Abstract
Socioeconomic disadvantage is consistently linked with higher risk for internalizing problems, and stress is likely one important mechanism explaining this increased risk. Few studies have examined socioeconomic differences in hair cortisol, a novel biomarker of long-term adrenocortical activity and chronic stress. Moreover, no studies have examined whether differences in hair cortisol might explain socioeconomic disparities in internalizing problems. To address these gaps, we first examined relations of socioeconomic status (SES; family income and parental education) to variation in both parents’ and children’s hair cortisol concentrations (HCC) and then tested whether HCC and perceptions of stress mediated relations of SES to parents’ and children’s internalizing symptoms. Participants were a socioeconomically diverse sample of 35 parents and 26 children (ages 5 to 7). Parents completed questionnaires, and hair samples were collected from parents and children. Parents reported on children’s internalizing symptoms on average 2 years after the initial visit. Results demonstrated that lower parental education was associated with higher HCC for both parents and children. Effects for child HCC held even after controlling for parent HCC. Lower family income was associated with higher parent HCC, but not child HCC. This relation was nonlinear, such that the relation between HCC and income was strongest among the most disadvantaged parents. Furthermore, associations of SES with parental anxiety were significantly mediated by parental perceptions of stress and marginally mediated by parent HCC. These findings suggest that socioeconomic disadvantage is associated with greater accumulation of cortisol in hair in parents and children, and that both perceived and biological markers of stress capture important facets of the experiences that underlie socioeconomic disparities in adult anxiety.
Keywords: Hair cortisol, education, income, anxiety, depression, children
1. Introduction
1.1 SES, Hair Cortisol and Internalizing Symptoms in Children and their Parents
There are well-established socioeconomic disparities in risk for internalizing problems, such as anxiety and depression, with a greater risk for such problems among both low SES adults (Alegria et al., 2000; Callan et al., 2015; Hudson, 2005; Lorant et al., 2003; Murali and Oyebode, 2004) and children from low SES families (Bradley and Corwyn, 2002; Evans and Cassells, 2014; McLaughlin et al., 2011; Reiss, 2013; Slopen et al., 2010; Tracy et al., 2008). Low-SES families frequently face a host of stressors, such as financial uncertainty, crowding, noise, household chaos, fewer family routines, and a generally higher level of unpredictability, all of which can contribute to an increase in stress for both parents and children (Adler and Snibbe, 2003; Combs-Orme and Cain, 2006; Evans et al., 2005). Indeed, socioeconomic disadvantage has been linked with higher levels of stress, at both the behavioral (e.g., perceptions of stress) and physiological levels (e.g., salivary cortisol) (Dowd et al., 2009). In addition, behavioral measures of stress and salivary cortisol have been linked with internalizing problems (Russell et al 2012; Staufenbiel et al 2013). Yet, few studies of SES have focused on measures of chronic physiological stress, such as hair cortisol concentration (HCC). There is also a lack of research investigating associations among SES, HCC, and risk of internalizing problems in parents and children. To address these gaps in the literature, we first examined relations of SES to HCC in parents and children. We then examined the extent to which HCC and parental perceptions of stress mediated the association between SES and internalizing symptoms in parents and children.
1.2 Associations between SES and Hair Cortisol
Several studies have demonstrated links between SES and variations in cortisol in both children and adults (Dowd et al., 2009). These earlier studies, however, used salivary, urinary, or serum measures of cortisol which are affected by acute factors and which provide estimates of HPA axis activity at a certain point in time. As such, they are limited in their ability to capture chronic stress (Staufenbiel et al., 2013). Recently, the measurement of cortisol in hair (HCC) has emerged as a promising technique for assessing chronic stress levels (Russell et al., 2012). Cortisol accumulates in hair as it grows and is stable for at least the first 6cm of hair, which corresponds to about 6 months of hair growth (Russell et al., 2012). As SES is a proxy for chronic stress, it may be that hair cortisol, as a biological marker of chronic stress, would be more strongly linked to SES and would better explain socioeconomic disparities in internalizing problems than would other physiological measures of stress.
Several recent studies have examined associations between SES and HCC, and findings have been mixed. In adults, one study reported that lower income was associated with higher HCC (Serwinski et al., 2016), but others have not found differences in adult HCC by income (Chen et al., 2013; Wosu et al., 2015) or education (Serwinski et al, 2016; Wosu et al., 2015). In children, some studies have reported that lower parental education (Rippe et al., 2016; Vaghri et al., 2013; Vliegenthart et al., 2016) and lower family income (Rippe et al., 2016) are associated with higher HCC, whereas others have not found associations between child HCC and parental income (Vaghri et al., 2013) or parental education (Groeneveld et al., 2013; Karlen et al., 2013; Liu et al., 2016). At least two of these studies, however, may have been limited in their ability to detect associations of SES with HCC because they utilized small samples, which were not purposefully recruited from a broad range of socioeconomic backgrounds (Groeneveld et al., 2013; Liu et al., 2016). Differences in the measurement of SES may also have contributed to these mixed findings. Even among those measuring the same construct (i.e., income or education), some studies used continuous measures whereas others used categorical measures, which also differed across studies. Interestingly, Karlen et al. (2013) did find that children living in apartments versus in villas had higher cortisol, suggesting that socioeconomic differences may have played a role. Moreover, because there may be some genetic heritability of HCC (Karlen et al., 2013), it may be important to control for parental HCC when examining SES disparities in child HCC, in order to rule out possible genetic bias.
1.3 Associations between Hair Cortisol and Internalizing Problems
There has long been interest in understanding the role of the HPA axis in anxiety and depressive disorders. However, most prior studies examining these associations have measured salivary or serum cortisol (Staufenbiel et al., 2013). Higher HCC have been hypothesized to be associated with anxiety and depression in both children and adults, but evidence regarding these associations has been mixed (Ouellette et al., 2015). One study reported higher HCC in adults diagnosed with depression (Dettenborn et al., 2012) whereas other work has found no difference in HCC by depression diagnosis in a sample of patients with coronary artery disease (Dowlati et al., 2010) and no relation of HCC to depressive symptoms (Ouellette et al., 2015). One study of adults found that lower HCC was associated with generalized anxiety disorder (Steudte et al., 2011). In children, higher maternal depression has been associated with lower HCC at 1 year of age (Palmer et al., 2013), but another study found no association between children’s HCC and their symptoms of anxiety or depression (Ouellette et al., 2015). This mixed pattern of results may be influenced by differences in the measurement of internalizing problems (i.e., diagnosis versus symptom report) or by diversity across samples in terms of demographic characteristics such as age, sex, and comorbidities.
