Abstract
Background:
Posttraumatic stress disorder (PTSD) is a very common mental condition and a unique anxiety disorder.
Aim:
The present study tried to examine the correlation between kind of delivery and PTSD.
Subjects and Methods:
This prospective study evaluated 240 Iranian female residents of Tehran, Iran, during the third trimester of their pregnancy and 6–8 weeks after labor. Data were collected using the customized screening form, the Symptom Checklist-90, PTSD Symptom Scale (PSS), and Social Support Questionnaire. The collected data were then analyzed with SPSS software.
Results:
According to the participants' responses to the subscales of the PSS, reexperiencing, avoidance, and hyperarousal symptoms were present in 100, 25, and 77 participants, respectively. Moreover, 15 individuals manifested all three groups of symptoms. Therefore, the prevalence of PTSD in the studied population was 6.2%. The logistic regression analysis revealed PTSD to be 0.06 times more prevalent in women with poor social support after delivery than in those enjoying a desirable level of support (P < 0.01; odds ratio = 0.06). Based onChisquare test results, there was no significant correlation between the kind of delivery and the incidence of PTSD after delivery (P = 0.48).
Conclusion:
Since PTSD was more common after cesarean sections (than after vaginal deliveries), health policymakers need to develop efficient strategies to promote vaginal delivery.
Keywords: Delivery, Kind of delivery, Posttraumatic stress disorder
Introduction
Posttraumatic stress disorder (PTSD) is one of the most common mental disorders and distinguished from other anxiety disorders in that it occurs in the aftermath of a stressful event. The prevalence of this disorder is twice as much in women as in men and is influenced by various stressors including childbirth, hormonal imbalances, stressful life events such as mishaps, disasters, problems, and domestic violence.[1,2]
According to the Diagnostic and Statistical Manual for Mental Disorders (DSM-IV), PTSD symptoms fall into three clusters including reexperiencing symptoms (such as nightmares about or remembrance of the delivery), avoidance symptoms (e.g., avoiding a future pregnancy and selective ignoring of the event, i.e., amnesia), and hyperarousal symptoms (such as irritability and concentration problems).[3]
Childbirth is known as a traumatic event in various studies, and about 1.5%–6% of women develop the disorder after childbirth.[3,4]
Childbirth or delivery is a normal, inevitable process performed through two different methods –normal childbirth or cesarean section. The important point is the method that is preferred in each particular instance and under each particular circumstance.[5] The incidence of this disorder is especially higher when an emergency cesarean section or an instrumental delivery is performed compared to when elective cesarean section or normal delivery is performed.[6]
Studies suggest that a series of factors related to pregnancy and childbirth make the mother susceptible to this disorder; in fact, in some cases, some of these factors come into play even before conception. The factors include the type of delivery performed, obstetric interventions, unpleasant experiences during childbirth, the lack of social support and the cultural factors at play (the significance of the infant's gender), experiencing unfortunate events during the course of the pregnancy (such as the death of loved ones, divorce, and homelessness), fear of childbirth, having a history of psychiatric disorders (especially postpartum depression), and having a childhood history of sexual abuse. Of all these factors, those issues associated with pregnancy, and childbirth is more significant than the others.[3,6,7]
The incidence of this disorder results in complications leading to a vulnerable mother–child relationship and with an adverse effect on the infant's cognitive development. The symptoms of this disorder are debilitating and affect the mother's social, occupational, and psychological functions and her communication with her child and family.[8] If these risk factors are identified during the course of pregnancy, the incidence of the disorder can potentially be prevented. About 1,363,542 women give birth in Iran every year;[9] 35% of whom give birth through a cesarean section and are likely to experience delivery trauma.[6]
The present study was, therefore, conducted to determine the relationship between the type of delivery and PTSD after childbirth in Iranian women admitted to selected hospitals of Tehran.
