Abstract
This article examines the causal effect of women’s education on maternal health in Peru, a country where maternal mortality has declined by more than 70% in the last two and a half decades. To isolate the effects of education, the author employs an instrumented regression discontinuity that takes advantage of an exogenous source of variation—an amendment to compulsory schooling laws in 1993. The results indicate that extending women’s years of schooling reduced the probability of several maternal health complications at last pregnancy/birth, sometimes by as much as 29%. Underlying these effects, increasing women’s education is found to decrease the probability of short birth intervals and unwanted pregnancies (which may result in unsafe abortions) and to increase antenatal healthcare use, potentially owing to changes in women’s cognitive skills, economic resources, and autonomy. These findings underscore the influential role of education in reducing maternal morbidity and highlight the contributions of women’s education to population health and health transitions.
Keywords: Peru, Maternal health, Education
Over the last twenty-five years Peru has experienced a dramatic decline in maternal mortality, from approximately 250 deaths per 100,000 live births in 1990 to 70 deaths per 100,000 live births in 2015 (World Bank 2015a). There are many potential explanations for this decline, including economic growth (Shen and Williamson 1999), the expansion of healthcare (Angeles, Guilkey and Mroz 2005), and falling fertility rates (Martin and Juarez 1995). This article investigates the potential role of women’s education, which has risen in Peru almost as dramatically as maternal mortality has fallen (World Bank 2015b). Specifically, it explores the individual-level effects of women’s education on maternal health outcomes that are associated with an increased risk of maternal mortality and further investigates related behavioral changes, such as changes in fertility practices and healthcare utilization.
A positive relationship between women’s education and maternal health is well documented (Falkingham 2003; Karlsen et al. 2011; Onah, Ikeako and Iloabachie 2006; Raghupathy 1996). However, few studies have been able to determine whether women’s education has a causal effect or whether the link between education and maternal health is attributable to factors correlated with both, such as household wealth (or poverty). Identifying whether increasing women’s education actually alters their behavior and improves their health outcomes is an important step toward refining theoretical models of the determinants of maternal mortality and requires exploiting an exogenous source of variation in education, for instance, randomly incentivizing school attendance for some children but not others (Baird et al. 2010), taking advantage of spatiotemporal variation in school construction (Duflo 2001), or leveraging changes in educational policies (Behrman 2015a; Behrman 2015b).
A small but growing number of studies employing exogenous sources of variation has recently confirmed that women’s education influences demographic behaviors related to reproductive health. These studies have shown, for example, that improving women’s access to schooling decreases their desired and realized fertility (Behrman 2015a; Breierova and Duflo 2004), delays their sexual debut (Baird et al. 2010), and improves their ability to negotiate sex (Baird et al. 2010). They’ve also shown that increasing women’s education protects against sexually transmitted infections (Behrman 2015b; De Neve et al. 2015) and reduces the risk of child mortality (Grépin and Bharadwaj 2015). These effects of women’s education on fertility, disease transmission, and child wellbeing give rise to the possibility that women’s education affects maternal health as well: as education expands and fertility falls, women’s exposure to maternal health complications should diminish alongside their number of pregnancies and births (Winikoff and Sullivan 1987). Moreover, if education enhances health-seeking behaviors, then this may lead to the prevention and early detection of complications during pregnancy and childbirth and reduce the risk of death when complications arise (Carroli, Rooney and Villar 2001).
In the following pages, I review the different perspectives on why women’s education should benefit maternal health, and in turn, lead to reductions in maternal mortality. I then assess the health effects of women’s education by exploiting an exogenous reform in compulsory schooling law in Peru that extended the required number of years of schooling by 5 years. I use an instrumented regression discontinuity (RD) to test the effects of education on preventable and semi-preventable1 maternal health conditions associated with an increased risk of maternal mortality and to examine the effects of women’s education on the precursors to maternal health.
Women’s Education and Maternal Health
Historically, Peru has had one of the highest rates of maternal mortality in the Western hemisphere, though these rates have fallen precipitously in recent years (World Bank 2015a). The most common causes of maternal mortality2 in Peru include complications related to unsafe abortion (which is highly restricted), hemorrhage, preeclampsia, infections, and obstructed birth (Amnesty International 2009). Many of these conditions are aggravated by short birth spacing and high fertility (>=5 births) (Conde-Agudelo, Rosas-Bermúdez and Kafury-Goeta 2007; Trussell and Pebley 1984). Fortunately, though, they can often be detected and managed by a healthcare professional before they become fatal (Kassebaum et al. 2014; McCarthy and Maine 1992). Fertility practices related to birth spacing and unwanted pregnancy, and the use of antenatal healthcare, are thus two of the most important contributors to maternal wellbeing.
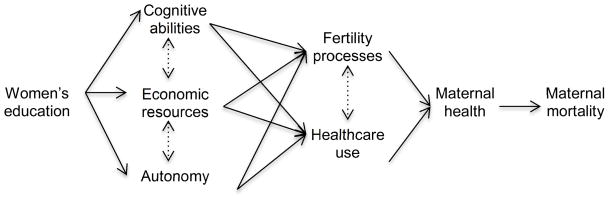
As depicted in Figure 1, this study conceptualizes women’s education as an essential, underlying determinant of maternal health (and implicitly maternal mortality). The effects of education are assumed to predominantly flow through women’s cognitive skills, material resources, and autonomy, which should in turn affect their fertility practices and healthcare use, and ultimately their health outcomes.
Figure 1.
Conceptual Model of Pathways by which Women’s Education Affects Maternal Health and Mortality
First, as others have shown, education should have a positive effect on women’s cognitive skills (Smith-Greenaway 2013). Greater cognitive skills, and especially literacy, should benefit maternal health by increasing women’s ability to seek information about their own health and by assuring that women are better able to follow written instructions (for example, understanding directions on a box of medication). Similar explanations have been given for why mothers’ literacy protects against child mortality (Smith-Greenaway 2013).
Second, women’s education should improve their economic opportunities and status (Psacharopoulos and Patrinos 2004). As depicted in Figure 1, increased opportunities for gainful employment may compete with childbearing in ways that lead women to reduce or postpone childbearing (Barber 2001). Moreover, the greater economic resources enjoyed by women with more education may influence maternal health by shaping the extent to which they can afford and access healthcare (Thaddeus and Maine 1994). This is especially true in Peru, where transportation costs and the cost of medical services are two of the most commonly cited barriers to ante- and postnatal healthcare (Amnesty International 2009).
Third, education may further improve maternal health by bolstering women’s autonomy in the home (Ahmed et al. 2010). In Peru, men have traditionally been the economic providers for their families and the ones to determine how household resources are spent (Fuller 2001). However, if education increases women’s employment or earnings, then women’s greater ability to provide for their families may grant them more decision-making power within the home (Lundberg and Pollak 1993), including decisions about whether resources are spent on their own healthcare (Ahmed et al. 2010). Under the assumption that at least some women would seek more medical attention given the opportunity to do so, increasing women’s decision-making over their own healthcare should result in improvements to their health (Figure 1).
