Abstract
Objectives
The purpose of this randomized controlled trial was to evaluate the effects of a specialized yoga program for individuals with a spinal cord injury (SCI) on pain, psychological, and mindfulness variables.
Materials and methods
Participants with SCI (n=23) were outpatients or community members affiliated with a rehabilitation hospital. Participants were randomized to an Iyengar yoga (IY; n=11) group or to a 6-week wait-list control (WLC; n=12) group. The IY group participated in a twice-weekly 6-week seated IY program; the WLC group participated in the same yoga program, after the IY group’s yoga program had ended. Pain, psychological, and mindfulness measures were collected at two time points for both groups (within 1–2 weeks before and after program 1 and at a third time point for the WLC group (within 1 week after program 2).
Results
Linear mixed-effect growth models were conducted to evaluate the main effects of group at T2 (postintervention), controlling for T1 (preintervention) scores. T2 depression scores were lower (F1,18=6.1, P<0.05) and T2 self-compassion scores higher (F1,18=6.57, P< 0.05) in the IY group compared to the WLC group. To increase sample size and power, the two groups were combined and analyzed across time by comparing pre- and postintervention scores. Main effects of time were found for depression scores, (F1,14.83=6.62, P<0.05), self-compassion, (F1,16.6=4.49, P<0.05), mindfulness (F1,16.79=5.42, P<0.05), mindful observing (F1,19.82=5.06, P<0.05), and mindful nonreactivity, (F1,16.53=4.92, P<0.05), all showing improvement after the intervention.
Discussion
The results indicated that a specialized 6-week yoga intervention reduced depressive symptoms and increased self-compassion in individuals with SCI, and may also have fostered greater mindfulness.
Keywords: spinal cord injury, Iyengar yoga, depressive symptoms, self-compassion
Introduction
Sustaining a spinal cord injury (SCI) is a life-changing experience that can result in motor, sensory, bladder, bowel, sexual, and autonomic impairments. These impairments contribute to a high number of secondary health conditions, including psychological disorders and chronic pain.1,2 Rehabilitation in the post-SCI period is often focused on physical therapies and psychological interventions to support the recovery process, which may include access to resources or services to foster physical activity and community engagement (eg, therapeutic recreation). The post-SCI period requires a reorientation to meaningful life activities and flexibility engaging with new challenges in the context of abrupt physical and emotional changes.3
Psychological distress and pain
The rates of psychological disorders (eg, major depressive disorder and generalized anxiety disorder) after SCI range from 17% to 25%, highlighting this population’s vulnerability to psychological distress,4 which is considerably higher than the general population.5,6 A longitudinal study evaluating psychological health in individuals with SCI from 12 weeks to 10 years postinjury demonstrated that the rates of anxiety and depression were relatively stable.7 Not surprisingly, the relationship between physical and mental health is correlated for individuals with SCI, such that those with higher levels of physical symptoms, such as pain or fatigue, also report greater psychological distress, such as depressive and anxiety symptoms and poorer quality of life (QoL).8–10
Eighty-one percent of individuals with SCI report chronic pain up to 5 years postinjury, which can impact physical, social, psychological, and functional facets of living.11,12 Pain in individuals who have sustained SCI is classified by the International SCI Pain Classification according to three tiers.13 The first tier classifies the type of pain (eg, nociceptive, neuropathic, or “other”), and the second tier classifies the subtype of pain. Subtypes of nociceptive pain are classified as musculoskeletal, visceral, or “other”, and subtypes of neuropathic pain are classified as “at level SCI”, “below level SCI”, and “other”. The third tier includes the primary pain source and pathology, and it is recommended to consider pain intensity also. This system parallels earlier systems that classify pain according to etiology, pathology, location, severity, and quality, and according to four dimensions: musculoskeletal, visceral, neuropathic, or “other” types, all of which significantly impact QoL.1 Pain is also classified relative to the level of the spinal injury: pain at or below the level of the injury tends to be neuropathic in nature, and depending on the completeness of the lesion may be akin to phantom pain. This pain is often referred to the lower limbs via the convergence and summation of inputs (somatic and visceral) in higher central nervous system structures. Pain above the level of the injury tends to be musculoskeletal in nature, and may arise from overuse. Musculoskeletal pain in individuals with traumatic SCI has been reported to be the most frequently reported type of pain.12
According to the fear-avoidance model of chronic pain, pain catastrophizing, pain-related fears, and pain-related anxiety all contribute to the development and maintenance of chronic pain through a network of escape and avoidance behaviors, behavioral inactivity, the deconditioning syndrome, and disability.14 Pain-related cognitions, such as pain catastrophizing, are recognized as negatively impacting pain-related experiences and functional ability in individuals with SCI.15 Both active and passive pain-related coping statements have been correlated with pain intensity and unpleasantness in individuals with SCI in a pilot, longitudinal study, and it is recommended that pain-coping styles be addressed in the rehabilitation process to tailor treatments best to different response types.16
Bolstering inner resources
Current rehabilitation models typically focus on symptom reduction or health vulnerabilities, but there is increasing recognition that augmenting inner resources, such as self-efficacy, posttraumatic growth, and resilience, may serve as a buffer from challenging experiences and/or create positive psychological change after SCI.17–20 These constructs may also function in secondary synergistic and interconnected relationships for individuals with SCI. A cross-sectional study employing a convenience population found that self-efficacy was positively correlated with resilience while in hospital and at 3 months post-SCI, and that levels of self-efficacy predicted levels of resilience while in hospital.21 Similarly, self-efficacy, as well as low levels of depressed mood, predict resilience in individuals with SCI at discharge and 6 months postdischarge from an inpatient rehabilitation setting into the community.22 It has been recommended that rehabilitation strategies enhance self-efficacy by strengthening the relationship between behaviors and perceived goals through increased self-monitoring and self-awareness.4
Posttraumatic growth refers to the profound self-transformation that can emerge from suffering, pain, and trauma, and posits that growth and adaptability can be natural consequences of traumatic experiences.23 A model examining posttraumatic growth, depression, demographics, and injury characteristics in a community-based, cross-sectional study found that most individuals with SCI experienced some experiential growth postinjury, and these authors recommended further development of conceptual models of this construct in the context of SCI.23 Also, posttraumatic growth has been associated with higher levels of psychological distress in community-based individuals with SCI, highlighting it as a potentially useful target for improving well-being in this population.7
A construct related to posttraumatic growth is resilience, which refers to adaptive coping and the ability to respond flexibly to adverse life events in a positive and growth-promoting way.24 This construct is particularly important in health conditions that can render an individual helpless or vulnerable to developing secondary psychological conditions. Resilience has been found to mediate the impact of pain on depression, such that resilience reduced the effect of pain severity on depression and was also found independently to predict both depression (negatively) and posttraumatic growth (positively).18 Latent growth mixture-modeling analysis of a longitudinal study evaluating individuals with SCI at 6 weeks, 3 months, 1 year, and 2 years found that resilient individuals had fewer SCI-related QoL problems, evaluated stressors as challenges rather than threats, had greater acceptance and did not cope by using behavioral avoidance.25 Higher levels of resilience have also been associated with higher levels of self-efficacy, internal locus of control, and lower levels of psychological distress in community-dwelling adults with SCI in a cross-sectional postal survey.17 Increasing resilience may be a useful target for rehabilitation and have secondary gains in terms of fostering positive growth post-SCI.18
Constructs embedded in third-wave therapies, such as psychological flexibility, mindfulness, and self-compassion, have origins in Buddhist and Eastern contemplative philosophies, and are being incorporated into contemporary psychological and health interventions.26–29 A common thread among these constructs is the disentanglement of pain and suffering and shared attitudes of openness, nonjudgment, and present-mindedness. Psychological flexibility is negatively associated with depression, pain-related anxiety, physical disability, and psychosocial disability in individuals undergoing interdisciplinary treatment for chronic pain.30 It has been suggested that psychological flexibility involves a willingness to experience distressing emotions or pain, rather than avoiding or “pushing up” against them, with consequent reductions in suffering and improvements in daily functioning.30 Similarly, mindfulness has been found negatively to predict pain intensity, pain catastrophizing, pain-related fear, pain hypervigilance, negative affect, and functional disability in chronic pain patients.31 The role of acceptance is an important factor in healthy psychological adaptation to SCI,32 and acceptance cognitions were associated with better mental health in a prospective study evaluating community-dwelling individuals with SCI over time.33 Self-compassion has been associated with self-efficacy and resilience in individuals with spina bifida,19 and is a significant predictor of positive and negative affect, pain catastrophizing, and pain disability in individuals with chronic pain and obesity.29 To date, there have been no studies to evaluate self-compassion or psychological flexibility in the context of a rehabilitation intervention or as theoretically relevant for an SCI population.
Yoga as a health intervention
Focus groups consisting of individuals with SCI and physicians indicate that there is a need for highly individualized treatment approaches and a desire for complementary health therapies for SCI-related pain.34 Yoga is an ancient mind–body practice dating back to 3,000 BC, and is traditionally defined as cultivating deep concentrative awareness, predominantly through the use of physical postures. The postures are a common thread through various schools of yoga, and are the primary focus in contemporary uses of yoga.35 In modern health care, yoga is gaining acclaim for improving health and well-being, and has been evaluated for both acute and chronic conditions in a variety of clinical populations.36,37 There is evidence from randomized controlled trials (RCTs) that yoga is effective in the treatment of a variety of chronic conditions as either a stand-alone treatment or as an adjuvant therapy. Yoga has been shown to be effective in reducing pain and disability for individuals with low-back pain,38 neck pain,39,40 knee and hand osteoarthritis,41,42 and rheumatic disease and fibromyalgia.43,44 RCTs have also demonstrated that yoga practice results in improvements in mental health (depression, anxiety, self-efficacy, psychological flexibility in relation to posttraumatic stress disorder, and sleep),45–47 and fatigue- and mood-related impacts in multiple sclerosis.48–50 Results from several pilot studies have shown that yoga also positively impacts other facets of psychological experiences, such as pain catastrophizing,51 self-compassion,52 and mindfulness51 in clinical and nonclinical populations.45,46,47,51–57 There is qualitative evidence for the positive impact of yoga on belongingness, sense of connectedness, self-transformation, sense of purpose, and acceptance of changes to one’s body in individuals who have sustained a stroke,58 which may be relevant to individuals with SCI who must face new limits in the context of their injury. In addition, the role of stress in the development, maintenance, and exacerbation of chronic diseases is now widely accepted, and thus lifestyle factors that remediate stress, such as yoga, are of increasing value.59
Although there is an abundance of research evaluating the impact of yoga on chronic conditions and limited mobility, there is sparse research on the use of yoga for SCI. To date, there has been only one pilot study outlining the potential benefits of a yoga intervention for individuals with SCI, in which descriptive qualitative analysis revealed that participating in a specialized 8-week yoga program provided therapeutic benefits in emotional (increased present mindedness), mental (decreased stress), and physical domains (decreased pain).60 A case report evaluating a twice-weekly, 12-week yoga intervention for an individual with SCI suggested that yoga may result in improvements in balance, strength, endurance, flexibility, posture, and functional outcomes.61 Yoga has also yielded benefits in individuals with scoliosis with respect to the degree of curvature of the spine, and there are now well-documented benefits for yoga reducing functional disability for chronic back pain.38,62 It has been suggested that Iyengar yoga (IY) be integrated into SCI rehabilitation therapies to increase physical functioning and to cultivate a positive mind–body experience.63 IY has been selected as an appropriate form of yoga for individuals with chronic conditions and mobility restrictions, as it emphasizes careful alignment of the muscles and bones in each posture, in order to execute each pose with optimum safety and awareness, and to minimize the risk of injury or strain.63,64 This type of yoga is based on the principles of precise alignment, purposeful sequencing, and specific timing to hold postures.65 Yoga programs may be easily modified for varying degrees of impairment and mobility, making yoga a highly accessible intervention for this population. The preliminary results on yoga from research trials suggest that yoga may provide therapeutic utility for individuals with SCI, but rigorous, methodologically sound RCTs are needed to evaluate the effects of yoga for this population formally.
