Abstract
Background:
Current transfemoral prosthetic sockets restrict function, lack comfort, and cause residual limb problems. Lower proximal trim lines are an appealing way to address this problem. Development of a more comfortable and possibly functional subischial socket may contribute to improving quality of life of persons with transfemoral amputation.
Objectives:
The purpose of this study was to (1) describe the design and fabrication of a new subischial socket and (2) describe efforts to teach this technique.
Study design:
Development project.
Methods:
Socket development involved defining the following: subject and liner selection, residual limb evaluation, casting, positive mold rectification, check socket fitting, definitive socket fabrication, and troubleshooting of socket fit. Three hands-on workshops to teach the socket were piloted and attended by 30 certified prosthetists and their patient models.
Results:
Patient models responded positively to the comfort, range of motion, and stability of the new socket while prosthetists described the technique as “straight forward, reproducible.”
Conclusion:
To our knowledge, this is the first attempt to create a teachable subischial socket, and while it appears promising, more definitive evaluation is needed.
Clinical relevance
We developed the Northwestern University Flexible Subischial Vacuum (NU-FlexSIV) Socket as a more comfortable alternative to current transfemoral sockets and demonstrated that it could be taught successfully to prosthetists.
Keywords: Artificial limb, prosthetic socket, gait, transfemoral amputation
Background
Current transfemoral (TF) prosthetic sockets often restrict function, lack comfort, and cause residual limb problems. Although designed to enable load transfer during activities (e.g. walking),1 sockets interface with soft tissues that are neither accustomed nor well-suited to the high pressure and shear loading that occurs during prosthesis use.2 Despite high levels of daily use, lack of socket comfort is the most common complaint of prosthesis users.3–5 Residual limb skin problems (e.g. cysts, calluses, allergic reactions, bacterial or fungal infections) have been reported by 25%–63% of persons with amputation, negatively influencing ability to perform household tasks, use the prosthesis, function socially, and participate in sports.3,6–8
Traditionally, there have been two basic designs of TF sockets both of which intentionally interact with the pelvis: the 1950s quadrilateral socket and the 1980s ischial containment socket (ICS).9 Fundamental to both designs is the proximal “brim” shape: in the quadrilateral socket, a horizontal ischial seat supports the ischial tuberosity,10,11 whereas in the ICS the ischial tuberosity and ramus are contained within the socket by higher, more rounded proximal trim lines creating more oblique supporting forces. Generally, the ICS is narrower in the mediolateral dimension than the quadrilateral socket, fitting intimately with the ischial ramus and greater trochanter and purportedly locking onto the pelvis for greater stability.12–14 Regardless, wearing either socket significantly reduces hip motion compared to motion without a socket.15,16
Lowering proximal trim lines of TF sockets is therefore appealing. A recent variant of the ICS, the Marlo Anatomical Socket (MAS), combines greater containment (i.e. contact) of the ischial ramus medially with lower anterior and posterior trim lines. The MAS allows increased hip range of motion compared to either ICS or quadrilateral sockets,17 providing sufficient control and stability for walking without loss of passive suction suspension.18–22 Newer vacuum suspension technology using a pump to maintain subatmospheric socket pressure has spurred additional reductions in proximal trim lines.23 The resulting sockets have been referred to as “brimless” or subischial since the proximal trim line is located distal to the ischial tuberosity and not intended to interact with the pelvis.24,25 Subischial sockets with vacuum suspension have the potential to provide not only increased hip range of motion and comfort but also less pistoning between the socket and limb and better proprioception and tissue health.24–32
The development of a more comfortable and possibly functional subischial socket may improve the quality of life of persons with TF amputation. While early reports suggest subischial sockets are feasible, no one has yet described a teachable subischial socket technique. Therefore, the purpose of this study was to (1) describe the design and fabrication of a new subischial socket and (2) describe efforts to teach this technique. An accompanying article illustrates socket use in two subjects.33
Method
Socket design/fabrication
The goal of our subischial socket was to have proximal trim lines that did not impinge on the pelvis, to be flexible so that muscles could move comfortably within the socket as they contract during activity and splay during sitting, and be held securely to the residual limb by compression of an undersized liner and socket as well as vacuum pump suction. An iterative reverse engineering approach was used wherein the technique initially developed in clinical practice by author R.C. was further developed by defining a clinical decision-making algorithm for socket casting and rectification and quantifying the rectifications.34–36 Socket development therefore involved defining subject and liner selection, residual limb evaluation, casting, positive mold rectification, check socket fitting, definitive socket fabrication, and troubleshooting of socket fit.
Teaching efforts
A series of three, 2-day, hands-on, continuing education workshops to teach the new socket were piloted. Courses were advertised on the university’s website, oandp-l, and by word of mouth. Courses were open to attendance by up to 12 certified prosthetists who were required to register both themselves and a TF amputee patient model. Prosthetists earned 15.5 continuing education credits from either the American Board for Certification in Orthotics Prosthetics and Pedorthics (ABC) or the Board of Certification (BOC). Participants engaged in lectures, demonstrations, and hands-on activities designed to teach how to cast, rectify, fit, and align a subischial check socket. Gait was assessed visually by the whole group using split frame coronal and sagittal videos of the patient models walking in their regularly used prosthesis and in the subischial socket. Course feedback was gathered via survey.
