Abstract
Contact lens-related problems are common and can result in severe sight-threatening complications or contact lens drop out if not addressed properly. We systematically reviewed the most important and the most common contact lens-related complications and their diagnosis, epidemiology, and management according to the literature published in the last 20 years.
Keywords: Complication, Contact Lens, Contact-lens-related Peripheral Ulcer, Discomfort, Giant Papillary Conjunctivitis, Infectious Keratitis, Superior Epithelial Arcuate Lesion
INTRODUCTION
The use of contact lenses is very common,[1,2] and constitutes a profitable industry.[3] The size of the global market of contact lenses is expected to reach 12,476.3 million US dollars by 2020, at a growth rate of 6.7%.[4]
Contact lenses are prescribed for the management of refractive errors that cannot be addressed by spectacles such as aphakia,[5,6,7,8,9,10] keratoconus,[6,7,8,11,12,13,14,15,16,17,18] irregular cornea,[19,20,21,22] and high anisometropia.[6,7,19,20,23] In addition, they can be used for the management of simple refractive errors as alternatives to spectacles. Moreover, contact lenses can be prescribed for the management of dry eye in Stevens-Johnson syndrome[19,23,24,25,26,27] or Sjogren syndrome,[14,27,28,29,30] post refractive surgery rehabilitation,[11,17,21,31,32,33] and persistent epithelial defect.[31,34,35,36] Furthermore, the cosmetic usage of contact lenses is very popular nowadays.[37]
Contact lenses have improved the quality of life not only by correcting refractive errors but also by providing better appearance and less restriction in activities.[38] Unfortunately, contact lenses can cause complications that are disappointing for the patients, forcing them to switch from habitual mode of vision correction to other modalities if possible,[39] which are not always simple or complication-free.
The purpose of this review is to provide a better concept of understanding contact lens-related problems. Addressing contact lens problems properly can prevent contact lens drop-out and lessen the consequences.
METHODS
PubMed and Scopus databases were searched for the related articles published from 1995 to 2015 having the keywords “contact lens” and “discomfort” or “complication” in their title, resulting in 819 articles (after exclusion of duplicated and non-related articles). After reviewing the full texts of the articles, 50 articles were chosen. For completing manuscript to be drafted properly, PubMed and Google Scholar were searched again with more detailed keywords. Finally, 139 articles published between 1982 and 2015 were used for writing this manuscript.
RESULTS
Contact lens-related problems are listed in Table 1. We discuss below the main complications in details.
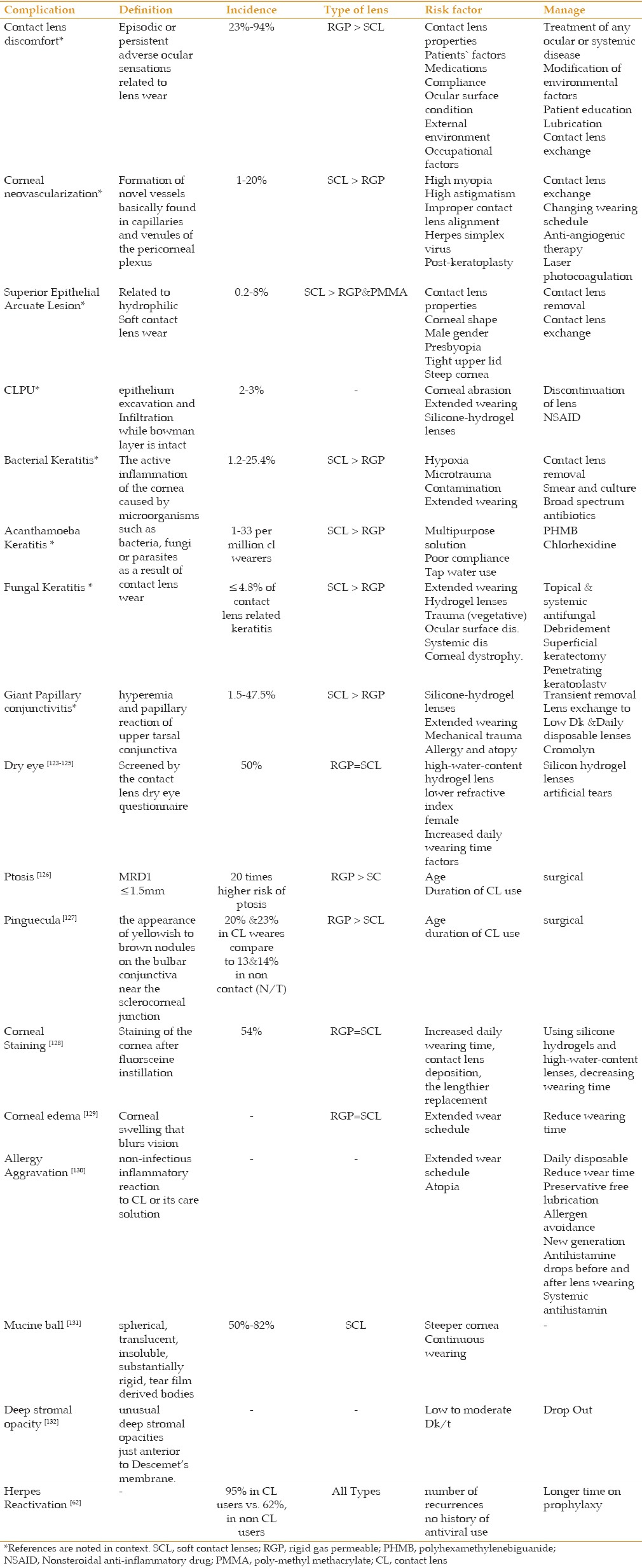
Table 1.
Contact lens-related problems
Contact Lens Discomfort
Definitions
According to the Tear Film & Ocular Surface Society (TFOS), contact lens discomfort is a condition characterized by episodic or persistent adverse ocular sensations related to lens wear, either with or without visual disturbance, resulting from reduced compatibility between the contact lens and the ocular environment. This complication can lead to decreased wearing time or even discontinuation of contact lens wear.[40]
These symptoms should occur after the initial period of adaptation and resolve or diminish with contact lens removal. Moreover, CLD may accompany physical signs such as conjunctival hyperemia or ocular surface staining, or may be diagnosed based only on the patient's subjective report of the discomfort.[40,41]
Epidemiology
The CLD prevalence ranges between 23 and 94% among patients who have symptoms attributable to contact lenses. The burden of the problem seems to be high. This wide range can be due to differences in the assessment tools, severity of the stages assessed, sampling methods, inherent factors of the studied population, and time frame between studies.[42,43,44,45]
Factors causing CLD can be either contact lens-related or environmental. Contact lens-related factors can be associated with (1) material (lubricity, water content), (2) design (edge, base curve, asphericity), (3) fit, (4) wearing schedule, and (5) care system (chemical composition, regimen).
Environmental factors[42,43,44] can be subdivided into (1) ocular surface condition (dry eye, tear composition), (2) external environment (humidity, wind, temperature), (3) occupational factors (computer, light, altitude, and other occupational related changes in the external environment), (4) medications, (5) compliance, and other factors (age, gender, background ocular or systemic diseases, psychiatric and psychological conditions). Out of these, young age, female gender, tear quality and quantity, seasonal allergies, psychological factors, the use of some medications, room humidity, and wind and blink-rate altering activities are clinically related to CLD.[42]
Management
The goal is to provide comfortable daily wearing time that suffices for the patients' desired activities; this varies from patient to patient.
The evaluation of predisposing factors for CLD should preferably be started at the first visit and fit. Therefore, meticulous history taking, slit lamp examination, and tear assessment tests for estimating the risk of CLD are required. Potential conditions that can cause CLD, such as blepharitis, meibomian gland dysfunction, and dry eye, should be addressed before starting contact lens use.
Patients who are inherently or occupationally prone to CLD should be advised to use more eye-friendly contact lenses and lens care systems. CLD can be prevented in these highly susceptible patients by daily wearing schedule, more frequently disposable lenses (preferably daily disposable), hydrogen peroxide based care system being more compliant to lens care, and frequent use of lubricating drops patients.
