Abstract
Seminal theories posit that fragmented trauma memories are critical to posttraumatic stress disorder (PTSD; van der Kolk & Fisler, 1995; Brewin, 2014) and that elaboration of the trauma narrative is necessary for recovery (e.g., Foa, Huppert, & Cahill, 2006). According to fragmentation theories, trauma narrative changes, particularly for those receiving trauma-focused treatment, should accompany symptom reduction. Trauma and control narratives in 77 men and women with chronic PTSD were examined pre- and post-treatment, comparing prolonged exposure (PE) and sertraline. Utilizing self-report, rater coding, and objective coding of narrative content, fragmentation was compared across narrative types (trauma, negative, positive) by treatment modality and response, controlling for potential confounds. Although sensory components increased with PE (d = 0.23 – 0.44), there were no consistent differences in fragmentation from pre- to post-treatment between PE and sertraline or treatment responders and non-responders. Contrary to theories, changes in fragmentation may not be a crucial mechanism underlying PTSD therapeutic recovery.
Keywords: PTSD, narrative fragmentation, treatment, memory organization
Seminal theories focus on memory disruptions and information processing deficits as crucial to the development and maintenance of PTSD (e.g., Brewin, 1996, 2001; Brewin, Gregory, Lipton, & Burgess, 2010; Ehlers & Clark, 2000; Horowitz, 1986; van der Kolk, 1987; 2014). Fragmented recall of traumatic events is posited as an important mechanism of PTSD (e.g., Brewin, 1996, 2001; Ehlers & Clark, 2000; van der Kolk, 1994, 2014). In particular, van der Kolk’s psychobiological theory (van der Kolk, 1987, 1994) and Brewin’s dual representation model of PTSD (Brewin 1996, 2001, 2014; Brewin et al., 2010) suggest that trauma memories are uniquely encoded in autobiographical memory, separated from the overall memory network, and difficult to recall verbally. They further suggest that trauma narratives are characterized by sensory aspects, incoherence, and a lack of sequence, collectively referred to as fragmentation. These aspects of memory processing and fragmentation are theorized as integral to the development, maintenance, and remission of PTSD symptoms. Besides being a key theory, the idea that trauma narratives are fragmented and become more organized over the course of treatment is a common clinical assumption that therapists often present as part of the rationale for treatment (e.g., Foa, Hembree, & Rothbaum, 2007). Thus, the construct of trauma narrative fragmentation is integrated into leading theories and common clinical descriptions of the etiology and treatment of PTSD.
Prospective studies show higher fragmentation soon after trauma exposure predicts higher PTSD over time (e.g., Jones, Harvey, & Brewin, 2007; Halligan, Michael, Clark, & Ehlers, 2003; Murray, Ehlers, & Mayou, 2002). However, only four small studies (N = 14 to N = 37) on PTSD (Foa, Molnar, & Cashman, 1995; Kindt, Buck, Arntz, Soeter, 2007; Mundorf & Paivio, 2011; van Minnen, Wessel, Dijkstra, & Roelofs, 2002) and one small study (N = 15) on acute stress disorder (ASD; Moulds & Bryant, 2005) have compared trauma fragmentation pre- to post- treatment, and findings are mixed. In two studies using the same narrative coding measure, some measures of organization such as planning and decision-making (Foa et al., 1995) and disorganized thoughts (van Minnen et al., 2002) improved with treatment and were related to decreased anxiety. However, fragmentation (e.g., unfinished thoughts) either did not change with treatment (Foa et al., 1995) or was unrelated to symptom improvement (van Minnen et al., 2002). Other studies do not show that fragmentation decreases with treatment or is related to changes in PTSD or ASD (Kindt et al., 2007; Moulds & Bryant, 2005), and incoherence, a construct similar to fragmentation, also did not decrease following therapy for childhood abuse (Mundorf & Paivio, 2011). However, these findings are hard to interpret given that studies are limited by reliance on subjective coding, a lack of treatment control groups, and by small sample sizes.
Empirically investigating narrative fragmentation is difficult. Operational definitions vary from self-report (e.g., perception of fragmentation) to narrative coding (e.g., programs that quantify content) and expert ratings (e.g., ratings assigned by trained raters). These are different constructs, as self-report measures assess meta-memory or self-judgment of memory quality, and may be biased by related information and past recall experiences (Schwartz, Benjamin, & Bjork, 1997). In addition, trauma severity (e.g., Bernsten et al., 2003), time since trauma (McNally, 2005), distress (Shobe & Kihlstrom, 1997), cognitive ability (e.g., Gray & Lombardo, 2001), and dissociation (e.g., Brewin, 1996) may be important to narrative quality but are often not examined. Finally, studies often do not include comparisons such as positive or negative narratives, even though they can help control for non-specific effects such as recounting style, emotionality, etc.
Well-controlled empirical research exploring narrative fragmentation changes with treatment are needed. A variety of treatments are considered efficacious for PTSD including cognitive behavioral psychotherapies and selective serotonin reuptake inhibitors (SSRIs; Watts, Schnurr, Mayo, Young-Xu, Weeks, & Friedman, 2013), and both may change fragmentation given their effect on PTSD symptoms. Many effective psychosocial treatments for PTSD use exposure to the trauma memory to improve integration, consolidation, and memory organization. Repeated prolonged exposure to the trauma narrative and other trauma-related reminders is thought to provide corrective information by allowing the patient to emotionally process the memory, alter the underlying fear structure, and reduce PTSD (e.g., Foa & Kozak, 1986; Foa et al., 2007; Foa et al., 2006). SSRIs may promote neurogenesis in the hippocampus and lead to increased hippocampal volume in individuals with PTSD (Bossini et al., 2007; Bremner & Vermetten, 2004; Vermetten, Vythilingam, Southwick, Charney, & Bremner, 2003). Abnormalities of the hippocampus may be related to verbal memory deficits in PTSD (Bremner et al., 2003; Bremner, 2006) and serotonergic agents are related to improved verbal memory in individuals with PTSD and depression (Vermetten et al., 2003; Vythilingam et al., 2004). Thus, both exposure-based and SSRI treatments may improve narrative fragmentation, although the former, which focuses directly on the memory as a target of treatment change may improve fragmentation more so than the latter, which does not focus explicitly on the trauma narrative.
This study examined the role of narrative fragmentation in the treatment of chronic PTSD examining multiple indices of fragmentation: self-report, objective coding, and subjective coding. It further improved upon previous research by using a larger sample than previous studies, comparing across emotional narrative types (i.e., positive, negative), including multiple indices of fragmentation, by controlling for key confounding variables specifically dissociation, cognitive ability, state anxiety, trauma severity, and by comparing a treatment modality that focuses on traumatic narratives (i.e., prolonged exposure [PE]) to one that does not (i.e., sertraline). Thus, the present study was well designed, solidly improving upon previous studies’ methods. Based on theories that exposure treatments facilitate organization of the trauma memory (e.g., Foa et al., 2006), we hypothesized that at post-treatment trauma narratives will be less fragmented for individuals who receive PE than those who receive sertraline. Based on theoretical relationships between fragmentation and PTSD recovery (Brewin, 2013; Ehlers & Clark, 2000; van der Kolk et al., 2001), we further hypothesized that post-treatment fragmentation of the trauma narrative will be lower for treatment responders than for non-responders across fragmentation measures.
Method
Participants
Seventy-seven individuals with chronic PTSD were recruited from a large NIMH-funded multisite randomized controlled trial and signed a separate consent to participate in this study. Participants were between ages 18 and 65 and had a primary diagnosis of current DSM-IV chronic PTSD. Exclusion criteria included: current diagnosis of schizophrenia or delusional disorder, medically unstable bipolar disorder, depression with psychotic features or depression severe enough to require immediate psychiatric treatment (e.g., actively suicidal), severe self-injurious behavior or suicide attempt within the past three months, no clear trauma memory or trauma memory only for an event before age of three years of age (i.e., normal developmental amnesia), diagnosis of alcohol or substance dependence within the previous three months, ongoing intimate relationship with the perpetrator (in assault cases), unwilling or unable to discontinue current psychotherapy or antidepressant medication, adequate trial of either PE (8 sessions or more) or sertraline (150 mg/d; 8 wks), or medical contraindication for sertraline (e.g., pregnancy/likely to become pregnant).
Demographic information is presented for all participants and separately by treatment type in Table 1. Mean age of participants was 37.38 (SD = 11.66). The sample was primarily female (76.6%) and two thirds of participants identified as Caucasian (66.2%).
Table 1.
