Abstract
Here we utilized social media to compare the toxidrome of three lethal chemical exposures worldwide. YouTube videos were the main source from which the data were collected, but published reports and news were also utilized to fill in some gaps. All videos were organized in a database detailing symptoms and severity of each victim, along with demographics such as approximate age and gender. Each symptom was rated as mild, moderate, or severe and corresponding pie graphs for each incident were compared. The videos displayed symptoms ranging from mild to severe cholinergic toxicity and life‐threatening convulsions. Social media may represent an important resource in developing a viable approach to the early detection and identification of chemical exposure, reinforce our preparedness for better antidotes, long‐term follow up, and training about deadly chemical nerve agent attacks.
Study Highlights
WHAT IS THE CURRENT KNOWLEDGE ON THE TOPIC?
✓ Chemical attack is becoming a real threat worldwide. In 2013, two deadly chemical exposures occurred in different countries. There were deaths of 23 children in Bihar, India from accidental poisoning with the farm‐grade organophosphate (OP) pesticide monocrotophos, with many more hospitalized. In Syria, about 1,400 civilians died from the weapons‐grade nerve gas sarin attacks. Over a decade ago Tokyo civilians were exposed to the lab‐grade sarin gas on the subway.
WHAT QUESTION DID THIS STUDY ADDRESS?
✓ While exposure to OP pesticides and nerve agents can result in severe detriment on the victimized population, including death in many cases, there is limited information on human exposure, especially the neurotoxicity sequelae after acute poisoning and the long‐term constellation of signs and symptoms after initial exposure. This study utilized a social media tool to compare the toxidrome of three lethal chemical exposures worldwide and attempted to differentiate a pesticide exposure that has more muscarinic effects from nerve agent that predominates with nicotinic toxicity.
WHAT THIS STUDY ADDS TO OUR KNOWLEDGE
✓ Analysis of mass exposures is now feasible by using a novel tool—social media. Videos are available on the Internet that allows each incident to be observed, categorized, and archived in digital format. Analysis of the rare videos of three distinct OP poisoning incidents uncovered a set of clinical fingerprints that indicate a specific group of cholinergic toxicants as lethal threat agents for humans.
HOW THIS MIGHT CHANGE CLINICAL PHARMACOLOGY OR TRANSLATIONAL SCIENCE
✓ Comparative toxidrome data might help optimize early detection toward creating better antidote therapies for chemical poisonings, improve preparedness for chemical attacks, and display the need for long‐term medical follow‐up for victims of nerve agent attacks. Such toxidrome analysis may help developing a triage system for long‐term monitoring of victims in case of mass attacks.
Among 110 million chemicals in the CAS registry, nearly 345 thousands are toxic chemicals. Organophosphate (OP) pesticides, nerve agents, vesicants, and cyanide are extremely lethal chemical agents. Nerve gases like sarin are classified as weapons of mass destruction by the United Nations. Monocrotophos is used widely as a pesticide in some countries due to effectiveness and cheap access, but is banned in the United States.1 Nerve agents were discovered in the 1930s and have been used throughout history. During World War I, Germany attacked Allied troops with chlorine gas2; this was the first time a lethal chemical agent had been used on a large scale. During World War II and the Cold War era, many nations had stockpiles of chemical weapons, but they were used sparingly.2 Chemical weapons were reportedly used in the Iran–Iraq war (Figure 1). American troops operating in the Gulf War in 1991 were potentially exposed to sarin after an exposure to an Iraqi chemical dump.3 Since the 1980s, there have been few incidents of chemical warfare reported, until the Tokyo subway attack by a terrorist group in 1995. Then there was another gap until the events of accidental poisonings with pesticides in India and the Syrian attack in 2013. These three recent incidents are the focus of this pilot toxidrome study to document the signs, symptoms, and treatments of chemical OP poisoning.
Figure 1.
