Abstract
Background:
Current transfemoral prosthetic sockets are problematic as they restrict function, lack comfort, and cause residual limb problems. Development of a subischial socket with lower proximal trim lines is an appealing way to address this problem and may contribute to improving quality of life of persons with transfemoral amputation.
Objectives:
The purpose of this study was to illustrate the use of a new subischial socket in two subjects.
Study design:
Case series.
Methods:
Two unilateral transfemoral prosthesis users participated in preliminary socket evaluations comparing functional performance of the new subischial socket to ischial containment sockets. Testing included gait analysis, socket comfort score, and performance-based clinical outcome measures (Rapid-Sit-To-Stand, Four-Square-Step-Test, and Agility T-Test).
Results:
For both subjects, comfort was better in the subischial socket, while gait and clinical outcomes were generally comparable between sockets.
Conclusion:
While these evaluations are promising regarding the ability to function in this new socket design, more definitive evaluation is needed.
Clinical relevance
Using gait analysis, socket comfort score and performance-based outcome measures, use of the Northwestern University Flexible Subischial Vaccum Socket was evaluated in two transfemoral prosthesis users. Socket comfort improved for both subjects with comparable function compared to ischial containment sockets.
Keywords: Artificial limb, prosthetic socket, gait, transfemoral amputation
Background
Current transfemoral (TF) prosthetic sockets are problematic as they restrict function, lack comfort, and cause residual limb problems. Lack of socket comfort is the most common complaint of prosthesis users.1–3 Traditionally, there have been two basic designs of TF sockets both of which intentionally interact with the pelvis: the 1950s quadrilateral socket and the 1980s ischial containment socket (ICS).4 Because of the pelvic interaction, wearing either socket significantly reduces hip motion compared to motion without a socket.5,6 A recent variant of the ICS, the Marlo Anatomical Socket (MAS), combines greater containment (i.e. contact) of the ischial ramus medially with lower anterior and posterior trim lines. While the MAS allows increased hip range of motion compared to either ICS or quadrilateral sockets,7 it still requires interaction with the pelvis. Development of a subischial socket with lower proximal trim lines is an appealing way to address these problems and may contribute to improving quality of life of persons with TF amputation.
Subischial sockets with vacuum suspension have the potential to provide not only increased hip range of motion and comfort, but also less pistoning between the socket and limb, and better proprioception and tissue health.8–16 However, the lower trim lines of subischial sockets challenge conventional understanding of the biomechanics of TF sockets wherein “locking onto the pelvis” is believed to stabilize the socket in the coronal plane. When coronal plane stability of the socket is poor, the proximal medial brim impinges on the soft tissues of the groin and the distal femoral end abducts inside the socket uncomfortably contacting the lateral wall.17 To minimize this discomfort and reduce the coronal plane hip joint moment, TF prosthesis users often increase trunk lateral displacement and step width.
Dillon18 argued that the ability of any TF socket to provide coronal plane stability may come from either ischial ramal containment or compression of the proximal medial soft tissue to increase stiffness. Preliminary research supports the idea that TF sockets without ischial containment (IC) rely on soft tissue compression for coronal plane stability, socket comfort, and functional gait.8,19 A recent study using the MAS showed that both ischial ramal containment and tissue loading contribute to socket comfort: with containment tissue loading did not influence socket comfort, but with no containment the socket was comfortable only when tissue loading was high.19 Kahle and Highsmith8 reported that gait and balance in a brimless socket were equivalent to an ICS, without any of the gait adaptations typically associated with coronal plane instability.
The development of a more comfortable and possibly functional subischial socket may improve the quality of life of persons with TF amputation. While early reports suggest subischial sockets are feasible, no one has yet illustrated functional performance of a teachable subischial socket technique. A related article describes the design and fabrication of a new subischial socket and describes our efforts to teach this technique.20 The purpose of this article is to illustrate the use of the Northwestern University Flexible Subischial Vacuum (NU-FlexSIV) Socket in two subjects.
Methods
With approval from the Northwestern University Institutional Review Board, two unilateral TF prosthesis users provided informed consent to participate in preliminary socket evaluation comparing functional performance of the subischial socket and ICS. All data were acquired in our motion analysis laboratory equipped with eight cameras (Motion Analysis Corporation, MAC, Santa Rosa, CA, USA) and six force plates (Advanced Mechanical Technology, Inc., Watertown, MA, USA).