Results
Socket design/fabrication
Subject and liner selection
The Northwestern University Flexible Subischial Vacuum (NU-FlexSIV) Socket is best suited for experienced, compliant amputees with residual limbs that are well-healed with well-regulated volume. Contraindications are primarily linked to the use of vacuum suspension (e.g. significant muscle bunching that results in loss of total contact with the liner, deep longitudinal invaginations that trap or allow air between the limb and liner, allergies to silicone liners, and non-compliance with clinical care).
The socket includes a highly compressive, cylindrical, fabric-covered silicone liner, a flexible inner socket, a shorter rigid outer socket, and a sealing sleeve that creates the seal needed to apply vacuum between the liner and inner socket (Figure 1). The liner compresses the limb to create a generic cylindrical shape, stiffening the soft tissues to achieve stability of the socket with respect to the residual limb. While heavily scarred or bulbous residual limbs may require a custom liner to ensure a total contact fit, most limbs can be fit with a transtibial off-the-shelf liner (Figure 2). Transtibial liners are preferred since their non-tapered, cylindrical profile provides relatively high compression of the softer proximal tissues. When measuring for a liner, manufacturer instructions are followed, but a liner one size below the manufacturer’s recommendation should be selected. This ensures limb compression and total contact distally. Liners that have worked well to date include the RELAX 3C Cushion Liner (medi GmbH, Bayreuth, Germany) and, when that does not work, the Iceross® Synergy™ Cushion Liner (Össur, Reykjavik, Iceland), both of which incorporate fabric on the exterior surface to wick air from between the liner and socket to maintain suction. If a liner without fabric is used, an air wick (e.g. a nylon sock) must be used. For our socket, we consider a liner to “work well” if it has high compressive stiffness, high shear stiffness, high coefficient of friction, and high thermal conductivity using the definitions provided on the prosthetic liner assistant website (http://www.linerassist.org/).
Figure 1.

(Left) NU-FlexSIV Socket on limb showing sealing sleeve and (right) definitive version of the NU-FlexSIV Socket fabricated by Advanced O&P Solutions (Hickory Hills, IL). Photo courtesy of Michael Angelico.
Figure 2.
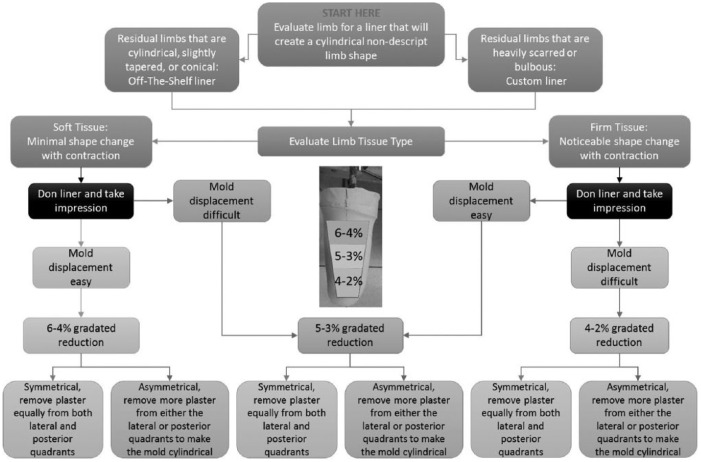
Clinical algorithm for NU-FlexSIV Socket. Regarding liner selection, almost all transfemoral limb shapes can be made more cylindrical by fitting an off-the-shelf transtibial liner; custom liners are only required when the limb is heavily scarred or bulbous. The manner in which the liner is customized should ensure that the liner clad limb shape is cylindrical. “Gradated reductions” refer to the reduction of circumferences more proximally than distally. For example, for 6%–4% reductions, the circumferences in the proximal third of the limb are reduced by 6%, the circumferences in the middle third of the limb are reduced by 5%, and the circumferences in the lower third of the limb are reduced by 4%.
