Abstract
Since the early days of coronary angiography, the extension and severity of coronary artery disease (CAD) have been used for risk stratification. The SYNTAX score objectively characterizes CAD in patients with multivessel disease. Furthermore, recalculating the SYNTAX score by the incorporation of the functional component coronary stenosis (i.e., FFR) increases the discrimination for the risk of adverse events. The calculation of the SYNTAX score derived from non-invasive modalities such as coronary computed tomography angiography (CTA) has emerged as a mean to obtain the SYNTAX score before invasive cardiac catheterization. Likewise, the computation of the non-invasive fractional flow reserve CT (FFRCT) allows for the calculation of the non-invasive functional SYNTAX score. Ultimately, the combination of anatomical and functional evaluations with clinical factors further refines the identification of patients at risk and provides a recommendation for the Heart Team regarding the treatment strategy (i.e., PCI or CABG) based on the predicted 4-year mortality. The purpose of this review is to describe the integration of a novel non-invasive functional coronary assessment with the angiographic risk score in patients with multivessel CAD.
Keywords: SYNTAX score, coronary computed tomography angiography (coronary CTA), non-invasive fractional flow reserve, SYNTAX III
Introduction
Since the early days of coronary angiography, the extension and severity of coronary artery disease (CAD) have been used for risk stratification. Risk scores were developed based on the amount of myocardium at risk and coronary lesion characteristics. In 1977, the Duke Jeopardy score was introduced. It was based on the amount of jeopardise myocardium which was defined by the localisation of a coronary stenosis (i.e., proximal, mid or distal segment) (1). In 1981, after the introduction of balloon angioplasty, the American College of Cardiology and the American Heart Association proposed a new classification of coronary lesions based on the risk of vessel occlusion associated with balloon angioplasty (i.e., type A, B and C) (2). This simple and practical lesion classification also was shown to predict outcomes after bare-metal and drug-eluting stent implantation; therefore, it has been widely adopted by the interventional community (3,4). In 2006, the SYNTAX score was created to objectively quantify the extension and severity of CAD in patients with multivessel disease (5). Further improvement in the accuracy of risk stratification was observed with detailed physiologic analysis recalculating the SYNTAX score based on the functional component of the lesions (6). In addition, a non-invasive approach for the SYNTAX score derived from coronary computed tomography angiography (CTA) has been described as a mean of obtaining the SYNTAX score before invasive heart catheterization (7). Likewise, the computation of the non-invasive fractional flow reserve derived from CT (FFRCT) allows for the calculation of the non-invasive functional SYNTAX score. Ultimately, the integration of the functional SYNTAX Score with clinical factors using the SYNTAX score II further identifies patients who might benefit from a particular type of revascularization (i.e., PCI or CABG). The SYNTAX score II provides a recommendation for the Heart Team regarding the treatment strategy (i.e., PCI or CABG) based on the predicted 4-year mortality. The purpose of this review is to describe the integration of a novel non-invasive functional coronary assessment with the angiographic risk scores in patients with multivessel CAD.
The SYNTAX score: a milestone in interventional cardiology
The SYNTAX score was developed in the context of the SYNTAX Trial (Synergy between PCI with Taxus and. Cardiac Surgery) with the aim to help the Heart Team to objectively characterize the severity and extension of CAD in patients with multivessel disease, aiding in the decision-making process between PCI and CABG (8). The SYNTAX score is an anatomical scoring system based on the number of coronary lesions. Lesions are defined by a visual diameter stenosis ≥50% in vessels greater than 1.5 mm in diameter assessed by invasive coronary angiography (ICA) (9). Coronary segments are identified according to the modification made to the American Heart Association classification by the Arterial Revascularization Therapies Study (ARTS) investigators (10). Each coronary segment is weighted based on the amount of subtended myocardium as described by Leaman et al. (11). Additional points are granted depending on high-risk lesion characteristics (i.e., long lesions, calcification, bifurcation, etc.). The score from each lesion is summed to obtain the final SYNTAX score.