1.4 The Current Study
In the current study, we first examined associations between SES (family income and parental education) and HCC in parents and children. Importantly, because there may be some genetic basis for HCC (Karlen et al., 2013), we controlled for parent HCC when examining socioeconomic differences in children’s HCC. Family income and parental education were analyzed separately because they contribute distinctly to children’s development (Duncan and Magnuson, 2012; Hanson et al., 2011; Noble et al., 2012). Second, we investigated associations between HCC and internalizing symptoms in parents and children. These analyses controlled for SES and parental perceptions of stress. Finally, given the large prior literature documenting socioeconomic disparities in risk for internalizing problems, we examined whether relations of SES to anxiety and depression in both parents and children were mediated by parental perceptions of stress and by parents’ or children’s own HCC, respectively. Given that perceptions of stress and physiological measures of stress are largely dissociable (e.g., Gunnar et al., 1981), we examined the independent roles of both parental perceptions of stress and HCC as mediating mechanisms.
2. Materials and Methods
2.1 Participants
We recruited a socioeconomically diverse sample of children and their parents through local street festivals, children’s events, and posting flyers in local neighborhoods in a large Northeastern U.S. city. Recruitment aimed to reach families from a range of socioeconomic backgrounds. More specifically, we aimed to enroll roughly equal numbers of mothers with high school, some college, college, and post-graduate education.
2.2 Procedure
During a lab visit, parents and their children first provided informed consent. Parents completed questionnaires, including measures of perceived stress and self-report measures of their own internalizing symptoms. Hair samples were collected from parents (n = 35) and children (n = 28) in order to assess cortisol accumulation in hair. Hair samples were not collected in instances when hair was too short or the participant did not agree to provide a sample. None of the parents were from the same household. Measures of child internalizing symptoms (n = 22 of the 28 children who provided hair samples) were collected during a follow-up phone call with parents, which on average, occurred 2 years after the initial visit. All procedures were approved by the Institutional Review Board at the New York State Psychiatric Institute.
2.3 Measures
2.3.1 Socioeconomic Status (SES)
Parental education
Parents reported the number of years of education completed by each parent in the household. Parental education level was averaged if there were two parents in the household to compute an average parental education measure.
Family income
Parents reported their annual household income and the number of people living in the household. Income-to-needs ratio (ITN) was calculated by dividing household income by the poverty threshold for the size of the family. Family income-to-needs ratio was used in all analyses and was Winsorized and log transformed to correct for a skewed distribution.
2.3.2 Hair Cortisol
A research staff member cut a small section of hair proximal to the posterior vertex of the participant’s scalp. Each hair sample weighed at least 15mg and was approximately 3cm long, thereby containing cortisol deposited during roughly the past 3 months. Samples were stored at −20ºC until all data collection was complete, after which they were sent to the University of Massachusetts for analysis. Samples were processed and analyzed using methods previously validated and described in detail (Davenport, et al., 2006; Meyer, et al., 2014). Briefly, each sample was weighed, washed twice in isopropanol to remove external contaminants, ground to a fine powder, and extracted with methanol. The methanol extract was evaporated, redissolved in assay buffer, and analyzed in duplicate along with standards and quality controls by a sensitive and specific enzyme-linked immunosorbent assay (Salimetrics, Carlsbad, CA). Assay readout was converted to pg cortisol per mg dry hair weight. Intra- and inter-assay coefficients of variation for this assay are <10%.
2.3.3 Parental Perceived Stress
Parents completed the Perceived Stress Scale (PSS) (Cohen et al., 1983), the Material Deprivation Scale, and the Life Experiences Survey (Sarason et al., 1978). The PSS is a 14-item scale that asked parents about their feelings and thoughts about their stress and ability to control their stress during the last month. For each item, they were asked to mark how often they felt or thought a certain way on a 5-point scale ranging from 0 (never) to 4 (very often). Items were reverse coded when appropriate and then summed to create a total score (α = .835).
In the Material Deprivation Scale, parents were asked a series of 14 questions based on five possible hardships in bills, utilities, food, medicine, homelessness, and housing instability. Parents were asked if they experienced hardships in these areas within the past 12 months, and provided a dichotomous answer (yes or no). All affirmative answers were recorded and summed to create a total score (α = .767).
In the Life Experiences Survey (LES; Sarason et al., 1978), parents were asked about 44 life events that may have occurred in the past year. For each event that occurred, parents rated the impact of the event on a 7-point scale ranging from -3 (extremely negative impact) to +3 (extremely positive impact). Scores from events rated as negative were summed to create a total negative life events impact score. The LES negative events scale has demonstrated good test-retest reliability (Sarason et al., 1978).
The Life Events negative impact score was positively correlated with both the material deprivation score (r = .434, p = .009) and the perceived stress scale score (r = .497, p = .002). The correlation between material deprivation and the perceived stress scale scores was also moderate and positive, although it did not reach significance (r = .261, p = .129). To reduce measurement error and increase power, we created a composite measure of parental perceptions of stress by standardizing and averaging the perceived stress scale score, LES negative impact score, and the material deprivation score.
2.3.4 Parental Internalizing Symptoms
Depression
Parental depressive symptoms were measured using the 9-item Patient Health Questionnaire (PHQ-9; Kroenke et al., 2001). The PHQ-9 is a self-report measure of depression based on the Diagnostic and Statistical Manual (DSM) criteria for major depressive disorder (MDD). Participants are asked to indicate how often in the past 2 weeks they have been bothered by depressive symptoms using a 4-point scale ranging from 0 (not at all) to 3 (nearly every day). Participant responses are then summed to create a total score, with higher total scores indicating greater depressive symptoms (α = .836). The PHQ-9 has well-established internal consistency, test-retest reliability, and validity (Kroenke et al., 2001; Lee et al., 2007) .