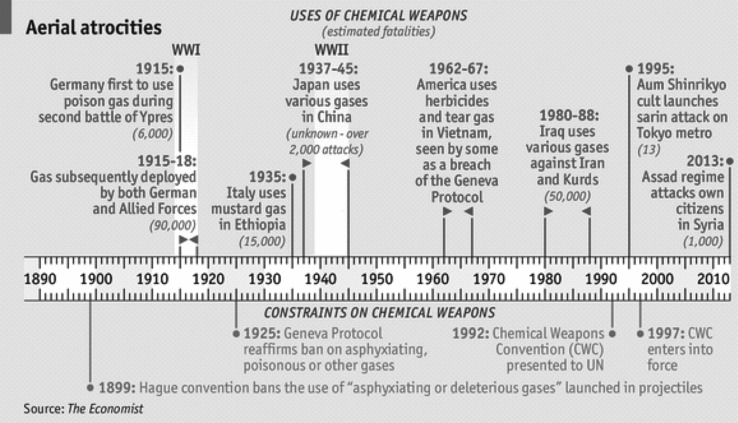
A timeline by The Economist visually lays out the history of chemical weapon use. Source: The shadow of Ypres: How a whole class of weaponry came to be seen as indecent (2013, August 31). The Economist. Retrieved July 22, 2014, from http://www.economist.com/news/briefing/21584397-how-whole-class-weaponry-came-be-seen-indecent-shadow-ypres
Nerve agents act by inhibiting the enzyme acetylcholinesterase (AChE), which is responsible for the breakdown of acetylcholine in the body. The irreversible inhibition of this enzyme by a nerve agent can cause cholinergic crisis and hyperstimulation by excess acetylcholine, eventually leading to death.4 Symptoms of OP poisoning include, but are not limited to: miosis, sustained muscle contraction, twitching, hypersalivation, excessive sweating, fainting, vomiting, respiratory depression, and seizures.4 Current antidotes available in the United States for OP poisoning are atropine, an antimuscarinic agent, and 2‐PAM (pralidoxime) which reactivates the AChE by competing with the nerve agent for the binding domain of the enzyme.5 Other oximes (obidoxime, HI‐6) are used elsewhere as antidotes for nerve agents. Atropine produces life‐saving effects by decreasing hypersecretions and relieving bronchoconstriction, which allows for more effective breathing of the exposed individual. The nicotinic effects of OPs, such as spasms and fasciculations, will not be improved by atropine.6 However, the use of oximes such as 2‐PAM has many limitations, including their poor entry into the brain. Thus, 2‐PAM has low permeability and only slowly reactivates brain AChE.7 Similarly, atropine has limited brain bioavailability and hence offers little protection against the devastating neurotoxicity, including lethal seizures.6 For a patient experiencing seizures, benzodiazepines such as diazepam or midazolam are recommended for controlling seizures and status epilepticus.5 Pyridostigmine bromide is currently available in the United States for military personnel at risk for a nerve agent exposure; it must be used prior to exposure and has no benefit if administered after exposure. The exposure to OP nerve agents, whether purposeful or accidental, results in severe detriment to the victimized population, including death in many cases. Chemical attacks are becoming a real threat worldwide.7 Analysis of mass exposures is now feasible by using a novel tool—social media. Videos are available on the Internet that allow each incident to be observed and categorized.4
In contrast to acute toxidrome data, there have been no long‐term follow‐up studies for either the Syrian or Indian cases. There have been a few studies published on long‐term follow‐up of the Tokyo victims but they were small, with limited scope. One study has identified posttraumatic stress disorder in the sarin‐exposed group.8 Another published study was a 3‐year follow‐up that included male firefighters and police officers who were exposed while rescuing victims.9 This study found a higher frequency of sister chromatid exchanges in the exposed subjects. The final study occurred 7 years after the attack and included 23 exposed subway workers. The study concluded that the exposed group had decreased psychomotor performance.10 These cases underscore the need for long‐term studies with a larger number of subjects to ascertain the chronic toxidrome of nerve agent exposure.
The aim of this pilot toxidrome study was to use YouTube videos to assess and identify distinct signs and symptoms of pesticide and nerve agent exposure, and help devise preparedness for better antidotes for chemical attacks. Analysis of the videos of three distinct OP poisoning incidents uncovers a set of clinical profiles that characterize three cholinergic toxicants that are extremely lethal chemical agents.
METHODS
We performed a search on the video‐sharing website YouTube (Google, Mountain View, CA; http://www.youtube.com) and other online news portals for videos available as of July 2014. In addition to video searches, comments and news items were searched for additional information regarding the victim and incident. Due to the public nature of the websites, the use of videos did not require approval. YouTube videos were collected for each of the three events (India, Syria, Tokyo), using key word searches on the Internet. Key words included: pesticide, nerve agent, organophosphate, sarin, chemical exposure, Syria, Tokyo, India, chemical exposure. The videos were downloaded and watched as described previously.1 Each video was assigned an identifier and information on each victim (estimated age, gender, and symptoms) was recorded in a spreadsheet. There were a total of 38 videos collected: 22 from Syria, 8 from Tokyo, and 8 from India. The lengths varied, as did symptoms, and the number of victims. Each victim from a particular video was treated as an independent sample.
