Abstract
Background
This study developed and validated a claims-based statistical model to predict rheumatoid arthritis (RA) disease activity, measured by the 28-joint count Disease Activity Score (DAS28).
Method
Veterans enrolled in the Veterans Affairs Rheumatoid Arthritis (VARA) registry with one year of data available for review before being assessed by the DAS28, were studied. Three models were developed based on initial selection of variables for analyses. The first model was based on clinically defined variables, the second leveraged grouping systems for high dimensional data and the third approach prescreened all possible predictors based on a significant bivariate association with the DAS28. The least absolute shrinkage and selection operator (LASSO) with fivefold cross-validation was used for variable selection and model development. Models were also compared for patients with <5 years to those ≥5 years of RA disease. Classification accuracy was examined for remission (DAS28 < 2.6) and for low (2.6–3.1), moderate (3.2–5.1) and high (>5.1) activity.
Results
There were 1582 Veterans who fulfilled inclusion criteria. The adjusted r-square for the three models tested ranged from 0.221 to 0.223. The models performed slightly better for patients with <5 years of RA disease than for patients with ≥5 years of RA disease. Correct classification of DAS28 categories ranged from 39.9% to 40.5% for the three models.
Conclusion
The multiple models tested showed weak overall predictive accuracy in measuring DAS28. The models performed poorly at predicting patients with remission and high disease activity. Future research should investigate components of disease activity measures directly from medical records and incorporate additional laboratory and other clinical data.
Keywords: Disease activity, Statistical methods, Rheumatoid arthritis
Background
The estimated prevalence of rheumatoid arthritis (RA) among US adults is approximately 0.6% (1.5 million people age ≥18 years) [1, 2]. Administrative claims databases continue to serve as one of the largest sources of data to study RA treatment and patient outcomes. Nevertheless, the utility of these studies is limited as disease activity is not directly captured in claims databases and there is no method to directly measure disease activity in relation to treatment modification and patient outcomes that are captured in claims data. Researchers have attempted to overcome this limitation by developing claims-based indexes of disease severity. Studies have typically used a Delphi approach to identify variables thought to be associated with disease activity and tested correlation between their approach and clinical information obtained from the electronic health record [3] or existing measures of RA disease activity [4]. A recent study by Desai et al. (2015) [5] attempted to validate the Claims-based Index for Rheumatoid Arthritis Severity (CIRAS) developed by Ting et al. [3], who used the Delphi approach, against the C-reactive-protein-based 28-joint Disease Activity Score (DAS28-CRP) in a relatively small population (n = 315) of patients enrolled in the Brigham Women’s Hospital Rheumatoid Arthritis Sequential Study (BRASS) and Medicare [5]. Unfortunately, they found the correlation between CIRAS and DAS28-CRP was poor and attempts to improve the performance by adding additional claims-derived variables also performed poorly (R 2 = 0.23).
These findings highlight the need to develop an algorithm to measure disease activity/severity in observational studies, as claims data are regularly used to evaluate disease progression and response to RA therapies. The ability to measure disease activity is also important in understanding how clinicians make therapeutic decisions, determining whether patients who may benefit from more aggressive treatment are escalating treatment, and providing real-world evidence of adoption of treatment guidelines.
The goal of this study was to develop and validate claims-based statistical models to predict disease activity measured by DAS28 in a larger population of Veteran patients enrolled in the Veterans Affairs Rheumatoid Arthritis (VARA) registry.
Methods
Design and data
A cohort study design was used on historical data available in the VARA registry and the Veterans Administration (VA) Informatics and Computing Infrastructure (VINCI), which houses the VA Corporate Data Warehouse (CDW) data available for research. This study used VARA and VINCI data from 1 January 2006 until 31 December 2014 to predict disease activity using data typically available in administrative claims databases. The gold standard clinical DAS28 was measured in Veteran patients enrolled in the VARA registry as part of routine care.
The VARA registry is a prospective, multicenter, observational registry involving 11 VA medical centers (Birmingham, AL; Brooklyn, NY; Dallas, TX; Denver, CO; Jackson, MS; Iowa City, IA; Little Rock, AR; Omaha, NE; Portland, OR; Salt Lake City, UT; and Washington, DC). Clinical disease activity measures (i.e., DAS28 and duration of disease) were obtained from the VARA registry, which has been described elsewhere [6, 7].
All administrative claims data were obtained from VINCI [8], which contains both CDW and Managerial Cost Accounting (MCA) system data. VINCI is a research and development environment jointly funded by Health Services Research & Development Service (HSR&D) and the Office of Information and Technology (OIT). VINCI contains rich clinical data in addition to administrative claims data. As the focus of this analysis was on developing a claims-based predictor of the DAS28 we limited our predictor variables to those available in patient tables, inpatient and outpatient procedure, diagnosis and pharmacy data domains.
Study population
Veteran patients had to be enrolled in the VARA registry to be included in the study, and had to be 18+ years of age, have a DAS28, and have at least 365 days of enrollment in the VA health care system prior to the DAS28 measurement. To ensure Veteran patients were actively using the system they were required to have had at least two encounters with the system during the 365-day baseline period. The first encounter with a DAS28 measurement that fulfilled other inclusion and exclusion criteria was eligible as the index date for training and testing the prediction model.
Veteran patients were excluded if they met any of the following criteria because their RA medications and treatment may be modified to treat cancer, transplant or other autoimmune disorders:
Diagnosed with any active cancer (Healthcare Cost and Utilization Project (HCUP) Single-level Clinical Classification System (CCS) [9] Diagnosis Category 11-45)
Undergone a transplant (HCUP CCS Procedure Category 64, 105, 176)
Diagnosed with other autoimmune disorders (HCUP CCS Diagnosis Category: 57, 210)
The index date was defined as the first encounter with a DAS28 after 1 January 2006 and before 31 December 2014 that fulfilled inclusion and exclusion criteria. The baseline period was defined as the 365-day observational period prior to the index date, which is the time we allowed comorbidities to accrue and contribute to the prediction of patient-level DAS.
Study variables
Dependent variables
The dependent variable was the continuous DAS28, which was collected at enrollment in the VARA registry and routinely thereafter. The DAS28 is a widely used disease activity assessment tool that affects treatment decisions by rheumatologists in daily clinical practice [10]. The DAS28 is a statistically derived composite index that takes into account the patient’s number of swollen joints, number of tender joints, erythrocyte sedimentation rate (ESR), and general health using patient global assessment [11].