Demographic information separately by treatment type.
| Full Sample (N = 77) | PE (n = 48) | Sertraline (n = 29) | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| M | SD | M | SD | M | SD | |
|
|
||||||
| Education Level (years) | 14.59 | 3.19 | 15.17a | 3.38 | 13.59b | 2.59 |
| Cognitive Ability (Shipley) | 60.99 | 12.46 | 61.76 | 12.50 | 59.73 | 12.51 |
| Verbal Ability (Shipley) | 31.52 | 5.18 | 31.78 | 5.27 | 31.10 | 5.08 |
| Peritraumatic Dissociation (PDEQ) | 29.04 | 10.99 | 28.77 | 10.74 | 29.49 | 11.56 |
| State Anxiety (STAI-S) | 53.31 | 11.95 | 52.30 | 11.89 | 54.88 | 12.13 |
| Trauma Narr Subjective Distress (SUDs) | 75.15 | 22.39 | 75.04 | 22.99 | 75.35 | 21.72 |
| Trauma Narr State Dissociation (CADSS) | 22.75 | 13.60 | 22.00 | 13.41 | 24.00 | 14.06 |
| Years Since Trauma | 13.22 | 12.99 | 13.32 | 12.80 | 13.05 | 13.52 |
| Trauma Type (%) | ||||||
| Adult Sexual Assault | 27.3 | 27.1 | 27.6 | |||
| Childhood Assault (e.g., CSA) | 40.3 | 31.3 | 24.1 | |||
| Adult Assault (non-sexual) | 18.2 | 29.2 | 31.0 | |||
| Accident (MVA, natural disaster) | 11.7 | 10.4 | 13.8 | |||
| Death/violence to loved one | 2.6 | 2.1 | 3.4 | |||
| % Sustained injury | 40.3 | 41.7 | 41.7 | |||
| % Threat of death/injury | 75.3 | 75.0 | 75.9 | |||
Note. Means in the same row that do not share subscripts differ at a significant level. Shipley = Shipley Institutue of Living Scale; CSA = Childhood Sexual Assault; MVA = Motor Vehicle Accident
Design
Using a mixed subjects design, there were between-subjects factors of treatment type (PE, sertraline) and response (responder, non-responder) and within-subjects factors of narrative type (traumatic, positive, negative) and time (pre, post). Dependent variables were subjective coding, objective coding, and meta-memory of fragmentation. Confounding variables of trauma severity, time since trauma, verbal ability, state distress, and dissociation also were assessed.
Interview and Self-Report Psychopathology Measures
Interview measures
The Posttraumatic Symptom Scale-Interview Version (PSS-I; Foa, Riggs, Dancu, & Rothbaum, 1993) was used to assess DSM-IV diagnosis (APA, 2000) and severity of chronic PTSD. The PSS-I is 17-items with symptoms rated on a 0–3 frequency and intensity scale. The PSS-I has good psychometrics (α = .85; κ = .91 – .97; Foa et al., 1993; Foa & Tolin, 2000). Coding of 10% of cases in the larger clinical trial indicated high interrater reliability for severity (ICC = .99).
The Structured Clinical Interview for the DSM-IV (SCID-IV; First, Spitzer, Gibbon, & Williams, 1994) was used to asssess DSM-IV Axis I disorders, primary diagnosis, eligibility, and comorbidity. The SCID-IV correlates highly with other interviews (Kessler, Berglund, Demler, Jin, & Walters, 2005). In the larger trial, reliability for diagnoses was good, based on 10% of cases (current MDD [κ = .68, ppos = .88, pneg = .80] anxiety [κ = 1.00, ppos = 1.00, pneg = 1.00], substance abuse [ppos = .00, pneg = 1.00], and other diagnoses [ppos = 0.00, pneg = 1.00]).
The Clinical Global Impressions Measure - Improvement (CGI-I) is a one-item rating of global improvement and was used in classification of responder status. The range is 1 (very much improved) to 7 (very much worse), with 3 or less indicating meaningful improvement.
Self-report measures
Measures with established reliability and validity were used to assess psychopathology and potential covariates. The 40-item State Trait Anxiety Inventory (STAI; Speilberger, Gorsuch, & Lushene, 1970) assessed anxiety. The 10-item Peritraumatic Dissociative Experiences Questionnaire (PDEQ; Marmar, Weiss, & Metzler, 1997) assessed self-report dissociation during or immediately after the traumatic event. The PDEQ is strongly associated with PTSD, exposure to stress, and general dissociative tendencies (e.g., Marmar et al., 1997). The 21-item Clinician Administered Dissociative States Scale self-report adaptation (CADSS; Bremner et al., 1998) assessed state dissociation during each narrative recounting. The CADSS correlates modestly with other dissociation measures such as the Dissociative Experiences Scale (.48) and the SCID-D (.42). Subjective Units of Distress (SUDs; Wolpe, 1958) measured participant self-reports of distress after each narrative. SUDs is a numerical rating of current distress level on a 0 to 100 point scale, with 0 being “no anxiety” and 100 being the “most anxious you can imagine”. The Shipley Institute of Living Scale (Shipley, 1967), a 60-item measure, assessed cognitive ability. The Shipley is used commonly as a brief measure of cognitive functioning and correlates highly with more complex measures of cognitive functioning (WAIS correlations .70 to .80; Kaufman, 1990). Trauma severity was assessed with ratings of perceived injury and life threat during the trauma using two dichotomous items (0 no; 1 yes) from the Standardized Trauma Interview (STI; Foa, Rothbaum, Riggs, & Murdock, 1991).
Narratives
Three types of verbal narratives were collected: trauma, positive, and negative.
Criterion A event narrative (Trauma narrative)
The traumatic event narrative was the primary Criterion A event, associated with the current PTSD symptoms and diagnosis, and was the event addressed specifically in PE as the target trauma.
Positive event and negative event narratives
Positive and negative event narratives were included to control for arousal and emotional valence. These comparison narratives were chosen to have occurred within six months before or six months after the trauamtic event to control for effects of time on memory recounting. Positive narratives were events that the participant rated as pleasant experiences. Common examples included weddings, job promotions, etc. Negative narratives were events that participants identified as negative, but not traumatic. Common examples included divorces, death of a loved one, losing a job, etc. All events, traumatic, positive and negative were rated on a 7 point scale for emotional valence with -3 being “very negative”, 0 being “neutral”, and +3 being “very positive”.
As expected, based on ratings of emotionality pre-treatment trauma (M = −2.92, SD = 0.71) narratives differed from negative narratives (M = −2.00, SD = 1.12) and positive narratives (M = 2.59, SD = 0.67), F(2, 132) = 850.30, p < .001, on emotional valence.
Narrative Analysis Measures
Subjective narrative coding
Similar to past studies (e.g., Halligan et al., 2003; Murray et al., 2002), trained coders, blind to study hypotheses, treatment modality, treatment response, and narrative time point, coded narratives on fragmentation indices. Narratives were coded on a scale from 0 (not at all) to 10 (extremely) on eight potential aspects of fragmentation. Sensory components were coded as the amount of detail in the narrative related to sensory experiencing (e.g., saw; loud). Clarity was coded as the overall amount of clear thoughts and ideas (e.g., finished descriptions of events, people, places; explicit where, when, how, why). Coherence was coded as how well concepts hung together logically (e.g., consistencies; continuous; logical). Vividness was coded as the amount of descriptive detail included (e.g., intensity; adjectives; adverbs). Cognitive processing was coded as the amount of content devoted to analyzing meaning (e.g., thinking, processing). Emotional processing was coded as the amount of feeling and emotion (e.g., happy; crying). Fragmentation was a global rating of illogical or unnecessary content (e.g., increased focus on sensory or illogical details, many speech fillers; unnecessary repetitions). Finally, disorganization was a global rating of disjointedness or confusion in the narrative (e.g., lacks a theme or focus; confusion; disjointed ideas). Interrater reliability for 10% of the narratives, across type, was calculated using an intraclass correlation coefficient (ICC). Inter-rater reliability was generally good: sensory = .75; clarity = .47; coherence = .73; vividness = .63; cognitive processing = .94; emotional processing = .86; fragmentation = .63; and disorganization = .70. Given the relatively low reliability for clarity, it was dropped from analyses.
Objective narrative coding
The Linguistic Inquiry and Word Count (LIWC) program (Francis & Pennebaker, 1992) was used to objectively code fragmentation. LIWC quantifies types of words (e.g., pronouns, verbs) and captures 80% of spoken English words (Pennebaker, Francis, & Booth, 2001). Similar to past studies (Alvarez-Conrad, Zoellner, & Foa, 2001) and consistent with our subjective categories, five fragmentation categories were selected a priori: sensory, words that refer actively or descriptively to the five senses; speech fillers, words used out of context that represent decreased clarity (e.g., you know, like); non-fluencies, words that signify a break in the narration and incoherence (e.g. hmm, uhh); cognitive processing, words representing thought or analysis (e.g., because, thinking); and emotional processing, words signifying emotional experiencing (e.g., felt, scared). The number of words for each category were totaled and divided by the total number of words in the narrative to create a percentage.