Objectives
The purpose of this pilot randomized controlled study was to conduct an evaluation of a 6-week specialized IY program for improving psychological factors, pain and related variables, and mindfulness in individuals with SCI. The present study had one primary hypothesis and two secondary hypotheses. Firstly, participants in the IY group would demonstrate greater improvements in psychological inflexibility from pre- to postintervention compared to the wait-list control (WLC) group. Specifically, it was predicted that scores on measures evaluating psychological inflexibility at postintervention would be significantly lower in the IY group compared to the WLC group. Secondly, the IY group was expected to show greater improvements in pain and psychological measures from pre- to postintervention compared to the WLC group. Specifically, it was predicted that scores on measures evaluating self-efficacy, posttraumatic growth, resilience, mindfulness, and self-compassion would be significantly higher in the IY group compared to the WLC group at postintervention. It was predicted that scores on measures evaluating depressive symptoms and anxiety would be significantly lower in the IY group compared to the WLC group at postintervention. For participants with ongoing chronic pain, it was predicted that scores on measures evaluating pain, pain interference, and pain catastrophizing would be significantly lower in the IY group compared to the WLC group at postintervention. Thirdly, when combining the two groups we expected to see significant improvement on all measures from pre- to postintervention. Specifically, it was predicted that scores on measures evaluating psychological inflexibility, depressive symptoms, anxiety, pain, pain interference, and pain catastrophizing would be significantly lower from pre- to postintervention and scores on measures evaluating self-efficacy, posttraumatic growth, resilience, mindfulness, and self-compassion would be significantly higher from pre- to postintervention.
Materials and methods
Trial-design overview
This two group, unblinded, crossover, pilot RCT was designed in accordance with the CONSORT guidelines, approved by the research ethics boards at the University Health Network (UHN)/Toronto Rehabilitation Institute (TRI) and York University, and registered at ClinicalTrials.gov (NCT02656927). This study employed an external pilot design, in order to provide preliminary evidence on the efficacy of a yoga intervention for individuals with SCI, and to provide a foundation for a larger-scale RCT.66,67 Recruitment and retention for a previous trial evaluating yoga for individuals with SCI had low retention,60 and so this pilot study would provide information on whether it is possible to recruit and retain individuals with SCI in compliance with an RCT design. This pilot study would also describe the intervention and its implementation, as well as determine safety and tolerability.68 This RCT used a parallel design with a crossover feature, such that the WLC group received the yoga intervention after it had been provided to the IY group. The trial evaluated the effects of a specialized IY intervention versus a WLC group on psychological well-being, pain and related variables, and mindfulness factors. Participants (n=23) were randomized to one of two groups in a 1:1 ratio. Participants assigned to the modified IY (n=11) group received a twice-weekly, 6-week IY intervention; participants assigned to the 6-week WLC (n=12) group received the same 6-week IY intervention, starting the week after the IY group had completed the yoga intervention.
It has been suggested that RCTs are not always categorical according to the pragmatic–explanatory dimension, and rather fit along a continuum in order best to evaluate a specific intention or research question.69 This study sought to assess meaningfully the impact of a yoga intervention using a pragmatic design with explanatory features. Participant recruitment followed a pragmatic design, such that all participants with a broad range of SCI or SC-related conditions, irrespective of comorbidities or past compliance, were included. The active intervention adhered to explanatory models of RCTs in that the yoga program was highly specialized for individuals with SCI, was rooted in classical physical and contemplative traditions of yoga, and was taught by yoga instructors with high-level certifications. However, the WLC group received standard care if they were outpatients or no treatment if they were community members, which is consistent with a pragmatic design. Similarly, the design for data collection also used both pragmatic and explanatory factors: data collection was done via standardized questionnaires rather than administrative databases (explanatory), and qualitative interviews were used to assess meaningfully the impact of the yoga intervention (pragmatic). Extensive training was not required to administer these questionnaires (pragmatic; no biological or physiological parameters). Special strategies were not used to maintain or monitor compliance and adherence, other than attendance, which was in line with a pragmatic design. In summary, this study used primarily a pragmatic design with explanatory features to balance feasibility of testing a yoga intervention for a complex population under usual conditions in a hospital and rehabilitation setting with experimental rigor.
Participants
The RCT took place at the TRI’s UHN Lyndhurst Centre (LC) Brain and Spinal Cord Rehabilitation Program. LC staff circulated/posted flyers describing the yoga study and recruiting participants. Recruitment was also done via email, announcement board (including electronic versions, eg, postings on websites), and verbally at various interprofessional meetings. TRI staff were provided with the inclusion and exclusion criteria for participation in the study for preliminary screening. A member of the research team completed a formal screen and determined eligibility for participation for individuals (n=45) who expressed interest in participating in the study. Of the 45 participants that were recruited, only 23 were eligible and available to participate. One of these participants was not able to provide a physician’s note and so this person was excluded (n=22).
The yoga program was offered to outpatients on the waiting list for the activity room and other individuals with SCI who were connected with the LC, which included persons interacting with Spinal Cord Injury Canada (http://sci-can.ca), an SCI consumer-advocacy organization. Specific inclusion criteria for participation were the presence of an SCI or spinal-related condition (all levels of injury), being aged 18 years or older, the ability to speak and read English, ability to commit to twice-weekly 1-hour yoga classes for 6 weeks, a referral from a clinician on the interdisciplinary team (if they were an outpatient at the LC), a sitting tolerance of 1 hour, ability to participate in gentle physical activity for 1 hour, awareness of health contraindications (ability to practice safely), and provision of a note from a physician indicating that it was safe for them to participate in a physical activity intervention, such as yoga. Gentle physical activity referred to actively engaging in low-impact activity in a purposeful and careful manner. Participants were excluded if there were not medically stable, had preexisting medical contraindications (determined by physician), had cognitive limitations or language-comprehension issues that would impact participation (determined by physician), or had had regular yoga practice in the previous 6 months (approximately once per week for a minimum of 1 month). The classification of SCI was broad, and included demyelinating diseases of the central nervous system or developmental/birth insult to the SC.
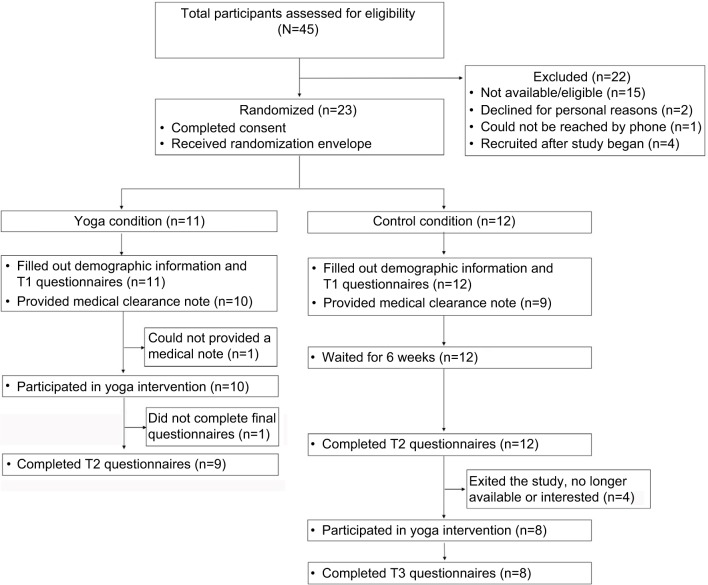
Persons who met eligibility requirements and who continued to express an interest in hearing more about the study were invited to a group-information session or to an individual meeting with a research team member (KC). Participants (n=23) were informed of the risks and benefits associated with participating in the study, and provided written, informed consent to participate. The flow of participants through the study is shown in Figure 1, and participant demographics can be seen in Table 1. Due to the small sample size, Fisher’s exact test was conducted to evaluate pretreatment differences. Ethnicity differed across the two conditions (P<0.05), but education and socioeconomic status did not. Visual inspection of the frequency data revealed that there were more participants with Caucasian heritage in the control condition, but representation of zero participants in several conditions precluded the ability to calculate odds ratios across ethnicities. Ethnicities were collapsed into Caucasian versus non-Caucasian, and Fisher’s exact test revealed a significant difference across ethnicity (P<0.05). The odds of being in the IY group were 11.67 (95% confidence interval 1.53–89.12) times higher for non-Caucasian than Caucasian participants. Injury characteristics did not differ between the groups: complete/incomplete, traumatic/atraumatic, paraplegia/tetraplegia/ambulatory, or in the use of mobility aids. The two groups did not differ in age (t12.95=−1, P>0.05), height (t20=−0.41, P>0.05), or weight (t20=−2, P>0.05).
Figure 1.
Flow of participants through the study
Table 1.
Demographics of the sample (n=22) by group
| Demographic information | Yoga group (n=10), mean (SD) | Control (n=12), mean (SD) |
|---|---|---|
| Age (years) | 47.9 (19.51) | 54.75 (10.11) |
| Height (cm) | 165.33 (6.83) | 167.43 (15.13) |
| Weight (kg) | 66.18 (10.42) | 78.43 (16.89) |
| n (%) | n (%) | |
| Injury origin | ||
| Traumatic | 7 (70) | 8 (66.7) |
| Non-traumatic | 3 (30) | 4 (33.3) |
| Completeness | ||
| Complete | 2 (20) | 5 (41.7) |
| Incomplete/disease-related | 8 (80) | 7 (58.3) |
| Level of injury | ||
| Paraplegia | 6 (60) | 4 (33.3) |
| Tetraplegia | 0 | 4 (33.3) |
| Ambulatory/unspecified | 4 (40) | 4 (33.3) |
| Mobility device | ||
| Wheelchair | 7 (70) | 7 (58.3) |
| Walker | 1 (10) | 2 (16.7) |
| Cane/poles | 2 (20) | 3 (25) |
| Race/ethnicity* | ||
| African-Canadian | 1 (10) | 0 |
| South Asian | 4 (40) | 0 |
| East Asian | 1 (10) | 1 (8.3) |
| Caucasian | 3 (30) | 10 (83.3) |
| Hispanic | 1 (10) | 0 |
| Other | 0 | 1 (8.3) |
| Annual income (CA$) | ||
| <25,000 | 6 (66.7) | 4 (36.4) |
| 25,000–39,000 | 1 (11.1) | 2 (18.2) |
| 40,000–59,000 | 1 (11.1) | 1 (9.1) |
| 60,000–100,000 | 1 (11.1) | 2 (18.2) |
| >100,000 | 0 | 2 (18.2) |
| Level of education | ||
| High school | 2 (20) | 2 (16.7) |
| University/college | 8 (80) | 9 (75) |
| Postgraduate school | 0 | 1 (8.3) |
Note:
P<0.05 (Fisher’s exact test).
Abbreviation: SD, standard deviation.