Together, education-related improvements in women’s cognitive skills, economic resources, and autonomy should affect maternal health via changes in their fertility practices (Figure 1). For instance, if education increases economic opportunities and economic opportunities disincentivize childbearing, then education should motivate contraceptive use (Behrman 2015b). These effects of education on contraceptive use should in turn decrease the likelihood of high fertility and short birth intervals, both of which increase the risk of pregnancy complications (Conde-Agudelo, Rosas-Bermúdez and Kafury-Goeta 2007). They should also decrease the likelihood of unintended pregnancies (Trussell et al. 2013), which may indirectly decrease the demand for unsafe abortions (Rose and Lawton 2012), which account for 6.1% of maternal deaths in Peru (Amnesty International 2009 p.14).
Beyond these fertility-related changes, women’s education may affect maternal health via their use of antenatal healthcare. Antenatal healthcare visits should increase the detection of hypertensive disorders and anemia (McCarthy and Maine 1992), which can contribute to preterm birth (Scholl and Reilly 2000) and convulsions, brain hemorrhaging, comas, or cardiac arrest during pregnancy (Duley 1992; Rush 2000; Sibai, Dekker and Kupferminc 2005). Moreover, delivering children in hospitals and other formal healthcare centers, as opposed to in one’s home, should improve postnatal health by reducing the risk of postpartum infection and providing skilled birth attendants who are equipped to address complications during delivery (Graham, Bell and Bullough 2001; Kowalewski and Jahn 2000). Thus, the hypothesized, positive effects of women’s education on healthcare utilization may help to alleviate the direct causes of maternal mortality through the prevention of semi-avoidable complications and the early detection and management of unpreventable complications or preexisting conditions.
To summarize, women’s education is theorized to protect maternal health by 1) influencing fertility practices that aggravate the risk of maternal morbidity and 2) increasing women’s access to and use of preventative and palliative antenatal healthcare. These changes in fertility practices and healthcare use should stem from education’s effects on women’s cognitive skills, economic resources, and autonomy (Figure 1).
Compulsory Schooling in Peru
Understanding whether education improves maternal health, rather than being associated with better health, requires the use of causal inference methods that isolate the effects of education from confounders such as childhood socioeconomic status. In this study, I isolate the effects of education with an instrumented regression discontinuity that takes advantage of a change in Peruvian compulsory schooling laws in the 1990s. Compulsory schooling was first implemented in Peru in 1905 (Freeburger and Hauch 1964), when children were mandated to attend primary school between the ages of 6 and 11. Six years of primary school continued to be compulsory until 1993, when 11 years were made compulsory by a constitutional amendment. This legislative change predominantly affected children who still had not completed their first six years of schooling (UNESCO 2001), drawing many of them into secondary school (which typically begins at age 12).
Extending compulsory schooling by five years contributed to a 36% increase the Gross Enrollment Ratio in secondary schools between 1990 and 2010 (World Bank 2014). Among those who benefited most from compulsory schooling were populations that had previously faced particular disadvantages, namely girls and rural indigenous children (UNECOSOC 2011; UNESCO 2014). However, because it was difficult to enforce, and was not accompanied by increased public expenditure (Ministerio de Educación 2007),3 the reform did not eradicate all preexisting disparities. For instance, government investments in public education continued to be negatively correlated with state-level poverty rates (GRADE 2003) and rural children continued to face unique challenges, such as having to travel long distances to school and attending schools that lacked well-trained teachers (especially in non-Spanish speaking communities) (Ames 2011; IPEBA 2011; OECD 2016). Moreover, education quality continued to be quite poor in Peru, with only 5% of Peruvian children testing in a range equivalent to the OECD average (World Bank 2007).
Data and Methods
Sample
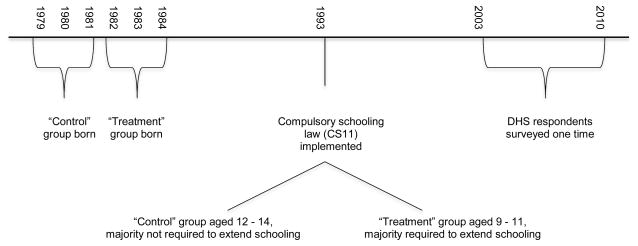
I use nationally representative, cross-sectional data from the continuous Demographic and Health Surveys (DHS) collected in Peru every year between 2003 and 2009.4 To isolate the effects of education reform in Peru, I compare respondents who were aged just above and just below the average age of primary school completion in 1993. As depicted in Figure 2, respondents who were just above the age of primary school completion (12 to 14 years in 1993) should not have been exposed to CS11 because they had already completed their required schooling by the time of policy implementation (N=3,083). Respondents who were just below the age (9 to 11) should have been exposed to CS11 because they were still enrolled in primary school at the time of implementation (N=2,358). All respondents in the analytic sample are therefore between the ages of 23 and 30 years. As a point of reference, I present the means of the outcomes of interest for all respondents in the DHS (thus depicting outcomes for the average Peruvian woman 15–49 years of age).
Figure 2.
Timeline of Events
Because the DHS only asked questions regarding reproductive healthcare utilization and pregnancy complications to women whose last pregnancy occurred within five years of survey, all analyses are limited to respondents whose last pregnancy occurred within this time frame. Given the age spectrum of the analytic sample, respondents’ most recent pregnancy must have occurred when they were aged 18 to 30 years.
Dependent Variables
Complications during last pregnancy
This study’s primary concern is the effect of increased education on maternal health outcomes related to maternal mortality. These include whether or not respondents reported a fever accompanied with vaginal bleeding during their most recent pregnancy (0/1) or a fever after their most recent pregnancy (0/1). Four and 7% of Peruvian women respectively reported having these symptoms at or after last pregnancy (Table 1). Because some women who experience postpartum hemorrhaging do so as the result of detectable risk factors (Combs, Murphy and Laros Jr 1991), I also predict postpartum hemorrhaging at last pregnancy (0/1). Likewise, because high blood pressure during pregnancy is a detectable and treatable risk factor for convulsions, I also predict convulsions during last pregnancy (0/1). These latter two complications are more prevalent than fevers—15% and 18% of women reported hemorrhaging and convulsing, respectively, at last pregnancy. As a falsification test, I examine one maternal condition that should not be affected by prenatal healthcare utilization—mastitis (0/1).5
Table 1.
