Abstract
Background and objective
Patient characteristics require consideration for optimal treatment in order to achieve clinical remission for an improved quality of life and social functioning. Prior evidence supports long-acting injectable antipsychotics (LAIs) in the relapse prevention of schizophrenia. This study aimed to characterize Japanese patients diagnosed with schizophrenia and to compare the outcomes of LAIs and oral antipsychotics (AP) in re-hospitalization or emergency room visit rates.
Methods
Diagnostic Procedure Combination (DPC) designated hospital data in Japan with ICD-10 code F20x between July 2013 and June 2015 were obtained from the Medical Data Vision Co. Ltd. Patients were divided into sub-groups in order to filter co-diagnostic conditions. Differences across sub-groups were assessed using a Chi square test or ANOVA. The incidence rate ratio (IRR) was calculated to compare the re-hospitalization (30 days post discharge) or emergency room visit rates between pharmacotherapy groups of oral versus LAI or typical versus atypical within LAI patients. Adjusted estimates were provided by propensity scores that were assigned for age, gender, and Charlson co-morbidity index (CCI) scores.
Results
A quarter of the data sourced were attributed to co-diagnosis with dementia/delirium with antipsychotic prescriptions despite reported risks of antipsychotic use. After adjusting for age, gender, and co-morbidity, LAI reduced re-hospitalization and emergency (ER) visit rates more than oral APs (LAI vs. oral IRR = 0.38 (95% CI 0.17–0.74), IRR = 0.56 (95% CI 0.34–0.91), respectively).
Conclusion
The study findings demonstrate usage of DPC hospital data in schizophrenia pharmacotherapy based on classification of co-diagnoses. In comparison with oral APs only, LAI utilization can provide an opportunity for reduced re-hospitalization and ER visit rates among patients with schizophrenia.
Key Points
| Administrative databases can be used for outcome studies in Japan when the study population is carefully selected. |
| A quarter of the sample population had a co-diagnosis with dementia/delirium with antipsychotic prescriptions despite reported risks of antipsychotic use. |
| Compared to oral antipsychotics, patients with schizophrenia receiving long-acting injectable antipsychotics may have a reduced incidence of re-hospitalization and emergency room visits. |
Background
Schizophrenia is a debilitating disease with high morbidity and mortality. Prevalence and incidence rates similar to other countries have been reported in Japan [1]. Even with these conservative [2] estimates, a recent study found that schizophrenia has the highest societal cost among psychiatric disorders in Japan. The estimated annual burden of the disease exceeded 3.5 million yen per patient (approx. US$30,000) [3]. Most of the costs can be attributed to the loss of working ability, since patients with schizophrenia face a higher likelihood of being unemployed. Hospitalization has been identified as another significant cost driver not only in Japan but also in the USA [4, 5] and Europe [6, 7]. Therefore, relapse prevention that helps reduce inpatient stays is an important element in the treatment of schizophrenia.
The common goal of pharmacotherapy with antipsychotics (APs) in patients with schizophrenia is to prevent relapse and to reduce the severity of subsequent acute episodes over time. A wide range of antipsychotic medications is available, ranging from conventional or typical [first-generation antipsychotics (FGA)], atypical [second-generation antipsychotics (SGA)] in oral form and typical and atypical long-acting injectable antipsychotics (LAIs). However, the effectiveness of oral AP treatment is often undermined by poor adherence, which is associated with an increased frequency of relapse and hospitalization rates, more severe symptoms, longer inpatient stays, and higher hospital costs [8–20].
LAI therapy has been shown to significantly improve adherence, reduce symptoms, and reduce the risk of relapse and re-hospitalization [6, 21–25]. On the other hand, LAIs are less flexible in regard to dose adjustments [26], delayed disappearance of side effects, and the possibility that some patients might feel pain at the injection site as well as skin irritation and lesions [27].
Limited evidence, however, has been confirmed in the Japanese population for patients with schizophrenia. Using Japanese cost data, a budget impact model study suggested that the use of LAIs could reduce healthcare expenditures in Japan [28]. However, this study relied on re-hospitalization rates from international clinical studies, whereas local Japanese data would more accurately reflect Japanese clinical practice. Therefore, this study aimed to analyze the impact of LAI therapy on healthcare utilization outcomes with data from the Japanese population.
Methodology
Data Source
A commercially available hospital claims data bank from Medical Data Vision Co., Ltd was utilized. This administrative database for inpatients and outpatients includes approximately 4,400,000 patients diagnosed with schizophrenia, which represents approximately 3% of the total Japanese population. Data were obtained from hospital electronic information systems derived from 147 acute-phase hospitals throughout Japan. These general ward hospitals operate 40,000 beds and are registered as Diagnosis Procedure Combination (DPC) hospitals. The DPC is a diagnosis-related group (DRG)-like flat fee system introduced in 2003 for comprehensive hospitals in Japan by the Japanese Medical Care Act [29]. The time span of the analysis was from 1 July 2013 to 30 June 2015.
Study Population and Study Design
Identification of the study population was based on the International Classification of Diseases, 10th revision (ICD-10). Patients with schizophrenia (SZ) were diagnosed with ICD 10: F20x. To ensure that patients regularly visited hospitals and also to reduce potential misclassification bias, the patients included were required to receive at least one medication in category 0–5 of antipsychotic drugs (Drug category: 0—other central nervous system medications, 1—antianxiety medications, 2—anti-insomnia medications, 3—antidepressants, 4—typical antipsychotics, and 5—atypical antipsychotics). The list of medications is shown in Appendix Table 6.
Table 6.
