Abstract
Background
While important for substance use outcomes, knowledge about treatment attendance patterns, and their relation with clinical outcomes is limited. We examined the association between attendance patterns and smoking outcomes in a randomized, controlled smoking cessation intervention trial.
Methods
In addition to standard smoking cessation treatment, participants were randomized to 15 weeks of an exercise intervention (n=72) or an education control condition (n=64). Latent class growth analysis (LCGA) tested whether intervention attendance would be better modeled as qualitatively distinct attendance patterns rather than as a single mean pattern. Multivariate generalized linear mixed modeling (GLMM) was used to evaluate associations between the attendance patterns and abstinence at the end of treatment and at 6-month follow-up.
Results
The LCGA solution with three patterns characterized by high probability of attendance throughout (Completers, 46.3%), gradual decreasing probability of attendance (Titrators, 23.5%), and high probability of dropout within the first few weeks (Droppers, 30.1%) provided the best fit. The GLMM analysis indicated an interaction of attendance pattern by treatment condition, such that titration was associated with lower probability of quit success for those in the control condition. Probability of quit success was not significantly different between Titrators and Completers in the exercise condition.
Conclusions
These findings underscore the importance of examining how treatment efficacy may vary as a function of attendance patterns. Importantly, treatment discontinuation is not necessarily indicative of poorer abstinence outcome.
Keywords: attendance, dropout, dose-response, exercise, smoking cessation, anxiety sensitivity
1. INTRODUCTION
Despite a reduction in smoking prevalence, there remain one billion cigarette smokers worldwide, over 40 million of whom live in the United States (Centers for Disease Control and Prevention [CDC], 2011). Over 50% of U.S. smokers attempt to quit annually, yet only 6% succeed (CDC, 2015, 2011). Although effective treatments exist, completion rates reported in smoking cessation trials range from 50%–70% (Baker et al., 2006; Borrelli et al., 2002; Curtin et al., 2000; Evins et al., 2008; Marcus et al., 1999). In some cases, a greater number of sessions attended or treatment completion have shown positive associations with outcomes (Baker et al., 2006; Fiore, 2008; Smits et al., 2016; Whiteley et al., 2012), but this is not ubiquitous, suggesting individual differences in dose-response exist (Baldwin et al., 2009; Barkham et al., 2006; Owen et al., 2016; Reese et al., 2011). The Good Enough Level (GEL) model posits that optimal treatment dosage varies as a function of individual improvement rates such that patients who improve quickly may self-modulate treatment dosage via early discontinuation (Owen et al., 2016; Reese et al., 2011).
Evidence consistent with the GEL model has been reported in the substance use disorder literature. For example, in a clinical trial of prolonged exposure with naltrexone for comorbid posttraumatic stress disorder (PTSD) and alcohol dependence, both fast and slow rates of PTSD symptom improvement, as well as fast rates of drinking improvement, were each associated with early dropout (Zandberg et al., 2016). Another treatment trial for comorbid PTSD and SUD used a person-centered approach to empirically derive distinct attendance patterns of early dropout, titration, and completion—importantly; treatment titration was not associated with poorer outcomes relative to completion (Hien et al., 2012). These results add to an emerging body of literature suggesting that treatment discontinuation is not necessarily an indicator of nonresponse.
The current study examined attendance patterns and their relations with treatment outcome in a randomized controlled trial evaluating the efficacy of exercise as an adjunctive intervention for smoking cessation among individuals with high anxiety sensitivity (AS). The core outcome analysis showed that participants high in AS randomized to exercise were more likely to remain abstinent following quit day and session attendance showed an overall positive association with abstinence (Smits et al., 2016). The present analysis tested whether qualitatively distinct attendance patterns could be identified using a person-centered cluster analytic approach, and whether these empirically-derived patterns moderated the effect of treatment on abstinence.
2. METHODS
2.1 Participants
Participants were 136 (52.2% female, AgeM=44.2 years [SD=11.3 years]) adult daily sedentary smokers (average of 19.4 [SD=9.7] cigarettes per day) with elevated AS who were motivated to quit. A complete description of eligibility criteria and participant demographics and smoking characteristics are presented in Smits et al. (2012, 2016).