Procedure and interventions
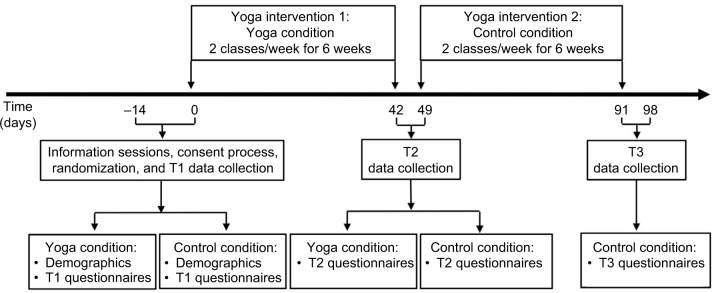
The time sequence of data collection relative to the intervention is shown in Figure 2. Data were collected at two time points for both groups and at a third for the WLC group: pre- (T1) and post- (T2) yoga intervention for the IY and WLC groups, and T3 after the WLC group had received the yoga intervention. Each assessment time point was approximately 1 hour long and occurred within 1–2 weeks of the beginning or ending of the yoga programs. Participants were provided with a questionnaire package to fill out independently at a table. A research-team member was available to answer questions. At T1, participants filled out the questionnaire package (see “Measures” section), and forms regarding demographic information (eg, ethnicity, income), SCI-related health information, medication, and a scale measuring secondary health conditions (Spinal Cord Injury Secondary Conditions Scale – modified).70,71 There were no semistructured questions. The questionnaire package took approximately 20–30 minutes to complete.
Figure 2.
Temporal sequence of the yoga interventions and data collection for both groups Iyengar yoga group
At T2, participants in the IY group had the option of remaining after the final yoga class to complete the T2 questionnaires or setting up an individual meeting with a member of the research team within the first week after the yoga program. Participants in the WLC group attended a separate T2 data-collection session or set up an individual meeting with a member of the research team. At T3, participants in the WLC group filled out the questionnaires after the final yoga class. Participants with any fine-motor difficulties were offered assistance by a member of the research team for recording their answers. All the data were deidentified, and each participant’s data was coded. Original participant names and codes were recorded in a password-protected document. All data were stored on the TRI research server, and hard-copy materials were kept in a locked cabinet at the LC.
Sample-size estimation
Sample-size estimation indicated that 24 participants (12 per group) would be required to demonstrate a moderate effect size of 0.7 in the main outcome variable (psychological inflexibility), using a type I error rate of 0.05 and a power of 0.9. Sample-size estimation was calculated using G*Power 3 (3.1.9.2; Universität Düsseldorf, Germany), based on a between-group analysis of covariance design with two groups and one covariate.
Randomization
A randomization schedule was generated (randomization.com) in advance of the study by a member of the research team, who was not directly involved with the clinical management of the participants or in the research project. Randomization was blocked according to sex, and specified the group (IY or WLC) to which each prospective participant would be allocated upon enrollment into the trial. An opaque envelope containing the participant number and group assignment was prepared, sealed, and numbered for each potential participant. This envelope was opened at the time that each participant was randomized.
Ethical considerations
Individuals with SCI represent a vulnerable population and are a relatively overresearched group. Respect for their dignity was ensured through a careful consent process and with a thorough explanation of risks and possible benefits of participation. As mentioned earlier, no special strategies were used to maintain enrollment throughout the study. Confidentiality for participant privacy and secure data storing was maintained at all phases of the research process. In order to reduce barriers to participation for low-income individuals, transport tokens were provided, which promoted values of inclusion and equality. There was no deception involved in this research project.
Iyengar yoga group
After informed, written consent to participate had been obtained, participants randomized to the IY group took part in a 6-week intervention of IY at a frequency of two 50- to 60-minute classes per week (approximately 12 hours total). The 6-week yoga intervention was held at the Therapeutic Recreation Department at the TRI/LC’s Brain and Spinal Cord Rehabilitation Program. The duration of 6 weeks, dosage of two classes a week, class length of 60 minutes and total intervention hours (12) was decided in alignment with the yoga literature,72 and participants were encouraged only to practice basic poses that had been determined safe and after they had practiced them with supervision for several classes.64 The classes were offered at no cost to the participants. The program was designed and taught by certified IY teachers, who were certified as intermediate senior 1 and intermediate junior 3 teachers of IY. Both of these certification levels are advanced, and involve multiple (two to four) trips to study at the Ramamani Iyengar Memorial Yoga Institute in Pune, India. Also, both teachers had 1) 22–26 years of teaching yoga, 2) advanced training in therapeutics of IY, 3) knowledge of yoga philosophy35 and mindfulness-based practices, and 4) experience teaching yoga to limited-mobility populations. The class structure and content was based upon a book written by one of the teachers on a major yoga-philosophy text35 and a manual previously used in a research trial evaluating yoga for individuals receiving complex care in a hospital setting.52 An LC recreation therapist was available for consultation during all the classes.
Wait-list control group
After informed, written consent to participate had been obtained, participants randomized to the WLC group received no additional treatment. They were informed that they would receive the same 6-week IY intervention after a period of 6 weeks, and should not start yoga practice while waiting for the intervention to commence.
Yoga program
The classes involved a broad and integrated approach to yoga and included breathing practices (prāṇāyāma), physical postures (āsana), yoga philosophy (jñāna), mindfulness (smṛti sādhanā), and meditation/relaxation (dhāraṇā, dhyāna) techniques. There is flexibility in the school of IY as to how the physical practices are applied (gentle versus more vigorous), and these can be easily modified according to the needs of the student. IY typically uses a variety of props as aids in performing āsanas (postures), and this intervention used blankets to accompany principles of right action and alignment, in particular with regard to posture and for the action of lifting the chest. The emphasis on self-development and awareness is inextricably linked with the physical āsanas, and the practice is conceptualized as a transformative process for mental, physical, and spiritual health, with consequent gains in energy and vitality.73
Each class opened with a brief philosophy concept (~5 minutes, see Table 2), which was based on relevant contemplative and reflective practices from Patañjali Yoga Sūtras that focused on self-study, personal development, observances, ethical discipline, and attitudes of acceptance, among others.35 This was followed by a concentration practice (dhāraṇā), with breathing, mindfulness, and relaxation components (~10–15 minutes). The āsana practice (~20–30 minutes) focused on upper-body postures that were sequenced in a purposeful way to build on awareness and actions learned in previous poses. The sequences consisted of preparatory arm work, ūrdhva hastāsana (single arm and both arms), baddhanguliyāsana, garuḍāsana, hastāsana with arms out to the side, gentle twist to either side, and neck stretch to either side and forward, using baddhanguliyāsana bound fingers. In addition, breath–movement coordination was used to transition between poses and to encourage sustained inward focus. There was a focus in each class on the principles of lifting the heart/chest, centering the head over the spine, and creating space in the spinal vertebrae. Repetition was emphasized so that participants could learn the sequence by the end of the study. Participants who required hands-on assistance were attended to by a yoga teacher. Participants were encouraged to push gently the edge of comfort and actively engage their muscles to build strength and flexibility, while also practicing safely within personal limits with respect to pain and fatigue. Safe variations or modifications were provided to participants with more limited arm movement, so that they could participate in all parts of the āsana portion of the class. One participant with tetraplegia used a table for support in some āsanas. Finally, the class ended with another concentration (dhāraṇā, dhyāna) component, with used principles of mindfulness (smṛti sādhanā), breath awareness (prāṇāyāma), philosophy (jñāna), or imagery.
Table 2.
Yoga philosophy concepts by class
| Class | Concept | Explanation |
|---|---|---|
| 1 | Witness consciousness and ahimsā (nonviolence); Sūtra 2.35 | Practicing “being with” challenging experiences without pushing them away or clinging to personal narratives. Practicing in a way that is safe and supportive. Doing without over- or underdoing. Using the right amount of effort for growth. |
| 2 | Abhyāsa (repeated practice); Sūtra 1.12 | The important of repeating practice to yield benefits in the mind and body. |
| 3 | Satya (truthfulness); Sūtra 2.36 | Honestly examining one’s experience to better understand one’s “starting point” and using yoga practice as a springboard for positive change. |
| 4 | Concept review: ahimsā, abhyāsa, satya; Sūtras 1.12, 2.35, 2.36 | Review and integration of preliminary concepts and emphasis of self as a friend and the use of compassion in practice. |
| 5 | Breath awareness to balance the nervous system and calm the mind; Sūtra 1.34 | Pain management through relaxation, training the attention to see tension patterns in the body, using imagery and visualization. |
| 6 | Sthira sukham āsanam; Sūtra 2.46 | Finding a balance between steadiness/stability/effort with ease/joy/relaxation. Link to teaching on ahimsā and dosing of effort in activity and rest. |
| 7 | Ekā gra (one pointed concentration); Sūtra 1.32 | Training attention and concentration by returning to a point of focus repeatedly, with a calming effect on the mind. |
| 8 | Meditation for relaxation, contemplation on the heart; Sūtra 1.36 | The heart as a resource, refuge, and source of inner luminosity. |
| 9 | Review of Ekā gra and breath as nourishment; Sūtras 1.32, 1.34 | Tying together concepts from previous classes regarding one pointed focus and the breath as calming and revitalizing. Training attention to return to the breath repeatedly, as a way to regulate the body–mind. |
| 10 | Aparigraha and santoṣa; Sūtras 2.39, 2.42 | Effort to make positive change in the body can be helpful to move toward health, but care is needed to prevent agitation in striving/grasping. Importance of cultivating contentment (santoṣa) with current abilities/body. |
| 11 | Śodhana, śoṣana, śobhāna, śamana; Iyengar’s teaching on the four elements of practice | Śodhana, purification through active āsana to lift heavy states of body–mind; śoṣana, integration of practice, doing one’s best, which changes over time; śobhāna, excellence and auspiciousness, good intention to do practice with care and good effort, śamana, practice as a vehicle for relaxation and calmness; one should feel better after practicing. |
| 12 | Śodhana, śoṣana, śobhāna, śamana; Iyengar’s teaching on the four elements of practice and taking the practice to life | Repetition of previous class content and explaining how to work with these elements of practice individually, should participants want to keep practicing after the program is completed. |
Measures
Main outcome measure: Acceptance and Action Questionnaire
The Acceptance and Action Questionnaire (AAQ)-II is a seven-item scale that evaluates psychological inflexibility and experiential avoidance, which are constructs that are associated with acceptance and commitment therapy.74 Items are scored from 1 (never true) to 7 (always true), and total scores range from 7 to 49, with higher scores reflecting higher levels of psychological inflexibility. The AAQ-II has good internal consistency (α=0.84 [0.78–0.88]) and good temporal stability (3- and 12-month test–retest reliability, α=0.81 and 0.79, respectively). Higher levels of psychological inflexibility, as measured by the AAQ-II, are associated with higher scores on measures of depression (r=0.61–0.71), anxiety (r=0.49–0.61), stress (r=0.57), and ill health (r=0.3–0.71; good concurrent validity), and higher scores on the AAQ-II are positively associated with higher scores on a measure of thought suppression (r=0.63; good convergent validity).74
Hospital Anxiety and Depression Scale
The Hospital Anxiety and Depression Scale (HADS) is a 14-item self-report questionnaire that measures symptoms of anxiety (7 items) and depression (7 items).75 For each item, respondents are asked to select one from among four possible choices (scored from 0 to 3) that best describes how they have been feeling over the past week. The HADS yields anxiety (HADS-A) and a depression (HADS-D) subscale scores, each with a maximum total score of 21. Internal consistency for the anxiety and depression subscales showed Cronbach’s α-values of 0.8–0.93 for the HADS-A and 0.81–0.9 for the HADS-D.76,77 Concurrent validity of the HADS is very good, as measured by correlation coefficients of 0.62–0.73 for the HADS-D with various well-validated depression scales (eg, Beck Depression Inventory, Symptom Checklist 90 – depression subscale) and correlation coefficients of 0.49–0.81 for the HADS-A with various well-validated anxiety measures (eg, Spielberger State-Trait Anxiety Inventory, Symptom Checklist 90 – anxiety subscale).76,77 The scale has shown good internal consistency when used with an SCI population (Cronbach’s α=0.85 for the anxiety subscale and α=0.79 for the depression subscale), though some items present as complex in this population (eg, “I can sit at ease and feel relaxed”).78