Anxiety
Parental anxiety symptoms were measured using the Beck Anxiety Inventory (BAI; Beck and Steer, 1990). The BAI is a 21-item self-report measure of physiological and cognitive anxiety symptoms. Participants are asked to indicate how often in the past week they were bothered by anxiety symptoms using a 4-point scale ranging from 0 (not at all) to 3 (severely/could barely stand it). Participant responses are then summed to create a total score with higher scores indicating greater anxiety symptoms (α = .912). The BAI has strong internal consistency, test-retest reliability, and concurrent validity (Beck and Steer, 1991).
2.3.5 Child Internalizing Symptoms
The Revised Child Anxiety and Depression Scale – Parent Version (RCADS-P; Chorpita et al., 2005) is a 47-item parent-report measure of child anxiety and depression. It has been used for children aged 6–18 years. Parents are asked to rate items on a scale ranging from 0 (never) to 3 (always). The RCADS-P has been found to have adequate internal consistency and validity (Ebesutani et al., 2015). Child anxiety symptoms were measured using the anxiety total score (α = .915) and child depression symptoms were measured using the depression subscale (α = .564).
The Child Behavior Problems Index (BPI; Peterson and Zill, 1986) is a 30-item parent-report scale measuring internalizing and externalizing symptoms in children aged 4–17 years. It has been used in large national studies such as the National Longitudinal Survey of Youth and the Panel Study of Income Dynamics. Child behaviors are rated using a 3-point scale ranging from 1 (not true) to 3 (very often true). Internalizing symptoms were measured by summing scores on 13 items pertaining to internalizing symptoms (α = .865) as was done in the Panel Study of Income Dynamics (The Child Development Supplement to the Panel Study of Income Dynamics User Guide: Release 1997).
Thus, child measures of internalizing symptoms included separate measures of child anxiety and depressive symptoms as well as an overall measure of internalizing symptoms.
2.4 Analysis Plan
Associations between SES and HCC
We first used regression analysis to examine whether parental education and family income were related to parental HCC. Next, we used regression analysis to examine whether parental education and family income were associated with children’s HCC, after controlling for parents’ HCC.
Associations between HCC and internalizing symptoms
We then used regression analysis to investigate whether HCC in parents and children were independently associated with internalizing symptoms in parents and children, respectively, after controlling for socioeconomic indicators and parental perceptions of stress.
Mediation models: SES, HCC, and internalizing symptoms
Finally, we examined whether SES disparities in internalizing symptoms were mediated by HCC and parental perceptions of stress. The INDIRECT macro was used to generate bias corrected confidence intervals from bootstrap mediation models (Preacher and Hayes, 2008).
All analyses controlled for either parent or child age, sex, and race as appropriate. Our current analyses were limited to the 35 parents and 28 children for whom parent or child HCC data were available. Analyses including both child and parent HCC were restricted to a subsample of 26 parent-child dyads for whom these data are available. Given these small sample sizes, power was sufficient to detect effects in the medium to large range. Analyses of child internalizing symptoms were restricted to the subset of 22 children for whom these data were available. Analyses were conducted with SPSS Statistics Version 22.
3. Results
3.1 Descriptive Statistics
Consistent with our sampling plan, parental education ranged from 6.5 – 20 years (M = 14.4, SD = 3). Family income-to-needs ratio, defined as family income divided by the federal poverty level for a family of that size, ranged from .32 to 14.08 (M = 2.91, SD = 2.73), which included families below the poverty line as well as very high-income families. Parent and child demographic characteristics are present in Table 1.
Table 1.
Descriptive Statistics
| Parents (n = 35) | Number | Mean | S.D. | Range |
|---|---|---|---|---|
| Parent age (years) | 34.9 | 7.3 | (23 – 51) | |
| Sex (male =1 ) | 4 | |||
| African American, non-Hispanic/Latino | 8 | |||
| Hispanic/Latino | 19 | |||
| White, non-Hispanic/Latino | 7 | |||
| Other | 1 | |||
| Family income-to-needs ratio | 2.91 | 2.73 | (.32–14.08) | |
| Parental education (years) | 14.44 | 3.00 | (6.5–20) | |
| Parent HCC (pg/mg) | 14.69 | 9.14 | (2.7–38.5) | |
|
| ||||
| Children (n = 28) | Number | Mean | S.D. | Range |
| Child age (months) | 76.2 | 9.0 | (60–90) | |
| Sex (male =1 ) | 6 | |||
| African American, non-Hispanic/Latino | 4 | |||
| Hispanic/Latino | 15 | |||
| White, non-Hispanic/Latino | 7 | |||
| Other | 2 | |||
| Family income-to-needs ratio | 3.28 | 2.91 | (.45–14.08) | |
| Parental education (years) | 15.20 | 2.50 | (11.5–20) | |
| Child HCC (pg/mg) | 23.35 | 11.88 | (7.9 – 58.9) | |
Note. HCC, hair cortisol concentration
3.2 Associations between SES and HCC
Parents
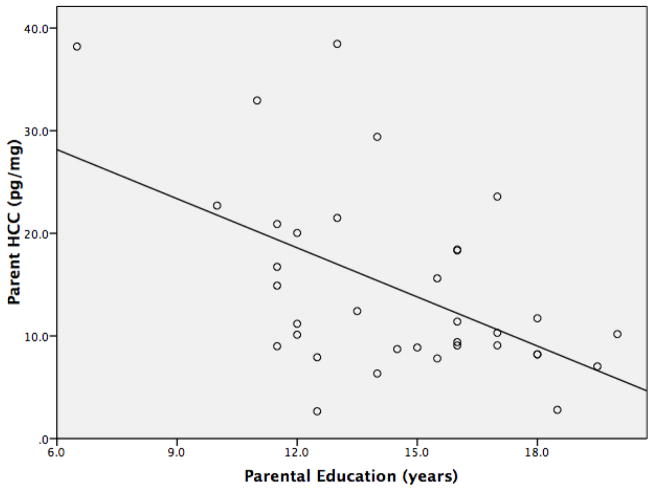
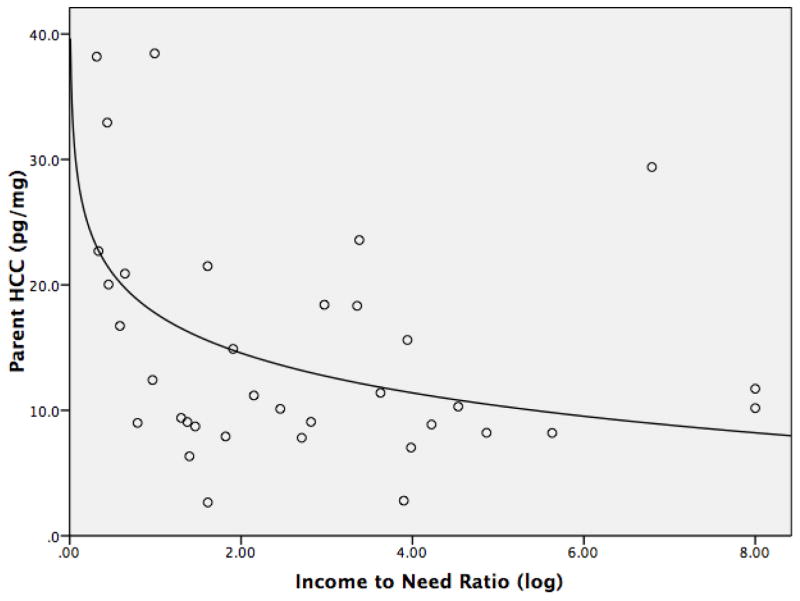
Lower parental education was linearly associated with higher parent HCC (β = −.602, p = .004) (Figure 1). Lower family income-to-needs ratio was associated with higher parental HCC. Here, the logarithmic function was the best fit for the data (β = −.445, p = .025), suggesting that the greatest differences in cortisol were seen at the lowest income levels (Figure 2). Parent age, sex, and race were unrelated to HCC in both of the models.