Current Fertility Practices, Utilization of Healthcare at Last Pregnancy, and Complications During and After Last Pregnancy in Peruvian Demographic and Health Survey
| Percent | |
|---|---|
| Complications during and after last pregnancy | |
| Fever, vaginal bleeding during pregnancy | 4 |
| Fever after pregnancy | 7 |
| Excessive bleeding during pregnancy | 15 |
| Convulsions | 18 |
| Mastitis | 8 |
| Fertility Outcomes | |
| Currently using modern contraception | 33 |
| Currently using LARC | 13 |
| Any birth interval <15mos in five years before survey | 14 |
| Last pregnancy unwanted | 26 |
| Utilization of healthcare at last pregnancy | |
| Any antenatal visits | 97 |
| First antenatal visit in first-trimester | 74 |
| Iron supplements | 77 |
| Delivery in healthcare center | 80 |
Current fertility practices
To understand how education affects maternal health I explore women’s fertility practices and healthcare utilization. The former is measured through contraceptive use, birth spacing, and unintended pregnancy. I operationalize contraceptive use with two dichotomous indicators, one that denotes whether a woman was using any form of modern contraception at survey (0/1),6 and one that denotes whether she was using a long-acting reversible form of contraception (an IUD or injectable) (0/1). Thirty-three percent of respondents in the DHS reported using a modern form of contraception at survey; 13% reported using LARCs specifically (Table 1).
Birth spacing is operationalized with a dichotomous measure of whether a mother reported two births within fifteen months of each other in the five years before survey (questions about spacing were not asked about births beyond these five years). This emphasis on fifteen months reflects the World Health Organization’s recommendations to reduce the risk of complications (WHO 2006). Fourteen percent of women reported having two births within fifteen months of each other in the last five years (Table 1).
Finally, because unintended pregnancies may lead women to seek unsafe abortions (Singh 2006), and unsafe abortion is one of the major causes of maternal mortality in Peru (Amnesty International 2009), I test a measure of whether respondents’ last pregnancy was unwanted, where (1) denotes that the respondent wanted no more pregnancies at the time she became pregnant and (0) denotes that she wanted the pregnancy at that time or at a later date. Twenty-six percent of women in the DHS reported that they did not want any more pregnancies when they last became pregnant.
Antenatal healthcare utilization at last pregnancy
To assess antenatal healthcare, I predict whether or not a respondent attended any antenatal visits at a healthcare facility (0/1); attended an antenatal visit during her first trimester (0/1); consumed an iron supplement during pregnancy (0/1); and delivered her baby in a hospital or clinic (public or private) (0/1). On the whole, many women reported utilizing maternal healthcare in Peru. For instance, 97% reported attending at least one antenatal visit; 80% reported that their last birth took place in a hospital or clinic (Table 1).
Potential Mechanisms
The final analytical component explores three underlying pathways by which women’s education may affect fertility practices and healthcare utilization, and implicitly maternal health. The first is cognitive skills, proxied only by literacy in the Peruvian DHS. Literacy was assessed by asking all respondents to read the same sentence. I define literate as (1) if a respondent was able to read the entire sentence and (0) if she was not. Ninety-one percent of respondents were literate.
The second is economic resources. The DHS does not include questions about income. Instead, I assess economic resources with a measure of respondent’s employment in the last twelve months (0/1). Seventy-five percent of DHS respondents were employed within the year before survey. Among these respondents, I test a measure of occupational status based on Treiman’s (1976) Occupational Prestige Scale (ranging 1–8). For all respondents in the sample, I also test a standardized measure of household wealth created by the DHS, based on household assets and durable goods. This measure is divided into quintiles and captures households’ wealth relative to other households in the survey. The last measure of economic resources is a dichotomous indicator of whether a respondent reported having health insurance at survey (0/1).
The third and final pathway is respondents’ autonomy, which I operationalize as whether respondents reported making decisions about their own healthcare. Respondents who reported participating in these decisions (alone or with someone else) are coded (1); respondents who did not are coded (0). Only 22% of DHS respondents reported not being involved in decisions about their own healthcare.
Instrumented Regression Discontinuity
To estimate the effects of women’s education on maternal health, I utilize an instrumented regression discontinuity (RD). In naïve OLS models, education partially captures unobservable characteristics that contribute to both educational attainment and health risks. For example, poverty may require women to leave school early in search of paid labor and may also inhibit women’s ability to pay for healthcare. Because poverty affects both years of education and healthcare utilization, estimates of the effects of education on healthcare would be downwardly biased in OLS models. RDs are free of such bias because they compare two groups that fall just above and just below an exogenously determined threshold that affects years of education. In this study the threshold is age 11 in 1993: women who were ages 11 and younger in 1993 should have been exposed to CS11 because they were still of primary school age when it was implemented; women who were ages 12 and older in 1993 should not have been exposed because they should not have been enrolled in primary school at the time of implementation (Figure 2).
Because women who were age 11 in 1993 should be very similar to women who were age 12 in 1993 (Appendix A), comparing the two groups should implicitly control for all unobservable characteristics. However, in Peru, grade repetition and delayed school entry are common (Pal 2004). Thus some women who were older than 11 in 1993 were still enrolled in primary school, exposed to CS11, and mandated to complete 11 years of schooling despite that this was not the case for the majority of their birth cohort. Likewise, because compulsory schooling is difficult to enforce, some women exposed to CS11 may have dropped out before they reached their required 11 years of schooling. Because I cannot know whether each individual woman was or was not still completing her first six years of schooling at the time of CS11 implementation, I exploit discontinuities in the probability of CS11 exposure given birth cohort. To do so, I use a two-stage least squares (2SLS) estimator in which I instrument years of education with birth cohort. In the first stage I regress years of schooling, D, on birth cohort (e.g. CS11 exposure at <=11years) Z (Equation 1).
| (1) |
Then, in the second stage, I regress the outcome, Y, on predicted values of D generated in the first stage (Equation 2).
| (2) |
Put simply, this two-stage model uses birth cohort (a proxy for CS11 exposure) to predict a woman’s number of years of education and then uses this estimate of education to predict maternal health outcomes. In all models, I adjust for appropriate characteristics of respondents’ childhood background, including respondents’ ethnolinguistic group (Spanish, Quechua, Aymara, or other indigenous group); childhood location (state capital, city, town, or rural); number of siblings (0 to 17); and whether the respondent grew up in a violent household (a proxy for a turbulent household environment). Although no measure of childhood poverty is available in the DHS, the combination of ethnolinguistic group and childhood location should capture some of the variance related to childhood socioeconomic status. Given that CS11 likely induced a larger change among women at the lower end of the education distribution, who tended to be rural and poorer (UNECOSOC 2011; UNESCO 2014), adjusting for these characteristics both improves the precision of model estimates and helps to produce a consistent estimator. All models also adjust for respondents’ current state of residence but do not adjust for other characteristics that could have occurred after school completion because the causal ordering between these characteristics and the dependent variables cannot be known (Gelman and Hill 2007).
Several assumptions are inherent to instrumented RDs. The first is that the instrument affects treatment assignment, e.g. that, on average, exposure to CS11 affects women’s years of schooling. This means that the effects of this instrumented RD are only generalizable to women for whom the policy induced a change in schooling. A second assumption, known as the exclusion restriction, is that the only way the instrument can affect the outcome is via the treatment. If there were other plausible pathways between the instrument and the outcome then there would be no way to isolate the effects of education. However, it is unlikely there were other avenues by which exposure to the CS11 policy would have increased maternal health other than through schooling.