Source: Reprinted with permission from the authors.37
Residual limb evaluation
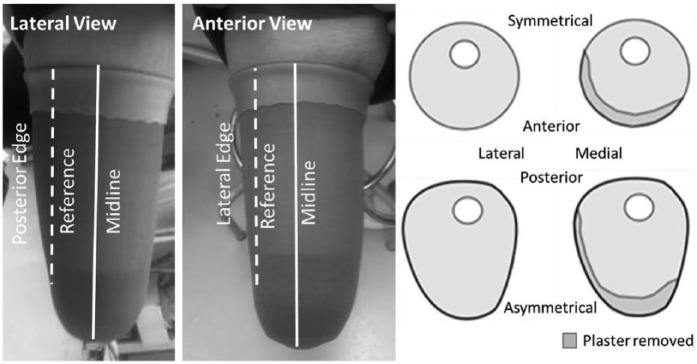
Before casting, residual limb soft tissue is evaluated with the patient sitting and classified as either soft (i.e. minimal shape change with contraction) or firm (i.e. noticeable shape change with contraction). Liners are donned by inverting and rolling as high on the limb as possible. The excess of the proximal aspect of the liner forms a 50-mm fold that provides additional compression of the softer proximal tissues. To assess the proximal mediolateral (ML) width, an ML gauge (i.e. a modified Ritz Stick) is positioned over the folded liner, parallel to the proximal liner edge, which is approximately level with the perineum. The medial arm of the ML gauge is held steady against the proximal edge of the liner approximately at perineal level, and the lateral arm moved toward the limb, noting how much compression can be achieved when pushing sub-trochanterically. Limb shape is evaluated by viewing it anteriorly and laterally to determine whether the lateral and posterior edges of the residual limb are parallel to midline of the long axis of the limb or if they angle away from midline of the long axis of the limb proximally (Figure 3). The limb is classified as symmetrical if the angulation away from midline of the long axis of the limb is of similar degree for both the lateral and posterior edges and asymmetrical if one edge angles away from midline of the long axis of the limb more than the other (Figure 3). Once a positive mold of the residual limb is taken and filled with plaster, a goal of mold rectification is to make the posterior and lateral edges nearer to parallel to midline of the long axis of the limb, with amount of plaster removed dependent on symmetrical or asymmetrical classification. Cross-sectional diagrams (Figure 3) show the relative amount of plaster removed posteriorly and laterally based on whether the residual limb is considered symmetrical or asymmetrical.
Figure 3.
Example of a symmetrical residual limb shape wherein the area of the residual limb bounded by the reference line and posterior or lateral edges of the limb are approximately the same: this area represents the material to be removed during rectification of the positive model. Cross-sectional diagrams show the plaster removed based on whether the residual limb is considered symmetrical or asymmetrical.
Casting
The impression is taken with the patient sitting in a chair such that the buttock of the amputated limb is at the edge of the seat and the residual limb is off the chair, flexed 90° and slightly abducted. This allows gravity to pre-modify the limb shape, creating a slight rectus relief, a generous medial flare, and a narrow ML due to posterior soft tissue droop. Slight residual limb abduction allows the impression medially to extend proximally as close to the perineum as possible. The liner clad limb is wrapped in cling film with a thin cast sock donned over the top. Fiberglass bandage is wrapped circumferentially without tension over the limb beginning proximal-laterally and moving medially over the anterior of the limb, overlapping each layer by half the bandage width. The folded proximal edge of the liner should be captured in the impression as it provides the initial, flared proximal socket trim line. The fiberglass over the distal end of the residual limb is contoured to ensure total contact with the liner clad limb. For most limbs, the proximal edge of the mold will be perpendicular to the midline of the residual limb but can be obliquely tapered with a higher lateral trim line for short residual limbs to increase the surface area in contact with the liner. An anterior midline reference is marked and the force required to slide the impression off the residual limb is noted: an impression that is difficult to remove from the residual limb requires less reduction of the positive mold than an impression that slides easily.
Positive mold rectification
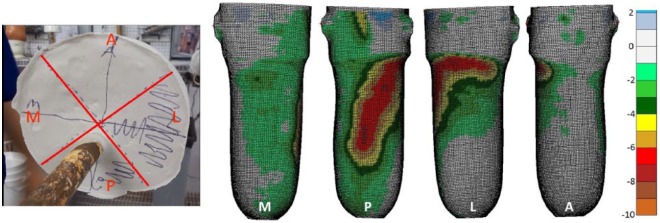
This technique requires only removal of plaster from the positive mold. Magnitude of plaster removal is graded based on the algorithm shown in Figure 2, with more plaster removed proximally versus distally to ensure the limb seats completely into the socket. Volume reduction, estimated using circumference measures of the positive mold taken in 1 in increments along the length of the limb, serves to further compress the soft tissue. The amount of reduction depends on whether the limb soft tissues were classified as soft or firm and removing the impression from the limb was easy or difficult. Using a quadrant system marked on the proximal end of the mold (Figure 4), reductions are concentrated in the lateral and posterior quadrants, with only light smoothing of the medial and anterior quadrants and distal end. The mold rectification map (Figure 4) depicts the target pattern, with plaster removed proximal-laterally to decrease the proximal ML diameter to that which was measured with the ML gauge, and the posterior flattened slightly. Magnitude of plaster removal is based on whether the limb was classified as symmetrical or asymmetrical: if symmetrical, the same amount of plaster is removed from the posterior and lateral quadrants to achieve target volume reduction; if asymmetrical, more plaster is removed from the quadrant in which the edge of the limb angled more away from the midline.
Figure 4.
Quadrant system and exemplar mold rectification map for NU-FlexSIV Socket (M: medial; P: posterior; L: lateral; A: anterior). Color coding on the rectification map indicates depth of plaster removed.
