Abstract
PURPOSE
The patient medical home (PMH) model aims to improve patient satisfaction and health outcomes in Canada, but since its introduction in 2009, there has been no evaluation of the extent to which primary care conforms with PMH attributes. Our objective was to compare current primary care across Canada with the 10 goals of the PMH model.
METHODS
A cross-sectional survey of primary care organization and delivery was conducted in Canadian provinces to evaluate the PMH-based attributes of primary care practices. Family physician and patient responses were mapped to the 10 goals of the PMH model. We used regression models to describe the provinces’ success in meeting the goals, taking specific practice characteristics into account. We created a PMH composite score by weighting each goal equally for each practice and aggregating these by province. The PMH score is the sum of the values for each goal, which were scored from 0 to 1; a score of 10 indicates that all 10 goals of the PMH model were achieved.
RESULTS
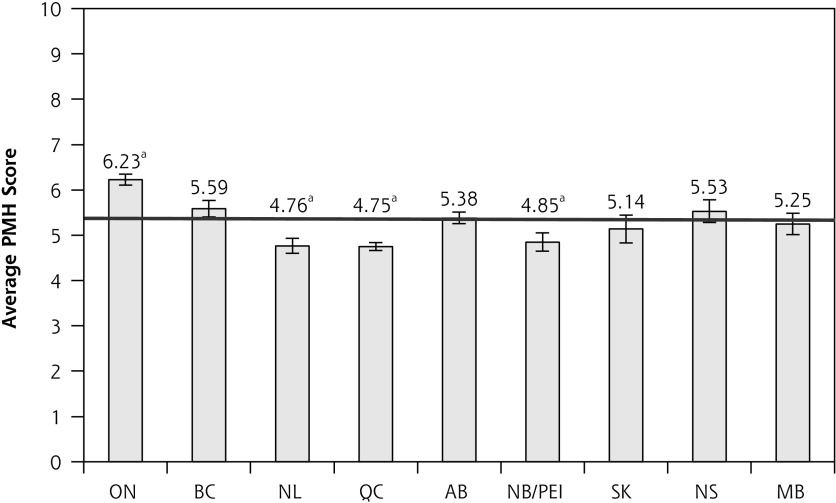
Seven hundred seventy-two primary care practices and 7,172 patients participated in the survey. The average national PMH score was 5.36 (range 4.75–6.23) of 10. Ontario was the only province to score significantly higher than Canada as a whole, whereas Québec, Newfoundland/Labrador, and New Brunswick/Prince Edward Island scored below the national average. There was little variation, however, among provinces in achieving the 10 PMH goals.
CONCLUSIONS
Provincial PMH scores indicate considerable room for improvement if the PMH goals are to be fully implemented in Canada.
Keywords: primary care, patient-centered care, patient medical home, Canada
INTRODUCTION
Effective primary care greatly improves overall population health while supporting general health systems performance.1,2 Strong primary care systems are associated with a more equitable distribution of health services and lower health care costs.3 One of the mechanisms underlying the positive impact of primary care is the delivery model.2 The patient-centered medical home (PCMH) is an approach to providing comprehensive primary care.4 Its fundamental principles include patients forming a relationship with a personal physician, striving for whole-person orientation, ensuring care is coordinated and/or integrated, and a focus on quality, safety, and access.4 In the United States, the PCMH is associated with lower health care costs and improved quality of and satisfaction with primary care.5
The College of Family Physicians Canada (CFPC) introduced the patient medical home (PMH), a made-in-Canada version of the PCMH, as a model for best practice in 2009.6 The CFPC defines the PMH by 10 goals (Table 1) that enable the best possible health outcomes for patients and the communities in which they live while emphasizing Canadian values in health care: equity, fairness, and access to care.7 The CFPC’s vision for the PMH model is to provide Canadian practices a shared PMH framework and to present a set of indicators with which family practices can evaluate the attributes of their primary care model.8
Table 1.