Reflective markers were taped to the skin over palpable boney landmarks or prosthetic equivalents using a modified Helen Hayes marker set.21 Specifically, markers were located on the shoe over the dorsum of the foot (between the second and third metatarsals immediately proximal to the metatarsal heads) and the heel counter at the same height as the toe marker; on the lateral malleolus and lateral femoral condyle; on the left and right anterior superior iliac spines (ASIS); and the L5/sacral interface. An additional marker was placed anteriorly on each thigh and shank. For consistency, the same experienced person placed all markers. Static trials were also collected with additional markers placed on the medial malleoli and medial femoral condyles. Medial markers were removed for dynamic trials.
Data were collected as each subject ambulated in each socket at self-selected normal, slow, and fast walking speeds over level ground until at least three force-plate strikes were recorded for each foot. EVa RealTime software (MAC) was used to determine the three-dimensional (3D) position of each marker relative to the laboratory coordinate system during each frame of each trial. The raw coordinate data were filtered using a second-order Butterworth bi-directional low-pass filter with an effective cutoff frequency of 6 Hz.22 Temporospatial data and gait events were calculated using OrthoTrak software (MAC).
Additional standardized clinical outcome measures included the socket comfort score (SCS),23 Rapid-Sit-To-Stand (RSTS) test,24,25 Four-Square-Step-Test (FSST),26 and Agility T-Test.27,28 For the SCS,23 subjects were asked, “On a 0–10 scale, if 0 represents the most uncomfortable socket fit you can imagine, and 10 represents the most comfortable socket fit, how would you score the comfort of the socket fit of your prosthesis at the moment?”
The RSTS test provides a standardized measure of active hip range of motion, lower limb muscle strength, and balance.24 Subjects were asked to rise from a chair without arm rests five times as fast as possible with their arms folded across their chest.24 Subjects performed two trials, with a 3-min rest period between trials.25
The FSST is a timed measure of dynamic standing stability involving rapid stepping in different directions and obstacle avoidance. A square cross was formed using four sticks laid flat on the floor. The stepping sequence was demonstrated and then one practice trial allowed. Subjects were instructed to “Try to complete the stepping sequence as fast as possible without touching the sticks. Both feet must make contact with the floor in each square. If possible, face forward during the entire sequence.”26 The test was timed twice and the best time taken as the score. A trial was repeated if the subject failed to complete the sequence successfully, lost balance, or made contact with a stick.
The Agility T-Test is typically used by athletes and includes forward, sideways, and backward running.27,28 Four markers were set out on the floor in the shape of a T. The subject started at the base of the T, sprinted forward to the top of the T and touched the marker, shuffled sideways and touched the marker, shuffled sideways in the opposite direction and touched the marker at the other end, shuffled back to touch the middle marker, before running backward to the initial marker. The trial was not counted if the subject crossed one foot in front of the other while shuffling sideways, failed to touch any markers, or failed to face forward throughout the test. The best time of three successful trials was used, with a 3-min rest period between trials.
Results
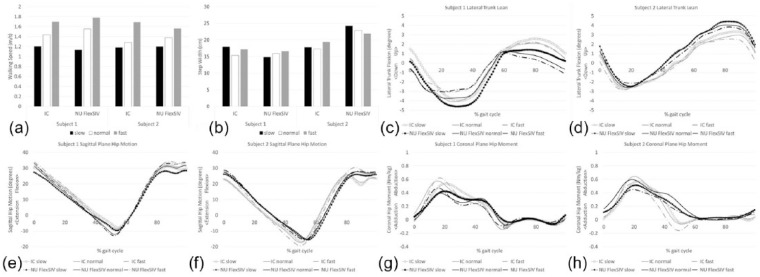
Two subjects participated in preliminary evaluation of socket use (Table 1). For both subjects, the NU-FlexSIV Socket was fabricated by author R.C., while the ICS was made for Subject 1 by a prosthetics instructor and Subject 2 wore his clinically prescribed ICS. For both subjects, socket comfort was better with the NU-FlexSIV Socket and gait and clinical outcomes data were generally comparable between sockets. Figure 1 illustrates the gait variables commonly thought to be affected by coronal plane socket stability19 and proximal trim lines.7 While walking speed was slightly faster at self-selected normal and fast speeds for both subjects with the NU-FlexSIV Socket, step width results were inconsistent, with Subject 1 unchanged but Subject 2 wider with the NU-FlexSIV Socket. NU-FlexSIV Socket coronal plane stability during walking was confirmed by lack of change in lateral trunk flexion when compared to ICS. No consistent changes in sagittal plane hip motion or coronal plane hip moments were observed for these two subjects.