For symptomatic patients, a thorough history taking may reveal the underlying cause of CLD. History should include the timing and course of the symptoms during the day, lens type, care system, wearing pattern and replacement schedule, compliance behavior, coexisting ocular or systemic diseases including allergy, ocular and systemic medications, and personal and environmental risk factors. Any coexisting ocular and systemic diseases unrelated to contact lens use should be treated appropriately. For example, ocular medicamentosa, which is an ocular irritation caused by chemical toxicity of topically applied eye drops (especially those with preservative) or cosmetics, can be confused with CLD. Conjunctival diseases such as pterygium, pinguecula, and conjunctivochalasis can cause ocular discomfort and are aggravated by contact lens use. Corneal diseases such as Salzmann nodules, corneal dystrophies, and recurrent corneal erosion (due to previous trauma or corneal dystrophies) may cause symptoms that mimic CLD. Careful slit lamp examination can reveal these pathologies. If the patient with these anatomical/pathological conditions wishes to continue wearing contact lenses, these problems should be treated either medically or surgically.
The modifiable environmental factors should be addressed first. Increasing room humidity, avoiding being in the direction of windy air conditioners, intermittently looking at far objects during computer work, and adjusting the angle of gaze at the computer monitor are simple modifications that can help.[46,47]
One of the most frequent background causes of CLD is the patients' non-compliant behavior. Poor compliance with the frequency of contact lens replacement should be addressed by educating the patients and helping them with reminders such as mobile applications.[48] Poor compliance with care system should be addressed by re-educating the patient and emphasizing the effect of lens rubbing. Modifiable environmental and occupational factors should be controlled.[49,50] Using lubricating eye drops can solve the CLD in the mild stages of the problem.[51]
Effective treatments of dry eye diseases with modalities such as punctual plugs have been proposed.[52] Ocular antihistamine drops such as olopatadine and epinastine can decrease CLD symptoms in patients with history of allergic conjunctivitis, even in the absence of symptoms,[52,53] while oral omega-3 fatty acids can decrease dry eye symptoms.[51]
For the patients who remain symptomatic despite the above-mentioned modifications, a trial of changing the lens type to another with a better surface wettability, and more frequent replacement schedule preferably daily disposable can be helpful.[54,55]
Corneal Neovascularization
Definition
Formation of new vessels basically found in capillaries and venules of the pericorneal plexus, which progress to the corneal stroma [Figure 1].
Figure 1.
Corneal neovascularization in a soft contact lens wearer.
Prevalence
It is reported that 10–30% of patients diagnosed with corneal neovascularization wear contact lens,[56,57] while corneal neovascularization develops in 1-20% of contact lens users.[58] Patients who use rigid gas permeable (RGP) or poly-methyl methacrylate (PMMA) lenses have a lower rate of neovascularization.[59] A higher prevalence has been reported in relation to soft contact lenses (SCL), especially in extended wearers.[56,59]
Risk factors
Intrinsic lens parameters including material properties (oxygen transmissibility) have an impact on the development of corneal neovascularization.[60] High myopia and astigmatism can probably influence the peripheral thickness of hydrogel SCL, which decreases peripheral oxygen transmissibility and enhances peripheral mechanical friction. Improper lens-corneal alignment, due to exceedingly flat or steep cornea, can result in peripheral hypoxic or mechanical trauma in SCL wearers.[60,61] As the available base curves for soft contact lenses is limited, the problem of poor lens fittingis not surprising.[60]
Other causes for corneal neovascularization include herpes simplex stromal keratitis and corneal transplantation. Indeed, contact lenses are frequently used to address the refractive errors induced by herpetic corneal scars and are themselves associated with increased prevalence of herpetic attacks;[62] therefore, contact lens practitioners should be aware of recurrent corneal herpetic ulcers and address them promptly. The risk for corneal neovascularization in the post-penetrating keratoplasty status without active inflammation increases in the presence of (1) suture knots in the host stroma, (2) active blepharitis, or (3) a large recipient bed.[63] Therefore, the possible role of the contact lens, especially poor fit, in the development of corneal neovascularization should be considered in these patients.
Management
Exchanging the lens with a more oxygen-permeable contact lens, changing wearing schedule from extended wear to daily wear, switching to RGP lenses instead of soft lenses, and discontinuing contact lenses in cases of active progressive corneal new vessels are recommended.[56,60] Anti-angiogenic therapy of the cornea (subconjunctival or intrastromal), as well as corticosteroids and non-steroidal anti-inflammatory agents, can help in cases with active neovascularizations that may endanger the survival of corneal graft or ocular surface health.[64,65] Laser photocoagulation of new vessels, photodynamic therapy, electrocoagulation, and stem cell transplant are surgical interventions recommended in severe cases.[66,67,68,69,70]
Contact Lens-related Keratitis
Contact lens-related peripheral ulcer
Definition
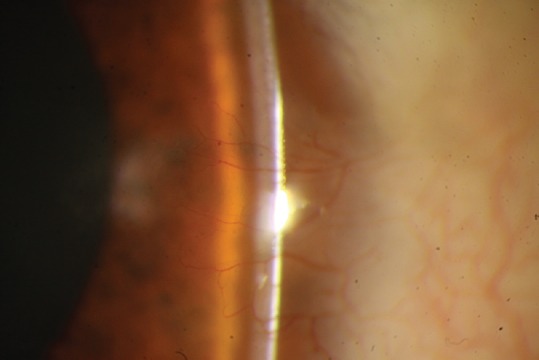
CLPU is characterized by epithelium excavation and infiltration and an intact bowman layer, in contrast to corneal ulcers. Typically, CLPU and corneal ulcers are differentiated by clinical features rather than histological examination. Microbial keratitis is more acute and severe, although overlapped characteristics may cause misdiagnosis. CLPU presents with mild and localized conjunctival injection, and focal infiltration usually less than 1.5 mm, always round or slightly oval in shape, white or white-gray, located at the peripheral cornea. Unlike microbial keratitis,[71,72] CLPU may be devoid of epithelial defects or present with punctuate epithelial erosions [Figure 2].
Figure 2.

Contact lens-related peripheral ulcer.
Cause
In animal models, CLPU is suggested to occur in the presence of live bacteria (e.g., Staphylococcus aureus) and corneal epithelial erosion is necessary. In this theory, bacterial toxins and immunogenic agents that enter via corneal abrasions may cause inflammation, leading to infiltration.[73,74] CLPU is more common in extended wear lenses, and its rate is increased in association with silicone hydrogel lenses.[72]
Incidence
In symptomatic patients, the incidence of CLPU for daily wear silicone hydrogel lenses is 2–3%, while it increases to 2–6% with extended wear schedules. In asymptomatic patients, CLPU incidence in daily wear and extended wear silicone hydrogel lenses is 7–20% and 6–25%, respectively.[75]
Management
Typically, CLPUs regress spontaneously after discontinuation of the contact lens use. Steroid or non-steroidal anti-inflammatory drops are rarely prescribed, in case microbial keratitis is not suspected.[71]
Microbial Keratitis
Definition
Active inflammation of the cornea caused by microorganisms such as bacteria, viruses, or parasites related to contact lens wear, which is its most important risk factor.[76,77]
Causes
Keratitis can occur in case of contact lens induced hypoxia, microtrauma, and contamination of the contact lens or contact lens solution. Direct inoculation of microorganisms into the eye when wearing contact lens with dirty hands can also cause keratitis. The risk can be increased up to 20 times with extended wearing schedules, which increase corneal hypoxia.[78] Mechanical microtrauma to the corneal epithelium, represented by punctuate epithelial erosions, has been associated with silicone hydrogel contact lenses despite their higher oxygen permeability. The broken epithelial barrier can be a serious risk factor for developing infectious keratitis.[79,80]
Management
Infectious keratitis can be effectively prevented by proper lens care. It is the responsibility of contact lens practitioners to educate patients, verify their compliance, and provide them with educational materials. Using opportunities such as weblogs, emails, social networks, and mobile applications for this purpose should be encouraged. If an infectious keratitis occurs despite these measures, it becomes the first priority to (1) eradicate the offensive organism, (2) control the inflammation to prevent disease progression and save the globe and sight, (3) provide appropriate anti-microbial agents, (4) adjust the treatment plan when necessary by closely monitoring the course of the disease, and (5) proceed to surgical interventions if necessary. Situations such as impending corneal perforation, progressing to scleritis or endophthalmitis, which are unresponsive to maximum medical treatments, must be managed surgically.