General Self-Efficacy Scale
The General Self-Efficacy Scale (GSES) is a ten-item construct that assesses optimistic self-beliefs regarding one’s perceived ability to cope with a variety of daily hassles and stressful life events.79 Items are scored using a 4-point scale: 1 (not at all true) to 4 (exactly true). Total scores range from 10 to 40, with higher scores reflecting higher perceived self-efficacy. The GSES demonstrates high internal consistency (α=0.86), unidimensionality, and construct validity.80 It has been negatively correlated with anxiety (r=−0.42 to −0.43) and depression (r=−0.33 to −0.46) and positively correlated with optimism (r=0.52–0.6).80 The GSES has been used in the SCI population, and the construct of self-efficacy has been tied to a number of favorable outcomes post-SCI.81–84
Posttraumatic Growth Inventory
The Posttraumatic Growth Inventory – short form (PTGI-SF) is a ten-item measure evaluating posttraumatic growth, a construct involving positive adaptability and self-transformation after trauma.85 The PTGI-SF asks respondents to consider how much various facets of their experience have changed as a result of their trauma according to a 6-item Likert scale, ranging from 0 (“I did not experience this change as a result of my crisis”) to 5 (“I experienced this change to a very great degree as a result of my crisis”). Scores range from 0 to 50, and higher scores reflect higher levels of posttraumatic growth. Both the original and the SF of this scale have five factors (relating to others, new possibilities, personal strength, spiritual change, and appreciation of life), and the SF has good internal consistency (total scale coefficient α=0.89 and subscale α=0.72–0.84).85,86 The PTGI-SF has good concurrent validity; scores on the PTGI-SF are negatively correlated with scores on measures of depression and positively correlated with scores on measures of QoL and resilience.87
Connor–Davidson Resilience Scale
The Connor–Davidson Resilience Scale (CD-RISC) is a self-report measure of resilience that evaluates the ability to adapt positively to stressful situations or experiences.88 The abridged version consists of ten items (CD-RISC-10), which measure the ability to tolerate experiences of change, personal problems, illness, pressure, failure, and painful feelings. Respondents are asked to read each item and indicate the extent to which an item has been true for them over the past month using a 5-point Likert scale from 0 (not true at all) to 4 (true nearly all the time). The CD-RISC-10 has good internal consistency, with an α-coefficient of 0.85.88,89 The original demonstrates good convergent validity: scores on the CD-RISC are positively correlated with scores on a measure of hardiness (r=0.87) and negatively correlated with scores on measures of stress (r=−0.76) and vulnerability (r=−0.32).89 Scores on the CD-RISC-10 have high correlation with scores on the 25-item version (r=0.92). There is some preliminary support for construct validity for the CD-RISC-10: scores on CD-RISC-10 items have been shown to moderate the relationship between retrospective reports of childhood abuse and current psychiatric symptoms.88 The CD-RISC-10 has been used in research studies evaluating individuals with SCI.17,90
Self-Compassion Scale
The Self-Compassion Scale (SCS)-SF is a 12-item self-report questionnaire that measures levels of self-compassion or the ability to hold one’s feelings of suffering with a sense of warmth, security, or concern.91 The SCS-SF has been demonstrated to comprise a unidimensional construct of self-compassion, and has six subscales: self-kindness, self-judgment, common humanity, isolation, mindfulness, and “overidentified”. Items are answered according to the statement “How I typically act toward myself in difficult times”, and are responded to on a Likert scale of 1 (almost never) and 5 (almost always). The SCS-SF has adequate internal consistency (Cronbach’s α=≥0.86 for three different samples) and excellent correlation with the full version (r=≥0.97 for three samples). It is negatively correlated with anxiety (r=−0.49), depression (r=−0.38), and stress (r=−0.52) and is positively correlated with mindfulness (r=0.39).92 The SCS-SF is scored by calculating the mean of the 12 items (personal communication, Kristen Neff, April 19, 2016).
Five Facet Mindfulness Questionnaire
The Five Facet Mindfulness Questionnaire (FFMQ)-SF is a 24-item version of the original 39-item FFMQ, and has been validated in individuals with depression, anxiety, and fibromyalgia.93 The FFMQ-SF measures the five factors observing, describing, acting with awareness, nonjudging of inner experience, and nonreactivity to inner experience. Participants respond to each item by selecting the number that is “most generally true” of their experience, on a scale of 1 (never or rarely true) to 5 (very often or always true). Total scores range from 0 to 120, with higher scores indicating greater levels of mindfulness. Total facet scores of the FFMQ-SF are highly correlated with the original version: r=0.89, 0.89, 0.92, 0.96, and 0.95, for observing, describing, acting with awareness, nonjudging, and nonreactivity, respectively.93 The correlation α-values are all above the defined criterion of 0.7, and all intercorrelations between facets and with other constructs are virtually the same as those derived from the FFMQ. Specifically, four subscales are negatively correlated with depression (describing, acting with awareness, nonjudging, and nonreactivity), three subscales are negatively correlated with anxiety (acting with awareness, nonjudging, and nonreactivity), and all subscales are positively correlated with psychological flexibility.93 All facets of the FFMQ-SF are sensitive to change and have moderate–large effect sizes.93
Brief Pain Inventory
The Brief Pain Inventory (BPI)-SF is a nine-item self-report questionnaire that measures various aspects of pain and pain interference with daily activities.94 In the BPI-SF, individuals are queried on pain history, asked to depict pain locations visually on a human-body diagram, and are asked to indicate best, worst, average, and current pain levels according to 11-point Likert scales, ranging from 0 (no pain) to 10 (pain as bad as you can imagine). Participants are also queried about pain medications and treatments and the perceived effectiveness of those medications. Finally, individuals respond to items regarding how pain interferes with seven domains of functioning: general activity, mood, walking ability, normal work, relationships with other people, sleep, and enjoyment of life, according to 11-point scales ranging from 0 (does not interfere) to 10 (completely interferes).
The nine items that comprise the BPI-SF show strong internal consistency (Cronbach’s α=0.85 and 0.88 for the intensity and interference scales, respectively) and adequate construct validity (scores on the interference scale correlate with other pain-disability measures), and is sensitive to treatment.95 The seven-item pain-interference subscale has been recommended for SCI, and item 9C (walking ability) should be changed to “ability to get around”, so this was done for the present study.96 The pain-interference subscale has been used in studies evaluating pain in individuals with SCI.11,97 It has excellent internal consistency (α>0.9), and is positively associated with pain intensity (r>0.6) and negatively associated with psychological distress (r>0.6).98
Pain Catastrophizing Scale
The Pain Catastrophizing Scale (PCS) is a 13-item self-report questionnaire that measures catastrophic thinking in relation to experienced or anticipated pain.99 Participants are asked to read each item and indicate the extent to which they experience certain thoughts and feelings when experiencing pain by selecting a number from 0 (not at all) to 4 (all the time). Scores range from 0 to 52, with higher scores reflecting higher levels of pain catastrophizing. The PCS yields a total score and three subscale scores assessing rumination (focus on pain sensations), magnification (exaggerating the threat value of pain sensations), and helplessness (perceiving oneself as unable to cope with pain symptoms). The PCS has high internal consistency (total PCS, α=0.87; rumination, α=0.87; magnification, α=0.66; and helplessness, α=0.78).99 It has been shown to be positively correlated with depression (r=0.26), trait anxiety (r=0.32), negative affectivity (r=0.32), and fear of pain (r=0.8).99
Data analysis
Preliminary analysis
The questionnaire data were entered and analyzed using SPSS version 23. Exploratory analysis was conducted to evaluate outliers, missing data, and assumptions of normality (kurtosis and skewness). The Shapiro–Wilk test (n=22) revealed that the assumption of normality was violated at T1 for the AAQ-II (IY), PTGI (WLC), GSES (WLC), at T2 for the AAQ-II (WLC) and HADS-D (WLC), and at T3 for the PTGI (WLC). For participants with pain (n=19 at T1, n=18 at T2, n=7 at T3), the Shapiro–Wilk test revealed that the assumption of normality was violated at T1 for the PCS (WLC) and at T3 for the BPI-4 (WLC). Visual examination of the z-scores on Q–Q plots for these scales revealed violations of normality were not extreme and that there were no outliers. Due to the robust nature of the F-test and the small sample size, transformations were not considered appropriate. Levene’s test revealed that variances were equal across conditions at T1 and T2, with the exception of the PCS at T1 and the HADS-A at T2.
Attendance
Of the 11 participants who were randomized to the IY group, 10 completed the yoga intervention (see Figure 1). One participant randomized to this condition was unable to provide a physician’s note, and was excluded. Of the 12 participants who were randomized to the WLC group, 8 actually participated in the intervention and all 8 completed it. Four participants withdrew from the study for logistical or non-study-related and illness reasons (eg, moved away, vertigo). Of the eligible participants, 100% who were randomized to the IY group and 66.67% who were randomized to the WLC group completed the study. The mean (± standard deviation) number of yoga classes attended for participants in the IY group was 10±1.83 (of 12 classes). The mean (± standard deviation) number of yoga classes attended for participants in the WLC group was 9.25±1.83 (of 12 classes). There were no adverse events reported.
Results
Between-group linear mixed-effect growth models
Linear mixed-effect growth models were conducted to evaluate the main effects of group at T2 after controlling for T1 scores. Two models were evaluated for each variable. The first model included fixed factors (intercept, time, condition), and the second model included these same fixed factors and also random intercepts. Consequently, each initial model had four parameters and each final model five parameters, including the residuals. The IY group had significantly lower T2 scores on the HADS-D (F1,18=6.1, P<0.05) and significantly higher T2 scores on the SCS-SF (F1,18=6.57, P<0.05) for the initial models with fixed factors. For the final models that used one random factor, the identity covariance-matrix structure was used. When random intercepts were added to the model, the model became unstable, as specified by warnings from the statistical program. As a result, the results of the models with random intercepts were not used.
Linear mixed-effect growth models: combined groups
The two groups were combined, and mixed-model analyses were conducted to evaluate differences from preintervention to postintervention. Specifically, T1 data for the IY group and T2 data from the WLC group were combined into one preintervention sample; likewise, T2 data for the IY group and T3 data for the WLC group were combined into one postintervention sample. Once the WLC and IY groups were combined, there was no longer a control group. The Shapiro–Wilk test revealed that the assumption of normality was violated at T1 for the HADS-D.
Linear mixed-effect growth models were conducted to evaluate the main effects of time (T1, T2) for each dependent variable. Two models were evaluated for each variable: the first included fixed factors (intercept, time), and the second included the same fixed factors and also random intercepts. Consequently, each initial model had three parameters and each final model four parameters, including the residuals. The identity covariance-matrix structure was used for the final models that used one random effect. The χ2 test was used to evaluate the change in −2LL values across the initial (fixed factors) and final (fixed factors and random intercepts) models to determine if the model was improved by adding the random factor and to determine the significance of random effects. Participants who reported having no chronic pain or musculoskeletal pain on the SCS (score of 0) and who reported zero levels of pain on the BPI (n=3) were excluded from the mixed-model analyses conducted for pain and related variables.