2.2 Interventions
All participants received a standard treatment (Fiore, 2000; Zvolensky et al., 2008) of seven weekly 60-minute sessions of cognitive behavioral therapy for smoking cessation and optional nicotine replacement therapy (NRT). Additionally, participants were randomized to a vigorous-intensity exercise intervention or a wellness education intervention, each consisting of three weekly 25-minute sessions for 15 weeks. All together, each session included treatment (either exercise or wellness education), therapist support, and optional NRT patches. For a detailed description of the procedures see (Smits et al., 2012).
2.3 Attendance
Participants were coded as either active or inactive for each of the 15 weeks of treatment. To be coded active completion of at least one of the three weekly sessions was required. We used weekly attendance (as opposed to using the 45 individual sessions as the repeated measure) because: 1) Key milestones (e.g., preparing for quit, target quit week, relapse prevention, follow-up) were defined on a week-by-week (not session-to-session) basis and 2) Fitting the model required equally spaced time points between participants.
2.4 Abstinence
Self-reported smoking status was verified by expired carbon monoxide at weekly visits, and with saliva cotinine at follow-up (SRNT Subcommittee on Biochemical Verification, 2002). If biological verification was not available to verify self-report, abstinence was considered missing data (Blankers et al., 2016). Point prevalence abstinence (PPA) was defined as no smoking, not even a puff, in the 7 days prior to any assessment. Failure to maintain prolonged abstinence (PA) at any assessment was defined by 7 or more consecutive days of smoking or smoking at least 1 cigarette over the 2 consecutive weeks prior to the assessment (Hughes et al., 2003; Smits et al., 2016).
2.5 Data Analyses
Latent class growth analysis (LCGA) in Mplus version 7 (Muthén and Muthén, 1998) tested the hypothesis that multiple patterns of weekly attendance would characterize the sample better than a single pattern. Weekly attendance was modeled across 15 weeks of treatment with a discontinuity at quit week. This piecewise approach mirrors the current and previous outcome models. Model information criteria, entropy, the adjusted Lo-Mendel-Rubin likelihood ratio test, and parsimony were all considered in the evaluation of model fit. Posterior probabilities of the best fitting model determined individual attendance pattern assignments.
Following Smits et al., (2016) two dichotomous measures of smoking behavior (PPA and PA) were examined in a three-phase (i.e., pre-quit, post-quit, post-treatment) generalized linear mixed model (GLMM) following the intent-to-treat approach recommended for smoking cessation trials (Hall et al., 2001). Attendance pattern, treatment condition, AS, and two-way interactions were included as predictors. To minimize Type II error, provide a more parsimonious model, and more clearly elucidate the overall relations between the predictors and abstinence, non-significant interaction terms were removed (Baldwin et al., 2009; Cohen, 1983).
3. RESULTS
3.1 Attendance Patterns
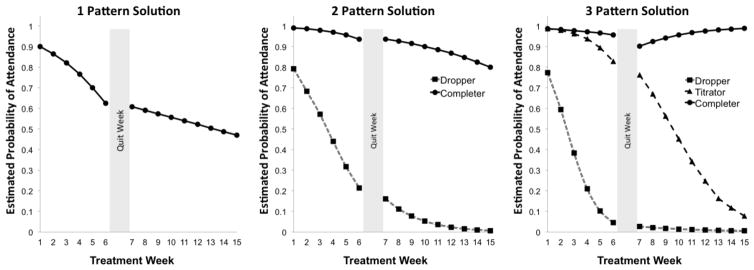
The 3-class LCGA provided the best fit with lowest information criteria, high entropy (0.96) suggestive of strong delineation of classes, and a significant adjusted Lo-Mendel-Rubin likelihood ratio test, p=.01. Three distinct attendance patterns were identified: Completers (n=63, 46.3%) had high probability of attending throughout the entire treatment duration, Titrators (n=32, 23.5%) showed a gradual decline in probability of attending throughout the 15 weeks of treatment, and Droppers (n=41, 31.1%) had a high probability of dropout within the first few weeks of treatment (Figure 1). The distribution of participants following each attendance pattern was significantly different between treatments, χ2(2)=7.46, p=.02. Specifically, there was a difference in the proportion of participants within each treatment who were Completers (exercise: n=26, 36.1% vs. control: n=37, 57.8%) or Droppers (exercise: n=28, 38.9% vs. control: n=13, 20.3%), whereas Titrator proportions were not significantly different (exercise: n=18, 25.0% vs. control: n=14, 21.9%). On weeks that participants were actively attending treatment, the average number of sessions attended was 2.51 sessions, 63% attended all 3 weekly sessions, 25% attended 2 out of the 3 weekly sessions, and 12% attended only one of the 3 weekly sessions.
