Abstract
Background
The chief aim of this study was to enlist the ethnobotanical uses of wild plants in district Sheikhupura, province Punjab, Pakistan. Due to extreme geographical and climatic conditions, Pakistan has a great floral diversity. Plants have been used by the indigenous people for treatment of different ailments since long. They are still dependent on the plants for their domestic purposes. Moreover, plants are used as first aid to treat diverse ailments such as cold, cough, influenza, asthma, cancer, antidote, gastric and hepatic disorders. The traditional uses of medicinal plants lead to the discovery of natural drugs. This is first quantitative ethnobotanical documentation of medicinal plants in NavaPind and ShahpurVirkan district Sheikhupura, province Punjab, Pakistan.
Methods
This ethnobotanical information was collected from about 400 informants including male and female. Sample size was determined by statistical formula. The informative data was based on semi-structured interviews, group discussions, Questionnaire and field visits. Then the data was analyzed by applying different quantitative indices such as Informant Consent Factor (ICF), Use value (UV), Relative Frequency of Citation (RFC), the Fidelity level (FL) and Jaccard Index (JI).
Results
Almost 96 plants belonging to 34 families were reported. Most-frequently cited families were Poaceae (16 species) and Fabaceae (15 species). The most dominant life form was herbs (30.20%). The most-used plant parts were leaves (31.14%), followed by whole plant (24.59%), Most common mode of administration is extraction (81.25%). Generally herbal medicines were acquired from fresh plant material. Among all 54.16% plants were toxic, 31.25% were nontoxic, whereas the remaining 14.58% may be toxic or nontoxic because of their dual attitude. Almost 34 species were reported with their different medicinal uses as has been reported in literature.
Conclusions
This ethnobotanical documentation revealed that the plants are still used by natives of rural areas in their day-to-day lives. This study provides basis for the conservation of local flora. Plants with high ICF, UV and FL can be further used for phytochemical and pharmacological studies. This documentation could provide baseline information which can be used to develop new plant-based commercial drugs.
Electronic supplementary material
The online version of this article (doi:10.1186/s13002-017-0151-1) contains supplementary material, which is available to authorized users.
Keywords: Ethnobotany, Fabaceae, Medicinal plant, Poaceae, Traditional knowledge
Background
Ethnobotanical assessment of medicinal plant species is prerequisite for conservation, protection, and development of herbal drugs [1–3]. Plant and plant products play an important part in the material culture of many of the world’s native societies. Since the start of humanity extraction and processing of the medicinal plants to cure diseases is in practice. It also subsidizes economic uplifting of deprived areas [4]. Moreover, ethnobotanical studies indicated the importance of medicinal species within the local sociocultural context. This sort of study may support the socioeconomic conditions of an area; preserve the indigenous plant-based knowledge of the local communities and ultimately leads to conserve the global heritage [5, 6]. It provides a baseline for the discovery of new active compounds from the plants and being used directly as patent drugs. There are over 20,000 species of wild edible plants in the world, yet fewer than 20 species now provide 90% of our food [7]. The relationship between food and health has become significant increasingly. As nowadays consumers demand healthy, tasty and natural functional foods that have been grown in uncontaminated environment.
Wild resources of medicinal plants have been used by man for eras in conventional healing systems. Almost every country of the world follows herbs and some traditional medicine systems very efficiently. In developing countries about 65–80% of the population depends essentially on plants for their primary health care [8, 9]. In Indo-Pak Subcontinent, these herbs and traditional systems are known as Unani or Ayurveda system [10]. Pakistan is included in those countries where traditional Unani medicine is popularly practiced among the large segment of populations. The Unani medicine system originated in Greece was found by ancient Greek philosophers. It was documented and adopted by Muslims during the glorious period of Islamic civilization. Unani medicine system was brought to Indo–Pak subcontinent by Muslims scholars and practiced for centuries. It benefited from the Ayu system of medicine, which was an important component of Hindu civilization. Traditional Unani medicines were greatly depending on medicinal plants, apart from the animals and minerals [11, 12]. However, despite of the rich heritage of knowledge on the uses of plant drugs, little attention had been paid to document them in the country till the latter part of the nineteenths century. From 1996 to date, a number of ethnobotanical investigations in various geographical regions of Pakistan had been conducted [9, 13–16]. Pie and Manadhara [17] reported that in Himalayan ranges almost 70% of the medicinal plants and animals in the region consist of wild species. Globally, about 85% of all medications for primary health care are derived from plants [18]. So, there is need to explore either the areas have treasure of knowledge about the medicinal uses of plants and bring them into documentation to save ethnobotanical information and plant life [19].
Pakistan, comprises of nine major ecological zones and four phytogeographical zones, is bestowed with unique biodiversity. The country has about 6000 species of wild plants of which about 400–600 are considered to be medically important [20]. Till mid of the 20th century, more than 80% of Pakistani population was dependent on ethnomedicines for their primary health care. Because of modernizing trends, now traditional system is largely experienced only in the rural areas. Natural resources and cultures are under the pressure of continuous change derived by these trends.
The village NavaPind and ShahpurVirkan district Sheikhupura are floristically quite rich tropical regions of Punjab. Ethnobotanical study of this area has never been conducted. The climate of the area is subjected to extreme variations. Wheat, Rice and Sugarcane are the main cash crops. Guavas, Strawberries and Citrus are grown at a larger scale in this district. Literacy rate of the villages is very low. Generally it is observed that most men in these areas are engaged in unskilled labor, while women are self-employed in petty trade of agriculture especially in the collection and trade of wild food and medicinal plants. Mostly plants are used for many purposes like food, shelter and therapeutic agents. However, lack of scientific knowledge about the useable parts, proper time of collection and wasteful methods of collection lead to mismanagement of these plants. So, the indigenous knowledge is going to be depleted, Hence ethnobotanical survey is planned for NavaPind and ShahpurVirkan district Sheikhupura, province Punjab to document the traditional uses of medicinal plants in the area before the information is lost. The main objective of present study was to document the indigenous therapeutic knowledge of plants. In addition to this it was also aimed to compile profile of medicinal plants by using quantitative indices like Use Values (UV), Relative Frequency Citation (RFC), Informant Consensus Factor (ICF), Fidelity Level (FL), Jacard Index (JI) and Relative Importance (RI) to evaluate available ethnobotanical data.
Methods
Study area
Sheikhupura an industrial city is formerly known as Kot Dayal Das. It is part of province Punjab. District Sheikhupura bounded on the North by Gujranwala district, North-East by Narowal district, West by Nankana Sahib District and East by Lahore district [21] (Fig. 1). Its Southern boundary is formed by district Kasur. District Sheikhupura is spread over an area of 3,241 square kilometers and comprises four tehsils of: 1) Sheikhupura, 2) Ferozewala, 3) Sharaqpur, 4) Sharif Muridke [21]. According to the 1998 census of Pakistan, the district has a population of 3,321,029 of 25.25% is urban. Rest of population is resident of town and villages. The overall literacy rate of this region is 43.8% and it is ranked 15th out of 34 district of Punjab in terms of literacy rate.
Fig. 1.
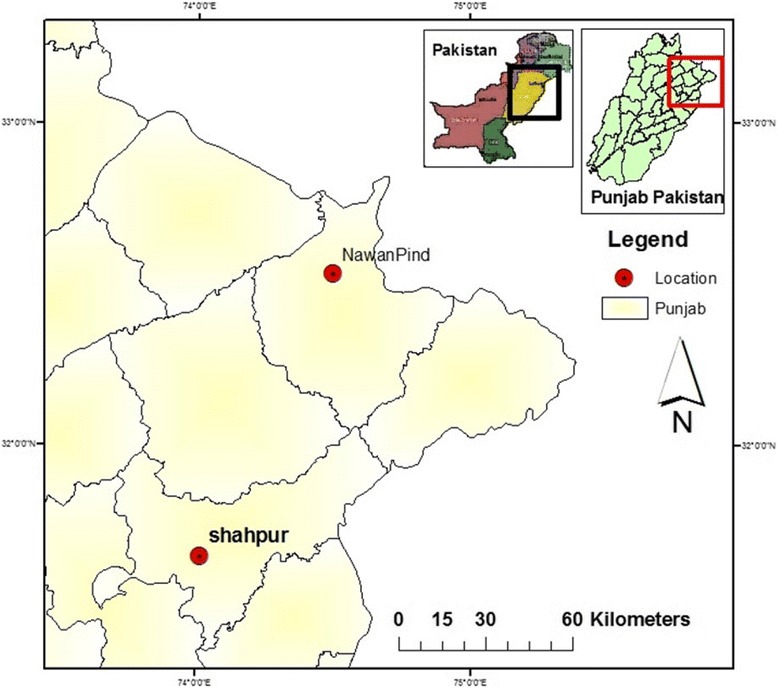
Map of NavaPind and Shahpur Virkan district Sheikhupura
From mid of December to mid March the air is very damp, cold and light to moderate, rain falls at intervals. In April the temperature rises fast and two successive months are very hot [21]. Towards the end of June Monsoon conditions appear and during the following two and a half months spells of rainy weather. The average rainfall in the district is about 635 mm. The fauna and flora of the area include: Kikar, Pipal, Bohar, Eucalyptus, Popular and Sharin [21]. Major cash crops usually grown in this area are wheat, rice and sugarcane while minor crops are maize, millet, sorghum, cotton and mash.
From an ethnographic point of view, the region is occupied by two religious communities, Muslims in the majority and Christians in the minority. The main languages spoken in the District Sheikhupura include Urdu and Punjabi. There is a lack of satisfactory health-care facilities, thus resulting in high maternal mortality rate (MMR) and infant mortality rate (IMR). Almost all ethnic groups use herbal medicines to cure different diseases, and these groups are rich with indigenous knowledge regarding the use of medicinal plants.
Experimentation
Experiment was conducted in two stages
Field work
Interview
Questionnaire
Inventory documentation
Quantitative analyses of enthnobotanical data
-
Field work:
The Study was carried out by interviewing 400 informants including male, female and herbalists of the study area during November 2014 to June 2015. Sample size was determined by following Kadam and Bhalerao [22]. For plant material and traditional information collection, trips were arranged during winter, spring summer time to cover all seasonal variations in vegetation. Before visiting the area permission was taken from Chairman (representative of local government) of Shahpur Virkan and NavaPind. Moreover, Chairman also helped us to hire a local person as guide to facilitate the process of data collection. The methodology was adopted by following the work of Ahmad et al. [23], Qureshi and Raza Bhatti [15]; Qureshi et al. [13] Yaseen et.al. [3]. The survey was unique as emphasis was on both male and female members of different ages of the community. Local people were interviewed. Questionnaire was also used. But the majority of the people were not very well educated therefore interviewee filled the questionnaire herself after getting response form the informant.
-
Inventory:
The ethno botanical data obtained, checked and compared with existing literature. Hence the indigenous knowledge about the plant resources, religious and cultural aspect such as population density was also documented
Ethnobotanical data Collection
The method used for data collection was based on semi-structured interviews, group discussions, and field visits. Interviews were conducted after obtaining informed consent (IC) from the interviewees. In many cases, a variety of techniques were used for selecting informants with traditional knowledge regarding the use of medicinal plants. The questionnaire (Additional file 1: Annex S1) used during the survey consisted of two parts: the first part was about the demographic data of the local informants, and the second part was about the medicinal plants. The ethnobotanical inventory consisted of local name of the plants, parts used, methods of preparation, mode of usage, and the diseases treated.
Botanical Identifications
During field surveys, identification was mainly based on the local names of plants, with the help of local informants. For taxonomic confirmation, the Flora of Pakistan (http://www.efloras.org/index.aspx) was followed, whereas the International Plant Name Index (IPNI) (www.ipni.org) was also used to obtain the correct botanical name confirmation.
-
Quantitative Analyses of Ethnobotanical data
The documented ethnobotanical data was elucidated to define plant parts, and preparation methods. Various quantitative indices, including Use Value (UV), Relative Frequency of Citation (RFC), the Informant Consensus factor (ICF), and the Fidelity Level (FL), were applied.-
i.Informant Consensus Factor (ICF)ICF is calculated by the following formula, as cited in the literature [3, 24, 25]. ICF was applied to highlight the homogeneity of the information regarding particular types of ailment categories [18, 26].Where “Nur” mentions the number of use reports for a particular ailment category and “Nt” refers to the number of taxa used for a particular ailment category. The result of this consensus ranges from zero to 1. A high value (close to 1) specifies that taxa are used by the large proportion of the informants for a number of conditions related to that broad category, whereas the low value (close to 0) indicates that the plants are chosen randomly for a few or a single condition or that informants did not exchange information about the use of plants [18, 27–29].
-
ii.Fidelity Level (FL)FL points out the preference shown for one species over others, for treating a particular ailment [18, 30]. The high FL confirms high usage of the plant species for a particular ailment, whereas low FL confirms a wide range of medicinal uses but with a low frequency for each ailment. It was calculated by the following formula:Where “Ip” is the number of informants, provided information about use of species for a particular ailment category. Whereas “Iu” is the number of informants stating the use of that plant for any ailment category. High FL value (near 100%) is obtained from plants for which almost all use reports mention using it in nearly the same way, whereas low FL value is obtained from plants that are used for many different purposes. Similarly, the high FL confirms high usage of the plant species for a particular ailment, whereas low FL confirms a wide range of medicinal uses but with a low frequency for each ailment.
-
iii.Use Value (UV)Where UV is the use value of species, “U” is the total number of use reports per species, and “n” represents the total number of informants interrogated for a given plant. UVs are higher if there are many use reports of a plant, implying that the plant is important, whereas they are near zero if there are few reports related to its use.
-
iv.Relative Frequency Citation (RFC)This relation displays the local prominence of every species, and it is calculated by dividing the FC, the number of informants reporting the use of the species divided by the total number of informers contributing in the survey (N), without bearing in mind the use-categories [2].
-
v.Relative Importance (RI)where PP stands for pharmacological properties, which indicate relative use reports, are calculated by dividing the number of use reports (UR) attributed to a species by the maximum number of use reports attributed to the most important species (the species with the highest number of use reports), and AC stands for ailments treated, which indicates the relative body systems treated. AC is calculated by dividing the number of body systems treated by a given species, by the maximum number of ailment categories treated by the species that are used most widely.
-
vi.Jacard Index (JI)
-
i.
where “a” is the number of species of the area A (the NavaPind or ShahpurVirkan); “b” is the number of species of the area B, which includes Thar desert, Pakistan; Alpine and Sub-alpine regions; District Mastung of Baluchistan; Makerwal and GullaKhel, Pakistan; Gilgit-Baltistan, Pakistan; Malakand, Pakistan; Lesser Himalayas-Pakistan; Cholistan Desert, Pakistan; Bhera, District Sargodha, Pakistan; Dir, Khyber Pakhtunkhwa, Pakistan; Pind Dadan Khan, district Jhelum, Punjab, Pakistan; Khushab, Punjab, Pakistan; Dir Kohistan valleys, KPK, Pakistan; Kabal, Swat District, KPK, Pakistan; Southern Rajasthan, India; Chitral valley, Pakistan; Mahal Kohistan (Khirthar National Park); Mianwali District Punjab, Pakistan; District Bagh, Azad Kashmir, Pakistan and “c” is the number of species common to both A and B.