List of anti-psychotic drugs category 0–5
| Drug category | Drug type | Form | Generic name |
|---|---|---|---|
| 4 | Oral | Oral | Clocapramine hydrochloride hydrate |
| 4 | Oral | Oral | Chlorpromazine phenolphthalein phosphate |
| 4 | Oral | Oral | Chlorpromazine hydrochloride |
| 4 | Oral | Oral | Sultopride hydrochloride |
| 4 | Oral | Oral | Sulpiride |
| 4 | Oral | Oral | Zotepine |
| 4 | Oral | Oral | Timiperone |
| 4 | Oral | Oral | Nemonapride |
| 4 | Oral | Oral | Haloperidol |
| 4 | Oral | Oral | Pipamperon hydrochloride |
| 4 | Oral | Oral | Pimozide |
| 4 | Oral | Oral | Full phenazine maleate |
| 4 | Oral | Oral | Bromperidol |
| 4 | Oral | Oral | Prochlorperazine maleate |
| 4 | Oral | Oral | Periciazine |
| 4 | Oral | Oral | Perphenazine |
| 4 | Oral | Oral | Perphenazine Fen-di-zone salt |
| 4 | Oral | Oral | Perphenazine maleate |
| 4 | Oral | Oral | Mosapramine hydrochloride |
| 4 | Oral | Oral | Reserpine |
| 4 | Oral | Oral | Levomepromazine maleate |
| 4 | LAI | Injection | Haloperidol decanoate ester |
| 4 | LAI | Injection | Full phenazine decanoate ester |
| 4 | SAI | Injection | Chlorpromazine hydrochloride |
| 4 | SAI | Injection | Sulpiride |
| 4 | SAI | Injection | Timiperone |
| 4 | SAI | Injection | Haloperidol |
| 4 | SAI | Injection | Perphenazine |
| 4 | SAI | Injection | Reserpine |
| 4 | SAI | Injection | Levomepromazine hydrochloride |
| 5 | Oral | Oral | Aripiprazole |
| 5 | Oral | Oral | Okishiperuchin |
| 5 | Oral | Oral | Olanzapine |
| 5 | Oral | Oral | Quetiapine fumarate |
| 5 | Oral | Oral | Clozapine |
| 5 | Oral | Oral | Paliperidone |
| 5 | Oral | Oral | Blonanserin |
| 5 | Oral | Oral | Perospirone hydrochloride hydrate |
| 5 | Oral | Oral | Risperidone |
| 5 | LAI | Injection | Paliperidone |
| 5 | LAI | Injection | Risperidone |
| 5 | SAI | Injection | Olanzapine |
LAI long-acting injectable antipsychotic, SAI short-acting injectable antipsychotic
Antipsychotic drugs can be used in indications other than schizophrenia such as attention-deficit hyperactivity disorder (ADHD), epilepsy, and dementia. These four sub-groups were identified based on the combination of their diagnostic codes. (Diagnoses were defined as the following: ADHD/CD (attention deficit hyperactive disorder/conduct disorder), ICD 10: F9x; Dementia/Delirium, ICD 10: F0x, G30x, G31x, G10x, G20x, B220, E756; Epilepsy, ICD 10: G40x, G41x, G09x, I694, O993.)
The study population is described in Fig. 1. True schizophrenia patients were defined as patients who had only a schizophrenia diagnosis during the study period without a co-diagnosis of any combination with ADHD/CD, dementia/delirium, or epilepsy. Patients selected were those who had treatment during first 6 months (1 July 2013 to 31 December 2013) and last 6 months (1 January 2015 to 30 June 2015). Patients classified within the LAI group had at least one administration during the study period. The oral AP group was defined as patients without any LAI prescription during the study period.
Fig. 1.
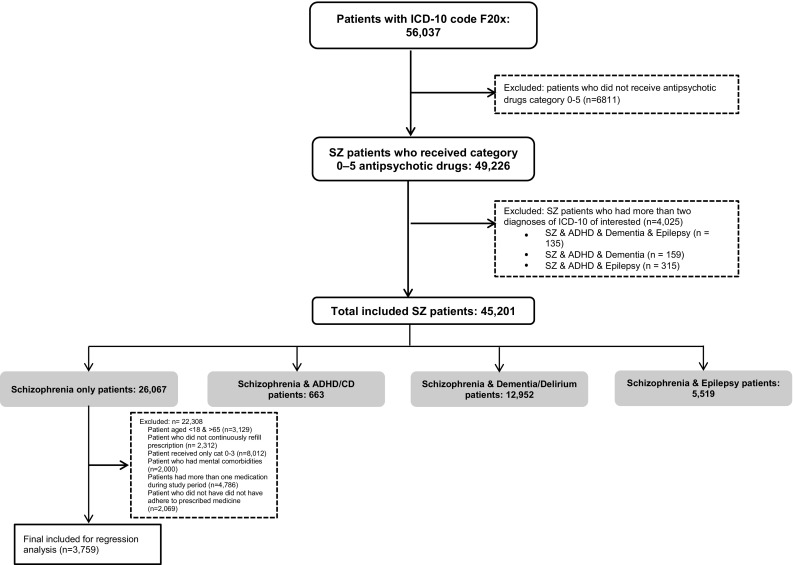
Study population. ICD10 International Classification of diseases, 10th revision, SZ schizophrenia patients, ADHD attention-deficit/hyperactivity disorder, CD conduct disorder
The patient population is described by the following baseline characteristics: age, gender, main co-morbidities, psychiatric co-morbidities, and Charlson Co-morbidity Index (CCI) scores. The ICD-10 coding algorithm for CCIs has been made available by Quan et al. [30]. The CCI includes 17 categories of co-morbidities (myocardial infarction, congestive heart failure, peripheral vascular disease, cerebrovascular disease, dementia, chronic pulmonary disease, rheumatic disease, peptic ulcer disease, mild liver disease, diabetes without chronic complication, diabetes with chronic complication, hemiplegia or paraplegia, renal disease, tumors including lymphoma and leukemia but excepting malignant neoplasms of the skin, moderate or severe liver disease, metastatic solid tumors, and AIDS/HIV) and assigns a weight between 1 and 6 for each of those co-morbidities. A higher CCI indicates a greater patient morbidity. Severity of co-morbidity was categorized into three grades: mild, with CCI scores of ≤2, moderate, with CCI scores of 3–5; and severe, with CCI scores ≥5.
The final patient subgroups for regression analysis that studies the relationship between medication type and outcomes were further selected for true schizophrenia patients aged between 18 and 65 years with continuous visits and without baseline mental co-morbidities as shown in Fig. 1. This population includes 3759 patients. The reason for excluding patients with these co-morbidities in the final analysis is that anecdotal evidence suggests that in those indications a schizophrenia diagnosis is just coded to justify the prescription of antipsychotics that were otherwise prescribed off label. These conditions may have similar symptoms to schizophrenia, which may be treated by antipsychotics. While this cannot be confirmed in claims data, we performed the analysis for conservative estimates.
Patients who did not continuously refill prescriptions were also excluded in the regression analysis to make sure that only those patients who were fully adherent to their medication regimen were compared. To impose this selection criterion, the “Medication Possession Ratio” (MPR) was calculated as the number of days’ supply of medication divided by the number of days the patient was in the database. Only those patients with an MPR of ≥1 were included for the final regression analysis.
Study Outcomes
We used two primary outcome measures: (i) the number of re-hospitalizations defined as re-admission to a hospital within 30 days of discharge, and (ii) the number of emergency room (ER) visits defined as the number of ER visits during the study period from 1 July 2013 to 30 June 2015. As secondary endpoints, we collected data on (iii) lengths of stay as defined by the number of days that patients stay in the hospital ward due to all-cause diagnosis, and (iv) number of outpatient doctor’s office (OPD) visits.