Meta-memory
The Memory Characteristics Questionnaire (MCQ; Johnson et al., 1988) assessed self-report memory quality using 39-items assessing characteristics such as visual detail, complexity, temporal information, and emotions for a past specific event. Items are rated from 1 (vague, little or none) to 7 (clear/distinct, a lot). Similar to Byrne, Hyman, and Scott (2001), we used items related to fragmentation. Specifically, five questions assessed sensory details of the memory (e.g., my memory for the event involves visual detail….), six assessed vividness (e.g., overall vividness is….), five assessed clarity (e.g., I remember what I thought at the time…), eleven assessed coherence (e.g., my memory for the time when the event takes place is…), and three assessed emotion (e.g., I remember how I felt at the time when the event took place…). Responses were combined to form subscales (sensory, vividness, clarity, coherence, and emotion) of fragmentation. All subscales showed good internal consistency as evidenced by Cronbach’s alpha (clarity = .91, vividness = .82, coherence = .87, and sensory = .73).
PTSD Treatment
Sertraline
Sertraline is a SSRI approved by the Food and Drug Administration (FDA) for treatment of PTSD. Treatment consisted of 10 weekly individual sessions of up to 30 min duration, the first session lasting 45 min, with a board certified psychiatrist to monitor side effects, manage dose, and provide minimal support. Sertraline dose was based on a standardized titration algorithm (Brady et al., 2000), starting at 25mg/day and proceeding up to 200mg/day, if indicated. If participant reported dose-limiting side effects, the maximum dose may not have been achieved. The pharmacotherapist engaged in necessary interpersonal intervention but avoided structured psychotherapeutic interventions deriving from any particular theory. The mean final dose of sertraline was 143.96 (SD = 56.95, Range 25–200).
Prolonged exposure (PE)
Treatment was 10, weekly 90–120 min individual sessions (Foa, Hembree, & Dancu, 2002). Therapists were masters or PhD level, had some cognitive behavioral experience, and were trained in PE prior to treating patients. Therapists received standardized PE training and had ongoing weekly supervision. PE included psychoeducation (Sessions 1–3), graduated in vivo exposure (Sessions 2–10), imaginal revisiting of the trauma memory (Sessions 3–10), and emotional processing (Sessions 3–10). The focus of the imaginal exposure was on an index event and was the same event that was used for fragmentation coding. Narratives used for coding were collected pre- and post-treatment, not during imaginal exposure.
Treatment Adherence
Adherence to sertraline and PE protocols was assessed by outside raters who rated 10% of sessions for essential treatment components and protocol violations. In the larger trial, PE providers completed 90% and sertraline providers completed 96% of essential components. No protocol violations were observed in either treatment. PE sessions were also rated for therapist competence (e.g., interactive with client) on a 3-point scale (1 = Inadequate, 3 = Adequate or Better). Overall PE therapist competence was very good (M = 2.73, SD = 0.32).
Treatment responder/nonresponder status
Treatment response was quantified as a 50% reduction in PTSD on the PSS-I and a CGI-I score of minimally improved or better (rating of 3 or less). The PSS-I definition was based on past studies (e.g., Pauvonic & Ost, 2001). The CGI-I rating allowed for independent evaluator’s judgment and has been used in past studies to classify response (e.g., Brady et al., 2000). This definition was selected a priori, as a conservative classification allowing for adequate sample sizes within responder and non-responder categories.
Procedures
An institutional review board at each site approved the protocol. After informed consent, independent evaluators blinded to treatment assignment assessed demographic information, PTSD (PSS-I), and other DSM-IV diagnoses (SCID-IV). Following an additional seperate consent for this study, each participant met with a research assistant and identified the primary traumatic event and positive and negative comparison narratives and then completed questionnaires (e.g., Shipley). Based on counterbalancing, participants received recounting instructions for their first narrative. Instructions were derived from Foa et al. (1995) to recall narratives as vividly as possible, in the present tense, with as much detail as possible.
Participants narrated the first narrative out loud for 5 min and were queried to continue if they finished before 2 min. After each narrative, participants completed state distress (SUDs), state dissociation (CADSS), and meta-memory (MCQ) measures. This procedure was repeated for the three event narratives based on counterbalancing order (e.g., trauma, positive, negative). Narratives were audiotaped for later transcription and analysis. Participants then completed 10 weeks of treatment, PE or sertraline, dependent on randomization. Participants completed the same procedures approximately two weeks after post-treatment, including both an independent evaluation (PSS-I, CGI) and narrative tasks, and were compensated $20 per hour at both pre- and post-treatment. At the end of their post-treatment session, participants were debriefed.
Data Analytic Strategy
Data analysis used the SuperMix program (Hedeker & Gibbons, 1996) to generate mixed-effects linear regression models nested by subject, with predictors of treatment type, response, time (pre-treatment narrative, post-treatment narrative), controlling for pre-treatment narrative quality for both positive and negative narratives, and dependent variables of post-treatment trauma narrative fragmentation. Random intercept and fixed slope models consistently fit the data the best. Missing data was handled using maximum likelihood estimation. Covariates (PDEQ, Shipley, STAI, SUDs, CADSS) were evaluated; and, when covariates altered the pattern of results, it was noted in the text. Categories indicative of fragmentation were examined: sensory, coherence, clarity, vividness, emotion, and cognition. In each category, relevant subjective coding, objective coding, and meta-memory outcomes were examined. Significance level was adjusted based on the number of dependent variables in each category using a Holmes correction (e.g., Jaccard & Guilamo-Ramos, 2002a, 2002b).
Missing data for self-report (MCQ, covariates) measures at pre-treatment was under 5%. Missing data for narratives (Subjective rater, LIWC coding) at pre-treatment was under 10%. Attrition rates (PE: 29.2%, SER: 27.6%; χ2 (1, 77) = 0.02, p = .88) were similar to other PTSD trials (e.g., Brady et al., 2000; Foa et al., 2005). There were no pre-treatment differences on PTSD severity or narrative fragmentation between completers and non-completers.
Results
Treatment Modality Effects on Fragmentation: PE versus Sertaline
Our first hypothesis examined differences in trauma narrative fragmentation by treatment type (PE vs. sertraline). Models were fit separately for subjectively coded, objectively coded, and meta-memory fragmentation outcomes, with treatment type, time, treatment type and time interactions as predictors. We also included relevant fragmentation scores on negative and positive narratives as predictors to examine effects of general recounting style. Table 2 presents means for trauma fragmentation measures for the whole sample and separately by treatment type.
Table 2.
Pre-post main trauma narrative fragmentation outcomes by treatment type.