Results and discussion
Demographic data
Eight field trips (to cover seasonal variations) were carried out to compile ethnobotanical data associated with uses of medicinal plants. The total duration of the field study was approximately 10 months, from November 2014 to June 2015. A total of 400 informants were interviewed. Among the 400 informants, mostly were indigenous people (Table 1). A large number of people were in the age of 30–40 years (36.5%) and less than 20 years (21%). Due to the lack of some educational facilities in that area, most of the informants were illiterate (50.25%) (Table 1). But some were educated showing that they had awareness about education. Many informants had completed their primary (24.75%) or secondary (10.25%) education. Some had completed even their secondary school certification (6.25%). Most of the informants spoke Punjabi and very often spoke Urdu. The majority of informants were female (71%) rather than male (29%). This may be because of female interviewer, hence females felt comfortable with her and talk freely.
Table 1.
Demographic data of informants in NavaPind and Shahpur Virkan district Sheikhupura
| Sr.no. | Variation | Category | No. of person | %age |
|---|---|---|---|---|
| 1. | Informant category | Traditional health practitioner | 0 | 0% |
| Indigenous people | 400 | 100% | ||
| 2. | Gender | Male | 116 | 29% |
| Female | 284 | 71% | ||
| 3. | Age | Less than 20 | 85 | 21.25% |
| 20–30 | 41 | 10.25% | ||
| 30–40 | 146 | 36.5% | ||
| 40–50 | 77 | 19.25% | ||
| 50–60 | 40 | 10% | ||
| 60–70 | 7 | 1.75% | ||
| 70–80 | 2 | 0.5% | ||
| More than 80 | 2 | 0.5% | ||
| 4. | Educational background | Illiterate | 201 | 50.25% |
| Completed 5 years education | 99 | 24.75% | ||
| Completed 8 years education | 41 | 10.25% | ||
| Completed 10 years education | 25 | 6.25% | ||
| Completed 12 years education | 17 | 4.25% | ||
| Some under grade degree | 10 | 2.5% | ||
| Graduate | 6 | 1.5% | ||
| Master | 1 | 0.25% |
Medicinal plant diversity
During ethnobotanical survey, 96 plant species were explored for medicinal properties (Fig. 2). The highest number of ethnobotanically used species were belonging to family Poaceae (16 species), followed by Fabaceae (15 species), Asteraceae (9 species), Brassicaceae (5 species), Euphorbiaceae and Moraceae (4 species), Amaranthaceae, Convolvulaceae, Malvaceae and Solanaceae (3 species/family). Other frequently used families were Chenopodiaceae, Lamiaceae, Liliaceae, Meliaceae, Myrtaceae, Ranunculaceae and Verbenaceae (2 species from each family). While Acanthaceae, Apiaceae, Asclepiadaceae, Cannabinaceae, Cucurbitaceae, Cyperaceae, Lythraceae, Oleaceae, Oxalidaceae, Papaveraceae, Polygonaceae, Primulaceae, Rhamnaceae, Rutaceae, Saliaceae, Scrophulariaceae, Urticaceae were represented by single species.
Fig. 2.
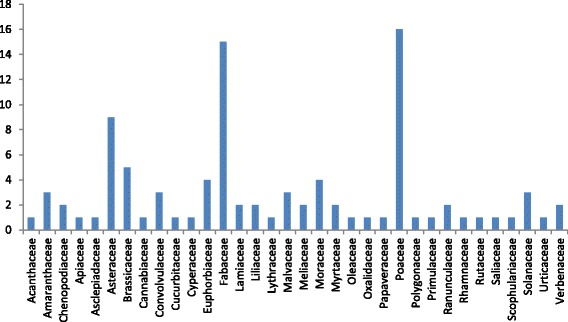
Plant families of medicinal plants
Life forms
In this survey, herbs were documented with highest frequency (30.20%), then herbaceous shrubs (27.08%) which was followed by trees (18.75%), graminoids (14.58%), shrubs (5.20%), vines (2.08%), weeds and succulents (1.04% each) (Fig. 3). The possible reason for the dominance of herbs, might be the presence of bioactive compounds helping them to adapt the habitat. [1, 25, 33, 34]. This observation is supported by the previous study carried out in the other regions of Pakistan [18, 35]. While the shrubs (8.33%) and bushes (2.77%) have the lowest frequency. Avena sativa L., Brassica campestris L., Triticum aestivum L., Coriandrum sativum L. reported to cultivate in the study area for satisfication of the local need.
Fig. 3.

Life forms of medicinal plants
Parts of medicinal plants used for curing diseases
In this survey, leaves (31.15%) were the dominant plant part used, followed by whole plant (24.59%), wood (9.29%), oil (4.92%) (Fig. 4). As leaves are easy to collect and require less effort than other parts such as root, seeds, flower and fruit [34], therefore they are frequently used for treatment of ailments. Another significant reason is that use of leaves can conserve the plant but the use of root can kill them [36, 37]. The lowest plant parts used were gum, oil, roots and straw (0.862% each). Moreover, mostly leaves were used for the preparation of herbal compositions [38–44]. This trend of plant part used is observed not only in NavaPind and Shahpur Virkan but throughout the province [45–48]. However, in other provinces particularly in KPK, whole plant utilization for curing various diseases is common practice [49].
Fig. 4.

Plant part used (%)
In the present study difference in plant part used is also noticed. Although the medicinal use of species is already reported from other regions of Pakistan and South Asia but the important discovery is different plant part is used for treating the same diseases. A. paniculata, whole plant [47, 48] was reported before for the treatment of GIT problem and also used as blood purifier whereas in present it is discovered that flower and leaves can also be used to treat the same disease. Stem of P. paniculata was reported in previous study to minimize severe body pain [50] but this study reveals that whole plant can be used to relieve stomach pain. Similarly, shoot [45], seed [35] and fruit [51] of C. sativum were reported for to treat GIT problems, while present study describe that whole plant can be used for the same purpose. For A. scoparia, shoot and seed [52] were reported earlier for stomach complaints. But this study explored that whole plant can also be used for the same disease as well. Shoot extract, oil [45] and seeds [52] of B. campestris were reported as hair tonic but present study reveals that extract of leaves and flower can also be used for the same purpose. Shoot of C. didymus was explored in literature [45] as blood purifier whereas whole plant especially stem and leaves can also be used to treat the same disease.
Similarly shoot of E. helioscopia, was previously recommended for animal disease [45], whole plant as skin tonic [53], Stem and root as laxative and for cholera [54] were reported’ however present exploration indicated that leaves, sap and seeds can also be used for the same purpose. Effective of A. arabica leaves and fruit [55] was explained for dysentery whereas this study provides information that bark could be used for the same purpose. As far as A. lebbeck, bark, fruit and roots previous exploration concern, they were used to treat cough [48] but present study explained that leaves, seed and wood can be used also for the treatment of same cough. Different plant parts of C. angustifolia were in use for treating various diseases such as leaves and roots for stomach disorder [3, 47] whereas branches, pods and seed can be used for stomach disorder as well. Stem of M. indica was reported in previous study as most plant part used for the treatment of stomach complaint [54]. However, according to present study findings whole plant can also be recommended for the same purpose. As leaves and flower of V. thapsus, were explored as for wound healing [11] while this study explained that seeds can also be used for wound healing.
Toxicity of medicinal plants
In this study, the documented ethnomedicinal data was generally confined to medicinal usage, with some information on the toxicity of plants. The majority of plants (63%) were reported having toxic effect (Fig. 5). The majority of the informants stated that they use medicinal plants based on experience of their elders as they do not believe that the plants are toxic. According to some of the informants, plant-based recipes, when used in excessive dosage, may have severe toxic effects [47, 48]. The reporting of toxic effects of plants may provide useful information that should be taken into consideration by researchers in future investigation. It will also help them to determine the toxic compounds of plants for safe medicinal usage [56].
Fig. 5.
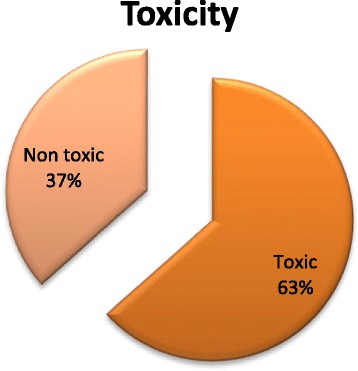
Toxicity of medicinal plants
Form and mode of utilization
In this survey, mostly plants were reported for internal applications. They were used either in the form of decoction (19.79%) or in the form of extract (81.25%) (Fig. 6). This form of utilization is common in other parts of Pakistan particularly and in World generally [35, 57, 58]. The decoction was made by boiling the plant parts in water [58–64]. While 44.44% were recommended for external use in the form of paste. The majorities of herbal medicines were prepared from fresh plant material rather than dried material.
Fig. 6.

Mode of administration
Quantitative analyses of ethnobotanical data
Informant Consensus Factor (ICF)
ICF was determined for 13 ailments (Respiratory diseases, GIT disease, Sexual disorder, Nail, skin, hair and teeth disorders, cardiac disorders, antidote, blood purifier, wound healing, fever cold and influenza disorders, Urinary disorders, Muscles disorders, glandular disorders and animals diseases) categories. The value of ICF for these 13 ailments was ranging from 0.02 to 0.82 (Table 2). The average ICF was 0.311. Commonly the value of ICF for disease treatment depends upon the availability of plant species in that area [65]. The highest value of ICF was reported for urinary diseases (0.82), sexual disease (0.68) and antidote (0.51). It showed that urinary diseases were the most common disease in the study area and most of the people had knowledge about its cure. They were using 7 different species (Amaranthus viridis, Chenopodium album, Artemisia scoparia, Sonchus arvensis, Brassica nigra, Vicia fava, and Anagallis arvensis). These seven species were not only used for urinary disease in this region but also reported from other regions of Pakistan like Semi-Tribal Area of Makerwal and Gulla Khel (Lying between Khyber Pakhtunkhwa and Punjab Provinces), Cholistan Desert and Thar Desert (Sindh). However these species used for curing cough and stomach disorders in Bhera, District Sargodha, Mastung district of Balochistan and Mountainous region of Gilgit-Baltistan [3, 49, 66] While the lowest value of ICF was for fever (0.02), muscles disorders (0.05) and glandular disorders (0.09) that may be due to lack of communication among the informants in the study area [65].
Table 2.
ICF value of plants used for the treatment of various diseases
| Category of diseases | No. of use reports | % Age of use reports | No. of taxa used | % Age of taxa | ICF |
|---|---|---|---|---|---|
| Respiratory diseases | 2383 | 18.31 | 22 | 15.38 | 0.16 |
| GIT diseases | 3499 | 26.88 | 34 | 23.78 | 0.11 |
| Sexual diseases | 294 | 2.26 | 2 | 1.40 | 0.68 |
| Nail, skin, hair, teeth disorders | 945 | 7.26 | 18 | 12.59 | 0.45 |
| Cardiac disorders | 521 | 4.00 | 4 | 2.80 | 0.4 |
| Antidote | 378 | 2.90 | 7 | 4.90 | 0.51 |
| Blood purifier | 410 | 3.15 | 4 | 2.80 | 0.16 |
| Wound healing | 1397 | 10.73 | 13 | 9.09 | 0.16 |
| Fever, cold, influenza disorders | 1419 | 10.90 | 16 | 11.19 | 0.02 |
| Urinary disorders | 221 | 1.70 | 7 | 4.90 | 0.82 |
| Muscles disorders | 571 | 4.39 | 6 | 4.20 | 0.05 |
| Glandular disorders | 591 | 4.54 | 7 | 4.90 | 0.09 |
| Animal disease | 389 | 2.99 | 3 | 2.10 | 0.44 |
Uses Value (UV)
In this study, UV ranged from 0.005 to 0.07 (Table 3). The highest UV was recorded for M. verticillata (0.07), A. farnesiana and C. occidentalis (0.04 each). Plants with high UV were also used in many parts of Pakistan. To develop the herbal drug after pharmacological and phytochemical screening in the future, focus on the plant species with higher UV, enhance plant resources sustainability and conservation (Qureshi et al. [67]). While the lowest UV was reported for C. sativum (0.005), T. tenellus (0.0053) and L. aphaca (0.0055). Most of the informants were not familiar about these plant species and had little knowledge about their enthobotanical uses. Lower UV values indicated less knowledge about particular species in the study area. Same observations of plant uses were also made by Abbasi et al. [68]; Ahmad et al. [58]; Bano et al. [69] in their study areas. Although it was impossible to match quantitative data within the region particularly in district Sheikhupura because this is first quantitative ethnobotanical documented data in this region.
Table 3.