Statistical Analysis
The descriptive statistics were tabulated using either the Chi square test or ANOVA to test for significant differences across patient groups. A P value of 0.05 was considered significant. To minimize potential confounders in the regression analysis, each patient in the LAI group was matched with three unique patients in the oral AP group, using propensity score weights as a matching method for age, gender, and CCI scores. Poisson regression was used to examine the association of the use of LAI compared to only oral medication with the outcomes of interest, respectively. Poisson regression is indicated for analyzing count data [31]. The coefficients of the Poisson regression can be exponentiated to express an incidence rate ratio (IRR). The IRR is the ratio of two incidence rates (LAI and oral medication). Further, we performed subgroup analysis for atypical versus typical LAI within the true schizophrenia population. Conditional Poisson regression was used for adjusted analysis.
Results
Patient Characteristics
A total of 45,201 schizophrenia patients were identified and included in the analysis. A total of 26,067 (58%) were diagnosed with schizophrenia only (i.e., without one of the pre-specified co-diagnoses with ADHD, dementia/delirium, or epilepsy) (Table 1) and 28.7% (n = 12,952) of all patients with schizophrenia diagnoses had a co-diagnosis of dementia/delirium. Of the patients, 1.5% (n = 663) had an ADHD co-diagnosis, and 12.2% (n = 5519) had a co-diagnosis of epilepsy.
Table 1.
Patient characteristics
| Characteristics | All patients | Schizophrenia only | Schizophrenia and ADHD/CD | Schizophrenia and dementia/delirium | Schizophrenia and epilepsy | P value |
|---|---|---|---|---|---|---|
| Number of patients | 45,201 | 26,067 | 663 | 12,952 | 5519 | |
| Age (years, mean ± SD) | 63.83 ± 20.44 | 61.91 ± 19.56 | 24.30 ± 21.15 | 75.12 ± 15.02 | 51.17 ± 19.13 | <0.001 |
| ≤20 | 1632 (4) | 785 (3) | 430 (65) | 62 (1) | 355 (6) | |
| 21–40 | 5341 (12) | 3434 (13) | 77 (12) | 528 (4) | 1302 (24) | |
| 41–60 | 9730 (22) | 6493 (25) | 87 (13) | 1209 (9) | 1941 (35) | |
| 61–80 | 17,659 (39) | 10,581 (41) | 62 (9) | 5426 (42) | 1590 (29) | |
| >80 | 10,839 (24) | 4774 (18) | 7 (1) | 5727 (44) | 331 (6) | |
| Gender | <0.001 | |||||
| Male | 24,067 (49) | 12,954 (50) | 457 (69) | 5853 (45) | 2780 (50) | |
| Female | 25,159 (51) | 13,113 (50) | 206 (31) | 7099 (55) | 2739 (50) | |
| CCI score (mean ± SD) | 1.89 ± 1.65 | 2.01 ± 1.76 | 1.62 ± 1.46 | 1.78 ± 1.5 | 1.75 ± 1.54 | <0.001 |
| ≤2 | 10,124 (82) | 5185 (80) | 54 (89) | 3772 (84) | 1113 (84) | |
| 3–5 | 1475 (12) | 809 (12) | 3 (5) | 526 (12) | 137 (10) | |
| >5 | 798 (6) | 520 (8) | 4 (7) | 204 (5) | 70 (5) | |
| Co-morbidities | ||||||
| Liver disease | 4126 (9) | 2376 (9) | 35 (5) | 1094 (8) | 621 (11) | <0.001 |
| Chronic pulmonary disease | 2323 (5) | 1275 (5) | 14 (2) | 695 (5) | 339 (6) | <0.001 |
| Diabetes without complications | 2462 (5) | 1468 (6) | 7 (1) | 786 (6) | 201 (4) | <0.001 |
| Diabetes with complications | 1675 (4) | 894 (3) | 4 (1) | 607 (5) | 170 (3) | <0.001 |
| Renal disease | 888 (2) | 482 (2) | 1 (0.2) | 333 (3) | 72 (1) | <0.001 |
| Mental co-morbidities | ||||||
| Depression | 7773 (17) | 4208 (16) | 80 (12) | 1956 (15) | 1529 (28) | <0.001 |
| Epilepsy, recurrent seizure | 3606 (8) | 0 | 0 | 0 | 3606 (65) | <0.001 |
| Anxiety disorder | 3349 (7) | 1923 (7) | 39 (6) | 716 (6) | 671 (12) | <0.001 |
| Dysthymia | 732 (2) | 391 (2) | 17 (3) | 152 (1) | 172 (3) | <0.001 |
| Alcohol dependence | 488 (1) | 280 (1) | 4 (1) | 111 (1) | 93 (2) | <0.001 |
Values are expressed as n (%) unless specified otherwise. P values show the difference between the four groups (schizophrenia only, schizophrenia and ADHD/CD, schizophrenia and dementia/delirium, and schizophrenia and epilepsy)
SD standard deviation, ADHD attention-deficit/hyperactivity disorder, CD conduct disorder, CCI Charlson co-morbidity index
The average age of the schizophrenia only population that was included in the study was 61.9 years, which was relatively old. Age, gender, and mean CCI score distribution differed across subgroups. Within the subgroup for ADHD/CD, 65% were patients under the age of 20 years. Similarly, in the dementia or delirium and schizophrenia sub-group, 86% of the patients were over the age of 60 years. The gender distribution was markedly different for the ADHD/CD subgroup, which was predominantly male (n = 457, 69%). Liver disease was the most common co-morbidity across the four groups at 9, 5, 8, and 11% for true schizophrenia, ADHD/CD, dementia/delirium, and epilepsy groups, respectively. The baseline prevalence within the most frequent somatic and psychiatric co-morbidity categories also differed across subgroups. The epilepsy subgroup had the highest prevalence of liver disease (n = 621; 11%) and chronic pulmonary disease (n = 339, 6%) as well as the most commonly reported mental disease co-morbidities such as depression (n = 1529, 28%) and anxiety disorder (n = 671, 12%). The dementia subgroup had the highest prevalence of diabetes (n = 1386, 11%) among the four groups. Renal disease was shown as one of the most common co-morbidities at 3% (n = 333) among dementia/delirium patients.
Resource Utilization and Medication
Table 2 shows that the epilepsy subgroup had the highest mean number of outpatient physician visits (28.15 ± 34.25) and number of ER visits (1.41 ± 0.88). This subgroup also had the highest percentage usage of oral typical APs as well as all other medication categories (antianxiety, anti-insomnia, antidepressants, and other). The number of hospitalizations was greatest among the schizophrenia-only subgroup (2.14 ± 2.23).
Table 2.