It should be highlighted that severe cases such as those involving the central part of the cornea, ulcers >3 mm in size, ulcers in immunocompromised patients such as those suffering from diabetes or using corticosteroid or immunosuppressive drugs, one-eyed patients, aggressive progression, resistance to initial treatment, and suspicious fungal or acanthamoebal infections must be referred to an ophthalmologist/ophthalmology hospital expert in managing infectious keratitis.
Bacterial Keratitis
Incidence
The approximate yearly incidence is 2 per 10,000 contact lens wearers, depending on the type of lens and wearing program, with a range between 1.2 (95% coefficient index [CI], 1.1–1.5) for diurnal wear RGP lenses and 25.4 (95% CI, 14.6–29.5) for extended wear of silicon hydrogel lenses.,[76,77] reports from 1999.[81] A confounding factor might be the approval for over-night wearing of the new generations of SCLs, which encourages contact lens wearers to extend the wearing schedule.
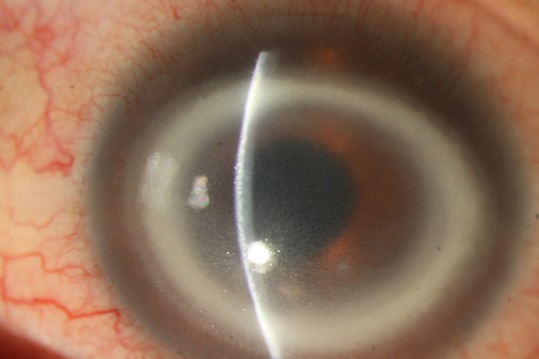
The reports on the most frequent causative organisms are not consistent,[82] although Gram-negative organisms are suggested (>70%, Figure 3).[76,77,79,80,81]
Figure 3.

Bacterial keratitis in a miniscleral lens wearer patient.
Management
The contact lens should be removed in any suspected keratitis. Smear and culture should be provided separately from the infiltration site, contact lens, and lens case. If the clinical picture cannot easily differentiate between fungal and acanthamoeba keratitis, confocal corneal scan should be considered.[83] Broad-spectrum antibiotic therapy should be started to cover all possible Gram-negative and gram-positive microorganisms. Moreover, attention should be paid toward the most possible organisms, based on the smear results and clinical picture. Antibiotics can be adjusted according to the culture and antibiogram results. Monotherapy with topical fluoroquinolones may be sufficient in small peripheral infiltrations. However, more aggressive therapy with fortified topical antibiotics and loading dose with admission or daily follow-ups should be considered in more severe cases. The choice of the antibiotics varies from center to center, based on the microbial resistance pattern, epidemiology of the keratitis, and drug availability.[84]
Acanthamoeba Keratitis
Definition
Protozoal infection of the eye, principally caused by using contaminated contact lenses or lens solutions. Free-living amoebae of the genus Acanthamoeba are the causal agents of this severe sight-threatening infection of the cornea [Figure 4].
Figure 4.
Acanthamoeba keratitis.
Prevalence
In the United States, an estimated 85% of AK cases are related to contact lenses. In developed countries, the incidence of AK is about 1–33 cases per million contact lens wearers.[85] Indeed, almost 80% of AK cases are associated with soft contact lenses. Although only 12% of AK cases have been attributed to RGP lenses, at least a part of this difference might be related to lower prevalence of RGP lens use compared with soft lenses.[86] However, these figures should not encourage RGP wearers to be less obsessed with their lens care.
Risk factors
Contact lens wear is the main risk factor for AK, which should be considered in any suspicious keratitis in contact lens wearers. Patients with AK can presumably experience pain associated with photophobia, ring-like stromal infiltrate, epithelial defect, radial perineuritis, and lid edema.[86] The clinical picture varies at different stages of the disease and the classical ring-shaped infiltration is seen in advanced stages. Diagnosis of AK requires confocal scan of the cornea or special culture and staining techniques. Delayed diagnosis results in deeper invasion, lower response to treatment, and poorer visual outcomes.[87] Usually, singular amoebae gain access to the lens case through tap water or air, swiftly grow to high densities in the lens if the case is not cleaned correctly and regularly, and subsequently attach to the lens and infect the eye. Wearers of SCLs who use multipurpose solutions are at greater risks given that acanthamoeba sticks particularly well to the hydrophilic plastic of these lenses.[86] Additionally, soft lenses are the most commonly used, also by occasional wearers (e.g., once a week for sport) or cosmetic colored lenses for social events. Indeed, these patterns are risk factors for poor compliance to lens care.[88]
For prophylaxis of any kind of infectious keratitis including AK, the use of tap water is forbidden, the lens case should be cleaned with hand rubbing and subsequently air dried, contact lenses should be cleaned and kept by using a proper cleaning method, and the lens cases must be exchanged at least every three months (preferably monthly).[89] Many multipurpose solutions have added anti-acanthamoeba agents such as polyhexamethylenebiguanide (PHMB), though their effectiveness in the clinical setting needs to be documented. The best method of disinfection remains the two-step hydrogen peroxide systems. Moreover, heat disinfection is highly effective in eradication of the acanthamoeba parasite.[90]
Management
In the case of suspicious AK based on the clinical setting, confocal corneal scan and appropriate culture media (e.g., non-nutrient agar with bacterial overlay or buffered charcoal-yeast extract agar) and staining methods (e.g., acridine orange, calcofluor white, or indirect immunofluorescence antibody) are recommended. Currently, AK treatment is based on topical antimicrobial agents that can accomplish high concentrations at the infection site.[89] Considering the presence of a cyst form in acanthamoeba, which is totally resistant to therapy, a combined therapy is advisable.[91,92] Chlorhexidine and PHMB are considered the most effective drugs for treating AK infections; especially when combined, they are effective against both cysts and trophozoites.[86,93] Other medications such as neomycin, paromomycin, voriconazole, miconazole, and imidazoles/triazoles family drugs are also effective against acanthamoeba. Failure to response to medical treatment necessitates surgical interventions such as corneal graft.
Fungal Keratitis
Definition
A sight-threatening complication of contact lenses, characterized by a grayish white infiltration with feathery borders and deep infiltration. Satellite lesions as a hallmark sign may be present, while hypopyon is not uncommon [Figure 5].[94,95] In addition, the diagnosis is confirmed by microbiological tests.
Figure 5.

Fungal keratitis.
Confocal biomicroscopy can be used to distinguish these infections from other causes and to follow the response to treatment.[94,95]
Incidence
In some countries such as India and Nepal, fungal keratitis are the majority of microbial keratitis.[95,96,97] In 21% of the patients with fungal keratitis, contact lens wear has been documented;[98] whereas this rate was reported to be 10% elsewhere.[99] Fungal pathogens have been found in up to 4.8% of contact lens associated keratitis.[98,100] Candida, Fusarium, and Aspergillus are the most commonly isolated organism.[101,102]
A worldwide outbreak of fungal keratitis in 2006 has been associated with the solution, ReNuMoistureLoc.[102] The rate of fusarium keratitis decreased after recall of this product; however, an increased number of contact lens-related fungal keratitis has been reported in 2007 & 2008, as demonstrated in 78 eyes of fungal keratitis collected from 1999 to 2008.[103]
Risk factors
Contact lens wear was the leading risk factor for the fungal keratitis, particularly those caused by yeast-like fungi.[94] Moreover, extended wear schedules increase this risk.[98] Indeed, the risk is highest in extended wear of hydrogel lenses compared with silicone hydrogel, while RGP contact lenses have the lowest risk. Other risk factors include trauma specially with vegetative material, topical steroids and underlying systemic diseases.[97,101]
Management
Topical medications commonly used in fungal keratitis include natamycin (5%), amphotericin B (0.15–0.30%), topical voriconazole (1%), and miconazole (1%).(101) In deep infiltrative cases, a systemic therapy may be added.