The 10 Goals of the Patient Medical Home Model
| 1. Patient centered | Provide services that are responsive to patients’ and their families’ feelings, preferences, and expectations |
| 2. Personal family physician | The most responsible provider of a given patient’s medical care Every person in Canada should have a personal family physician |
| 3. Team-based care | Offer a broad scope of services carried out by teams or networks of clinicians; inclusive of nurses, peer physicians, and others |
| 4. Timely access | Timely access to appointments in the practice Advocate for and coordinate timely appointments with other health and medical services required |
| 5. Comprehensive care | Provide a comprehensive scope of family practice services by working collaboratively with other professionals Address public health needs Taking population health effects into account |
| 6. Continuity | Offer continuous care over time and in different settings Advocate on the patients’ behalf for continuity of care throughout the health care system Preserve constant relationships and continuous medical information for patients |
| 7. Electronic records and health information | Maintain electronic medical records |
| 8. Education, training, and research | Serve as a model place for training students, residents, and other health professionals Carry out and/or encourage staff to be involved in primary care research |
| 9. Evaluation | Carry out ongoing evaluation as part of the commitment to continuous quality improvement |
| 10. System support | Internal support through governance and management structures External support by stakeholders, the public, and other medical and health professionals and their organizations across Canada |
The de facto guidelines for evaluating primary care models in the United States are the National Committee for Quality Assurance’s Patient-Centered Medical Home Standards, developed in collaboration with interested stakeholders and updated every 3 years.9–12 In Canada, different primary care reform initiatives have been implemented in each province during the past decade, but there is no systematic evaluation tool to determine how these reform strategies have influenced family practices’ conformity to the PMH vision. The CFPC has developed a self-assessment questionnaire for family physicians to analyze their practice’s performance as a PMH; however, this tool is intended as a guide solely for family physicians and fails to address the patient perspective.13
We endeavored to determine to what extent the structure and processes that define primary care in Canada14 are aligned with the goals set by the PMH model by analyzing findings from the Canadian Quality and Costs of Primary Care (QUALICO-PC) study.
METHODS
The QUALICO-PC study was initially designed to systematically evaluate the scope of European primary care systems and their effects on health outcomes by gathering data on 3 major components: system level (financing and governance), provision level (general practitioners), and user level (patient experiences and values).15,16 With these same evaluation goals, a Canadian research team adopted the study and collected survey data in all 10 provinces. The results of this survey provide valuable baseline measurements on the standard of primary care across Canada.
Attributes of the PMH Model
We based our assessment of primary care on the core attributes of the PMH model, which have been summarized and validated by previous studies.7 Haggerty et al17 provide operational definitions and a framework for evaluation of primary care models in Canada, outlining 7 of the 10 PMH goals. The 3 additional attributes included in the PMH goals are timely access; electronic medical records; and education, training, and research. Timely access is referenced throughout the operational definitions of other attributes, whereas the electronic medical records goal is included under informational continuity and clinical information management. The CFPC considers education, training, and research an important goal because practices demonstrating adherence to the PMH goals are understood to be ideal sites for training the next generation of health professionals and for evaluating the effectiveness of their practice model.7
Data Collection
The European QUALICO-PC research team constructed and validated 4 questionnaires that were adapted for compatibility with Canadian health care systems. Data were collected in Canadian provinces in 2013–2014.14 The surveys were directed at family physicians and their service delivery, primary care practices, patients’ experiences with physicians, and the importance patients place on various aspects of primary care.16,18
The Canadian QUALICO-PC study was guided by provincial leads, and each team followed similar surveying methods.14 Survey implementation in New Brunswick and Prince Edward Island was merged because of small populations, narrowing the comparison to 9 jurisdictions. Seven hundred seventy-two primary care practices and 7,172 of their patients participated in the survey. On average, 9 patients from each practice responded to the patient experience questionnaire. Data were pooled to generate the data set used in this study. Ethics approvals were obtained by lead investigators in each jurisdiction.14
Main Outcomes
To assess how well practices aligned with the PMH model in each province, we used the QUALICO-PC survey data to calculate an overall PMH score and scores for the 10 individual PMH goals. First, we matched questions from 3 of the 4 questionnaires (family physician, family practice, and patient experience questionnaires) to the 10 PMH goals in the CFPC document.7 The response to each survey question was coded according to whether the answer demonstrated the practice’s ability to meet a PMH goal (Supplemental Appendix 1, available at http://www.annfammed.org/content/15/3/230/suppl/DC1/). Two researchers independently applied the codes using the coding manual. Where consensus could not be reached, the input of a third researcher was sought. Some responses demonstrated the practice’s ability to meet more than 1 goal, and in this case, they were matched to all suitable goals. The 3 questionnaires used in our analyses are presented in Supplemental Appendix 2, available at http://www.annfammed.org/content/15/3/230/suppl/DC1/. The fourth questionnaire (on patient values) does not relate to the PMH goals.