Healthcare utilization and medication use for each group
| Characteristics | All patients | Schizophrenia only | Schizophrenia and ADHD/CD | Schizophrenia and dementia/delirium | Schizophrenia and epilepsy | P value |
|---|---|---|---|---|---|---|
| Number of OPD visits | <0.001 | |||||
| Mean ± SD | 21.89 ± 29.34 | 21.56 ± 28.60 | 18.93 ± 15.41 | 19.89 ± 28.65 | 28.15 ± 34.25 | |
| Median (IQR) | 15 (6–28) | 15 (6–28) | 16 (9–25) | 13 (5–26) | 22 (11–34) | |
| Number of hospitalizations | <0.001 | |||||
| Mean ± SD | 2.03 ± 2.00 | 2.14 ± 2.23 | 1.76 ± 1.37 | 1.83 ± 1.52 | 2.02 ± 1.91 | |
| Median (IQR) | 1 (1–2) | 1 (1–2) | 1 (1–2) | 1 (1–2) | 1 (1–2) | |
| Length of stay, days | <0.001 | |||||
| Mean ± SD | 27.70 ± 34.80 | 25.12 ± 31.35 | 33.38 ± 58.99 | 32.67 ± 38.95 | 29.40 ± 39.66 | |
| Median (IQR) | 16 (8–34) | 15 (7–31) | 13 (5–40) | 20 (10–41) | 17 (8–36) | |
| Number of ER visits | < 0.001 | |||||
| Mean ± SD | 1.33 ± 0.75 | 1.30 ± 0.73 | 1.28 ± 0.66 | 1.36 ± 0.73 | 1.41 ± 0.88 | |
| Median (IQR) | 1 (1–1) | 1 (1–1) | 1 (1–1) | 1 (1–2) | 1 (1–2) | |
| Medication used | ||||||
| Category 0: Other | 316 (1) | 226 (1) | 1 (0) | 40 (0) | 49 (1) | <0.001 |
| Category 1: Anti-anxiety medications | 20,942 (46) | 12,477 (48) | 169 (25) | 5145 (40) | 3151 (57) | |
| Category 2: Anti-insomnia medications | 28,744 (64) | 16,332 (63) | 201 (30) | 8252 (64) | 3959 (72) | <0.001 |
| Category 3: Antidepressants | 10,592 (23) | 5835 (22) | 127 (19) | 2888 (22) | 1742 (32) | <0.001 |
| Category 4: Typical antipsychotics | <0.001 | |||||
| Oral form | 14,853 (33) | 9417 (36) | 139 (21) | 3101 (24) | 2196 (40) | |
| LAI | 291 (1) | 170 (1) | 1 (0) | 62 (1) | 58 (1) | |
| SAI | 9332 (21) | 5362 (21) | 27 (4) | 3236 (25) | 707 (13) | |
| Category 5: Atypical antipsychotics | <0.001 | |||||
| Oral form | 32,451 (72) | 17,085 (66) | 574 (87) | 10,678 (82) | 4114 (75) | |
| LAI | 150 (0.3) | 79 (0) | 1 (0) | 34 (0) | 36 (1) | |
| SAI | 77 (0.2) | 40 (0) | 0 | 17 (0) | 20 (0) |
Values are expressed as n (%) unless specified otherwise. P values show the difference between the four groups (schizophrenia only, schizophrenia and ADHD/CD, schizophrenia and dementia/delirium, and schizophrenia and epilepsy)
SD standard deviation, ADHD attention-deficit/hyperactivity disorder, CD conduct disorder, IQR interquartile range, OPD outpatient department, LAI long-acting injectable antipsychotic, SAI short-acting injectable antipsychotic
Regression Analysis
Tables 3 and 4 show the patient characteristics of the schizophrenia patients receiving oral APs compared to LAIs and typical LAIs compared to atypical LAIs before and after matching applied, respectively.
Table 3.
Comparison of patient characteristics of true schizophrenia patients between patients receiving oral and LAIs before and after matching
| Characteristic | All patients | Before matching | All patients | After matching | P value | ||
|---|---|---|---|---|---|---|---|
| Oral | LAI | Oral | LAI | ||||
| Total number of patients | 3759 | 3625 (96) | 134 (4) | 536 | 402 (75) | 134 (25) | |
| Age, years (mean ± SD) | 46.58 ± 11.97 | 46.54 ± 11.98 | 47.72 ± 11.56 | 48.28 ± 11.28 | 48.47 ± 11.20 | 47.72 ± 11.56 | 0.597 |
| Gender | 0.517 | ||||||
| Female | 1987 (53) | 1925 (53) | 62 (46) | 261 (49) | 199 (49) | 62 (46) | |
| Male | 1772 (47) | 1700 (47) | 72 (54) | 275 (51) | 203 (51) | 72 (54) | |
| CCI score (mean ± SD) | 0.26 ± 0.81 | 0.26 ± 0.81 | 0.22 ± 0.57 | 0.18 ± 0.50 | 0.16 ± 0.48 | 0.22 ± 0.57 | 0.217 |
| ≤1 | 3588 (95) | 3460 (95) | 128 (95) | 520 (97) | 392 (97) | 128 (96) | |
| 1–3 | 134 (4) | 128 (4) | 6 (5) | 15 (3) | 9 (3) | 6 (5) | |
| >3 | 37 (1) | 37 (1) | 0(0) | 1 (0) | 1 (0) | 0 (0) | |
| Co-morbidities | |||||||
| Liver disease | 379 (10) | 362 (10) | 17 (13) | 59 (11) | 42 (10) | 17 (13) | 0.473 |
| Chronic pulmonary disease | 80 (2) | 78 (2) | 2 (1) | 5 (1) | 3 (1) | 2 (1) | 0.436 |
| Diabetes without complications | 59 (2) | 57 (2) | 2 (1) | 4 (1) | 2 (1) | 2 (1) | 0.246 |
| Diabetes with complications | 61 (2) | 66 (2) | 3 (2) | 8 (1) | 5 (1) | 3 (2) | 0.411 |
| Re-hospitalization | |||||||
| Readmission patient | 1001 (26) | 989 (27) | 13 (8) | 60 (11) | 47 (12) | 13 (8) | |
| Number of re-hospitalizations (mean ± SD) | 0.37 ± 1.43 | 0.63 ± 1.92 | 0.10 ± 0.25 | 0.19 ± 0.57 | 0.22 ± 0.61 | 0.10 ± 0.25 | 0.022 |
| ER visit | |||||||
| Patient visits ER | 1025 (27) | 1006 (28) | 19 (14) | 82 (15) | 63 (16) | 19 (14) | |
| Number of ER visits (mean ± SD) | 0.36 ± 0.70 | 0.34 ± 0.70 | 0.13 ± 0.42 | 0.23 ± 0.59 | 0.25 ± 0.63 | 0.13 ± 0.42 | 0.045 |
Values are expressed as n (%) unless specified otherwise
LAI long-acting injectable antipsychotic, SD standard deviation, CCI Charlson Co-morbidity Index, ER emergency visit
Table 4.