| Pre-Treatment | Post-Treatment | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Full (N = 77) | PE (n = 48) | Sertraline (n = 29) | Full (N = 45) | PE (n = 26) | Sertraline (n = 19) | |||||||
|
|
||||||||||||
| M | SD | M | SD | M | SD | M | SD | M | SD | M | SD | |
| Subjective Rater | ||||||||||||
|
| ||||||||||||
| Sensory | 3.67 | 2.31 | 3.64a | 2.45 | 3.71b | 2.11 | 4.47 | 2.50 | 4.75 | 2.61 | 4.05 | 2.34 |
| Coherence | 5.60 | 2.80 | 5.52 | 2.22 | 5.71 | 1.88 | 5.62 | 1.76 | 5.93 | 1.96 | 5.16 | 1.34 |
| Vividness | 4.07 | 2.02 | 4.36 | 2.08 | 3.61 | 1.87 | 4.75 | 1.88 | 5.14 | 1.99 | 4.16 | 1.57 |
| Cognitive Processing | 3.89 | 2.27 | 3.73 | 2.35 | 4.14 | 2.16 | 4.55 | 1.83 | 4.16 | 2.12 | 4.68 | 1.34 |
| Emotional Processing | 3.47 | 2.16 | 3.48 | 2.25 | 3.46 | 2.06 | 3.66 | 2.45 | 3.36 | 2.44 | 4.11 | 2.47 |
| Fragmentation | 4.79 | 1.96 | 4.66 | 1.89 | 5.00 | 2.09 | 5.06 | 2.12 | 4.82 | 2.33 | 5.42 | 1.77 |
| Disorganization | 2.96 | 1.87 | 3.11 | 2.00 | 2.71 | 1.63 | 3.28 | 1.85 | 3.21 | 2.10 | 3.37 | 1.46 |
|
| ||||||||||||
| LIWC Objective Coding | ||||||||||||
|
| ||||||||||||
| Sensory | 2.66 | 1.32 | 2.70 | 1.51 | 2.59 | .97 | 2.94 | 1.56 | 3.31 | 1.83 | 2.39 | .80 |
| Speech Fillers | .77 | .81 | .92a | .90 | .52b | .58 | 1.04 | 1.04 | 1.18 | 1.19 | .83 | .73 |
| Non-fluencies | 2.26 | 1.81 | 2.37 | 1.60 | 2.10 | 2.13 | 2.19 | 2.40 | 1.99 | 1.50 | 2.48 | 3.34 |
| Cognitive Processing | 19.49 | 3.76 | 19.47 | 3.93 | 19.53 | 3.55 | 19.69 | 3.04 | 19.86 | 2.65 | 19.44 | 3.60 |
| Emotional Processing | 2.96 | 1.30 | 2.93 | 1.21 | 3.00 | 1.46 | 3.16 | 1.52 | 3.17 | 1.62 | 3.15 | 1.40 |
|
| ||||||||||||
| Meta-Memory | ||||||||||||
|
| ||||||||||||
| Sensory | 20.67 | 6.23 | 20.96 | 7.05 | 20.18 | 4.60 | 21.43 | 6.88 | 22.64 | 7.28 | 19.52 | 5.87 |
| Vividness | 34.59 | 7.08 | 34.91 | 6.32 | 34.04 | 8.29 | 36.20 | 6.05 | 36.33 | 5.96 | 36.00 | 6.32 |
| Clarity | 27.73a | 6.48 | 27.51 | 6.51 | 28.11 | 6.54 | 29.54b | 6.39 | 29.39 | 6.39 | 29.76 | 6.53 |
| Coherence | 56.05 | 14.24 | 55.17 | 14.21 | 57.54 | 14.42 | 57.72 | 14.63 | 56.70 | 15.56 | 59.33 | 13.23 |
Note. Means in the same row that do not share subscripts differ at a significant level: Subjective Coding sensory: p < .017, LIWC Objective Coding speech fillers: p < .013, Meta-memory clarity p < .013
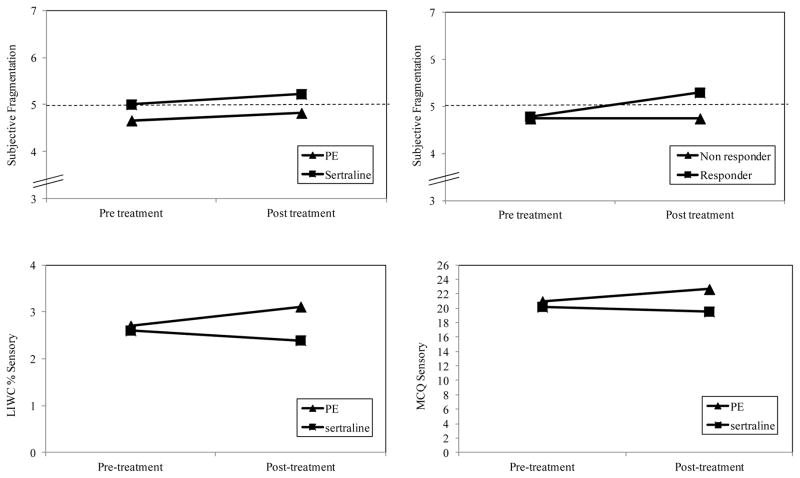
For subjectively coded fragmentation (sensory, coherence, vividness, cognitive processing, fragmentation, disorganization), no treatment, time, or treatment by time interactions were significant. Figure 1 depicts the subjectively coded fragmentation outcome over time by treatment type and depicts a lack of significant change from pre- to post-treatment for both PE and sertraline. As shown in Figure 1, mean scores on fragmentation actually increased, albeit at a non-significant level, from pre to post treatment for both PE (d = .08) and sertraline (d = .22). Consistent with a general recounting style, pre-treatment positive and negative narrative fragmentation indices were associated with the same trauma narrative indices. Subjectively coded fragmentation in negative narratives at pre-treatment predicted higher subjectively coded trauma narrative fragmentation (B = .44, SE = 0.09, z = 4.90, p < .001). When examining pre-treatment positive narratives, coded coherence (B = .35, SE = 0.10, z = 3.38, p < .001), vividness (B = .30, SE = 0.08, z = 4.03, p < .001), and fragmentation (B = .25, SE = 0.09, z = 2.65, p = .004) predicted the same indices in trauma narratives.
Figure 1.
Minimal pre to post changes in fragmentation for PE and sertraline (1a), an increase in subjectively coded fragmentation from pre to post treatment for treatment responders (1b), and an increase in both objectively coded (1c) and self-reported sensory components (1d) from pre to post treatment for PE compared to sertraline.
Note. For subjective fragmentation graphs (1a and 1b) Y axis has been condensed to 3–7. The horizontal line at 5 on the Y axis, indicates neutral ratings of fragmentation.
For objectively coded fragmentation (LIWC: speech fillers, non-fluencies, cognitive, emotional processing), there were no significant treatment, time, or treatment by time interaction effects. There was a treatment x time interaction for coded sensory aspects (LICW; B = 0.71, SE = 0.33, z = 2.14, p = 0.03) that was in the opposite direction than what was hypothesized, with PE showing an increase from pre- to post-treatment (d = .36) and those in sertraline showing a slight decrease (d = .22), depicted in Figure 1. Similarly, consistent with a general recounting style above, pre-treatment negative and positive narratives predicted trauma fragmentation. Pre-treatment indices in negative narratives predicted the same indices for trauma narratives, higher coded affect (B = .33, SE = 0.08, z = 4.12, p < .001), sensory aspects (B = .28, SE = 0.12, z = 2.45, p = .03), cognitive mechanisms (B = .34, SE = 0.08, z = 4.02, p < .001), speech fillers (B = .32, SE = 0.10, z = 3.10, p < .001), and non-fluencies (B = .39, SE = 0.09, z = 4.27, p < .001). Pre-treatment positive indices predicted the same indices of speech fillers (B = .34, SE = 0.10, z = 2.96, p < .001) and non-fluencies (B = .45, SE = 0.08, z = 5.31, p < .001) in trauma narratives.
Finally, for meta-memory (MCQ: sensory, vividness, clarity, coherence, emotion), similarly, with the exception of sensory components, there were no treatment, time, or treatment by time interactions. Similar to objectively coded sensory components, there was a significant treatment by time interaction for self-reported sensory aspects (B = 3.83, SE = 1.55, z = 2.47, p = 0.01) opposite to hypotheses, with those in PE reporting an increase in sensory components from pre- to post treatment (d = .23) and those in sertraline reporting a slight decrease (d = .13), depicted in Figure 1. Pre-treatment negative narrative indices did not significantly predict any meta-memory outcomes, but positive narrative indices predicted several meta-memory outcomes for the trauma narrative, including higher self-reported coherence (B = .46, SE = 0.08, z = 5.60, p < .001), sensory (B = .37, SE = 0.07, z = 5.05, p < .001), and vividness (B = .31, SE = 0.07, z = 4.18, p < .001).
Overall, from pre- to post-treatment the vast majority of fragmentation indices did not change significantly, and neither PE nor sertraline predicted change in trauma fragmentation, with the exception of sensory components, which increased particularly for individuals receiving PE. As can be seen in Figure 1 and Table 2, many of the outcomes showed means that changed in the opposite to hypothesized direction with treatment (i.e., subjective sensory, vividness, fragmentation, disorganization; objective sensory, speech fillers; meta-memory sensory, vividness). Pre-treatment positive and negative narrative fragmentation predicted trauma narrative fragmentation, suggesting that general recounting style is a stronger predictor of trauma fragmentation across subjective, objective, and meta-memory outcomes than treatment modality.
Treatment Response versus Non-Response Effects on Fragmentation
Our second hypothesis examined fragmentation and treatment response. We examined effects of treatment response, time, and treatment response by time interactions. Table 3 presents means and standard deviations by response. Similar to treatment type, we included pre-treatment negative and positive fragmentation as a predictor of trauma fragmentation.
Table 3.
Pre-post main trauma narrative fragmentation outcomes by treatment response.