Subjects and Methods
The present prospective analytical study was carried out from December 2012 to May 2013. The study participants included 240 pregnant women of Iranian origin aged 15–45 residing in Tehran, and in their third trimester of pregnancy at the initial stage of the study, who were then followed up with at 6–8 weeks postpartum, and who were admitted to health-care centers for receiving prenatal and delivery services. The appropriate sample size was determined according to the following formula:
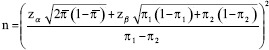
α = 0.05 → Zα = 1.65.
1 – β = 0.80 → Zβ = 0.85.
The study inclusion criteria consisted of a willingness to participate in the study and having no history of depression, other psychiatric disorders, hospitalization due to pregnancy complications, recent or old history of sexual, physical, or emotional abuse, and bearing or having delivered a healthy infant weighing more than 2500gr.
Data and measures
Data were collected using a researcher-made customized screening form comprising items on demographic, obstetric (maternal and neonatal), mental, and neurological characteristics of the participants. Content validity was used to confirm the validity of the form. Moreover, test–retest (on 10 individuals) with a 1-week interval resulted in a correlation coefficient of 98% and suggested the reliability of the tool.
The anxiety and depression subscales of the Symptom Checklist-90 (SCL-90) were administered to evaluate the subjects' mental health. The mentioned subscales contained consisted nine and 13 items, respectively. All items were scored on a five-point Likert scale from zero (never) to four (always). Levels of depression and anxiety were determined by dividing the total score of each subscale by the number of its items. While values <1 indicated the absence of the disorder, values 1–2, 2–3, and >3 suggested mild, moderate, and severe levels of the disorder, respectively. Previous studies have reported the validity of anxiety and depression subscales as 0.90 and 0.97, respectively. The test–retest reliability of the mentioned subscales has also been calculated as 0.85 and 0.75, respectively.[10] Social support after delivery was assessed using the second section of the Social Support Questionnaire. The questionnaire was developed by Winfield and Tiggemann and contained six yes/no items. The reliability and internal consistency of this questionnaire have been previously calculated as 0.80 and 0.95, respectively.[11]
The PTSD Symptom Scale (PSS) was administered to examine the presence of PTSD symptoms among the participating women. The PSS is a 17-item scale commonly used to diagnose PTSD and determine the severity of PTSD symptoms based on the DSM-IV criteria. It has been previously applied to measure the effects of delivery with a high degree of specificity. The PSS consists of three symptom clusters including reexperiencing (items 1–5), avoidance (items 6–12), and hyperarousal (items 13–17). All items are scored on a four-point scale from zero (not at all) to three (5 or more times per week/almost always). PTSD is present if the subject achieves a score ≥1 in at least one reexperiencing item, three avoidance items, and two hyperarousal items.[12,13,14,15,16,17,18,19] Concurrent validity and test–retest reliability of the PSS have been reported as 0.91 and 0.74, respectively.[12]
Data were collected in two stages – prenatal and postpartum.
Procedures
The study began after obtaining permissions from the relevant authorities and giving the study subjects' all the necessary information and inviting them for cooperation. Multistage sampling was performed. Health-care centers were first selected through the cluster sampling method, and then each cluster was allocated a specific share based on the number of patients admitted to the center. Sampling days were randomly set, and qualified women were selected through convenience sampling. First, the prenatal maternal factors' questionnaire and the anxiety and depression section of the SCL-90 were completed for the pregnant women in their third trimester of pregnancy and provided they met the inclusion criteria, a demographic questionnaire was completed for them and their telephone numbers and addresses were taken for evaluation at 6–8 weeks postpartum. At 6–8 weeks postpartum, their type of delivery was recorded, and they were then divided into two groups based on this variable. The posttraumatic stress diagnostic scale, the postpartum maternal and neonatal factors assessment, Winfield and Taigman's social support questionnaire, and the anxiety and depression section of the SCL-90 were completed for the subjects.
The study was approved by Shahid Beheshti University of Medical Sciences, Tehran, Iran. The code of Ethical Committee is 90-86-8375-1.
Statistical analysis
Data were analyzed in SPSS version 16 (Chicago, IL, USA) using the independent t-test, Chi-square test, Fisher's exact test, and Kruskal–Wallis test with a 95% confidence interval and given P < 0.05.