Comparison of characteristics of patients receiving typical LAIs and atypical LAIs before and after matching
| Characteristics | All patients | Before matching | All patients | After matching | P value | ||
|---|---|---|---|---|---|---|---|
| Typical LAIs | Atypical LAIs | Typical LAIs | Atypical LAIs | ||||
| Total number of patients | 134 | 100 | 34 | 102 | 68 | 34 | |
| Age, years (mean ± SD) | 47.72 ± 11.55 | 49.59 ± 10.79 | 42.23 ± 12.13 | 43.02 ± 12.12 | 43.43 + 12.19 | 42.23 ± 12.13 | 0.642 |
| Gender | 0.884 | ||||||
| Female | 62 (46) | 50 (50) | 12 (35) | 37 (36) | 25 (37) | 12 (35) | |
| Male | 72 (54) | 50 (50) | 22 (65) | 65 (64) | 43 (63) | 22 (65) | |
| CCI score (mean ± SD) | 0.22 ± 0.57 | 0.23 ± 0.60 | 0.20 ± 0.47 | 0.16 ± 0.46 | 0.13 ± 0.45 | 0.20 ± 0.47 | 0.451 |
| <1 | 128 (95) | 95 (95) | 33 (97) | 100 (98) | 67 (99) | 33 (97) | |
| 1–3 | 6 (5) | 5 (5) | 1 (3) | 2 (2) | 1 (1) | 1 (3) | |
| >3 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Co-morbidities | |||||||
| Liver disease | 17 (13) | 13 (13) | 4 (12) | 10 (10) | 6 (9) | 4 (12) | 0.638 |
| Chronic pulmonary disease | 2 (1) | 2 (2) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Diabetes without complications | 2 (1) | 1 (1) | 1 (3) | 1 (1) | 0 (0) | 1 (3) | 0.155 |
| Diabetes with complications | 3 (2) | 2 (2) | 1 (3) | 2 (2) | 1 (1) | 1 (3) | 0.614 |
| Re-hospitalization | |||||||
| Readmission patient | 13 (10) | 11 (11) | 2 (6) | 8 (8) | 6 (9) | 2 (6) | 0.602 |
| Number of re-hospitalizations (mean ± SD) | 0.18 ± 1.24 | 0.23 ± 0.11 | 0.09 ± 0.29 | 0.17 ± 0.50 | 0.22 ± 0.57 | 0.09 ± 0.29 | 0.205 |
| ER visit | |||||||
| Patient visits ER | 18 (13) | 14 (14) | 4 (12) | 13 (13) | 9 (13) | 4 (12) | 0.834 |
| Number of ER visits (mean ± SD) | 0.19 ± 0.67 | 0.23 ± 0.34 | 0.12 ± 0.33 | 0.19 ± 0.50 | 0.22 ± 0.57 | 0.12 ± 0.33 | 0.331 |
Values are expressed as n (%) unless specified otherwise
LAI long-acting injectable antipsychotic, SD standard deviation, CCI Charlson Co-morbidity Index, ER emergency visit
Table 5 reports the regression results of the conditional Poisson model with adjusted coefficients. Across all categories, the incidences of both re-hospitalization and ER visits were significantly lower among patients who had an LAI prescription compared to patients prescribed only oral APs (IRR = 0.38, 95% CI 0.17–0.74; IRR = 0.56, 95% CI 0.34–0.91). Although patients on atypical LAIs exhibited a reduced re-hospitalization or ER visit rate in comparison to patients on typical LAIs, no statistical significance was detected (IRR = 0.40, 95% CI 0.11–1.38; IRR = 0.53, 95% CI 0.18–1.61).
Table 5.
Association between LAI used in re-hospitalization and ER visits (conditional Poisson regression)
| Characteristic | LAI vs. oral IRR (95% CI) | Atypical LAI vs. typical LAI IRR (95% CI) |
|---|---|---|
| Re-hospitalization | 0.38 (0.17–0.74) | 0.40 (0.11–1.38) |
| ER visit | 0.56 (0.34–0.91) | 0.53 (0.18–1.61) |
LAI long-acting injectable antipsychotic, IRR incidence rate ratio, CI confidence interval, ER emergency
Discussion
One of the major study findings is the high percentage of schizophrenia patients with a co-diagnosis of dementia and epilepsy. We are not able to tell if patients with those co-diagnoses are really suffering from schizophrenia or whether patients were just diagnosed with schizophrenia in order to prescribe off-label antipsychotic medications, which is apparently very common [32]. With regard to dementia/delirium, a total of 28.7% of all patients with schizophrenia diagnoses had this co-diagnosis, although large-scale meta-analyses of clinical trials in other countries have demonstrated an increased risk of mortality with the use of antipsychotics in dementia [33–35]. However, their use is very common in practice for treating neuropsychiatric symptoms of dementia such as delusions, depression, or agitation [36, 37]. In Japan, previous studies have observed a high utilization of antipsychotics in the elderly with Alzheimer disease [38], and it is estimated that around 18% of patients with Alzheimer disease in Japan receive antipsychotics [39].
Within this elderly population, LAIs are slightly more common than in the overall population. However, the market share is still low. It has been suggested that for patients who will not or cannot take oral medications on a regular daily basis or have other characteristics, such as memory, vision, or auditory impairment, which contribute to partial compliance, LAI medication offers a solution [40]. However, their use in the dementia population is disturbing because it is not evidence based and also not recommended by clinical experts [41]. The study identified 12.2% co-diagnosed patients with epilepsy. It has been suggested that antipsychotic drugs can often be used successfully and safely in patients with epilepsy to reduce the risk of seizures [42, 43]. The introduction of evidence-based medicine (EBM) in Japan has also influenced clinical guidelines for epilepsy management [44]. Cautionary use of antipsychotics in epilepsy treatment regimens has been recommended to avoid side effects, including risk of seizure aggravation, even if seizure frequency may not be affected [42].
Approximately 1.5% of the study patients had an ADHD/CD co-diagnosis. Antipsychotics in this indication are prescribed to treat psychotic, mood, and anxiety disorders that are manifested with ADHD/CD [45, 46]. A Japanese study of 337 patients with ADHD/CD reported that 80 (23.7%) received antipsychotic medications [47]. ADHD/CD diagnoses utilized in this study were age dependent for childhood or adolescence, and the condition is associated with symptoms that are possibly similar to those in schizophrenia.
With co-morbidities other than ADHD, dementia/delirium, or epilepsy, this study found a high prevalence of diseases of hepatorenal function or diabetes that reflect the high incidence of metabolic diseases associated with schizophrenia. Although information about smoking status was not available, prevalence of chronic pulmonary disease suggests concern for smokers among patients independent of other factors such as genetics or pollution.