The Indian case was covered widely in press and social media. On 16 July 2013, at least 23 students died and dozens more fell ill at a primary school in the village of Dharmashati Gandaman in the Saran district of the Indian state of Bihar after eating a midday meal contaminated with pesticide.1, 17, 18 Official investigations stated that the cooking oil had been placed in a container that was previously used to store insecticides. A forensic report confirmed the cooking oil contained "very toxic" levels of monocrotophos, an agricultural OP pesticide. The amount consumed was not estimated, but victims had approximately the same serving of lunch from the same contaminated pot. Within 30 min after eating the meal, the children complained of stomach pain and soon after were taken ill with vomiting, diarrhea, and body jerks. Sixteen victims died at the site, and all others died in the hospital. Many children who fell ill from the contaminated food survived with medical treatment.
The Syrian case had the most YouTube hits, perhaps due to the demographics of the event. It happened on August 21, 2013; cell phones were available and popular and videos were relatively easy to record. Events in India had fewer video hits. There were probably fewer hits in India because the incident was food poisoning in a school that not only caused delayed effects, but was initially presumed “normal” food poisoning and an illicit attack was not suspected. In addition, while cell phones were readily available in 2013, camera phones would not be a norm for children or school administration in Bihar, India. The Tokyo case occurred in 1995, before video cell phones were commonplace. The only video access would have been if a person had a video recorder, or a news crew was nearby.
Image searches on Google were also utilized to find still pictures of the attacks to identify symptoms. The pictures were also given a unique identifier and recorded in a spreadsheet with corresponding victim information such as estimated age, gender, and symptoms. It was visually checked by the investigators that many of the pictures were obtained from the videos previously collected, and therefore the duplicative information was not included in the overall analysis. News reports of each incidence, along with published literature (primary, secondary, and tertiary) were also collected and documented to determine additional details about each individual incident of nerve agent exposure.
After the data were compiled into a spreadsheet, each symptom was tallied by incident. Each symptom was assigned a severity scale. Severe symptoms included: respiratory depression, seizure activity, unconsciousness, convulsions, and hypersecretion. Moderate symptoms included: fasciculations, miosis, vomiting, and any eye pain or blurred vision reported verbally in the videos. Mild symptoms included: weakness or limpness of the body, excessive sweating, coughing, headache, and screaming, crying, or any visibly upset or distressed state. Victims who had no noticeable signs of life or considered dead were excluded from the symptomatic analysis. For each OP chemical exposure, a pie graph was created to determine the respective percentage of severe, moderate, and mild symptoms. These graphs were then used, along with the published literature, to draw conclusions from the data collected.
RESULTS
Figure 2 shows representative images and descriptions of symptoms observed after pesticide and nerve agent poisoning of the victims. Table 1 shows the comparative analysis of the data documented from each of the three different incidents. Videos collected from Syria showed the largest age range, from infants to elderly. The age range seen in the Tokyo videos was from mostly young to middle‐aged adults, probably due to the fact that the time of the event occurred during the commute to work. No children were observed in the Tokyo case. The Indian case had the least variability in age, ranging from 5 to 12 years, which was expected as this occurred at a primary school. Victims were approximately the same age and probably had similar maximum exposures of pesticide mixed with lunch food of similar servings. In contrast to Tokyo and Syria, the Indian victims were accidently exposed to monocrotophos, a pesticides used in agriculture, as compared with intentional terrorist attacks of nerve agents in the other two cases.
Figure 2.
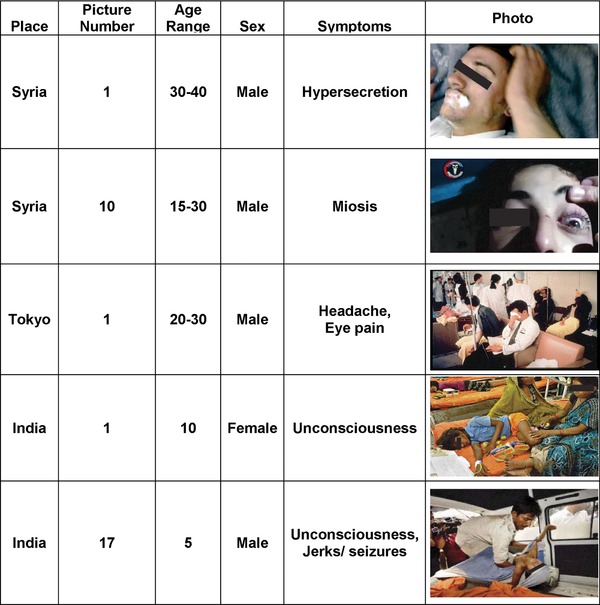
Severity of signs and symptoms of organophosphate and nerve agent poisoning by incident.