Ethnobotanical uses of plants in NavaPind and Shahpur Virkan, Sheikhupura (Punjab), Pakistan
| Sr. no. | Family | Local name | Life form | Habitat | Part used | Methods of preparation | Diseases treated | Toxicity | FL % | UV | RFC | R.I |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. |
Andrographis paniculata (Burm.f.) Wall. ex Nees LCWU-15-01. Acanthaceae |
Jungle charaita | Herb | Wild | Flowers/leaves | Extract | Cough, influenza, diarrhea, blood purifier | Non toxic | 32.19 | 0.015 | 0.66 | 50.8 |
| 2. |
Amaranthus spinosus L. LCWU-15-02 Amaranthaceae |
kurand | Herb | Wild | Branches stem/leaves | Extract | Diarrhea, antidote, fever, fodder | No toxic | 41.60 | 0.026 | 0.765 | 3.7 |
| 3. |
Amaranthus viridis L. LCWU-15-03 Amaranthaceae |
Chulai | Herb | Wild/cultivated | Leaves | Extract, decoction, paste | Constipation, skin tonic, antidote, diuretic, cooking | Non toxic | 51.84 | 0.02 | 0.92 | 25.5 |
| 4. |
Chenopodium album L. LCWU-15-04 Chenopodiaceae |
Bathu | Herb | Wild/cultivated | Leaves/stem (whole plant) | Extract, decoction | Laxative, diuretic, cough, cooking | Non toxic | 36.30 | 0.01 | 0.95 | 14.6 |
| 5. |
Chenopodium murale L. LCWU-15-05 Chenopodiaceae |
Jasag | Herb | Wild/cultivated | Whole plant | Extract, decoction | Laxative, cooking, Fodder, dye | Non toxic | 27.77 | 0.02 | 0.94 | 5.9 |
| 6. |
Achyranthes aspera (L.) Hill LCWU-15-06 Amaranthacea |
Puth kanda | Herb | Wild/cultivated | Leaves | Decoction, extract, fresh | Cough, laxative, stomach complains, fodder, fuel | Toxic | 12.35 | 0.02 | 0.68 | 7.5 |
| 7. |
Coriandrum sativum L. LCWU-15-07 Apiaceae |
Dhaniya | Herb | Wild/cultivated | Whole plant | Oil, extract | Joint pain, stomach complaints, cooking | Non toxic | 14.55 | 0.005 | 0.91 | 29.7 |
| 8. |
Calotropis procera R. Br. LCWU-15-08 Asclepiadaceae |
Aak | Shrub | Wild | Leaves/sap milk | Latex, extract, decoction | Asthma, skin tonic, fever, fodder | Toxic | 24.48 | 0.03 | 0.81 | 38 |
| 9. |
Artemisia scoparia Waldst. & Kitt. LCWU-15-0902 Asteraceae |
Char/Krund | Herb | Wild | Leaves/(Whole plant) | Oil, extract | Diuretic, stomach complains, fodder | Non toxic | 8.09 | 0.013 | 0.77 | 7.3 |
| 10. |
Carthamus ticntorius L. LCWU-15-10 Asteraceae |
Jungle poli | Herbaceous | Wild | Whole plant | Extract | Laxative, wound healing, fodder | Toxic | 3.09 | 0.0062 | 0.795 | 9.26 |
| 11. |
Conyza bonariensis L. LCWU-15-1102 Asteraceae |
Aflatoon/jungle boti | Herbaceous | Wild | Whole plant | Extract, oil | Asthma, diarrhea, ulcer, fodder | Toxic/Non toxic | 37.33 | 0.014 | 0.635 | 8.83 |
| 12. |
Conyza erigeron L. LCWU-15-1202 Asteraceae |
Jungle kurand/jungle boti | Weed | Wild | Whole plant | Decoction | Stomach disorder, cold and cough, fever, fodder | Non toxic | 9.905 | 0.013 | 0.81 | 8.83 |
| 13. |
Eclipta alba (L.) Hassk. LCWU-15-13 Asteraceae |
Jungle booti | Herb | Wild | Whole plant | Paste, extract | Liver tonic, hair tonic, antidote of scorpio, fodder | Non toxic | 2.59 | 0.0075 | 0.665 | 5.87 |
| 14. |
Parthenium hysterophorus L. LCWU-15-14 Asteraceae |
Shah-tara/boti | Herbaceous | Wild | Whole plant/leaves | Extract | blood purifier, back pain, fodder, Decoration | Toxic | 56.29 | 0.02 | 0.96 | 20.8 |
| 15. |
Silybum marianum L. LCWU-15-1501 Asteraceae |
Poli/boti | Herbaceous | Wild | Whole plant | Decoction, infusion | Anticancer, liver tonic, wound healing, fodder | Toxic | 27.52 | 0.02 | 1.39 | 29.82 |
| 16. |
Sonchus arvensis L. LCWU-15-1601 Asteraceae |
Dodak | Herbaceous | Wild | Leaves/flower | Extract | Anti-kidney stone, asthma, cough, fodder | Toxic | 13.74 | 0.012 | 0.87 | 13 |
| 17. |
Xanthium strumarium L. LCWU-15-17 Asteraceae |
Jungle booti | Herb | Wild | Leaves | Extract | Fever, mother postnatal care, fodder | Toxic | 2.61 | 0.0074 | 0.67 | 4.28 |
| 18. |
Brassica compestris L. LCWU-15-18 Brassicaceae |
Sarson | Herb | Wild/cultivated | Leaves/flower | Extract, paste | Skin tonic, hair tonic, anti-cancerous | Non toxic | 41.73 | 0.0075 | 0.7975 | 4.76 |
| 19. |
Brassica nigra L. LCWU-15-19 Brassicaceae |
Jungle sarson | Herbaceous | Wild | Whole plant | Extract, decoction | Diuretic, respiratory problems, fodder | Toxic if in excess | 2.73 | 0.0081 | 0.61 | 20.45 |
| 20. |
Capsella bursapastoris L. LCWU-15-20 Brassicaceae |
Mirch boti | Herb | Wild | Whole plant | Decoction, infusion | Internal and external bleeding, diarrhea, fodder | Toxic | 17.74 | 0.02 | 0.77 | 17.2 |
| 21. |
Coronopus didymus (L.)Sm. LCWU-15-2003 Brassicaceae |
Jungli pudina/jungle boti | Herb | Wild | Stem/leaves (whole plant) | Extract | Asthma, Blood purifier | Non toxic | 13.96 | 0.015 | 0.7525 | 7.05 |
| 22. |
Sisymbrium irio L. LCWU-15-96 Brassicaceae |
Boti | Herb | Wild | Whole plant | Extract, powder | Asthma, fodder, | Non toxic | 24.13 | 0.01 | 0.96 | 13 |
| 23. |
Cannabis sativa L. LCWU-15-22 Cannabiaceae |
Bhang | Herbaceous | Wild | Leaves | Extract, paste | Stomach complaints, Relaxant, Severe pains repellent | Toxic | 42.31 | 0.021 | 0.945 | 3.7 |
| 24. |
Convolvulus arvensis L. LCWU-15-23 Convolvulaceae |
Lilly | Herbaceous | Wild | Leaves | Extract | Fodder, animal fever | Toxic | 34.18 | 0.02 | 0.81 | 17.6 |
| 25. |
Cuscuta reflexa Roxb. LCWU-15-24 Convolvulaceae |
Amar-bail | Climber | Wild | Stem | Extract | Wound healing, Hair tonic | Toxic | 20.42 | 0.0186 | 0.805 | 10.8 |
| 26. |
Poranopsis paniculata (Roxb.)Roberty LCWU-15-25 Convolvulaceae |
Gulu | Herb | Wild | Whole plant | Extract, | Decoration, stomach pain, diarrhea, wound healing | Toxic to animals | 27.65 | 0.007 | 0.69 | 29.57 |
| 27. |
Cucurbita pepo L. LCWU-15-2601 Cucurbitaceae |
Chibbar booti | Vine | Wild/cultivated | Leaves/flower/fruit/whole plant | Extract | Skin tonic, cardiac problem, stomach disorder, Cooking, | Toxic/Non toxic | 20.75 | 0.025 | 0.60 | 33.83 |
| 28. |
Schoenoplectus supinus (L.)Pall. LCWU-15-27 Cyperaceae |
Dala | Herb | Wild | Flower/leaves | – | Fodder, animal cough | Non toxic | 2.70 | 0.0071 | 0.695 | |
| 29. |
Euphorbia helioscopia L. LCWU-15-28 Euphorbiaceae |
Dhdtar boti | Herbaceous | Wild | Leaves/sap/seeds | Extract, decoction | Anticancerous, cholera | Toxic in excess | 54.68 | 0.0136 | 0.695 | 50.8 |
| 30. |
Euphorbia hirta L. LCWU-15-29 Euphorbiaceae |
Boti | Herb | Wild | Whole plant | – | Fodder | Toxic | 2.64 | 0.01 | 0.98 | |
| 31. |
Euphorbia thymifolia L. LCWU-15-30 Euphorbiaceae |
It-sit | Herb | Wild | Whole plant | – | Fodder | Toxic | 2.55 | 0.0152 | 0.655 | |
| 32. |
Ricinus communis L. LCWU-15-3101 Euphorbiaceae |
Rind/Rnola | Herbaceous | Wild/cultivated | Leaves/seeds/whole plant | Extract | Wound healing, fuel, hair tonic | Seed are toxic | 15.53 | 0.012 | 0.65 | 8.83 |
| 33. |
Sapium sebiferum L. LCWU-15-32 Fabaceae |
Jungli Tahli | Tree | Wild | Leaves/wood | Decoction | Antidote, diuretic, Fodder, fuel, furniture | Toxic/non toxic | 9.94 | 0.01 | 0.85 | |
| 34. |
Acacia nilotica (Linn.) Delile. LCWU-15-93 Fabaceae |
Jawa | Herbaceous | Wild | Leaves | – | Fodder | Non toxic | 1.81 | 0.007 | 0.68 | |
| 35. |
Acacia arabica Willd. LCWU-15-3301 Fabaceae |
Desi kikkar | Tree | Wild | Bark | Decoction | Diarrhea, Skin tonic, roofing, fuel, fodder | Non toxic | 19.35 | 0.015 | 0.635 | 20.8 |
| 36. |
Acacia farnesiana L. LCWU-15-34 Fabaceae |
Kabli kikar | Tree | Wild | Wood/flower/leaves | Extract | Diarrhea, scent, fuel, furniture, | Non toxic | 16.48 | 0.04 | 0.65 | 9 |
| 37. |
Albizia lebbeck (L.) Benth. LCWU-15-3501 Fabaceae |
Shireen | Tree | Wild | Leaves/seed/wood | Extract | Fuel, wound healing, Cough, burning, postnatal care | Non toxic | 33.22 | 0.02 | 0.66 | 11.15 |
| 38. |
Cassia angustifolia L. LCWU-15-3602 Fabaceae |
Sukh chain | Tree | Wild | Branches/pods/seeds | Extract | Purgative, hair tonic, teeth tonic | Toxic/Non toxic | 64.33 | 0.02 | 0.87 | 13 |
| 39. |
Cassia fistula L. LCWU-15-37 Fabaceae |
Amaltas | Tree | Wild | Leaves/ legumes | Infusion, extract | Laxative, fodder, cough, stomach pain | Toxic in excess | 21.39 | 0.02 | 0.77 | 7.83 |
| 40. |
Cassia occidentalis L. LCWU-15-38 Fabaceae |
Boti | Herb | Wild | Wood/leaves | Extract | Stomach disorder, laxative, fuel, roofing, bitter taste | Toxic | 19.45 | 0.04 | 0.72 | 8.83 |
| 41. |
Dalbergia sissoo Roxb. ex DC. LCWU-15-3901 Fabaceae |
Tali | Tree | Wild | Wood/leaves | Extract | Wound healing, hair tonic, fodder, fuel, furniture | Toxic/non toxic | 34.64 | 0.025 | 0.91 | 8.83 |
| 42. |
Indigofera linifolia (L.f) Retz. LCWU-15-40 Fabaceae |
Gorakh pan/jungle boti | Herbaceous | Wild | Whole plant | Extract | Stomach complaints, blood purifier, liver problems, fodder, obtain dye | Toxic to some extent | 55.13 | 0.02 | 0.722 | 75.8 |
| 43. |
Lathyrus aphaca L.
LCWU-15-41 Fabaceae |
Jungli matter/gangla | Herbaceous | Wild | Leaves | – | Fodder | Toxic/non toxic | 3.52 | 0.0055 | 0.905 | |
| 44. |
Melilotus indica L. LCWU-15-4202 Fabaceae |
Jungle meeni or meena/Jungli shatala | Herbaceous | Wild | Leaves/whole plant | Extract | Laxative, diarrhea, cooking, fodder, bitter taste, skin tonic | Toxic to some extent | 18.17 | 0.02 | 0.78 | 8.58 |
| 45. |
Mimosa pudica L. LCWU-15-94 Fabaceae |
Chijan | Herb | Wild | Leaves | Extract | Antidote, wound healing, diarrhea, fuel, fodder | Toxic in excess | 4.44 | 0.01 | 0.68 | |
| 46. |
Tamarindus indica L. LCWU-15-4301 Fabaceae |
Imli/khatti imli | Tree | Wild | Branchesstem/leaves/fruit/whole plant | Extract | Malaria, fever, bitter taste, Laxative, burning | Non toxic | 39.61 | 0.03 | 0.83 | 27.1 |
| 47. |
Vicia faba L. LCWU-15-4402 Fabaceae |
Jungli cheraal/Phalya/Arari | Herbaceous | Wild | Legumes/leaves | Extract | Diuretic, fodder, food, soap | Non toxic | 43.04 | 0.02 | 0.86 | 25.8 |
| 48. |
Ocimum basilicum L. LCWU-15-45 Lamiaceae |
Niazbo | Herb | Wild | Leaves | Extract | Scent, flavoring, cough, headache, diarrhea | Non toxic | 37.96 | 0.0176 | 0.85 | |
| 49. |
Ocimum sanctum L. LCWU-15-4601 Lamiaceae |
Jungle booti | Herbaceous | Wild | Leaves/whole plant | Powder, extract, oil | Appetizer, mosquito repellent, fodder, fever, cough | Toxic/non toxic | 11.50 | 0.008 | 0.798 | 14.7 |
| 50. |
Allium roylei Strearn. LCWU-15-47 Liliaceae |
Bola ganda | Herbaceous | Wild | Leaves | Oil, extract | Cholera, curative, flavoring | Non toxic | 62.03 | 0.0163 | 0.915 | 25.8 |
| 51. |
Aloe vera (L.) Burm. f. LCWU-15-48 Asphodelaceae |
Kwal qandal | Succulent plant | Wild | Leaves | Oil, extract | Skin tonic, cough, hair tonic, fever | Non toxic | 18.80 | 0.03 | 0.70 | 30.5 |
| 52. |
Lawsonia Inermis L. LCWU-15-49 Lythraceae |
Mehndi | Shrub | Wild | Leaves/roots | Paste, extract | Wound healing, hair tonic | Non toxic | 28.04 | 0.0213 | 0.935 | 10.8 |
| 53. |
Malva verticillata L.