Our secondary endpoint was to determine if the predicted DAS28 could be correctly categorized to reflect typical clinical classification of disease, which includes remission (<2.6), low (2.6–3.1), moderate (3.2–5.1), and high (>5.1) disease activity.
Predictor variables
Potential predictor variables for model development were established using three distinct but complementary approaches. The first approach identified a list of potential predictors from literature review and discussion with clinical domain experts (GWC, DC, and MT). The second approach utilized hierarchical grouping software to generate drug categories, medical conditions and procedures at a feasible level for model development - described as the “all predictor” model. The third approach started with all possible predictors (i.e., a priori clinically defined variables and potential predictors based on hierarchical grouping systems) then used a prescreening approach that preselected variables exhibiting significant correlation with the DAS28 (p value <0.05). An automatic variables selection technique, described in the “Statistical approach” section, was then used to identify final sets of predictor variables for the three approaches used to identify the initial pool of potential predictor variables.
Table 4 in Appendix 1 lists the a priori clinically defined potential predictors used for model development. It is important to keep in mind that we restricted potential predictors to information available in administrative claims databases. For example, we recorded when specific laboratory measurements occurred but did not attempt to make use of the laboratory results. The potential baseline predictors involved patient demographics, whether specific laboratory tests or radiographs were performed, counts of clinic visits for primary, rheumatology, orthopedic, physical rehabilitation, occupational therapy, and emergency care. Hospital admissions and the number of unique drug classes served as proxies for healthcare utilization. Administrative codes were used to identify surgical procedures, hand surgery, orthopedic surgery and joint injections. Surgical procedures were identified using the Healthcare Cost and Utilization Project (HCUP) Surgical Flag Software [12, 13]. We measured specific comorbidities and implemented the Rheumatic Disease Comorbidity Index (RDCI) to account for comorbidities [14]. Procedure codes were also used to measure the use of assistive devices, such as a cane, crutch, or wheelchair.
Careful attempts were made to accurately measure disease modifying anti-rheumatic drug (DMARD) use during the baseline period and up to 14 days following the index date to reflect treatment changes in response to the DAS28. Three variables were produced for each generic ingredient and by therapeutic classes to represent: (1) days since start of therapy from the beginning of the baseline period, (2) days since ending a course of therapy from the index date (e.g., a value of 25 means the drug was discontinued 25 days before the index date), and (3) the proportion of days covered during the baseline year. Initiation and discontinuation of these therapies was also tracked during the 14 days post index date to account for the potential association between treatment modification and changes in disease activity.
In addition to the a priori defined potential predictors of disease activity, we leveraged existing grouping software to organize procedures, diagnoses and pharmacy claims into levels of aggregation that support prediction of RA disease activity. Specifically, we used counts of all single-level HCUP Clinical Classification System (CCS) condition and procedure groups [9]. We also used counts of all VA drug class codes (e.g., CV200: calcium channel blocker, CV300: antiarrhythmic, etc.) to account for pharmaceutical exposures, dispensed vitamins and dispensed prosthetics/supplies/devices during the baseline period (http://www.pbm.va.gov/nationalformulary.asp. - VA National Formulary by Class April 2016 Excel Spreadsheet). Dichotomous variables were required to have >1% prevalence in the population to be included in the statistical models.
Statistical approach
Least absolute shrinkage and selection operator (LASSO) is a widely used regularization technique used for developing high-dimensional prediction models without high variance [15]. LASSO selection arises from a form of ordinary least squares regression where the sum of the absolute value of the regression coefficients is constrained to be smaller than a specified parameter. Let X = (x 1, x 2, x 3…x m) denote the matrix of predictor variables (e.g., Table 1 with 250+ predictors) and let y denote the DAS28, (i.e., the response variable), where the x i s have been centered and scaled to have unit standard deviation and mean zero and y has a mean of zero. For a given tuning parameter t, the LASSO regression coefficients minimize:
Table 1.
Attrition table for model development
| Inclusion/exclusion criteria | Population and encounters | |
|---|---|---|
| 1. | VARA registry patients April 1, 2015 | 2161 Veterans, 25,464 Encounters |
| 2. | At least one valid DAS28 | 2063 Veterans, 19,064 Encounters |
| 3. | Study period of interest (Jan 1, 2006 to Dec 31, 2014) | 2002 Veterans, 17,000 Encounters |
| 4. | Meet 365 days of enrollment criteria with ≥2 visits during baseline period | 1976 Veterans with index date |
| 5. | Remove patients with cancer | 1631 Veterans |
| 6. | Remove patients with transplant | 1631 Veterans |
| 7. | No other autoimmune disorders | 1582 Veterans |
VARA Veterans Affairs Rheumatoid Arthritis, Das28 28-joint disease activity score
Provided that the LASSO parameter t is small enough, some of the regression coefficients will be exactly zero. Therefore, the LASSO can be viewed as having a built-in variable selection technique. By increasing the LASSO parameter in discrete steps a sequence of regression coefficients is obtained, where the non-zero coefficients at each step correspond to selected parameters. The LASSO method produces a series of models, M 0, M 1 …..M k, with each model being the solution for a unique tuning parameter value. In this series, M 0 can be thought of as the least complex model, for which the maximum penalty is imposed on the regression coefficient, and M k is the most complex model, for which no penalty is imposed. The prediction error is then computed for each model and the model that yields the minimum prediction error is chosen.
Cross-validation is important in guarding against overfitting the model to the data, meaning the model is fit to random error instead of true underlying relationships among the variables. Overfitting reduces model performance when applied to an independent dataset that was not involved in the training of the model. Fivefold “external” cross-validation was applied using randomly selected folds to train and test the statistical model. Every fold was used for both training and testing, e.g., when fold 0 was the testing set then folds 1–4 were used for training and when fold 4 was the testing set then folds 0–3 were used for training. SAS GLMSELECT (SAS version 9.4 with Enterprise Guide version 6.1 (Cary, NC, USA)) was used to implement the cross-validated LASSO procedure and the model that minimizes the cross-validated external predicted sum of squares was used as the primary model selection criterion [16].
Classification analysis
As the secondary study endpoint, we attempted to use the predicted DAS28 to correctly classify patients who were categorized into typical clinical categories of remission and low, moderate, and high disease activity using the actual DAS28.
The correct classification rate (CCR) was used to determine how well the predicted values were classified into the four clinical groups based on the clinical DAS28. CCR is the percentage of correct observations (suitability with the expected value). CCR can be calculated using the following formula:
The higher percentage of CCR shows higher accuracy [17]. Exact binomial 95% confidence internals were computed for the CCR [18].
