mosby, St Louis, 1996; A-1–A-20.
- 18.Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, Harbarth S, Hindler JF, Kahlmeter G, Olsson-Liljequist B, Paterson DL, Rice LB, Stelling J, Struelens MJ, Vatopoulos A, Weber JT, Monnet DL. Multidrug-resistant, extensively-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012; 18: 268–81. doi: 10.1111/j.1469-0691.2011.03570.x [DOI] [PubMed] [Google Scholar]
- 19.Gulen TA, Guner R, Celikbilek N, Keske S, Tasyaran M. Clinical importance and cost of bacteremia caused by nosocomial multi drug resistant Acinetobacter baumannii. International Journal of Infectious Diseases 2015; 38: 32–35. doi: 10.1016/j.ijid.2015.06.014 [DOI] [PubMed] [Google Scholar]
- 20.WHO. Collaborating center for drugs statistics methodology. anatomical Therapeutic Chemical (ATC), Classification index with Defined Daily Doses (DDD), Oslo, Norway. World Health Organization. (http://www.whocc.no). 2000.
- 21.CLSI. Performance Standards for Antimicrobial Susceptibility Testing. Clinical and Laboratory Standards Institute. Doc M100-S20. 2010.
- 22.CLSI. Performance Standards for Antimicrobial Susceptibility Testing: Twenty-first Informational Supplement. Clinical Laboratory Standards Institute, Wayne, PA, USA. Doc M100-S21. 2011.
- 23.CLSI. Performance standards for antimicrobial susceptibility testing; 19th informational supplement. Clinical Laboratory Standards Institute, Wayne, PA. Doc M100-S19. 2009.
- 24.Arakawa Y, Shibata N, Shibayama K, Kurokawa H, Yagi T, Fujiwara H, Goto M. Convenient test for screening metallo-β-lactamase-producing gram-negative bacteria by using thiol compounds. J Clin Microbiol 2000; 38: 40–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dunne WMJ, Hardin D. Use of several inducer and substrate antibiotic combinations in a disk approximation assay format to screen for AmpC induction in patients isolates of Pseudomonas aeruginosa, Enterobacter spp., Citrobacter spp. and Serratia spp. Journal of Clinical Microbiology 2005; 43: 5945–5949. doi: 10.1128/JCM.43.12.5945-5949.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Xavier DE, Picão RC, Girardello R, Fehlberg LC, Gales AC. Efflux pumps expression and its association with porin down-regulation and b-lactamase production among Pseudomonas aeruginosa causing bloodstream infections in Brazil. BMC Microbiology 2010; 10: 217–223. doi: 10.1186/1471-2180-10-217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Woodford N. Rapid Characterization of β-lactamases by Multiplex PCR. In: Gillespie, s. h.; McHugh, T. D. Antibiotic Resistance Protocols: Second Edition, Methods in Molecular Biology 2010; 642: 181–192. [DOI] [PubMed]
- 28.Galetti R. Estudo de Pseudomonas aeruginosa produtoras de metalo-beta-lactamases e de genes envolvidos na resistência aos carbapenêmicos. 49 f. Thesis, Universidade de São Paulo, Ribeirão Preto. 2010.
- 29.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods 2001; 25: 402–408. doi: 10.1006/meth.2001.1262 [DOI] [PubMed] [Google Scholar]
- 30.Pfaffl MW. A new mathematical model for relative quantification in real-time RT-PCR. Nucleic Acids Research 2001; 29: 2002–2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Livermore DM. Multiple mechanism of antimicrobial resistance in Pseudomonas aeruginosa: Our worst nightmare? Clinical Infection Diseases 2002; 34: 634–640. [DOI] [PubMed] [Google Scholar]
- 32.Neves PR, Silva MTN, Goncalves TM, Lincopan N, Mamizuka EM. Multirresistência mediada por metalo-beta-lactamase, porinas, bombas de efluxo e metilases, em isolados clinicos de Pseudomonas aeruginosa. In: XI CONGRESSO Brasileiro de Controle de Infecção e Epidemiologia Hospitalar, Rio de Janeiro. Brazilian Journal of Infectious Disease 2008; 12: 30. [Google Scholar]
- 33.Gonçalves DC, Lima AB, Leao LS, Filho JR, Pimenta FC, Vierira JD. Detection of metallo-beta-lactamase in Pseudomonas aeruginosa isolated from hospitalized patients in Goiânia, State of Goias. Revista da Sociedade Brasileira de Medicina Tropical 2009; 42: 411–414. [DOI] [PubMed] [Google Scholar]