LCWU-15-50 Malvaceae |
Booti | Herb | Wild | Whole plant | Paste | Fodder, animal ulcer | Non toxic | 2.51 | 0.07 | 0.645 | |
| 54. |
Malva indica
LCWU-15-51 Malvaceae |
Sonchal booti/jungle boti | Herbaceous | Wild | Whole plant | Decoction, extract | Cough, cooking, fodder | Toxic in excess | 11.26 | 0.011 | 0.628 | 7.04 |
| 55. |
Malvastrum coromandelianum L. LCWU-15-52 Malvaceae |
Boti | Herbaceous | Wild | Whole plant | Extract | Fodder, wound healing | Toxic | 16.06 | 0.02 | 0.60 | 8.83 |
| 56. |
Azadirachta indica A. Juss LCWU-15-53 Meliaceae |
Neem | Tree | Wild | Leaves/wood | Extract, oil | Fodder, skin tonic, fuel | Toxic to some extend | 20.62 | 0.03 | 0.79 | 10.5 |
| 57. |
Melia azadirachta L. LCWU-15-5402 Meliaceae |
Bakain/dhareek | Tree | Wild | Leaves/wood/seed | Extract | Wound healing, cough, fuel, furniture, fodder | Seeds are toxic | 22.04 | 0.03 | 0.94 | 9.22 |
| 58. |
Ficus sarmentosa Bush: Ham. Ex J.E. Smith LCWU-15-95 Moraceae |
Walaiti bohr | Tree | Wild | Wood/leaves | Decoction | Fuel, fodder | Toxic | 6.89 | 0.01 | 0.85 | |
| 59. |
Ficus benghalensis L. LCWU-15-5501 Moraceae |
Borh/desi borh | Tree | Wild | Leaves/sap milk/fruit/wood | Decoction, extract | Influenza, diarrhea, fuel, decoction | Toxic to some extend | 40.06 | 0.03 | 0.85 | 29.82 |
| 60. |
Ficus religiosa L. LCWU-15-56 Moraceae |
Peepal | Tree | Wild | Wood/leaves/bark | Decoction, extract | Asthma, diarrhea fuel, fodder, ulcer, molar pain, cardiac problem | Toxic in excess | 28.33 | 0.03 | 0.902 | 19.4 |
| 61. |
Morus alba L. LCWU-15-5701 Moraceae |
Shehtoot/Toot | Tree | Wild/cultivated | Wood/fruit/branches/leaves | Extract | Cough, fodder, respiratory disorders | Sap is toxic | 13.58 | 0.02 | 0.98 | 7.64 |
| 62. |
Eucalyptus globulus Labill. LCWU-15-58 Myrtaceae |
Sufaida | Tree | Wild | Leaves/wood/oil | Extract, infusion | Influenza, skin tonic, Fuel, furniture, stomach disorder | Toxic in excess | 31.32 | 0.02 | 0.83 | 17.32 |
| 63. |
Syzygium cumini L. LCWU-15-59 Myrtaceae |
Jaman | Tree | Wild | Fruit/wood/leaves | Extract | Heart problem, diarrhea Fruit, fuel, fodder, | Non toxic | 24.76 | 0.03 | 0.98 | 25.5 |
| 64. |
Jasminum nudiflorum Lindl. LCWU-15-6002 Oleaceae |
Chasko | Shrub | Wild | Leaves/flower/fruit | Extract | Vegetable, stomach pain, Cooking, | Toxic | 9.71 | 0.03 | 0.59 | |
| 65. |
Oxalis corniculata L. LCWU-15-6101 Oxalidaceae |
Khatmal booti/jungle boti | Herb | Wild | Whole plant | Extract | Antidote, stomach disorder, cooking, fodder | Toxic | 38.35 | 0.012 | 0.773 | 8.83 |
| 66. |
Fumaria indica Linn. LCWU-15-6202 Papaveraceae |
Soye/Papra | Herb | Wild | Branches/stem/leaves/whole plant | Extract | Laxative, fodder | Non toxic | 11.04 | 0.01 | 0.83 | 3.7 |
| 67. |
Acrachne racemosa (Roem&schult) LCWU-15-63 Poaceae |
Jungle ghaas | Grass | Wild | Whole plant | Decoction | Fodder | Toxic on skin | 3.17 | 0.0061 | 0.815 | |
| 68. |
Asthenatherum forkalii (Vahl)Nexski. LCWU-15-64 Poaceae |
Jungle ghass | Grass | Wild | Whole plant | Extract | Fodder, animal fever | Toxic/non toxic | 3.27 | 0.0059 | 0.84 | |
| 69. |
Avena sativa L. LCWU-15-65 Poaceae |
Jo | Herb | Wild | Staw | Extract | Postnatal care | Toxic to some extend | 51.40 | 0.01 | 0.945 | 5.3 |
| 70. |
Cenchrus setigerus Vahl. LCWU-15-66 Poaceae |
Jungli boti | Grass | Wild | Whole plant | Extract | Fodder | Non toxic | 2.11 | 0.006 | 0.79 | |
| 71. |
Chloris barbata Sw. LCWU-15-67 Poaceae |
Jungle boti | Herb | Wild | Whole plant | Fodder, skin disorder | Toxic | 22.70 | 0.01 | 0.78 | 10.5 | |
| 72. |
Chloris virgata Sw. LCWU-15-68 Poaceae |
Boti | Grass | Wild | Whole plant | Fodder, wound healing, malaria | Toxic | 50.09 | 0.02 | 0.71 | 25.5 | |
| 73. |
Chrysopogon aucheri Bioss LCWU-15-69 Poaceae |
Goad ghass | Grass | Wild | Whole plant | Fodder, fuel | Toxic | 5.26 | 0.01 | 0.73 | ||
| 74. |
Cynodon dactylon (L.) Pers. LCWU-15-70 Poaceae |
Ghaas | Grass | Wild | Whole plant | Extract | Stomach complaint, constipation, antidote for snake and dogs, fodder | Non toxic | 50.81 | 0.02 | 0.83 | 3.7 |
| 75. |
Digitaria ciliaris (Retz.)Koel. LCWU-15-71 Poaceae |
Jungle ghass | Grass | Wild | Whole plant | Fodder, animal stomach disorder | Toxic | 3.29 | 0.0059 | 0.84 | ||
| 76. |
Digitaria nodosa Parl. LCWU-15-72 Poaceae |
Swank | Grass | Wild | Whole plant | Fresh, dry | Fodder, blood purification | Toxic | 3.43 | 0.011 | 0.88 | |
| 77. |
Eleusine indica (L.)Gaertn. LCWU-15-73 Poaceae |
Jungle ghaas | Grass | Wild | Whole plant | Extract | Fodder | Toxic/non toxic | 3.04 | 0.0064 | 0.78 | |
| 78. |
Pennisetum divisum (Fosslk.ex.J.F.Gmel) LCWU-15-74 Poaceae |
Jungle ghaas | Grass | Wild | Whole plant | Extract | Fodder | Non toxic | 3.39 | 0.0057 | 0.87 | |
| 79. |
Phragmites karka (Retz.) Trin. Ex Steud. LCWU-15-75 Poaceae |
Nur | Grass | Wild | Wood/stem | Extract | Cardiac problem, fuel | Toxic/non toxic | 23.80 | 0.01 | 0.62 | 13 |
| 80. |
Saccharum bengalensis L. LCWU-15-76 Poaceae |
Kana | Grass | Wild | Wood | Paste, extract | Animal disease roofing, fuel, pre/post natal care | Toxic | 35.46 | 0.02 | 0.84 | 17.16 |
| 81. |
Tetrapogon tenellus (Roxb.)Chiov. LCWU-15-77 Poaceae |
Dumbi seeti | Grass | Wild | Whole plant | Extract | Fodder, cough | Toxic | 3.64 | 0.0053 | 0.935 | |
| 82. |
Triticum aestivum L. LCWU-15-78 Poaceae |
Joi | Grass | Wild | Whole plant | Extract | Fodder, anticancerous, gastrointestinal disease | Toxic/non toxic | 3.19 | 0.01 | 0.985 | 8.9 |
| 83. |
Rumex chalepensis Mill. LCWU-15-79 Polygonaceae |
Boti | Herbaceous | Wild | Whole plant | Extract | Fodder | Toxic | 2.05 | 0.01 | 0.76 | |
| 84. |
Anagallis arvensis L. LCWU-15-8001 Primulaceae |
Jungli golo/Matri | Herbaceous | Wild | Leaves/wood (whole plant) | Extract | Fodder, skin tonic, Diuretic, hair tonic | Toxic/non toxic | 31.44 | 0.02 | 0.855 | 18.15 |
| 85. |
Ranunculus muricatus L. LCWU-15-8101 Ranunculaceae |
Jungli dhaniya/boti | Herbaceous | Wild | Leaves/whole plant | Crude extract | Fodder, fever, asthma, Fodder | Toxic | 14.5 | 0.01 | 0.738 | 25.5 |
| 86. |
Ranunculus repens L. LCWU-15-82 Ranunculaceae |
Jungle jugnoo | Herbaceous | Wild | Leaves/flower | Extract | Fodder | Toxic | 2.47 | 0.007 | 0.635 | |
| 87. |
Zizyphus jujuba (L.)Lam. LCWU-15-8301 Rhamnaceae |
Ber | Tree | Wild | Leaves/gum/fruit/wood/leaves | Extract, oil | Fruit, furniture, digestion, skin tonic, joints pain, hair tonic, backache, burning | Toxic/non toxic | 51.75 | 0.03 | 0.97 | 30.65 |
| 88. |
Murraya koenigii L. LCWU-15-84 Rutaceae |
Marva | Tree | Wild | Branches/stem/leaves | Extract | Stomach diseases, wound healing, vomiting, scent, decoration | Toxic/non toxic | 34.86 | 0.017 | 0.87 | 14.5 |
| 89. |
Salix lanata L. LCWU-15-85 Salicaceae |
Boti | Shrub | Wild | Whole plant | Extract | Fever, reduce internal pain, fodder, bitter taste | Toxic | 14.93 | 0.02 | 0.57 | 26.98 |
| 90. |
Verbascum thapsus L. LCWU-15-86 Scrophulariaceae |
Geedar tabbaco | Herb | Wild | Seeds | Extract, infusion | Male disease, internal bleeding | Toxic to some extent | 42.17 | 0.008 | 0.62 | 25.8 |
| 91. |
Lycium barbarum L. LCWU-15-87 Solanaceae |
Kashni | Herbaceous | Wild | Leaves | Extract | Anticancerous, asthma, scent, fodder | Non toxic | 55.71 | 0.022 | 0.895 | 33.8 |
| 92. |
Solanum americanum Mill. LCWU-15-88 Solanaceae |
Peelak | Herb | Wild | Leaves/stem | Extract | Joints pain, cooking, scent, vegetable, fodder | Toxic in excess | 66.14 | 0.03 | 0.85 | 10.8 |
| 93. |
Withania somnifera L. LCWU-15-89 Solanaceae |
Aak-Singh | Herbaceous | Wild | Leaves/flower/fruit | Extract | Lung disorder, animal disease, asthma, male disease | Toxic in excess | 44.09 | 0.0085 | 0.79 | 42.32 |
| 94. |
Urtica dioca L. LCWU-15-90 Urticaceae |
Kharish booti | Herbaceous | Wild | Stem/leaves | Extract | Joints pain, cold and flu, liver disease | Toxic in excess | 16.33 | 0.010 | 0.945 | 10.8 |
| 95. |
Lantana camara L. LCWU-15-9101 Verbenaceae |
Cingii | Shrub | Wild | Leaves | Extract | Fodder, snake bite, cold and flu | Toxic | 48.16 | 0.02 | 0.70 | 50.5 |
| 96. |
Phyla nodiflora L. LCWU-15-92 Verbenaceae |
Bakan | Herb | Wild | Branches/stem/leaves | Extract, decoction | Fodder | Toxic | 2.08 | 0.018 | 0.535 |
FL Fidelity Level, RFC Relative Frequency of Citation, UV Use Value, RI Relative Importance
Bold Uses/Ailment treated = Main use of plant on which FL (%) is based
Relative Frequency of Citation (RFC)
The value of RFC ranged from 0.535 to 1.39. (Table 3). The highest value of RFC present in S. marianum (1.39), T. aestivum (0.985), E. hirta, M. alba and S. cumini (0.98 each). It can be seen that plants with highest RFC are the most common plant in that region and majority people agreed by its medicinal value [35]. While the lowest value of RFC was present in P. nodiflora (0.535), S. lanata (0.57) and J. nudiflorum (0.59). RFC was compared with previous studies including Yaseen et al. [18]; Xavier et al. [70]; Bibi et al. [35].
Fidelity Level (FL)
In present study the FL ranged from 1.81 to 66.14% (Table 3). The higher the FL value the more would be use of plant [18]. The highest value of FL was present in S. americanum (66.14%), C. angustifolia (64.33%) and A. roylei (62.03%). These plants were used by informants for disease cure and other purposes. The choice of informants dealing with the specific ailments indicated maximum value of FL (Rajakumar and Shivanna, [65]; Islam, [71]. While lowest FL value was in A. nilotica. (1.81%), R. chalepensis (2.05%) and P. nodiflora (2.08%).
Comparison with other studies in neighboring regions
To compare our documented data regarding important plant species in the NavaPind and ShahpurVirkan ethnobotanical data from 17 published studies of neighboring regions (Table 4) were cited. The ethnobotanical studies of India (because Pakistan and India both are Asian countries and sharing same physical and biological conditions with minute differences) were also included for the comparative studies. The percentage similarity for uses of the total comparative study varied from 14.28% [72] to 66.66% [73]. While the percentage of dissimilarity for uses of the total comparative study ranged from 85.71% [72] to 6.66% [18]. The highest value of JI was calculated to be 32.98 [45], followed by 19.58 [49]. Whereas the lowest value of JI was 2.29 [66], followed by 4.43 [72]. From this comparison, it can be calculated that more similarity means the sharing of same flora and cross-cultural exchange of medicinal plant knowledge in the past.
Table 4.
Comparison of medicinal plant species of NavaPind/Shahpur Virkan and Allied areas
| Area | Study year | No. of recorded plant species | Total species common in both area | Species enlisted only in study area | Species enlisted only in aligned area | Plant with similar uses (%) | Plant with dissimilar uses (%) | JI | Citation | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Thar desert, Pakistan | 2015 | 87 | 16 | 81 | 72 | 60 | 6.66 | 10.8 | [18] |
| 3. | District Mastung of Balochistan | 2014 | 102 | 12 | 84 | 90 | 16.66 | 83.33 | 7.40 | [35] |
| 4. | Makerwal & Gulla Khel, Pakistan | 2013 | 131 | 28 | 68 | 103 | 35.71 | 64.2 | 19.58 | [49] |
| 5. | Gilgit-Baltistan, Pakistan | 2013 | 49 | 7 | 89 | 42 | 57.14 | 42.85 | 5.64 | [93] |
| 6. | Malakand, Pakistan | 2013 | 92 | 14 | 82 | 78 | 42.85 | 57.14 | 9.58 | [11] |
| 7. | Lesser Himalayas-Pakistan | 2013 | 45 | 8 | 88 | 37 | 37.5 | 62.5 | 6.83 | [68] |
| 8. | Cholistan Desert, Pakistan | 2012 | 90 | 4 | 92 | 86 | 50 | 50 | 2.29 | [66] |
| 9. | Bhera, District Sargodha, Pakistan | 2012 | 97 | 32 | 64 | 65 | 37.5 | 62.5 | 32.98 | [45] |
| 10. | Dir, Khyber Pakhtunkhwa, Pakistan | 2012 | 67 | 18 | 78 | 49 | 33.33 | 66.66 | 16.51 | [53] |
| 11. | Pind Dadan Khan, district Jhelum, Punjab, Pakistan | 2011 | 69 | 14 | 82 | 55 | 35.71 | 64.28 | 11.38 | [46] |
| 12. | Khushab, Punjab, Pakistan | 2011 | 48 | 15 | 81 | 33 | 26.66 | 73.33 | 15.15 | [54] |
| 13. | Dir Kohistan valleys, KPK, Pakistan | 2011 | 65 | 9 | 87 | 56 | 66.66 | 33.33 | 6.71 | [73] |
| 14. | Kabal, Swat District, KPK, Pakistan | 2011 | 140 | 24 | 72 | 116 | 25 | 75 | 14.63 | [9] |
| 15. | Southern Rajasthan, India | 2010 | 31 | 5 | 91 | 26 | 40 | 60 | 4.46 | [98] |
| 16. | Chitral valley, Pakistan | 2009 | 83 | 7 | 89 | 76 | 14.28 | 85.71 | 4.43 | [99] |
| 17. | Mahal Kohistan (Khirthar National Park) | 2007 | 50 | 11 | 86 | 40 | 36.36 | 63.63 | 8.62 | [76] |
| Average | 73.29 | 13.17 | 77.29 | 60.23 | 36.19 | 55.94 | 10.41 |
Man learnt to cure health problems with plant and plant products by trails and errors. With the passage of time this knowledge got the shape of traditional medicinal system. This system got transferred from one generation to other generation orally without any documentation. Hence in last few decade lack of interest by generation created gap in knowledge transformation and highlighted the need to bring information about traditional medicine into documentation.