Table 1.
Comparative signs and symptoms of organophosphate and nerve agent poisonings in humans in three separate incidents worldwide.
| Syria | Tokyo | India | |
|---|---|---|---|
| Total victims/ videos observed | 22 | 8 | 8 |
| Signs/ symptoms |
|
|
|
| Severity | Mostly severe | Severe/moderate | Mild |
| Treatment |
|
|
IV medication (assumed atropine) |
| Time to treat | Hard to determine: Slow due to lack of medication and hospital space | Hard to determine: On site emergency and hospital response |
|
| Age | Infant to ∼60 yrs | 20‐50 yrs | 5‐12 yrs |
| Gender |
|
|
|
| Long‐term Follow‐up | N/A |
|
N/A |
| Acute neurological signs |
|
|
N/A |
| Chronic neurological impact | N/A |
|
N/A |
| Chemical weapon | Sarin | Sarin | Monocrotophos |
| Quality of agent | High grade | Low grade (∼35%) | Farming pesticide |
| Fault | Military | Civilian/ terrorist | Accidental |
| Death count | 1,400 | 13 | 23 |
| Date | August 21, 2013 | March 20, 1995 | July 16, 2013 |
From the analysis of the videos and collected data (Figure 2), Syria had the largest percentage of severe symptoms, which corresponds with the large number of deaths (1,400). Syria was followed by Tokyo, with 46% severe symptoms, but in Tokyo there was also a notable percentage of mild symptoms (32%). India had over 50% mild symptoms, but a notable number of either moderate or severe cases. A chart was created to depict a side‐by‐side comparison of each incident (Figure 3). Tokyo had the most resources for advanced treatment, which may account for the limited number of lives lost. Tokyo is also a large metropolitan city, with easy and fast access to healthcare and medications, whereas the events in Syria and India were in more rural areas that required travel to seek medical attention.
Figure 3.
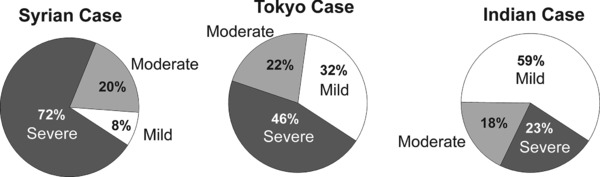
Percent of severity of symptoms observed in the three distinct human organophosphate poisoning incidents worldwide.
The outcomes from this study attest that the toxidrome can be predictable based on the agent (pesticide vs. nerve agent) and exposure (ingestion vs. inhalation). The pilot toxidrome observed from these videos show the constellation of signs and symptoms that are distinctly different in each of the three incidents. OPs are different from nerve agents and the route was ingestion, while the Syrian nerve gas attacks were, as noted, military with higher concentrations/dose delivered vs. Tokyo with many so‐called exposed getting minimal to no exposure. These factors, as well as healthcare resources, impacted morbidity and mortality in the three cases.
DISCUSSION
The novel research application of social media brings a useful tool to bear on these exposures. The findings from observing the videos of the Syrian and Tokyo attacks can be used as a model for the Indian pesticide poisoning. Lessons learned from the two larger cases with more severe symptomology can be applied to smaller pesticide cases such as what occurred in India. This is important because, although the Indian cases resulted in the majority of victims with mild symptoms, they are more at risk for severe delayed neurological effects.8, 9, 10 Because many survivors in India are young, long‐term follow‐up in this group is feasible. Tokyo and Syria can be used as a model for the toxidrome crisis of the Indian incident because all the compounds fall into the chemical classification of OPs, and most OPs are irreversible AChE inhibitors; thus, acting much like chemical weapons such as soman, VX, and sarin.1 In the Indian videos, the severe symptoms such as convulsions, seizures, and respiratory depression were less frequent. This is probably due the fact that a longer time elapsed between diagnosis and treatment, compared with the events recorded in Tokyo and Syria. It is also likely that such symptoms did occur in the Indian children who died and possibly others who survived, but whose symptoms were not videotaped because it happened in a remote village.