The second major finding was that among those patients diagnosed with schizophrenia only, the utilization of LAIs is associated with better outcomes. Our analysis suggests that there was a significant decrease in re-hospitalizations in the LAI group of −62% (adjusted) (Table 5). Those results are consistent with international findings. For instance, a meta-analysis by the UK National Institute for Health and Care Excellence (NICE) found annual relapse rates of 33.20% for conventional oral antipsychotics [48]. LAIs, on the other hand, are associated with relapse rates of 14.4% for risperidone LAI [49], 11.5% for paliperidone LAI [50], and 10% for aripiprazole LAI [51]. This suggests a −43 to −69% reduction in relapse rates when patients are treated with an LAI instead of an oral AP. In mirror-image studies in Japan, a strong superiority for LAIs over oral APs in preventing hospitalization (risk ratio = 0.43; 95% CI 0.35–0.53) or decreasing the number of hospitalizations (risk ratio = 0.38; 95% CI 0.28–0.51) was reported [52]. The observed adjusted reduction of 62% in re-hospitalizations is relatively similar in comparison.
Reductions in ER visits were −44% adjusted for LAIs over oral APs (Table 4). Very few studies used ER visits as an outcome measure. One example is a large hospital database analysis in France, which demonstrated that relapsed patients with schizophrenia treated with atypical LAIs were associated with a 19% lower likelihood of re-hospitalizations, compared with patients receiving oral APs. Atypical LAIs were also associated with significantly lower ER (−12%) visit rates [53]. It is also worth mentioning that we did not find significant differences in the use of LAIs and oral medications with regard to patient characteristics. There were only some numerical differences that were related to the CCI. Contrary to our expectations, LAI users were slightly healthier than oral users, although LAIs are primarily used as a “last resort” medication for very severe cases [54].
Strengths and Limitations
Understanding treatment patterns that ensure treatment continuity can maximize clinical remission where patients demonstrate significantly better social functioning and quality of life [27]. This study demonstrates a greater reduction in the magnitude of hospital readmissions by LAIs, in comparison to the sole administration of oral medications. The reduction in hospital readmission or ER visit rates was not statistically significant for the comparison between atypical and typical LAIs. Decreased sample size in these subgroup analyses contributed to low confidence in the estimates that were obtained. The observation of reduced rates in hospital readmission or emergency room visits suggests improved patient well-being due to better symptom control without urgent hospital care management. Some patients have also reported a preference towards an injectable medication because of increased convenience when compared with oral antipsychotics [55]. Due to the limited duration of follow-up, the study outcomes of re-hospitalization or ER visits were defined within the study period. This results in the limitation that the direction of association for all patients may not be consistent.
A key limitation of this study is the nature of the DPC hospital designation in Japan. General wards may be operated by university hospitals, or general hospitals with a wide variety of sick bed count size and psychiatric hospitals. However, psychiatric hospitals lack general wards in hospital management due to their specialization in psychiatric care. Because these hospitals do not receive DPC assignment, the study’s data source does not include psychiatric hospital data.
General wards provide specialties that address somatic conditions, which psychiatric care wards lack. Therefore, patients at DPC hospitals may have mild symptoms compared to psychiatric hospital patients. Another possibility is that regardless of the primary psychiatric symptom severity, these patients may have severe somatic co-morbidities, for which psychiatric hospitals cannot provide adequate treatment, such as surgery. General ward hospital clinicians may also have different prescription practices or be less familiar than their psychiatric specialists with psychiatric pharmacotherapy options including LAIs.
The study results found that hospital duration is shorter than reported data for psychiatric hospitalizations. Reimbursement regulations require that general wards discharge patients within a certain duration determined by factors such as medical staff count and proportion of patients with severe conditions. This healthcare administration system effect may have truncated patient treatment follow-up time in comparison to their natural disease course.
Conclusion
This study highlights patient characteristics among those diagnosed with schizophrenia at DPC hospitals in Japan. We present a rigorous approach to identifying patients with schizophrenia. We report a high usage of antipsychotics for psychiatric conditions that overlap in specific symptoms with schizophrenia or may have no symptom specific pharmacotherapy available. Our analysis suggests a drastic decrease (62%) in re-hospitalizations in the LAI group and a 44% decline in ER visits. This is greater than the majority of previously reported studies. Further investigation is necessary in order to promote understanding of how patients may achieve the greatest benefit from different modes of pharmacotherapy.
Acknowledgements
The authors would like to express their utmost gratitude to Daisuke Sato at the Department of Systems Science, Kyoto University for his indispensable clinical insight and research guidance for this manuscript.
Appendix
See Table 6.
Compliance with Ethical Standards
Funding
This study was funded by Janssen Pharmaceutical KK.
Conflict of interest
JM, RS, and ST are employed at Janssen Pharmaceutical KK. SC, YH, and TN declared that he has no conflict of interest in this work.
Ethical approval
The study was in line with the guidelines provided by Johnson & Johnson and was approved by the Janssen Approval Committee.
References
- 1.Nakane Y, Ohta Y, Radford MH. Epidemiological studies of schizophrenia in Japan. Schizophr Bull. 1992;18(1):75–84. doi: 10.1093/schbul/18.1.75. [DOI] [PubMed] [Google Scholar]
- 2.McGrawth JJ. Variations in the incidence of schizophrenia: data versus dogma. Schizophr Bull. 2006;32(1):195–197. doi: 10.1093/schbul/sbi052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sado M, Inagaki A, Koreki A, Knapp M, Kissane LA, Mimura M, Yoshimura K. The cost of schizophrenia in Japan. Neuropsychiatr Dis Treat. 2013;9:787–798. doi: 10.2147/NDT.S41632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lin I, Muser E, Munsell M, Benson C, Menzin J. Economic impact of psychiatric relapse and recidivism among adults with schizophrenia recently released from incarceration: a Markov model analysis. J Med Econ. 2014;26:1–11. doi: 10.3111/13696998.2014.971161. [DOI] [PubMed] [Google Scholar]