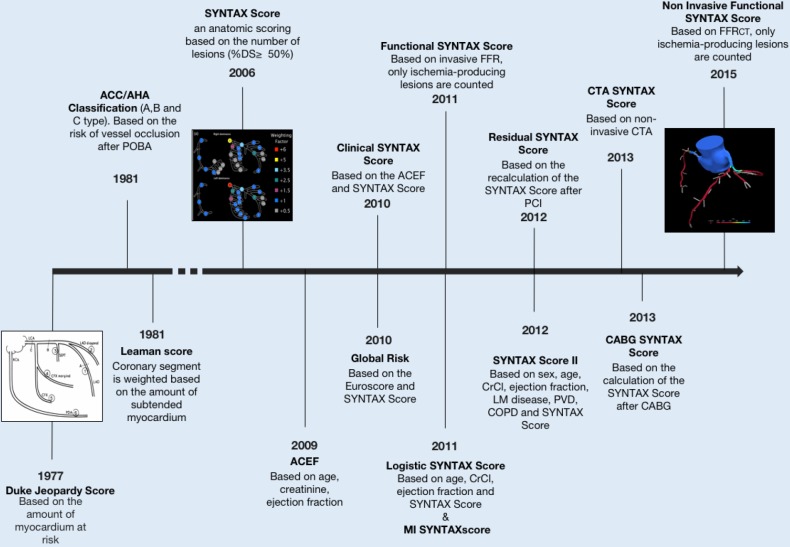
The SYNTAX has shown to correlate with major adverse cardiovascular events [MACE (all-cause death, myocardial infarction, stroke and target vessel revascularization)] rates after PCI. In the SYNTAX trial, MACE rates increased progressively according to the SYNTAX score tertiles, i.e., for the low SYNTAX score [0–22] 14.5% events rate, medium score group [23–32] 16.7% events rate and high score group [>32] 23.4% (12). Interestingly, in the CABG arm of the trial, no impact of the SYNTAX score on the MACE rate was observed. External validations of the SYNTAX score in a broad range of patient populations have been performed. The SYNTAX score has proved to be an independent predictor of mortality, myocardial infarction, and stent thrombosis (13,14). The SYNTAX score is advocated in both the European and American revascularization guidelines for decision making between PCI and CABG and has been used as inclusion criteria in the recently published EXCEL trial (15,16). Figure 1 shows the chronological development of the SYNTAX and derived scores.
Figure 1.
The evolution of the SYNTAX score.
Functional SYNTAX score: anatomy meets physiology
Over the past decade, there has been an increased awareness of the importance of the functional component of an anatomical obstruction, namely the influence of a coronary stenosis on blood flow and pressure. Fractional flow reserve (FFR), the ratio of the distal and proximal pressures of an epicardial coronary stenosis has proved to accurately detect myocardial ischemia and is now recognised as the gold standard (17). In lesions with FFR >0.80, coronary interventions can be safely deferred regardless of the obstruction severity (18). Moreover, FFR-guided PCI has reduced the rates of MACE compared to angiography-guided PCI (17). Against this background, the functional evaluation of coronary lesion was translated into the SYNTAX score, recalculating the score counting only ischemia-producing lesions (i.e., FFR <0.80) to create a physiology-based SYNTAX score. The functional SYNTAX score was validated in 497 patients from the Fractional Flow Reserve vs. Angiography for Multivessel Evaluation (FAME) study. The occurrence of death and myocardial infarction increased according to the functional SYNTAX score tertile (4.8%, 7.5% and 15.8% in the low, medium and high score, respectively) (19). The use of the functional SYNTAX score reclassified 32% of the patients from the high to the medium risk SYNTAX score whereas 59% of the cases were reclassified from medium-risk to the low-risk group. Furthermore, the functional SYNTAX score had demonstrated a better predictive accuracy for the occurrence of MACE compared to the anatomical SYNTAX score with higher inter-observer reproducibility (19).
Anatomical SYNTAX score derived from CTA
Coronary CTA has emerged as a method for CAD diagnosis and PCI planning (20). The presence of atherosclerotic plaque, its localization, morphology and composition can be assessed. Moreover, the degree of luminal obstruction, presence and extension of calcium, bifurcation lesions and the optimal angle for interventions are obtained using coronary CTA (20). Novel CT scanners have a spatial resolution of 250–400 microns, which is in the range of the resolution achieved by invasive angiography systems (i.e., 200 microns). Therefore, the comprehensive and accurate non-invasive evaluation allows for the calculation of the anatomical SYNTAX score in patients with multivessel disease before invasive procedures (7).