Figure 1.
Each panel in Figure 1 depicts a step in the latent growth class modeling analysis. Each step in the analysis allows for an additional cluster of individuals who followed a similar attendance pattern. The 3 pattern solution provides the most accurate description of participant’s engagement over the 15-week intervention
3.2 Abstinence Outcomes
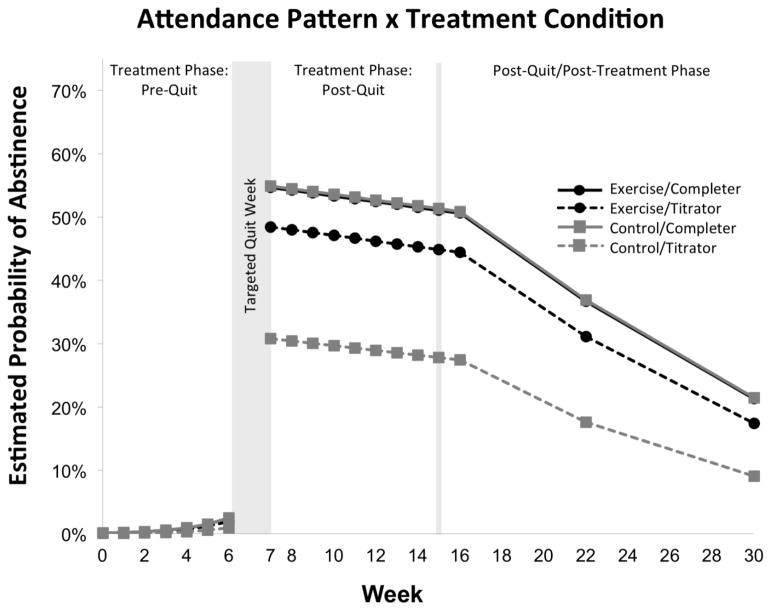
Subsequent analysis of the relation between treatment attendance pattern and abstinence was restricted to the Completer versus Titrator since Droppers withdrew prior to quit week. The final model yielded a significant attendance pattern by treatment interaction, β=0.758, 95% CI [−0.293, 1.223], t(3047)=3.195, p=.001 (Figure 2). Although the probability of abstinence at post-treatment was not significantly different between Completers and Titrators in the exercise condition, β=0.248, 95% CI [−0.086, 0.583], t(3047)=1.455, p=0.146, Completers in the control condition were more likely to be abstinent than Titrators, β=1.006, 95% CI [0.683, 1.329], t(3047)=6.102, p < .001. Moreover, among Completers, there were no significant differences between those in the exercise vs. the control condition, β=0.120, 95% CI [−0.104, 0.344], t(3047)=1.054, p=.292, whereas Titrators in the exercise condition were more likely to be abstinent than Titrators in the control condition, β=0.637, 95% CI [0.238, 1.037], t(3047)=3.127, p=.002. Full model statistics are reported in Supplementary Material1.
Figure 2.
Estimated probability of abstinence throughout the 30-weeks of treatment for participants by treatment condition and Titrator or Completer attendance patterns. The analysis indicated an attendance pattern by treatment condition interaction at the end of treatment and at 6-month follow-up such that only Titrators in the control condition had significantly lower probability of quit success. ASI was centered at high ASI (ASI=23).
4. DISCUSSION
Three distinct attendance patterns were empirically-derived in a smoking cessation trial: 1) Droppers attended only the first few weeks of treatment, 2) Titrators gradually reduced their attendance, and 3) Completers attended throughout the entire treatment. Within each treatment, there were fewer Completers and more Droppers in the exercise relative to control condition, whereas similar proportions of Titrators were observed across treatments. Although Droppers lacked outcome data, subsequent analyses of abstinence rates showed that Titrators did not necessarily show poorer outcomes compared to Completers.