The results of the fixed-factor models revealed that postintervention HADS-D scores were significantly lower than at preintervention, (F1,37=4.22, P<0.05), with time predicting HADS-D scores (b=−1.9, t37=−2.06; P<0.05). There was a trend for FFMQ-SF – total scores (F1,37=2.98, P=0.09) and FFMQ-SF – observing scores (F1,37=3.65, P=0.06) to improve from preintervention to postintervention. When random intercepts were added to the models, the models improved and random intercepts varied for all variables, except the observing and acting with awareness subscales of the FFMQ-SF and the magnification subscale of the PCS (see Table 3).
Table 3.
Variance across intercepts and change in −2LL for the combined groups
| Measure | Var(U0j) | Δ–2LL, χ2 |
|---|---|---|
| AAQ-II | 72.16* | 10.67* |
| HADS-A | 24.76* | 28.26* |
| HADS-D | 6.7* | 7.72* |
| GSES | 10.25* | 12.1* |
| PTGI-SF | 127.98* | 26.78* |
| CD-RISC-10 | 28.21* | 8.12* |
| SCS-SF | 0.36* | 10.26* |
| FFMQ-SF – total | 84.68* | 9.57* |
| FFMQ-SF – describing | 16.93* | 14.59* |
| FFMQ-SF – observing | 1.9 | 0.93 |
| FFMQ-SF – acting with awareness | 4.4 | 1.95 |
| FFMQ-SF – nonreactivity | 9.87* | 10.25* |
| FFMQ-SF – nonjudging | 14.65* | 12.57* |
| BPI-SF – worst pain | 4.79* | 8.15* |
| BPI-SF – least pain | 4.52* | 23.32* |
| BPI-SF – average pain | 3.67* | 16.48* |
| BPI-SF – pain right now | 6.42* | 17.15* |
| BPI-SF – pain interference | 316.4* | 12.42* |
| PCS – total | 146.02* | 9.88* |
| PCS – magnification | 6.32 | 3.58 |
| PCS – helplessness | 33.88* | 12.79* |
| PCS – rumination | 17.62* | 13.32* |
Note:
P<0.05.
Abbreviations: AAQ-II, Acceptance and Action Questionnaire; HADS-A, Hospital Anxiety and Depression Scale – anxiety; HADS-D, HADS – depression; GSES, General Self-Efficacy Scale; PTGI-SF, Posttraumatic Growth Inventory – short form; CD-RISC-10, ten-item Connor–Davidson Resilience Scale; SCS-SF, Self Compassion Scale – short form; FFMQ-SF, Five Facet Mindfulness Questionnaire – short form; BPI-SF, Brief Pain Inventory – short form; PCS, Pain Catastrophizing Scale.
The mixed (fixed and random factors) models revealed that postintervention scores were significantly lower than preintervention scores for the HADS-D and significantly higher than preintervention scores for the SCS-SF, FFMQ-SF – total, FFMQ-SF – observing and FFMQ-SF – nonreactivity (Table 4). Time was a significant predictor for each variable. Although the model with random intercepts did not improve for the observing subscale of the FFMQ-SF, the effect of time for this subscale was significant for the fixed-factor model, and so the results from the mixed-effect model were considered appropriate for interpretation. Scores for all variables for the combined group are presented in Table 5.
Table 4.
Results from the mixed-model analysis (n=22)
| Measure | F | t | df | b |
|---|---|---|---|---|
| HADS-D | 6.62* | −2.57* | 1, 14.83 | −1.37 |
| SCS-SF | 4.49* | 2.12* | 1, 16.6 | 0.27 |
| FFMQ-SF – total | 5.42* | 2.33* | 1, 16.79 | 4.87 |
| FFMQ-SF – observing | 5.06* | 2.25* | 1, 19.82 | 1.88 |
| FFMQ-SF – nonreactivity | 4.92* | 2.22* | 1, 16.53 | 1.5 |
Note:
P<0.05
Abbreviations: HADS-D, Hospital Anxiety and Depression Scale – depression; SCS-SF, Self-Compassion Scale – short form; FFMQ-SF, Five Facet Mindfulness Questionnaire – short form.
Table 5.
Mean (SD) values for psychological, mindfulness, and pain variables pre- (n=22) and postintervention (n=17) for all participants
| Measure | Preintervention | Postintervention | P-value |
|---|---|---|---|
| AAQ-II | 17.59 (10) | 14.24 (6.09) | 0.226 |
| HADS-A | 6.64 (5.35) | 5.53 (3.37) | 0.795 |
| HADS-D | 4.95 (3.18) | 3.06 (2.36) | 0.021* |
| GSES | 34.09 (3.64) | 34.88 (3.48) | 0.551 |
| PTGI-SF | 31.45 (12.62) | 33.76 (12.15) | 0.462 |
| CD-RISC-10 | 30.73 (6.74) | 32.59 (5.59) | 0.568 |
| SCS-SF | 3.36 (0.73) | 3.71 (0.66) | 0.049* |
| FFMQ-SF – total | 82.27 (11.43) | 88.41 (10.43) | 0.033* |
| FFMQ-SF – describing | 17.82 (4.81) | 19.24 (3.95) | 0.551 |
| FFMQ-SF – observing | 14.68 (3.29) | 16.47 (2.29) | 0.036* |
| FFMQ-SF – acting with awareness | 17.82 (3.79) | 18.65 (3.6) | 0.497 |
| FFMQ-SF – nonreactivity | 15.5 (3.91) | 17.35 (3.33) | 0.041* |
| FFMQ-SF – nonjudging | 16.45 (4.66) | 16.71 (3.53) | 0.784 |
| BPI-SF – worst pain | 5.79 (2.37) | 6.14 (2.77) | 0.845 |
| BPI-SF – least pain | 2.79 (2.37) | 3.07 (2.13) | 0.528 |
| BPI-SF – average pain | 5.11 (2.13) | 5.14 (2.03) | 0.196 |
| BPI-SF – pain right now | 3.89 (2.85) | 3.79 (2.39) | 0.107 |
| BPI-SF – pain interference | 30.42 (20.54) | 28.86 (17.06) | 0.275 |
| PCS – total | 18.95 (14.97) | 14.64 (8.89) | 0.328 |
| PCS – magnification | 3.36 (3.62) | 2.79 (2.61) | 0.522 |
| PCS – helplessness | 9 (6.85) | 6.57 (4.47) | 0.191 |
| PCS – rumination | 6.32 (5.04) | 5.29 (3.36) | 0.461 |
Notes:
P<0.05. For pain variables (BPI-SF and PCS), only participants with pain were included in the analysis (preintervention, n=19; postintervention, n=14).
Abbreviations: AAQ-II, Acceptance and Action Questionnaire; HADS-A: Hospital Anxiety and Depression Scale – anxiety; HADS-D, HADS – depression; GSES, General Self-Efficacy Scale; PTGI-SF, Posttraumatic Growth Inventory – short form; CD-RISC-10, ten-item Connor–Davidson Resilience Scale; SCS-SF, Self Compassion Scale – short form; FFMQ-SF, Five Facet Mindfulness Questionnaire – short form; BPI-SF, Brief Pain Inventory – short form; PCS, Pain Catastrophizing Scale.
Discussion
The results of this RCT indicate that self-reported symptoms of depression improved and self-compassion increased in individuals with SCI who participated in a specialized 6-week yoga intervention compared to a WLC. The results also suggest that the yoga intervention increased levels of mindfulness broadly, and also for specific components of mindfulness, such as the capacity to observe and not react to internal experience. These results do not confirm hypothesis one, but partially confirm hypotheses two and three. The yoga program was considered safe, with no reported adverse effects. All participants who began the yoga intervention completed it. Some attrition occurred at the time of randomization, with mostly logistical reasons of not being able to attend the sessions. This contrasts with our previous study, in which there was a high rate of attrition.60
The lower scores for depressive symptoms at postintervention for the IY group were consistent with improvements from other yoga trials evaluating mood for limited-mobility populations and with previously documented evidence regarding the efficacy of yoga for clinical depression, according to the Oxford Centre for Evidence-Based Medicine method of appropriateness.45 Depression was found to improve clinically in individuals with poststroke hemiparesis after participation in a 10-week yoga trial compared to no treatment controls.100 For participants with osteoarthritis, participation in a twice-weekly 8-week, “sit ‘n’ fit” yoga program resulted in improvements in depression symptoms compared to an attention control group.101 A pilot trial evaluating the utility of yoga plus intensive physical therapy for individuals with multiple sclerosis found improvements in depressive symptoms when using the same scale as the present study (HADS-D).102 In addition, a pilot RCT evaluating the impact of an innovative yoga program consisting of classical breath exercises, relaxation, and meditation for individuals with Guillain–Barré syndrome found improvements in depressive symptoms for individuals randomized to the yoga group compared to individuals receiving standard rehabilitation program, as measured by the HADS-D.103 The classification of SCI in this present study was broad and included demyelinating diseases of the central nervous system, and so the results of similar studies emphasizing the breath-exercise and meditative components of a yoga program indicate that these accessible and more subtle elements of yoga may be useful and applicable for individuals who have limited range of motion or who have had trauma to the central nervous system.
The increased levels of self-compassion postintervention indicate that individuals in the yoga condition experienced a change in psychological orientation to pain and suffering compared to the WLC group. The present finding that self-compassion increased significantly from preintervention to postintervention parallels the results from other yoga-research trials involving chronic health populations. Individuals living with an implantable cardioverter defibrillator who were randomized to a once weekly 8-week yoga intervention demonstrated increased self-compassion at the end of the yoga program compared to a treatment-as-usual group.57 Improvements in self-compassion were also observed from preintervention to postintervention in a pilot research trial evaluating an 8-week yoga intervention for individuals with chronic complex disease and disability.52 Notably, self-compassion was found to mediate changes in anxiety from preintervention to postintervention, speaking to the mechanisms of yoga practice and philosophy didactics on psychological experience. The authors concluded that self-compassion may enable individuals to contact distressing inner experience without ascribing evaluative or judgmental meaning, to bypass ruminative tendencies, and to select healthful and agential actions to create positive change.52
Corroborating the increases in self-compassion were changes in levels of mindfulness, which is an overlapping third-wave construct. Total levels of mindfulness and the subscales of observing and nonreactivity all increased from preintervention to postintervention when the participants were evaluated as one cohort. These findings parallel results from trials that evaluated mindfulness in the context of a yoga intervention for individuals with chronic pain and limited mobility. Specifically, an 8-week pilot yoga program for individuals with fibromyalgia resulted in improvements in the total scale and in the describing and nonreactivity to inner experience subscales of the FFMQ.51 Improvements in two subscales of the FFMQ – nonjudging of inner experience and acting with awareness – were observed for cancer survivors who participated in a 7-week yoga intervention.104 The fact that different subscales demonstrated improvements across the studies may be attributable to the differences in the intervention’s philosophical focus, specific attentional or meditative training, variations in the teaching style, or to the specific health populations. In addition, there were also qualitative reports of increased present-mindedness (being in the moment, letting go, new way of being in old experience, increased awareness of body, increased concentration) for individuals with SCI who participated in an 8-week yoga program.60 Taken together, these studies indicate that yoga programs that are comprehensive in nature and that include philosophical concepts that bridge the two disciplines (eg, witness consciousness, one pointed concentration, non-judgment, openness) have demonstrated increased levels of mindfulness in individuals with health-related impacts or disability.