Third, the instrument is assumed to be exogenous (Angrist and Imbens 1995). Besides the fact that the policy was implemented 9 to 14 years after respondents were born, and that parents were therefore unlikely to manipulate the timing of births in anticipation of the reform, t-tests and chi-square tests comparing means and proportions of observable background characteristics between the unexposed and exposed groups yield null results (Appendix A), suggesting that there was no systematic selection into CS11 exposure. A manipulation test based on local polynomial density estimation (McCrary 2008), which yields null results (p=0.6), further confirms that the density of observations on either side of the threshold are equivalent. Moreover, to ensure that the instrument is determined independently of both the outcomes and the treatment, I limit my analysis to a narrow band of cohorts—three years above and below the CS11 age cutoff in 1993. As a robustness check, I run more conservative models in which the sample is restricted to women within two years of the CS11 age cutoff in 1993. The results lead to substantively similar conclusions to those of the primary analyses (results available upon request).
Fourth, the jump in education associated with CS11 exposure is assumed to capture a true discontinuity, rather than a time trend that may have affected cross-cohort changes independently of education reform. I test this possibility in two ways. First, I rerun all models controlling for birth cohort. With the exception of one point estimate,7 the results remain similar in terms of magnitude, direction, and significance (available upon request), thus confirming that the results presented below are not systematically biased by independent changes in health outcomes across cohorts. Second, I conduct a placebo test of the first stage, comparing the adjusted years of schooling for women who were aged 12 to 14 in 1993 to women who were aged 15 to 17 in 1993. Because neither group should have been exposed to CS11 there should be no significant difference in their years of schooling. As expected, the results of this placebo test were null.
Results of Instrumented Regression Discontinuity Analyses
First-Stage Results
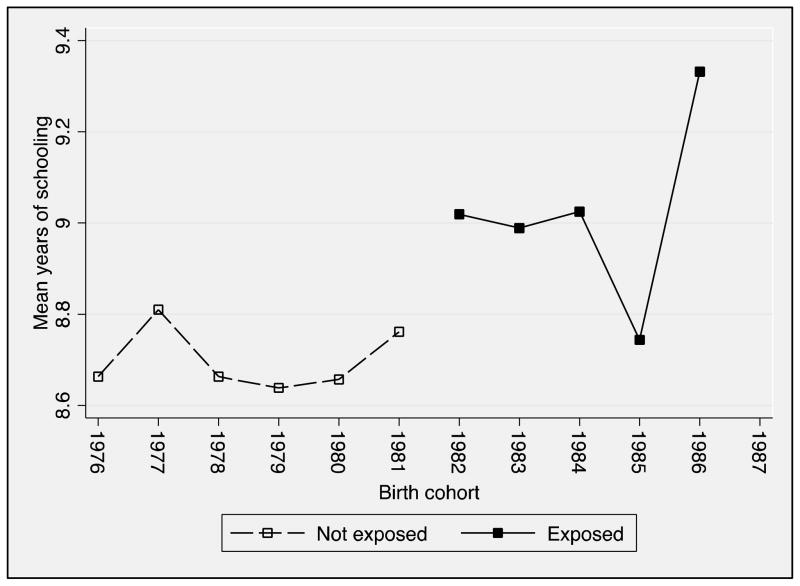
For CS11 exposure to be a valid instrument for women’s education, it must be strongly predictive of years of schooling. Specifically, the validity of the instrument rests on CS11 exposure having a t-value greater than 3.2 or a corresponding p-value below 0.0016; and an F statistic for the excluded instrument above 10 (Stock, Wright and Yogo 2002). Table 2 presents the results of the first-stage model estimating the relationship between respondents’ CS11 exposure and highest year of education. The results of this first-stage indicate that women who were exposed to CS11 had an average of 0.32 more years of formal education than women who were not exposed (p<.001). The F-test for the excluded instrument (F=47.21, p<.001) also confirmed that the relationship between CS11 exposure and years of education is sufficiently strong for CS11 to serve as a valid instrument. Figure 3 presents a visual representation of mothers’ average years of schooling by birth cohort.
Table 2.
First-Stage Regression Estimates Predicting the Number of Years of Schooling Completed
| Exposed to CS11 | 0.32*** (0.10) |
| No. of siblings | −0.20*** (0.02) |
| Childhood residence (ref: large city): | |
| Small city | −0.63*** (0.16) |
| Town | −1.87*** (0.15) |
| Countryside | −3.58*** (0.15) |
| Ethnolinguistic group (ref: Spanish) | |
| Quechua | −2.78*** (0.22) |
| Aymara or other | −0.87* (0.34) |
| Grew up in violent household | 0.10 (0.10) |
| Constant | 11.07*** (0.28) |
| Observations | 4,495 |
| R-squared | 0.35 |
Note: Model also adjusts for state of residence (complete table available upon request).
Robust standard errors, clustered by survey cluster, in parentheses
p<0.001,
p<0.01,
p<0.05,
p<0.10
Figure 3. Average Years of Schooling Among Mothers in the DHS, by Birth Cohort.
Note: Figure based on author’s own calculations using DHS data from 2003–2010.
Second Stage Results of the Effect of Education on Complications During Last Pregnancy
In the second stage, I regress semi-preventable pregnancy complications on the predicted value of education taken from the first stage. The results in the first two columns of Table 3 suggest that increasing women’s education by one year reduced the probability of fever accompanied by vaginal bleeding during pregnancy by 1 percentage point (p<.05) and the probability of fever after birth by 2 percentage points (p<.05). To place the magnitude of these effects in context, a 1 percentage point decrease in fever with vaginal bleeding during pregnancy is equivalent to a 25% decrease compared to the average Peruvian woman’s probability; a 2 percentage point decrease in fever after birth is equivalent to a 29% decrease compared to the average woman. Moreover, increasing women’s education had a weak negative effect on postpartum hemorrhaging, decreasing its probability by 2 percentage points (p<.1). However, women’s education had no significant effect on convulsions despite that the direction of the effect estimate is in the expected, negative direction. In the falsification test, increasing women’s education had no effect on mastitis (an unpreventable condition).
Table 3.
Second-Stage Regression Estimates Predicting Complications During and After Last Pregnancy
| Preventable
|
Semi-preventable
|
Not preventable (falsification test)
|
|||
|---|---|---|---|---|---|
| Fever, vaginal bleeding during pregnancy | Fever after pregnancy | Excessive bleeding during pregnancy | Convulsions | Mastitis | |
| Years of education | −0.01* (0.005) | −0.02* (0.01) | −0.02† (0.01) | −0.01 (0.003) | −0.01 (0.01) |
| Constant | 0.12* (0.05) | 0.40*** (0.10) | 0.34*** (0.10) | 0.05 (0.04) | 0.27*** (0.08) |
| N | 4,495 | 4,495 | 4,495 | 4,494 | 4,495 |
Note: All models adjust for childhood residence, ethnolinguistic group, and state of residence (complete table available upon request).