Consistent with the GEL model (Hien et al., 2012; Reese et al., 2011), Titrators in the exercise condition had cessation outcomes that were not significantly different than for those completing the intervention, despite attending fewer sessions. Exercise may assist smoking cessation by mitigating anxiety during acute withdrawal symptoms (Leventhal and Zvolensky, 2015), which may be most pronounced after the initial quit attempt. Since success with abstinence within the first 24 hours after quit is predictive of continued abstinence (Perkins, 2014), Titrators who were likely to remain engaged in the exercise intervention through quit week may have benefited comparably to Completers despite lower overall attendance. Given evidence of rapid benefits from exercise on anxiety, mood, and anxiety sensitivity in other studies (Medina et al., 2014; Smits et al., 2008), exercise may exert its influence on risk factors for smoking relapse in only a few sessions early on in treatment.
Interestingly, our analysis provided no evidence of differential treatment effects among Completers. It is possible that the treatments themselves confer comparable benefits at this dosage, or that treatment completion marks individuals who are highly motivated, both in terms of completing the intervention and remaining abstinent. Future studies that manipulate treatment dose would allow testing of causal relations. However, Titrators in the control condition showed lower rates of abstinence compared to control Completers, suggesting that the wellness education-augmented intervention may exert its effects vis-à-vis ongoing social support and accountability. Thus, attendance through the post-quit phase may be necessary to optimize benefits.
It is important to note there were fewer Completers and more Droppers in the exercise relative to control condition, whereas similar proportions of Titrators were observed across treatments. The disproportionate number of Droppers in the exercise condition may indicate that the exercise intervention was more aversive or challenging to adhere to. If so, higher motivation to engage with the intervention or remain abstinent among the Titrators and Completers in the exercise condition may again provide an alternative explanation for the differences in abstinence rates.
The findings reported here expand on those reported in the main outcome paper (Smits et al., 2016) by showing that the relation between attendance patterns and treatment success may not be linear and, importantly, may depend on the type of intervention. Nevertheless, several limitations should be noted. The original study was not designed to compare intervention lengths, thus results reflect participant-determined attendance patterns as opposed to “prescribed” treatment dosage. Furthermore, since the study was not designed to compare treatment dosage, it was not powered specifically for the present analysis; therefore, the lack of statistical differences between attendance patterns in the exercise condition may be a reflection of inadequate power to detect small differences. Thus, while intriguing and hypothesis generating, these findings require replication and further study. Additionally, since Droppers were excluded from abstinence analyses due to lack of outcome data, our ability to capture the full scope of the relationship between treatment attendance and outcome was limited. Future studies may benefit from increasing participant engagement with data collection after dropout to better understand the reasons for early dropout and the outcome after a brief dose of treatment.
Together, the present findings show that treatment attendance patterns can be empirically-derived and related to efficacy, helping to generate testable hypotheses for follow-up studies that aim to refine interventions. Future studies can also examine individual characteristics that interact with treatment length to predict outcomes, which is critical to interventions with disproportionate level of Droppers, as was observed in the current exercise condition. Importantly, an improved understanding of participants’ reasons for treatment discontinuation may help inform approaches to either re-engagement when desired outcomes have not been achieved, or to the maintenance of gains among early responders. In conclusion, our results add to the growing literature suggesting that optimal treatment dosage may vary as a function of individuals’ improvement rate.
Supplementary Material
HIGHLIGHTS.
Attendance was characterized by three patterns; Completers, Titrators, and Droppers
Titration was associated with lower quit success within the control condition
Titrators and Completers had similar quit success within the exercise intervention
Acknowledgments
Role of Funding Source: This study was funded by a grant from the National Institute on Drug Abuse (NIDA; R01DA027533, 2009). NIDA plays no role in approving the publications.
Footnotes
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:...
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:...
Contributions: JJ, along with SP, was the primary contributors to the initial draft. JJ, SP, and DR analyzed the data. MLD, LBH, and SOB, were involved in original data collection as well as manuscript preparation. DR, MBP, GMF, BHM, TSC, MWO, MJZ, and JAJS were all involved in the original study conceptualization and implementation, oversaw all data analyses from this dataset, and contributed to the manuscript. All authors have approved the final version and provided consent to their names on the manuscript.