In 1950 Hocking reported that almost 84% of Pakistan population relied on natural medicinal resources for their health care [74]. With reference to Pakistan first enthnobotanical study was made by Chaudhary from West Pakistan [75]. According to the survey, almost 1500 medicinal plant species were being used to cure many aliments. Even now modern pharmacopoeia contains at least 25% drug which can be derived from natural resources. The scope of medicinal plants can revolutionize the lives of the people in the rural areas of Pakistan and also increase the socio-cultural values of that area of Pakistan. With the opening of new era, ethnobotany provides a solid vision of plant resources through which new targeting active compounds can be developed and can be used for every major and minor disease. diversity richness will provide germplam, leading to more targeting compounds.
The information presented in this document was collected from reliable informants based on personal observation. Different plant recipes were used to cure ailments. This is notable that most of the remedies consist of a single plant species. However, in other cases, one plant species is used in combination of other plant species to cure ailments like Cassia fistula and T, indica. One teaspoon Amaltas fruit pulp and 1 teaspoon of tamarind in one cup of water left overnight mashed and strained is used for stomach problem, Similarly, 1 plant species can be used more than one disease like Amaranthus spinosus is used as antidote and as well as for constipation. Moreover, a single ailment can be treated with a list of plant species like asthma can be cured (Additional file 1: Table S2).
Results of present study revealed that 12 out of 96 species were first time explored for the medicinal values. These species are C. tinctorius, C. erigeron, S. supinus, O. sanctum, A. roylei, M. verticillata, M. indica, J. nudiflorum, A. forkalii, D. ciliaris, D. nodosa and T. tenellus. These species belong to seven different families. These species have not been reported for their medicinal properties from any region of the Pakistan and South Asia before this report [9, 13–16, 28, 76]. Four species (A. forkalii, D. ciliaris, D. nodosa and T. tenellus) belong to family Poaceae [77]. This family is well known for food and fodder species. Members of this family are rich in phytochemicals like phenol, alkaloid, coumarins, glycosides, lignin, quinones, saponins, steroids, tannins, terpenoids and flavonoids [78]. Therefore they have been in used for treatment of various human and animals ailments. These four species are not only used as fodder but also for the treatment of animal fever, animal stomach disorders, blood purification and animal cough respectively. This information may lead toward the discovery of new fodder sources. They may also use for the exploration of number of phytochemicals to give another alternative way to compensate the drug needs. That’s why; this finding will help many pharmacologists in near future to determine many new pharmacologically active constituents from these plant species.
Two species (M. verticillata and M. indica) belong to family Malvaceae. This family is characterized by large number of phytochemicals including tannins, polysaccharides, coumarins, flavonoids, malvin, folic acid, and terpenoids, Vitamin A, Vitamin C and Vitamin E [79]. These phytochemicals make them suitable for the treatment of various human and animal ailments. These two species are not only used as fodder but can also be used for the treatment of various ailments including animal ulcer and cough respectively. Similarly, two species (C. tinctorius and C. erigeron) belong to family Asteraceae. This family is rich in many active compounds like saponin, glycosides, steroids, tannins, diterpenoids, tritepenoids and Flavonoids [80]. That’s why; the members of this family are being used for the ailments of human and animals as well. These two species are used for the treatment of GIT and respiratory disorders respectively in our study area. One species (O. sanctum) belongs to family Lamiaceae. Most of the members of this family are well known of having many phytochemicals (alkaloids, tannins, flavonoids, terpenoids and carbohydrates) [81]. They are used for the ailments of human and animals as well. This species is reported for the treatment of fever and cough. This could be an addition into herbs used for the treatment of fever and cough.
A. roylei is among the 12 species reported first time from present study area for their medicinal uses. This species belongs to family Liliaceae. Phytochemical analysis of other member of this family indicates the presences of phenols, flavonoids, tannins, saponins, steroids, terpenoids [82]. So, they are medicinally used for the treatment of cholera. A. roylei is reported for curing cholera. J. nudiflorum belongs to family Oleaceae. This family is characterized by alkaloids, glycosides, carbohydrates, anthraquinone, steroids, saponins, flavonoids, tannins and phenols [81]. It can be predicted that J. nudiflorum might be rich in these phytochemicals. This species is an effective herbal remedy to relieve stomach pain. S. supinus is belongs to family Cyperaceae. Based on previous literature [17] it could be predicted that S. supinus is rich in alkaloids, saponins, phenolic, flavonoids (Bhardwaj et al. [83]). This species is used for treating animal cough in NavaPind and Shahpur Virkan. This medical use of species is not report earlier [28, 76, 84]. This species could be further explored for the discovery of new drugs and active phytochemicals.
Present investigation provides baseline information to screen out biological activities of these valuable plants in order to develop new antiseptic and insecticidal medicines from plant origin. This can be possible when focus on the different medicinal uses of a plant species which are not reported in literature before. There were 96 species reported from NavaPind and Shahpur Virkan, Shiekhupura, Pakistan. To compare their medicinal uses with previous research work in Pakistan and neighboring country, almost 34 plant species were found that has been mentioned as herbal medicines but in the present study new medicinal uses were reported. In the study area A. paniculata is being used for cough and influenza while in literature, it was reported for malarial fever and liver complaints [47, 48]. From Shahpur Virkan and NavaPind C. sativum is reported for joints pain while in previous study it was reported as diuretic and for other digestive problems [35, 51]. Present study indicated that A. scoparia is diuretic in nature however it has been reported for earache, cardiac problem, fever and blood pressure [9, 54, 85]. Indigenous people of NavaPind and Shahpur Virkan are being using C. bonariensis for asthma and ulcer but in previous study it was reported for hemorrhage and diuretic [9, 86]. E. alba is discovered to be used as antidote of scorpio while previous researches indicated its use as laxative [48]. P. hysterophorus is used as blood purifier and backache, whereas in literature it was used in dysentery, fever and toothache [13, 14, 85, 86]. S. marianum is used as anticancer and wound healing but in literature it was used for Tuberculosis [58]. Another important discovery made during this study was use of B. campestris as anticancer while in previous study it was used for body massage and ulcer problems [52]. C. didymus is used for asthma while comparing to previous study it is used in rheumatism and bone disorder [48]. P. paniculata is used for stomach pain and wound healing while it was reported to minimize severe pain in the body [87]. C. pepo is used as skin tonic but according to the previous reports it was used as liver tonic [11]. E. helioscopia member of family Euphorbiacae expected to have large number of alkaloid is used for cancer and cholera treatment but in the study of Jandool Valley and Pind Dadan Khan, it was reported as laxative, skin tonic and respiratory disorders [88, 89].
A. arabica is an endangered species of Pakistan, used as skin tonic. Previous literature showed its efficacy for dysentery and cough [55]. A. farnesiana is used in diarrhea as it was used for toothache and leucorrhoea in the study of Shah et al. [49]. A. lebbeck is species very commonly used in Ayurveda, Siddha and Unani medicinal systems. Local people used this species for wound healing and postnatal care while in literature it was reported as antiallergic, skin tonic and for sexual disorder [49, 90], C. angustifolia is used as purgative, hair tonic and teeth tonic whereas in previous study it was used in rheumatism, blood purifier, CNS disorder and joints disorder [3, 47]. I. linifolia is used as liver tonic, blood purifier and for stomach complaints while in literature it was reported as amenorrhea [91]. M. indica recorded as skin tonic whereas it was reported for respiratory disorder and abdominal pain in the study of Azad Jammu and Kashmir [54]. M. pudica is being used as antidote and wound healing but it was reported in literature for menstrual disorder and asthma [86, 92]. Local use of V. faba is reported as diuretic while in other regions it was used for kidney pain and eye infection [68]. A. vera belonging to family Aleoaceae is used as cough and hair tonic. However previously it was use for sexual and stomach disorder [51, 92]. M. azadirachta is effective for wound healing. Already reported use of this species is as tonic for skin and sexual disorders [54, 93]. F. benghalensis an important rubber yielding species could also be used for diarrhea while it was already reported in the study of Makerwal and Gulla Khel as blood purifier and for diabetes [49, 94]. F. religiosa is locally used for asthma, diarrhea, ulcer, molar pain and cardiac problem as in literature it was reported as laxative and wound healing [55, 95]. Local use of E. globulus is used for influenza and stomach disorder but in the previous study it was reported for respiratory disorders [48].
S. cumini member of family Myrtaceae is used for the treatment of cancer whereas it was reported for respiratory disorder, ulcer and fever [45, 86]. Efficacy of A. sativa for postnatal care is recorded but literature indicates its use as diuretic, laxative, nerve tonic [9, 96]. The medicinal use of C. barbata is as skin tonic however it has been used for diabetes [86]. S. bengalensis could also be used for postnatal care and animal diseases while it was reported as diuretic too [47]. T. aestivum, cereal crop in Pakistan is discovered as anticancer and for GIT but from other regions of Pakistan it was reported for postnatal care and backache [45]. It is discover from present study that A. arvensis is good skin and hair tonic and diuretic. However its efficacy is already reported in rheumatism and CNS disorder [76, 86]. Z. jujube vernacular name is bari used as skin tonic, hair tonic and also good for joints disorder whereas it was reported for diarrhea, fever and blood purifier [45, 48]. V. thapsus is being for sexual disorder and internal bleeding in present study area while it was already reported to be effective as pain killer and used for stomach complaints, respiratory disorder [11, 97]. L. barbarum is used as anticancer and for asthma in present study area. but it was reported from Dhinodhar Hill for sexual disorder and skin tonic [89]. S. americanum is uncovered for joint disorders, while traditionally it is reported for fever and diarrhea [86]. W. somnifera is considered effective for animal diseases in Shahpur Virkan and NavaPind. However according to Kala [47] and Pervaiz [86] this could also be used for treating ulcer and eye infections.
Conclusions
This study is first quantitative documented information about the traditional uses of wild plants of NavaPind and Shahpur Virkan district Sheikhupura. This survey revealed that this area is rich in wild plants which are medicinally important. Mostly ethnobotanical information in study area is retained by elders, and most of them gained their knowledge from their fore fathers. Unfortunately present generation is not interested to carry this knowledge because of trends of modernization. Hence, there is a gradual loss of traditional knowledge about these plants in new generation. So, it is necessary to document the knowledge for future generation. From this ethnobotanical documented data it can be concluded that the most of plants species having medicinal value belong to family Fabaceae and Poaceae. Both of these families in NavaPind and Shahpur Virkan are represented by fifteen and sixteen species respectively. Both of these families are inhabitant of tropical and subtropical areas. As the most of areas in Punjab have tropical and subtropical conditions. Therefore Fabaceae and Poaceae are not only common in NavaPind and Shahpur Virkan but in the whole Punjab Province. The mode of preparation was decoction followed by extractions from various parts of plants. Quantitative values of ICF, UV, RFC, and FL reflect that study area is blessed with great diversity of medicinal plant and large number of plants are still used by the local people to cure various diseases of human being and animals. The comparative analysis (JI) strengthens the ethnobotanical findings and provides new useful knowledge.it is concluded there were almost 34 plant species reported with different medicinal uses as has been reported previously from different regions of Pakistan and neighboring countries (Table 5). These species were A. spinosus (antidote), A. viridis (antidote and diuretic), C. album (cough), C. sativum (joints pain), C. bonariensis (asthma and ulcer), E. alba (antidote of scorpion), P. hysterophorus (blood purifier and for back pain), S. marianum (anticancer and wound healing), B. campestris (anticancer), C. reflexa (wound healing), C. pepo (skin tonic), E. helioscopia (anticancer and cholera), R. communis (wound healing and hair tonic), A. lebbeck (wound healing, cough and postnatal care), C. angustifolia (purgative, hair tonic and teeth tonic), D. sissoo (hair tonic), M. indica (skin tonic), V. faba (diuretic), A. vera (cough and hair tonic), M. azadirachta (wound healing), F. benghalensis (influenza and diarrhea), F. religiosa (asthma, diarrhea, ulcer, molar pain and cardiac problem), S. cumini (heart problem), O. corniculata (antidote), A. sativa (postnatal care), T. aestivum (Anticancer and for GIT), A. arvensis (skin tonic, hair tonic and diuretic), R. muricatus (fever and asthma), V. thapsus (male disease and internal bleeding), L. barbarum (anticancer and for asthma), S. americanum (joints pain), W. somnifera (lung disorder, animal disease, male disease and asthma), U. dioca (joints pain, cold,flu and liver disease) and L. camara (cold and flu). Moreover 12 species (Carthamus ticntorius, Conyza erigeron, Schoenoplectus supinus, Ocimum sanctum, Allium roylei, Malva verticillata, Malva indica, Jasimunum nudiflorum, Asthenatherum forkalii, Digitalis ciliaris, Digitalis nodosa and Tetrapagon tenellus) were reported first time from Pakistan particularly for their medicinal uses. Comparison with ethnobotanical documentation from other Asian and SAARC (South Asian Association for regional Co-operation) countries indicated almost 8 species including Conyza erigero, Allium roylei, Malva verticillata, Malva indica, Jasimunum nudiflorum, Digitalis ciliaris, Digitalis nodosa and Tetrapagon tenellus were explored first time for their medicinal uses. All these medicinal plants either used in decoction, plaster form or in combination with other medicinal plants or salt for treatment of various diseases (Additional file 1: Table S2).
Table 5.