Figure 1.
Parental education is inversely linearly associated with parents’ hair cortisol concentration (HCC). Figure depicts unadjusted bivariate association.
Figure 2.
Parental income is logarithmically associated with parents’ hair cortisol concentration (HCC). Figure depicts unadjusted bivariate association.
Children
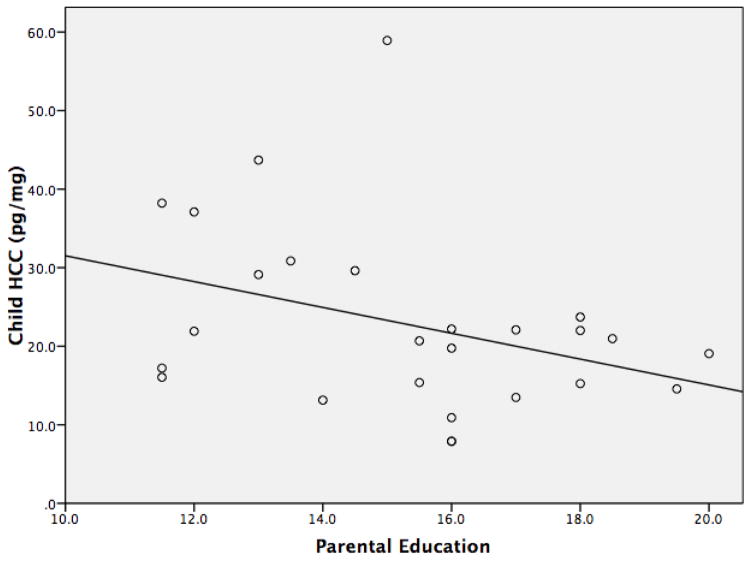
Lower parental education was linearly associated with higher child HCC (β = −.675, p = .009) when controlling for parent HCC and child characteristics (Figure 3). Family income was not significantly related to child HCC in either a linear or logarithmic pattern. Being Hispanic/Latino was also associated with lower child HCC (β = −.551, p = .05). Child age, sex, and parent HCC were unrelated to child HCC.
Figure 3.
Parental education is inversely linearly associated with children’s hair cortisol concentration (HCC). Figure depicts unadjusted bivariate association.
3.3 Associations between HCC and Internalizing Symptoms
Parents
We next examined whether parental HCC was independently associated with parent internalizing symptoms after controlling for socioeconomic factors and parental perceived stress. As shown in Table 2 (Model A), higher parental HCC (β = .25, p = .047) was associated with higher parental anxiety symptoms, independent of family income and parental perceptions of stress. Higher parental perceived stress was associated with higher parental anxiety symptoms (β = .586, p < .001). The same pattern of results was found when parental education was substituted for family income.
Table 2.
Associations of SES and stress with parent anxiety and depression.
| Parent Anxiety | Model A | ||
|---|---|---|---|
| Beta | t | p-value | |
| Income-to-Needs Ratio | −0.219 | −1.482 | .150 |
| Age | −0.125 | −0.873 | .390 |
| Sex | −0.147 | −1.218 | .234 |
| African American | −0.206 | −1.357 | .186 |
| Hispanic/Latino | −0.548 | −3.170 | .004 |
| HCC | 0.250 | 2.079 | .047 |
| Perceptions of Stress | 0.586 | 4.523 | < .001 |
|
| |||
| Parent Depression | Model B | ||
| Beta | t | p-value | |
| Income-to-Needs Ratio | −0.271 | −1.652 | .110 |
| Age | −0.309 | −1.947 | .062 |
| Sex | −0.137 | −1.025 | .314 |
| African American | −0.052 | −0.307 | .761 |
| Hispanic/Latino | −0.563 | −2.934 | .007 |
| HCC | 0.109 | 0.813 | .423 |
| Perceptions of Stress | 0.514 | 3.570 | .001 |
Note. HCC, hair cortisol concentration
As shown in Table 2 (Model B), parental HCC (β = .109, p = .423) was not significantly associated with parental depression symptoms after accounting for family income and parental perceptions of stress. Parental perceived stress was associated with higher parental depressive symptoms (β = .514, p = .001). The same pattern of results was found when parental education was substituted for family income.
Children
We then examined whether child HCC was independently associated with internalizing symptoms after controlling for socioeconomic factors and parental perceived stress. As shown in Table 3, child HCC was not significantly associated with any measure of children’s internalizing symptoms. Higher parental perceptions of stress were associated with higher internalizing symptoms in children as measured by the BPI (β = .485, p = .035) when income was used as the measure of SES (Model C). The same pattern of results was found when parental education was substituted for family income.
Table 3.