The responses were analyzed as binary variables. Responses to multiple-choice questions were aggregated to create a dichotomous response. The individual PMH goals were scored as 0 or 1 at the practice level based on questionnaire responses, and averaged across practices in each province. For example, if three-fourths of practice responses for a PMH goal were scored as yes (1), the result was a provincial score of 0.75 for that goal. The composite PMH score was calculated by summing the values for each goal (to a maximum of 10). A perfect score of 10 would indicate that the practice was operating in full accordance with the PMH model.
Statistical Analysis
We used linear regression modeling to describe the degree to which each province and Canada as a whole attained the PMH goals 1 through 9. Other practice characteristics were considered as confounders, and province was the exposure variable. For PMH goal 10, we used logistic regression modeling, as this goal was evaluated using dichotomous questions (Supplemental Appendix 3, available at http://www.annfammed.org/content/15/3/230/suppl/DC1/). Province was not included in the model for goal 10 because many of the provinces had no primary care practices that met this goal.
RESULTS
Practice characteristics are displayed in Table 2, the geographic distribution of responses is presented in Table 3, and the average PMH scores for Canada as a whole and for each province are shown in Figure 1. The national average PMH score was 5.36 (range 4.75–6.23). Ontario was the only province to achieve a mean PMH score significantly higher than the national average, whereas Newfoundland/Labrador, Québec, and the combined jurisdiction of New Brunswick and Prince Edward Island had significantly lower scores.
Table 2.
Practice Characteristics Included in the Statistical Model
| No. (%) | |
|---|---|
| Community size | |
| Large city center | 238 (30.36) |
| Suburbs | 133 (16.96) |
| (Small) town | 152 (19.39) |
| Mixed urban-rural | 107 (13.65) |
| Rural | 154 (19.64) |
| Funding model | |
| New model of primary care with special funding | 421 (53.16) |
| Traditional model | 371 (46.84) |
| Practice population size | |
| ≤800 | 185 (23.36) |
| 801–1600 | 310 (39.14) |
| 1,601–2,400 | 162 (20.45) |
| 2,401–3,200 | 71 (8.96) |
| >3,200 | 64 (8.08) |
| Wait time between scheduled appointment and consultation | |
| <15 min | 3,592 (50.08) |
| 15–30 min | 2,074 (28.92) |
| 31–45 min | 630 (8.78) |
| >46 min | 481 (6.70) |
| Hours of operation | |
| Clearly indicated outside office entrance | 480 (62.18) |
| Not clearly indicated | 276 (35.75) |
| How to get care outside of office hours | |
| Clearly indicated outside office entrance | 216 (27.98) |
| Not clearly indicated | 526 (68.13) |
| Parking for people with disabilities | |
| Yes | 684 (88.6) |
| No | 81 (10.49) |
| Physical accessibility of practice | |
| Ground floor | 477 (61.79) |
| Elevator | 255 (33.03) |
| No elevator/not ground floor | 35 (4.53) |
| Physical access for patients with a wheelchair or stroller | |
| Very easy | 453 (58.68) |
| Easy | 273 (35.36) |
| Difficult/Impossible to access | 46 (5.96) |
| Accessible toilet for patients with disabilities | |
| Yes | 672 (87.05) |
| No | 87 (11.27) |
Note: All practice characteristics were included in the model regardless of their significance (P <.05). Practice characteristics related to physical accessibility (last 6 characteristics above) were combined into 1 variable, “superior access.” The reference category for practice population size was 801–1600, as this response was most common. For wait time, we calculated each practice’s average wait time. Québec was chosen as a reference category for province because it represented the largest sample.