Check socket fitting
An initial polyethylene terephthalate glycol (PETG) diagnostic socket is fabricated with a hole drilled into the distal end to expel air when the liner clad residual limb is pushed into the socket. If more than modest resistance is experienced during donning or distal end contact cannot be achieved until vacuum is applied, it is likely that the user will have trouble donning the definitive flexible socket as it has a higher coefficient of friction. Once the socket is donned, the proximal liner is folded over the edge of the socket. A static check fit is conducted to ensure volume reductions are appropriate and total distal end contact achieved. Initially, check socket trim lines may be too high resulting in contact with the ischial ramus or tuberosity. This can be relieved by a combination of trimming and flaring of the socket to gradually lower the trim line until boney contact with the socket no longer occurs. This may be a slow process as it is important to keep as much of the limb within the socket as possible to maximize tissue containment and stiffening, as well as surface area for vacuum suspension.
If initial fit is satisfactory, an attachment plate and barb are adhered to the socket. No specific socket alignment is required other than what is needed for prosthetic knee function. For dynamic fitting, the socket is attached to the prosthetic components, including a vacuum pump (either mechanical or electrical), and donned with the liner folded over the proximal edge of the socket and sealed to the exterior socket wall with a sealing sleeve. While weight bearing with vacuum on, the user should feel a general tightness of the socket without any specific pressure points, especially on the distal end. There should be minimal or no contact with the pelvis during weight bearing or hip adduction and extension. Note that minor proximal trim line issues may be resolved by transitioning to a flexible inner socket.
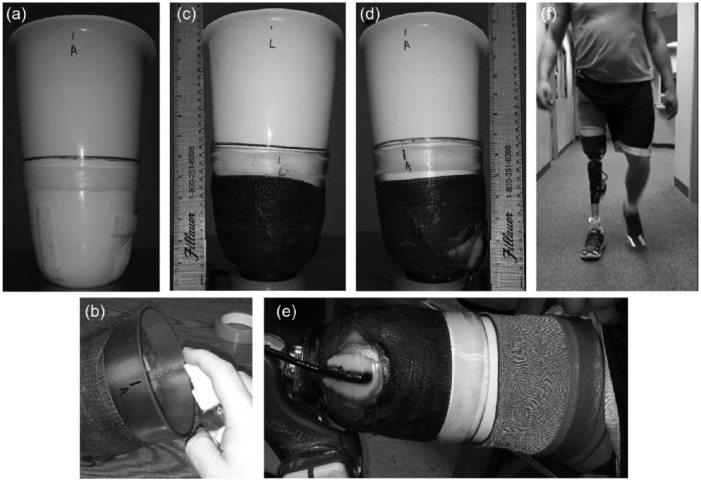
Check socket fit is successful if a liner-only fit is achieved; there is only slight resistance seating the limb into the socket upon standing; total contact between the limb and socket is maintained at all times, specifically at the distal end, the lateral proximal trim line in standing and the anterior proximal trim line in sitting; there is little or no contact between the socket and pelvis; and there is no excessive flaring of the socket anywhere along the proximal trim line. Rigid check sockets should be used only for short periods to avoid liner breakdown, with a second flexible check socket made for extended wear trials. The flexible check socket is made using Flex ethyl vinyl acetate (EVA; medi GmbH) with an outer rigid socket of PETG reinforced with fiberglass (Figure 5). Flex EVA provides sufficient rigidity to support the residual limb axially while maintaining flexibility to reduce edge pressures (i.e. pressure at the proximal socket trim line between the limb and socket as well as the liner and socket) and conform to the residual limb in the seated position. Using blister forming, the Flex EVA inner socket can be very thin and light.
Figure 5.
Flexible check socket fabrication: (a) flexible inner socket with Velcro and sealing ring to hold rigid polyethylene terephthalate glycol (PETG) outer socket in place (distal port hole for air not shown); (b) outer socket sprayed with alcohol to allow it to be pushed onto inner socket; (c) lateral and (d) anterior view of flexible inner socket inserted into outer socket and reinforced with fiberglass tape, black line indicates top of rigid socket; (e) donned socket showing attachment of barb to distal end of outer socket (vacuum is drawn from between the liner and inner socket through port hole and between inner and outer socket via barb); and (f) mid-stance of gait with flexible check socket.
Definitive socket fabrication
If deemed to fit well, the flexible inner socket used as part of the second check socket can be re-used as part of the definitive socket by replacing the outer rigid PETG socket with a definitive, carbon-fiber-laminated version (Figure 1). In the definitive socket, flexible inner socket trim lines are approximately 12 mm distal to the ischial tuberosity and 25 mm distal to the greater trochanter. The height of the rigid outer socket is subject specific but should be at least 75 mm below the proximal trim line of the flexible inner socket, allowing the liner to fold over the proximal trim line of the flexible inner socket and seal with a sleeve that is secured distally by sandwiching between the rigid outer and flexible inner sockets.
Troubleshooting socket fit
When distal end contact is not achieved, the proximal trim line should be checked to ensure that it does not contact the pelvis and prevent the limb from seating into the distal end of the socket. Short-term use of padding or gel spots distally in the check socket are permissible to achieve total contact until this issue can be corrected in the next socket iteration. The proximal lateral wall of the socket must remain tightly secure to the residual limb during walking especially at mid-stance as gapping will cause blistering along the proximal lateral trim line over time. If gapping occurs, pad the proximal medial wall of the socket to effectively pull the lateral socket wall tightly into the residual limb. The proximal anterior wall of the socket must remain tightly secure to the residual limb in sitting as gapping will lead to loss of suspension. A small amount of gapping anteriorly may occur with the rigid check socket when sitting: if this gapping is minimal, it will likely resolve when a flexible inner socket material is used, but if gapping is more than minimal, pad the proximal posterior wall of the socket to effectively pull the anterior socket wall tightly into the residual limb.