Sensitivity analysis
We developed three models that varied by the initial pool of variables available for model development. As described above, the first model comprised the clinically defined variables identified from our comprehensive literature review and use of clinical domain experts. The second model comprised these same clinically defined variables, plus HCUP CCS condition and procedure codes, and Veterans Health Administration (VHA) drug class codes. The third model comprised variables from the second model; however, only those variables statistically associated with the DAS28 were included (prescreening). Additional sensitivity analysis was applied on duration of RA disease. Models were compared for RA patients with <5 years of disease and ≥5 years of disease.
Results
Population
During the observation period from 1 January 2006 to 31 December 2014 there were 1582 VARA patients meeting all inclusion criteria for the model development phase. Study attrition is presented in Table 1. The average age at index for the population was 63 years (standard deviation (SD): 11) and 90% (95% CI: 88–91%) of the population were male. The DAS28 was normally distributed with an average DAS28 of 3.8 (SD: 1.54) and average Rheumatoid Disease Comorbidity Index (RDCI) of 2.2 (SD: 1.6).
Model development and testing
The clinical experts identified 253 a priori claims-based variables representing clinical concepts thought to be associated with the DAS28. After applying the restriction that variables must be present in >1% of the population we ended up with 175 potential predictor variables. After model development with the LASSO regularized regression, the final model contained 32 variables and the adjusted R-square was 0.221 (Table 2). The “all predictors” and prescreening models started with different initial potential predictor variables but produced similar cross-validated adjusted R-square values, 0.221 and 0.223, respectively.
Table 2.
Model validation by initial set of predictor variables
| Variable sets | All clinical predictors | All predictors | Prescreening |
|---|---|---|---|
| Potential predictors | 253 | 1275 | 279 |
| Potential predictors with ≥1% prevalence (i.e., predictors put into model) | 175 | 567 | 230 |
| Predictors in final model | 32 | 45 | 46 |
| Fivefold cross-validated R-square (test) | 0.237 | 0.243 | 0.246 |
| Fivefold cross-validated Adj R-square (test) | 0.221 | 0.221 | 0.223 |
| <5 Years of RA disease Adj R-square | 0.218 | 0.190 | 0.196 |
| ≥5 years of RA disease Adj R-square | 0.186 | 0.185 | 0.185 |
RA rheumatoid arthritis, Adj adjusted
Review of the scatter plots presented in Fig. 1a-c show that the predicted DAS28 did not contain the same range of values as the true DAS28. The predicted DAS28 overestimated those with low DAS28 and underestimated the predicted value for Veteran patients with high DAS28.
Fig. 1.
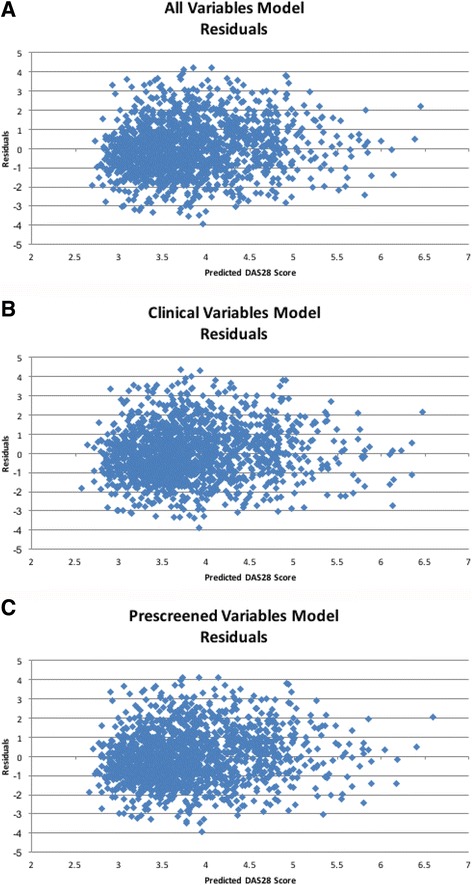
Predicted 28-joint disease activity score (DAS28) vs true DAS28 for test data. a Clinical predictors. b All predictors. c Pre-screened variables
Model-retained predictor variables
Variables selected and their standardized estimates for each model are presented in Appendix 2: Tables 5-7. Variables are ordered by the magnitude of the standardized estimate. Healthcare utilization (total visit count, primary care visits and occupational health visits) were relatively strong predictors of higher DAS28. Starting a new DMARD (biologic or non-biologic) 14 days after the DAS28 measurement was also consistently associated with higher DAS28. Higher baseline proportion of days covered (PDC) for DMARDs during the prior year was associated with lower DAS28. Measures indicating higher comorbidity, such as the RDCI and number of distinct VA drug classes were associated with higher DAS28. In the two models that used grouping software, we found analgesics, antidepressants and other agents acting on the central nervous system to be associated with higher DAS28. Please review Appendix 2 for a complete list of variables retained in each model.
Secondary analysis: correct classification of disease activity categories
The overall CCR for correctly classifying patients with the predicted DAS28 into clinical categories based on the true DAS28 ranged from 39.9% to 40.5% (Table 3). The true positive rate (TPR), which essentially represents measurement sensitivity, was fairly low in the group classified as having high disease activity by the predicted DAS28 and ranged from 9.9% to 10.8% (Table 3), while the positive predicted value (PPV) ranged from 57.9% to 63.0%. The TPR for those classified as having moderate disease ranged from 84.6% to 87.6%, while the PPV ranged from 42.5% to 43.0%. The TPR for low disease acitivity ranged from 17.9% to 20.2%, while the PPV ranged from 21.0% to 21.6%. None of the prediction models developed and tested accurately classified patients with remission. The TPR ranged from 0.0% to 0.3%, while the PPV ranged from 100% to 0%. Attempts to statistically define the cut points for the predicted DAS28 to optimize correct classification did not meaningfully improve the CCR. The optimized CCR only increased by approximately 3% (not presented).
Table 3.