Like a previous study,4 this study has some caveats, such as limited authenticity or validation of the videos, lack of medical orientation of the videos cited, lack of background control data, and incomplete medical information of the victims. Nevertheless, the abundance of information helps to validate the information in a way similar to “crowd wisdom,” in which quantity and diversity compensate for quality.4 Nevertheless, this pilot study may set the stage for a large‐scale, multinational social media study on nerve agent toxidrome, treatment efficacy, and follow‐up on long‐term effects of survivors.
In all three incidents, only intravenous atropine was observed being administered in the videos. Atropine is a highly recommended treatment, but this requires intravenous access and must be administered by a medical professional in a healthcare setting. This is not always feasible during mass chemical attacks.11 The quick access to antidote autoinjectors would allow faster administration of the drug and decrease mortality.12 Currently, atropine and 2‐PAM autoinjectors are only available to military personnel in the United States. Allowing such access to populations at risk of a chemical attack should increase survival rates and allow for more time for victims to seek medical attention. Adequate stocks of better antidotes that can provide neurological protection would be beneficial in populations of people who are at risk for OP exposure. The need for quick diagnosis of a specific toxidrome and access to these medications is also an area in need of improvement.
When severe symptoms such as seizure activity ensue, it is a concern that long‐term damage or development of neurological dysfunction could result in victims after the acute symptoms subside. Due to neuronal damage by cholinergic crisis, there is a greater likelihood for chronic neurological and neuropsychiatric complications in the future. Perhaps an even more alarming fact is that those exposed people who may not have shown acute symptoms of OP poisoning, could be more sensitive to long‐term neurotoxic effects.1 This is consistent with the notion that long‐term toxicity from OP exposure may be underreported and more prevalent in cases of mild exposure, such as the Indian case. Long‐term toxicity could also be displayed as delayed polyneuropathy or neuropsychiatric disorder. Such symptoms could be attributed to a different origin, when in fact it is a result of OP exposure. These concerns illustrate the importance of chronic follow‐up data on the harm of OP poisoning given the limited effectiveness of current antidote treatments.
Animal models are important in the understanding of some of the neurotoxic effects that may be experienced short‐ and long‐term in humans.13, 14 The long‐term effects of OP exposure first seen after the Tokyo attack arose from non‐AChE inhibition, because OPs have secondary targets.15 Glutamate is an excitatory neurotransmitter in the brain responsible for critical functions such as cognition, memory, and learning.16 When glutamate is in excess, it can cause excitotoxic neurotoxicity and massive neuronal synaptic damage leading to long‐term neuropsychiatric dysfunction.16 Excess glutamate is a caused by superfluous activation of cholinergic receptors in the brain. Seizures are initially triggered by excess cholinergic hyperactivation, but are continued by persistent glutamatergic transmission within the brain synapses. Effective control of seizures is critical for survival as well as preventing neuronal damage or long‐term neurological dysfunction.
In conclusion, with the vast availability of social media, chemical attacks can be well documented and accessed worldwide. The videos can be used as a research tool to draw conclusions about the victimized population as a whole. By analyzing three separate OP attacks, we were able to compare the toxidrome from each and use a large‐scale deconstruction as a model for comparison and drawing conclusions. By possibly utilizing the Indian case as a future population for long‐term follow‐up and development of chronic toxicity, we can better categorize the delayed neurotoxicity of OP exposure in survivors, as well as increase preparedness should another attack occur. These incidents underscore the need for better antidotes and follow‐up of victims for neurological or long‐term symptoms.
Acknowledgments
The author's preclinical research was supported by the CounterACT Program, National Institutes of Health, Office of the Director and the National Institute of Neurologic Disorders and Stroke [Grant U01 NS083460]. We are grateful to The Economist for the permission to use the timeline chart. The open access publishing fees for this article have been covered by the Texas A&M University Online Access to Knowledge (OAK) Fund, supported by the University Libraries and the Office of the Vice President for Research.
Author Contributions
D.S.R. and E.C. wrote the article; D.S.R. designed the research; D.S.R. and E.C. performed the research; D.S.R. and E.C. analyzed the data.
Conflict of Interest
The authors report no conflicts of interest. The views expressed in this article are those of the authors and do not reflect the official policy of Texas A&M University, the National Institutes of Health, the Department of Defense, or any other United States Government agency.