Associations of SES and stress with child internalizing symptoms.
| BPI Internalizing | Model C | ||
|---|---|---|---|
| Beta | t | p-value | |
| Income-to-Needs Ratio | −0.153 | −0.695 | .499 |
| Age | 0.252 | 1.108 | .286 |
| Sex | 0.617 | 2.796 | .014 |
| African American | −0.345 | −1.284 | .220 |
| Hispanic/Latino | −0.847 | −3.329 | .005 |
| Child HCC | −0.243 | −1.252 | .231 |
| Parental Perceptions of Stress | 0.485 | 2.341 | .035 |
|
| |||
| RCADS Anxiety | Model D | ||
| Beta | t | p-value | |
| Income-to-Needs Ratio | −0.249 | −1.067 | .304 |
| Age | 0.364 | 1.509 | .154 |
| Sex | 0.350 | 1.498 | .156 |
| African American | −0.512 | −1.797 | .094 |
| Hispanic/Latino | −0.587 | −2.180 | .047 |
| Child HCC | −0.280 | −1.361 | .195 |
| Parental Perceptions of Stress | 0.478 | 2.178 | .047 |
|
| |||
| RCADS Depression | Model E | ||
| Beta | t | p-value | |
| Income-to-Needs Ratio | −0.035 | −0.140 | .891 |
| Age | −0.153 | −0.599 | .559 |
| Sex | 0.582 | 2.351 | .034 |
| African American | 0.053 | 0.175 | .863 |
| Hispanic/Latino | −0.613 | −2.150 | .050 |
| Child HCC | 0.049 | 0.226 | .824 |
| Parental Perceptions of Stress | 0.515 | 2.215 | .044 |
Note. HCC, hair cortisol concentration; BPI, Behavior Problems Index; RCADS, Revised Child Anxiety and Depression Scale.
As shown in Table 3, higher parental perceptions of stress were associated with higher levels of child anxiety symptoms as measured by the RCADS (β = .478, p = .047) when family income was used as the measure of SES (Model D), but this relation was only marginally significant when parental education was used as the measure of SES.
As shown in Table 3, higher parental perceptions of stress were associated with higher levels of child depression symptoms as measured by the RCADS (β = .515, p = .044) when family income was used as the measure of SES (Model E), but this relation was only marginally significant when parental education was used as the measure of SES.
3.4 HCC and Parental Perceptions of Stress as Mediators of Socioeconomic Differences in Internalizing Symptoms
Preliminary analysis indicated that parental HCC and parental perceptions of stress were not significantly related to each other (r = .274, p = .112).
Parents
Family income to needs ratio (β = −.613, p = .001; β = −.567, p = .001) and parental education (β = −.574, p = .005; β = −.542, p = .006) were both significantly inversely associated with parental anxiety and depressive symptoms, respectively (even after controlling for parent age, sex, and race), raising questions about potential mediating factors. We used bootstrap mediation models to examine whether parental perceptions of stress and parental HCC mediated relations of family income and parental education to parental internalizing symptoms.
The association of family income with parent anxiety was significantly mediated by parental perceptions of stress (95% CI: [−7.199, −.958]) and marginally mediated by parent HCC (90% CI: [−4.126, −.051]).
The association of parental education with parent anxiety was significantly mediated by parental perceptions of stress 95% CI: [−2.832, −.307] and marginally mediated by parent HCC 90% CI: [−1.537, −.024].
The association of family income with parent depression was significantly mediated by parental perceptions of stress 95% CI: [−3.251, −.251] but not by parent HCC.
The association of parental education with parent depression was significantly mediated by parental perceptions of stress 95% CI: [−1.261, −0.098] but not by parent HCC.
Children
In regression models, family income and parental education were unrelated to internalizing symptoms. There were no significant indirect effects of family income or parental education on any measure of child internalizing symptoms through parental perceived stress or child HCC.
4. Discussion
This is the first study to examine socioeconomic differences in HCC of children and their parents and to examine the ways in which HCC and parental perceptions of stress may mediate relations between SES and internalizing symptoms in both parents and children. Our results indicated that lower parental education and lower family income were related to higher HCC among parents. Interestingly, the relation between family income and parental HCC was logarithmic such that differences in HCC were more pronounced among those at the lower end of the income distribution. This finding is consistent with a large body of research indicating that incremental differences in income have the largest effects at the lowest income levels (Duncan and Magnuson, 2003; Noble et al., 2015).
Additionally, we found that lower parental education was related to higher HCC in children, which is consistent with two prior studies (Vaghri et al., 2013; Vliegenthart et al., 2016), but contrasts with three studies reporting null relations (Groeneveld et al., 2013; Karlen et al., 2013; Liu et al., 2016). These three studies, however, had restricted ranges of parental education, which may have made it more difficult to detect an effect. Importantly, the relation of parental education to child HCC was robust to controlling for parental HCC. Although prior work has suggested that HCC may be heritable (Karlen et al., 2013), no studies to date have controlled for parent hair cortisol when examining SES differences in children’s HCC. By controlling for parent HCC, our results suggest that parental education may have unique effects on children’s cortisol that are independent of familial heritable differences in stress physiology. Interestingly, family income was not associated with child HCC, consistent with prior work (Vaghri et al., 2013).
We did not hypothesize a priori that only parental education, and not family income, would predict children’s HCC. One possible explanation for this finding comes from a large literature suggesting that parental education may be particularly associated with the quality of parenting that children experience, whereas family income may be more highly associated with children’s experience of material resources (Duncan and Magnuson, 2003). It is thus possible that characteristics of parenting, such as warmth and harshness, affect children’s stress physiology more directly than access to material goods. For parents, on the other hand, it is possible that both low income and low education may lead to increased stress as parents are faced with the tasks of paying for food, housing, utilities, and other daily expenses as well as with the tasks of organizing and managing their families’ lives. Future work would benefit from including more specific measures of parenting and parenting related stress, such as the Parenting Stress Index (Abidin, 1995), in order to examine these pathways in more detail.