There were no demonstrated improvements in pain intensity, pain interference, or pain catastrophizing. It may be that the questionnaire used to measure pain (BPI) was limited in scope, as it used gross numeric rating scales for worst, least, average, and present pain levels, and did not query for pain quality or type. The use of more specific pain-measurement tools, such as the McGill Pain Questionnaire, may provide more detailed information about the type (eg, neuropathic, musculoskeletal) and quality (eg, affective, cognitive, evaluative) of pain and whether various types of pain respond differently to yoga practice. Similarly, there were no improvements in other psychological constructs, such as psychological flexibility, anxiety, self-efficacy, resilience, or posttraumatic growth. Scores on psychological flexibility, self-efficacy, resilience, and posttraumatic growth were all high at the beginning of the study, which may have served as a ceiling effect, resulting in limited room for improvement. The lack of a signification reduction in anxiety differs from an RCT evaluating yoga for individuals with chronic back pain compared to an exercise control group105 and from a previous pilot trial using a similar yoga-program manual.52 One possible explanation for this discrepancy is the components of the yoga program: active arm work and philosophy didactics may have provided an uplifting quality, rather than a calming or anxiolytic quality.
Given the breadth and variety of yoga interventions that are used in yoga research, it is imperative to document properly the specific components of a yoga program and delineate how interventions are tailored for various populations.72,106 The present study used an integrated yoga intervention that incorporated many “limbs” or aspects of yoga, including breathing practices, physical postures, yoga philosophy, mindfulness, and meditation/relaxation techniques. Although such a comprehensive program is not a new format in the yoga literature,72 this combination of limbs has not been applied to an SCI population and was innovative in the consideration and application of yoga philosophical concepts. This intervention was designed in accordance with the teaching philosophy of IY, in terms of progression of instruction with the skill development of the students/participants, in modeling the ethical principles through the style of teaching, the use of therapeutic variations of classical poses, and of the selection of practices that are considered within this yogic lineage both to calm the nervous system (eg, breathing and meditation), to promote vitality, and to lift depressive or “heavy” states of mind.65 The authors have provided a table of philosophical concepts in order to document which yogic theories from traditional texts and the Iyengar lineage were considered appropriate for this population and to assist with replicability.
Limitations
The present study was limited by its small sample size, which increased the possibility of type 2 errors, and by the exclusive use of self-report measures. The evaluation of multiple measures also introduced the possibility of a type 1 error, and so results should be replicated with a larger-scale RCT. Study methodology using a WLC design is limited by the possibility that participants in the WLC group may change their behavior in the waiting period. The authors instructed the participants to refrain from practicing yoga in that time, to prevent a possible confound. As well, there was the possibility of an expectancy effect for WLC participants, which should be considered when interpreting the results of the combined-group analysis, and in particular the findings that emerged in this analysis only (eg, increases in mindfulness). Although there was one member of the research team present at all assessment points, there were additional research assistants at each time point, which may have introduced variability in the assessment process.
In addition, there were a higher number of individuals of Caucasian heritage in the WLC group, and this discrepancy should be considered when interpreting the results. Although this pilot RCT tailored the yoga intervention to individuals with SCI who had limited mobility and instability of the musculoskeletal system, it was not specialized to the degree of injury and thus did not differentiate between individuals with varying levels of injury. Future studies should specialize yoga programs to a greater extent, especially for individuals with tetraplegia or complete SCI who may need greater one-on-one care and modification of āsanas, due to the unique presentation of each SCI. The use of props was limited to IY blankets for spinal and postural support, and greater precision and effect of āsana practice could be attained with the use of other traditional yoga props, such as straps and bolsters.
Future research
The emerging field of yoga research for individuals with severe and impairing disability would benefit from larger trials to explore further the impact of yoga interventions on psychological, pain-related, functional, and mindfulness constructs. Given that levels of mindfulness and self-compassion increased in this study, and have been shown to be mediating variables of improvements in psychological experience in other yoga-research trials, future research should evaluate the mediating role of these constructs for individuals with SCI. It has been proposed that mindfulness may provide therapeutic gains by increasing compassion and psychological flexibility and by decreasing the propensity for rumination,107 and so modeling of the relationships of these variables in the context of a yoga intervention is warranted.
In order to create meaningful yoga interventions for individuals with tetraplegia, it is recommended that larger trials use a multiwave design rather than increased class sizes, so that individualized care is possible. Researchers employing an RCT design may consider stratifying participants by injury level, degree of completeness, or mobility characteristics, which may require multisite involvement, due to recruitment limitations. It may also be beneficial to have a high teacher:student ratio to ensure that participants maximize in obtaining benefits from the degree of movement that is accessible for each student. Previous research has documented that participation in an IY-intervention resulted in reduced pain-medication consumption for individuals with chronic low-back pain,108 and so evaluation of the impact of yoga on pain-medication consumption for individuals with SCI may provide important information regarding alternate pain-management strategies. In communities where public and accessible transport is not possible, such as rural and remote settings, the use of electronic resources or videoconferencing for service provision may be useful and increase access for individuals who encounter physical limitations to attending institutionally based yoga interventions. Finally, interventions should be evaluated at follow-up intervals using a longitudinal research design to determine the lasting effect of yoga on psychological experience. It is important to conduct yoga research for this population, as yoga represents a mind–body intervention that can simultaneously address physical and mental health impacts and thus improve multiple facets of patient well-being. Yoga is a relatively low-cost therapeutic intervention that once learned, can be practiced safely and independently, thereby empowering patients and partially reducing dependence on care providers.
Conclusion
The results of this pilot RCT revealed improvements in depressive symptoms and self-compassion for individuals randomized to IY compared to a WLC group. The results also suggest that a yoga program may result in increases in mindfulness from preintervention to postintervention, with an increased capacity to observe and not react to immediate physical and emotional experience. Yoga is a safe and supportive mind–body practice that may simultaneously attenuate some of the negative psychological impacts of SCI, while also bolstering inner resources. Therapies, such as yoga, that incorporate mindfulness concepts, such as acceptance and openness, and that focus on positive and adaptive coping may offer protection from some of the devastating and life-altering consequences of SCI, and should be integrated in tertiary care settings offering rehabilitative services.
Acknowledgments
The authors would like to thank Manouso Manos (advanced senior Iyengar yoga instructor) and Gloria Goldberg (advanced junior 2 Iyengar yoga instructor), for their generous insights toward the design of the yoga program so that it was safe, therapeutic, and impactful for individuals with SCI.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Hassanijirdehi M, Khak M, Afshari-Mirak S, et al. Evaluation of pain and its effect on quality of life and functioning in men with spinal cord injury. Korean J Pain. 2015;28(2):129–136. doi: 10.3344/kjp.2015.28.2.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kirshblum S. Rehabilitation of spinal cord injury. In: DeLisa JA, Gans BM, Bockenek WL, et al., editors. Physical Medicine and Rehabilitation: Principles and Practice. 4th ed. Philadelphia: Lippincott Williams & Wilkins; 2005. pp. 1715–1752. [Google Scholar]
- 3.Littooij E, Widdershoven GA, Stolwijk-Swüste JM, Doodeman S, Leget CJ, Dekker J. Global meaning in people with spinal cord injury: content and changes. J Spinal Cord Med. 2016;39(2):197–205. doi: 10.1179/2045772314Y.0000000290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Craig A, Perry KN, Guest R, et al. Prospective study of the occurrence of psychological disorders and comorbidities after spinal cord injury. Arch Phys Med Rehabil. 2015;96(8):1426–1434. doi: 10.1016/j.apmr.2015.02.027. [DOI] [PubMed] [Google Scholar]
- 5.Migliorini C, Tonge B, Taleporos G. Spinal cord injury and mental health. Aust N Z J Psychiatry. 2008;42(4):309–314. doi: 10.1080/00048670801886080. [DOI] [PubMed] [Google Scholar]
- 6.Williams R, Murray A. Prevalence of depression after spinal cord injury: a meta-analysis. Arch Phys Med Rehabil. 2015;96(1):133–140. doi: 10.1016/j.apmr.2014.08.016. [DOI] [PubMed] [Google Scholar]
- 7.Pollard C, Kennedy P. A longitudinal analysis of emotional impact, coping strategies and post-traumatic psychological growth following spinal cord injury: a 10-year review. Br J Health Psychol. 2007;12(Pt 3):347–362. doi: 10.1348/135910707X197046. [DOI] [PubMed] [Google Scholar]
- 8.Craig A, Tran Y, Wijesuriya N, Middleton J. Fatigue and tiredness in people with spinal cord injury. J Psychosom Res. 2012;73(3):205–210. doi: 10.1016/j.jpsychores.2012.07.005. [DOI] [PubMed] [Google Scholar]
- 9.Wijesuriya N, Tran Y, Middleton J, Craig A. Impact of fatigue on the health-related quality of life in persons with spinal cord injury. Arch Phys Med Rehabil. 2012;93(2):319–324. doi: 10.1016/j.apmr.2011.09.008. [DOI] [PubMed] [Google Scholar]
- 10.Al-Owesie RM, Moussa NM, Robert AA. Anxiety and depression among traumatic spinal cord injured patients. Neurosciences (Ryadh) 2012;17(2):145–150. [PubMed] [Google Scholar]
- 11.Jensen MP, Hoffman AJ, Cardenas DD. Chronic pain in individuals with spinal cord injury: a survey and longitudinal study. Spinal Cord. 2005;43(12):704–712. doi: 10.1038/sj.sc.3101777. [DOI] [PubMed] [Google Scholar]
- 12.Siddall PJ, McClelland JM, Rutkowski SB, Cousins MJ. A longitudinal study of the prevalence and characteristics of pain in the first 5 years following spinal cord injury. Pain. 2003;103(3):249–257. doi: 10.1016/S0304-3959(02)00452-9. [DOI] [PubMed] [Google Scholar]