Teaching efforts
The three courses were attended collectively by 30 certified prosthetists and their patient models from across North America. For 2/30 sockets, a second check socket was made to improve fitting, in one case as a result of switching liner type. Overall, 28/30 patient models were able to walk comfortably in the rigid check socket with little visual change in gait when compared to the patient models’ regularly used socket (Figure 6). Course feedback is summarized in Table 1. The participants were generally positive about the quality and value of course content, pre-course planning and communication, and course organization; they indicated that their understanding of subischial socket and vacuum technology improved after taking the course; and most were confident that they could fabricate the NU-FlexSIV Socket and anticipated using it in their clinical practice.
Figure 6.
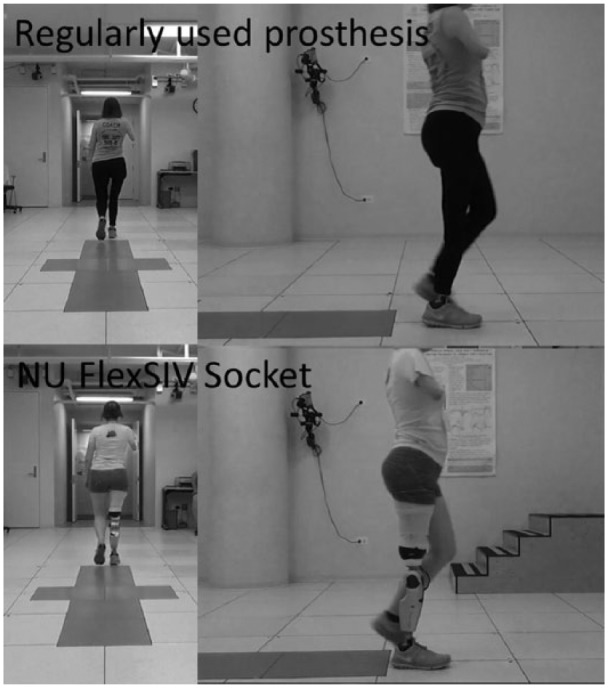
Still frame from one of the split-screen videos used to visually assess gait in both sockets during the courses.
Table 1.
Prosthetist feedback on NU-FlexSIV Socket courses.
| Instruction |
With 5 being the best and 1 being the worst, please indicate rank of content, quality, and value on the scale provided.
|
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Scale | Course 1 (n = 6) |
Course 2 (n = 12) |
Course 3 (n = 12) |
||||||||||||
| 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | |
| Content | 0 | 0 | 0 | 0 | 100 | 0 | 0 | 0 | 17 | 83 | 0 | 0 | 0 | 0 | 100 |
| Quality of presentation | 0 | 0 | 0 | 0 | 100 | 0 | 0 | 0 | 25 | 75 | 0 | 0 | 0 | 10 | 90 |
| Value of hands-on casting | 0 | 0 | 0 | 0 | 100 | 0 | 8 | 0 | 8 | 84 | 0 | 0 | 0 | 0 | 100 |
| Value of hands-on rectification | 0 | 0 | 0 | 0 | 100 | 0 | 0 | 0 | 25 | 75 | 0 | 0 | 0 | 10 | 90 |
| Value of hands-on check socket fitting | 0 | 0 | 0 | 0 | 100 | 0 | 0 | 0 | 17 | 83 | 0 | 0 | 0 | 10 | 90 |
| Pre-course understanding of subischial socket and vacuum technology | 0 | 50 | 25 | 0 | 25 | 8 | 8 | 25 | 50 | 0 | 0 | 10 | 40 | 10 | 40 |
| Post-course understanding of subischial socket and vacuum technology | 0 | 0 | 0 | 75 | 25 | 0 | 0 | 8 | 25 | 67 | 0 | 0 | 0 | 0 | 100 |
| Post-course ability to fabricate NU-FlexSIV Socket | 0 | 0 | 0 | 75 | 25 | 0 | 8 | 17 | 25 | 50 | 0 | 10 | 0 | 10 | 80 |
| Anticipated clinical use | 0 | 0 | 0 | 0 | 100 | 0 | 0 | 17 | 8 | 75 | 0 | 10 | 10 | 30 | 50 |
| Pre-course planning | 0 | 0 | 0 | 25 | 75 | 0 | 0 | 0 | 17 | 83 | 0 | 0 | 0 | 0 | 100 |
| Pre-course communications | 0 | 0 | 0 | 0 | 100 | 0 | 0 | 0 | 8 | 92 | 0 | 0 | 0 | 10 | 90 |
| On-site organization | 0 | 0 | 0 | 10 | 90 | 0 | 0 | 0 | 0 | 100 | 0 | 0 | 0 | 10 | 90 |
Responses indicated as percent of participants who selected that number on the scale. Not all responses sum to 100% due to unanswered items.