Coronary CTA vs. angiography-based SYNTAX score: a systematic review and meta-analysis
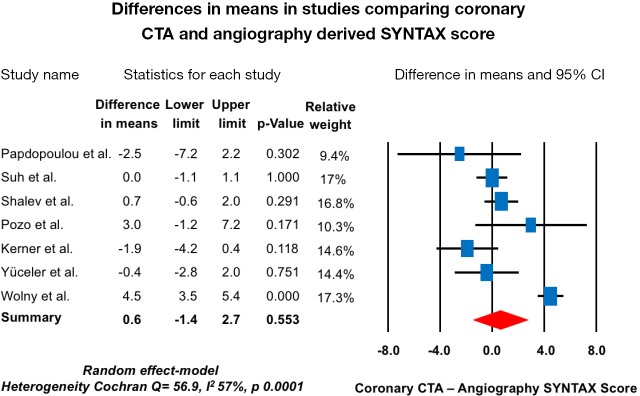
The coronary CTA-derived SYNTAX score has been evaluated in several studies with ICA as a reference. Overall, seven studies comprising n=1,100 patients have been published (14,15,21-25). A high correlation between coronary CTA and the ICA-derived SYNTAX score was found. The mean difference of the SYNTAX score between modalities ranged from −2.5 to 4.5 points. Overall, no difference was found between coronary CTA and the ICA-derived SYNTAX score. The weighted mean difference using the random-effect model was 0.6 (95% CI, −1.4 to 2.7; P=0.553), with a high heterogeneity among studies (Cochran Q =56.9, I2 57%, P=0.0001) (Table 1,Figure 2). Therefore, the CTA-derived SYNTAX score can be used before cardiac catheterizations to help the Heart Team recommend the strategy for revascularization and aid in the procedural planning. However, the agreement in the SYNTAX score between modalities should be evaluated in the context of the severity of the disease and the extent of calcification, since these factors have been shown to interfere with accurate coronary CTA assessment. More evidence is required particularly in patients with multivessel disease.
Table 1. Summary of studies comparing the anatomical SYNTAX score derived from coronary CTA and invasive angiography.
| Author | n | CT SYNTAX score | Angiography SYNTAX score |
|---|---|---|---|
| Papdopoulou et al. | 50 | 10.5 (IQR: 5.0–20.7) | 13.0 (IQR: 7–24) |
| Suh et al. | 399 | 7.0 (IQR: 3–14) | 7.0 (IQR: 2–14) |
| Shalev et al. | 302 | 10.9±8.3 | 10.2±8.0 |
| Pozo et al. | 57 | 26 (IQR: 18–36) | 23 (IQR: 17–30.3) |
| Kerner et al. | 104 | 10.3±6.9 | 14.2±10.3 |
| Yüceler et al. | 108 | 14.5 (IQR: 9–20.1) | 15.9 (IQR: 7.3–21.1) |
| Wolny et al. | 90 | 16.0 (IQR: 14.3–19.4) | 11.5 (IQR: 10.2–14.0) |
Figure 2.
Forest plot of the mean differences in the anatomical SYNTAX score calculation between coronary CTA and invasive angiography. CTA, computed tomography angiography.