Table 1.
Subject and prosthesis characteristics and temporospatial data.
| Subject 1 | Subject 2 | |||
|---|---|---|---|---|
| Age (years) | 29 | 26 | ||
| Sex | Male | Male | ||
| Height (cm) | 181 | 188 | ||
| Weight (kg) | 88.4 | 89.6 | ||
| Amputation | Right transfemoral | Left knee disarticulation | ||
| Cause of amputation | Trauma | Tumor | ||
| Time since amputation (years) | 9 | 15 | ||
| Activity level | Very active (construction worker) | Very active (athletic trainer) | ||
| ICS | NU-FlexSIV | ICS | NU-FlexSIV | |
| Suspension | Suction one-way valve | Origin liner Ottobock ePulse |
Suction one-way valve | Custom polyurethane liner Ottobock ePulse |
| Knee | Ottobock C-leg | Ottobock C-leg | Ottobock 3R45 | Ottobock C-leg |
| Foot | Ottobock Highlander | Ottobock Highlander | Össur Ceterus | Ottobock Highlander |
| Socket Comfort Score (SCS) | 2 | 10 | 8 | 9 |
| Rapid Sit-to-Stand (RSTS)a | 11.81 | 11.66 | 9.41 | 10.46 |
| Four-Square-Step-Test (FSST)a | 9.52 | 10.6 | 5.47 | 6.95 |
| Agility T-Testb | 26.6 | 26.81 | 15.75 | 13.1 |
Figure 1.
Selected gait data for Subjects 1 and 2 walking at three self-selected speeds (slow, normal, and fast) in an ischial containment and NU-FlexSIV Socket. (a) Walking Speed; (b) Step Width; (c) Subject 1 Lateral Trunk Lean; (d) Subject 2 Lateral Trunk Lean; (e) Subject 1 Sagittal Plane Hip Motion; (f) Subject 2 Sagittal Plane Hip Motion; (g) Subject 1 Coronal Plane Hip Moment; and (h) Subject 2 Coronal Plane Hip Moment.
Discussion
To our knowledge, this is the first attempt to create a teachable subischial socket with the potential to be more comfortable without compromising function. Gait and clinical outcomes data suggest improved comfort and comparable function to IC sockets, confirming previous reports.8,30 NU-FlexSIV Socket coronal plane stability during walking was confirmed by both lack of change in lateral trunk flexion (assessed with gait analysis) and lateral socket gapping at mid-stance (assessed visually). For self-selected normal walking speed, step width was slightly less for Subject 1 and within normal limits for Subject 2 for both sockets when compared to other unilateral TF amputees (20.7 ± 4.4 cm), while self-selected normal walking speed was substantially faster than other unilateral TF amputees (0.96 ± 0.01 m/s) in both sockets.31 A report of initial evaluation of the NU-FlexSIV Socket with a military TF amputee is similarly promising.32
An obvious limitation of this work is the preliminary nature of socket evaluation. Subject 1 was not as accustomed to an ICS as Subject 2 and Subject 2 wore different knees with each socket. Lack of standardization of socket accommodation may have influenced the results. More definitive evaluation in the form of randomized cross-over trials comparing comfort and functional performance with the NU-FlexSIV Socket to the ICS in persons with unilateral TF amputation are needed, and fortunately underway (https://clinicaltrials.gov/ct2/show/NCT02678247).
Conclusion
Overall, this preliminary work describes a subischial socket technique that appears to be more comfortable for users and results in gait that is at least comparable to that of conventional TF sockets with a proximal brim.
Acknowledgments
The authors acknowledge Jared Howell, CPO, MS, for ICS fabrication; the assistance of Rebecca Stine, MS, in acquiring data for the study; and the use of the Jesse Brown VA Chicago Motion Analysis Research Laboratory for data collection. The authors acknowledge the contribution of Brian Robillard, Wei Chen, Steven Gard, RJ Garrick, Andrew Hansen, Brett Johnson, Oluseeni Komolafe, Matthew Major, Joshua Rollock, Brian Ruhe, Cheng Sun, Lilly Tran, Kerice Tucker, and Sean Wood to various aspects of this project.