Discussion
To our knowledge, this is the first attempt to create a teachable subischial socket with the potential to be more comfortable without compromising function. The idea that soft tissue compression can be used to create stability between the residual limb and socket by stiffening the soft tissue and more efficiently transferring force between the underlying skeleton and prosthesis is not new.38 However, the degree to which limbs can be compressed and the socket successfully donned has increased with availability of more compliant socket materials. Most recently, tissue compression and subsequent stiffening has been proposed as the underlying principle for the compression and release socket, which applies three or more localized, longitudinal areas of high compression to the residual limb.39 By contrast, the NU-FlexSIV Socket provides high global compression via an undersized liner and socket, and it is believed that tissue stiffness is further enhanced by use of vacuum, which has been reported to increase volume of the residual limb compared to other types of suspension.25 It may be that the combination of socket/liner compression globally and volume stabilization by vacuum creates better locking of the residual limb within the socket than other forms of suspension.
Some clinicians have expressed concerns regarding the potential for increased fall-related femoral fracture risk while wearing TF sockets with lower trim lines. However, the incidence of post-amputation fall-related fracture is very low (2%–3%),40–43 and Gailey et al.44 reported that the literature to date does not conclusively support a direct relationship between low bone mineral density and residual limb fractures among people with lower limb amputation. Additionally, little is known about the circumstances in which fall-related injuries occur in people with lower limb amputation, especially community-dwelling individuals, so it is unclear what effect socket design might have on fracture risk. For inpatients, most falls occur during unassisted transfers.40,42,45 Gonzalez and Matthews40 reported that the prosthesis was in use at the time of falling in only three of nine cases studied, while Pauley et al.42 reported that only 3.7% of falls occurred during walking. However, since falls appear to be the leading cause of post-amputation fracture with the femur and hip being the most common site of fracture in both transtibial and TF amputees,44 and since there is a threefold increase in fall risk for persons with TF amputation,42 it would be prudent for future research to assess the relationship between any socket design and fall-related fracture risk in community-dwelling individuals with TF amputation.
Survey feedback from our courses was largely positive. Additionally, patient models who participated in pilot courses responded positively to the comfort, range of motion, and stability of the socket while prosthetists described the technique as “straight forward, reproducible.” Group review of the split-screen videos confirmed that gait was comparable in the NU-FlexSIV Socket to the regularly used sockets, consistent with more formal evaluation of two subjects.33 Initial courses were 2-days long and involved fitting only an initial rigid check socket. Participants suggested that future courses should include fitting of a second flexible check socket to more fully grasp how transition to a flexible socket would resolve minor fitting issues and further improve comfort.
Having prosthetists participate in the course with their own patient and being able to take home the rigid check socket and liner were intended to incentivize implementation of the technique in clinical practice. However, it was anticipated that prosthetists would encounter additional questions or issues. To facilitate course participants’ ongoing learning and troubleshooting, a post-course online forum was created using a free, invitation-only, instant messaging application (hipchat.com). The forum was intended as a collaborative platform where early adopters of the NU-FlexSIV Socket could share information/questions regarding their experiences and exchange advice and troubleshooting tips with each other and the course instructors. It is believed that this type of support will help the NU-FlexSIV Socket gain long-term traction with these early adopters.
Given the preliminary nature of the research efforts to date, we have been conservative in suggesting that the NU-FlexSIV Socket is best suited for experienced, compliant amputees with residual limbs that are well-healed with well-regulated volume. However, during 10 years of clinical experience with this socket, author R.C. has successfully fit more complex limbs with open wounds, scarring, invaginations, heterotrophic ossification, bone spurs, and skin grafts, suggesting that with experience, broader application may be possible. Overall, this preliminary work describes a subischial socket technique that appears to be teachable to prosthetists.
Conclusion
We developed the NU-FlexSIV Socket as a more comfortable alternative to current transfemoral sockets and demonstrated that it could be taught successfully to prosthetists. To our knowledge, this is the first attempt to create a teachable subischial socket, and while it appears promising, more definitive evaluation is needed.
Acknowledgments
The authors acknowledge the support and contribution of Northwestern University Prosthetics-Orthotics Center (NUPOC) faculty, staff, and students in holding the NU-FlexSIV Socket courses. They also acknowledge the support of Össur and medi in donating liners for patient models who participated in the NU-FlexSIV Socket courses. The authors acknowledge the contribution of Brian Robillard, Wei Chen, Steven Gard, RJ Garrick, Andrew Hansen, Brett Johnson, Oluseeni Komolafe, Matthew Major, Joshua Rollock, Brian Ruhe, Cheng Sun, Lilly Tran, Kerice Tucker, and Sean Wood to various aspects of this project.
Footnotes
Author contribution: All authors contributed equally in the preparation of this manuscript.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The US Army Medical Research and Materiel Command Acquisition Activity, 820 Chandler 10 Street, Fort Detrick, MD 21702-5014, is the awarding and administering acquisition office (Award #W81XWH-10-1-0744). The content of this presentation does not necessarily reflect the position or the policy of the Government, and no official endorsement should be inferred.