- 13.Mehta S, Guy SD, Bryce TN, et al. The CanPain SCI clinical practice guidelines for rehabilitation management of neuropathic pain after spinal cord: screening and diagnosis recommendations. Spinal Cord. 2016;54(Suppl 1):S7–S13. doi: 10.1038/sc.2016.89. [DOI] [PubMed] [Google Scholar]
- 14.Vlaeyen JW, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain. 2000;85(3):317–332. doi: 10.1016/S0304-3959(99)00242-0. [DOI] [PubMed] [Google Scholar]
- 15.Jensen MP, Moore MR, Bockow TB, Ehde DM, Engel JM. Psychosocial factors and adjustment to chronic pain in persons with physical disabilities: a systematic review. Arch Phys Med Rehabil. 2011;92(1):146–160. doi: 10.1016/j.apmr.2010.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Taylor J, Huelbes S, Albu S, Gomez-Soriano J, Penacoba C, Poole HM. Neuropathic pain intensity, unpleasantness, coping strategies, and psychosocial factors after spinal cord injury: an exploratory longitudinal study during the first year. Pain Med. 2012;13(11):1457–1468. doi: 10.1111/j.1526-4637.2012.01483.x. [DOI] [PubMed] [Google Scholar]
- 17.Kilic SA, Dorstyn DS, Guiver NG. Examining factors that contribute to the process of resilience following spinal cord injury. Spinal Cord. 2013;51(7):553–557. doi: 10.1038/sc.2013.25. [DOI] [PubMed] [Google Scholar]
- 18.Min JA, Lee CU, Hwang SI, et al. The moderation of resilience on the negative effect of pain on depression and post-traumatic growth in individuals with spinal cord injury. Disabil Rehabil. 2014;36(14):1196–1202. doi: 10.3109/09638288.2013.834985. [DOI] [PubMed] [Google Scholar]
- 19.Hayter MR, Dorstyn DS. Resilience, self-esteem and self-compassion in adults with spina bifida. Spinal Cord. 2014;52(2):167–171. doi: 10.1038/sc.2013.152. [DOI] [PubMed] [Google Scholar]
- 20.Nooijen CF, Stam HJ, Schoenmakers I, et al. Working mechanisms of a behavioural intervention promoting physical activity in persons with subacute spinal cord injury. J Rehabil Med. 2016;48(7):583–588. doi: 10.2340/16501977-2110. [DOI] [PubMed] [Google Scholar]
- 21.Driver S, Warren AM, Reynolds M, et al. Identifying predictors of resilience at inpatient and 3-month post-spinal cord injury. J Spinal Cord Med. 2016;39(1):77–84. doi: 10.1179/2045772314Y.0000000270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guest R, Craig A, Tran Y, Middleton J. Factors predicting resilience in people with spinal cord injury during transition from inpatient rehabilitation to the community. Spinal Cord. 2015;53(9):682–686. doi: 10.1038/sc.2015.32. [DOI] [PubMed] [Google Scholar]
- 23.Kalpakjian CZ, McCullumsmith CB, Fann JR, et al. Post-traumatic growth following spinal cord injury. J Spinal Cord Med. 2014;37(2):218–225. doi: 10.1179/2045772313Y.0000000169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Monden KR, Trost Z, Catalano D, et al. Resilience following spinal cord injury: a phenomenological view. Spinal Cord. 2014;52(3):197–201. doi: 10.1038/sc.2013.159. [DOI] [PubMed] [Google Scholar]
- 25.Bonanno GA, Kennedy P, Galatzer-Levy IR, Lude P, Elfström ML. Trajectories of resilience, depression, and anxiety following spinal cord injury. Rehabil Psychol. 2012;57(3):236–247. doi: 10.1037/a0029256. [DOI] [PubMed] [Google Scholar]
- 26.Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: model, processes and outcomes. Behav Res Ther. 2006;44(1):1–25. doi: 10.1016/j.brat.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 27.Neff K. Self-compassion: an alternative conceptualization of a healthy attitude toward oneself. Self Identity. 2003;2(2):85–101. [Google Scholar]
- 28.Kabat-Zinn J. Wherever You Go, There You Are: Mindfulness Meditation for Everyday Life. New York: Hyperion; 1994. [Google Scholar]
- 29.Wren AA, Somers TJ, Wright MA, et al. Self-compassion in patients with persistent musculoskeletal pain: relationship of self-compassion to adjustment to persistent pain. J Pain Symptom Manage. 2012;43(4):759–770. doi: 10.1016/j.jpainsymman.2011.04.014. [DOI] [PubMed] [Google Scholar]
- 30.McCracken LM, Zhao-O’Brien J. General psychological acceptance and chronic pain: there is more to accept than the pain itself. Eur J Pain. 2010;14(2):170–175. doi: 10.1016/j.ejpain.2009.03.004. [DOI] [PubMed] [Google Scholar]
- 31.Schütze R, Rees C, Preece M, Schütze M. Low mindfulness predicts pain catastrophizing in a fear-avoidance model of chronic pain. Pain. 2010;148(1):120–127. doi: 10.1016/j.pain.2009.10.030. [DOI] [PubMed] [Google Scholar]
- 32.Bailey KA, Gammage KL, van Ingen C, Ditor DS. “It’s all about acceptance”: a qualitative study exploring a model of positive body image for people with spinal cord injury. Body Image. 2015;15:24–34. doi: 10.1016/j.bodyim.2015.04.010. [DOI] [PubMed] [Google Scholar]
- 33.van Leeuwen CM, Edelaar-Peeters Y, Peter C, Stiggelbout AM, Post MW. Psychological factors and mental health in persons with spinal cord injury: an exploration of change or stability. J Rehabil Med. 2015;47(6):531–537. doi: 10.2340/16501977-1953. [DOI] [PubMed] [Google Scholar]
- 34.Norrbrink C, Löfgren M. Needs and requests: patients and physicians voices about improving the management of spinal cord injury neuropathic pain. Disabil Rehabil. 2016;38(2):151–158. doi: 10.3109/09638288.2015.1035456. [DOI] [PubMed] [Google Scholar]
- 35.Bechsgaard G. The Gift of Consciousness: Patanjali’s Yoga Sutras – Book One: Samadhi Pada. Newcastle: Cambridge Scholars Publishing; 2013. [Google Scholar]
- 36.McCall MC, Ward A, Roberts NW, Heneghan C. Overview of systematic reviews: yoga as a therapeutic intervention for adults with acute and chronic health conditions. Evid Based Complement Alternat Med. 2013;2013:945895. doi: 10.1155/2013/945895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wren AA, Wright MA, Carson JW, Keefe FJ. Yoga for persistent pain: new findings and directions for an ancient practice. Pain. 2011;152(3):477–480. doi: 10.1016/j.pain.2010.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Holtzman S, Beggs RT. Yoga for chronic low back pain: a meta-analysis of randomized controlled trials. Pain Res Manag. 2013;18(5):267–272. doi: 10.1155/2013/105919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Michalsen A, Traitteur H, Lüdtke R, et al. Yoga for chronic neck pain: a pilot randomized controlled clinical trial. J Pain. 2012;13(11):1122–1130. doi: 10.1016/j.jpain.2012.08.004. [DOI] [PubMed] [Google Scholar]
- 40.Cramer H, Lauche R, Hohmann C, et al. Randomized-controlled trial comparing yoga and home-based exercise for chronic neck pain. Clin J Pain. 2013;29(3):216–223. doi: 10.1097/AJP.0b013e318251026c. [DOI] [PubMed] [Google Scholar]
- 41.Ebnezar J, Nagarathna R, Yogitha B, Nagendra HR. Effects of an integrated approach of hatha yoga therapy on functional disability, pain, and flexibility in osteoarthritis of the knee joint: a randomized controlled study. J Altern Complement Med. 2012;18(5):463–472. doi: 10.1089/acm.2010.0320. [DOI] [PubMed] [Google Scholar]
- 42.Garfinkel MS, Schumacher HR, Jr, Husain A, Levy M, Reshetar RA. Evaluation of a yoga based regimen for treatment of osteoarthritis of the hands. J Rheumatol. 1994;21(12):2341–2343. [PubMed] [Google Scholar]
- 43.Ward L, Stebbings S, Cherkin D, Baxter GD. Yoga for functional ability, pain and psychosocial outcomes in musculoskeletal conditions: a systematic review and meta-analysis. Musculoskeletal Care. 2013;11(4):203–217. doi: 10.1002/msc.1042. [DOI] [PubMed] [Google Scholar]
- 44.Cramer H, Lauche R, Langhorst J, Dobos G. Yoga for rheumatic diseases: a systematic review. Rheumatology (Oxford) 2013;52(11):2025–2030. doi: 10.1093/rheumatology/ket264. [DOI] [PubMed] [Google Scholar]
- 45.Balasubramaniam M, Telles S, Doraiswamy PM. Yoga on our minds: a systematic review of yoga for neuropsychiatric disorders. Front Psychiatry. 2013;3:117. doi: 10.3389/fpsyt.2012.00117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bonura KB, Tenenbaum G. Effects of yoga on psychological health in older adults. J Phys Act Health. 2014;11(7):1334–1341. doi: 10.1123/jpah.2012-0365. [DOI] [PubMed] [Google Scholar]
- 47.Dick AM, Niles BL, Street AE, DiMartino DM, Mitchell KS. Examining mechanisms of change in a yoga intervention for women: the influence of mindfulness, psychological flexibility, and emotion regulation on PTSD symptoms. J Clin Psychol. 2014;70(12):1170–1182. doi: 10.1002/jclp.22104. [DOI] [PubMed] [Google Scholar]
- 48.Cramer H, Lauche R, Azizi H, Dobos G, Langhorst J. Yoga for multiple sclerosis: a systematic review and meta-analysis. PLoS One. 2014;9(11):e112414. doi: 10.1371/journal.pone.0112414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Braun TD, Park CL, Conboy LA. Psychological well-being, health behaviors, and weight loss among participants in a residential, Kripalu yoga-based weight loss program. Int J Yoga Therap. 2012;(22):9–22. [PubMed] [Google Scholar]
- 50.Salgado BC, Jones M, Ilgun S, McCord G, Loper-Powers M, van Houten P. Effects of a 4-month Ananda yoga program on physical and mental health outcomes for persons with multiple sclerosis. Int J Yoga Therap. 2013;23(2):27–38. [PubMed] [Google Scholar]
- 51.Curtis K, Osadchuk A, Katz J. An eight-week yoga intervention is associated with improvements in pain, psychological functioning and mindfulness, and changes in cortisol levels in women with fibromyalgia. J Pain Res. 2011;4:189–201. doi: 10.2147/JPR.S22761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Curtis K, Kuluski K, Bechsgaard G, Ridgway J, Katz J. Evaluation of a specialized yoga program for persons admitted to a complex continuing care hospital: a pilot study. Evid Based Complement Alternat Med. 2016;2016:6267879. doi: 10.1155/2016/6267879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bussing A, Michalsen A, Khalsa SB, Telles S, Sherman KJ. Effects of yoga on mental and physical health: a short summary of reviews. Evid Based Complement Alternat Med. 2012;2012:165410. doi: 10.1155/2012/165410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Vadiraja HS, Rao MR, Nagarathna R, et al. Effects of yoga program on quality of life and affect in early breast cancer patients undergoing adjuvant radiotherapy: a randomized controlled trial. Complement Ther Med. 2009;17(5–6):274–280. doi: 10.1016/j.ctim.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 55.van Uden-Kraan CF, Chinapaw MJ, Drossaert CH, Verdonck-de Leeuw IM, Buffart LM. Cancer patients’ experiences with and perceived outcomes of yoga: results from focus groups. Support Care Cancer. 2013;21(7):1861–1870. doi: 10.1007/s00520-013-1728-4. [DOI] [PubMed] [Google Scholar]
- 56.Pascoe MC, Bauer IE. A systematic review of randomised control trials on the effects of yoga on stress measures and mood. J Psychiatr Res. 2015;68:270–282. doi: 10.1016/j.jpsychires.2015.07.013. [DOI] [PubMed] [Google Scholar]
- 57.Toise SC, Sears SF, Schoenfeld MH, et al. Psychosocial and cardiac outcomes of yoga for ICD patients: a randomized clinical control trial. Pacing Clin Electrophysiol. 2014;37(1):48–62. doi: 10.1111/pace.12252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Garrett R, Immink MA, Hillier S. Becoming connected: the lived experience of yoga participation after stroke. Disabil Rehabil. 2011;33(25–26):2404–2415. doi: 10.3109/09638288.2011.573058. [DOI] [PubMed] [Google Scholar]
- 59.Khalsa SB, Telles S, Cohen L, McCall T. Introduction to Yoga in Health Care. Edinburgh: Handspring Publishing; 2016. [Google Scholar]