After having established relations between SES factors and both parental and child HCC, we were next interested in extending these findings to examine the role that HCC might play in socioeconomic disparities in anxiety and depression. Among parents, higher education and higher family income were both associated with lower anxiety and lower depressive symptoms, consistent with a large body of work demonstrating SES disparities in internalizing symptoms (Alegria et al., 2000; Callan et al., 2015; Hudson, 2005; Lorant et al., 2003). After controlling for family income or education, both higher parental perceptions of stress and parent HCC were significantly related to anxiety symptoms. Only parental perceptions of stress were related to depressive symptoms. This is consistent with two prior studies, which found no relations of HCC to depression diagnosis or symptoms (Dowlati et al., 2010; Ouellette et al., 2015). In the present study, the magnitudes of the effects of HCC were moderately large, and the magnitudes of the effects of parental perceptions of stress were large with a one standard deviation difference in parental perceived stress accounting for over half (.514 – .657) of a standard deviation difference in anxiety or depressive symptoms. These findings add to an emerging body of literature examining relations of HCC to internalizing problems in adults. More broadly, the findings illustrate the importance of considering both physiological and psychosocial aspects of stress, as both of these components were significantly associated with parental anxiety symptoms. Moreover, the finding that these two components were unrelated to each other further highlights the importance of considering both physiological and psychosocial aspects. We did not hypothesize that the psychosocial measure of stress would be more strongly related to anxiety symptoms than would HCC, but it is possible that the strength of this association is in part driven by the fact that both of these measures were assessed through the same method (i.e., parent self-report).
Our formal tests of mediation demonstrated that parental perceptions of stress significantly mediated associations of family income and parental education to both parental depressive and anxiety symptoms. This finding is consistent with a broader body of work, which has suggested that the SES disparities in health are in part explained by greater exposure to stressors (Evans and Kim, 2010; Evans and Cassells, 2014; Matthews et al., 2010). We hypothesized that physiological stress as measured by HCC would also play a role in explaining the SES disparities in anxiety and depression. However, HCC only marginally mediated relations of family income and parental education to parent anxiety, and did not play a role in parent depression. This marginally significant result suggests that examining this pathway in a larger sample may be a productive direction for future research.
For children, we found some evidence that parental perceived stress was related to internalizing symptoms, which was consistent with our adult findings. It is possible that events and circumstances perceived as stressful by parents are also perceived by their children to be stressful. Alternatively, or in conjunction, parental perceived stress may be transmitted to children through differences in parenting behaviors or other facets of the home environment. In contrast to our findings for parents, however, we did not find any associations between SES or HCC and internalizing symptoms. The lag in time between the measurement of HCC and the measurement of internalizing symptoms, however, may have played a role in this null result. Unfortunately, measures of children’s internalizing symptoms concurrent to HCC measurement were not available. Given evidence linking early experiences of stress with psychopathology in adolescence (Grant et al., 2004), it is highly possible that early chronic stress as measured by HCC could be related to later internalizing symptoms. However, the very small sample for this analysis made it impossible to detect all but large effects. Moreover, it may be that internalizing symptoms associated with early life stress would not appear until children approach adolescence. Future work examining concurrent measures of HCC and internalizing symptoms will help to clarify some of these possibilities.
Finally, although not hypothesized a priori, we found that Hispanic/Latino ethnicity was associated with lower depressive and anxious symptoms among adults and children and with lower HCC in children. This finding is consistent with epidemiological work demonstrating a lower lifetime prevalence of anxiety and depressive disorders among Latinos as compared to non-Latino whites (Alegria et al., 2008). This body of work, however, has also shown that prevalence of these disorders differs by sub-ethnicity and immigrant status, which are two factors that should be considered in future work aiming to clarify the effects of Hispanic ethnicity on HCC and internalizing symptoms.
4.1 Limitations
Overall, the study was limited by its relatively small sample size. The purposeful recruitment of participants from diverse SES backgrounds, however, likely strengthened the ability to detect significant associations between SES factors and HCC, despite the small number of participants. Additionally, the analyses of internalizing symptoms in children were particularly limited by an even smaller sample size than the other analyses and by an average lag in time of two years between the time when SES and hair cortisol were measured and when internalizing symptoms were assessed. As such, these analyses should be viewed as exploratory. Given the positive findings in adults, future work should continue to examine these associations in larger samples of children where the measurement of physiological and perceived stress are contemporaneous with the measurement of children’s internalizing symptoms. Moreover, including child report of internalizing symptoms (for children 8 years of age and older) could be a productive direction for future work.
4.2 Conclusions
This study demonstrates important links between family SES and HCC in both parents and children. Importantly, it is the first study to show that the association between SES and child HCC is independent of parent HCC. Moreover, this is the first study to examine HCC as a mediator of SES disparities in internalizing symptoms. Our finding that HCC and parental perceived stress were independently associated with parents’ internalizing symptoms suggests that it is important to simultaneously consider multiple aspects of stress in order to understand the emergence of internalizing symptoms.