| Pre-Treatment | Post-Treatment | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Responder (n = 36) | Non-Responder (n = 27) | Responder (n = 28) | Non-Responder (n = 19) | |||||
|
|
||||||||
| M | SD | M | SD | M | SD | M | SD | |
| Subjective Rater | ||||||||
|
| ||||||||
| Sensory | 3.58 | 2.21 | 4.07 | 2.16 | 4.36 | 2.57 | 4.63 | 2.45 |
| Coherence | 5.50 | 2.20 | 5.44 | 1.97 | 5.39 | 1.59 | 5.95 | 1.99 |
| Vividness | 4.00 | 2.07 | 4.19 | 1.82 | 4.71 | 1.96 | 4.79 | 1.81 |
| Cognitive Processing | 3.83 | 2.38 | 3.93 | 2.13 | 4.46 | 1.84 | 4.68 | 1.86 |
| Emotional Processing | 3.72 | 2.08 | 3.00 | 2.08 | 3.46 | 2.50 | 3.95 | 2.41 |
| Fragmentation | 4.78 | 2.29 | 4.74 | 1.63 | 5.29 | 2.03 | 4.74 | 2.26 |
| Disorganization | 3.11 | 2.11 | 3.00 | 1.66 | 3.50 | 1.80 | 2.95 | 1.93 |
|
| ||||||||
| LIWC Objective Coding | ||||||||
|
| ||||||||
| Sensory | 2.61 | 1.43 | 2.82 | 1.31 | 2.99 | 1.46 | 2.87 | 1.74 |
| Speech Fillers | .82 | 1.00 | .68 | .53 | .94 | .87 | 1.19 | 1.26 |
| Non-fluencies | 2.39 | 1.75 | 1.73 | 1.46 | 2.52 | 2.82 | 1.69 | 1.52 |
| Cognitive Processing | 19.52 | 4.26 | 19.43 | 3.19 | 19.59 | 2.94 | 19.84 | 3.25 |
| Emotional Processing | 3.01 | 1.41 | 3.00 | 1.21 | 3.12 | 1.55 | 3.23 | 3.25 |
|
| ||||||||
| Meta-Memory | ||||||||
|
| ||||||||
| Sensory | 20.46 | 6.04 | 21.43 | 6.92 | 21.78 | 6.57 | 20.91 | 7.43 |
| Vividness | 34.51 | 7.26 | 35.78 | 6.11 | 36.16 | 6.04 | 36.27 | 6.20 |
| Clarity | 26.84 | 7.02 | 29.39 | 5.53 | 28.97 | 6.62 | 30.36 | 6.08 |
| Coherence | 55.14 | 13.15 | 58.39 | 14.62 | 56.50 | 14.93 | 59.50 | 14.33 |
Note. Means in the same row that do not share subscripts differ at a significant level
For the subjective coding indices, neither treatment response, time, nor response by time interactions were significant. Figure 1 shows a lack of significant change for subjectively rated fragmentation from pre- to post-treatment for both treatment responders and non-responders, and a lack of significant group differences by response. As can be seen in Figure 1, subjectively coded fragmentation actually increased with treatment for responders (d = .28) and remained unchanged for non-responders (d = .00), although at a non-significant level, opposite to hypotheses. Pre-treatment fragmentation in comparison narratives predicted corresponding indices in trauma narratives. In negative narratives, higher subjectively coded fragmentation (B = .44, SE = 0.09, z = 4.64, p < .001) predicted fragmentation of trauma narratives, and pre-treatment indices in positive narratives predicted higher coherence (B = .39, SE = 0.10, z = 3.84, p < .001), vividness (B = .38, SE = 0.09, z = 4.47, p < .001), and fragmentation (B = .26, SE = 0.09, z = 2.72, p = .006) of the trauma narrative.
For LIWC coding, there were no significant differences for treatment response, time, or treatment response by time interactions. Pre-treatment negative narrative indices predicted higher LIWC coded affect (B = .33, SE = 0.08, z = 4.18, p < .001), cognitions (B = .34, SE = 0.09, z = 3.91, p < .001), non fluencies (B = .38, SE = 0.09, z = 4.16, p < .001), and speech fillers (B = .32, SE = 0.10, z = 3.16, p = .001) in the trauma narrative. Pre-treatment positive narrative fragmentation predicted the same indices of higher non-fluencies (B = .45, SE = 0.08, z = 5.31, p < .001) and speech fillers (B = .33, SE = 0.11, z = 2.94, p = .003) in the trauma narrative.
For meta-memory, there were no significant differences for treatment response, time, or treatment response by time interactions, except for meta-memory clarity. For clarity, there was a main effect of response (B = −3.24, SE = 1.51, z = −2.14, p = .03), which was modified by a trend toward a treatment response by time interaction (B = 1.97, SE = 1.04, z = 1.90, p = .06), with responders reporting less clarity collapsed over time but reporting more increased clarity from pre- to post treatment (d = .31) than non-responders (d = .17).1 Pre-treatment negative narrative indices predicted higher vividness (B = .27, SE = 0.08, z = 3.51, p < .001), coherence (B = .39, SE = 0.08, z = 4.69, p < .001), and sensory (B = .33, SE = 0.08, z = 4.12, p < .001) aspects in the trauma narrative.
Across multiple indices of fragmentation, fragmentation or changes in fragmentation were not strongly associated with treatment response. As shown in Figure 1 and Table 3, an opposite to predicted pattern emerged in which responders showed a general trend for many fragmentation indices to go in the opposite to predicted direction such as an increase in subjectively coded sensory aspects, vividness, fragmentation, and disorganization and a decrease in subjectively coded coherence following treatment. General recounting style, as measured in associations with pre-treatment negative and positive control narratives, was consistently associated with fragmentation in trauma narratives more consistently than response to treatment.
Discussion
The present study explored the influential theory and common clinical assumption that changes in trauma narrative fragmentation is a key mechanism in reduction of PTSD symptoms (e.g., Brewin, 2013; van der Kolk, 1987; 2014). The findings do not suggest that changes in fragmentation are crucial to recovery, and thus have important implications for conceptualizing etiology and treatment of PTSD. Across subjectively coded, objectively coded, and meta-memory indices, fragmentation did not reliably change from pre- to post-treatment. Notably, neither treatment type, comparing PE and sertraline, nor treatment response, comparing those who recovered versus those who did not, were associated with changes in trauma narrative fragmentation. When we did observe differences means often went in the opposite to predicted direction. Specifically, we observed an increase rather than a decrease in key outcomes of subjectively coded sensory aspects, fragmentation and disorganization, objectively coded sensory aspects and speech fillers, and meta-memory sensory and vividness self-report ratings. Finally, pre-treatment fragmentation in non-trauma narratives, specifically the negative and positive narratives, predicted trauma narrative fragmentation, highlighting the importance of a general recounting style rather than specificity of the trauma narrative in terms of fragmentation.
To our knowledge this is the first study to investigate narrative changes in regard to pharmacotherapy for PTSD and to compare psychotherapy and pharmacotherapy on narrative indices. Given the focus on revisiting the memory in PE, it is notable that differential treatment effects were not observed and suggests that changes in fragmentation may not be crucial to recovery. In PE, it is often thought that increased narrative organization is a possible explanation for treatment efficacy (e.g., Foa & Riggs, 1993; Foa et al., 2006). Similarly, SSRIs might impact PTSD by improving verbal memory (e.g., Vythilingam et al., 2004). Despite these theories, results of this study suggest that for both PE and sertraline, if treatment is impacting the recounting of the trauma narrative it is not being captured by these measures of fragmentation.
The only consistent and significant difference to emerge was an increase in subjectively coded and meta-memory reported sensory details from pre- to post-treatment, with a greater increase for PE than for sertraline. Theories of fragmentation and perceptual processing (e.g., Brewin, 2013; van der Kolk, 2014) suggest that trauma narratives become less sensory focused with recovery. Indeed, it is theorized that PTSD re-experiencing symptoms result from unintegrated, sensory dominated trauma memories (Brewin & Holmes, 2003; Brewin et al., 2010; Brewin, 2014). The present findings are inconsistent with this aspect of these theories. However, it is also possible that with treatment individuals convert sensory dominated details to details that are more verbally accessible (Brewin et al., 2010). Another explanation is that in PE the therapist prompts for more sensory details during the repeated revisiting of the narrative (e.g., Foa et al., 2007). Thus, the change in sensory components following PE may be a “side effect” of the treatment approach and of imaginal exposure specifically decreasing avoidance of the memory.
A second focus of this study was to investigate the relationship between recovery and changes in fragmentation. The present findings are not consistent with theories that improvement in PTSD symptoms are caused by changes in fragmentation and organization (Brewin, 1996; Ehlers & Clark, 2000; Foa & Riggs, 1993; van der Kolk et al., 2001). Instead, across multiple measures of fragmentation, responder status consistently did not predict fragmentation. This finding builds on previous findings (Foa et al., 1995; Kindt et al., 2007; Moulds & Bryant, 2005; van Minnen et al., 2002) by showing a failure to consistently find changes in memory quality to be related to PTSD recovery.
So the question remains, if it is not memory fragmentation that is related to PTSD recovery, then what is the relationship between the trauma memory and successful recovery from PTSD? Prominent cognitive theories have shifted the emphasis from fragmentation to the meaning associated with the trauma memory as crucial to psychotherapeutic recovery (e.g., Ehlers & Clark, 2000; Ehlers et al., 2005; Ehlers et al., 2004). Changes in trauma-related beliefs precede changes in PTSD during PE and cognitive therapies, suggesting the importance of changes in meaning to recovery (e.g., Kleim et al., 2013; McLean, Yeh, Rosenfield, & Foa, 2015; Zalta et al., 2014). These conceptual changes may not have been captured by the narrative measures of perceptual aspects and memory quality included in this study. Notably, a recent study (Jaeger, Lindblom, Parker-Guilbert, & Zoellner, 2014) found that content indices in the trauma narrative (e.g., emotion, cognitive words) were more strongly predictive of PTSD than narrative structure, lending further support to the notion that narrative meaning is more related to PTSD than narrative quality per se. Related theories posit that the importance of the trauma narrative in PTSD recovery is to facilitate inhibitory learning by providing corrective learning (e.g., Craske et al., 2008; Foa & Kozak, 1986). Indeed, enhancing the inhibitory control of the medial prefontal cortex is implicated in both the extinction processes inherent in PE (e.g., Quirk, Garcia, & González-Lima, 2006) and in SSRI treatment (e.g., Sachinvala, Kling, Suffin, Lake, & Cohen, 2000). Changes in narrative quality may be less crucial than changes in the individual’s emotional experiencing in response to the narrative, and changes in fragmentation may not be necessary for increased emotional processing and extinction.