In the cases that do not respond or poorly respond to medical therapy and in patients who suffer from severe thinning impending to perforation, surgical interventions are required. Surgical methods range from debridement and superficial keratectomy in small lesions to penetrating keratoplasty in large lesions.[94,104]
Giant Papillary Conjunctivitis
Definition
Giant papillary conjunctivitis, also referred to as contact lens-induced papillary conjunctivitis (CLPC), is one of the most common contact lens-related adverse effects.[105] Patients usually complain of irritation, redness, itching, decreased lens tolerance, excessive lens movements (especially superior displacement), and increased mucous discharge. Hyperemia and papillary reaction larger than 0.3 mm are remarkable in upper tarsal conjunctiva.[106,107,108]
Incidence
A CLPC incidence rate of 1.5%[109] to 47.5%[110] has been reported, with an incidence of 4.6% for wearers of first generation silicone hydrogels.[111] The prevalence of CLPC is higher in patients using silicone hydrogel lenses compared with those wearing hydrogel lenses,[112,113] probably as a consequence of greater mechanical irritation caused by relatively high modulus silicone hydrogel lenses.[114] Moreover, a decrease in CLPC rate has been seen in disposable lens users.[107]
Risk factors
CLPC has been associated with certain lens types and lens materials,[112] and is seen more often with soft contact lenses (85%) compared with rigid contact lenses (15%),[112,115,116,117] Mechanical trauma may play a role in the etiology of this complication.[117] Indeed, a history of allergy and atopy may be present in many cases of CLPC.[106]
Management
It is recommended to consider the possibility of this complication in every visit. Detecting and managing the problem in early stages, even in asymptomatic cases, usually result in the ability to prevent lens drop out. Adherence to lens care recommendations and frequent use of lubricating drops sometimes resolve the problem in its early stages. In both localized and generalized forms of CLPC, it is advisable to discontinue lens wear until signs and symptoms subside, and/or change to a different lens. If symptoms do not resolve, changing to a daily disposable or daily wear schedule can be useful. In the generalized forms, mast cell stabilizers (sodium cromoglycate 2%, ketotifenfumarate 0.05%, levocabastine hydrochloride 0.025%, or olopatadine HCL 0.1%) may be used to manage persistent symptomatic and recurrent events.[106,108,118,119]
Superior Epithelial Arcuate Lesion
Definition
First characterized in the 1970s, SEALs are corneal complications related to SCL wear that have also been known as epithelial splits or superior arcuate keratopathy. The lesions occur in the superior cornea, within about 2 mm of the superior limbus, between the limbus and the contact lens rim. This lesion can be detected via slit lamp examination of the cornea with the eyelid wide open. It is usually a white or opalescent lesion bearing an epithelial defect, which can be confirmed using fluorescein staining. An irregular shaped epithelial defect surrounded by a superficial and punctate staining is characteristic. Moreover, SCL wearers with SEALs are typically asymptomatic, albeit some of them can suffer from a mild foreign body sensation. SEALs normally present within the first 8 weeks of wearing new or replacement lenses. It can occur in high and low water content SCLs, with daily and extended wear schedules.[120,121,122]
Recurrence can occur in newly replaced lenses, both of an identical or new design. SEAL has not been reported in relation to RGP or PMMA lenses. Although silicone hydrogel lenses eliminate contact lens complications related to hypoxia, other physical conditions, such as SEAL and papillary conjunctivitis, still arise. SEALs can happen much later with high DK lenses.[122]
Incidence
The incidence of SEAL in the SCL wearing population is obviously low (0.2–8%). Continuous wear, including high DK/t silicon hydrogel lenses can probably result in higher incidence of SEAL in the contact lens wearing population. The incidence of SEAL has been roughly the same between extended wear conventional hydrogel lenses (0.9–4.0%) and continuous wear with first generation silicone hydrogel lenses (0.2–4.5%).[120,121] Moreover, first generation silicone hydrogel lenses showed a higher incidence of complications than the second generation lenses when they were worn on a daily wear basis. Comparing the results of various studies, the reported incidence of SEALs seems to be greater with extended wear than with daily wear.[121]
Risk factor
The combination of lens design, substance and surface properties, and corneal shape are the major parameters for developing SEAL. Patients' factors include male gender, presbyopia, tight upper lids, and steep cornea. Lens-related contributing factors include lathe cut hydrogel lenses, lenses made of high rigidity or thick materials, monocurve lenses, or plus design lenses.[121]
Management
The patient should stop wearing lenses until resolution of the staining and any infiltration (1–7 days). Subsequently, patients can use the lenses they had been wearing earlier or identical fresh lenses. Nevertheless, if the SEAL recurs, a different lens (in substance and/or design) should be used.[122] All patients should be checked accurately considering the high risk of recurrence and the asymptomatic nature of the lesion. If recurrence occurs after changing lens material or design, soft lenses should be replaced by RGP lenses. Withdrawing contact lens wear temporarily for 1–2 days is normally acceptable for the resolution of the lesion in the majority of cases.[120] In conclusion, according to our review on the most common and/or important contact lens-related complications by referring to their definition, risk factors, prevalence, and management, these complications are the main cause for contact lens withdrawal. Some complications such as infectious keratitis are sight-threatening. Although this complication is not common, its impact makes it a necessity to be considered. Other complications such as discomfort are more common and, although have little to no effect on vision or eye health, should be considered seriously due to their high impact on the contact lens market. Contact lens practitioners must empower themselves by staying updated. 132
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
Acknowledgements
We acknowledge the valuable participation of Dr. Mohammad Soleimani, Assistant Professor at the Emergency Department, Farabi Eye Hospital, who provided the images for fungal and acanthamoebal keratitis from his own archive.
REFERENCES
- 1.Fonn D. Targeting contact lens induced dryness and discomfort: What properties will make lenses more comfortable. Optom Vis Sci. 2007;84:279–285. doi: 10.1097/OPX.0b013e31804636af. [DOI] [PubMed] [Google Scholar]
- 2.Barr J. Annual report. Contact lens spectrum January 2005. 2004 [Google Scholar]
- 3.Nichols JJ. [Last accessed on 2017 Jan 27];Contact lenses 2008, Contact Lens Spectrum. 2009 24:24–32. Available at: www.clspectrum.com/articleViewer.aspx?articleID=102473 . [Google Scholar]
- 4.Contact Lenses Market Size, Share, Industry Report, 2020. Radiant Insights Inc. 2015 [Google Scholar]