Table 3.
QUALICO-PC Surveys Undertaken in Each Province
| Province | Family Physician No. | Practice No. | Patient Experience No. | Total by Province No. | Completion Rate % |
|---|---|---|---|---|---|
| Ontario | 184 | 183 | 1,698 | 2,065 | 81 |
| British Columbia | 59 | 58 | 537 | 654 | 84 |
| Newfoundland and Labrador | 41 | 41 | 320 | 402 | 57 |
| Alberta | 116 | 117 | 1,240 | 1,473 | 70 |
| New Brunswick/PEI | 54 | 53 | 497 | 604 | 70 |
| Saskatchewan | 20 | 20 | 185 | 225 | 77 |
| Nova Scotia | 59 | 58 | 544 | 661 | 75 |
| Manitoba | 41 | 24 | 353 | 418 | 67 |
| Québec | 218 | 218 | 1,798 | 2,234 | 84 |
| Total surveys by type | 792 | 772 | 7,172 |
PEI = Prince Edward Island; QUALICO-PC = Quality and Costs of Primary Care.
Note: Completion rates calculated as the number of physicians who completed the survey package divided by the number of physicians who received the survey package.
Figure 1.
Average crude patient medical home scores in the Canadian provinces.
AB = Alberta; BC = British Columbia; MB = Manitoba; NB = New Brunswick; NL = Newfoundland/Labrador;
NS = Nova Scotia; O = Ontario; QC = Quebec; PEI = Prince Edward Island; SK = Saskatchewan.
Note: Error bars represent 95% confidence intervals.
aDenotes a significant difference (P <.05) from the national average.
The crude linear regression model estimates for each PMH goal are presented in Supplemental Appendix 3.
After adjusting for practice characteristics, we compared PMH scores among jurisdictions. The mean differences in PMH scores between provinces are displayed in Table 4. Province is a key variable, as it represents the differences in the organization of care among jurisdictions, which may not have been captured by the practice characteristics we measured. After controlling for all covariates, Ontario stood out as achieving significantly higher standards of primary care than Québec across more goals (8 of 10) than any other province, although British Columbia and Nova Scotia also scored higher than Québec in 6 of 10 goals. When examining the individual goals of the PMH model, there was generally little variation among provinces. All provinces scored higher than Québec in continuity. Alberta scored lower than Québec on patient centeredness, team-based care, and comprehensive care, but higher on continuity, electronic records and health information, evaluation, and overall.
Table 4.
Adjusted Mean Differences in Patient Medical Home Scores Among Canadian Provinces, Using Québec as the Reference Province
| Patient Medical Home Goal | Mean Differences (95% CI) | Mean Differences (95% CI) | ||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Ontario | British Columbia | Newfoundland/Labrador | Alberta | New Brunswick/Prince Edward Island | Saskatchewan | Nova Scotia | Manitoba | |
| Patient medical home (overall) | 1.48 (1.33 to 1.63)a | 0.84 (0.62 to 1.05)a | 0.01 (−0.23 to 0.26) | 0.63 (0.46 to 0.80)a | 0.10 (−0.13 to 0.32) | 0.39 (0.04 to 0.74)a | 0.78 (0.56 to 0.99)a | 0.50 (0.25 to 0.75)a |
| Patient centered | 1.03 (0.31 to 1.75)a | 0.90 (−0.16 to 1.95) | 0.52 (−0.71 to 1.74) | 1.64 (−2.43 to −0.84)a | 0.46 (−0.63 to 1.54) | 0.69 (−0.99 to 2.37) | 0.78 (−0.27 to 1.83) | −0.54 (−1.76 to 0.69) |
| Personal family physician | 2.37 (1.53 to 3.20)a | 2.31 (1.08 to 3.54)a | 1.26 (−0.17 to 2.68) | −0.71 (−1.64 to 0.21) | 1.16 (−0.10 to 2.42) | 1.58 (−0.37 to 3.54) | 1.67 (0.45 to 2.89)a | 1.73 (0.31 to 3.15)a |
| Team-based care | −0.34 (−1.20 to 0.51) | −0.96 (−2.22 to 0.29) | −0.79 (−2.25 to 0.66) | −2.44 (−3.38 to −1.49)a | −0.04 (−1.33 to 1.25) | −1.60 (−3.60 to 0.39) | −0.40 (−1.64 to 0.85 | −4.88 (−6.34 to −3.43)a |
| Timely access | 1.69 (1.10 to 2.28)a | 0.39 (−0.48 to 1.26) | −0.19 (−1.20 to 0.82) | −0.59 (−1.24 to 0.07) | −1.40 (−2.29 to −0.51)a | −0.06 (−1.44 to 1.32) | 0.02 (−0.84 to 0.88) | −1.07 (−2.08 to −0.07)a |