Pre-treatment fragmentation in negative and positive narratives predicted trauma narrative fragmentation, even when treatment type and response did not. This highlights the important role of recounting style on traumatic event recall. Past studies looking at subjectively coded (Jelinek et al., 2009) and meta-memory fragmentation (Halligan et al., 2003) show trauma narratives to be more fragmented than comparison narratives in individuals with PTSD, although several studies on meta-memory fragmentation have not replicated this difference (Rubin et al., 2004; Rubin, 2011; Rubin, Boal, & Bernsten, 2008). To our knowledge, this is the first study to look at fragmentation in comparison narratives as a predictor of narrative quality pre and post PTSD treatment and suggests that trauma narratives are not recalled in a unique manner. Indeed, narrative recounting style may reflect a general tendency of how an individual integrates autobiographical information, potentially reflecting a general rather than specific vulnerability factor in PTSD. Accordingly, past studies that have not controlled for narrative type may be missing a key explanatory factor in understanding narrative quality.
In many respects, the present study represents a definitive study design to examine the role of narrative fragmentation on therapeutic recovery. Namely, all participants had chronic PTSD and received either a psychotherapy directly targeting the trauma narrative or a pharmacotherapy that did not address the trauma narrative. Assessment of narratives was entirely separate from therapeutic procedures, multiple indices of fragmentation via patient report, objective coding, and rater coding were obtained, and control narratives were included. Nevertheless, the next generation of research examining trauma memory processing, trauma-related psychopathology, and targeted interventions, needs to better bridge the gap between experimental analogue studies and real-world clinical interventions. Analogue studies suffer from artificially constructed observed, rather than experienced, analogue events (e.g., series of distressing video clips, still images); whereas clinical studies utilize retrospective memory for a previously experienced trauma, without any control of the nature of the event or the processing of the event. Bridge studies need to control or manipulate encoding of the event while maintaining generalizability to life-threatening traumatic events. One way to do this is to conduct studies wherein participants are exposed to an event that contains key salient aspects of traumatic events, such as active participation, personal relevance or meaning, uncontrollability, and sense of impending life threat or danger, actual threat, and termination of threat; elements that are absent from lower intensity analogue stimuli. Importantly, with controlled event-like exposure, salient aspects of the events could be manipulated such as factors that influence memory encoding and retrieval such as duration, proximity, and chronicity. Memory processes could be assessed or even manipulated prior, during, immediately after, and crucially over days, weeks, and months following the event. These designs require much more in-depth preparation and likely collaboration with established entities or programs. Within the military context, survival, evasion, resistance, and escape (SERE) training required for personnel considered at high risk of capture is one such example. The training is highly controlled and standardized but also sufficiently personal and “traumatic.” Other more “real life” events, such as common scary environments (e.g., haunted houses), could also be used for experimental manipulation designs.
These “bridge” designs need to build on previous analogue and real world findings. Given our findings that properties of control narratives were associated trauma narrative properties, a stronger emphasis on individual differences in general, rather than trauma-specific, recounting or memory processing style merit attention. Ideally, bridge studies would include control events (e.g., positive autobiographical events), similar to what was included in this study. The examination of individual differences dovetails with existing research highlighting the role of processes such as reduced autobiographical memory specificity (e.g., Bryant, Sutherland, & Guthrie, 2007; Kleim & Ehlers, 2008; Moore & Zoellner, 2007) and data-driven processing (Halligan et al., 2002; Regambal & Alden, 2009). The ultimate design needed to isolate fragmentation as a unique mechanism for the development and therapeutic recovery of PTSD would generate narratives that were and were not fragmented, link this fragmentation to persistent PTSD-like symptoms, and then systematically reduce fragmentation, showing that this reduced fragmentation is related to a reduction in PTSD-like symptoms. In summary, bridge designs would help identify whether these memory processes represent a true causal factor or merely an associated feature, separating whether it represents a pre-existing vulnerability or risk, consequence of trauma exposure, consequence of persistent psychopathology, or epiphenomenon (e.g., third variable not causally related) and would provide a benchmark for translational science to compare across findings from experimental and real world designs.
This study is unique in that it included measurements focused on narrative content (e.g., LIWC objective coding), recounting style (e.g., subjective coding), and self-perception of the narrative (e.g., self-report). Further, it compared a narrative-focused treatment (PE) to a non-narrative focused treatment (sertraline) and treatment response to non-response. If indeed, fragmentation is a crucial mechanism of recovery, then we might expect it to be ubiquitous and to emerge as an important predictor no matter how we define the construct. Critically, this study did not show consistent differences across multiple assessment indices. Yet, there are several limitations. Narrative recounting per event was brief. Accordingly, it may have altered the portions of the story that were included, although it also allowed for consistency across retellings. We time-matched comparison narratives to traumatic events to control for the effects of time on recall, which may have influenced the salience of the comparison events. However, we observed high ratings of emotional valence for all narrative types, suggesting that memories were emotionally salient. This study included an active control condition (i.e., sertraline) due to our focus on examining the effects of treatment and recovery on fragmentation, and we only looked at changes during active treatment. Narrative changes may continue after treatment, as individuals continue to process the memory and reduce trauma-related anxiety. In addition, although our sample is larger than previous studies and we were powered to detect medium-to-large effects, the key findings with implications for theory development in this study were null. Notably, fragmentation indices often went opposite of prediction, increasing rather than decreasing over time, and, accordingly, increasing our sample size would not increase the likelihood of finding a significant effect. Further, a significant increase in sensory details was detected for PE, arguing against lack of follow-up time points, other control conditions, or a larger sample altering findings.
In summary, fragmentation is poorly understood despite theories on its clinical and theoretical importance to PTSD (e.g., Brewin, 2013; van der Kolk, 2014). Our findings were inconsistent with hypotheses that narrative-focused therapy would lead to greater fragmentation decreases than pharmacotherapy and that treatment responders would show greater decreases in fragmentation than non-responders. Accordingly, fragmentation may not be a crucial mechanism in PTSD treatment and other explanations of change, such as those emphasizing meaning and new learning, should be emphasized.
Acknowledgments
This research was funded in part by grants from the National Institute of Mental Health F31 MH74225 (PI: Bedard), R01 MH066347 (PI: Zoellner), and R01 MH066348 (PI: Feeny). NIMH had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Footnotes
This analysis was also run controlling for the effect of peritraumatic dissociation (PDEQ), as scores on the PDEQ were significantly associated with meta-memory clarity ratings. When controlling for the PDEQ, the main effect of treatment response was significant only at the trend level (B = −2.43, SE = 1.35, z = −1.80, p = 0.07) as was the interaction of treatment response and time (B = 1.75, SE = 1.02, z = 1.71, p = 0.09).
Author Contributions
M.B.G. and L.Z. were responsible for developing the study idea and design. Data collection was performed by M.B.G., L.Z., and N.C.F. Data analysis and interpretation were performed by M.B.G. with input from L.Z. The full manuscript was drafted by M.B.G. and critical revisions were provided by L.Z. and N.C.F. All authors approved the final version of the paper for submission.
Contributor Information
Michele Bedard-Gilligan, University of Washington.