- 5.Fitch K, Iwasaki K, Villa K. Resource utilization and cost in a commercially insured population with schizophrenia. Am Health Drug Benefits. 2014;7(1):18–26. [PMC free article] [PubMed] [Google Scholar]
- 6.Willis M, Svensson M, Löthgren M, Eriksson B, Berntsson A, Persson U. The impact of schizophrenia-related hospital utilization and cost of switching to long-acting risperidone injections in Sweden. Eur J Health Econ. 2010;11(6):585–594. doi: 10.1007/s10198-009-0215-9. [DOI] [PubMed] [Google Scholar]
- 7.Frey S. The economic burden of schizophrenia in Germany: a population-based retrospective cohort study using genetic matching. 2014;29(8):479–89. [DOI] [PubMed]
- 8.Kuwabara H, Saito Y, Mahlich J. Adherence and Re-hospitalizations in patients with schizophrenia: evidence from Japanese Claims Data. Neuropsychiatr Dis Treat. 2015;11:935–940. doi: 10.2147/NDT.S81677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lang K, Meyers JL, Korn JR, Lee S, Sikirica M, Crivera C, Dirani R, Menzin J. Medication adherence and hospitalization among patients with schizophrenia treated with antipsychotics. Psychiatr Serv. 2010;61(12):1239–1247. doi: 10.1176/ps.2010.61.12.1239. [DOI] [PubMed] [Google Scholar]
- 10.Tafesse E, Hines PL, Carson W. Atypical antipsychotic adherence and hospitalization in patients with schizophrenia. Schizophr Res. 2003;60:346. doi: 10.1016/S0920-9964(03)80353-5. [DOI] [Google Scholar]
- 11.Ascher-Svanum H, Zhu B, Faries D, Lacro JP, Dolder CR. A prospective study ofrisk factors for nonadherence with antipsychoticmedication in the treatment of schizophrenia. J Clin Psychiatry 67: 1114–1123. [DOI] [PubMed]
- 12.Eaddy M, Grogg A, Locklear J. Assessment of compliance with antipsychotic treatment and resource utilization in a Medicaid population. Clin Ther. 2005;27:263–272. doi: 10.1016/j.clinthera.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 13.Valenstein M, Copeland L, Blow F, McCarthy J, Zeber J, Gillon L, et al. Pharmacy data identify poorly adherent patients with schizophrenia at increased risk for admission. Med Care. 2002;40:630–639. doi: 10.1097/00005650-200208000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Ahn J, McCombs J, Jung C, Croudace T, McDonnell D, Ascher-Svanum H, et al. Classifying patients by antipsychotic adherence patterns using latent class analysis: characteristics of nonadherent groups in the California Medicaid (Medi-Cal) program. Value Health. 2008;11:48–56. doi: 10.1111/j.1524-4733.2007.00214.x. [DOI] [PubMed] [Google Scholar]
- 15.Kozma C, Weiden P. Partial compliance with antipsychotics increases mental health hospitalizations in schizophrenic patients: analysis of a national managed care database. Am Health Drug Benefits. 2009;2:31–38. [PMC free article] [PubMed] [Google Scholar]
- 16.Gilmer T, Dolder C, Lacro J, Folsom D, Lindamer L, Garcia P, et al. Adherence to treatment with antipsychotic medication and health care costs among Medicaid beneficiaries with schizophrenia. Am J Psychiatry. 2004;161:692–699. doi: 10.1176/appi.ajp.161.4.692. [DOI] [PubMed] [Google Scholar]
- 17.Morken G, Widen J, Grawe R. Nonadherence to antipsychotic medication, relapse and rehospitalisation in recent-onset schizophrenia. BMC Psychiatry. 2008;8:32. doi: 10.1186/1471-244X-8-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Knapp M, King D, Pugner K, Lapuerta P. Non-adherence to antipsychotic medication regimens: associations with resource use and costs. Br J Psychiatry. 2004;184:509–516. doi: 10.1192/bjp.184.6.509. [DOI] [PubMed] [Google Scholar]
- 19.Higashi K, Medic G, Littlewood KJ, Diez T, Granström O, De Hert M. Medication adherence in schizophrenia: factors influencing adherence and consequences of nonadherence, a systematic literature review. Ther Adv Psychopharmacol. 2013;3(4):200–218. doi: 10.1177/2045125312474019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zeidler J, Mahlich J, Greiner W, Heres S. Cost-effectiveness of paliperidone palmitate for the treatment of schizophrenia in Germany. Appl Health Econ Health Policy. 2013;11(5):509–521. doi: 10.1007/s40258-013-0050-0. [DOI] [PubMed] [Google Scholar]
- 21.Acosta FJ, Bosch E, Sarmiento G, et al. Evaluation of noncompliance in schizophrenia patients using electronic monitoring (MEMS) and its relationship to sociodemographic, clinical and psychopathological variables. Schizophr Res. 2009;107(2):213–217. doi: 10.1016/j.schres.2008.09.007. [DOI] [PubMed] [Google Scholar]
- 22.Tiihonen J, Haukka J, Taylor M, et al. A nationwide cohort study of oral and depot antipsychotics after first hospitalization for schizophrenia. Am J Psychiatry. 2011;168(6):603–609. doi: 10.1176/appi.ajp.2011.10081224. [DOI] [PubMed] [Google Scholar]
- 23.Grimaldi-Bensouda L, Rouillon F, Astruc B, et al. Does longacting injectable risperidone make a difference to the real-life treatment of schizophrenia? Results of the cohort for the general study of schizophrenia (CGS) Schizophr Res. 2012;134(2–3):187–194. doi: 10.1016/j.schres.2011.10.022. [DOI] [PubMed] [Google Scholar]
- 24.Leucht C, Heres S, Kane JM, et al. Oral versus depot antipsychotic drugs for schizophrenia—a critical systematic review and meta-analysis of randomised long-term trials. Schizophr Res. 2011;127(1–3):83–92. doi: 10.1016/j.schres.2010.11.020. [DOI] [PubMed] [Google Scholar]
- 25.Rossi G, Frediani S, Rossi R, Rossi A. Long-acting antipsychotic drugs for the treatment of schizophrenia: use in daily practice from naturalistic observations. BMC Psychiatry. 2012;12:122. doi: 10.1186/1471-244X-12-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gerlach J. Depot neuroleptics in relapse prevention: advantages and disadvantages. Int Clin Psychopharmacol. 1995;9(Suppl. 5):17–20. doi: 10.1097/00004850-199501005-00004. [DOI] [PubMed] [Google Scholar]
- 27.Brissos S, Ruiz Veguilla M, Taylor D, Balanzá-Martinez V. The role of long-acting injectable antipsychotics in schizophrenia: a critical appraisal. Ther Adv Psychopharmacol. 2014;4(5):198–219. doi: 10.1177/2045125314540297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mahlich J, Nishi M, Saito Y. Modelling the budget impact of long acting injectable paliperidone palmitate in the treatment of schizophrenia in Japan. Clin Econ Outcomes Res. 2015;7:267–272. doi: 10.2147/CEOR.S85514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang K, Li P, Chen L, Kato K, Kobayashi M, Yamauchi K. Impact of the Japanese diagnosis procedure combination-based payment system in Japan. J Med Syst. 2010;34(1):95–100. doi: 10.1007/s10916-008-9220-2. [DOI] [PubMed] [Google Scholar]