- 5.Berkowitsch A. Cosmetic haptic contact lens. J Am Optom Assoc. 1984;55:277–279. [PubMed] [Google Scholar]
- 6.Tan DTH, Pullum KW, Buckley RJ. Medical applications of scleral contact lenses: 2.Gas-permeable scleral contact lenses. Cornea. 1995;14:130–137. [PubMed] [Google Scholar]
- 7.Tan DTH, Pullum KW, Buckley RJ. Medical applications of scleral contact lenses: 1.A retrospective analysis of 343 cases. Cornea. 1995;14:121–129. [PubMed] [Google Scholar]
- 8.Pullum KW, Buckley RJ. A study of 530 patients referred for rigid gas permeable scleral contact lens assessment. Cornea. 1997;16:612–622. [PubMed] [Google Scholar]
- 9.Schein OD, Rosenthal P, Ducharme C. A gas-permeable scleral contact lens for visual rehabilitation. Am J Ophthalmol. 1990;109:318–322. doi: 10.1016/s0002-9394(14)74558-1. [DOI] [PubMed] [Google Scholar]
- 10.Aasuri MK, Venkata N, Preetam P, Rao NT. Management of pediatric aphakia with Silsoft contact lenses. CLAO Journal. 1999;25:209–212. [PubMed] [Google Scholar]
- 11.Baran I, Bradley JA, Alipour F, Rosenthal P, Le H-G, Jacobs DS. PROSE treatment of corneal ectasia. Cont Lens Anterior Eye. 2012;35:222–227. doi: 10.1016/j.clae.2012.04.003. [DOI] [PubMed] [Google Scholar]
- 12.Dalton K, Sorbara L. Fitting an MSD (mini scleral design) rigid contact lens in advanced keratoconus with INTACS. Cont Lens Anterior Eye. 2011;34:274–281. doi: 10.1016/j.clae.2011.05.001. [DOI] [PubMed] [Google Scholar]
- 13.Ortenberg I, Behrman S, Geraisy W, Barequet IS. Wearing time as a measure of success of scleral lenses for patients with irregular astigmatism. Eye Contact Lens. 2013;39:381–384. doi: 10.1097/ICL.0b013e31829e8faa. [DOI] [PubMed] [Google Scholar]
- 14.Visser E-S, Van der Linden BJ, Otten HM, Van der Lelij A, Visser R. Medical applications and outcomes of bitangential scleral lenses. Optom Vis Sci. 2013;90:1078–1085. doi: 10.1097/OPX.0000000000000018. [DOI] [PubMed] [Google Scholar]
- 15.Vreugdenhil W, Geerards AJ, Vervae CJ. A new rigid gas-permeable semi-scleral contact lens for treatment of corneal surface disorders. Cont Lens Anterior Eye. 1998;21:85–88. doi: 10.1016/s1367-0484(98)80028-3. [DOI] [PubMed] [Google Scholar]
- 16.Jagadeesh D, Mahadevan R. Visual performance with changes in eccentricity in PROSE device: A case report. J Optom. 2014;7:108–110. doi: 10.1016/j.optom.2013.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Romero-Jiménez M, Flores-Rodríguez P. Utility of a semi-scleral contact lens design in the management of the irregular cornea. Cont Lens Anterior Eye. 2013;36:146–150. doi: 10.1016/j.clae.2012.12.006. [DOI] [PubMed] [Google Scholar]
- 18.Abdalla YF, Elsahn AF, Hammersmith KM, Cohen EJ. Synergeyes lenses for keratoconus. Cornea. 2010;29:5–8. doi: 10.1097/ICO.0b013e3181a9d090. [DOI] [PubMed] [Google Scholar]
- 19.Arumugam AO, Rajan R, Subramanian M, Mahadevan R. PROSE for irregular corneas at a tertiary eye care center. Eye Contact Lens. 2014;40:71–73. doi: 10.1097/ICL.0000000000000006. [DOI] [PubMed] [Google Scholar]
- 20.Pullum KW, Whiting MA, Buckley RJ. Scleral contact lenses: The expanding role. Cornea. 2005;24:269–277. doi: 10.1097/01.ico.0000148311.94180.6b. [DOI] [PubMed] [Google Scholar]
- 21.Lee JC, Chiu GB, Bach D, Bababeygy SR, Irvine J, Heur M. Functional and visual improvement with prosthetic replacement of the ocular surface ecosystem scleral lenses for irregular corneas. Cornea. 2013;32:1540–1543. doi: 10.1097/ICO.0b013e3182a73802. [DOI] [PubMed] [Google Scholar]
- 22.Alipour F, Jabarvand Behrouz M, Samet B. Mini-scleral lenses in the visual rehabilitation of patients after penetrating keratoplasty and deep lamellar anterior keratoplasty. Cont Lens Anterior Eye. 2015;38:54–58. doi: 10.1016/j.clae.2014.10.001. [DOI] [PubMed] [Google Scholar]
- 23.Foss AJ, Trodd TC, Dart JK. Current indications for scleral contact lenses. CLAO J. 1994;20:115–118. [PubMed] [Google Scholar]
- 24.Rosenthal P, Cotter J. The Boston Scleral Lens in the management of severe ocular surface disease. Ophthalmol Clin North Am. 2003;16:89–93. doi: 10.1016/s0896-1549(02)00067-6. [DOI] [PubMed] [Google Scholar]
- 25.Romero-Rangel T, Stavrou P, Cotter J, Rosenthal P, Baltatzis S, Foster CS. Gas-permeable scleral contact lens therapy in ocular surface disease. Am J Ophthalmol. 2000;130:25–32. doi: 10.1016/s0002-9394(00)00378-0. [DOI] [PubMed] [Google Scholar]
- 26.Tappin MJ, Pullum KW, Buckley RJ. Scleral contact lenses for overnight wear in the management of ocular surface disorders. Eye. 2001;15:168–172. doi: 10.1038/eye.2001.54. [DOI] [PubMed] [Google Scholar]
- 27.Alipour F, Kheirkhah A, Jabarvand Behrouz M. Use of mini scleral contact lenses in moderate to severe dry eye. Cont Lens Anterior Eye. 2012;35:272–276. doi: 10.1016/j.clae.2012.07.006. [DOI] [PubMed] [Google Scholar]
- 28.Rosenthal P, Croteau A. Fluid-ventilated, gas-permeable scleral contact lens is an effective option for managing severe ocular surface disease and many corneal disorders that would otherwise require penetrating keratoplasty. Eye Contact Lens. 2005;31:130–134. doi: 10.1097/01.icl.0000152492.98553.8d. [DOI] [PubMed] [Google Scholar]
- 29.Dimit R, Gire A, Pflugfelder SC, Bergmanson JP. Patient ocular conditions and clinical outcomes using a PROSE scleral device. Cont Lens Anterior Eye. 2013;36:159–163. doi: 10.1016/j.clae.2013.02.004. [DOI] [PubMed] [Google Scholar]
- 30.Pullum K, Buckley R. Therapeutic and ocular surface indications for scleral contact lenses. Ocul Surf. 2007;5:40–49. doi: 10.1016/s1542-0124(12)70051-4. [DOI] [PubMed] [Google Scholar]
- 31.Pecego M, Barnett M, Mannis MJ, Durbin-Johnson B. Jupiter scleral lenses: The UC Davis Eye Center experience. Eye Contact Lens. 2012;38:179–182. doi: 10.1097/ICL.0b013e31824daa5e. [DOI] [PubMed] [Google Scholar]
- 32.Segal O, Barkana Y, Hourovitz D, Behrman S, Kamun Y, Avni I, et al. Scleral contact lenses may help where other modalities fail. Cornea. 2003;22:308–310. doi: 10.1097/00003226-200305000-00006. [DOI] [PubMed] [Google Scholar]
- 33.Ahmed IIK, Breslin CW. Role of the bandage soft contact lens in the postoperative laser in situ keratomileusis patient. J Cataract Refract Surg. 2001;27:1932–1936. doi: 10.1016/s0886-3350(01)01183-x. [DOI] [PubMed] [Google Scholar]
- 34.Lim P, Ridges R, Jacobs DS, Rosenthal P. Treatment of persistent corneal epithelial defect with overnight wear of a prosthetic device for the ocular surface. Am J Ophthalmol. 2013;156:1095–1101. doi: 10.1016/j.ajo.2013.06.006. [DOI] [PubMed] [Google Scholar]
- 35.Ling JD, Gire A, Pflugfelder SC. PROSE therapy used to minimize corneal trauma in patients with corneal epithelial defects. Am J Ophthalmol. 2013;155:615–619. doi: 10.1016/j.ajo.2012.09.033. [DOI] [PubMed] [Google Scholar]
- 36.Ciralsky JB, Chapman KO, Rosenblatt MI, Sood P, Fernandez AGA, Lee MN, et al. Treatment of Refractory persistent corneal epithelial defects: A standardized approach using continuous wear PROSE therapy. Ocul Immunol Inflamm. 2015;23:219–224. doi: 10.3109/09273948.2014.894084. [DOI] [PubMed] [Google Scholar]
- 37.Abdelkader A. Cosmetic soft contact lens associated ulcerative keratitis in Southern Saudi Arabia. Middle East Afr J Ophthalmol. 2014;21:232–235. doi: 10.4103/0974-9233.134677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Porisch E. Football players' contrast sensitivity comparison when wearing amber sport-tinted or clear contact lenses. Optometry. 2007;78:232–235. doi: 10.1016/j.optm.2006.11.014. [DOI] [PubMed] [Google Scholar]