Classification accuracy by disease activity category
| All clinical predictors | All predictors | Prescreening | |||
|---|---|---|---|---|---|
| 4 Categories | High (>5.1) | TPR | 10.5% | 9.9% | 10.8% |
| PPV | 57.9% | 62.0% | 63.0% | ||
| Moderate (3.2–5.1) | TPR | 84.6% | 87.6% | 86.9% | |
| PPV | 42.5% | 43.0% | 43.0% | ||
| Low (2.6–3.1) | TPR | 20.2% | 17.9% | 18.3% | |
| PPV | 21.6% | 21.2% | 21.0% | ||
| Remission (<2.6) | TPR | 0.3% | 0.0% | 0.0% | |
| PPV | 100.0% | 0.0% | 0.0% | ||
| CCR (95% CI) | 39.9% (37.5–42.3%) | 40.5% (38.1–43.0%) | 40.5% (38.1–43.0%) | ||
CCR correct classification rate, TPR true positive rate, PPV positive predicted value
Discussion
This study developed and internally validated statistical models to predict RA disease activity using data available in administrative claims data but was not successful in establishing a high level of predictive value. The relatively low adjusted R-square value and the inability to accurately classify patients into categories of disease activity using the predicted DAS28, draw into question the ability of a claims-based predictor to successfully represent patient disease activity in RA.
The sensitivity analysis focused on development of multiple models based on the initial pool of variables and applying these models to subsets of patients with <5 years of RA disease and ≥5 years of disease. This cut point was chosen because it has been used in other studies (e.g., TICORA 2004 study) [19] to represent early disease and because the data did not support comparisons with earlier cut-points.
The initial pool of predictors did not impact predictive accuracy, as the three models had similar adjusted R-square values. The models performed slightly better for patients with <5 year of disease. Similar results were found for patients with <2 years of disease (not presented). Duration of RA disease was recorded at VARA enrollment and would not be available in claims data, but could be approximated based on duration of enrollment and indicators of disease in claims-based data.
Variables retained in the three models were intuitive and interpretable. Variables indicating increased healthcare utilization, comorbidities, the use of agents that act on the central nervous system, and new DMARD prescriptions after the DAS28 measurement were associated with higher DAS28. Variables indicating longer exposure and a higher proportion of days covered by DMARDs in the baseline period were associated with lower DAS28. Even though many variables were associated with DAS28 the models poorly explained the variation in DAS28.
The classification accuracy of predicted DAS28 was evaluated by categorizing the true DAS28 and predicted DAS28 into remission (<2.6), low disease activity (2.6–3.1), moderate disease activity (3.2–5.1), and high disease activity (>5.1). The overall classification accuracy across the three models was modest. The models were poor predictors of remission and high levels of disease activity, which is likely due to the relatively small number of Veterans in the lower and higher end of the DAS28 scale. They performed best at classifying patients with moderate disease activity, which is the range for the majority of the population. In an additional analysis (not presented), we identified the optimal cut points of the predicted DAS28 to correctly classify patients by true DAS28 category of disease activity but were only able to increase classification accuracy to 43% across the three models.
A recent study evaluating the accuracy of a claims-based model to predict DAS28-CRP also performed poorly and found other claims-based measures of RA disease severity were not well correlated with true DAS28-CRP. Desai et al. (2015) [5] evaluated the claims-based index for RA severity (CIRAS) developed by Ting et al. [3] using a Delphi panel and found poor correlation with the true DAS28-CRP. They added additional variables to CIRAS that included medical claims for rheumatoid lung involvement, hand surgery, tuberculin test ordered and anti-CCP test orders. Furthermore, they also added pharmacy claims for steroids, opioids, non-steroidal anti-inflammatory drugs (NSAIDs), number of non-biologic DMARDs, and number of biologic DMARDs, and found the model R-square value (0.23) was similar to ours, even though they had a relatively small sample of Medicare patients (n = 315). They concluded that CIRAS may not approximate RA disease in observational cohorts and its use for confounding adjustment should be carefully considered. They also concluded that claims-based algorithms developed for clinical disease activity should be rigorously tested in a population with actual measures of disease activity to establish their generalizability before implementing in research. Our study leveraged a substantially larger population and rigorously tested our models to reduce the likelihood of overfitting the models to the data, yet had similar results.
Strength and limitations
The primary strength of this study was the access to DAS28 in a relatively large number of patients. This is the largest study that attempted to train and validate a claims-based predictor of RA disease activity using the actual DAS28. In addition, we used statistical methods that supported high-dimensional variable selection and prevented overfitting the model to the actual data. Of note, we replicated model development and classification accuracy using the Clinical Disease Activity Index (CDAI) and found similar adjusted R-square values and classification accuracy (results not presented).
One weakness of this study is that the population studied may not represent average RA patients. Veterans tend to be older and more likely male than the general population. Another weakness of this study was the reliance on claims-based predictors. Even though observational comparative effectiveness and safety studies often rely on commercial and Federal claims databases there is a new paradigm for population health analytics that involves the integration of the electronic health record with claims data. Accurate prediction models of disease activity will likely require integration of clinical data, such as laboratory test results and information captured in structured electronic health data or in medical notes. The use of standardized templates would be required to extract components of disease activity scores, such as the number of swollen or tender joints, and used in models to predict future disease activity and to better understand what features of the disease activity score influence changes in treatment patterns. Our future work aims to develop natural language processing tools to extract components of the DAS28 from templated notes within the VA and use this information along with other clinical data in the development of future RA disease activity prediction models.
Conclusions
The prediction models developed and tested found a relatively low level of predictive accuracy, drawing into question their use for confounding adjustment or to evaluate treatment decisions in patients with predicted DAS28. Our findings are consistent with other recent studies that attempted to use claims-based data to predict RA disease activity. Future work to predict disease activity in patient populations should incorporate clinical data from the electronic health record in addition to key variables available in administrative claims data.
Acknowledgements
This material is based upon work supported by Amgen, the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development and Value and Epidemiology Research using Causal Inference and Data Science (VERITAS). The authors would like to thank Tina Huynh for her administrative support.
Funding
This work was funded by Amgen Inc. Supplemental funding was provided by a Veterans Affairs Health Services Research and Development Award.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available because they obtain protected health information (PHI) but the codes and protocols will be shared if requested. Investigators who have Veterans Affairs credentialing and obtain data use approvals will be able to gain access to the data used for this study.
Authors’ contributions
All authors contributed to the design and interpretation of the study. BCS, GWC, C-CT, and ZB accessed and analyzed the data. BCS and GWC obtained funding and provided project management. BCS provided the initial draft of the manuscript. All authors read and contributed to revisions and approved the final manuscript.