Comparison of traditional uses of plant species in the study area with other regions of Pakistan and neighboring country
| Sr. No. | Plant species | Uses reported in study area | Uses reported in previous study | References |
|---|---|---|---|---|
| 1 | Andrographis paniculata (Burm. f.) Wall. ex Nees | Cough, influenza, diarrhea, blood purifier | Liver complaints, malaria | [47, 48] |
| 2 | Amaranthus spinosus L. | Diarrhea, antidote, fever, fodder | Eye vision, skin tonic | [48, 68] |
| 3 | Amaranthus viridis L. | Constipation, skin tonic, antidote, diuretic, cooking | Joints pain, burning of feet | [35, 45] |
| 4 | Chenopodium album L. | Laxative, diuretic, cough, cooking | Throat trouble, paralysis, rheumatism, jaundice | [45, 49, 66] |
| 5 | Chenopodium murale L. | Laxative, vegetable, Fodder, dye | Anthelmintic | [72] |
| 6 | Achyranthes aspera (L.) Hill | Cough, laxative, stomach complains, fodder, fuel | Skin tonic, blood purifier, malaria fever | [3, 45, 90] |
| 7 | Coriandrum sativum L. | Joint pain, stomach complaints, cooking | Sexual disease | [100] |
| 8 | Calotropis procera R. Br. | Asthma, skin tonic, fever, fodder | Hair tonic, hepatitis, antidote, tooth tonic | [3, 48, 49, 53, 66] |
| 9 | Artemisia scoparia Waldst. & Kitt. | Diuretic, stomach complains, fodder | Antidote, fever, skin infection | [101] |
| 10 | Conyza bonariensis L. | Asthma, diarrhea, ulcer, fodder | Diuretic, blood purifier | [102, 103] |
| 11 | Eclipta alba (L.) Hassk. | Liver tonic, hair tonic, antidote of scorpio, fodder | GIT disorders | [48, 104] |
| 12 | Parthenium hysterophorus L. | blood purifier, back pain, fodder, Decoration, grow in crop | Fever | [45] |
| 13 | Silybum marianum L. | Anticancer, liver tonic, wound healing, fodder | Tuberculosis | [97] |
| 14 | Sonchus arvensis L. | Anti-kidney stone, asthma, cough, fodder | Wound healing | [45] |
| 15 | Xanthium strumarium L. | Fever, mother postnatal care, fodder | Toothache | [72] |
| 16 | Brassica campestris L. | Skin tonic, hair tonic, anti-cancerous | Headache, animal fever | [52, 95] |
| 17 | Brassica nigra L. | Diuretic, respiratory problems, fodder | GIT disease, toothache | [55, 105] |
| 18 | Capsella bursapastoris L. | Fodder, internal and external bleeding, diarrhea | Respiratory disease, sexual disease | [51] |
| 19 | Coronopus didymus (L.) Sm. | Asthma, Blood purifier | Insect repellent, joints disorder | [13, 85] |
| 20 | Sisymbrium irio L. | Fodder, asthma | Fever, skin tonic, cough | [35, 46, 72] |
| 21 | Cannabis sativa L. | Stomach complaints, Relaxant, Severe pains repellent | Male disease | [97] |
| 22 | Convolvulus arvensis L. | Fodder, animal fever, grow in crop | Skin tonic, liver tonic, GIT disorder | [3, 53] |
| 23 | Cuscuta reflexa Roxb. | Wound healing, Hair tonic | Blood purifier, relaxant, fever | [46, 97, 106] |
| 24 | Poranopsis paniculata (Roxb.) Roberty | Decoration, stomach pain, diarrhea, wound healing | Body pain | [50] |
| 25 | Cucurbita pepo L. | Skin tonic, cardiac problem, stomach disorder, Cooking, | Jaundice | [53] |
| 26 | Euphorbia helioscopia L. | Anticancerous, cholera | Skin tonic, GIT disorder, wound healing | [35, 46, 53] |
| 27 | Euphorbia hirta L. | Fodder | Skin tonic, sexual disorder, relaxant, GIT disorder, respiratory disorder |
[3, 90, 97, 106] |
| 28 | Euphorbia thymifolia L. | Fodder | Blood pressure | [3] |
| 29 | Ricinus communis L. | Wound healing, fuel, hair tonic | GIT disorder, postnatal care, headache, hepatitis | [45, 48, 53, 98] |
| 30 | Sapium sebiferum L. | Antidote, Fodder, fuel, furniture | GIT disorder | [107] |
| 31 | Acacia.nilotica | Fodder | GIT disorder, sexual disorder wound healing, skin tonic | [3, 46, 98, 106, 108] |
| 32 | Acacia arabica Willd. | Diarrhea, Skin tonic, roof, fuel, fodder, exported | Respiratory disorder | [106] |
| 33 | Acacia farnesiana L. | Diarrhea, perfume, fuel, furniture, exported | Toothache, sexual disorder | [49] |
| 34 | Albizia lebbeck (L.) Benth. | Fuel, wound healing, Cough, burning, postnatal care | Skin tonic | [48, 49] |
| 35 | Cassia angustifolia L. | Purgative, hair tonic, teeth tonic | Blood purifier, sexual disorder, rheumatism | [3, 47] |
| 36 | Cassia fistula L. | Laxative, constipation, fodder, cough, stomach pain | Hepatitis | [48, 90, 106] |
| 37 | Cassia occidentalis L. | Fuel, roof, bitter taste, stomach disorder, laxative | Respiratory disorder | [48] |
| 38 | Dalbergia sissoo Roxb. ex DC. | Fodder, fuel, furniture, wound healing, hair tonic | Sexual disease, GIT disease, fever, diuretic | [48, 49] |
| 39 | Indigofera linifolia (L.f) Retz. | Fodder, obtain dye, Stomach complaints, blood purifier, for liver | Sexual disease | [67, 85] |
| 40 | Lathyrus aphaca L. | Fodder | Cough | [45] |
| 41 | Melilotus indica L. | Laxative, diarrhea, cooking, fodder, bitter taste, skin tonic | Respiratory disorder, sexual disease | [54, 109] |
| 42 | Mimosa pudica L. | Fuel, fodder, antidote, wound healing, diarrhea | Menstrual disorder, respiratory disease | [86, 92] |
| 43 | Tamarindus indica L. | Malaria, fever, bitter taste, Laxative, burning | Jaundice | [48] |
| 44 | Vicia faba L. | Diuretic, fodder, food, soap | Eye infection | [68] |
| 45 | Ocimum basilicum L. | Scent, flavoring, cough, headache, diarrhea | Influenza, cardiac problem, antidote | [53, 104] |
| 46 | Ocimum sanctum L. | Appetizer, mosquito repellent, fodder, fever, cough | Liver tonic | [47, 106, 110] |
| 47 | Aloe vera (L.) Burm. f. | Skin tonic, cough, hair tonic, fever | Liver tonic | [48, 108] |
| 48 | Lawsonia inermis L. | Wound healing, hair tonic | Diuretic, jaundice | [46, 48] |
| 49 | Malvastrum coromandelianum L. | Fodder, wound healing | Fever, GIT disorders | [49] |
| 50 | Azadirachta indica A. Juss | Fodder, skin tonic, fuel | Hair tonic, sexual disorders, eye infection, GIT disorders, liver tonic | [3, 48, 106, 108] |
| 51 | Melia azadirachta L. | Wound healing, shade, cough, fuel, furniture, fodder | Skin tonic, hair tonic | [93] |
| 52 | Ficus sarmentosa Bush: Ham. ex J.E. Smith | Fuel, fodder | Respiratory disease, GIT disorder | [111] |
| 53 | Ficus benghalensis L. | Influenza, shade, diarrhea, fuel, decoction | Asthma, liver tonic | [45, 47, 49] |
| 54 | Ficus religiosa L. | Asthma, diarrhea Shade, fuel, fodder, ulcer, molar pain, cardiac problem | Wound healing | [49] |
| 55 | Morus alba L. | Cough, fodder, respiratory disorders | GIT disorder | [11] |
| 56 | Eucalyptus globulus Labill. | Influenza, skin tonic, Fuel, furniture, stomach disorder | Liver tonic | [48] |
| 57 | Syzygium cumini L. | Fruit, fuel, fodder, cancer, heart problem, diarrhea | Nervous disorder, fever | [45, 108] |
| 58 | Oxalis corniculata L. | Antidote, stomach disorder, vegetable, fodder | Liver tonic, diuretic, joints problem | [46, 88] |
| 59 | Fumaria indica Linn. | Laxative, fodder | GIT disorder, liver tonic, diuretic, skin tonic | [45, 53, 93] |
| 60 | Acrachne racemosa (Roem & schult) | Fodder | General debility | [48] |
| 61 | Avena sativa L. | Postnatal care | Nervous disorder, GIT disorders | [53, 97] |
| 62 | Cenchrus setigerus Vahl. | Fodder | Fever, skin tonic, GIT disorder | [66] |
| 63 | Chloris barbata Sw. | Fodder, skin disorder | Respiratory disease | [112] |
| 64 | Chrysopogon aucheri Bioss | Fodder, fuel | GIT disorder | [54] |
| 65 | Cynodon dactylon (L.) Pers. | Stomach complaint, constipation, antidote for snake and dogs, fodder | Diuretic, wound healing, fever | [3, 48, 49, 108] |
| 66 | Eleusine indica (L.) Gaertn. | Fodder | Diuretic, GIT disorder | [96] |
| 67 | Pennisetum divisum (Fosslk. ex J. F. Gmel) | Fodder | GIT disorder | [66] |
| 68 | Phragmites karka (Retz.) Trin. ex Steud. | Cardiac problem, fuel | Respiratory disorder | [16] |
| 69 | Saccharum bengalensis L. | Roof, fuel, pre/post natal care, animal disease | Diuretic | [91] |
| 70 | Triticum aestivum L. | Fodder, anticancerous, gastrointestinal disease | Postnatal care, backache | [45] |
| 71 | Rumex chalepensis Mill. | Fodder | Insect repellent | [113] |
| 72 | Anagallis arvensis L. | Fodder, skin tonic, Diuretic, hair tonic | Nervous disorder | [90, 104] |
| 73 | Ranunculus muricatus L. | Fodder, fever, asthma, Fodder | Wound healing, skin tonic | [45, 46] |
| 74 | Ranunculus repens L. | Fodder | Nervous disorder, blood purification | [84] |
| 75 | Zizyphus jujuba (L.) Lam. | Fruit, furniture, skin tonic, joints pain, hair tonic, backache, burning | Liver tonic, GIT disorder | [45, 48] |
| 76 | Murraya koenigii L. | Stomach diseases, wound healing, vomiting, scent, decoration | Blood purification | [86] |
| 77 | Salix lanata L. | Fever, reduce internal pain, fodder, bitter taste | Respiratory disorder | [3] |
| 78 | Verbascum thapsus L. | Male disease, internal bleeding | Wound healing, nervous disorder, respiratory disorder | [11, 49] |
| 79 | Lycium barbarum L. | Anticancerous, asthma, scent, fodder | Diuretic, skin tonic | [89, 114] |
| 80 | Solanum americanum Mill. | Joints pain, cooking, Perfume, vegetable, fodder | GIT disorders. fever | [48] |
| 81 | Withania somnifera L. | Lung disorder, animal disease, asthma, male disease | Fever, joint pain, liver tonic, sexual disorder, eye infection | [45–47, 53, 66, 108] |
| 82 | Urtica dioica L. | Joints pain, cold and flu, liver disease | Skin tonic, GIT disorder, fever | [91, 115] |
| 83 | Lantana camara L. | Fodder, snake bite, cold and flu | Malaria fever | [49] |
| 84 | Phyla nodiflora L. | Fodder | GIT disorder, diuretic, blood purifier, wound healing, hair tonic | [45, 46, 49, 104] |
Fl value is calculated for Bold diseases
The traditional medicine used in the region lacks physiotherapeutic evidence. It is necessary to perform phytochemical and pharmacological studies to explore the potential of such plants herbal drug discovery. This study also provides basis for the conservation of the local flora. It will also provide various socio-economic dimensions associated with the common people. Further strategies should be taken for conservation of these medicinal plants on priority in NavaPind and ShahpurVirkan, Sheikhupura, Pakistan.
Acknowledgments
Not applicable.
Funding
No funding was available for this particular project. Already available resource of Molecular taxonomy lab, Lahore College for Women University, Lahore were utilized for this study.
Availability of data and materials
Voucher specimens were deposited in Herbarium of Lahore College for Women University for future use (Additional file 1: List S1).
Authors’ contributions
MZ and TA visited study area and collect the information they also play main role in writing manuscript. ZY supervise the whole study, help to identify the collected specimen and help in writing manuscript. MH, NS, SJ and MQ help in preserving the collected specimen they also assist in collecting ethno botanical information from the study area. AA and HR helps in statistical analysis and language corrections. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Permission was taken from Chairman (representative of local government) of Shahpur Virkan and NavaPind, Sheikhupura to visit the area and collect the plant specimen. Moreover permission was taken from each individual prior to interview.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
List S1. Names of plant species with accession numbers. Table S1. Preparation and administration of various herbal remedies frequently used in NavaPind and Shahpur Virkan, district Sheikhupura, Province Punjab, Pakistan. Annex S1. Questionnaire. (DOCX 46 kb)
Contributor Information
Maria Zahoor, Email: maria.zahoor12345@gmail.com.
Zubaida Yousaf, Email: z4zubaida@yahoo.com, Email: mussab.wajahat@gmail.com.
Tahreem Aqsa, Email: Taqsa1236@gmail.com.
Manahil Haroon, Email: haroon@yahoo.com.
Nadia Saleh, Email: nadiasaleh14@yahoo.com.
Arusa Aftab, Email: arusa_ravi@yahoo.com.
Sadia Javed, Email: jsadia93@gmail.com.
Mouzma Qadeer, Email: mouzma@hotmail.com.
Habiba Ramazan, Email: habibalcwu0@gmail.com.
References
- 1.Mesfin F, Demissew S, Teklehaymanot T. An ethnobotanical study of medicinal plants in WonagoWoreda, SNNPR, Ethiopia. J Ethnobiol Ethnomed. 2009;5:28. doi: 10.1186/1746-4269-5-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vitalini S, Iriti M, Puricelli C, Ciuchi D, Segale A, Fico G. Traditional knowledge on medicinal and food plants used in Val San Giacomo (Sondrio, Italy) an alpine ethnobotanical study. J Ethnopharmacol. 2013;145:517–29. doi: 10.1016/j.jep.2012.11.024. [DOI] [PubMed] [Google Scholar]
- 3.Yaseen G, Ahmad M, Sultana S, Alharrasi AS, Hussain J, Zafar S, Rehman SU. Ethnobotany of medicinal plants in the Thar Desert (Sindh) of Pakistan. J Ethnopharmacol. 2015;163:43–59. doi: 10.1016/j.jep.2014.12.053. [DOI] [PubMed] [Google Scholar]
- 4.Ahmed H. Issues regarding the medicinal plants of Pakistan. Dyane Today. 1999; 6:6–7.