References
- 1. Mak AF, Zhang M, Boone DA. State-of-the-art research in lower-limb prosthetic biomechanics-socket interface: a review. J Rehabil Res Dev 2001; 38: 161–174. [PubMed] [Google Scholar]
- 2. Mak AFT, Zhang M, Tam EWC. Biomechanics of pressure ulcer in body tissues interacting with external forces during locomotion. Annu Rev Biomed Eng 2010; 12: 29–53. [DOI] [PubMed] [Google Scholar]
- 3. Dillingham TR, Pezzin LE, MacKenzie EJ, et al. Use and satisfaction with prosthetic devices among persons with trauma-related amputations: a long-term outcome study. Am J Phys Med Rehab 2001; 80: 563–571. [DOI] [PubMed] [Google Scholar]
- 4. Pezzin LE, Dillingham TR, MacKenzie EJ, et al. Use and satisfaction with prosthetic limb devices and related services. Arch Phys Med Rehab 2004; 85: 723–729. [DOI] [PubMed] [Google Scholar]
- 5. Berke GM, Fergason J, Milani JR, et al. Comparison of satisfaction with current prosthetic care in veterans and service members from Vietnam and OIF/OEF conflicts with major traumatic limb loss. J Rehabil Res Dev 2010; 47: 361–371. [DOI] [PubMed] [Google Scholar]
- 6. Dudek NL, Marks MB, Marshall SC, et al. Dermatologic conditions associated with use of a lower-extremity prosthesis. Arch Phys Med Rehab 2005; 86: 659–663. [DOI] [PubMed] [Google Scholar]
- 7. Meulenbelt HE, Geertzen JH, Jonkman MF, et al. Skin problems of the stump in lower limb amputees: 1. A clinical study. Acta Derm-Venereol 2011; 91: 173–177. [DOI] [PubMed] [Google Scholar]
- 8. Meulenbelt HE, Geertzen JH, Jonkman MF, et al. Skin problems of the stump in lower-limb amputees: 2. Influence on functioning in daily life. Acta Derm-Venereol 2011; 91: 178–182. [DOI] [PubMed] [Google Scholar]
- 9. Schuch CM, Pritham CH. Current transfemoral sockets. Clin Orthop Relat Res 1999; 361: 48–54. [DOI] [PubMed] [Google Scholar]
- 10. Foort J. Socket design for the above-knee amputee. Prosthet Orthot Int 1979; 3: 73–81. [DOI] [PubMed] [Google Scholar]
- 11. Radcliffe C. Functional considerations in the fitting of above-knee prostheses. Artif Limbs 1955; 2: 35–60. [PubMed] [Google Scholar]
- 12. Sabolich J. Contoured adducted trochanteric-controlled alignment method (CAT-CAM): introduction and basic principles. Clin Prosthet Orthotics 1985; 9: 15–26. [Google Scholar]
- 13. Hoyt C, Littig D, Lundt J, et al. The Ischial containment above-knee prosthesis. UCLA Prosthetics Education and Research Program, Los Angeles, CA, 1987. [Google Scholar]
- 14. Pritham CH. Biomechanics and shape of the above-knee socket considered in light of the ischial containment concept. Prosthet Orthot Int 1990; 14: 9–21. [DOI] [PubMed] [Google Scholar]
- 15. Hagberg K, Haggstrom E, Uden M, et al. Socket versus bone-anchored trans-femoral prostheses: hip range of motion and sitting comfort. Prosthet Orthot Int 2005; 29: 153–163. [DOI] [PubMed] [Google Scholar]
- 16. Tranberg R, Zugner R, Karrholm J. Improvements in hip and pelvic motion for patients with osseointegrated trans-femoral prostheses. Gait Posture 2011; 33: 165–168. [DOI] [PubMed] [Google Scholar]
- 17. Klotz R, Colobert B, Botino M, et al. Influence of different types of sockets on the range of motion of the hip joint by the transfemoral amputee. Ann Phys Rehabil Med 2011; 54: 399–410. [DOI] [PubMed] [Google Scholar]
- 18. Pike A. A new concept in above-knee socket design. The O&P Edge, November 2002. http://www.oandp.com/articles/2002-11_01.asp
- 19. Ortiz Vazquez del Mercado M. Evolution of ischial containment socket. Paper presented at the American Academy of Orthotists and Prosthetists, 19–22 March 2003, San Diego, CA. [Google Scholar]
- 20. Fairley MMAS. Socket: a transfemoral revolution. The O&P Edge, June 2004. http://www.oandp.com/articles/2004-06_03.asp
- 21. Fatone S, Dillon M, Stine R, et al. Coronal plane socket stability during gait in persons with unilateral transfemoral amputation: pilot study. J Rehabil Res Dev 2015; 51: 1217–1228. [DOI] [PubMed] [Google Scholar]
- 22. Traballesi M, Delussu AS, Averna T, et al. Energy cost of walking in transfemoral amputees: comparison between Marlo Anatomical Socket and Ischial Containment Socket. Gait Posture 2011; 34: 270–274. [DOI] [PubMed] [Google Scholar]
- 23. Fairley M. “Hanging Tight”: elevated vacuum suspension systems step forward. The O&P Edge, March 2008. http://www.oandp.com/articles/2008-03_03.asp