Non-invasive functional SYNTAX score
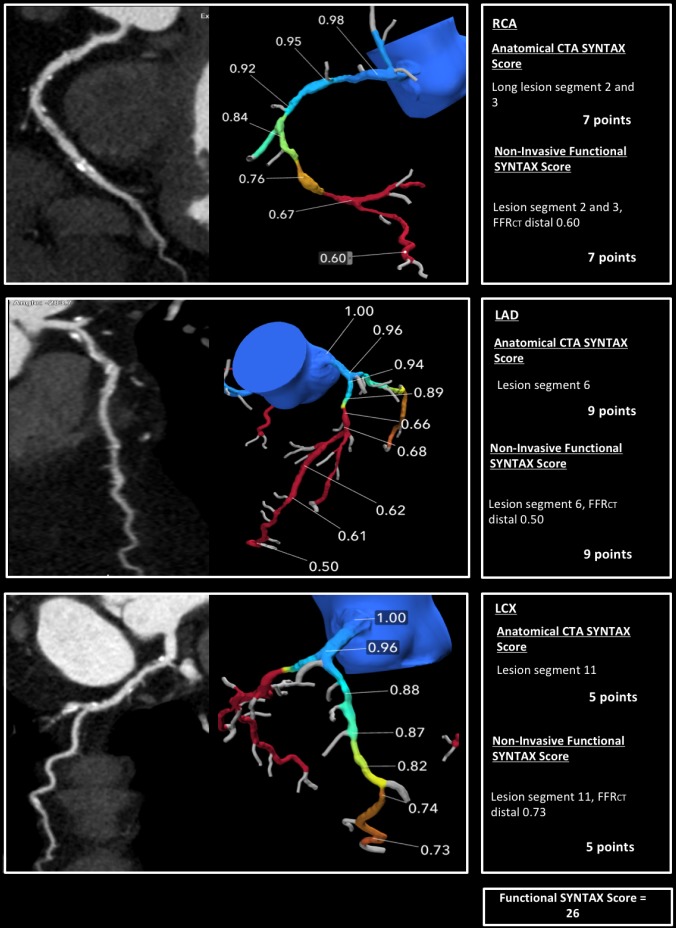
Using coronary CTA, a three-dimensional (3D) patient-specific coronary geometry can be generated. Applying a computational fluid dynamic to these geometries, blood flow can be simulated to compute the non-invasive FFR. The FFR derived from CT, i.e., FFRCT (HeartFlow Inc., Redwood City, California, USA) has been shown to have a high correlation with invasive FFR. In the NXT Trial, which included a low-risk population, the per-patient diagnostic accuracy, sensitivity, specificity, PPV and NPV were 81%, 86%, 79%, 65%, and 93%, respectively (26). The diagnostic performance of FFRCT in a more complex population still requires further validation. Using this technology, a lesion-specific approach for the calculation of the non-invasive functional SYNTAX score can be performed. In the same manner as the invasive approach, the non-invasive functional SYNTAX score is obtained by recalculating the SYNTAX score counting only the ischemia-producing lesions (i.e., FFRCT <0.80) and providing a comprehensive anatomical thus physiological risk stratification before an invasive procedure. In the context of clinical trials, FFRCT computation has been shown to be feasible in more than 85% of the cases (26). The main reasons for the inability to calculate the FFRCT are image artifacts, extensive coronary calcification or prior revascularization with metallic stents. What is worth mentioning is the advent of ICA-derived FFR; this tool has potential to allow for the calculation of the functional SYNTAX score after ICA without the need for a pressure wire. In Figures 3,4, examples of the non-invasive SYNTAX score derived from coronary CTA are shown.
Figure 3.
An example of the calculation of the non-invasive functional SYNTAX score. In the three main coronary vessels (RCA, LAD and LCX) the anatomic lesions were functionally significant; therefore, the anatomical and functional SYNTAX.
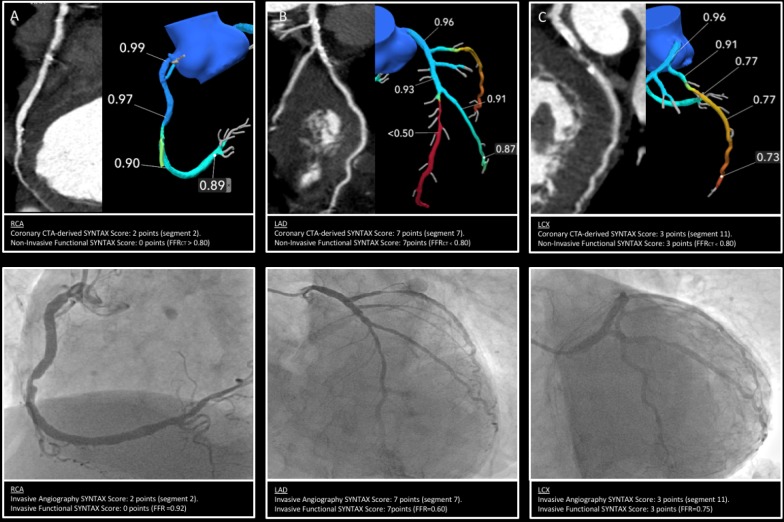
Figure 4.