Robust standard errors, clustered by survey cluster, in parentheses
p<0.001,
p<0.01,
p<0.05,
p<0.10
Second Stage Results of the Effect of Education on Current Fertility Practices and Antenatal Healthcare Utilization at Last Pregnancy
I next investigate two avenues by which education may influence maternal health: fertility practices and antenatal healthcare utilization. Starting with the former, the results in Table 4 indicate that a one-year increase in mothers’ education increased the probability of modern contraceptive use at survey by 3 percentage points (p<.05), but had no effect on LARC use specifically. Consistent with the positive effect of education on modern contraceptive use, increasing education by one year decreased the probability of having two births within fifteen months of each other by 4 percentage points (p<.05), a reduction of 29% from the mean in Peru; and further reduced the probability that a woman’s last pregnancy was reported as unwanted by 3 percentage points (p<.01), a reduction of 12% from the mean.
Table 4.
Second-Stage Regression Estimates Predicting Current Fertility Practices
| Currently using modern contraception | Currently using LARC | Any birth interval <15mos in five years before surveya | Last pregnancy unwanted | |
|---|---|---|---|---|
| Years of education | 0.03* (0.01) | 0.02 (0.01) | −0.04** (0.01) | −0.03** (0.01) |
| Constant | 0.26† (0.14) | 0.05 (0.13) | 0.42** (0.12) | 0.42*** (0.11) |
| N | 4,495 | 4,495 | 3,068 | 4,495 |
Note: All models adjust for childhood residence, ethnolinguistic group, and state of residence (complete table available upon request).
Birth spacing is only estimated among women who have had 2 or more births in the five years before survey.
Robust standard errors, clustered by survey cluster, in parentheses
p<0.001,
p<0.01,
p<0.05,
p<0.10
Moving to antenatal healthcare, Table 5 presents second-stage regression estimates. The results in the first two columns suggest that increasing women’s education by one year increased their probabilities of attending at least one antenatal checkup during their last pregnancy and of attending one in their first trimester specifically by 1 (p<.05) and 4 (p<.01) percentage points, respectively. This increase in visits to healthcare facilities may have presented important opportunities for respondents to determine their risk of complications during pregnancy or childbirth and to take informed, preventative measures to protect their health. Despite this possibility, the results in the third column suggest that women’s education had no effect on their consumption of iron supplements at last pregnancy. Nevertheless, increasing women’s education by one year heightened their probability of delivering their last birth in a healthcare center by 4 percentage points (p<.001).
Table 5.
Second-Stage Regression Estimates Predicting Utilization of Reproductive Healthcare Service at Last Pregnancy
| Any antenatal healthcare visits | First visit in first trimester | Iron supplements | Delivery in healthcare center | |
|---|---|---|---|---|
| Years of education | 0.01* (0.005) | 0.04** (0.01) | 0.01 (0.01) | 0.04*** (0.01) |
| Constant | 0.89*** (0.05) | 0.36** (0.12) | 0.76*** (0.12) | 0.37*** (0.11) |
| N | 4,490 | 4,351 | 4,495 | 4,495 |
Note: All models adjust for childhood residence, ethnolinguistic group, and state of residence (complete table available upon request).
Robust standard errors, clustered by survey cluster in parentheses
p<0.001,
p<0.01,
p<0.05,
p<0.10
Second Stage Results Investigating Potential Mechanisms
Table 6 explores the mechanisms that may underlie the relationship between women’s education, fertility processes, and antenatal healthcare. The first of these mechanisms is literacy, a proxy for women’s cognitive skills. The results presented in Table 6 confirm that a one-year increase in women’s schooling increased the probability of literacy by 2 percentage points (p<.05).
Table 6.
Second-Stage Regression Estimates Predicting Indicators of Potential Mechanisms
| Cognitive skills
|
Economic resources
|
Autonomy
|
||||
|---|---|---|---|---|---|---|
| Literate | Employed | Occupational status | Household wealth | Has health insurancea | Decides own healthcareb | |
| Years of education | 0.02* (0.01) | −0.00 (0.01) | 0.44*** (0.07) | 0.21*** (0.02) | 0.04* (0.01) | 0.04*** (0.01) |
| Constant | 0.83*** (0.08) | 0.72*** (0.12) | −0.22 (0.76) | 0.76** (0.24) | 0.05 (0.15) | 0.44*** (0.11) |
| N | 4,494 | 4,494 | 3,049 | 4,495 | 4,051 | 4,425 |
Note: All models adjust for childhood residence, ethnolinguistic group, and state of residence (complete table available upon request).
Occupational status is only estimated among employed respondents.
Participation in decisions about healthcare was not assessed in 2009, resulting in the exclusion of 99 respondents from this model.
Robust standard errors, clustered by survey cluster, in parentheses
p<0.001,
p<0.01,
p<0.05,
p<0.10
The second is economic resources. Here the results indicate that women’s education had no effect on their employment (Table 1) but that among employed women, increasing education by one year increased occupational status by an average of 0.44 points (p<.001, equivalent to a 6% increase on the 8-point scale). In accord with this latter finding, increasing women’s education by one year increased their household wealth by 0.21 points (p<.001) and their probability of being insured by 4 percentage points (p<.05).
Finally, the last proposed mechanism is women’s autonomy. The results presented in the last column of Table 6 indicate that each one-year increase in respondents’ education resulted in a four percentage point higher probability of making decisions about their own healthcare (p<.001; an 18% increase compared to the DHS sample mean).
Comparisons with Naïve OLS estimates
To highlight the importance of isolating the effects of education I compare the results of RD analyses to those of naïve OLS models (Appendix B). On the one hand, these naïve results suggest an effect of education on any antenatal visits that is more than two times the magnitude of the effect estimated by the RD model (Table 5). On the other hand, they suggest no effect of education on fevers during or immediately following pregnancy. This contradiction highlights how unobservable factors simultaneously contributing to educational attainment, healthcare use, and health outcomes bias results, leading them to be less consistent. Further illustrating this problem is the significant, positive effect of education on mastitis estimated by the naïve OLS model. Mastitis cannot be anticipated and is not contingent on detectable risk factors earlier in pregnancy. As such, education should not affect its probability. Instead, the positive effect estimated by the naïve model may reflect that unobservable factors contributing to women’s education must also contribute to women’s probability of surviving the infection (and thus being able to report it at survey).
Limitations
Despite its merits, this study faces several limitations. One is that the only measure of cognitive skills in the DHS—literacy—is basic and exhibits little variation across women. Further analyses are therefore needed to verify the extent to which cognitive skills are a plausible driver of changes in women’s fertility practices, healthcare use, and maternal health. Another limitation is that DHS data do not provide a full employment history. This prevents me from controlling for childhood labor force participation and from testing whether education reform may have affected maternal health via changes in women’s labor force participation as children.