- 39.Walker MK, Bergmanson JP, Miller WL, Marsack JD, Johnson LA. Complications and fitting challenges associated with scleral contact lenses: A review. Cont Lens Anterior Eye. 2016;39:88–96. doi: 10.1016/j.clae.2015.08.003. [DOI] [PubMed] [Google Scholar]
- 40.Nichols KK, Redfern RL, Jacob JT, Nelson JD, Fonn D, Forstot SL, et al. The TFOS International Workshop on Contact Lens Discomfort: Report of the definition and classification subcommittee. Invest Ophthalmol Vis Sci. 2013;54:TFOS14–9. doi: 10.1167/iovs.13-13074. [DOI] [PubMed] [Google Scholar]
- 41.Efron N, Jones L, Bron AJ, Knop E, Arita R, Barabino S, et al. The TFOS International Workshop on Contact Lens Discomfort: Report of the contact lens interactions with the ocular surface and adnexa subcommittee. Invest Ophthalmol Vis Sci. 2013;54:TFOS98–122. doi: 10.1167/iovs.13-13187. [DOI] [PubMed] [Google Scholar]
- 42.Dumbleton K, Caffery B, Dogru M, Hickson-Curran S, Kern J, Kojima T, et al. The TFOS International Workshop on Contact Lens Discomfort: Report of the subcommittee on epidemiology. Invest Ophthalmol Vis Sci. 2013;54:TFOS20–36. doi: 10.1167/iovs.13-13125. [DOI] [PubMed] [Google Scholar]
- 43.McMonnies CW. How contact lens comfort may be influenced by psychiatric and psychological conditions and mechanisms. Clin Exp Optom. 2014;97:308–310. doi: 10.1111/cxo.12122. [DOI] [PubMed] [Google Scholar]
- 44.Su SB, Lu CW, Sheen JW, Kuo SC, Guo HR. Tear secretion dysfunction among women workers engaged in light-on tests in the TFT-LCD industry. BMC Public Health. 2006;6:303. doi: 10.1186/1471-2458-6-303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wolkoff P, Kärcher T, Mayer H. Problems of the “outer eyes” in the office environment: An ergophthalmologic approach. J Occup Environ Med. 2012;54:621–631. doi: 10.1097/JOM.0b013e31824d2e04. [DOI] [PubMed] [Google Scholar]
- 46.González-Méijome JM, Parafita MA, Yebra-Pimentel E, Almeida JB. Symptoms in a population of contact lens and noncontact lens wearers under different environmental conditions. Optom Vis Sci. 2007;84:E296–302. doi: 10.1097/OPX.0b013e318041f77c. [DOI] [PubMed] [Google Scholar]
- 47.Reddy SC, Low C, Lim Y, Low L, Mardina F, Nursaleha M. Computer vision syndrome: A study of knowledge and practices in university students. Nepal J Ophthalmol. 2013;5:161–168. doi: 10.3126/nepjoph.v5i2.8707. [DOI] [PubMed] [Google Scholar]
- 48.Izquierdo JC, Garcia M, Buxo C, Izquierdo N. Factors leading to the Computer Vision Syndrome: An issue at the contemporary workplace. Bol Asoc Med P R. 2003;96:103–110. [PubMed] [Google Scholar]
- 49.Dayer L, Heldenbrand S, Anderson P, Gubbins PO, Martin BC. Smartphone medication adherence apps: Potential benefits to patients and providers. J Am Pharm Assoc. 2013;53:172–181. doi: 10.1331/JAPhA.2013.12202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dumbleton K, Woods C, Jones L, Richter D, Fonn D. Comfort and vision with silicone hydrogel lenses: Effect of compliance. Optom Vis Sci. 2010;87:421–425. doi: 10.1097/OPX.0b013e3181d95aea. [DOI] [PubMed] [Google Scholar]
- 51.Tam NK, Pitt WG, Perez KX, Hickey JW, Glenn AA, Chinn J, et al. Prevention and Removal of Lipid Deposits by Lens Care Solutions and Rubbing. Optom Vis Sci. 2014;91:1430–1439. doi: 10.1097/OPX.0000000000000419. [DOI] [PubMed] [Google Scholar]
- 52.Brodsky M, Berger WE, Butrus S, Epstein AB, Irkec M. Evaluation of comfort using olopatadine hydrochloride 0.1% ophthalmic solution in the treatment of allergic conjunctivitis in contact lens wearers compared to placebo using the conjunctival allergen-challenge model. Eye Contact Lens. 2003;29:113–116. doi: 10.1097/01.ICL.0000063576.32087.F7. [DOI] [PubMed] [Google Scholar]
- 53.Nichols KK, Morris S, Gaddie IB, Evans D. Epinastine 0.05% ophthalmic solution in contact lens-wearing subjects with a history of allergic conjunctivitis. Eye Contact Lens. 2009;35:26–31. doi: 10.1097/ICL.0b013e318193a3df. [DOI] [PubMed] [Google Scholar]
- 54.Hickson-Curran S, Spyridon M, Hunt C, Young G. The use of daily disposable lenses in problematic reusable contact lens wearers. Cont Lens Anterior Eye. 2014;37:285–291. doi: 10.1016/j.clae.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 55.Riley C, Chalmers RL, Pence N. The impact of lens choice in the relief of contact lens related symptoms and ocular surface findings. Cont Lens Anterior Eye. 2005;28:13–19. doi: 10.1016/j.clae.2004.09.002. [DOI] [PubMed] [Google Scholar]
- 56.Abdelfattah NS, Amgad M, Zayed AA, Salem H, Elkhanany AE, Hussein H, et al. Clinical correlates of common corneal neovascular diseases: A literature review. Int J Ophthalmol. 2015;8:182–193. doi: 10.3980/j.issn.2222-3959.2015.01.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Papas E. Corneal vascularisation and contact lenses. Arch Soc Esp Oftalmol. 2006;81:309–312. [PubMed] [Google Scholar]
- 58.Shah SS, Yeung KK, Weissman BA. Contact lens-related deep stromal vascularization. Int Contact Lens Clin. 1998;25:128–136. [Google Scholar]
- 59.Liesegang TJ. Physiologic changes of the cornea with contact lens wear. CLAO J. 2002;28:12–27. [PubMed] [Google Scholar]
- 60.Lee DS, Kim MK, Wee WR. Biometric risk factors for corneal neovascularization associated with hydrogel soft contact lens wear in Korean myopic patients. Korean J Ophthalmol. 2014;28:292–297. doi: 10.3341/kjo.2014.28.4.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Martin R. Corneal conjunctivalisation in long-standing contact lens wearers. Clin Exp Optom. 2007;90:26–30. doi: 10.1111/j.1444-0938.2006.00083.x. [DOI] [PubMed] [Google Scholar]
- 62.Mucci JJ, Utz VM, Galor A, Feuer W, Jeng BH. Recurrence rates of herpes simplex virus keratitis in contact lens and non-contact lens wearers. Eye Contact Lens. 2009;35:185–187. doi: 10.1097/ICL.0b013e3181a9d788. [DOI] [PubMed] [Google Scholar]
- 63.Dana M-R, Schaumberg DA, Kowal VO, Goren MB, Rapuano CJ, Laibson PR, et al. Corneal neovascularization after penetrating keratoplasty. Cornea. 1995;14:604–609. [PubMed] [Google Scholar]
- 64.Hashemian MN, Moghimi S, Kiumehr S, Riazi M, Amoli FA. Prevention and treatment of corneal neovascularization: Comparison of different doses of subconjunctival bevacizumab with corticosteroid in experimental rats. Ophthalmic Res. 2009;42:90–95. doi: 10.1159/000224783. [DOI] [PubMed] [Google Scholar]
- 65.Cursiefen C, Colin J, Dana R, Diaz-Llopis M, Faraj LA, Garcia-Delpech S, et al. Consensus statement on indications for anti-angiogenic therapy in the management of corneal diseases associated with neovascularisation: Outcome of an expert roundtable. Br J Ophthalmol. 2012;96:3–9. doi: 10.1136/bjo.2011.204701. [DOI] [PubMed] [Google Scholar]
- 66.Lim KJ, Wee WR, Lee JH. Treatment of corneal neovascularization with argon laser. Korean J Ophthalmol. 1993;7:25–27. doi: 10.3341/kjo.1993.7.1.25. [DOI] [PubMed] [Google Scholar]
- 67.Al-Torbak AA. Photodynamic therapy with verteporfin for corneal neovascularization. Middle East Afr J Ophthalmology. 2012;19:185–189. doi: 10.4103/0974-9233.95246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hassan AA, Ghoneim DF, El-dib AA, Ahmed SA, Abdel-Salam AM. Photothrombosis of Corneal Neovascularization by Photodynamic Therapy Utilizing Verteporfin and Diode Laser. Jo Lasers Med Sci. 2013;4:131–139. [PMC free article] [PubMed] [Google Scholar]