Results
From the 240 women who participated in the study, the 20–35 age group was the most frequent in both groups (normal delivery and cesarean section) and the age group over 35 the least frequent. The two groups were not significantly different in their socioeconomic status (monthly income, housing status, and floor area per capita) and, based on the subgroups of the posttraumatic stress diagnostic scale, 100 women showed reexperiencing symptoms, 25 showed abstinence symptoms, 77 increased arousal symptoms, and 15 showed all three symptoms and were therefore identified as suffering from PTSD after childbirth. The incidence of PTSD after childbirth was thus estimated at 6.2% (15/240) in the present study [Table 1].
Table 1.
The relationship between the subjects’ sociopersonal variables and posttraumatic stress disorder after childbirth in the normal delivery and the cesarean section groups in selected health-care centers in 2013
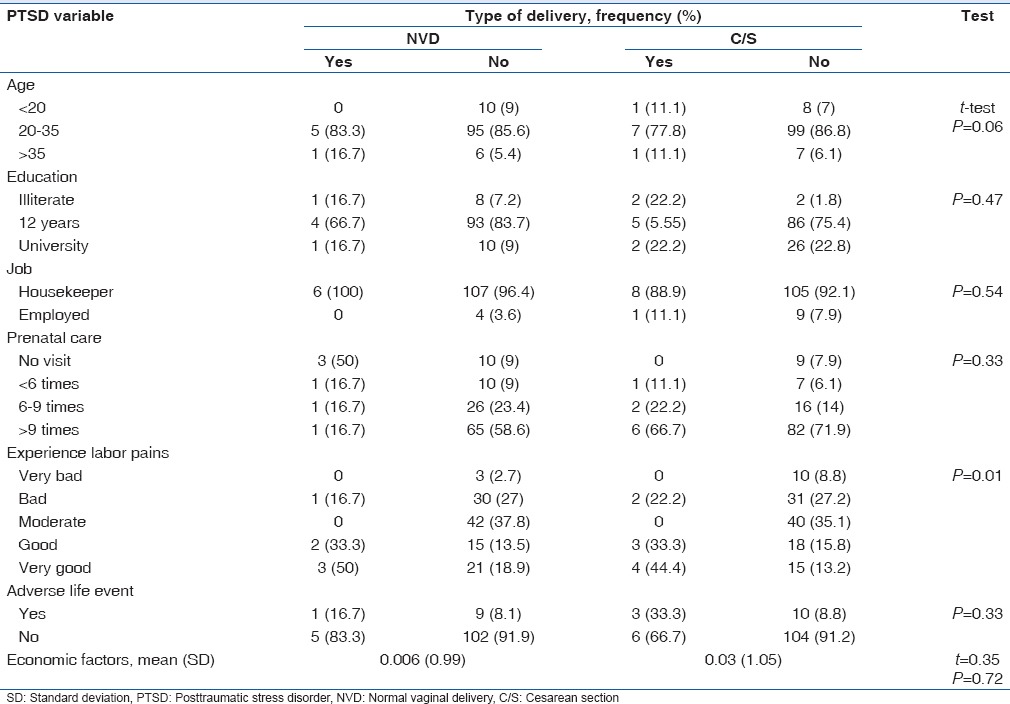
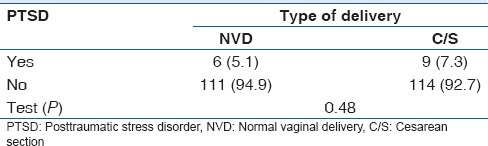
The Chi-square test revealed a significant relationship between the postpartum level of social support and PTSD after childbirth (P < 0.01). The logistic regression analysis also showed that the risk of experiencing PTSD is 0.06 times greater in women with poor social support than in women with good social support after childbirth (P < 0.01 and odds ratio = 0.06). The results of Kruskal–Wallis test revealed a significant relationship between depression and anxiety levels and PTSD after childbirth (P < 0.01) [Table 2]. Based on the results of Chi-square test, there is no significant relationship between the type of delivery and PTSD after childbirth (P = 0.48) [Table 3]. Nearly 64.2% (154/240) of the women had an emergency cesarean section, whereas 35.8% (86/240) of those had elective cesarean section. Almost 8.4% (13/154) of the women with an emergency cesarean section and 4.5% (4/86) of those with an elective cesarean section experienced PTSD. Although there was no significant relationship between the incidence rate of PTSD and the type of cesarean section (P = 0.37), based on the results of the study, the rate of the incidence of this disorder is higher after an emergency delivery than after the elective type.