Discussion
This study expands existing scholarship by using an exogenous source of variation to demonstrate a causal link between women’s schooling and maternal health. The observed protective effects of education against complications such as fevers and hemorrhaging have important implications for women’s risk of disability, morbidity, and mortality over the course of their reproductive years. In the aggregate, these effects may contribute to falling maternal mortality rates and extend women’s life expectancy.
To better understand the maternal health advantage enjoyed by women with greater education, this study investigated two interrelated pathways: women’s fertility practices and use of antenatal healthcare. The results yielded evidence in support of both pathways, suggesting that education increases modern contraceptive use and relatedly reduces the probability of short birth spacing and unwanted pregnancies; and increases women’s antenatal healthcare visits and deliveries in formal healthcare centers. The former should benefit maternal health by preventing conditions that contribute to pregnancy complications (Trussel and Pebley 1984; WHO 2006b) and by reducing the number of pregnancies for which women have cause to seek unsafe abortions (which are illegal under most circumstances in Peru). The latter should improve maternal health by increasing the prevention or early detection of pregnancy complications and/or providing treatment once complications arise.
Moving further back in the causal chain, this study also provided suggestive evidence that the health benefits of education stem from improvements to women’s cognitive skills, economic status, and autonomy. These additional benefits of education may explain how and why education influences fertility practices, healthcare use, and ultimately, maternal morbidity. The extent to which each of these pathways uniquely mediates the effects of education remains a question for future research, and will be especially important for scholars to consider in low and middle-income settings amidst stalled demographic and health transitions.
This study’s findings have important policy implications. By investing in women’s and girl’s education, policymakers can enhance women’s use of reproductive and maternal healthcare, and in this way, advance health transitions. Furthermore, simultaneously increasing women’s education and improving their health should have long-term financial benefits such as reducing expenditure on medical emergencies.
Though this study focuses on the specific case of Peru, it clearly identifies the protective value that women’s formal schooling has on maternal health in a low-income, high-risk context. Moreover, given the relatively poor quality of schooling in Peru (World Bank 2007), the effects of education on maternal health may be even larger in neighboring contexts with comparatively higher quality schools. Additional studies investigating the effects of education on maternal health in other country contexts, such as Brazil or Colombia, where compulsory schooling has more recently been implemented (Los Angeles Times 2010; Reimers 2006; World Bank 2006), are needed to understand whether and how the effects of women’s education vary with school quality and with broader sociocultural and political characteristics. Nevertheless, the results presented here provide important new evidence that extending women’s formal schooling protects their health and improves their longevity throughout their reproductive years.
Highlights.
This study investigates the causal effect of education on maternal health.
The study employs increased compulsory schooling in Peru as a natural experiment.
Improving women’s education reduces the risk of select maternal complications.
Education has the strongest protective effect on preventable conditions like fever.
Women’s education has corresponding effects on their fertility and healthcare use.
Acknowledgments
The author would like to thank Julia Behrman, Liz Ela, and Anne Clark for their invaluable feedback on earlier drafts of this paper.. This research was made possible with the support of an NIA training grant (T32 AG000221).
Appendix A. Descriptive Statistics for Treatment and Control Samples
| Not exposed to 11-year compulsory schooling at age 11 (N=3,083)
|
Exposed to 11-year compulsory schooling at age 11 (N=2,358)
|
Results of t-test and chi-square tests | |||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Number of siblings | 5.52 | 2.88 | 5.35 | 2.93 | |
| Childhood residence: state capital | .31 | .31 | |||
| Childhood residence: city | .16 | .15 | |||
| Childhood residence: town | .20 | .20 | |||
| Childhood residence: rural area | .33 | .34 | |||
| Ethnolinguistic group: Spanish | .89 | .90 | |||
| Ethnolinguistic group: Quechua | .09 | .08 | |||
| Ethnolinguistic group: Aymara or other | .02 | .02 | |||
| Grew up in a violent household | .48 | .48 | |||
Note:
p<0.001,
p<0.01,
p<0.05,
p<0.10
Appendix B. Naïve OLS Regression Estimates
| Fever, vaginal bleeding during preg. | Fever after preg. | Excessive bleeding during preg. | Convulsions | Mastitis | Currently using modern contra. | Currently using LARC | Any birth interval <15mos in five years before survey | Last pregnancy unwanted | Any antenatal healthcare visits | First visit in first trimester | Iron supp. | Delivery in healthcare center | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Years of education | −0.001 (0.001) | 0.002 (0.002) | −0.003† (0.002) | −0.0003 (0.001) | 0.005*** (0.001) | 0.003 (0.002) | −0.005* (0.002) | −0.01*** (0.002) | −0.02*** (0.002) | 0.004*** (0.001) | 0.01*** (0.002) | 0.01*** (0.002) | 0.02*** (0.002) |
| Constant | 0.02 (0.01) | 0.15*** (0.03) | 0.19*** (0.04) | −0.002 (0.01) | 0.12*** (0.03) | 0.49*** (0.04) | 0.29*** (0.04) | 0.14*** (0.03) | 0.38*** (0.03) | 0.95*** (0.02) | 0.67*** (0.04) | 0.72*** (0.05) | 0.57*** (0.05) |
| N | 4,495 | 4,495 | 4,495 | 4,494 | 4,495 | 4,495 | 4,495 | 3,068 | 4,495 | 4,490 | 4,351 | 4,495 | 4,495 |
Note: All models adjust for childhood residence, ethnolinguistic group, and state of residence (complete table available upon request).
Robust standard errors, clustered by survey cluster, in parentheses
p<0.001,
p<0.01,
p<0.05,
p<0.10
Footnotes
Semi-preventable refers to conditions that can be detected and managed before they become life threatening.
Maternal mortality is defined as death during or within 42 days after pregnancy owing to pregnancy-related conditions (Say et al. 2014).
Between 1990 and 2000, the amount of public funds spent per student actually declined by 40% (Ministerio de Educación 2007, p.26).
DHS data from 2010–2012 are not included because they do not provide pertinent maternal health measures.
Less than 1% of respondents report never breastfeeding. Rerunning analyses without these women yields nearly identical results. The DHS includes several other maternal health indicators. These indicators are not analyzed for theoretical reasons: either they should not be affected by education or the expected direction is ambiguous.
Modern contraception is defined as oral contraceptives, implants, injectables, intrauterine devices, male or female condoms or sterilization, lactational amenorrhea, and emergency contraception (WHO 2015).