Competing interests
Brian C. Sauer is employed by the University of Utah and Salt Lake City Veterans Affairs Medical Center and received research grant funding from Amgen Inc. Chia-Chen Teng is employed by the University of Utah and received research grant funding from Amgen Inc. Neil A. Accortt is employed by Amgen Inc. and holds stock in Amgen Inc. Zachary Burningham is employed by the University of Utah and Salt Lake City Veterans Affairs Medical Center and received research grant funding from Amgen Inc. David Collier and Mona Trivedi are employed by Amgen Inc. and hold stock in Amgen Inc. Grant W. Cannon is employed by the University of Utah and Salt Lake City Veterans Affairs Medical Center and received research grant funding from Amgen Inc.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The research was approved by the Institutional Review Board of the University of Utah (IRB_00012917), Scientific, Ethical, and Advisory Committee (SEAC) of VARA, and reviewed by the Salt Lake City VA research review committee. Consent from patients involved in the study was not required due to the waiver of authorization.
Disclaimer
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- BRASS
Brigham Women’s Hospital Rheumatoid Arthritis Sequential Study
- CCR
Correct classification rate
- CCS
Clinical Classification System
- CDAI
Clinical Disease Activity Index
- CDW
Corporate Data Warehouse
- CIRAS
Claims-base Index for Rheumatoid Arthritis Severity
- DAS28
28-Joint Disease Activity Score
- DAS28-CRP
C-reactive protein-based 28-Joint Disease Activity Score
- DMARD
Disease modifying anti-rheumatic drug
- ESR
Erythrocyte sedimentation rate
- HCUP
Healthcare Cost and Utilization Project
- HSR&D
Health Services Research & Development Service
- LASSO
Least absolute shrinkage and selection operator
- MCA
Managerial Cost Accounting
- OIT
Office of Information and Technology
- PDC
Proportion of days covered
- PPV
Positive predicted value
- RA
Rheumatoid arthritis
- RDCI
Rheumatic Disease Comorbidity Index
- SEAC
Scientific, Ethical, and Advisory Committee
- TPR
True positive rate
- VA
Veterans Administration
- VARA
Veterans Affairs Rheumatoid Arthritis
- VINCI
Veterans Administration (VA) Informatics and Computing Infrastructure
Appendix 1
Table 4.
List of a priori Clinically Defined Predictors and their Measurement
| Measurement | Value | Variable | Table |
|---|---|---|---|
| Laboratory | |||
| Number ESR tests | 85651, 85652 | CPT | CDW.OutpatProcedure |
| Number CRP tests | 86140 | CPT | CDW.OutpatProcedure |
| aCCP – (Y/N) | 86200 | CPT | CDW.OutpatProcedure |
| RF – (Y/N) | 86431 | CPT | CDW.OutpatProcedure |
| Number. complete blood counts | 85025 | CPT | CDW.OutpatProcedure |
| Number. chemistry panels ordered or any electrolyte | 80053, 82248, 82465, 82977, 83540, 83615, 84100, 84478, 84550 | CPT | CDW.OutpatProcedure |
| Radiology | |||
| Radiographs (Y/N) | 70010-79999 | CPT | CDW.OutpatProcedure |
| Number radiographs | Count of 70010-79999 | CPT | CDW.OutpatProcedure |
| Hand or foot (Y/N) (toes, fingers, wrist) | 73620, 73630, 73650, 73660, 73100, 73110,73120, 73130 | CPT | CDW.OutpatProcedure |
| C-spine (Y/N) | 72040, 75052 | CPT | CDW.OutpatProcedure |
| Other bone x-ray (Y/N) | Master file | CPT | CDW.OutpatProcedure |
| Clinic Visits | |||
| Any visit | Any | stopcode | CDW.outpatVisit |
| Rheumatology | 314 | stopcode | CDW.outpatVisit |
| Primary care | 323, 342 | stopcode | CDW.outpatVisit |
| Orthopedic | 60, 509 | stopcode | CDW.outpatVisit |
| Physical Rehabilitation | 201, 250 | stopcode | CDW.outpatVisit |
| Occupational Therapy | 21, 206, 460 | stopcode | CDW.outpatVisit |
| Number ED visits | 130, 101 | stopcode | CDW.outpatVisit |
| Utilization | |||
| Number Inpatient stay | Row count per person | Admission date | Inpatient.inpatient |
| Unique Drug class codes | Row count per person | VAdrugclasscode | CDW.Rxoutpat |
| Procedures | |||
| Any surgery | 10021-6990 | CPT | |
| Any surgery | Master file | ICD9 | CDW.outpatProcedure, inpatProcedure, inpatientCPT |
| Hand surgery | 26500, 26502, 26504, 26494, 26989 | CPT | CDW.Outpat.Procedure, inpatientCPT |
| Hand surgery | Master filea | ICD9 | CDW.inpatientProcedure |
| Any orthopedic (include spine) surgery | Master file | CPT | CDW.inpatientCPT, Outpat.Procedure |
| Joint injections | Master file | Jcode | CDW.Outpat.Procedure, inpatientCPT |
| Comorbidity | |||
| RDCI RA comorbidity score | See published paper | ICD9 | CDW.outpatDiagnosis |
| Rheumatoid lung involvement | 714.81 | ICD9 | CDW.outpatDiagnosis |
| Felty’s syndrome | 714.1 | ICD9 | CDW.outpatDiagnosis |
| Sjogrens | 710.2 | ICD9 | CDW.outpatDiagnosis |
| Assistive Devices | |||
| Cane (Y/N) | Master file | CPT/ICD9 procedure | CDW.outpatProcedure, inpatProcedure |
| Crutch (Y/N) | Master file | CPT/ICD9 procedure | CDW.outpatProcedure, inpatProcedure |
| Walker (Y/N) | Master file | CPT/ICD9 procedure | CDW.outpatProcedure, inpatProcedure |
| Wheelchair (Y/N) | Master file | CPT/ICD9 procedure | CDW.outpatProcedure, inpatProcedure |
| Other Assist Device (Y/N) | Master file | CPT/ICD9 procedure | CDW.outpatProcedure, inpatProcedure |
| Medications dispensed | |||
| Number NSAID | MS102 | VA drug Class | CDW.Rxoutpatfill |
| Number Non-biologic DMARD | String search - list below | drugnamewithoutdose | CDW.Rxoutpatfill |
| Methotrexate (Y/N) | String search | drugnamewithoutdose | CDW.Rxoutpatfill |
| Leflunomide (Y/N) | String search | drugnamewithoutdose | CDW.Rxoutpatfill |
| Sulfasalazine (Y/N) | String search | drugnamewithoutdose | CDW.Rxoutpatfill |
| Hydroxychloroquine (Y/N) | String search | drugnamewithoutdose | CDW.Rxoutpatfill |
| Azathioprine (Y/N) | String search | drugnamewithoutdose | CDW.Rxoutpatfill |
| TNFi (Y/N) | String search: etanercept, adalimumab, infliximab, golimumab, certolizumab | drugnamewithoutdose | CDW.MCA, Rxoutpatfill, outpatProcedure, TIU notes |
| Other biologics | rituximab, abatacept, anakinra, tocilizumab, | drugnamewithoutdose | CDW.MCA, Rxoutpatfill, outpatProcedure, TIU notes |
| Tofacitinib (Y/N) | String search | drugnamewithoutdose | CDW.Rxoutpatfill |
| Glucocorticosteroids (Y/N and Dose) | HS051 | VA drug Class | CDW.MCA and Rxoutpatfill |
| Minor DMARDs (Any Y/N) | Doxycyline, minocycline, auranofin, d-penicillamine, cyclosporine | drugnamewithoutdose | CDW.Rxoutpatfill |
| Smoking cessation medication (Y/N) | Chantix Nicotine substitutes | Drugnamewithoutdose | CDW.Rxoutpatfill |
| Processed Medication Data for DMARDs | |||
| Days since start med | All meds | drugnamewithoutdose | CDW.Rxoutpatfill |
| Days since end med (90-day gap to end) | All meds | drugnamewithoutdose | CDW.Rxoutpatfill |
| PDC from start therapy to end of observation period | All meds | drugnamewithoutdose | CDW.Rxoutpatfill |
| Demographics | |||
| Age | Age | DOB | CDW.patient |
| Gender | M/F | Gender | CDW.patient |
aMaster File = primary excel workbook containing all measured concepts and is available by request (brian.sauer@utah.edu)
ESR erythrocyte sedimentation rate, CRP c-reactive protein, PDC proportion of days covered
Appendix 2
Table 5.