Footnotes
Author contribution: All authors contributed equally in the preparation of this manuscript.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The US Army Medical Research and Materiel Command Acquisition Activity, 820 Chandler 10 Street, Fort Detrick, MD 21702-5014, is the awarding and administering acquisition office (Award #W81XWH-10-1-0744). The content of this presentation does not necessarily reflect the position or the policy of the Government, and no official endorsement should be inferred.
References
- 1. Dillingham TR, Pezzin LE, MacKenzie EJ, et al. Use and satisfaction with prosthetic devices among persons with trauma-related amputations: a long-term outcome study. Am J Phys Med Rehabil 2001; 80: 563–571. [DOI] [PubMed] [Google Scholar]
- 2. Pezzin LE, Dillingham TR, MacKenzie EJ, et al. Use and satisfaction with prosthetic limb devices and related services. Arch Phys Med Rehabil 2004; 85: 723–729. [DOI] [PubMed] [Google Scholar]
- 3. Berke GM, Fergason J, Milani JR, et al. Comparison of satisfaction with current prosthetic care in veterans and servicemembers from Vietnam and OIF/OEF conflicts with major traumatic limb loss. J Rehabil Res Dev 2010; 47: 361–371. [DOI] [PubMed] [Google Scholar]
- 4. Schuch CM, Pritham CH. Current transfemoral sockets. Clin Orthop Relat Res 1999; 361: 48–54. [DOI] [PubMed] [Google Scholar]
- 5. Hagberg K, Haggstrom E, Uden M, et al. Socket versus bone-anchored trans-femoral prostheses: hip range of motion and sitting comfort. Prosthet Orthot Int 2005; 29: 153–163. [DOI] [PubMed] [Google Scholar]
- 6. Tranberg R, Zugner R, Karrholm J. Improvements in hip- and pelvic motion for patients with osseointegrated trans-femoral prostheses. Gait Posture 2011; 33: 165–168. [DOI] [PubMed] [Google Scholar]
- 7. Klotz R, Colobert B, Botino M, et al. Influence of different types of sockets on the range of motion of the hip joint by the transfemoral amputee. Ann Phys Rehabil Med 2011; 54: 399–410. [DOI] [PubMed] [Google Scholar]
- 8. Kahle JT, Highsmith MJ. Transfemoral interfaces with vacuum assisted suspension comparison of gait, balance, and subjective analysis: ischial containment versus brimless. Gait Posture 2014; 40: 315–320. [DOI] [PubMed] [Google Scholar]
- 9. Kahle JT, Orriola JJ, Johnston W, et al. The effects of vacuum-assisted suspension on residual limb physiology, wound healing, and function: a systematic review. Technol Innov 2014; 15: 333–341. [Google Scholar]
- 10. Arndt B, Caldwell R, Fatone S. Use of a partial foot prosthesis with vacuum-assisted suspension: a case study. J Prosthet Orthot 2011; 23: 82–88. [Google Scholar]
- 11. Street G. Vacuum suspension and its effects on the limb. Berlin, Orthopadie Technik, 2006. [Google Scholar]
- 12. Beil TL, Street GM, Covey SJ. Interface pressures during ambulation using suction and vacuum-assisted prosthetic sockets. J Rehabil Res Dev 2002; 39: 693–700. [PubMed] [Google Scholar]
- 13. Board WJ, Street GM, Caspers C. A comparison of trans-tibial amputee suction and vacuum socket conditions. Prosthet Orthot Int 2001; 25: 202–209. [DOI] [PubMed] [Google Scholar]
- 14. Hoskins R, Sutton E, Kinor D, et al. Using vacuum-assisted suspension to manage limb wounds in persons with transtibial amputation: a case series. Prosthet Orthot Int 2014; 38: 68–74. [DOI] [PubMed] [Google Scholar]
- 15. Klute GK, Berge JS, Biggs W, et al. Vacuum-assisted socket suspension compared with pin suspension for lower extremity amputees: effect on fit, activity, and limb volume. Arch Phys Med Rehabil 2011; 92: 1570–1575. [DOI] [PubMed] [Google Scholar]