References
- 1. Krause, K.H. , van Thriel, C. , De Sousa, P.A. , Leist, M. & Hengstler, J.G. Monocrotophos in Gandaman village: India school lunch deaths and need for improved toxicity testing. Arch. Toxicol. 87, 1877–1881 (2013). [DOI] [PubMed] [Google Scholar]
- 2. Maass, H. A brief history of chemical warfare. The Week. Retrieved July 24, 2014, from http://theweek.com/article/index/249224/a-brief-history-of-chemical-Warfare [Google Scholar]
- 3. Holstege, C.P. , Kirk, M. & Sidell, F.R. Chemical warfare: nerve agent poisoning. Med. Toxicol. 13, 923–942 (1997). [DOI] [PubMed] [Google Scholar]
- 4. Rosman, Y. et al Lessons Learned from the syrian sarin attack: evaluation of a clinical syndrome through social media. Ann. Intern. Med. 160, 644–468 (2014). [DOI] [PubMed] [Google Scholar]
- 5. Reddy, S.D. & Reddy, D.S. Midazolam as an anticonvulsant antidote for organophosphate intoxication: A pharmacotherapeutic appraisal. Epilepsia 56, 813–821 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Reddy, D.S. Neurosteroids for the protection of humans against organophosphate toxicity. Ann. N. Y. Acad. Sci. 1378, 25–32 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Worek, F. & Thiermann, H. The value of novel oximes for treatment of poisoning by organophosphorus compounds. Pharmacol. Ther. 139, 249–259 (2013). [DOI] [PubMed] [Google Scholar]
- 8. Yokoyama, K. et al Chronic neurobehavioral and central and autonomic nervous system effects of Tokyo subway sarin poisoning. J. Physiol. 92, 317–323 (1998). [DOI] [PubMed] [Google Scholar]
- 9. Li, Q. , Hirata, Y. , Kawada, T. & Minami, M. Elevated frequency of sister chromatid exchanges of lymphocytes in sarin‐exposed victims of the Tokyo sarin disaster 3 years after the event. Toxicology. 201, 209–217 (2004). [DOI] [PubMed] [Google Scholar]
- 10. Miyaki, K. et al Effects of sarin on the nervous system of subway workers seven years after the Tokyo subway sarin attack. J. Occup. Health 47, 299–304 (2005). [DOI] [PubMed] [Google Scholar]
- 11. Tharoor, I. Syria's Lurking Terror: A History of Sarin Gas | TIME.com. World Syria's Lurking Terror a History of Sarin Gas Comments. Retrieved July 8, 2014, from http://world.time.com/2013/05/07/syrias-lurking-terror-a-history-of-sarin-gas/
- 12. Rebmann, T. , Clements, B.W. , Bailey, J.A. & Evans, R.G. Organophosphate antidote autoinjectors vs. traditional administration: A time motion study. J. Emerg. Med. 37, 139–143 (2009). [DOI] [PubMed] [Google Scholar]
- 13. Skovira, J.W. , McDonough, J.H. & Shih, T.M. Protection against sarin‐induced seizures in rats by direct brain microinjection of scopolamine, midazolam or MK‐801. J. Mol. Neurosci. 40, 56–62 (2010). [DOI] [PubMed] [Google Scholar]
- 14. Reddy, D.S. Experimental models of status epilepticus and neuronal injury for evaluation of therapeutic interventions. Int. J. Mol. Sci. 14, 18284–18318 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Garrett, T.L. , Rapp, C.M. , Grubbs, R.D. , Schlager, J.J. & Lucot, J.B. A murine model for sarin exposure using the carboxylesterase inhibitor CBDP. Neurotoxicology 31, 502–508 (2010). [DOI] [PubMed] [Google Scholar]
- 16. Eisenkraft, A. , Falk, A. & Finkelstein, A. The role of glutamate and the immune system in organophosphate induced CNS damage. Neurotox. Res. 24, 265–279 (2013). [DOI] [PubMed] [Google Scholar]
- 17. Harris, G. & Kumar, H. (17 July 2013). Contaminated lunches kill 22 children in India. The New York Times. New York City. Retrieved 17 July 2013.
- 18. Idrovo, A.J. Food poised with pesticide in Bihar India: new disaster, same story. Occup. Environ. Med. 71, 228–228 (2014). [DOI] [PubMed] [Google Scholar]