Conflicts of Interest: The authors have declared that no competing interests exist.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Baker A, Richmond R, Haile M, Lewin TJ, Carr VJ, Taylor RL, Jansons S, Wilhelm K. A randomized controlled trial of a smoking cessation intervention among people with a psychotic disorder. Am J Psychiatry. 2006;163:1934–1942. doi: 10.1176/ajp.2006.163.11.1934. [DOI] [PubMed] [Google Scholar]
- Baldwin SA, Berkeljon A, Atkins DC, Olsen JA, Nielsen SL. Rates of change in naturalistic psychotherapy: Contrasting dose-effect and good-enough level models of change. J Consult Clin Psychol. 2009;77:203–211. doi: 10.1037/a0015235. [DOI] [PubMed] [Google Scholar]
- Barkham M, Connell J, Stiles WB, Miles JNV, Margison F, Evans C, Mellor-Clark J. Dose-effect relations and responsive regulation of treatment duration: The good enough level. J Consult Clin Psychol. 2006;74:160–167. doi: 10.1037/0022-006X.74.1.160. [DOI] [PubMed] [Google Scholar]
- Blankers M, Smit ES, van der Pol P, de Vries H, Hoving C, van Laar M. The missing=smoking assumption: A fallacy in internet-based smoking cessation trials? Nicotine Tob Res Off J Soc Res Nicotine Tob. 2016;18:25–33. doi: 10.1093/ntr/ntv055. [DOI] [PubMed] [Google Scholar]
- Borrelli B, Hogan JW, Bock B, Pinto B, Roberts M, Marcus B. Predictors of quitting and dropout among women in a clinic-based smoking cessation program. Psychol Addict Behav. 2002;16:22–27. doi: 10.1037/0893-164X.16.1.22. [DOI] [PubMed] [Google Scholar]
- Centers for Disease and Prevention (CDC) Current cigarette smoking among adults—United States, 2005–2014. Morb Mortal Wkly Rep. 2015;64:1233–40. doi: 10.15585/mmwr.mm6444a2. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Quitting smoking among adults--United States, 2001–2010. Morb Mortal Wkly Rep. 2011;60:1513–1519. [PubMed] [Google Scholar]
- Cohen J. Applied Multiple Regression/correlation Analysis for the Behavioral Sciences. Taylor and Francis; 1983. [Google Scholar]
- Curtin L, Brown RA, Sales SD. Determinants of attrition from cessation treatment in smokers with a history of major depressive disorder. Psychol Addict Behav J Soc Psychol Addict Behav. 2000;14:134–142. doi: 10.1037//0893-164x.14.2.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evins AE, Culhane MA, Alpert JE, Pava J, Liese BS, Farabaugh A, Fava M. A controlled trial of bupropion added to nicotine patch and behavioral therapy for smoking cessation in adults with unipolar depressive disorders. J Clin Psychopharmacol. 2008;28:660–666. doi: 10.1097/JCP.0b013e31818ad7d6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiore MC. Treating Tobacco Use and Dependence: 2008 Update: Clinical Practice Guideline. DIANE Publishing; 2008. [Google Scholar]
- Fiore MC. US public health service clinical practice guideline: Treating tobacco use and dependence. Respir Care. 2000;45:1200–1262. [PubMed] [Google Scholar]
- Hall SM, Delucchi KL, Velicer WF, Kahler CW, Ranger-Moore J, Hedeker D. Statistical analysis of randomized trials in tobacco treatment: longitudinal designs with dichotomous outcome. Nicotine Tob Res. 2001;3:193–202. doi: 10.1080/14622200110050411. [DOI] [PubMed] [Google Scholar]
- Hien DA, Morgan-Lopez AA, Campbell ANC, Saavedra LM, Wu E, Cohen L, Ruglass L, Nunes EV. Attendance and substance use outcomes for the Seeking Safety program: Sometimes less is more. J Consult Clin Psychol. 2012;80:29–42. doi: 10.1037/a0026361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes JR, Keely JP, Niaura RS, Ossip-Klein DJ, Richmond RL, Swan GE. Measures of abstinence in clinical trials: Issues and recommendations. Nicotine Tob Res Off J Soc Res Nicotine Tob. 2003;5:13–25. [PubMed] [Google Scholar]