Anatomic and Functional SYNTAX score based on coronary CTA and invasive angiography. In the RCA (panel A), the anatomical CTA-derived SYNTAX score was 2; however, this lesion was non-functionally significant (FFRCT distal =0.89) thus no points are counted for the non-invasive functional SYNTAX score. In panel B, the anatomical CTA-derived SYNTAX score in the LAD was 7 points; this lesion was functionally significant (FFRCT distal <0.5) thus the same amount of points were included in the non-invasive functional SYNTAX score. In panel C, the anatomical CTA-derived SYNTAX score in the LCX was 3 points; this lesion was functionally significant (FFRCT distal =0.73) thus 3 points were included in the non-invasive functional SYNTAX score. The final CTA-derived anatomical SYNTAX score was 12 points, whereas the non-invasive functional SYNTAX score was 10 points. The bottom of the image portrays the corresponding invasive angiography images with the corresponding invasive FFR. In this case, a complete agreement between the invasive and non-invasive assessment was found. CTA, computed tomography angiography; FFRCT, fractional flow reserve CT.
The SYNTAX score II: bringing it all together
The main limitation of the SYNTAX score is the lack of clinical variables for a truly individualized approach (27). The inclusion of clinical characteristics has significantly enhanced risk prediction providing a personalized risk stratification. The SYNTAX score II (www.syntaxscore.com) is a multivariable Cox proportional model derived from the SYNTAX trial data. It was shown to predict 4-year all-cause mortality in patients with multivessel or left main disease treated with PCI or CABG (28). Independent predictors of mortality that showed interaction effect with the revascularization modality were included. To calculate the SYNTAX score II, the patient’s clinical characteristics such as: gender, age, the presence of peripheral vascular disease (defined as aorta or arteries others than coronaries, with exercise-related claudication, revascularization surgery, reduced or absent pulsation, or angiographic stenosis of more than 50%), chronic obstructive pulmonary disease (defined as the long-term use of chronic bronchodilator or steroids for lung disease), the LVEF (as percentage) and CrCl (defined by Cockcroft and Gault formula, expressed in mL/min) are combined with the angiographic presence of unprotected left main coronary disease and the anatomical SYNTAX score to obtain the SYNTAX score II. The SYNTAX score II provides the patient predicted 4-year mortality if treated with PCI or CABG and a recommendation for treatment with PCI and/or CABG. For example, in a 60-year-old woman with a low anatomical SYNTAX score (which favours PCI) and a reduced LVEF (which favours CABG), the SYNTAX score II will favour CAGB due to a higher predicted 4-year mortality with PCI. In contrast, for a 73-year-old male with a high anatomical SYNTAX score (which favours CABG), left main disease and COPD (which favours PCI) with normal LVEF, the SYNTAX score II will favour PCI compared to CABG. Nevertheless, if the same patient presented without COPD, the treatment recommendation would equipoise PCI and CABG (6). This accurate individualized risk prediction provided by the SYNTAX score II enhances the clinical decision-making process aiding the Heart Team in the selection for a revascularization strategy.
The ongoing SYNTAX III REVOLUTION Trial (A Randomized Pilot Study investigating the use of CT scans and angiography of the heart to help the doctors decide which treatment is the best to improve the blood supply to the heart in patients with complex CAD) will randomize Heart Teams to assess patients using coronary CTA with FFRCT versus conventional ICA to decide the revascularization strategy (i.e., CABG or PCI) in patients with multivessel and/or left main disease (29). The non-invasive functional SYNTAX score will be used to calculate the SYNTAX score II. The results of this trial will provide the foundation for the integration of the non-invasive functional SYNTAX score in clinical practice.
Summary
Since the creation of the SYNTAX score, several derived scores have been developed. The CTA-derived SYNTAX score has been shown to provide an accurate assessment of disease complexity prior to cardiac catheterization. Furthermore, the incremental value of FFRCT with the calculation of the non-invasive functional SYNTAX score allows for a lesion-specific stratification. Finally, the integration of the coronary anatomy and physiology with the comorbidities offers a personalized risk stratification to aid the Heart Team in the decision-making process for a revascularization strategy.