Table 2.
Correlation between anxiety, depression, and social support with posttraumatic stress disorder after childbirth in the normal delivery and the cesarean section groups in selected healthcare centers in 2013
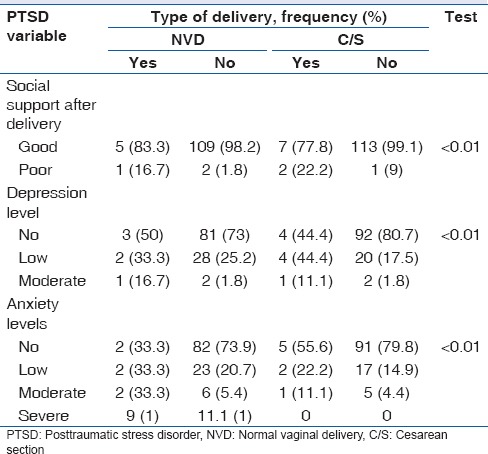
Table 3.
Correlation between kind of delivery with posttraumatic stress disorder after childbirth in the normal delivery and the cesarean section groups in selected health-care centers in 2013
Discussion
According to the findings of the present study, the prevalence of PTSD after childbirth is 6.2%. Shaban et al. reported the prevalence of this disorder to be 17.2% among women living in Zahedan and Modarres et al. reported it to be 20% among women living in Bushehr,[6,13] Andersen et al. reported the global prevalence of this disorder to be 1.5%–6%.[4]
While Grekin and O'Hara found its prevalence to be 3.1% in the general population and 15.7% in the high-risk population (identified by having a history of depression or psychiatric disorders, having unpleasant experiences, and encounters during childbirth, etc.).[8] The disparity of findings might be due to the cultural and socioeconomic differences between the different ethnic groups and countries studied, the populations surveyed, and the time and method of diagnosis with the disorder.
Although there was no statistically significant difference between the type of delivery (normal/cesarean section) and PTSD after childbirth, due to the 2.2% difference in the incidence rate of this disorder after cesarean section and normal childbirth, caesarean section was found to cause more cases of the disorder. Furthermore, the rate was different among women who had cesarean sections on emergency or electively, and the disorder was reported to be more prevalent among women who had an emergency cesarean section than those who had the elective type.
Compared to elective cesarean section and normal childbirth, emergency cesarean section is associated with more adverse postpartum and childbirth experiences, which count as risk factors for the incidence of stress disorder after childbirth; in fact, emergency cesarean can be an obstetric predictor for the development of this disorder. This type of delivery can also be a risk factor for postpartum psychiatric disorders. Evidence suggests that women who have undergone emergency cesarean sections have a more negative understanding and feeling about delivery.[6,7,8,9,10,11,12,13,14] However, Söderquist et al. found that the majority of women showing symptoms of PTSD have had normal deliveries. They argued that just as an emergency cesarean section is not necessarily traumatic and normal delivery can also be a traumatic experience for the mother.[15] The duration of labor, the experience of severe pain during childbirth, poor treatments by the personnel, and medical interventions are among factors associated with the incidence of this disorder.[4,8,13,14]
There was a significant difference between the postpartum level of social support and PTSD after childbirth, and the risk of the incidence of this disorder was 0.06 times greater in women with poor social support compared to the women with good social support. Studies reveal a significant relationship between social support and health. People with higher levels of social support enjoy better health. Studies also suggest that physiological responses to stress change depending on the level of social support; that is to say, the individual's intensity of reaction is lower in the presence of family and friends than when facing stress alone.[16,17] Social support acts as a buffer against stress and helps eliminate and manage the consequences of stressors, disease complications, etc.[18] A number of studies including those conducted by Ayers et al., Andersen et al., and Beck et al. confirmed the effective role of the spouse or sexual partner's support in reducing this disorder.[4,10,19]