- 69.Romano V, Spiteri N, Kaye SB. Angiographic-guided treatment of corneal neovascularization. JAMA Ophthalmol. 2015;133:e143544. doi: 10.1001/jamaophthalmol.2014.3544. [DOI] [PubMed] [Google Scholar]
- 70.Koenig Y, Bock F, Kruse FE, Stock K, Cursiefen C. Angioregressive pretreatment of mature corneal blood vessels before keratoplasty: Fine-needle vessel coagulation combined with anti-VEGFs. Cornea. 2012;31:887–892. doi: 10.1097/ICO.0b013e31823f8f7a. [DOI] [PubMed] [Google Scholar]
- 71.Aasuri MK, Venkata N, Kumar VM. Differential diagnosis of microbial keratitis and contact lens-induced peripheral ulcer. Eye Contact Lens. 2003;29:S60–S62. doi: 10.1097/00140068-200301001-00017. [DOI] [PubMed] [Google Scholar]
- 72.Grant T, Chong MS, Vajdic C, Swarbrick HA, Gauthier C, Sweeney DF, et al. Contact lens induced peripheral ulcers during hydrogel contact lens wear. CLAO J. 1998;24:145–151. [PubMed] [Google Scholar]
- 73.Wu P, Stapleton F, Willcox M. The causes of and cures for contact lens-induced peripheral ulcer. Eye Contact Lens. 2003;29:S63–S66. doi: 10.1097/00140068-200301001-00018. [DOI] [PubMed] [Google Scholar]
- 74.Jalbert I, Willcox MD, Sweeney DF. Isolation of Staphylococcus aureus from a contact lens at the time of a contact lens–induced peripheral ulcer: Case report. Cornea. 2000;19:116–120. doi: 10.1097/00003226-200001000-00023. [DOI] [PubMed] [Google Scholar]
- 75.Szczotka-Flynn L, Chalmers R. Incidence and epidemiologic associations of corneal infiltrates with silicone hydrogel contact lenses. Eye Contact Lens. 2013;39:49–52. doi: 10.1097/ICL.0b013e318271d3dc. [DOI] [PubMed] [Google Scholar]
- 76.Schein OD, McNally JJ, Katz J, Chalmers RL, Tielsch JM, Alfonso E, et al. The incidence of microbial keratitis among wearers of a 30-day silicone hydrogel extended-wear contact lens. Ophthalmology. 2005;112:2172–2179. doi: 10.1016/j.ophtha.2005.09.014. [DOI] [PubMed] [Google Scholar]
- 77.Seal D, Kirkness C, Bennett H, Peterson M, Group KS. Population-based cohort study of microbial keratitis in Scotland: Incidence and features. Cont Lens Anterior Eye. 1999;22:49–57. doi: 10.1016/s1367-0484(99)80003-4. [DOI] [PubMed] [Google Scholar]
- 78.Zaidi T, Mowrey-Mckee M, Pier GB. Hypoxia increases corneal cell expression of CFTR leading to increased Pseudomonas aeruginosa binding, internalization, and initiation of inflammation. Invest Ophthalmol Vis Sci. 2004;45:4066–4074. doi: 10.1167/iovs.04-0627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Alarcon I, Tam C, Mun JJ, LeDue J, Evans DJ, Fleiszig SM. Factors impacting corneal epithelial barrier function against Pseudomonas aeruginosa traversal. Invest Ophthalmol Vis Sci. 2011;52:1368–1377. doi: 10.1167/iovs.10-6125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Fleiszig SMJ. The pathogenesis of contact lens-related keratitis. Optom Vis Sci. 2006;83:866–873. doi: 10.1097/01.opx.0000250045.85499.55. [DOI] [PubMed] [Google Scholar]
- 81.Cheng KH, Leung SL, Hoekman HW, Beekhuis WH, Mulder PG, Geerards AJ, et al. Incidence of contact-lens-associated microbial keratitis and its related morbidity. Lancet. 1999;354:181–185. doi: 10.1016/S0140-6736(98)09385-4. [DOI] [PubMed] [Google Scholar]
- 82.Rahimi F, Hashemian MN, Khosravi A, Moradi G, Bamdad S. Bacterial keratitis in a tertiary eye centre in Iran: A retrospective study. Middle East Afr J Ophthalmol. 2015;22:238–244. doi: 10.4103/0974-9233.151870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Narsani AK, Jatoi SM, Khanzada MA, Lohana MK. Etiological diagnosis of microbial keratitis. J Coll Physicians Surg Pak. 2010;20:604–607. [PubMed] [Google Scholar]
- 84.Shah VM, Tandon R, Satpathy G, Nayak N, Chawla B, Agarwal T, et al. Randomized clinical study for comparative evaluation of fourth-generation fluoroquinolones with the combination of fortified antibiotics in the treatment of bacterial corneal ulcers. Cornea. 2010;29:751–757. doi: 10.1097/ICO.0b013e3181ca2ba3. [DOI] [PubMed] [Google Scholar]
- 85.Acanthamoeba Keratitis Fact Sheet [Health Professionals] Atlanta: Centers for Disease Control and Prevention; Available from: http://www.cdc.gov/parasites/acanthamoeba/health_professionals/acanthamoeba_keratitis_hcp.html . [Google Scholar]
- 86.Lorenzo-Morales J, Khan NA, Walochnik J. An update on Acanthamoeba keratitis: Diagnosis, pathogenesis and treatment. Parasite. 2015;22:10. doi: 10.1051/parasite/2015010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Dart JK, Saw VP, Kilvington S. Acanthamoeba keratitis: Diagnosis and treatment update 2009. Am J Ophthalmol. 2009;14:487–499. doi: 10.1016/j.ajo.2009.06.009. [DOI] [PubMed] [Google Scholar]
- 88.Radford C, Minassian D, Dart J. Acanthamoeba keratitis in England and Wales: Incidence, outcome, and risk factors. Br J Ophthalmol. 2002;86:536–542. doi: 10.1136/bjo.86.5.536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Anger C, Lally JM. Acanthamoeba: A review of its potential to cause keratitis, current lens care solution disinfection standards and methodologies, and strategies to reduce patient risk. Eye Contact Lens. 2008;34:247–253. doi: 10.1097/ICL.0b013e31817e7d83. [DOI] [PubMed] [Google Scholar]
- 90.Lim N, Goh D, Bunce C, Xing W, Fraenkel G, Poole TR, et al. Comparison of polyhexamethylene biguanide and chlorhexidine as monotherapy agents in the treatment of Acanthamoeba keratitis. Am J Ophthalmol. 2008;145:130–135. doi: 10.1016/j.ajo.2007.08.040. [DOI] [PubMed] [Google Scholar]
- 91.Coulon C, Collignon A, McDonnell G, Thomas V. Resistance of Acanthamoeba cysts to disinfection treatments used in health care settings. J Clin Microbiol. 2010;48:2689–2697. doi: 10.1128/JCM.00309-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Marciano-Cabral F, Cabral G. Acanthamoeba spp. as agents of disease in humans. Clin Microbiol Rev. 2003;16:273–307. doi: 10.1128/CMR.16.2.273-307.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Ferrari G, Matuska S, Rama P. Double-biguanide therapy for resistant Acanthamoeba keratitis. Case Rep Ophthalmol. 2011;2:338–342. doi: 10.1159/000334270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Thomas P, Kaliamurthy J. Mycotic keratitis: Epidemiology, diagnosis and management. Clin Microbiol Infect. 2013;19:210–220. doi: 10.1111/1469-0691.12126. [DOI] [PubMed] [Google Scholar]
- 95.Ng JK, Fraunfelder FW, Winthrop KL. Review and Update on the Epidemiology, Clinical Presentation, Diagnosis, and Treatment of Fungal Keratitis. Curr Fungal Infect Rep. 2013;7:293–300. [Google Scholar]
- 96.Hagan M, Wright E, Newman M, Dolin P, Johnson G. Causes of suppurative keratitis in Ghana. Br J Ophthalmol. 1995;79:1024–1028. doi: 10.1136/bjo.79.11.1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Gopinathan U, Garg P, Fernandes M, Sharma S, Athmanathan S, Rao GN. The epidemiological features and laboratory results of fungal keratitis: A 10-year review at a referral eye care center in South India. Cornea. 2002;21:555–559. doi: 10.1097/00003226-200208000-00004. [DOI] [PubMed] [Google Scholar]
- 98.Alfonso EC, Miller D, Cantu-Dibildox J, O'Brien TP, Schein OD. Fungal keratitis associated with non-therapeutic soft contact lenses. Am J Ophthalmol. 2006;142:154–155. doi: 10.1016/j.ajo.2006.04.025. [DOI] [PubMed] [Google Scholar]