- 60.Curtis K, Hitzig SL, Leong N, Wicks C, Ditor D, Katz J. Evaluation of a modified yoga program for persons with spinal cord injury. Ther Recreation J. 2015;49(2):97–117. [Google Scholar]
- 61.Moriello G, Proper D, Cool S, Fink S, Schock S, Mayack J. Yoga therapy in an individual with spinal cord injury: a case report. J Bodyw Mov Ther. 2015;19(4):581–591. doi: 10.1016/j.jbmt.2014.08.004. [DOI] [PubMed] [Google Scholar]
- 62.Fishman LM, Groessl EJ, Sherman KJ. Serial case reporting yoga for idiopathic and degenerative scoliosis. Glob Adv Health Med. 2014;3(5):16–21. doi: 10.7453/gahmj.2013.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zwick D. Integrating Iyengar yoga into rehab for spinal cord injury. Nursing. 2006;36(Suppl):18–22. doi: 10.1097/00152193-200610002-00006. [DOI] [PubMed] [Google Scholar]
- 64.Ward L, Stebbings S, Sherman KJ, Cherkin D, Baxter GD. Establishing key components of yoga interventions for musculoskeletal conditions: a Delphi survey. BMC Complement Altern Med. 2014;14:196. doi: 10.1186/1472-6882-14-196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Iyengar BK. Light on Yoga. London: HarperCollins; 2010. [Google Scholar]
- 66.Thabane L, Ma J, Chu R, et al. A tutorial on pilot studies: the what, why and how. BMC Med Res Methodol. 2010;10:1. doi: 10.1186/1471-2288-10-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lancaster GA, Dodd S, Williamson PR. Design and analysis of pilot studies: recommendations for good practice. J Eval Clin Pract. 2004;10(2):307–312. doi: 10.1111/j..2002.384.doc.x. [DOI] [PubMed] [Google Scholar]
- 68.Hagen NA, Biondo PD, Brasher PM, Stiles CR. Formal feasibility studies in palliative care: why they are important and how to conduct them. J Pain Symptom Manage. 2011;42(2):278–289. doi: 10.1016/j.jpainsymman.2010.11.015. [DOI] [PubMed] [Google Scholar]
- 69.Thorpe KE, Zwarenstein M, Oxman AD, et al. A pragmatic-explanatory continuum indicator summary (PRECIS): a tool to help trial designers. CMAJ. 2009;180(10):E47–E57. doi: 10.1503/cmaj.090523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kalpakjian CZ, Scelza WM, Forchheimer MB, Toussaint LL. Preliminary reliability and validity of a spinal cord injury secondary conditions scale. J Spinal Cord Med. 2007;30(2):131–139. doi: 10.1080/10790268.2007.11753924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Craven C, Hitzig SL, Mittmann N. Impact of impairment and secondary health conditions on health preference among Canadians with chronic spinal cord injury. J Spinal Cord Med. 2012;35(5):361–370. doi: 10.1179/2045772312Y.0000000046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sherman KJ. Guidelines for developing yoga interventions for randomized trials. Evid Based Complement Alternat Med. 2012;2012:143271. doi: 10.1155/2012/143271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Muktibodhananda S. Hatha Yoga Pradipika: Light on Hatha Yoga. Bihar, India: Yoga Publications Trust; 2005. [Google Scholar]
- 74.Bond FW, Hayes SC, Baer RA, et al. Preliminary psychometric properties of the Acceptance and Action Questionnaire-II: a revised measure of psychological inflexibility and experiential avoidance. Behav Ther. 2011;42(4):676–688. doi: 10.1016/j.beth.2011.03.007. [DOI] [PubMed] [Google Scholar]
- 75.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 76.Herrmann C. International experiences with the Hospital Anxiety and Depression Scale: a review of validation data and clinical results. J Psychosom Res. 1997;42(1):17–41. doi: 10.1016/s0022-3999(96)00216-4. [DOI] [PubMed] [Google Scholar]
- 77.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale: an updated literature review. J Psychosom Res. 2002;52(2):69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 78.Woolrich RA, Kennedy P, Tasiemski T. A preliminary psychometric evaluation of the Hospital Anxiety and Depression Scale (HADS) in 963 people living with a spinal cord injury. Psychol Health Med. 2006;11(1):80–90. doi: 10.1080/13548500500294211. [DOI] [PubMed] [Google Scholar]
- 79.Schwarzer RM. Generalized self-efficacy scale. In: Johnston M, Wright S, Weinman J, editors. Measures in Health Psychology: A User’s Portfolio. Windsor, UK: NFER-Nelson; 1995. pp. 35–37. [Google Scholar]
- 80.Scholz U, Gutiérrez-Dona B, Sud S, Schwarzer R. Is general self-efficacy a universal construct? Psychometric findings from 25 countries. Eur J Psychol Assess. 2002;18(3):242–251. [Google Scholar]
- 81.Hampton NZ. Disability status, perceived health, social support, self-efficacy, and quality of life among people with spinal cord injury in the People’s Republic of China. Int J Rehabil Res. 2011;24(1):69–71. doi: 10.1097/00004356-200103000-00010. [DOI] [PubMed] [Google Scholar]
- 82.Kennedy P, Taylor N, Hindson L. A pilot investigation of a psychosocial activity course for people with spinal cord injuries. Psychol Health Med. 2006;11(1):91–99. doi: 10.1080/13548500500330494. [DOI] [PubMed] [Google Scholar]
- 83.Mortenson WB, Noreau L, Miller WC. The relationship between and predictors of quality of life after spinal cord injury at 3 and 15 months after discharge. Spinal Cord. 2010;48(1):73–79. doi: 10.1038/sc.2009.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Nicholson Perry K, Nicholas MK, Middleton J. Spinal cord injury-related pain in rehabilitation: a cross-sectional study of relationships with cognitions, mood and physical function. Eur J Pain. 2009;13(5):511–517. doi: 10.1016/j.ejpain.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 85.Cann A, Calhoun LG, Tedeschi RG, et al. A short form of the Posttraumatic Growth Inventory. Anxiety Stress Coping. 2010;23(2):127–137. doi: 10.1080/10615800903094273. [DOI] [PubMed] [Google Scholar]
- 86.Tedeschi RG, Calhoun LG. The Posttraumatic Growth Inventory: measuring the positive legacy of trauma. J Trauma Stress. 1996;9(3):455–471. doi: 10.1007/BF02103658. [DOI] [PubMed] [Google Scholar]
- 87.Kaler ME, Erbes CR, Tedeschi RG, Arbisi PA, Polusny MA. Factor structure and concurrent validity of the Posttraumatic Growth Inventory - short form among veterans from the Iraq war. J Trauma Stress. 2011;24(2):200–207. doi: 10.1002/jts.20623. [DOI] [PubMed] [Google Scholar]
- 88.Campbell-Sills L, Stein MB. Psychometric analysis and refinement of the Connor-Davidson Resilience Scale (CD-RISC): validation of a 10-item measure of resilience. J Trauma Stress. 2007;20(6):1019–1028. doi: 10.1002/jts.20271. [DOI] [PubMed] [Google Scholar]
- 89.Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC) Depress Anxiety. 2003;18(2):76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- 90.Shin JI, Chae JH, Min JA, et al. Resilience as a possible predictor for psychological distress in chronic spinal cord injured patients living in the community. Ann Rehabil Med. 2012;36(6):815–820. doi: 10.5535/arm.2012.36.6.815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Raes F, Pommier E, Neff KD, Van Gucht D. Construction and factorial validation of a short form of the Self-Compassion Scale. Clin Psychol Psychother. 2011;18(3):250–255. doi: 10.1002/cpp.702. [DOI] [PubMed] [Google Scholar]
- 92.Garcia-Campayo J, Navarro-Gil M, Andres E, Montero-Marin J, Lopez-Artal L, Demarzo MM. Validation of the Spanish versions of the long (26 items) and short (12 items) forms of the Self-Compassion Scale (SCS) Health Qual Life Outcomes. 2014;12:4. doi: 10.1186/1477-7525-12-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Bohlmeijer E, ten Klooster PM, Fledderus M, Veehof M, Baer R. Psychometric properties of the five facet mindfulness questionnaire in depressed adults and development of a short form. Assessment. 2011;18(3):308–320. doi: 10.1177/1073191111408231. [DOI] [PubMed] [Google Scholar]
- 94.Mendoza TR, Chen C, Brugger A, et al. The utility and validity of the modified brief pain inventory in a multiple-dose postoperative analgesic trial. Clin J Pain. 2004;20(5):357–362. doi: 10.1097/00002508-200409000-00011. [DOI] [PubMed] [Google Scholar]
- 95.Tan G, Jensen MP, Thornby JI, Shanti BF. Validation of the Brief Pain Inventory for chronic nonmalignant pain. J Pain. 2004;5(2):133–137. doi: 10.1016/j.jpain.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 96.Bryce TN, Budh CN, Cardenas DD, et al. Pain after spinal cord injury: an evidence-based review for clinical practice and research. J Spinal Cord Med. 2007;30(5):421–440. doi: 10.1080/10790268.2007.11753405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Stroud MW, Turner JA, Jensen MP, Cardenas DD. Partner responses to pain behaviors are associated with depression and activity interference among persons with chronic pain and spinal cord injury. J Pain. 2006;7(2):91–99. doi: 10.1016/j.jpain.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 98.Raichle KA, Osborne TL, Jensen MP, Cardenas D. The reliability and validity of pain interference measures in persons with spinal cord injury. J Pain. 2006;7(3):179–186. doi: 10.1016/j.jpain.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 99.Sullivan MJ, Bishop SC, Pivik J. The Pain Catastrophizing Scale: development and validation. Psychol Assess. 1995;7(4):524–532. [Google Scholar]
- 100.Immink MA, Hillier S, Petkov J. Randomized controlled trial of yoga for chronic poststroke hemiparesis: motor function, mental health, and quality of life outcomes. Top Stroke Rehabil. 2014;21(3):256–271. doi: 10.1310/tsr2103-256. [DOI] [PubMed] [Google Scholar]
- 101.Park J, McCaffrey R, Newman D, Cheung C, Hagen D. The effect of sit ‘n’ fit chair yoga among community-dwelling older adults with osteoarthritis. Holist Nurs Pract. 2014;28(4):247–257. doi: 10.1097/HNP.0000000000000034. [DOI] [PubMed] [Google Scholar]
- 102.Chobe S, Bhargav H, Raghuram N, Garner C. Effect of integrated yoga and physical therapy on audiovisual reaction time, anxiety and depression in patients with chronic multiple sclerosis: a pilot study. J Complement Integr Med. 2016;13(3):301–309. doi: 10.1515/jcim-2015-0105. [DOI] [PubMed] [Google Scholar]
- 103.Sendhilkumar R, Gupta A, Nagarathna R, Taly AB. Effect of pranayama and meditation as an add-on therapy in rehabilitation of patients with Guillain-Barré syndrome: a randomized control pilot study. Disabil Rehabil. 2013;35(1):57–62. doi: 10.3109/09638288.2012.687031. [DOI] [PubMed] [Google Scholar]
- 104.Mackenzie MJ, Carlson LE, Ekkekakis P, Paskevich DM, Culos-Reed SN. Affect and mindfulness as predictors of change in mood disturbance, stress symptoms, and quality of life in a community-based yoga program for cancer survivors. Evid Based Complement Alternat Med. 2013;2013:419496. doi: 10.1155/2013/419496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Tekur P, Nagarathna R, Chametcha S, Hankey A, Nagendra HR. A comprehensive yoga programs [sic] improves pain, anxiety and depression in chronic low back pain patients more than exercise: an RCT. Complement Ther Med. 2012;20(3):107–118. doi: 10.1016/j.ctim.2011.12.009. [DOI] [PubMed] [Google Scholar]
- 106.Elwy AR, Groessl EJ, Eisen SV, et al. A systematic scoping review of yoga intervention components and study quality. Am J Prev Med. 2014;47(2):220–232. doi: 10.1016/j.amepre.2014.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Chiesa A, Anselmi R, Serretti A. Psychological mechanisms of mindfulness-based interventions: what do we know? Holist Nurs Pract. 2014;28(2):124–148. doi: 10.1097/HNP.0000000000000017. [DOI] [PubMed] [Google Scholar]
- 108.Williams K, Abildso C, Steinberg L, et al. Evaluation of the effectiveness and efficacy of Iyengar yoga therapy on chronic low back pain. Spine (Phila Pa 1976) 2009;34(19):2066–2076. doi: 10.1097/BRS.0b013e3181b315cc. [DOI] [PMC free article] [PubMed] [Google Scholar]