- 5.Lentini F, Di Martino A, Amenta R. Le piante di usopopolarenell’ arcipelagodelle Pelagie (Ag). L’uomo e l’ambiente. 1995; 19:117–121.
- 6.Sanz-Biset J, Campos-de-la-Cruz J, Epiquién-Rivera MA, Cañigueral S. A first survey on the medicinal plants of the Chazuta valley (Peruvian Amazon) J Ethnopharmacol. 2009;122:333–62. doi: 10.1016/j.jep.2008.12.009. [DOI] [PubMed] [Google Scholar]
- 7.Ladio AH, Lozada M. Patterns of use and knowledge of wild edible plants in distinct ecological environments: a case study of a Mapuche community from northwestern Patagonia. Biodivers Conserv. 2004;13:1153–73. doi: 10.1023/B:BIOC.0000018150.79156.50. [DOI] [Google Scholar]
- 8.Goleniowski ME, Bongiovanni GA, Bongiovanni L, Palacio CO, Cantero JJ. Medicinal plants from the “Sierra de Comechingones”, Argentina. J Ethnopharmacol. 2006;107:324–41. doi: 10.1016/j.jep.2006.07.026. [DOI] [PubMed] [Google Scholar]
- 9.Ahmad I, Ibrar M, Barkatullah, Ali N. Ethnobotanical Study of Tehsil Kabal, Swat District, KPK, Pakistan. J Bot. 2011;2011:1–9. doi: 10.1155/2011/368572. [DOI] [Google Scholar]
- 10.Marwat SK, Rehman FU, Khan MA, Ahmad M, Zafar M, Ghulam S. Medicinal folk recipes used as traditional phyto therapies in district Dera Ismail Khan, KPK, Pakistan. Pak J Bot. 2011;43(2):1453–62. [Google Scholar]
- 11.Alamgeer TA, Rashid M, Malik MNH, Mushtaq MN, Khan J, Qayyum R, Khan AQ, Muhammad N. Ethnomedicinal survey of plants of valley Allad and Dehri, Tehsil Batkhela, District Malakand, Pakistan. IJBMSP. 2013;3(1):23–32. [Google Scholar]
- 12.Goodman SM, Ghafoor A. The ethnobotany of Southern Baluchistan, Pakistan, with particular reference to medicinal plants. Fieldiana Bot. 1995;1(31):1–84. [Google Scholar]
- 13.Qureshi R, Waheed A, Arshad M, Umbreen T. Medico-ethnobotanical inventory of Tehsil Chakwal, Pakistan. Pak J Bot. 2009;41(2):529–38. [Google Scholar]
- 14.Qureshi RA, Ghufran MA, Gilani SA, Yousaf Z, Abbas G, Batool A. Indigenous medicinal plants used by local women in southern Himalayan regions of Pakistan. Pak J Bot. 2009;41:19–25. [Google Scholar]
- 15.Qureshi R, RazaBhatti G. Ethnobotany of plants used by the Thari people of Nara Desert, Pakistan. Fitoterapia. 2008;79:468–73. doi: 10.1016/j.fitote.2008.03.010. [DOI] [PubMed] [Google Scholar]
- 16.Khan T, Khan IA, Rehman A, Ali H. Ethnobatanical studies on non-medicinal plants of Shinaki Valley Hunza, Gilgit-Baltistan. Int J Biosci. 2013;3:63–70. doi: 10.12692/ijb/3.11.63-70. [DOI] [Google Scholar]
- 17.Pie, Manandhara The percentage of medicinal wild species in himalayan ranges. Pak J Bot. 1987;10(6):65–74. [Google Scholar]
- 18.Farnsworth NR. Screening plants for new medicines. In: Wilson EO, Peter FM, editors. Biodiversity. Washington, D. C: National Academy Press; 1988. pp. 83–97. [Google Scholar]
- 19.Qureshi R. Floristic and Ethnobotanical study of Desert-Nara region, Sindh, Pakistan (Doctoral dissertation) Research Repository. Shah Abdul Latif University, Khairpur. 2004;4(1):1–454. [Google Scholar]
- 20.Hamayun M. Ethnobotanical studies of some useful shrubs and trees od district Buner, NWFP, Pakistan. J Ethnobotanical Leaflets. 2003;2003(1):1–12. [Google Scholar]
- 21.Malik TJ. Pre-investment study district Sheikhupura. Pak J Bot. 2009; 9–31.
- 22.Kadam P, Bhalerao S. Sample size calculation. Int J Ayurveda Res. 2010;1(1):55–7. doi: 10.4103/0974-7788.59946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ahmad M, Khan MA, Zafar M, Sultana S. Treatment of common ailments by plant based remedies among the people of district Attock (Punjab) of Northern, Pakistan. Afr J Tradit Complement Altern Med. 2007;4(1):112–20. doi: 10.4314/ajtcam.v4i1.31201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tabuti J, Lye K, Dhillion S. Traditional herbal drugs of Bulamogi, Uganda: plants, use and administration. J Ethnopharmacol. 2003;88:19–44. doi: 10.1016/S0378-8741(03)00161-2. [DOI] [PubMed] [Google Scholar]
- 25.Teklehaymanot T. Ethnobotanical study of knowledge and medicinal plants use by the people in Dek Island in Ethiopia. J Ethnopharmacol. 2009;124:69–78. doi: 10.1016/j.jep.2009.04.005. [DOI] [PubMed] [Google Scholar]
- 26.Canales M, Hernández T, Caballero J, Vivar A, Avila G, Duran A, Lira R. Informant consensus factor and antibacterial activity of the medicinal plants used by the people of San Rafael Coxcatlán, Puebla, México. J Ethnopharmacol. 2005;97:429–39. doi: 10.1016/j.jep.2004.11.013. [DOI] [PubMed] [Google Scholar]
- 27.Akerele O. Medicinal plants and primary health care: an agenda for action. Fitoterapia. 1988;59:355–63. [Google Scholar]
- 28.Kloutsos G, Balatsouras DG, Kaberos AC, Kandiloros D, Ferekidis E, Economou C. Upper airway edema resulting from use of Ecballium elaterium. Laryngoscope. 2001;111:1652–5. doi: 10.1097/00005537-200109000-00030. [DOI] [PubMed] [Google Scholar]
- 29.Abu-Irmaileh BE, Afifi FU. Herbal medicine in Jordan with special emphasis on commonly used herbs. J Ethnopharmacol. 2003;89:193–7. doi: 10.1016/S0378-8741(03)00283-6. [DOI] [PubMed] [Google Scholar]
- 30.Friedman J, Yaniv Z, Dafni A, Palewitch D. A preliminary classification of the healing potential of medicinal plants, based on a rational analysis of an ethnopharmacological field survey among Bedouins in the Negev Desert, Israel. J Ethnopharmacol. 1986;16:275–87. doi: 10.1016/0378-8741(86)90094-2. [DOI] [PubMed] [Google Scholar]
- 31.Bennett BC, Prance GT. Introduced plants in the indigenous pharmacopoeia of Northern South America. Econ Bot. 2000;54:90–102. doi: 10.1007/BF02866603. [DOI] [Google Scholar]
- 32.González-Tejero M, Casares-Porcel M, Sánchez-Rojas C, Ramiro-Gutiérrez J, Molero-Mesa J, Pieroni A, Giusti M, Censorii E, De Pasquale C, Della A. Medicinal plants in the Mediterranean area: synthesis of the results of the project Rubia. J Ethnopharmacol. 2008;116:341–57. doi: 10.1016/j.jep.2007.11.045. [DOI] [PubMed] [Google Scholar]
- 33.Lulekal E, Asfaw Z, Kelbessa E, VanDamme P. Ethnomedicinal study of plants used for human ailments in Ankober District, North Shew Zone, Amhara region. J Ethnobiol Ethnomed. 2013;9:63. doi: 10.1186/1746-4269-9-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Giday M, Asfaw Z, Woldu Z. Medicinal plants of the Meinit ethnic group of Ethiopia: an ethnobotanical study. J Ethnopharmacol. 2009;124:513–21. doi: 10.1016/j.jep.2009.05.009. [DOI] [PubMed] [Google Scholar]
- 35.Bibi T, Ahmad M, Tareen RB, Tareen NM, Jabeen R, Rehman SU, Sultana S, Zafar M, Yaseen G. Ethnobotany of medicinal plants in district Mastung of Balochistan province, Pakistan. J Ethnopharmacol. 2014;157:79–89. doi: 10.1016/j.jep.2014.08.042. [DOI] [PubMed] [Google Scholar]
- 36.Kadir MF, Bin Sayeed MS, Mia M. Ethnopharmacological survey of medicinal plants used by indigenous and tribal people in Rangamati, Bangladesh. J Ethnopharmacol. 2012;144:627–37. doi: 10.1016/j.jep.2012.10.003. [DOI] [PubMed] [Google Scholar]
- 37.Kadir MF, Bin Sayeed MS, Mia M. Ethnopharmacological survey of medicinal plants used by traditional healers in Bangladesh for gastrointestinal disorders. J Ethnopharmacol. 2013;147:148–56. doi: 10.1016/j.jep.2013.02.023. [DOI] [PubMed] [Google Scholar]
- 38.Mahishi P, Srinivasa B, Shivanna M. Medicinal plant wealth of local communities in some villages in Shimoga District of Karnataka, India. J Ethnopharmacol. 2005;98:307–12. doi: 10.1016/j.jep.2005.01.035. [DOI] [PubMed] [Google Scholar]
- 39.Ignacimuthu S, Ayyanar M, Sankarasivaraman K. Ethnobotanical study of medicinal plants used by Paliyartribals in Theni district of Tamil Nadu, India. Fitoterapia. 2008;79:562–8. doi: 10.1016/j.fitote.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 40.Ignacimuthu S, Shanmugam N. Antimycobacterial activity of two natural alkaloids, vasicine acetate and 2-acetyl benzylamine, isolated from Indian shrub Adhatodavasica Ness, Leaves. J Biosciences. 2010;35:565–70. doi: 10.1007/s12038-010-0065-8. [DOI] [PubMed] [Google Scholar]
- 41.Srithi K, Balslev H, Wangpakapattanawong P, Srisanga P, Trisonthi C. Medicinal plant knowledge and its erosion among the Mien (Yao) in northern Thailand. J Ethnopharmacol. 2009;123:335–42. doi: 10.1016/j.jep.2009.02.035. [DOI] [PubMed] [Google Scholar]
- 42.Cakilcioglu U, Turkoglu I. An ethnobotanical survey of medicinal plants in Sivrice (Elazığ-Turkey) J Ethnopharmacol. 2010;132:165–75. doi: 10.1016/j.jep.2010.08.017. [DOI] [PubMed] [Google Scholar]
- 43.González JA, García-Barriuso M, Amich F. Ethnobotanical study of medicinal plants traditionally used in the Arribesdel Duero, western Spain. J Ethnopharmacol. 2010;131:343–55. doi: 10.1016/j.jep.2010.07.022. [DOI] [PubMed] [Google Scholar]
- 44.Ayyanar M, Ignacimuthu S. Ethnobotanical survey of medicinal plants commonly used by Kanitribals in Tirunelveli hills of Western Ghats, India. J Ethnopharmacol. 2011;134:851–64. doi: 10.1016/j.jep.2011.01.029. [DOI] [PubMed] [Google Scholar]
- 45.Qureshi R, Ain Q, Ilyas M, Rahim G, Ahmad W, Shaheen H, Ullah K. Ethnobotanical study of Bhera, District Sargodha, Pakistan. Archives Des Sciences. 2012;65(11):690–707. [Google Scholar]
- 46.Iqbal H, Sher Z, Khan ZU. Medicinal plants from salt range Pind Dadan Khan, district Jhelum, Punjab, Pakistan. J Med Plant Res. 2011;5(11):2157–68. [Google Scholar]
- 47.Kala CP, Dhyani PP, Sajwan BS. Developing the medicinal plants sector in northern India: challenges and opportunities. J Ethnobio and Ethnomed. 2006;2(1):32. doi: 10.1186/1746-4269-2-32. [DOI] [Google Scholar]
- 48.Kumar MS, Ankit S, Gautam DN, Anil Kumar S. Biodiversity and indigenous uses of medicinal plant in the Chandra Prabha wildlife sanctuary, Chandauli district, Uttar Pradesh. Int J Biodiv. 2015;2015:1–11. doi: 10.1155/2015/394307. [DOI] [Google Scholar]
- 49.Shah A, Marwat SK, Gohar F, Khan A, Bhatti KH, Amin M, Din N, Ahmad M, Zafar M. Ethnobotanical study of medicinal plants of semi-tribal area of Makerwal and GullaKhel (lying between Khyber Pakhtunkhwa and Punjab provinces), Pakistan. Am J Plant Sci. 2013;4:98–116. doi: 10.4236/ajps.2013.41015. [DOI] [Google Scholar]
- 50.Acharya KP, Rokaya MB. Ethnobotanical survey of medicinal plants traded in the streets of Kathmandu valley. Scientific World. 2005;3(3):44–8. [Google Scholar]
- 51.Sadeghi Z, Mahmood A. Ethno-gynecological knowledge of medicinal plants used by Baluch tribes, southeast of Baluchistan, Iran. Rev Brass Farmacogn. 2014;24:706–15. doi: 10.1016/j.bjp.2014.11.006. [DOI] [Google Scholar]
- 52.Akhtar N, Rashid A, Murad W, Bergmeier E. Diversity and use of ethno-medicinal plants in the region of Swat, North Pakistan. J Ethnobio and Ethnomed. 2013;9(25):1–13. doi: 10.1186/1746-4269-9-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Nasrullah Nisar M, Suliman Ali Z. Ethnobotanical wealth of Jandool Valley, Dir Lower, Khyber Pakhtunkhwa (KPK), Pakistan. Int J Phytomed. 2012;4:351–354. [Google Scholar]
- 54.Amjad MS, Arshad M, Qureshi R. Ethnobotanical inventory and folk uses of indigenous plants from Pir Nasoora National Park, Azad Jammu and Kashmir. Asian Pac J Trop Biomed. 2015;5(3):234–41. doi: 10.1016/S2221-1691(15)30011-3. [DOI] [Google Scholar]
- 55.Ghani A, Ali Z, Perveen S. Folk recipes and ethno botanical survey of medicinal plants Mianwali district (Pakistan). Int J Current Pharma Res. 2012;4(2):61–3. [Google Scholar]
- 56.Shrestha PM, Dhillion SS. Medicinal plant diversity and use in the highlands of Dolakha district, Nepal. J Ethnopharmacol. 2003;86(1):81–96. doi: 10.1016/S0378-8741(03)00051-5. [DOI] [PubMed] [Google Scholar]
- 57.Gurdal B, Kultur S. An ethnobotanical study of medicinal plants in Marmaris (Mŭgla, Turkey) J Ethnopharmacol. 2013;146:113–26. doi: 10.1016/j.jep.2012.12.012. [DOI] [PubMed] [Google Scholar]