Acknowledgements
None.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Dash H, Johnson RA, Dinsmore RE, et al. Cardiomyopathic syndrome due to coronary artery disease. I: Relation to angiographic extent of coronary disease and to remote myocardial infarction. Br Heart J 1977;39:733-9. 10.1136/hrt.39.7.733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ryan TJ, Faxon DP, Gunnar RM, et al. Guidelines for percutaneous transluminal coronary angioplasty. A report of the American College of Cardiology/American Heart Association Task Force on Assessment of Diagnostic and Therapeutic Cardiovascular Procedures (Subcommittee on Percutaneous Transluminal Coronary Angioplasty). Circulation 1988;78:486-502. 10.1161/01.CIR.78.2.486 [DOI] [PubMed] [Google Scholar]
- 3.Kastrati A, Schömig A, Elezi S, et al. Prognostic value of the modified american college of Cardiology/American heart association stenosis morphology classification for long-term angiographic and clinical outcome after coronary stent placement. Circulation 1999;100:1285-90. 10.1161/01.CIR.100.12.1285 [DOI] [PubMed] [Google Scholar]
- 4.Khattab AA, Hamm CW, Senges J, et al. Prognostic value of the modified American College of Cardiology/American Heart Association lesion morphology classification for clinical outcome after sirolimus-eluting stent placement (results of the prospective multicenter German Cypher Registry). Am J Cardiol 2008;101:477-82. 10.1016/j.amjcard.2007.09.094 [DOI] [PubMed] [Google Scholar]
- 5.Sianos G, Morel MA, Kappetein AP, et al. The SYNTAX score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention 2005;1:219-27. [PubMed] [Google Scholar]
- 6.Sotomi Y, Collet C, Cavalcante R, et al. Tools and Techniques - Clinical: SYNTAX score II calculator. EuroIntervention 2016;12:120-3. 10.4244/EIJV12I1A21 [DOI] [PubMed] [Google Scholar]
- 7.Papadopoulou SL, Girasis C, Dharampal A, et al. CT-SYNTAX score: a feasibility and reproducibility Study. JACC Cardiovasc Imaging 2013;6:413-5. 10.1016/j.jcmg.2012.09.013 [DOI] [PubMed] [Google Scholar]
- 8.Ong AT, Serruys PW, Mohr FW, et al. The SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery (SYNTAX) study: design, rationale, and run-in phase. Am Heart J 2006;151:1194-204. 10.1016/j.ahj.2005.07.017 [DOI] [PubMed] [Google Scholar]
- 9.Serruys PW, Onuma Y, Garg S, et al. Assessment of the SYNTAX score in the Syntax study. EuroIntervention 2009;5:50-6. 10.4244/EIJV5I1A9 [DOI] [PubMed] [Google Scholar]
- 10.Serruys PW, Unger F, van Hout BA, et al. The ARTS study (Arterial Revascularization Therapies Study). Semin Interv Cardiol 1999;4:209-19. [DOI] [PubMed] [Google Scholar]
- 11.Leaman DM, Brower RW, Meester GT, et al. Coronary artery atherosclerosis: severity of the disease, severity of angina pectoris and compromised left ventricular function. Circulation 1981;63:285-99. 10.1161/01.CIR.63.2.285 [DOI] [PubMed] [Google Scholar]
- 12.Serruys PW, Morice MC, Kappetein AP, et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med 2009;360:961-72. 10.1056/NEJMoa0804626 [DOI] [PubMed] [Google Scholar]
- 13.Garg S, Sarno G, Girasis C, et al. A patient-level pooled analysis assessing the impact of the SYNTAX (synergy between percutaneous coronary intervention with taxus and cardiac surgery) score on 1-year clinical outcomes in 6,508 patients enrolled in contemporary coronary stent trials. JACC Cardiovasc Interv 2011;4:645-53. 10.1016/j.jcin.2011.02.018 [DOI] [PubMed] [Google Scholar]
- 14.Yadav M, Palmerini T, Caixeta A, et al. Prediction of coronary risk by SYNTAX and derived scores: synergy between percutaneous coronary intervention with taxus and cardiac surgery. J Am Coll Cardiol 2013;62:1219-30. 10.1016/j.jacc.2013.06.047 [DOI] [PubMed] [Google Scholar]