Highlights.
Parents with lower family incomes had higher hair cortisol concentration (HCC)
Relation between HCC and income was strongest among the most disadvantaged parents
Lower parental education was associated with higher HCC in parents and children
Perceived stress mediated socioeconomic disparities in parents’ anxiety symptoms
HCC marginally mediated socioeconomic disparities in parents’ anxiety symptoms
Acknowledgments
Funding: Alexandra Ursache’s role in this work was supported by the National Institutes of Health [NIH/NINDS T32-NS07153]. In addition, a National Institute of Mental Health training grant supported Emily Merz [NIH/NIMH T32MH13043]. We also gratefully acknowledge funding from the GH Sergievsky Center, the Irving Institute for Clinical and Translational Research and Teachers College, Columbia University
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abidin RR. Parenting Stress Index (PSI) Charlottesville, VA: Pediatric Psychology Press; 1990. [Google Scholar]
- Adler NE, Snibbe AC. The role of psychosocial processes in explaining the gradient between socioeconomic status and health. Current Directions in Psychological Science. 2003;12:119–123. [Google Scholar]
- Alegria M, Bijl RV, Lin E, Walters EE, Kessler RC. Income differences in persons seeking outpatient treatment for mental disorders: a comparison of the United States with Ontario and The Netherlands. Arch Gen Psychiatry. 2000;57:383–391. doi: 10.1001/archpsyc.57.4.383. [DOI] [PubMed] [Google Scholar]
- Alegría M, Canino G, Shrout PE, Woo M, Duan N, Vila D, … Meng XL. Prevalence of mental illness in immigrant and non-immigrant US Latino groups. Am J Psychiatry. 2008;165:359–369. doi: 10.1176/appi.ajp.2007.07040704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Steer RA. Manual for the Beck anxiety inventory. San Antonio, TX: Psychological Corporation; 1990. [Google Scholar]
- Beck AT, Steer RA. Relationship between the Beck anxiety inventory and the Hamilton anxiety rating scale with anxious outpatients. J Anxiety Disord. 1991;5:213–223. [Google Scholar]
- Bradley RH, Corwyn RF. Socioeconomic status and child development. Annu Rev Psychol. 2002;53:371–399. doi: 10.1146/annurev.psych.53.100901.135233. [DOI] [PubMed] [Google Scholar]
- Callan MJ, Kim H, Matthews WJ. Predicting self-rated mental and physical health: The contributions of subjective socioeconomic status and personal relative deprivation. Frontiers in psychology. 2015:6. doi: 10.3389/fpsyg.2015.01415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Z, Li J, Zhang J, Xing X, Gao W, Lu Z, Deng H. Simultaneous determination of hair cortisol, cortisone and DHEAS with liquid chromatography–electrospray ionization-tandem mass spectrometry in negative mode. Journal of Chromatography B. 2013;929:187–194. doi: 10.1016/j.jchromb.2013.04.026. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Moffitt CE, Gray J. Psychometric properties of the Revised Child Anxiety and Depression Scale in a clinical sample. Behav Res Ther. 2005;43:309–322. doi: 10.1016/j.brat.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- Combs-Orme T, Cain DS. Poverty and the daily lives of infants. Journal of Children & Poverty. 2006;12:1–20. [Google Scholar]
- Davenport MD, Tiefenbacher S, Lutz CK, Novak MA, Meyer JS. Analysis of endogenous cortisol concentrations in the hair of rhesus monkeys. General and Comparative Endocrinology. 2006;147:255–261. doi: 10.1016/j.ygcen.2006.01.005. [DOI] [PubMed] [Google Scholar]
- Dettenborn L, Muhtz C, Skoluda N, Stalder T, Steudte S, Hinkelmann K, Kirschbaum C, Otte C. Introducing a novel method to assess cumulative steroid concentrations: increased hair cortisol concentrations over 6 months in medicated patients with depression. Stress. 2012;15:348–353. doi: 10.3109/10253890.2011.619239. [DOI] [PubMed] [Google Scholar]
- Dowd JB, Simanek AM, Aiello AE. Socio-economic status, cortisol and allostatic load: a review of the literature. Int J Epidemiol. 2009;38:1297–1309. doi: 10.1093/ije/dyp277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowlati Y, Herrmann N, Swardfager W, Thomson S, Oh PI, Van Uum S, Koren G, Lanctot KL. Relationship between hair cortisol concentrations and depressive symptoms in patients with coronary artery disease. Neuropsychiatr Dis Treat. 2010;6:e400. [PMC free article] [PubMed] [Google Scholar]
- Duncan GJ, Magnuson KA. Off with Hollingshead: Socioeconomic resources, parenting, and child development. Socioeconomic status, parenting, and child development. 2003:83–106. [Google Scholar]
- Duncan GJ, Magnuson K. Socioeconomic status and cognitive functioning: moving from correlation to causation. Wiley Interdisciplinary Reviews: Cognitive Science. 2012;3:377–386. doi: 10.1002/wcs.1176. [DOI] [PubMed] [Google Scholar]
- Ebesutani C, Tottenham N, Chorpita B. The Revised Child Anxiety and Depression Scale-Parent version: Extended applicability and validity for use with younger youth and children with histories of early-life caregiver neglect. Journal of Psychopathology and Behavioral Assessment. 2015;37:705–718. doi: 10.1007/s10862-015-9494-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans GW, Gonnella C, Marcynyszyn LA, Gentile L, Salpekar N. The role of chaos in poverty and children's socioemotional adjustment. Psychological Science. 2005;16:560–565. doi: 10.1111/j.0956-7976.2005.01575.x. [DOI] [PubMed] [Google Scholar]
- Evans GW, Kim P. Multiple risk exposure as a potential explanatory mechanism for the socioeconomic status–health gradient. Ann N Y Acad Sci. 2010;1186:174–189. doi: 10.1111/j.1749-6632.2009.05336.x. [DOI] [PubMed] [Google Scholar]
- Evans GW, Cassells RC. Childhood poverty, cumulative risk exposure, and mental health in emerging adults. Clinical Psychological Science. 2014;2:287–296. doi: 10.1177/2167702613501496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groeneveld MG, Vermeer HJ, Linting M, Noppe G, van Rossum EF, van IJzendoorn MH. Children’s hair cortisol as a biomarker of stress at school entry. Stress. 2013;16:711–715. doi: 10.3109/10253890.2013.817553. [DOI] [PubMed] [Google Scholar]
- Gunnar MR, Fisch RO, Korsvik S, Donhowe JM. The effects of circumcision on serum cortisol and behavior. Psychoneuroendocrinology. 1981;6:269–275. doi: 10.1016/0306-4530(81)90037-8. [DOI] [PubMed] [Google Scholar]
- Hanson JL, Chandra A, Wolfe BL, Pollak SD. Association between income and the hippocampus. PloS one. 2011;6:e18712. doi: 10.1371/journal.pone.0018712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson CG. Socioeconomic status and mental illness: tests of the social causation and selection hypotheses. Am J Orthopsychiatry. 2005;75:3. doi: 10.1037/0002-9432.75.1.3. [DOI] [PubMed] [Google Scholar]