- 24. Kahle JT, Highsmith MJ. Transfemoral interfaces with vacuum assisted suspension comparison of gait, balance, and subjective analysis: ischial Containment versus brimless. Gait Posture 2014; 40: 315–320. [DOI] [PubMed] [Google Scholar]
- 25. Kahle JT, Orriola JJ, Johnston W, et al. The effects of vacuum-assisted suspension on residual limb physiology, wound healing, and function: a systematic review. Technol Innov 2014; 15: 333–341. [Google Scholar]
- 26. Arndt B, Caldwell R, Fatone S. Use of a partial foot prosthesis with vacuum-assisted suspension: a case study. J Prosthet Orthot 2011; 23: 82–88. [Google Scholar]
- 27. Street G. Vacuum suspension and its effects on the limb. Dortmund: Orthopadie Technik, 2006. [Google Scholar]
- 28. Beil TL, Street GM, Covey SJ. Interface pressures during ambulation using suction and vacuum-assisted prosthetic sockets. J Rehabil Res Dev 2002; 39: 693–700. [PubMed] [Google Scholar]
- 29. Board WJ, Street GM, Caspers C. A comparison of trans-tibial amputee suction and vacuum socket conditions. Prosthet Orthot Int 2001; 25: 202–209. [DOI] [PubMed] [Google Scholar]
- 30. Hoskins R, Sutton E, Kinor D, et al. Using vacuum assisted suspension to manage limb wounds in persons with trans-tibial amputation: a case series. Prosthet Orthot Int 2014; 38: 68–74. [DOI] [PubMed] [Google Scholar]
- 31. Klute GK, Berge JS, Biggs W, et al. Vacuum-assisted socket suspension compared with pin suspension for lower extremity amputees: effect on fit, activity, and limb volume. Arch Phys Med Rehab 2011; 92: 1570–1575. [DOI] [PubMed] [Google Scholar]
- 32. Traballesi M, Delussu AS, Fusco A, et al. Residual limb wounds or ulcers heal in transtibial amputees using an active suction socket system. A randomized controlled study. Eur J Phys Rehabil Med 2012; 48: 613–623. [PubMed] [Google Scholar]
- 33. Fatone S, Caldwell R. Northwestern University Flexible Subischial Vacuum Socket for persons with transfemoral amputation-Part 2: preliminary evaluation. Prosthet Orthot Int, 2016. DOI: 10.1177/0309364616685230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Sidles J, Boone DH, Harlan JS, et al. Rectification maps: a new method of describing residual limb and socket shapes. J Prosthet Orthot 1989; 1: 149–153. [Google Scholar]
- 35. Zachariah SG, Sorenson E, Sanders JE. A method for aligning trans-tibial residual limb shapes so as to identify regions of shape change. IEEE T Neur Sys Reh 2005; 13: 551–557. [DOI] [PubMed] [Google Scholar]
- 36. Sanders J, Severance M. Assessment technique for computer-aided manufactured sockets. J Rehabil Res Dev 2011; 48: 763–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Fatone S, Caldwell R. Instructional manual for NU-FlexSIV socket. Chicago, IL: Northwestern University Prosthetics-Orthotics Center, 2015. [Google Scholar]
- 38. Redhead R. Total surface bearing self suspending above-knee sockets. Prosthet Orthot Int 1979; 3: 126–136. [DOI] [PubMed] [Google Scholar]
- 39. Alley R, Williams T, Albuquerque M, et al. Prosthetic sockets stabilized by alternating areas of tissue compression and release. J Rehabil Res Dev 2011; 48: 679–696. [DOI] [PubMed] [Google Scholar]
- 40. Gonzalez E, Matthews M. Femoral fractures in patients with lower extremity amputation. Arch Phys Med Rehab 1980; 61: 276–280. [PubMed] [Google Scholar]
- 41. Denton J, McClelland S. Stump fractures in lower extremity amputees. J Traum 1985; 25: 1074–1078. [PubMed] [Google Scholar]
- 42. Pauley T, Devlin M, Heslin K. Falls sustained during inpatient rehabilitation after lower limb amputation: prevalence and predictors. Am J Phys Med Rehab 2006; 85: 521–532. [DOI] [PubMed] [Google Scholar]
- 43. Gooday H, Hunter J. Preventing falls and stump injuries in lower limb amputees during inpatient rehabilitation: completion of the audit cycle. Clin Rehabil 2004; 18: 379–390. [DOI] [PubMed] [Google Scholar]
- 44. Gailey RS, Allen K, Castles J, et al. Review of secondary physical conditions associated with lower-limb amputation and long-term prosthesis use. J Rehabil Res Dev 2008; 45: 15–30. [DOI] [PubMed] [Google Scholar]
- 45. Dyer D, Bouman B, Davey M, et al. An intervention program to reduce falls for adult in-patients following major lower-limb amputation. Healthc Q 2008; 11: 117–121. [DOI] [PubMed] [Google Scholar]