They claimed one of the main factors predicting PTSD after childbirth (regardless of the type of delivery) to be proper support from the husband and family. The family support, the mother receives at home and at work from her family and coworkers have a critical role in determining her vulnerability to psychiatric disorders including the one investigated in the present study.[20]
Depression and anxiety levels were the other variables found to have a significant relationship with this disorder. One of the factors causing anxiety in mothers is fear of childbirth and its associated problems, and researchers believe that fear of childbirth is a key factor in developing traumatic responses after childbirth. In one study, Garthus-Niegel et al. found that women who confessed to their fear of childbirth at week 32 of their pregnancy showed more symptoms of PTSD than the other women. Studies on neurological and psychological factors indicate that fear of injury or the death of oneself or the infant has a significant relationship with PTSD. Examining women with PTSD revealed that these mothers experience excessive worry and fear about their own and their infant's health during the course of their pregnancy until childbirth. Other studies have also found that fear of injury or the death of oneself or the infant during labor and childbirth is a major predictor of postpartum psychiatric disorders. This factor might, therefore, be a strong predictor of adverse obstetric outcome.[3,4,21]
Conclusion
As discussed earlier, despite the absence of a significant correlation between the kind of delivery (cesarean section and normal delivery) and the incidence of PTSD, the disorder was 2.2% more prevalent in women who gave birth through cesarean section.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We would like to express our sincere gratitude to the Deputy of Research of Shahid Beheshti University of Medical Sciences for their encouragement.
References
- 1.Sadock BJ, Sadock VA, Kaplan HI. Kaplan and Sadock's Concise textbook of Child and Adolescent Psychiatry. Lippincott Williams and Wilkins; 2009. [Google Scholar]
- 2.Stein MB, Jang KL, Taylor S, Vernon PA, Livesley WJ. Genetic and environmental influences on trauma exposure and posttraumatic stress disorder symptoms: A twin study. Am J Psychiatry. 2002;159:1675–81. doi: 10.1176/appi.ajp.159.10.1675. [DOI] [PubMed] [Google Scholar]
- 3.Garthus-Niegel S, von Soest T, Vollrath ME, Eberhard-Gran M. The impact of subjective birth experiences on post-traumatic stress symptoms: A longitudinal study. Arch Womens Ment Health. 2013;16:1–10. doi: 10.1007/s00737-012-0301-3. [DOI] [PubMed] [Google Scholar]
- 4.Andersen LB, Melvaer LB, Videbech P, Lamont RF, Joergensen JS. Risk factors for developing post-traumatic stress disorder following childbirth: A systematic review. Acta Obstet Gynecol Scand. 2012;91:1261–72. doi: 10.1111/j.1600-0412.2012.01476.x. [DOI] [PubMed] [Google Scholar]
- 5.Souza JP, Gülmezoglu A, Lumbiganon P, Laopaiboon M, Carroli G, Fawole B, et al. Caesarean section without medical indications is associated with an increased risk of adverse short-term maternal outcomes: The 2004-2008 WHO Global Survey on Maternal and Perinatal Health. BMC Med. 2010;8:71. doi: 10.1186/1741-7015-8-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Modarres M, Afrasiabi S, Rahnama P, Montazeri A. Prevalence and risk factors of childbirth-related post-traumatic stress symptoms. BMC Pregnancy Childbirth. 2012;12:88. doi: 10.1186/1471-2393-12-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ayers S. Delivery as a traumatic event: Prevalence, risk factors, and treatment for postnatal posttraumatic stress disorder. Clin Obstet Gynecol. 2004;47:552–67. doi: 10.1097/01.grf.0000129919.00756.9c. [DOI] [PubMed] [Google Scholar]