Lori A. Zoellner, University of Washington
Norah C. Feeny, Case Western Reserve University
References
- Alvarez-Conrad J, Zoellner LA, Foa EB. Linguistic predictors of trauma pathology and physical health. Applied Cognitive Psychology. 2001;15:S159–S170. doi: 10.1002/acp.839. [DOI] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, D.C: American Psychiatric Press; 2000. Text Revision. [Google Scholar]
- Bernsten D, Willert M, Rubin D. Splintered memories or vivid landmarks? Qualities and organization of traumatic memories with and without PTSD. Applied Cognitive Psychology. 2003;17:675–693. doi: 10.1002/acp.894. [DOI] [Google Scholar]
- Bossini L, Tavanti M, Lombardelli A, Calossi S, Riccardo Polizzotto N, Galli R, Vatti G, Pieraccini F, Castrofiovanni P. Changes in hippocampal volume in patients with post-traumatic stress disorder after sertraline treatment. Journal of Clinical Psychopharmacology. 2007;27:233–235. doi: 10.1097/01.jcp.0000264979.09862.a8. [DOI] [PubMed] [Google Scholar]
- Brady K, Pearlstein T, Asnis GM, Baker D, Rothbaum B, … Farfel GM. Efficacy and safety of sertraline treatment of posttraumatic stress disorder. Journal of the American Medical Association. 2000;283:1837–1844. doi: 10.1001/jama.283.14.1837. [DOI] [PubMed] [Google Scholar]
- Bremner JD. The relationship between cognitive and brain changes in posttraumatic stress disorder. Annals of New York Academy of Sciences. 2006;1071:80–86. doi: 10.1196/annals.1364.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bremner JD, Krystal JH, Putnam FW, Soutwick SM, Maramar C, Charney DS, Mazure CM. Measurement of dissociative states with the clinician-administered dissociative states scale (CADSS) Journal of Traumatic Stress. 1998;11:125–136. doi: 10.1023/A:1024465317902. [DOI] [PubMed] [Google Scholar]
- Bremner JD, Vermetten E. Neuroanatomical changes associated with pharmacotherapy in posttraumatic stress disorder. Annals of New York Academy of Sciences. 2004;1032:154–157. doi: 10.1196/annals.1314.012. [DOI] [PubMed] [Google Scholar]
- Bremner JD, Vythilingam M, Vermetten E, Southwick SM, McGlashan T, … Charney DS. MRI and PET study of deficits in hippocampal structure and function in women with childhood sexual abuse and posttraumatic stress disorder. American Journal of Psychiatry. 2003;160:924–932. doi: 10.1176/appi.ajp.160.5.924. [DOI] [PubMed] [Google Scholar]
- Brewin CR. Cognitive processing of adverse experiences. International Review of Psychiatry. 1996;8(4):333–339. doi: 10.3109/09540269609051548. [DOI] [Google Scholar]
- Brewin CR. A cognitive neuroscience account of posttraumatic stress disorder and its treatment. Behaviour Research and Therapy. 2001;39:373–393. doi: 10.1016/S0005-7967(00)00087-5. [DOI] [PubMed] [Google Scholar]
- Brewin CR. Episodic memory, perceptual memory, and their interaction: Foundations for a theory of posttraumatic stress disorder. Psychological Bulletin. 2014;140(1):69–97. doi: 10.1037/a0033722. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Gregory JD, Lipton M, Burgess N. Intrusive images in psychological disorders: Characteristics, neural mechanisms, and treatment implications. Psychological Review. 2010;117(1):210–232. doi: 10.1037/a0018113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewin CR, Holmes EA. Psychological theories of posttraumatic stress disorder. Clinical Psychology Review. 2003;23:339–376. doi: 10.1016/S0272-7358(03)00033-3. [DOI] [PubMed] [Google Scholar]
- Byrne CA, Hyman EE, Scott KL. Comparison of memories for traumatic events and other experiences. Applied Cognitive Psychology. 2001;15:S119–S133. doi: 10.1002/acp.837. [DOI] [Google Scholar]
- Bryant RA, Sutherland K, Guthrie RM. Impaired specific autobiographical memory as a risk factor for posttraumatic stress after trauma. Journal of Abnormal Psychology. 2007;116(4):837. doi: 10.1037/0021-843X.116.4.837. [DOI] [PubMed] [Google Scholar]
- Craske MG, Kircanski K, Zelikowsky M, Mystkowski J, Chowdhury N, Baker A. Optimizing inhibitory learning during exposure therapy. Behaviour Research and Therapy. 2008;46:5–27. doi: 10.1016/j.brat.2007.10.003. [DOI] [PubMed] [Google Scholar]
- Ehlers A, Clark DM. A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy. 2000;38:219–245. doi: 10.1016/S0005-7967(99)00123-0. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RB, Gibbon M, Williams JBW. Structured clinical interview for Axis 1 DSM- IV disorders. New York: Biometrics, Research Department, New York State Psychiatric Institute; 1994. [Google Scholar]
- Foa EB, Rothbaum BO, Riggs DS, Murdock TB. Treatment of posttraumatic stress disorder in rape victims: A comparison between cognitive-behavioral procedures and counseling. Journal of Consulting and Clinical Psychology. 1991;59(5):715–723. doi: 10.1037/0022-006X.59.5.715. [DOI] [PubMed] [Google Scholar]
- Foa EB, Hembree EA, Cahill SP, Rauch SAM, Riggs DS, … Yadin E. Randomized trial of prolonged exposure for posttraumatic stress disorder with and without cognitive restructuring: Outcome at academic and community clinics. Journal of Consulting and Clinical Psychology. 2005;73(5):953–964. doi: 10.1037/0022-006X.73.5.953. [DOI] [PubMed] [Google Scholar]
- Foa EB, Riggs DS. Posttraumatic stress disorder in rape victims. In: Oldham J, Riba MB, Tasman A, editors. American Psychiatric Press Review of Psychiatry. Vol. 12. Washington DC: American Psychiatric Press; 1993. pp. 273–303. [Google Scholar]
- Foa EB, Riggs DS, Dancu CV, Rothbaoum BO. Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. Journal of Traumatic Stress. 1993;6:459–473. doi: 10.1002/jts.2490060405. [DOI] [Google Scholar]
- Foa EB, Tolin DF. Comparison of the PTSD Symptom Scale-Interview Version and the Clinician-Administered PTSD Scale. Journal of Traumatic Stress. 2000;13:181–191. doi: 10.1023/A:1007781909213. [DOI] [PubMed] [Google Scholar]
- Foa EB, Hembree E, Rothbaum BO. Prolonged Exposure Therapy for PTSD: Emotional Processing of Traumatic Experiences. Oxford Univeristy Press; 2007. [Google Scholar]
- Foa EB, Huppert JD, Cahill SP. Emotional processing theory: An update. In: Rothbaum BO, editor. Pathological anxiety: Emotional processing in etiology and treatment. New York: Guilford Press; 2006. pp. 3–24. [Google Scholar]
- Foa EB, Kozak MJ. Emotional processing of fear: Exposure to corrective information. Psychological Bulletin. 1986;99:20–35. doi: 10.1037/0033-2909.99.1.20. [DOI] [PubMed] [Google Scholar]
- Foa EB, Molnar C, Cashman L. Change in rape narratives during exposure therapy for posttraumatic stress disorder. Journal of Traumatic Stress. 1995;8:675–690. doi: 10.1002/jts.2490080409. [DOI] [PubMed] [Google Scholar]
- Foa EB, Hembree EA, Dancu CV. Prolonged Exposure (PE) Manual: Revised Version. University of Pennsylvania; 2002. [Google Scholar]
- Francis ME, Pennebaker JW. Putting stress into words: Writing about personal upheavals and health. American Journal of Health Promotions. 1992;6:280–287. doi: 10.4278/0890-1171-6.4.280. [DOI] [PubMed] [Google Scholar]
- Gray MJ, Lombardo TW. Complexity of trauma narratives as an index of fragmented memory in PTSD: A critical analysis. Applied Cognitive Psychology. 2001;15:S171–S186. doi: 10.1002/acp.840. [DOI] [Google Scholar]
- Halligan SL, Clark DM, Ehlers A. Cognitive processing, memory, and the development of PTSD symptoms: Two experimental analogue studies. Journal of Behavior Therapy and Experimental Psychiatry. 2002;33:73–89. doi: 10.1016/s0005-7916(02)00014-9. [DOI] [PubMed] [Google Scholar]
- Halligan SA, Michael T, Clark DM, Ehlers A. Posttraumatic stress disorder following assault: The role of cognitive processing, trauma memory, and appraisals. Journal of consulting and Clinical Psychology. 2003;71:419–431. doi: 10.1037/0022-006X.71.3.419. [DOI] [PubMed] [Google Scholar]
- Hedeker D, Gibbons RD. MIXREG: a computer program for mixed-effects regression analysis with autocorrelated errors. Computer Methods and Programs in Biomedicine. 1996;49:229–252. doi: 10.1016/0169-2607(96)01723-3. [DOI] [PubMed] [Google Scholar]
- Horowitz M. Stress response syndrome. 2. New Jersey: Jason Aronson; 1986. [Google Scholar]
- Jaccard J, Guilamo-Ramos V. Analysis of variance frameworks in clinical child and adolescent psychology: Issues and recommendations. Journal of Clinical Child and Adolescent Psychology. 2002a;31:130–46. doi: 10.1207/S15374424JCCP3101_15. [DOI] [PubMed] [Google Scholar]