- 34.Zavascki AP, Cruz RP, Goldani LZ. High rate of antimicrobial resistance in Pseudomonas aeruginosa at a tertiary-care teaching hospital in southern Brazil. Infectious Control of Hospital Epidemiology 2004; 25: 805–807. [DOI] [PubMed] [Google Scholar]
- 35.Furtado GH, D’Azevedo PA, Santos AF, Gales AC, Pignatari AC, Medeiros EA. Intravenous polymyxin B for the treatment of nosocomial pneumonia caused by multidrug-resistant Pseudomonas aeruginosa. International Journal of Antimicrobial Agents 2007; 30: 315–319. doi: 10.1016/j.ijantimicag.2007.05.017 [DOI] [PubMed] [Google Scholar]
- 36.Levin SS, Barone AA, Penco J, Santos MV, Marinho IS, Arruda EA, Manrique EI, Costas SF. Intravenous colistin as therapy for nosocomial infections caused by multidrug-resistant Pseudomonas aeruginosa and Acinetobacter baumannii. Clinical Infectious Diseases 1999; 28: 1008–1011. doi: 10.1086/514732 [DOI] [PubMed] [Google Scholar]
- 37.Franco MR, Caiaffa-Filho HH, Burattini MN Rossi F. Metallo-beta-lactamases among imipenem-resistant Pseudomonas aeruginosa in a Brazilian university hospital. Clinics 2010; 65: 825–829. doi: 10.1590/S1807-59322010000900002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Laupland KB. Population-based epidemiological study of infections caused by carbapenem-resistant Pseudomonas aeruginosa in the Calgary Health Region: importance of metallo-beta-lactamase (MBL)-producing strains. Journal of Infectious Disease 2005; 192: 1606–1612. [DOI] [PubMed] [Google Scholar]
- 39.Haak H, Radyowijati A. Determinants of Antimicrobial Use: Poorly Understood–Poorly, in: Sosa, A.J., Byarugaba, D.K., Amábile-Cuevas, C.F., Hsueh, P., Kariuki, S., Okeke, I.N. (Eds.), Antimicrobial resistance in developing countries. 2010.
- 40.Porto JP, Mantese OC, Arantes A, Freitas C, Gontijo-Filho PP, Ribas RM. Nosocomial infections in a pediatric intensive care unit of a developing country: NHSN surveillance. Revista da Sociedade Brasileira de Medicina Tropical 2012; 45: 475–479. [DOI] [PubMed] [Google Scholar]
- 41.WHO. World Health Organization. Antimicrobial resistance. World Health Organization. (http://www.who.int/mediacentre/factsheets/fs194/en/). 2015.
- 42.Davies J, Davies D. Origins and Evolution of Antibiotic Resistance. Microbiology and Molecular Biology Reviews 2010; 74: 417–433. doi: 10.1128/MMBR.00016-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tuon FF, Gortz LW, Rocha JL. Risk factors for pan-resistant Pseudomonas aeruginosa bacteremia and the adequacy of antibiotic therapy, Brazillian Journal of Infectious Disease 2012; 16: 351–356. [DOI] [PubMed] [Google Scholar]
- 44.Vitkauskienė A, Skrodenienė E, Dambrauskienė A, Macas A, Sakalauskas R. Pseudomonas aeruginosa bacteremia: resistance to antibiotics, risk factors, and patient mortality. Medicina (Kaunas) 2010; 46: 490–495. [PubMed] [Google Scholar]
- 45.Lemmen SW, Hafner H, Kotterik S, Lutticken R, Topper R. Influence of an infectious disease service on antibiotic prescription behaviour and selection of multiresistant pathogens. Journal of Infectious Disease 2000; 28: 384–387. [DOI] [PubMed] [Google Scholar]
- 46.Lepper PM, Grusa E, Reichl H, Hogel J, Trautmann M. Consumption of imipenem correlates with beta-lactam resistance in Pseudomonas aeruginosa. Antimicrobial Agents and Chemoterapy 2002; 46: 2920–2925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Samonis G, Vardakas KZ, Kofteridis DP, Dimopoulou D, Andrianaki AM, Chatzinikolaou I, Katsanevaki E, Maraki S, Falagas ME. Characteristics, risk factors and outcomes of adult cancer patients with extensively drug-resistant Pseudomonas aeruginosa infections. Infection 2014; 42: 721–728. doi: 10.1007/s15010-014-0635-z [DOI] [PubMed] [Google Scholar]
- 48.Meyer E, Jonas D, Schwab F, Rueden H, Gastmeier P, Daschner FD. Design of a Surveillance System of Antibiotic Use and Bacterial Resistance in German Intensive Care Units (SARI). Infection 2003; 47: 208–215. [DOI] [PubMed] [Google Scholar]
- 49.Sader HS, Reis AO, Silbert S, Gales AC. IMPs, VIMs and SPMs: the diversity of metallo-b-lactamases produced by carbapenem-resistant Pseudomonas aeruginosa in a Brazilian hospital. Clinical Microbiology and Infection 2005; 11: 73–76. doi: 10.1111/j.1469-0691.2004.01031.x [DOI] [PubMed] [Google Scholar]