| Comprehensive care | 3.88 (2.06 to 5.69)a | 7.42 (4.75 to 10.09)a | 6.34 (3.25 to 9.44)a | −2.36 (−4.37 to −0.35)a | 1.88 (−0.86 to 4.63) | 6.92 (2.67 to 11.17)a | 4.01 (1.36 to 6.66)a | 1.87 (−1.22 to 4.97) |
| Continuity | 1.14 (0.83 to 1.45)a | 1.56 (1.10 to 2.01)a | 0.72 (0.19 to 1.24)a | 0.66 (0.32 to 1.00)a | 0.98 (0.51 to 1.45)a | 0.88 (0.16 to 1.60)a | 1.29 (0.84 to 1.75)a | 1.05 (0.52 to 1.57)a |
| Electronic records and health information | 2.73 (2.34 to 3.13)a | 2.28 (1.70 to 2.86)a | 0.07 (−0.61 to 0.74) | 2.32 (1.87 to 2.78)a | −0.30 (−0.90 to 0.30) | 1.63 (0.70 to 2.55)a | 1.79 (1.21 to 2.37)a | 2.75 (2.08 to 3.42)a |
| Education, training, and research | −0.18 (−0.75 to 0.40) | −0.08 (−0.92 to 0.75) | −0.59 (−1.57 to 0.39) | −0.21 (−0.86 to 0.45) | −0.44 (−1.31 to 0.42) | 0.23 (−1.10 to 1.56) | 0.05 (−0.79 to 0.89) | 0.01 (−0.96 to 0.98) |
| Evaluation | 2.22 (1.89 to 2.56)a | 1.56 (1.07 to 2.05)a | −0.22 (−0.80 to 0.35) | 1.16 (0.78 to 1.55)a | 0.22 (−0.29 to 0.73) | 0.47 (−0.32 to 1.25) | 1.31 (0.81 to 1.80)a | 1.73 (1.16 to 2.30)a |
Note: Estimates are adjusted for variables shown in Table 2.
Values are significantly different (P <.05) from the reference province (Québec).
DISCUSSION
In this study, we derived measurable indicators of the PMH model and applied them across 10 Canadian provinces. The national average PMH score was 5.63 of 10, which indicates that major work remains to fully meet the PMH goals. Despite the implementation of specific primary care reform strategies across several provinces during the past decade, Ontario was the only province to achieve a higher overall PMH score than the national average.
In examining the individual goals of the PMH model, we found that Ontario’s primary care clinics also performed better than any other province, scoring higher than the reference province (Québec) in 7 of 10 PMH goals, and achieving a higher overall PMH score. Primary care reform initiatives across Canadian jurisdictions have emphasized quality improvement and system-level changes to practice, including creating collaborative primary care teams or networks.19 Ontario has arguably undergone the largest system-level primary care reform among provinces, with the introduction of diverse payment schemes and organizational models, such as Family Health Teams established in 2005.20,21 These and other reforms that focus heavily on supporting alternate health care clinicians may have afforded an advantage in PMH scoring, because they were accounted for in 2 PMH goals (team-based care and comprehensive care). In Québec, a reform initiative based on assigning patients to a duty roster and collaboration between physicians and nurses (Groupes de Médecine de Famille) has been recognized for improving access to primary care; however, clinician uptake has been low.22
Other challenges in meeting PMH goals were evident, particularly for the team goal, where Alberta and Manitoba scored significantly lower than Québec. These results were unexpected, given the reform initiatives active in these provinces. In Alberta, implementation of Primary Care Networks, a team model comprised of doctors, nurses, dieticians, and pharmacists, began in 2005.23 In Manitoba, improvements from the Physician Integrated Network supporting access to and quality of primary care might not be reflected in the results, as it was implemented only a few years before the study began.24 Carter et al19 recently evaluated the impact of primary care reform initiatives on Canadian health system performance by measuring indicators of health service use, processes of care, and physician productivity. They found a reduction in rates of emergency department visits that could be attributed to interdisciplinary team-based models.19 We were unable to determine, however, how health services utilization has been affected by reform initiatives, because the QUALICO-PC questionnaires placed minimal emphasis on these indicators.