Model Generated from Clinically Defined Predictors
| Effect | Estimate | Standardized Est |
|---|---|---|
| Intercept | 4.639526 | 0 |
| Baseline Visit Count | 0.001981 | 0.02366 |
| Baseline RDCI Score | 0.005026 | 0.00521 |
| Baseline Labtest Days for Chem Panel | -0.001423 | -0.0026 |
| Baseline Primary Care Visit Count | 0.005222 | 0.01475 |
| Baseline Occupational Visit Count | 0.010707 | 0.01553 |
| Bupropion Rx in Baseline (Y/N) | 0.106174 | 0.0135 |
| Distinct VA Drug Class Rx | 0.030526 | 0.13957 |
| Joint Injection Count | 0.019454 | 0.0097 |
| Rheumatism, Unspecified And Fibrosis Dx Count (ICD:729) | 0.008102 | 0.00519 |
| Baseline Surgery Count | -0.058006 | -0.0162 |
| Days End of Prednisone | -0.000912 | -0.09845 |
| Days End of Sulfasalazine | -0.000063599 | -0.00505 |
| Baseline PDC for Etanercept | -0.152669 | -0.02073 |
| Days Start of Golimumab | -0.001374 | -0.00927 |
| Baseline PDC for Non-Biologic DMARDs | -0.708075 | -0.16342 |
| Start Methotrexate in 14 Days after Index Date (Y/N) | 0.077462 | 0.01148 |
| Start Leflunomide in 14 Days after Index Date (Y/N) | 0.073709 | 0.00598 |
| Start in TNFi Biologic DMARDs in 14 Days after Index Date (Count of distinct Rx) | 0.542521 | 0.06171 |
| Start in Non-Biologic DMARDs in 14 Days after Index Date (Count of distinct Rx) | 0.380811 | 0.09612 |
| Start in Steroid in 14 Days after Index Date (Count of distinct Rx) | 0.45952 | 0.06632 |
| Rheumatism, Unspecified And Fibrosis Dx (ICD:729) (Y/N) | 0.003294 | 0.00075 |
| Baseline Labtest for Chem Panel (Y/N) | -0.482788 | -0.0294 |
| Baseline Labtest for RF (Y/N) | 0.022162 | 0.00714 |
| Baseline Foot Surgery (Y/N) | 0.037806 | 0.01158 |
| Baseline Hand Surgery (Y/N) | 0.105081 | 0.02942 |
| Baseline Occupational Visit (Y/N) | 0.116702 | 0.02344 |
| Baseline Rheumatology Visit (Y/N) | -0.033104 | -0.00143 |
| Start in Non-Biologic DMARDs in 14 Days after Index Date (Y/N) | 0.340854 | 0.07459 |
| Start in DMARDs in 14 Days after Index Date (Y/N) | 0.590044 | 0.08356 |
| Baseline Use of Sulfasalazine (Y/N) | 0.158241 | 0.03893 |
| Baseline Use of Rituximab (Y/N) | 0.112073 | 0.00872 |
| Baseline Use of Infliximab (Y/N) | 0.003816 | 0.00057 |
Table 6.