- 15.Windecker S, Kolh P, Alfonso F, et al. 2014 ESC/EACTS guidelines on myocardial revascularization. EuroIntervention 2015;10:1024-94. 10.4244/EIJY14M09_01 [DOI] [PubMed] [Google Scholar]
- 16.Fihn SD, Blankenship JC, Alexander KP, et al. 2014 ACC/AHA/AATS/PCNA/SCAI/STS focused update of the guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines, and the American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation 2014;130:1749-67. 10.1161/CIR.0000000000000095 [DOI] [PubMed] [Google Scholar]
- 17.De Bruyne B, Fearon WF, Pijls NH, et al. Fractional flow reserve-guided PCI for stable coronary artery disease. N Engl J Med 2014;371:1208-17. 10.1056/NEJMoa1408758 [DOI] [PubMed] [Google Scholar]
- 18.Pijls NH, van Schaardenburgh P, Manoharan G, et al. Percutaneous coronary intervention of functionally nonsignificant stenosis: 5-year follow-up of the DEFER Study. J Am Coll Cardiol 2007;49:2105-11. 10.1016/j.jacc.2007.01.087 [DOI] [PubMed] [Google Scholar]
- 19.Nam CW, Mangiacapra F, Entjes R, et al. Functional SYNTAX score for risk assessment in multivessel coronary artery disease. J Am Coll Cardiol 2011;58:1211-8. 10.1016/j.jacc.2011.06.020 [DOI] [PubMed] [Google Scholar]
- 20.de Araújo Gonçalves P, Campos CA, Serruys PW, et al. Computed tomography angiography for the interventional cardiologist. Eur Heart J Cardiovasc Imaging 2014;15:842-54. 10.1093/ehjci/jeu053 [DOI] [PubMed] [Google Scholar]
- 21.Stähli BE, Bonassin F, Goetti R, et al. Coronary computed tomography angiography indicates complexity of percutaneous coronary interventions. J Invasive Cardiol 2012;24:196-201. [PubMed] [Google Scholar]
- 22.Suh YJ, Hong YJ, Lee HJ, et al. Accuracy of CT for Selecting Candidates for Coronary Artery Bypass Graft Surgery: Combination with the SYNTAX score. Radiology 2015;276:390-9. 10.1148/radiol.15141216 [DOI] [PubMed] [Google Scholar]
- 23.Kerner A, Abadi S, Abergel E, et al. Direct comparison between coronary computed tomography and invasive angiography for calculation of SYNTAX score. EuroIntervention 2013;8:1428-34. 10.4244/EIJV8I12A216 [DOI] [PubMed] [Google Scholar]
- 24.Wolny R, Jastrzębski J, Szubielski M, et al. Coronary computed tomography angiography for the assessment of SYNTAX score. Kardiol Pol 2016;74:40-6. 10.5603/KP.a2015.0135 [DOI] [PubMed] [Google Scholar]
- 25.Yüceler Z, Kantarcı M, Tanboğa İH, et al. Coronary lesion complexity assessed by SYNTAX score in 256-slice dual-source MDCT angiography. Diagn Interv Radiol 2016;22:334-40. 10.5152/dir.2015.15298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nørgaard BL, Leipsic J, Gaur S, et al. Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: the NXT trial (Analysis of Coronary Blood Flow Using CT Angiography: Next Steps). J Am Coll Cardiol 2014;63:1145-55. 10.1016/j.jacc.2013.11.043 [DOI] [PubMed] [Google Scholar]
- 27.Farooq V, Head SJ, Kappetein AP, et al. Widening clinical applications of the SYNTAX score. Heart 2014;100:276-87. 10.1136/heartjnl-2013-304273 [DOI] [PubMed] [Google Scholar]
- 28.Farooq V, van Klaveren D, Steyerberg EW, et al. Anatomical and clinical characteristics to guide decision making between coronary artery bypass surgery and percutaneous coronary intervention for individual patients: development and validation of SYNTAX score II. Lancet 2013;381:639-50. 10.1016/S0140-6736(13)60108-7 [DOI] [PubMed] [Google Scholar]
- 29.PW S. SYNTAX III REVOLUTION Trial: A Randomized Study to Evaluate the Feasibility of Heart-Team Clinical Decision Making Regarding the Optimal (Surgical or Percutaneous Based) Revascularization Strategy in Patients With Complex Coronary Artery Disease, Based on Non-invasive Coronary CT Angiography (CTA) Imaging Utilising High-definition GE RevolutionTM Multi-slice CT and HeartFlow FFRCT Compared to the Current Standard of Care With Conventional Invasive Coronary Angiography (CA). 2016. [Google Scholar]