- 8.Grekin R, O'Hara MW. Prevalence and risk factors of postpartum posttraumatic stress disorder: A meta-analysis. Clin Psychol Rev. 2014;34:389–401. doi: 10.1016/j.cpr.2014.05.003. [DOI] [PubMed] [Google Scholar]
- 9.Ahmad-Nia S, Delavar B, Eini-Zinab H, Kazemipour S, Mehryar AH, Naghavi M. Caesarean section in the Islamic Republic of Iran: Prevalence and some sociodemographic correlates. East Mediterr Health J. 2009;15:1389–98. [PubMed] [Google Scholar]
- 10.Beck CT, Gable RK, Sakala C, Declercq ER. Posttraumatic stress disorder in new mothers: Results from a two-stage U.S. national survey. Birth. 2011;38:216–27. doi: 10.1111/j.1523-536X.2011.00475.x. [DOI] [PubMed] [Google Scholar]
- 11.Lapp LK, Agbokou C, Peretti CS, Ferreri F. Management of post traumatic stress disorder after childbirth: A review. J Psychosom Obstet Gynaecol. 2010;31:113–22. doi: 10.3109/0167482X.2010.503330. [DOI] [PubMed] [Google Scholar]
- 12.Winefield HR, Winefield AH, Tiggemann M. Social support and psychological well-being in young adults: The multi-dimensional support scale. J Pers Assess. 1992;58:198–210. doi: 10.1207/s15327752jpa5801_17. [DOI] [PubMed] [Google Scholar]
- 13.Shaban Z, Dolatian M, Shams J, Alavi-Majd H, Mahmoodi Z, Sajjadi H. Post-traumatic stress disorder (PTSD) following childbirth: Prevalence and contributing factors. Iran Red Crescent Med J. 2013;15:177. doi: 10.5812/ircmj.2312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xie RH, Lei J, Wang S, Xie H, Walker M, Wen SW. Cesarean section and postpartum depression in a cohort of Chinese women with a high cesarean delivery rate. J Womens Health (Larchmt) 2011;20:1881–6. doi: 10.1089/jwh.2011.2842. [DOI] [PubMed] [Google Scholar]
- 15.Söderquist J, Wijma K, Wijma B. Traumatic stress after childbirth: The role of obstetric variables. J Psychosom Obstet Gynaecol. 2002;23:31–9. doi: 10.3109/01674820209093413. [DOI] [PubMed] [Google Scholar]
- 16.Berkman LF. The role of social relations in health promotion. Psychosom Med. 1995;57:245–54. doi: 10.1097/00006842-199505000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Bovier PA, Chamot E, Perneger TV. Perceived stress, internal resources, and social support as determinants of mental health among young adults. Qual Life Res. 2004;13:161–70. doi: 10.1023/B:QURE.0000015288.43768.e4. [DOI] [PubMed] [Google Scholar]
- 18.Spiegel D, Butler LD, Giese-Davis J, Koopman C, Miller E, DiMiceli S, et al. Effects of supportive-expressive group therapy on survival of patients with metastatic breast cancer: A randomized prospective trial. Cancer. 2007;110:1130–8. doi: 10.1002/cncr.22890. [DOI] [PubMed] [Google Scholar]
- 19.Ayers S, Jessop D, Pike A, Parfitt Y, Ford E. The role of adult attachment style, birth intervention and support in posttraumatic stress after childbirth: A prospective study. J Affect Disord. 2014;155:295–8. doi: 10.1016/j.jad.2013.10.022. [DOI] [PubMed] [Google Scholar]
- 20.Mitani S, Fujita M, Nakata K, Shirakawa T. Impact of post-traumatic stress disorder and job-related stress on burnout: A study of fire service workers. J Emerg Med. 2006;31:7–11. doi: 10.1016/j.jemermed.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 21.Garthus-Niegel S, von Soest T, Knoph C, Simonsen TB, Torgersen L, Eberhard-Gran M. The influence of women's preferences and actual mode of delivery on post-traumatic stress symptoms following childbirth: A population-based, longitudinal study. BMC Pregnancy Childbirth. 2014;14:191. doi: 10.1186/1471-2393-14-191. [DOI] [PMC free article] [PubMed] [Google Scholar]