The estimate loses its statistical significance but remains similar with regard to direction and magnitude.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Development of Education. Paris: UNESCO and the Peruvian Ministry of Education; 2001. National Report of the Republic of Peru. [Google Scholar]
- Informe de Progreso Educativo. Lima, Peru: Grupo de Análisis para el Desarollo (GRADE); 2003. [Google Scholar]
- di Gropello Emanuela., editor. Meeting the Challenges of Secondary Education in Latin America and East Asia. Washington D.C: World Bank; 2006a. [Google Scholar]
- Report of a WHO Technical Consultation on Birth Spacing. Geneva: World Health Organization; 2006b. [Google Scholar]
- Plan Estratégico Institucional. Lima, Peru: Ministerio de Educación; 2007a. [Google Scholar]
- Toward High-Quality Education in Peru: Standards, Accountability, and Capacity Building. Wahington, D.C: The World Bank/The International Bank for Reconstruction and Development; 2007b. [Google Scholar]
- Fatal Flaws: Barriers to Maternal Health in Peru. London: Amnesty International; 2009. [Google Scholar]
- Los Angeles Times. Los Angeles: 2010. Educating All in Colombia. [Google Scholar]
- Challenges for Education with Equity in Latin America and the Caribbean: Regional Preparatory Meeting. Buenos Aires: UNECOSOC; 2011a. [Google Scholar]
- Estudios y Experiencias. Lima, Peru: Instituto Peruano de Evaluación, Acreditación y Certificación de la Calidad de la Educación Básica (IPEBA); 2011b. Ruralidad y Escuela: Apuntes para la Acreditación de Instituciones Educativas en Áeas Rurales. [Google Scholar]
- Regional Report about Education for All in Latin America and the Caribbean. Santiago: UNESCO; 2014a. [Google Scholar]
- School enrollment, secondary (% gross) World Bank; Washington D.C: 2014b. [Google Scholar]
- Family Planning/Contraception Factsheet no. 351. Geneva: World Health Organization; 2015a. [Google Scholar]
- Maternal mortality ratio (modeled estimate, per 100,000 live births) Washington D.C: World Bank; 2015b. [Google Scholar]
- Making Development Happen. Lima, Peru: Organisation for Economic Cooperatoin and Development (OECD); 2016. Avanzando Hacia Una Mejor Educación para Perú. [Google Scholar]
- Ahmed Saifuddin, Creanga Andreea A, Gillespie Duff G, Tsui Amy O. Economic status, education and empowerment: implications for maternal health service utilization in developing countries. PLoS ONE. 2010;5(6):e11190. doi: 10.1371/journal.pone.0011190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ames Patricia, Rojas Vanessa. Young Lives. Lima, Peru: Grupo de Análisis para el Desarollo (GRADE) Niños del Milenio; 2011. Cambios y oportunidades: La transición de la escuela primaria a la secundaria en el Perú. [Google Scholar]
- Angeles Gustavo, Guilkey David K, Mroz Thomas A. The Determinants of Fertility in Rural Peru: Program Effects in the Early Years of the National Family Planning Program. Journal of Population Economics. 2005;18(2):367–89. [Google Scholar]
- Angrist Joshua D, Imbens Guido W. Two-stage least squares estimation of average causal effects in models with variable treatment intensity. Journal of the American Statistical Association. 1995;90(430):431–42. [Google Scholar]
- Baird Sarah, Chirwa E, Alison McIntosh C, Ozler B. The short-term impacts of a schooling conditional cash transfer program on the sexual behavior of young women. Health Economics. 2010;19:55–68. doi: 10.1002/hec.1569. [DOI] [PubMed] [Google Scholar]
- Barber Jennifer S. Ideational Influences on the Transition to Parenthood: Attitudes toward Childbearing and Competing Alternatives. Social Psychology Quarterly. 2001;64(2):101–27. [Google Scholar]
- Behrman Julia Andrea. Does Schooling Affect Women’s Desired Fertility? Evidence From Malawi, Uganda, and Ethiopia. Demography. 2015a:1–23. doi: 10.1007/s13524-015-0392-3. [DOI] [PubMed] [Google Scholar]
- Behrman Julia Andrea. The effect of increased primary schooling on adult women’s HIV status in Malawi and Uganda: Universal Primary Education as a natural experiment. Social Science & Medicine. 2015b;127:108–15. doi: 10.1016/j.socscimed.2014.06.034. [DOI] [PubMed] [Google Scholar]
- Breierova Lucia, Duflo Esther. The impact of education on fertility and child mortality: Do fathers really matter less than mothers? National Bureau of Economic Research; 2004. [Google Scholar]
- Carroli Guillermo, Rooney Cleone, Villar Jose. How effective is antenatal care in preventing maternal mortality and serious morbidity? An overview of the evidence. Paediatric and Perinatal Epidemiology. 2001;15(s1):1–42. doi: 10.1046/j.1365-3016.2001.0150s1001.x. [DOI] [PubMed] [Google Scholar]
- Combs C Andrew, Murphy Edward L, Laros Russell K., Jr Factors associated with postpartum hemorrhage with vaginal birth. Obstetrics & Gynecology. 1991;77(1):69–76. [PubMed] [Google Scholar]
- Conde-Agudelo Agustin, Rosas-Bermúdez Anyeli, Kafury-Goeta Ana C. Effects of birth spacing on maternal health: a systematic review. American Journal of Obstetrics & Gynecology. 2007;196(4):297–308. doi: 10.1016/j.ajog.2006.05.055. [DOI] [PubMed] [Google Scholar]
- De Neve Jan-Walter, Fink Günther, Subramanian SV, Moyo Sikhulile, Bor Jacob. Length of secondary schooling and risk of HIV infection in Botswana: evidence from a natural experiment. The Lancet Global Health. 2015;3(8):e470–e77. doi: 10.1016/S2214-109X(15)00087-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duflo Esther. Schooling and Labor Market Consequences of School Construction in Indonesia: Evidence from an Unusual Policy Experiment. American Economic Review. 2001;91(4):795–813. [Google Scholar]
- Duley Lelia. Maternal mortality associated with hypertensive disorders of pregnancy in Africa, Asia, Latin America and the Caribbean. BJOG: An International Journal of Obstetrics & Gynaecology. 1992;99(7):547–53. doi: 10.1111/j.1471-0528.1992.tb13818.x. [DOI] [PubMed] [Google Scholar]
- Falkingham Jane. Inequality and changes in women’s use of maternal Health-care services in tajikistan. Studies in Family Planning. 2003;34(1):32–43. doi: 10.1111/j.1728-4465.2003.00032.x. [DOI] [PubMed] [Google Scholar]
- Freeburger Adela R, Hauch Charles C. In: Education in Peru. Celebreeze Anthony J, Keppel Francis., editors. Washington D.C: U.S. Department of Health, Education, and Welfare; 1964. [Google Scholar]
- Fuller Norma. The social constitution of gender identity among Peruvian men. Men and Masculinities. 2001;3(3):316–31. [Google Scholar]