- 99.Ritterband DC, Seedor JA, Shah MK, Koplin RS, McCormick SA. Fungal keratitis at the New York eye and ear infirmary. Cornea. 2006;25:264–267. doi: 10.1097/01.ico.0000177423.77648.8d. [DOI] [PubMed] [Google Scholar]
- 100.Mah-Sadorra JH, Yavuz SGA, Najjar DM, Laibson PR, Rapuano CJ, Cohen EJ. Trends in contact lens–related corneal ulcers. Cornea. 2005;24:51–58. doi: 10.1097/01.ico.0000138839.29823.57. [DOI] [PubMed] [Google Scholar]
- 101.Srinivasan M. Fungal keratitis. Curr Opin Ophthalmol. 2004;15:321–327. doi: 10.1097/00055735-200408000-00008. [DOI] [PubMed] [Google Scholar]
- 102.Iyer SA, Tuli SS, Wagoner RC. Fungal keratitis: Emerging trends and treatment outcomes. Eye Contact Lens. 2006;32:267–271. doi: 10.1097/01.icl.0000249595.27520.2e. [DOI] [PubMed] [Google Scholar]
- 103.Yildiz EH, Abdalla YF, Elsahn AF, Rapuano CJ, Hammersmith KM, Laibson PR, et al. Update on fungal keratitis from 1999 to 2008. Cornea. 2010;29:1406–1411. doi: 10.1097/ICO.0b013e3181da571b. [DOI] [PubMed] [Google Scholar]
- 104.Thomas PA. Current perspectives on ophthalmic mycoses. Clin Microbiol Rev. 2003;16:730–797. doi: 10.1128/CMR.16.4.730-797.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Skotnitsky CC, Naduvilath TJ, Sweeney DF, Sankaridurg PR. Two presentations of contact lens-induced papillary conjunctivitis (CLPC) in hydrogel lens wear: Local and general. Optom Vis Sci. 2006;83:27–36. doi: 10.1097/01.opx.0000195565.44486.79. [DOI] [PubMed] [Google Scholar]
- 106.Elhers WH, Donshik PC. Giant papillary conjunctivitis. Curr Opin Allergy Clin Immunol. 2008;8:445–449. doi: 10.1097/ACI.0b013e32830e6af0. [DOI] [PubMed] [Google Scholar]
- 107.Porazinski AD, Donshik PC. Giant papillary conjunctivitis in frequent replacement contact lens wearers: A retrospective study. CLAO J. 1999;25:142–147. [PubMed] [Google Scholar]
- 108.Skotnitsky C, Kalliris A, Sankaridurg P, Sweeney D. Contact lens-induced papillary conjunctivitis is either local or general. Clin Exp Optom. 2000;27:193–195. doi: 10.1111/j.1444-0938.2002.tb03034.x. [DOI] [PubMed] [Google Scholar]
- 109.Lamer L. Extended wear contact lenses for myopes: A follow-up study of 400 cases. Ophthalmology. 1983;90:156–161. doi: 10.1016/s0161-6420(83)34584-x. [DOI] [PubMed] [Google Scholar]
- 110.Alemany A, Redal P. Giant papillary conjunctivitis in soft and rigid lens wear. Contactologica. 1991;13:14–17. [Google Scholar]
- 111.Skotnitsky C. Contact lens induced papillary conjunctivitis (CLPC) & high Dk SH lenses. [Last Accessed on 2011 Nov 11]. Available from: http://wwwsiliconehydrogelsorg/editorials/feb_07asp.Feb.2007 .
- 112.Donshik PC. Contact lens chemistry and giant papillary conjunctivitis. Eye Contact Lens. 2003;29:S37–S39. doi: 10.1097/00140068-200301001-00011. [DOI] [PubMed] [Google Scholar]
- 113.Tan ME, Demirci G, Pearce D, Jalbert I, Sankaridurg P, Willcox MD. Lacrimal Gland, Tear Film, and Dry Eye Syndromes 3. Springer; 2002. Contact lens-induced papillary conjunctivitis is associated with increased albumin deposits on extended wear hydrogel lenses; pp. 951–955. [DOI] [PubMed] [Google Scholar]
- 114.Sorbara L, Jones L, Williams-Lyn D. Contact lens induced papillary conjunctivitis with silicone hydrogel lenses. Cont Lens Anterior Eye. 2009;32:93–96. doi: 10.1016/j.clae.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 115.Skotnitsky C, Sankaridurg PR, Sweeney DF, Holden BA. General and local contact lens induced papillary conjunctivitis (CLPC) Clin Exp Optom. 2002;85:193–197. doi: 10.1111/j.1444-0938.2002.tb03034.x. [DOI] [PubMed] [Google Scholar]
- 116.Stern J, Skotnitsky C, O'Hare N, Tan J, Wong R, Sweeney D, et al. Comparison of the incidence of Contact Lens Papillary Conjunctivitis between high Dk soft CLs worn on a 6 and 30 night schedule. Invest Ophthalmol Vis Sci. 2001 [Google Scholar]
- 117.Jones L, Subbaraman L, Rogers R, Dumbleton K. Surface treatment, wetting and modulus of silicone hydrogels. Optician. 2006;232:28–34. [Google Scholar]
- 118.Meisler DM, Berzins UJ, Krachmer JH, Stock EL. Cromolyn treatment of giant papillary conjunctivitis. Arch Ophthalmol. 1982;100:1608–10. doi: 10.1001/archopht.1982.01030040586005. [DOI] [PubMed] [Google Scholar]
- 119.Uchio E. Treatment of allergic conjunctivitis with olopatadine hydrochloride eye drops. Clin Ophthalmol. 2008;2:525–531. doi: 10.2147/opth.s3294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Holden BA, Stephenson A, Stretton S, Sankaridurg PR, O'Hare N, Jalbert I, et al. Superior epithelial arcuate lesions with soft contact lens wear. Optom Vis Sci. 2001;78:9–12. doi: 10.1097/00006324-200101010-00008. [DOI] [PubMed] [Google Scholar]
- 121.Lin MC, Yeh TN. Mechanical complications induced by silicone hydrogel contact lenses. Eye Contact Lens. 2013;39:115–24. doi: 10.1097/ICL.0b013e31827c77fd. [DOI] [PubMed] [Google Scholar]
- 122.Dumbleton K. Noninflammatory silicone hydrogel contact lens complications. Eye Contact Lens. 2003;29:S186–S189. doi: 10.1097/00140068-200301001-00051. [DOI] [PubMed] [Google Scholar]
- 123.Ramamoorthy P, Sinnott LT, Nichols JJ. Treatment, material, care, and patient-related factors in contact lens-related dry eye. Optom Vis Sci. 2008;85:764–772. doi: 10.1097/OPX.0b013e318181a91f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Nichols JJ, Sinnott LT. Tear film, contact lens, and patient-related factors associated with contact lens–related dry eye. Invest Ophthalmol Vis Sci. 2006;47:1319–1328. doi: 10.1167/iovs.05-1392. [DOI] [PubMed] [Google Scholar]
- 125.Nichols JJ, Mitchell GL, Nichols KK, Chalmers R, Begley C. The performance of the contact lens dry eye questionnaire as a screening survey for contact lens-related dry eye. Cornea. 2002;21:469–475. doi: 10.1097/00003226-200207000-00007. [DOI] [PubMed] [Google Scholar]
- 126.Kitazawa T. Hard contact lens wear and the risk of acquired blepharoptosis: A case-control study. Eplasty. 2013;19:e30. [PMC free article] [PubMed] [Google Scholar]
- 127.Mimura T, Usui T, Mori M, Yamamoto H, Obata H, Yamagami S, et al. Pinguecula and contact lenses. Eye. 2010;24:1685–1691. doi: 10.1038/eye.2010.120. [DOI] [PubMed] [Google Scholar]
- 128.Nichols JJ, Sinnott LT. Tear film, contact lens, and patient factors associated with corneal staining. Invest Ophthalmol Vis Sci. 2011;52:1127–1137. doi: 10.1167/iovs.10-5757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Dart J. Disease and risks associated with contact lenses. Br J Ophthalmol. 1993;77:49–53. doi: 10.1136/bjo.77.1.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Urgacz A, Mrukwa E, Gawlik R. Adverse events in allergy sufferers wearing contact lenses. Postepy Dermatol Alergol. 2015;32:204–209. doi: 10.5114/pdia.2015.48071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Szczotka-Flynn L, Benetz BA, Lass J, Albright M, Gillespie B, Kuo J, et al. The association between mucin balls and corneal infiltrative events during extended contact lens wear. Cornea. 2011;30:535–542. doi: 10.1097/ICO.0b013e3181fb8644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Pimenides D, Steele C, McGhee C, Bryce I. Deep corneal stromal opacities associated with long term contact lens wear. Br J Ophthalmol. 1996;80:21–24. doi: 10.1136/bjo.80.1.21. [DOI] [PMC free article] [PubMed] [Google Scholar]