The adoption of new primary care models in response to reform initiatives remains relatively low or incomplete, which may limit their impact on provincial PMH scores. Although the PMH is a pan-Canadian model proposed by the CFPC, implementation is dependent on provincial and regional or local policies. During the past 15 years, new primary care funding models have been introduced without consistency in timing, key model components, or implementation strategies across provinces.20 As a result, implementation of PMH attributes depends on local factors (physician- or practice-led initiatives) or are only indirectly linked to the reform models. If our goal is to improve health and health care outcomes for patients, we should work toward achieving the PMH model while strengthening other community-based services, such as home care and public health, on a local and regional scale.
This analysis of the largest national primary care survey to date includes both province- and practice-level data, providing insight into the impact of both provincial policy and local governance on primary care service delivery in Canada. Including patient-reported measures in combination with the practice- and system-level variables is unique to the QUALICO-PC study design. The study identifies a potential avenue for aligning other practices with the PMH model, given that practices that were part of a new model benefitting from special funding or government-led reform performed better for many of the goals.
The study is limited by several of its design features. Recruitment for this study was not systematic, because no directory of family physicians exists at the practice level. Even though the sample size is large, the number of respondents per practice was limited and relied on a convenience sample, and the recruitment of the practices varied slightly among jurisdictions.14 The cross-sectional nature of the data does not reflect the evolving stages of primary care reform across jurisdictions. The survey was not designed specifically to measure the PMH goals, which resulted in some goals being better represented than others. We also recognize that our analyses do not do justice to the complexity of the integrated PMH concept or the depth of the individual components of the PMH model. Future qualitative or multimethod analyses would compliment and expand this study.
The national achievement of PMH standards remains low with statistically significant but relatively minor variations among provinces. Although meeting the PMH goals was not the primary objective of primary care reform in Canada, Ontario has invested most heavily in primary care reform in Canada,20 resulting in Ontario’s primary care delivery coming closest to the PMH model. There is, however, certainly room for improvement. The findings presented here should stimulate future research into the effects of reform on practice characteristics and processes. It should also encourage assessment of health services utilization and quality measures for clinical conditions. These activities would provide valuable information on clinical performance and may motivate further uptake of the PMH model’s attributes in all provinces.
Acknowledgments
We gratefully acknowledge Dr Dan Chateau for providing statistical expertise, and Dr Jennifer Enns for assistance with writing the manuscript.
Footnotes
Conflicts of interest: authors report none.
Supplementary materials: Available at http://www.AnnFamMed.org/content/15/3/230/suppl/DC1/.
References
- 1.Kringos DS, Boerma WG, Hutchinson A, van der Zee J, Groenewegen PP. The breadth of primary care: a systematic literature review of its core dimensions. BMC Health Serv Res. 2010;10:65 10.1186/1472-6963-10-65.:65-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Macinko J, Starfield B, Shi L. The contribution of primary care systems to health outcomes within Organization for Economic Cooperation and Development (OECD) countries, 1970–1998. Health Serv Res. 2003;38(3):831–865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patient-Centered Primary Care Collaborative. Joint Principles of the Patient-Centered Medical Home. 2007; http://www.aafp.org/dam/AAFP/documents/practice_management/pcmh/initiatives/PCMH-Joint.pdf.
- 5.Nielsen M, Buelt L, Patel K, Nicholas L. The patient-centered medical home’s impact on cost and quality: annual review of evidence, 2014–2015. Patient-Centered Primary Care Collaborative. https://www.pcpcc.org/resource/patient-centered-medical-homes-impact-cost-and-quality-2014-2015. Published Feb 2016.