- Karlen J, Frostell A, Theodorsson E, Faresjo T, Ludvigsson J. Maternal influence on child HPA axis: a prospective study of cortisol levels in hair. Pediatrics. 2013;132:e1333–40. doi: 10.1542/peds.2013-1178. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The Phq-9. Journal of general internal medicine. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee PW, Schulberg HC, Raue PJ, Kroenke K. Concordance between the PHQ-9 and the HSCL-20 in depressed primary care patients. J Affect Disord. 2007;99:139–145. doi: 10.1016/j.jad.2006.09.002. [DOI] [PubMed] [Google Scholar]
- Liu CH, Snidman N, Leonard A, Meyer J, Tronick E. Intra-individual stability and developmental change in hair cortisol among postpartum mothers and infants: Implications for understanding chronic stress. Dev Psychobiol. 2016;58:509–518. doi: 10.1002/dev.21394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorant V, Deliege D, Eaton W, Robert A, Philippot P, Ansseau M. Socioeconomic inequalities in depression: a meta-analysis. Am J Epidemiol. 2003;157:98–112. doi: 10.1093/aje/kwf182. [DOI] [PubMed] [Google Scholar]
- Matthews KA, Gallo LC, Taylor SE. Are psychosocial factors mediators of socioeconomic status and health connections? Ann N Y Acad Sci. 2010;1186:146–173. doi: 10.1111/j.1749-6632.2009.05332.x. [DOI] [PubMed] [Google Scholar]
- McLaughlin KA, Breslau J, Green JG, Lakoma MD, Sampson NA, Zaslavsky AM, Kessler RC. Childhood socio-economic status and the onset, persistence, and severity of DSM-IV mental disorders in a US national sample. Soc Sci Med. 2011;73:1088–1096. doi: 10.1016/j.socscimed.2011.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer J, Novak M, Hamel A, Rosenberg K. Extraction and analysis of cortisol from human and monkey hair. Journal of Visualized Experiments. 2014;83:e50882. doi: 10.3791/50882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murali V, Oyebode F. Poverty, social inequality and mental health. Advances in psychiatric treatment. 2004;10:216–224. [Google Scholar]
- Noble KG, Houston SM, Brito NH, Bartsch H, Kan E, Kuperman JM, Akshoomoff N, Amaral DG, Bloss CS, Libiger O. Family income, parental education and brain structure in children and adolescents. Nat Neurosci. 2015;18:773–778. doi: 10.1038/nn.3983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noble KG, Houston SM, Kan E, Sowell ER. Neural correlates of socioeconomic status in the developing human brain. Developmental Science. 2012;15:516–527. doi: 10.1111/j.1467-7687.2012.01147.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouellette SJ, Russell E, Kryski KR, Sheikh HI, Singh SM, Koren G, Hayden EP. Hair cortisol concentrations in higher-and lower-stress mother–daughter dyads: A pilot study of associations and moderators. Dev Psychobiol. 2015;57:519–534. doi: 10.1002/dev.21302. [DOI] [PubMed] [Google Scholar]
- Palmer FB, Anand KJ, Graff JC, Murphy LE, Qu Y, Völgyi E, Rovnaghi CR, Moore A, Tran QT, Tylavsky FA. Early adversity, socioemotional development, and stress in urban 1-year-old children. J Pediatr. 2013;163:1733–1739. doi: 10.1016/j.jpeds.2013.08.030. [DOI] [PubMed] [Google Scholar]
- Peterson JL, Zill N. Marital disruption, parent-child relationships, and behavior problems in children. Journal of Marriage and the Family. 1986;48:295–307. [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Reiss F. Socioeconomic inequalities and mental health problems in children and adolescents: a systematic review. Soc Sci Med. 2013;90:24–31. doi: 10.1016/j.socscimed.2013.04.026. [DOI] [PubMed] [Google Scholar]
- Rippe RC, Noppe G, Windhorst DA, Tiemeier H, van Rossum EF, Jaddoe VW, Verhulst FC, Bakermans-Kranenburg MJ, van IJzendoorn MH, van den Akker, Erica LT. Splitting hair for cortisol? Associations of socio-economic status, ethnicity, hair color, gender and other child characteristics with hair cortisol and cortisone. Psychoneuroendocrinology. 2016;66:56–64. doi: 10.1016/j.psyneuen.2015.12.016. [DOI] [PubMed] [Google Scholar]
- Russell E, Koren G, Rieder M, Van Uum S. Hair cortisol as a biological marker of chronic stress: current status, future directions and unanswered questions. Psychoneuroendocrinology. 2012;37:589–601. doi: 10.1016/j.psyneuen.2011.09.009. [DOI] [PubMed] [Google Scholar]
- Sarason IG, Johnson JH, Siegel JM. Assessing the impact of life changes: development of the Life Experiences Survey. J Consult Clin Psychol. 1978;46:932. doi: 10.1037//0022-006x.46.5.932. [DOI] [PubMed] [Google Scholar]
- Serwinski B, Salavecz G, Kirschbaum C, Steptoe A. Associations between hair cortisol concentration, income, income dynamics and status incongruity in healthy middle-aged women. Psychoneuroendocrinology. 2016;67:182–188. doi: 10.1016/j.psyneuen.2016.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slopen N, Fitzmaurice G, Williams DR, Gilman SE. Poverty, food insecurity, and the behavior for childhood internalizing and externalizing disorders. Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49:444–452. doi: 10.1097/00004583-201005000-00005. [DOI] [PubMed] [Google Scholar]
- Staufenbiel SM, Penninx BW, Spijker AT, Elzinga BM, van Rossum EF. Hair cortisol, stress exposure, and mental health in humans: a systematic review. Psychoneuroendocrinology. 2013;38:1220–1235. doi: 10.1016/j.psyneuen.2012.11.015. [DOI] [PubMed] [Google Scholar]
- Steudte S, Stalder T, Dettenborn L, Klumbies E, Foley P, Beesdo-Baum K, Kirschbaum C. Decreased hair cortisol concentrations in generalised anxiety disorder. Psychiatry Res. 2011;186:310–314. doi: 10.1016/j.psychres.2010.09.002. [DOI] [PubMed] [Google Scholar]
- Tracy M, Zimmerman FJ, Galea S, McCauley E, Vander Stoep A. What explains the relation between family poverty and childhood depressive symptoms? J Psychiatr Res. 2008;42:1163–1175. doi: 10.1016/j.jpsychires.2008.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaghri Z, Guhn M, Weinberg J, Grunau RE, Yu W, Hertzman C. Hair cortisol reflects socio-economic factors and hair zinc in preschoolers. Psychoneuroendocrinology. 2013;38:331–340. doi: 10.1016/j.psyneuen.2012.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vliegenthart J, Noppe G, van Rossum E, Koper J, Raat H, van den Akker E. Socioeconomic status in children is associated with hair cortisol levels as a biological measure of chronic stress. Psychoneuroendocrinology. 2016;65:9–14. doi: 10.1016/j.psyneuen.2015.11.022. [DOI] [PubMed] [Google Scholar]
- Wosu AC, Gelaye B, Valdimarsdóttir U, Kirschbaum C, Stalder T, Shields AE, Williams MA. Hair cortisol in relation to sociodemographic and lifestyle characteristics in a multiethnic US sample. Ann Epidemiol. 2015;25:90–95. doi: 10.1016/j.annepidem.2014.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]