- 50.Cezário RC, Duarte de Morais L, Ferreira JC, Costa-Pinto RM, Da Costa Darini AL, Gontijo-Filho PP. Nosocomial outbreak by imipenem-resistant metallo-β-lactamase-producing Pseudomonas aeruginosa in an adult intensive care unit in a Brazilian teaching hospital. Enfermedades Infecciosas y Microbiología Clínica 2009; 27: 269–274. doi: 10.1016/j.eimc.2008.09.009 [DOI] [PubMed] [Google Scholar]
- 51.Cholley P, Thouverez M, Hocquet D, Mee-Marquet NVD, Talon D, Bertrand X. Most Multidrug-Resistant Pseudomonas aeruginosa Isolates from Hospitals in Eastern France Belong to a Few Clonal Types. Journal of Clinical Microbiology 2011; 49: 2578–2583. doi: 10.1128/JCM.00102-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cortes JA, Cuervo SI, Urdaneta AM, Potdevin G, Arroyo P, Bermúdez D, Correa A, Villegas MV. Identifying and Controlling a Multiresistant Pseudomonas aeruginosa Outbreak in a Latin-American Cancer Centre and Its Associated Risk Factors. The Brazilian Journal of Infectious Diseases 2009; 13: 99–103. [DOI] [PubMed] [Google Scholar]
- 53.Tacconelli E, Cataldo MA, Dancer SJ, De Angelis G, Falcone M, Frank U, Kahlmeter G, Pan A, Petrosillo N, Rodrıguez-Bano J, Singh N, Venditti M, Yokoe DS, Cookson B. ESCMID guidelines for the management of the infection control measures to reduce transmission of multidrug-resistant Gram-negative bacteria in hospitalized patients. Clin Microbiol Infect. 2014; 20: 1–55. [DOI] [PubMed] [Google Scholar]
- 54.Askoura M, Mottawea W, Abujamel T, Taher I. Efflux pump inhibitors (EPIs) as new antimicrobial agents against Pseudomonas aeruginosa. Libyan Journal of Medicine 2011; 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Neves PR. Alterações da permeabilidade e expressão de bombas de efluxo em isolados clínicos de Pseudomonas aeruginosa resistente ao imipenem. PhD Thesis. Universidade de São Paulo, São Paulo. 2010.
- 56.Pereira DC. Sistemas de efluxo MexABOprM e MexXY e produção de carbapenemases em Pseudomonas aeruginosa: efeito na resistência aos carbapenêmicos. Thesis. Universidade Federal do Rio Grande do Sul. Porto Alegre. 2013.
- 57.Khuntayaporn P, Montakantikul P, Santanirand P, Kiratisin P, Chomnawang MT. Molecular investigation of carbapenem resistance among multidrug-resistant Pseudomonas aeruginosa isolated clinically in Thailand. Microbiology and Immunology 2013; 57: 170–178. doi: 10.1111/1348-0421.12021 [DOI] [PubMed] [Google Scholar]
- 58.Bonomo RR, Szabo D. Mechanisms of multidrug resistance in Acinetobacter species and Pseudomonas aeruginosa. Clinical Infectious Diseases 2006; 43: 49–56. [DOI] [PubMed] [Google Scholar]
- 59.Fusté E, López-Jiménez L, Segura C, Gainza E, Vinuesa T, Viñas M. Carbapenem-resistance mechanisms of multidrug-resistant Pseudomonas aeruginosa. Journal of Medical Microbiology 2013; 62: 1317–1325. doi: 10.1099/jmm.0.058354-0 [DOI] [PubMed] [Google Scholar]
- 60.Lee JY, Ko KS. OprD mutations and inactivation, expression of efflux pumps and AmpC, and metallo-β-lactamases in carbapenem-resistant Pseudomonas aeruginosa isolates from South Korea. International Journal Antimicrobial 2012; 40: 168–172. [DOI] [PubMed] [Google Scholar]
- 61.Lister PD. Chromosomally-encoded resistance mechanisms of Pseudomonas aeruginosa: therapeutic implications. American Journal of Pharmacogenomics 2002; 2: 235–243. [DOI] [PubMed] [Google Scholar]
- 62.Livermore D. Of Pseudomonas, porins, pumps and carbapenems. Journal of Antimicrobial and Chemotherapy 2001; 47: 247–250. [DOI] [PubMed] [Google Scholar]
- 63.Clímaco E. Análise molecular de mecanismos determinantes de resistência a antibióticos em Pseudomonas aeruginosa e Acinetobacter spp. PhD Thesis; Universidade de São Paulo. Ribeirão Preto. 2011.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A similarity coefficient of 80% was chosen for cluster definition. 1Metallo-β-lactamase.
(TIF)
(DOCX)
(DOCX)
Data Availability Statement
Data is available on figshare at 10.6084/m9.figshare.4286534.