Model Generated from All Predictors
| Effect | Estimate | Standardized Est |
|---|---|---|
| Intercept | 4.027342 | 0 |
| Baseline Visit Count | 0.002189 | 0.02615 |
| Baseline Occupational Visit Count | 0.008477 | 0.01229 |
| Bupropion Rx in Baseline (Y/N) | 0.020813 | 0.00265 |
| Non-Opioid Analgesics Rx Count (CN103) | 0.001982 | 0.005 |
| Sedative/Hypnotics, Other Rx Count (CN309) | 0.002925 | 0.00222 |
| Tricyclic Antidepressants Rx Count (CN601) | 0.001475 | 0.00207 |
| Local Anesthetics, Topical Rx Count (DE700) | 0.016648 | 0.00492 |
| Calcium Rx Count (TN402) | -0.050907 | -0.01654 |
| Decongestants, Systemic Rx Count (RE200) | 0.030669 | 0.00639 |
| Platelet Aggregation Inhibitors Rx Count (BL700) | 0.001719 | 0.00095 |
| Distinct VA Drug Class Rx | 0.017323 | 0.07921 |
| Baseline Surgery Count | -0.007242 | -0.00202 |
| Days End of Prednisone | -0.000873 | -0.09417 |
| Baseline PDC for Etanercept | -0.102578 | -0.01393 |
| Days Start of Golimumab | -0.000198 | -0.00133 |
| Baseline PDC for Non-Biologic DMARDs | -0.662683 | -0.15295 |
| Start Methotrexate in 14 Days after Index Date (Y/N) | 0.037588 | 0.00557 |
| Start in TNFi Biologic DMARDs in 14 Days after Index Date (Count of distinct Rx) | 0.446665 | 0.05081 |
| Start in Non-Biologic DMARDs in 14 Days after Index Date (Count of distinct Rx) | 0.352313 | 0.08893 |
| Start in Steroid in 14 Days after Index Date (Count of distinct Rx) | 0.173564 | 0.02505 |
| Disease of Mouth Excluding Dental Dx Count in Baseline (CCS137) | 0.03199 | 0.00289 |
| Calculus of Urinary Tract Dx Count in Baseline (CCS160) | -0.013249 | -0.00541 |
| Other Non-Traumatic Joint Disorders Dx Count in Baseline (CCS204) | 0.000382 | 0.00074 |
| Other Connective Tissue Disease Dx Count in Baseline (CCS211) | 0.00293 | 0.00464 |
| Disease of White Blood Cells Dx Count in Baseline (CCS63) | 0.044243 | 0.00827 |
| Conditions Associated With Dizziness or Vertigo Dx Count in Baseline (CCS93) | 0.005453 | 0.00187 |
| Baseline Labtest for Chem Panel (Y/N) | -0.314001 | -0.01912 |
| Baseline Foot Surgery (Y/N) | 0.006726 | 0.00206 |
| Baseline Hand Surgery (Y/N) | 0.106317 | 0.02977 |
| Opioid Analgesics Rx (CN101) (Y/N) | 0.183042 | 0.05861 |
| Non-Opioid Analgesics Rx (CN103) (Y/N) | 0.065908 | 0.02006 |
| Tricyclic Antidepressants Rx (CN601) (Y/N) | 0.080738 | 0.01271 |
| Antidepressants, Other Rx (CN609) (Y/N) | 0.059894 | 0.01824 |
| CNS Medications, Other Rx (CN900) (Y/N) | 0.047949 | 0.00365 |
| Loop Diuretics Rx (CV702) (Y/N) | 0.073401 | 0.01455 |
| Diagnostics, Other Rx (DX900) (Y/N) | 0.142061 | 0.03273 |
| Insulin Rx (HS051) (Y/N) | 0.002114 | 0.00069 |
| Thyroid Supplements Rx (HS851) (Y/N) | 0.00651 | 0.0013 |
| Immune Suppressants Rx (IM600) (Y/N) | 0.033029 | 0.0059 |
| Calcium Rx (TN420) (Y/N) | -0.080805 | -0.01165 |
| Baseline Occupational Visit (Y/N) | 0.045223 | 0.00908 |
| Start in Non-Biologic DMARDs in 14 Days after Index Date (Y/N) | 0.375004 | 0.08206 |
| Start in DMARDs in 14 Days after Index Date (Y/N) | 0.816375 | 0.11562 |
| Baseline Use of Sulfasalazine (Y/N) | 0.144504 | 0.03555 |
| Baseline Use of Rituximab (Y/N) | 0.028977 | 0.00226 |
Table 7.
Model Generated from Pre-screened Predictors
| Effect | Estimate | Standardized Est |
|---|---|---|
| Intercept | 4.268844 | 0 |
| Baseline Visit Count | 0.001667 | 0.01991 |
| Baseline Primary Care Visit Count | 0.000924 | 0.00261 |
| Baseline Occupational Visit Count | 0.011031 | 0.016 |
| Bupropion Rx in Baseline (Y/N) | 0.052414 | 0.00666 |
| Non-Opioid Analgesics Rx Count (CN103) | 0.003163 | 0.00798 |
| Anti-rheumatics, Other Rx Count (MS190) | -0.000129 | -0.00032 |
| Sedative/Hypnotics, Other Rx Count (CN309) | 0.00711 | 0.0054 |
| Tricyclic Antidepressants Rx Count (CN601) | 0.002659 | 0.00374 |
| Local Anesthetics, Topical Rx Count (DE700) | 0.026352 | 0.00779 |
| Soaps/Shampoos/Soap-Free Cleansers Rx Count (DE400) | 0.012432 | 0.00283 |
| Decongestants, Systemic Rx Count (RE200) | 0.055989 | 0.01166 |
| Distinct VA Drug Class Rx | 0.014658 | 0.06702 |
| Joint Injection Count | 0.003921 | 0.00196 |
| Days End of Prednisone | -0.000913 | -0.09852 |
| Baseline PDC for Etanercept | -0.131689 | -0.01788 |
| Days Start of Golimumab | -0.000651 | -0.00439 |
| Baseline PDC for Non-Biologic DMARDs | -0.672468 | -0.1552 |
| Start Methotrexate in 14 Days after Index Date (Y/N) | 0.04705 | 0.00697 |
| Start Leflunomide in 14 Days after Index Date (Y/N) | 0.013983 | 0.00113 |
| Start in TNFi Biologic DMARDs in 14 Days after Index Date (Count of distinct Rx) | 0.471838 | 0.05367 |
| Start in Non-Biologic DMARDs in 14 Days after Index Date (Count of distinct Rx) | 0.364512 | 0.09201 |
| Start in Steroid in 14 Days after Index Date (Count of distinct Rx) | 0.175888 | 0.02539 |
| Varicose Veins of Lower Extremity (CCS119) | 0.020937 | 0.00268 |
| Disease of Mouth Excluding Dental Dx Count in Baseline (CCS137) | 0.064254 | 0.00581 |
| Other Connective Tissue Disease Dx Count in Baseline (CCS211) | 0.003949 | 0.00625 |
| Disease of White Blood Cells Dx Count in Baseline (CCS63) | 0.066725 | 0.01247 |
| Conditions Associated With Dizziness or Vertigo Dx Count in Baseline (CCS93) | 0.013165 | 0.0045 |
| Baseline Lab test for Chem Panel (Y/N) | -0.378938 | -0.02308 |
| Baseline Lab test for RF (Y/N) | 0.001583 | 0.00051 |
| Baseline Foot Surgery (Y/N) | 0.019935 | 0.00611 |
| Baseline Hand Surgery (Y/N) | 0.10473 | 0.02932 |
| Opioid Analgesics Rx (Y/N) | 0.190656 | 0.06105 |
| Non-Opioid Analgesics Rx (CN103) (Y/N) | 0.070215 | 0.02137 |
| Tricyclic Antidepressants Rx (CN601) (Y/N) | 0.098618 | 0.01553 |
| Antidepressants, Other Rx (CN609) (Y/N) | 0.064811 | 0.01974 |
| CNS Medications, Other Rx (CN900) (Y/N) | 0.095795 | 0.00729 |
| Loop Diuretics Rx (CV702) (Y/N) | 0.084218 | 0.01669 |
| Diagnostics, Other Rx (DX900) (Y/N) | 0.15962 | 0.03678 |
| Insulin Rx (HS501) (Y/N) | 0.013138 | 0.00212 |
| Thyroid Supplements Rx (HS851) (Y/N) | 0.02656 | 0.00532 |
| Antigout Agents Rx (MS400) (Y/N) | 0.003596 | 0.00046 |
| Baseline Occupational Visit (Y/N) | 0.052566 | 0.01056 |
| Start in Non-Biologic DMARDs in 14 Days after Index Date (Y/N) | 0.357809 | 0.0783 |
| Start in DMARDs in 14 Days after Index Date (Y/N) | 0.834045 | 0.11812 |
| Baseline Use of Sulfasalazine (Y/N) | 0.157077 | 0.03865 |
| Baseline Use of Rituximab (Y/N) | 0.08026 | 0.00625 |
Contributor Information
Brian C. Sauer, Phone: (801) 582-1565, Email: brian.sauer@utah.edu
Chia-Chen Teng, Email: jenny.teng@hsc.utah.edu.