- 30.Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, Saunders LD, Beck CA, Feasby TE, Ghali WA. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 31.Winkelmann R. Econometric analysis of count data. Heidelberg: Springer; 2007. [Google Scholar]
- 32.Haw C, Stubbs J. Off-label use of antipsychotics: are we mad? Expert Opin Drug Saf. 2007;6(5):533–545. doi: 10.1517/14740338.6.5.533. [DOI] [PubMed] [Google Scholar]
- 33.Schneider LS, Dagerman K, Insel P. Risk of death with atypical antipsychotic drug treatment for dementia: meta-analysis of randomized placebo-controlled trials. JAMA. 2005;294:1934–1943. doi: 10.1001/jama.294.15.1934. [DOI] [PubMed] [Google Scholar]
- 34.Trifirò G, Spina E, Gambassi G. Use of antipsychotics in elderly patients with dementia: do atypical conventional agents have a similar safety profile? Pharmacol Res. 2009;59:1–12. doi: 10.1016/j.phrs.2008.09.017. [DOI] [PubMed] [Google Scholar]
- 35.Maust DT, Kim HM, Seyfried LS, Chiang C, Kavanagh J, Schneider LS, Kales HC. Antipsychotics, other psychotropics, and the risk of death in patients with dementia: number needed to harm. JAMA Psychiatry. 2015;72(5):438–445. doi: 10.1001/jamapsychiatry.2014.3018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jeste DV, Blazer D, Casey D, Meeks T, Salzman C, Schneider L, Tariot P, Yaffe K. ANCP White Paper: update on use of antipsychotic drugs in elderly persons with dementia. Neuropsychopharm. 2008;33:957–970. doi: 10.1038/sj.npp.1301492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Steinberg M, Lyketsos C. Atypical antipsychotic use in patients with dementia: sanaging safety concerns. Am J Psychiatry. 2012;169(9):900–906. doi: 10.1176/appi.ajp.2012.12030342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Urushihara H, Kobayashi S, Honjo Y, Kosugi S, Kawakami K. Utilization of antipsychotic drugs in elderly patients with Alzheimer’s disease seen in ambulatory practice in Japan. Sci Postprint. 2014;1(1):e00014. doi: 10.14340/spp.2014.01C0003. [DOI] [Google Scholar]
- 39.Kadohara K., Sato I, Doi Y, Arai M, Fujii Y, Matsunaga T, Kawakami K. Prescription patterns of medications for Alzheimer’s disease in Japan from 2010 to 2015: a descriptive pharmacy claims database study. Neurol Ther 2016 (ahead of print). [DOI] [PMC free article] [PubMed]
- 40.Masand PS, Gupta S. Long-acting injectable antipsychotics in the elderly: guidelines for effective use. Drugs Aging. 2003;20(15):1099–1110. doi: 10.2165/00002512-200320150-00003. [DOI] [PubMed] [Google Scholar]
- 41.Llorca PM, Abbar M, Courtet P, Guillaume S, Lancrenon S, Samalin L. Guidelines for the use and management of long-acting injectable antipsychotics in serious mental illness. BMC Psychiatry. 2013;13:340. doi: 10.1186/1471-244X-13-340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Okazaki M, Ito M, Kato M, Watanabe M, Watanabe Y, Onuma T. Effect of antipsychotics in epilepsy patients with psychiatric symptoms. Neurol Asia. 2010;15(Supplement 1):55. [Google Scholar]
- 43.Koch-Stoecker S. Antipsychotic drugs and epilepsy: indications and treatment guidelines. Epilepsia. 2002;43(Suppl. 2):19–24. doi: 10.1046/j.1528-1157.2002.043s2019.x. [DOI] [PubMed] [Google Scholar]
- 44.Tsuji S. Clinical guidelines for epilepsy. Nihon Rinsho. 2014;72(5):803–808. [PubMed] [Google Scholar]
- 45.Olfson M, Blanco C, Liu L, Moreno C, Laje G. National trends in the outpatient treatment of children and adolescents with antipsychotic drugs. Arch Gen Psychiatry. 2006;63(6):679–685. doi: 10.1001/archpsyc.63.6.679. [DOI] [PubMed] [Google Scholar]
- 46.Sohn M, Moga D, Blumenschein K, Talbert J. National trends in off-label use of atypical antipsychotics in children and adolescents in the United States. Medicine. 2016;95(23):e3784. doi: 10.1097/MD.0000000000003784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Inagaki A, Nishimura Y, Otsuka H, Hirakawa H, Hatou K, Kubota Y, Watanabe Y, Miki K, Endoh Y. Outpatient treatment of adolescents in japan with drugs for attention deficit disorders. Value Health. 2014;17(7):A455. doi: 10.1016/j.jval.2014.08.1245. [DOI] [PubMed] [Google Scholar]
- 48.National Collaborating Centre for Mental Health. Schizophrenia. The NICE Guideline on Core Interventions in the Treatment and Management of Schizophrenia in Adults in Primary and Secondary Care. London: The British Psychological Society and The Royal College of Psychiatrists; 2010.
- 49.Gaebel W, Schreiner A, Bergmans P, et al. Relapse prevention in schizophrenia and schizoaffective disorder with risperidone long-acting injectable vs quetiapine: results of a long-term, open-label, randomized clinical trial. Neuropsychopharmacology. 2010;35:2367–2377. doi: 10.1038/npp.2010.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Fu DJ, Turkoz I, Simonson BR, et al. Paliperidone palmitate once monthly reduces risk of relapse of psychotic, depressive, and manic symptoms and maintains functioning in a double-blind, randomized study of schizoaffective disorder. J Clin Psychiatry. 2015;76(3):253–262. doi: 10.4088/JCP.14m09416. [DOI] [PubMed] [Google Scholar]
- 51.Kane J, Sanchez R, Perry PP, et al. Aripiprazole intramuscular depot as maintenance treatment in patients with schizophrenia: a 52-week, multicenter, randomized, double-blind, placebo-controlled study. J Clin Psychiatry. 2012;75:617–624. doi: 10.4088/JCP.11m07530. [DOI] [PubMed] [Google Scholar]
- 52.Kishimoto T, Nitta M, Borenstein M, Kane JM, Correll CU. Long-acting injectable versus oral antipsychotics in schizophrenia: a systematic review and meta-analysis of mirror-image studies. J Clin Psychiatry. 2013;74(10):957–965. doi: 10.4088/JCP.13r08440. [DOI] [PubMed] [Google Scholar]
- 53.Lafeuille, et al. Impact of atypical long-acting injectable versus oral antipsychotics on rehospitalization rates and emergency room visits among relapsed schizophrenia patients: a retrospective database analysis. BMC Psychiatry. 2013;13:221. doi: 10.1186/1471-244X-13-221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Waddell L, Taylor M. Attitudes of patients and mental health staff to antipsychotic long-acting injections: systematic review. Br J Psychiatry. 2009;195:s43–s50. doi: 10.1192/bjp.195.52.s43. [DOI] [PubMed] [Google Scholar]
- 55.Heres S, Schmitz FS, Leucht S, Pajonk FG. The attitude of patients towards antipsychotic depot treatment. Int Clin Psychopharmacol. 2007;22(5):275–282. doi: 10.1097/YIC.0b013e3280c28424. [DOI] [PubMed] [Google Scholar]