- 6.The College of Family Physicians of Canada. Patient-centered care in Canada: bring it on home. The College of Family Physicians of Canada. http://www.cfpc.ca/uploadedFiles/Resources/Resource_Items/Bring20it20on20Home20FINAL20ENGLISH.pdf. Published Oct 2009.
- 7.The College of Family Physicians of Canada. A vision for Canada: family practice, the patient’s medical home. The College of Family Physicians of Canada. http://www.cfpc.ca/uploadedFiles/Resources/Resource_Items/PMH_A_Vision_for_Canada.pdf. Published Sep 2011.
- 8.Gutkin C. The future of family practice in Canada: The Patient’s Medical Home. Can Fam Physician. 2011;57(10):1224. [Google Scholar]
- 9.Stange KC, Nutting PA, Miller WL, et al. Defining and measuring the patient-centered medical home. J Gen Intern Med. 2010;25(6):601–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.The American Academy of Family Physicians. The patient-centered medical home (PCMH). The American Academy of Family Physicians. http://www.aafp.org/practice-management/transformation/pcmh.html. Published 2016.
- 11.The Agency for Healthcare Research and Quality. A guide to real-world evaluations of primary care interventions: Some practical advice. https://www.pcmh.ahrq.gov/sites/default/files/attachments/PCMH_Evaluation_Guide.pdf. Published 2014.
- 12.The National Committee for Quality Assurance (NCQA). Standards and guidelines for NCQA’s patient-centered medical home (PCMH) 2011. NCQA. https://www.communitycarenc.org/media/files/ncqap-cmh2011_standardsandguidelines.pdf. Published Mar 2011.
- 13.The College of Family Physicians Canada. The patient’s medical home. http://patientsmedicalhome.ca/. Published 2016.
- 14.Wong ST, Chau LW, Hogg W, et al. An international cross-sectional survey on the Quality and Costs of Primary Care (QUALICO-PC): recruitment and data collection of places delivering primary care across Canada. BMC Fam Pract. 2015;16:20 10.1186/s12875-015-0236-7.:20-0236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Netherlands Institute for Health Services Research. The QUALICOPC project. NIVEL. http://www.nivel.nl/en/qualicopc/.
- 16.Schafer WL, Boerma WG, Kringos DS, et al. QUALICOPC, a multi-country study evaluating quality, costs and equity in primary care. BMC Fam Pract 2011;%20;12:115 10.1186/1471-2296-12-115.:115-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Haggerty J, Burge F, Lévesque JF, et al. Operational definitions of attributes of primary health care: consensus among Canadian experts. Ann Fam Med. 2007;5(4):336–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schäfer WL, Boerma WG, Kringos DS, et al. Measures of quality, costs and equity in primary health care instruments developed to analyse and compare primary care in 35 countries. Qual Prim Care. 2013;21(2):67–79. [PubMed] [Google Scholar]
- 19.Carter R, Riverin B, Levesque JF, Gariepy G, Quesnel-Vallée A. The impact of primary care reform on health system performance in Canada: a systematic review. BMC Health Serv Res. 2016;16:324 10.1186/s12913-016-1571-7.:324-1571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hutchison B, Levesque JF, Strumpf E, Coyle N. Primary health care in Canada: systems in motion. Milbank Q. 2011;89(2):256–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rosser WW, Colwill JM, Kasperski J, Wilson L. Progress of Ontario’s Family Health Team model: a patient-centered medical home. Ann Fam Med. 2011;9(2):165–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Breton M, Lévesque JF, Pineault R, Hogg W. Primary care reform: can Quebec’s family medicine group model benefit from the experience of Ontario’s family health teams? Healthc Policy. 2011;7(2):e122–e135. [PMC free article] [PubMed] [Google Scholar]
- 23.Health Alberta. Primary care networks. Government of Alberta. http://www.health.alberta.ca/services/primary-care-networks.html. Published 2016.
- 24.Health Manitoba. Primary care. Government of Manitoba. http://www.gov.mb.ca/health/primarycare/public/index.html. Published 2016.