- 58.Ahmad M, Shazia S, Fazl-i-Hadi S, Hadda TB, Rashid S, Zafar M, Khan MA, Khan MPZ, Yaseen G. An ethnobotanical study of medicinal plants in high mountainous region of Chail valley (District Swat-Pakistan) J Ethnobiol Ethnomed. 2014;10:1–36. doi: 10.1186/1746-4269-10-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Andrade-Cetto A. Ethnobotanical study of the medicinal plants from Tlanchinol, Hidalgo, México. J Ethnopharmacol. 2009;122:163–71. doi: 10.1016/j.jep.2008.12.008. [DOI] [PubMed] [Google Scholar]
- 60.Poonam K, Singh GS. Ethnobotanical study of medicinal plants used by the Taungya community in Terai Arc Landscape, India. J Ethnopharmacol. 2009;123:167–76. doi: 10.1016/j.jep.2009.02.037. [DOI] [PubMed] [Google Scholar]
- 61.Mood SG. A contribution to some ethnobotanical aspects of Birjand flora (Iran) Pak J Bot. 2008;40:1783–91. [Google Scholar]
- 62.Lee S, Xiao C, Pei S. Ethnobotanical survey of medicinal plants at periodic markets of Honghe Prefecture in Yunnan Province, SW China. J Ethnopharmacol. 2008;117:362–77. doi: 10.1016/j.jep.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 63.Ssegawa P, Kasenene JM. Medicinal plant diversity and uses in the Sango bay area, Southern Uganda. J Ethnopharmacol. 2007;113:521–40. doi: 10.1016/j.jep.2007.07.014. [DOI] [PubMed] [Google Scholar]
- 64.Prashanth D, Asha M, Amit A, Padmaja R. Anthelmintic activity of Butea monosperma. Fitoterapia. 2001;72:421–2. doi: 10.1016/S0367-326X(00)00333-6. [DOI] [PubMed] [Google Scholar]
- 65.Rajakumar N, Shivanna MB. Ethnomedicinal application of plants in the eastern region of Shimoga District, Karnataka, India. J Ethnopharmacol. 2009;126:64–73. doi: 10.1016/j.jep.2009.08.010. [DOI] [PubMed] [Google Scholar]
- 66.Ahmad S, Wariss HM, Alam K, Anjum S, Mukhtar M. Ethnobotanical studies of plants resources of Cholistan Desert, Pakistan. Int J Sci Res. 2012;3(6):1782–8. [Google Scholar]
- 67.Qureshi R, Bhatti GR, Memon RA. Ethnomedicinal uses of herbs from northern part of Nara desert, Pakistan. Pak J Bot. 2010;42:839–51. [Google Scholar]
- 68.Abbasi AM, Mir AK, Munir HS, Mohammad MS, Mushtaq A. Ethnobotanical appraisal and cultural values of medicinally important wild edible vegetables of Lesser Himalayas-Pakistan. Ethnobiol Ethnomed. 2013;9:84. doi: 10.1186/1746-4269-9-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bano A, Ahmad M, Saboor A, Hadda BT, Zafar M, Sultana S, Khan MP, Arshad M, Ashraf MA. Quantitative ethnomedicinal study of plants used in the Skardu valley at high altitude of Karakoram-Himalayan range, Pakistan. J Ethnobiol Ethnomed. 2014;10:43–71. doi: 10.1186/1746-4269-10-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Xavier TF, Kannan M, Lija L, Auxillia A, Rose AK, Kumar SS. Ethnobotanical study of Kani tribes in Thoduhills of Kerala, South India. J Ethnopharmacol. 2014;152:78–90. doi: 10.1016/j.jep.2013.12.016. [DOI] [PubMed] [Google Scholar]
- 71.Islam MK, Saha S, Mahmud I, Mohamad K, Awang K, Jamal-Uddin S, Rahman MM, Shilpi JA. An ethnobotanical study of medicinal plants used by tribal and native people of Madhupur forest area, Bangladesh. J Ethnopharmacol. 2014;151:921–30. doi: 10.1016/j.jep.2013.11.056. [DOI] [PubMed] [Google Scholar]
- 72.Ali H, Qaiser M. The ethnobotany of Chitral Valley, Pakistan with particular reference to medicinal plants. Pak J Bot. 2009;41(4):2009–41. [Google Scholar]
- 73.Jan G, Khan MA, Farhatullah, Jan FG, Ahmad M, Jan M, Zafar M. Ethnobotanical studies on some useful plants of Dir Kohistan Valleys, KPK, Pakistan. Pak J Bot. 2011;43(4):1849–52. [Google Scholar]
- 74.Hocking GM. Pakistan Medicinal Plants 1. Qualitas Plantarum. et Materiae Vegetabiles. 1958; 5:145–153.
- 75.Chaudhary II. Distribution of some important medicinal plants of West Pakistan. Pak J Sci Ind Res. 1961;4(4):207–11. [Google Scholar]
- 76.Panhwar AQ, Abro H. Ethnobotanical studies of mahalkohistan (Khirthar national park) Pak J Bot. 2007;39(7):2301–15. [Google Scholar]
- 77.Haq F, Ahmad H, Alam M, Ahmad I, Rahatullah Species diversity of vascular plants of Nandiar valley western Himalaya, Pakistan. Pak J Bot. 2010;42:213–29. [Google Scholar]
- 78.Babu RH, Savithramma N. Phytochemical screening of underutilized species of Poaceae. An Int J. 2013;1(10):947–51. [Google Scholar]
- 79.Paul D. A review on biological activities of common mallow (Malva sylvestris L.). Innovare J. Life Sci. 2016;4(5):1–5. [Google Scholar]
- 80.Shah NZ, Muhammad N, Khan AZ, Samie M, Khan H, Uddin G, Rauf A. Phytochemical analysis and antioxidant studies of Conyza bonarensis. Acad J Plant Sci. 2013;6(3):109–112. [Google Scholar]
- 81.Bhushan B, Sardana S, Bansal G. Phytochemical and pharmacognostical studies of leaves of Jasminum mesyni Hance. J Chem Pharma Res. 2015;7(4):922–926. [Google Scholar]
- 82.Adawiz K, Rawaa A-K, Ghalia S. Phytochemical screening and antioxidant activity of selected wild plants in Liliaceae family growing Syria. Int J Pharmco & Phytochem Res. 2016;8(2):2025–32. [Google Scholar]
- 83.Bhardwa A, Shakil NA, Jha V, Gupta RK. Screening of nutritional, phytochemical, antioxidant and antibacterial activity of underutilized seeds of Scirpus articulatus: the basis of Khubahi Ramdana industry. J Pharmaco and Phytochem. 2014;3(4):11–20. [Google Scholar]
- 84.Aslam MS, Choudhary BA, Uzair M, Ijaz AS. The genus Ranunculus: a phytochemical and ethnopharmacological review. Int J Pharm Pharmaceu Sci. 2012;4(5):15–22. [Google Scholar]
- 85.Mahmood A, Qureshi RA, Mahmood A, Sangi Y, Shaheen H, Ahmad I, Nawaz Z. Ethnobotanical survey of common medicinal plants used by people of district Mirpur, AJK, Pakistan. J Med Plants Res. 2011;5(18):4493–8. [Google Scholar]
- 86.Parvaiz M. Ethnobotanical studies on plant resources of Mangowal, District Gujrat, Punjab, Pakistan. AJP. 2014;4(5):364–370. [PMC free article] [PubMed] [Google Scholar]
- 87.Acharya D, Shrivastava K. Indigenous Herbal Medicines: Tribal Formulations and Traditional Herbal Practices, Aavishkar Publishers Distributor, Jaipur- India. 2008:2008(1):440.
- 88.Kayani S, Ahmad M, Sultana S, Shinwari ZK, Zafar M, Yaseen G, Hussain M, Bibi T. Ethnobotany of medicinal plants among the communities of Alpine and Sub-alpine regions of Pakistan. J Ethnopharmaco. 2015;164:186–202. doi: 10.1016/j.jep.2015.02.004. [DOI] [PubMed] [Google Scholar]
- 89.Patel Y, Patel RM, Mahato AKR, Joshi PN. Status and diversity of ethno-medicinal plants of Dhinodhar hill, Kachchh district, Gujarat. Int J Plant Animal Envir Sci. 2013;3(1):265–73. [Google Scholar]
- 90.Kumar M, Sheikh MA, Bussmann RW. Ethnomedicinal and ecological status of plants in Garhwal Himalaya. India J Ethnobio and Ethnomed. 2011;7(1):32. doi: 10.1186/1746-4269-7-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Qureshi RA, Ghufran MA, Gilani SA, Sultana K, Ashraf M. Ethnobotanical studies of selected medicinal plants of Sudhan gali and Ganga chotti hills, district Bagh, Azad Kashmir. Pak J Bot. 2007;39(7):2275–83. [Google Scholar]
- 92.Nduche MU, Omosum G, Okwulehie IC. Ethnobotanical survey of plants used as remedy for fertility conditions in Ebonyi State of Nigeria. SAJB. 2015;3(2B):214–221. [Google Scholar]
- 93.Awan MR, Jamal Z, Khan A. Ethnobotanical studies of economically important plants from mountainous region of Gilgit-Baltistan. Pak Sci Technol Dev. 2013;32(4):308–18. [Google Scholar]
- 94.Hamayum M, Afzal S, Khan MA. Ethnopharmacology, indigenous collection and preservation techniques of some frequently used medicinal plants of Utror and Gabral, District Swat, Pakistan. Afr J Trad Comp Alt Medi. 2006;3:57–73. [Google Scholar]
- 95.Mussarat S, Abdel-Salam NM, Tariq A, Wazir SM, Ullah R, Adnan M. Use of Ethnomedicinal plants by the people living around Indus River. Hind Pub Co. 2014;2014:1–14. doi: 10.1155/2014/212634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Razzaq A, Rashid A, Islam M, Iqbal A. Medicinal biodiversity of weeds and livelihood security of District Shangla, Pakistan. J Med Plants Res. 2013;7(16):1039–42. [Google Scholar]
- 97.Ahmad K, Hussain M, Ashraf M, Luqman M, Ashraf MY, Khan ZI. Indigenous vegetation of soon valley; at the risk of extinction. Pak J Bot. 2007;39(3):679–690. [Google Scholar]
- 98.Meena KL, Yadav BL. Some ethnomedicines plants of Southern Rajasthan, India. Indian J Tradit Knowl. 2010;9(1):169–72. [Google Scholar]
- 99.Ali SI. Significance of Flora with special reference Pakistan. Pak J Bot. 2008;40(3):967–971. [Google Scholar]
- 100.Ch MI, Khan MA. An ethnomedicinal inventory of plants used for family planning and sex diseases in Samahni valley, Pakistan. Ind J Traditional Knowledge. 2008;7(2):277–83. [Google Scholar]
- 101.Nadeem M, Shinwari ZK, Qaiser M. Screening of folk remedies by genus Artemisia based on ethnomedicinal surveys and traditional knowledge of native communities of Pakistan. Pak J Bot. 2013;45(1):111–117. [Google Scholar]
- 102.Shinwari ZK, Malik S, Karim AM, Faisal R, Qaiser M. Biological activities of commonly used medicinal plants from Ghazi Brotha, Attock district. Pak J Bot. 2015;47(1):113–120. [Google Scholar]
- 103.Ahmad SS. Medicinal wild plants from Lahore-Islamabad motorway (M-2) Pak J Bot. 2007;39(2):355. [Google Scholar]
- 104.Panhwar AQ, Abro H. Ethnobotanical studies of Mahal Kohistan (Khirthar National Park) Pak J Bot. 2007;39(7):2301–15. [Google Scholar]
- 105.Malik F, Hussain S, Mirza T, Hameed A, Ahmad S, Riaz H, Shah PA, Usmanghani K. Screening for antimicrobial activity of thirty-three medicinal plants used in the traditional system of medicine in Pakistan. J Med Plants Res. 2011;5(14):3052–60. [Google Scholar]
- 106.Sharma M, Kumar A. Ethnobotanical uses of medicinal plants: a review. Life. 2013;50:52. [Google Scholar]
- 107.Qureshi H, Arshad M, Bibi Y. Invasive flora of Pakistan: a critical analysis. J Biodiver Environ Sci. 2014;4:407–24. [Google Scholar]
- 108.Qureshi R, Maqsood M, Arshad M, Chaudhry AK. Ethnomedicinal uses of plants by the people of Kadhi areas of Khushab, Punjab, Pakistan. Pak J Bot. 2011;43(1):121–33. [Google Scholar]
- 109.Ghani A, Mustafa I, Ali Z, Ishtiaq M, Ahmed I, Hasan N. Ethno-medicinal survey of plants of Soon Valley, Khushab District, Punjab, Pakistan. J Med Plants Res. 2014;8(32):1031–4. doi: 10.5897/JMPR2012.292. [DOI] [Google Scholar]
- 110.Jha AK, Yogesh G. Ethnobotanical Studies of Plants Growing in the Forest Area of Bihar. Int J Innov Res and Dev. 2015;4(10):357–359. [Google Scholar]
- 111.Haq F, Ahmad H, Ullah R, Iqbal Z. Species diversity and ethno botanical classes of the Flora of Allai Valley District Battagram Pakistan. Int J Plant Res. 2012;2(4):111–23. doi: 10.5923/j.plant.20120204.03. [DOI] [Google Scholar]
- 112.Sher H, Aldosari A. Ethnobotanical survey on plants of veterinary importance around Al-Riyadh (Saudi Arabia) African J Pharm and Pharmaco. 2013;7(21):1404–10. doi: 10.5897/AJPP2012.2177. [DOI] [Google Scholar]
- 113.Abbasi AM, Khan MA, Ahmad M, Qureshi R, Arshad M, Jahan S, Zafar M, Sultana S. Ethnobotanical study of wound healing herbs among the tribal communities in Northern Himalaya Ranges District Abbottabad, Pakistan. Pak J Bot. 2010;6:3747–53. [Google Scholar]
- 114.Pai PG, Habeeba U, Ramya K, Pradeepthi MS, Belagali Y. Evaluation of diuretic effect of Lycium barbarum Linn. (Goji Berry) in rats. IJPSR. 2014;5(4):1411–1415. [Google Scholar]
- 115.Bokhari TZ, Raja R, Younis U, Bushra E, Ummara U. Medicinal importance of few plants from Azad Jammu & Kashmir, Pakistan. Fuuast J Biol. 2013;3(1):93–9. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Voucher specimens were deposited in Herbarium of Lahore College for Women University for future use (Additional file 1: List S1).