- Leventhal AM, Zvolensky MJ. Anxiety, depression, and cigarette smoking: A transdiagnostic vulnerability framework to understanding emotion-smoking comorbidity. Psychol Bull. 2015;141:176–212. doi: 10.1037/bul0000003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus BH, Albrecht AE, King TK, Parisi AF, Pinto BM, Roberts M, Niaura RS, Abrams DB. The efficacy of exercise as an aid for smoking cessation in women: A randomized controlled trial. Arch Intern Med. 1999;159:1229–1234. doi: 10.1001/archinte.159.11.1229. [DOI] [PubMed] [Google Scholar]
- Medina JL, DeBoer LB, Davis ML, Rosenfield D, Powers MB, Otto MW, Smits JAJ. Gender moderates the effect of exercise on anxiety sensitivity. Ment Health Phys Act. 2014;7:147–151. doi: 10.1016/j.mhpa.2014.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 7. Muthén and Muthén; Los Angeles, CA: 1998. [Google Scholar]
- Owen JJ, Adelson J, Budge S, Kopta SM, Reese RJ. Good-enough level and dose-effect models: Variation among outcomes and therapists. Psychother Res. 2016;26:22–30. doi: 10.1080/10503307.2014.966346. [DOI] [PubMed] [Google Scholar]
- Perkins KA. Improving efficiency of initial tests for efficacy in smoking cessation drug discovery. Expert Opin Drug Discov. 2014;9:1259–1264. doi: 10.1517/17460441.2014.951632. [DOI] [PubMed] [Google Scholar]
- Reese RJ, Toland MD, Hopkins NB. Replicating and extending the good-enough level model of change: Considering session frequency. Psychother Res J Soc Psychother Res. 2011;21:608–619. doi: 10.1080/10503307.2011.598580. [DOI] [PubMed] [Google Scholar]
- Smits JAJ, Berry AC, Rosenfield D, Powers MB, Behar E, Otto MW. Reducing anxiety sensitivity with exercise. Depress Anxiety. 2008;25:689–699. doi: 10.1002/da.20411. [DOI] [PubMed] [Google Scholar]
- Smits JAJ, Zvolenksy MJ, Davis ML, Rosenfield D, Marcus BH, Church TS, Powers MB, Frierson GM, Otto MW, Hopkins LB, Baird SO. The efficacy of vigorous-intensity exercise as an aid to smoking cessation in adults with high anxiety sensitivity: A randomized controlled trial. Psychosom Med. 2016;78:354–364. doi: 10.1097/PSY.0000000000000264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smits JAJ, Zvolensky MJ, Rosenfield D, Marcus BH, Church TS, Frierson GM, Powers MB, Otto MW, Davis ML, DeBoer LB, Briceno NF. The efficacy of vigorous-intensity exercise as an aid to smoking cessation in adults with elevated anxiety sensitivity: Study protocol for a randomized controlled trial. Trials. 2012;13:207–221. doi: 10.1186/1745-6215-13-207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SRNT Subcommittee on Biochemical Verification. Biochemical verification of tobacco use and cessation. Nicotine Tob Res Off J Soc Res Nicotine Tob. 2002;4:149–159. doi: 10.1080/14622200210123581. [DOI] [PubMed] [Google Scholar]
- Whiteley JA, Williams DM, Dunsiger S, Jennings EG, Ciccolo JT, Bock BC, Albrecht A, Parisi A, Linke SE, Marcus BH. YMCA commit to quit: Randomized trial outcomes. Am J Prev Med. 2012;43:256–262. doi: 10.1016/j.amepre.2012.05.025. [DOI] [PubMed] [Google Scholar]
- Zandberg LJ, Rosenfield D, Alpert E, McLean CP, Foa EB. Predictors of dropout in concurrent treatment of posttraumatic stress disorder and alcohol dependence: Rate of improvement matters. Behav Res Ther. 2016;80:1–9. doi: 10.1016/j.brat.2016.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zvolensky MJ, Yartz AR, Gregor K, Gonzalez A, Bernstein A. Interoceptive exposure-based cessation intervention for smokers high in anxiety sensitivity: A case series. J Cogn Psychother. 2008;22:346–365. doi: 10.1891/0889-8391.22.4.346. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.