- Gelman Andrew, Hill Jennifer. Data Analysis Using Regression and Multilevel/Hierarchical Models. Cambridge: Cambridge University Press; 2007. [Google Scholar]
- Graham Wendy J, Bell Jacqueline S, Bullough Colin HW. Can skilled attendance at delivery reduce maternal mortality in developing countries. Safe motherhood strategies: a review of the evidence. 2001;17:97–130. [Google Scholar]
- Grépin Karen Ann, Bharadwaj Prashant. Maternal education and child mortality in Zimbabwe. Journal of Health Economics. 2015;44:97–117. doi: 10.1016/j.jhealeco.2015.08.003. [DOI] [PubMed] [Google Scholar]
- Karlsen Saffron, Say Lale, Souza João-Paulo, Hogue Carol J, Calles Dinorah L, Metin Gülmezoglu A, Raine Rosalind. The relationship between maternal education and mortality among women giving birth in health care institutions: analysis of the cross sectional WHO Global Survey on Maternal and Perinatal Health. BMC Public Health. 2011;11(1):1. doi: 10.1186/1471-2458-11-606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassebaum Nicholas J, Bertozzi-Villa Amelia, Coggeshall Megan S, Shackelford Katya A, Steiner Caitlyn, Heuton Kyle R, Gonzalez-Medina Diego, Barber Ryan, Huynh Chantal, Dicker Daniel. Global, regional, and national levels and causes of maternal mortality during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet. 2014;384(9947):980–1004. doi: 10.1016/S0140-6736(14)60696-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kowalewski Marga, Jahn Albrecht. Health professionals for maternity services: Experiences on covering the population with quality maternity care. Safe motherhood strategies: a review of the evidence 2000 [Google Scholar]
- Lundberg Shelly, Pollak Robert A. Separate Spheres Bargaining and the Marriage Market. The Journal of Political Economy. 1993;101(6):988–1010. [Google Scholar]
- Martin Teresa Castro, Juarez Fatima. The impact of women’s education on fertility in Latin America: Searching for explanations. International Family Planning Perspectives. 1995:52–80. [Google Scholar]
- McCarthy James, Maine Deborah. A framework for analyzing the determinants of maternal mortality. Studies in Family Planning. 1992;23(1):23–33. [PubMed] [Google Scholar]
- McCrary Justin. Manipulation of the running variable in the regression discontinuity design: A density test. Journal of econometrics. 2008;142(2):698–714. [Google Scholar]
- Onah Hyacinth Eze, Ikeako Lawrence C, Iloabachie Gabriel C. Factors associated with the use of maternity services in Enugu, southeastern Nigeria. Social Science & Medicine. 2006;63(7):1870–78. doi: 10.1016/j.socscimed.2006.04.019. [DOI] [PubMed] [Google Scholar]
- Pal Sarmistha. Child schooling in Peru: Evidence from a sequential analysis of school progression. Journal of Population Economics. 2004;17(4):657–80. [Google Scholar]
- Psacharopoulos George, Patrinos Harry Anthony. Returns to investment in education: a further update. Education Economics. 2004;12(2):111–34. [Google Scholar]
- Raghupathy Shobana. Education and the use of maternal health care in Thailand. Social Science & Medicine. 1996;43(4):459–71. doi: 10.1016/0277-9536(95)00411-4. [DOI] [PubMed] [Google Scholar]
- Reimers Fernando. Education and Social Progress. In: Bulmer-Thomas Victor, Coatsworth John, Cortes-Conde Roberto., editors. The Cambridge Economic History of Latin America. Cambridge: Cambridge University Press; 2006. [Google Scholar]
- Rose Sally B, Lawton Beverley A. Impact of long-acting reversible contraception on return for repeat abortion. American Journal of Obstetrics and Gynecology. 2012;206(1):37. e1–37. e6. doi: 10.1016/j.ajog.2011.06.102. [DOI] [PubMed] [Google Scholar]
- Rush David. Nutrition and maternal mortality in the developing world. The American Journal of Clinical Nutrition. 2000;72(1):212s–40s. doi: 10.1093/ajcn/72.1.212S. [DOI] [PubMed] [Google Scholar]
- Say Lale, Chou Doris, Gemmill Alison, Tunçalp Özge, Moller Ann-Beth, Daniels Jane, Metin Gülmezoglu A, Temmerman Marleen, Alkema Leontine. Global causes of maternal death: a WHO systematic analysis. The Lancet Global Health. 2014;2(6):e323–e33. doi: 10.1016/S2214-109X(14)70227-X. [DOI] [PubMed] [Google Scholar]
- Scholl Theresa O, Reilly Thomas. Anemia, Iron and Pregnancy Outcome. The Journal of Nutrition. 2000;130(2):443. doi: 10.1093/jn/130.2.443S. [DOI] [PubMed] [Google Scholar]
- Shen Ce, Williamson John B. Maternal mortality, women’s status, and economic dependency in less developed countries: a cross-national analysis. Social Science & Medicine. 1999;49(2):197–214. doi: 10.1016/s0277-9536(99)00112-4. [DOI] [PubMed] [Google Scholar]
- Sibai Baha, Dekker Gus, Kupferminc Michael. Pre-eclampsia. The Lancet. 2005;365(9461):785–99. doi: 10.1016/S0140-6736(05)17987-2. [DOI] [PubMed] [Google Scholar]
- Singh Susheela. Hospital admissions resulting from unsafe abortion: estimates from 13 developing countries. The Lancet. 2006;368(9550):1887–92. doi: 10.1016/S0140-6736(06)69778-X. [DOI] [PubMed] [Google Scholar]
- Smith-Greenaway Emily. Maternal reading skills and child mortality in Nigeria: a reassessment of why education matters. Demography. 2013;50(5):1551–61. doi: 10.1007/s13524-013-0209-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stock James H, Wright Jonathan H, Yogo Motohiro. A survey of weak instruments and weak identification in generalized method of moments. Journal of Business & Economic Statistics. 2002;20(4) [Google Scholar]
- Thaddeus Sereen, Maine Deborah. Too far to walk: maternal mortality in context. Social Science & Medicine. 1994;38(8):1091–110. doi: 10.1016/0277-9536(94)90226-7. [DOI] [PubMed] [Google Scholar]
- Treiman Donald J. A Standard Occupational Prestige Scale for Use with Historical Data. The Journal of Interdisciplinary History. 1976;7(2):283–304. [Google Scholar]
- Trussell James, Henry Nathaniel, Hassan Fareen, Prezioso Alexander, Law Amy, Filonenko Anna. Burden of unintended pregnancy in the United States: potential savings with increased use of long-acting reversible contraception. Contraception. 2013;87(2):154–61. doi: 10.1016/j.contraception.2012.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trussell James, Pebley Anne R. The Potential Impact of Changes in Fertility on Infant, Child, and Maternal Mortality. Studies in Family Planning. 1984;15(6):267–80. [PubMed] [Google Scholar]
- Winikoff Beverly, Sullivan Maureen. Assessing the role of family planning in reducing maternal mortality. Studies in Family Planning. 1987:128–43. [PubMed] [Google Scholar]