- 16. Traballesi M, Delussu AS, Fusco A, et al. Residual limb wounds or ulcers heal in transtibial amputees using an active suction socket system. A randomized controlled study. Eur J Phys Rehabil Med 2012; 48: 613–623. [PubMed] [Google Scholar]
- 17. Radcliffe C. Functional considerations in the fitting of above-knee prostheses. Artif Limbs 1955; 2: 35–60. [PubMed] [Google Scholar]
- 18. Dillon M. Insights into socket geometry and coronal plane alignment. In: 12th World Congress of the International Society for Prosthetics and Orthotics, Vancouver, BC, Canada, 29 July–3 August 2007 http://www.ispoint.org/sites/default/files/ispo2007-programme-july3.pdf [Google Scholar]
- 19. Fatone S, Dillon M, Stine R, et al. Coronal plane socket stability during gait in persons with unilateral transfemoral amputation: pilot study. J Rehabil Res Dev 2015; 51: 1217–1228. [DOI] [PubMed] [Google Scholar]
- 20. Fatone S, Caldwell R. Northwestern University Flexible Subischial Vacuum Socket for persons with transfemoral amputation-Part 1: description of technique. Prosthet Orthot Int 2016, DOI: 10.1177/0309364616685229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kadaba MP, Ramakrishnan HK, Wooten ME, et al. Repeatability of kinematic, kinetic and electromyographic data in normal adult gait. J Orthop Res 1989; 7: 849–860. [DOI] [PubMed] [Google Scholar]
- 22. Winter D. Biomechanics and motor control of human movement. 2nd ed. New York: John Wiley & Sons, 1990. [Google Scholar]
- 23. Hanspal RS, Fisher K, Nieveen R. Prosthetic socket fit comfort score. Disabil Rehabil 2003; 25: 1278–1280. [DOI] [PubMed] [Google Scholar]
- 24. Whitney SL, Wrisley DM, Marchetti GF, et al. Clinical measurement of sit-to-stand performance in people with balance disorders: validity of data for the Five-Times-Sit-to-Stand Test. Phys Ther 2005; 85: 1034–1045. [PubMed] [Google Scholar]
- 25. Lusardi M, Pellecchia G, Schulman M. Functional performance in community living older adults. J Geriatr Phys Ther 2003; 26: 14–22. [Google Scholar]
- 26. Dite W, Temple VA. A clinical test of stepping and change of direction to identify multiple falling older adults. Arch Phys Med Rehabil 2002; 83: 1566–1571. [DOI] [PubMed] [Google Scholar]
- 27. Gailey RS, Gaunaurd IA, Raya MA, et al. Development and reliability testing of the Comprehensive High-Level Activity Mobility Predictor (CHAMP) in male servicemembers with traumatic lower-limb loss. J Rehabil Res Dev 2013; 50: 905–918. [DOI] [PubMed] [Google Scholar]
- 28. Gailey RS, Scoville C, Gaunaurd IA, et al. Construct validity of Comprehensive High-Level Activity Mobility Predictor (CHAMP) for male servicemembers with traumatic lower-limb loss. J Rehabil Res Dev 2013; 50: 919–930. [DOI] [PubMed] [Google Scholar]
- 29. Wilken JM, Darter BJ, Goffar SL, et al. Physical performance assessment in military service members. J Am Acad Orthop Surg 2012; 20 (Suppl. 1): S42–S47. [DOI] [PubMed] [Google Scholar]
- 30. Kahle JT, Highsmith MJ. Transfemoral sockets with vacuum-assisted suspension comparison of hip kinematics, socket position, contact pressure, and preference: ischial containment versus brimless. J Rehabil Res Dev 2013; 50: 1241–1252. [DOI] [PubMed] [Google Scholar]
- 31. Highsmith MJ, Schulz BW, Hart-Hughes S, et al. Differences in the spatiotemporal parameters of transtibial and transfemoral amputee gait. J Prosthet Orthot 2010; 22: 26–30. [Google Scholar]
- 32. Esposito E, Fatone S, Wilken J, et al. Sub-ischial prosthetic sockets improve hip range of motion and performance for individuals with transfemoral amputations. In: 41st American Academy of Orthotists and Prosthetists annual meeting & scientific symposium, New Orleans, LA, 18–21 February 2015 http://www.oandp.org/publications/jop/2015/2015-36.pdf [Google Scholar]