Neil A. Accortt, Email: naccortt@amgen.com
Zachary Burningham, Email: zach.burningham@hsc.utah.edu.
David Collier, Email: collierd@amgen.com.
Mona Trivedi, Email: monat@amgen.com.
Grant W. Cannon, Email: grant.cannon@va.gov
References
- 1.Scott DL, Wolfe F, Huizinga TWJ. Rheumatoid arthritis. Lancet. 2010;376(9746):1094–108. doi: 10.1016/S0140-6736(10)60826-4. [DOI] [PubMed] [Google Scholar]
- 2.Helmick CG, Felson DT, Lawrence RC, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part I. Arthritis Rheum. 2008;58(1):15–25. doi: 10.1002/art.23177. [DOI] [PubMed] [Google Scholar]
- 3.Ting G, Schneeweiss S, Scranton R, Katz J, Weinblatt M, Young M, et al. Development of a health care utilisation data-based index for rheumatoid arthritis severity: a preliminary study. Arthritis Res Ther. 2008;10:R95. doi:10.1186/ar2482. [PMC free article] [PubMed] [Cross Ref]. [DOI] [PMC free article] [PubMed]
- 4.Baser O, Du J, Xie L, Wang H, Dysinger AH, Wang L. Derivation of severity index for rheumatoid arthritis and its association with healthcare outcomes. J Med Econ. 2012;15(5):918–24. doi: 10.3111/13696998.2012.688905. [DOI] [PubMed] [Google Scholar]
- 5.Desai RJ. An external validation study reporting poor correlation between the claims-based index for rheumatoid arthritis severity and the disease activity score. Arthritis Res Ther. 2015;17(1):1–5. doi: 10.1186/s13075-015-0599-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mikuls TR, Reimold A, Kerr GS, Cannon GW. Insights and implications of the VA Rheumatoid Arthritis Registry. Fed Pract. 2015;32:24–9. [PMC free article] [PubMed] [Google Scholar]
- 7.Cannon GW, Mikuls TR, Hayden CL, et al. Merging Veterans Affairs rheumatoid arthritis registry and pharmacy data to assess methotrexate adherence and disease activity in clinical practice. Arthritis Care Res (Hoboken) 2011;63(12):1680–90. doi: 10.1002/acr.20629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fihn SD, Francis J, Clancy C, et al. Insights from advanced analytics at the Veterans Health Administration. Health Aff. 2014;33(7):1203–11. doi: 10.1377/hlthaff.2014.0054. [DOI] [PubMed] [Google Scholar]
- 9.HCUP. HCUP CCS. Healthcare Cost and Utilization Project (HCUP). www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp. Accessed 24 Apr 2017.
- 10.Sato M, Schneeweiss S, Scranton R, et al. The validity of a rheumatoid arthritis medical records-based index of severity compared with the DAS28. Arthritis Res Ther. 2006;8(3):R57. doi: 10.1186/ar1921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Prevoo ML, Hof MA v ‘t, Kuper HH, van Leeuwen MA, van de Putte LB, van Riel PL. Modified disease activity scores that include twenty-eight-joint counts. Development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum. 1995;38(1):44–8. doi: 10.1002/art.1780380107. [DOI] [PubMed] [Google Scholar]
- 12.HCUP. Surgical Flag Software. Healthcare Cost and Utilization Project (HCUP). www.hcup-us.ahrq.gov/toolssoftware/surgflags/surgeryflags.jsp. Accessed 24 Apr 2017.
- 13.Weiser TG, Semel ME, Simon AE, et al. In-hospital death following inpatient surgical procedures in the United States, 1996–2006. World J Surg. 2011;35(9):1950–6. doi: 10.1007/s00268-011-1169-5. [DOI] [PubMed] [Google Scholar]
- 14.England BR, Sayles H, Mikuls TR, Johnson DS, Michaud K. Validation of the Rheumatic Disease Comorbidity Index. Arthritis Care Res (Hoboken) 2015;67(6):865–72. doi: 10.1002/acr.22456. [DOI] [PubMed] [Google Scholar]
- 15.Tibshirani R. Regression shrinkage and selection via the lasso. J R Stat Soc Ser B. (…. 1996. https://statweb.stanford.edu/~tibs/lasso/lasso.pdf.
- 16.Gunes F. Penalized regression methods for linear models in SAS/STAT®. https://support.sas.com/rnd/app/stat/papers/2015/PenalizedRegression_LinearModels.pdf.
- 17.David W, Hosmer J, Lemeshow S, Sturdivant RX. Applied logistic regression. Hoboken: John Wiley & Sons; 2013. doi:10.1002/9781118548387
- 18.Agresti A. Dealing with discreteness: making ‘exact’ confidence intervals for proportions, differences of proportions, and odds ratios more exact. Stat Methods Med Res. 2003;12(1):3–21. doi: 10.1191/0962280203sm311ra. [DOI] [PubMed] [Google Scholar]
- 19.Grigor C, Capell H, Stirling A, et al. Effect of a treatment strategy of tight control for rheumatoid arthritis (the TICORA study): a single-blind randomised controlled trial. Lancet. 2004;364(9430):263–9. doi: 10.1016/S0140-6736(04)16676-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analyzed during the current study are not publicly available because they obtain protected health information (PHI) but the codes and protocols will be shared if requested. Investigators who have Veterans Affairs credentialing and obtain data use approvals will be able to gain access to the data used for this study.