- Jaccard J, Guilamo-Ramos V. Analysis of variance frameworks in clinical child and adolescent psychology: Advanced issues and recommendations. Journal of Clinical Child and Adolescent Psychology. 2002b;31:278–294. doi: 10.1207/S15374424JCCP3102_13. [DOI] [PubMed] [Google Scholar]
- Jaeger J, Lindblom KM, Parker-Guilbert K, Zoellner LA. Trauma narratives: It’s what you say, not how you say it. Psychological Trauma: Theory, Research, Practice, and Policy. 2014;6:473–481. doi: 10.1037/a0035239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jelinek L, Randjbar S, Seifert D, Kellner M, Moritz S. The organization of autobiographical and nonautobiographical memory in posttraumatic stress disorder (PTSD) Journal of Abnormal Psychology. 2009;118:288–298. doi: 10.1037/a0015633. [DOI] [PubMed] [Google Scholar]
- Johnson MK, Foley MA, Suengas AG, Raye CL. Phenomenal characteristics of memories for perceived and imagined autobiographical events. Journal of Experimental Psychology: General. 1988;117:371–376. doi: 10.1037/0096-3445.117.4.371. [DOI] [PubMed] [Google Scholar]
- Jones C, Harvey AG, Brewin CR. The organisation and content of trauma memories in survivors of road traffic accidents. Behavior Research and Therapy. 2007;45:151–162. doi: 10.1016/j.brat.2006.02.004. [DOI] [PubMed] [Google Scholar]
- Kaufman AS. Assessing Adolescent and Adult Intelligence. Boston: Allyn & Bacon; 1990. [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kindt M, Buck N, Arntz A, Soeter M. Perceptual and conceptual processing as predictors of treatment outcome in PTSD. Journal of Behavior Therapy. 2007;38:491–506. doi: 10.1016/j.jbtep.2007.10.002. [DOI] [PubMed] [Google Scholar]
- Kleim B, Ehlers A. Reduced autobiographical memory specificity predicts depression and posttraumatic stress disorder after recent trauma. Journal of Consulting and Clinical Psychology. 2008;76(2):231. doi: 10.1037/0022-006X.76.2.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleim B, Grey N, Wild J, Nussbeck FW, Stott R, Hackmann A, … Ehlers A. Cognitive change predicts symptom reduction with cognitive therapy for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 2013;81(3):383–393. doi: 10.1037/a0031290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmar CR, Weiss DS, Metzler TJ. The peritraumatic dissociative experiences questionnaire. In: Wilson JP, Keane TM, editors. Assessing psychological trauma and PTSD. New York and London: The Guilford Press; 1997. pp. 144–167. [Google Scholar]
- McLean CP, Yeh R, Rosenfield D, Foa EB. Changes in negative cognitions mediate PTSD symptom reductions during client-centered therapy and prolonged exposure for adolescents. Behaviour Research and Therapy. 2015;68:64–69. doi: 10.1016/j.brat.2015.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNally RJ. Debunking myths about trauma. Canadian Journal of Psychiatry. 2005;50:817–822. doi: 10.1177/070674370505001302. [DOI] [PubMed] [Google Scholar]
- Moulds ML, Bryant RA. Traumatic memeories in acute stress disorder: An analysis of narratives before and after treatment. Clinical Psychologist. 2005;9:10–14. doi: 10.1080/13284200500116971. [DOI] [Google Scholar]
- Mundorf ES, Paivio SC. Narrative quality and disturbance pre-and post-emotion-focused therapy for child abuse trauma. Journal of Traumatic Stress. 2011;24:643–650. doi: 10.1002/jts.20707. [DOI] [PubMed] [Google Scholar]
- Murray J, Ehlers A, Mayou RA. Dissociation and posttraumatic stress disorder: Two prospective studies of road traffic accident survivors. British Journal of Psychiatry. 2002;180:363–368. doi: 10.1192/bjp.180.4.363. [DOI] [PubMed] [Google Scholar]
- Paunovic N, Öst L. Cognitive-behavior therapy vs exposure therapy in the treatment of PTSD in refugees. Behaviour Research and Therapy. 2001;39:1183–1197. doi: 10.1016/S0005-7967(00)00093-0. [DOI] [PubMed] [Google Scholar]
- Pennebaker JW, Francis ME, Booth RJ. Linguistic Inquiry and Word Count (LIWC):LIWC 2001. Mahwah, NJ: Erlbaum; 2001. [Google Scholar]
- Quirk GJ, Garcia R, Gonzalez-Lima F. Prefrontal mechanisms in extinction of conditioned fear. Biological Psychiatry. 2006;60:337–343. doi: 10.1016/j.biopsych.2006.03.010. [DOI] [PubMed] [Google Scholar]
- Regambal MJ, Alden LE. Pathways to intrusive memories in a trauma analogue paradigm: A structural equation model. Depression and Anxiety. 2009;26:155–166. doi: 10.1002/da.20483. [DOI] [PubMed] [Google Scholar]
- Rubin DC. The coherence of memories for trauma: Evidence from posttraumatic stress disorder. Consciousness and Cognition. 2011;20(3):857–865. doi: 10.1016/j.concog.2010.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin DC, Feldman ME, Beckham JC. Reliving, emotions, and fragmentation in the autobiographical memories of veterans diagnosed with PTSD. Applied Cognitive Psychology. 2004;18:17–35. doi: 10.1002/acp.950. [DOI] [Google Scholar]
- Rubin DC, Boals A, Berntsen D. Memory in posttraumatic stress disorder: properties of voluntary and involuntary, traumatic and nontraumatic autobiographical memories in people with and without posttraumatic stress disorder symptoms. Journal of Experimental Psychology: General. 2008;137(4):591. doi: 10.1037/a0013165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sachinvala N, Kling A, Suffin S, Lake R, Cohen M. Increased regional cerebral perfusion by Tc Hexamenthyl Propylene Amine Oxime single photon emission computed tomotgraphy in posttraumatic stress disorder. Military Medicine. 2000;165:473–479. [PubMed] [Google Scholar]
- Schwartz BL, Benjamin A, Bjork R. The inferential and experiential bases of metamemory. Current Directions in Psychological Science. 1997;6:132–137. doi: 10.1111/1467-8721.ep10772899. [DOI] [Google Scholar]
- Shipley WC. The Shipley Institute of Living Scale. Los Angeles, CA: Western Psychological Services; 1967. [Google Scholar]
- Shobe KK, Kihlstrom JF. Is traumatic memory special? Current Directions in Psychological Science. 1997;6:70–74. doi: 10.1111/1467-8721.ep11512658. [DOI] [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene RE. Manual for the State-Trait Anxiety Inventory (Self-Evaluation Questionnaire) Palo Alto, CA: Consulting Psychologists Press; 1970. [Google Scholar]
- van der Kolk BA. Psychological Trauma. Washington DC: American Psychiatric Press; 1987. [Google Scholar]
- van der Kolk BA. The body keeps score: Memory and the evolving psychobiology of posttraumatic stress. Harvard Review of Psychiatry. 1994;1:253–265. doi: 10.3109/10673229409017088. [DOI] [PubMed] [Google Scholar]
- van der Kolk BA. The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma. United Kingdom: Penguin Publishing; 2014. [Google Scholar]
- van der Kolk BA, Hopper JW, Osterman JE. Exploring the nature of traumatic memory: Combining clinical knowledge with laboratory methods. Journal of Aggression, Maltreatment, and Trauma. 2001;4:9–31. doi: 10.1300/J146v04n02_02. [DOI] [Google Scholar]
- van Minnen A, Wessel I, Dijkstra T, Roelofs K. Changes in PTSD patients’ narratives during prolonged exposure therapy: A replication and extension. Journal of Traumatic Stress. 2002;15:255–258. doi: 10.1023/A:1015263513654. [DOI] [PubMed] [Google Scholar]
- Vermetten E, Vythilingam M, Southwick SM, Charney DS, Bremner JD. Long-term treatment with paroxetine increases verbal declarative memory and hippocampal volume in posttraumatic stress disorder. Biological Psychiatry. 2003;54:693–702. doi: 10.1016/S0006-3223(03)00634-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vythilingam M, Vermetten E, Anderson GM, Luckenbaugh D, Anderson ER, Bremner JD. Hippocampal volume, memory, and cortisol status in major depressive disorder: Effects of treatment. Biological Psychiatry. 2004;56:101–112. doi: 10.1016/j.biopsych.2004.04.002. [DOI] [PubMed] [Google Scholar]
- Watts BV, Schnurr PP, Mayo L, Young-Xu Y, Weeks WB, Friedman MJ. Meta-analysis of the efficacy of treatments for posttraumatic stress disorder. The Journal of Clinical Psychiatry. 2013;(74):e541–e550. doi: 10.4088/JCP.12r08225. [DOI] [PubMed] [Google Scholar]
- Wolpe J. Psychotherapy by Reciprocal Inhibition. Stanford, CA: Stanford University Press; 1958. [Google Scholar]
- Zalta AK, Gillihan SJ, Fisher AJ, Mintz J, McLean CP, Yehuda R, Foa EB. Change in negative cognitions associated with PTSD predicts symptom reduction in prolonged exposure. Journal of Consulting and Clinical Psychology. 2014;82:171. doi: 10.1037/a0034735. [DOI] [PMC free article] [PubMed] [Google Scholar]