Abstract
In this study, two telephone interviews that assessed both religious involvement and health-related quality of life were conducted approximately 2.5 years apart in a national sample of 290 African Americans. Religious involvement was assessed with an instrument that measured both personal religious beliefs (e.g., having a personal relationship with God) and more public religious behaviors (e.g., attending church services). Health-related quality of life was measured with version 2 of the Medical Outcomes Study 12-item short form (SF-12v2). Structural equation models indicated that higher religious beliefs at baseline predicted better physical and mental health 2.5 years later. Higher religious behaviors at baseline contributed smaller, complementary suppression effects. Physical and mental health indicators from the SF-12v2 at baseline did not predict changes in either religious beliefs or religious behaviors over time. These findings indicate that, for African Americans, personal religious beliefs lead to beneficial health effects over time, whereas individual differences in health do not appear to predict changes in religious involvement.
Keywords: religious involvement, health, African American, longitudinal, cross-lagged panel analysis
Introduction
There is extensive literature on the potential associations between religious involvement and various health-related outcomes. Reviews of several studies suggest that religious involvement can have a beneficial effect on health that either prevents or delays adverse health outcomes such as mortality (Koenig, McCullough, and Larson 2001; Levin 2001). However, many of these studies are cross-sectional or only measure religious involvement once, and even the mortality studies could be subject to alternative interpretations. Poor health, for example, may be associated with both an increased risk for mortality and a reduced tendency to participate in religious activities. One study, for example, found women with a childhood onset of major depressive disorder to be less likely to attend religious services as an adult than women without such a history (Maselko et al. 2012). In addition to possible positive associations between religious involvement and health, there are also possible negative associations. High religious involvement might lead to negative health outcomes in some cases, particularly on measures of mental health, if persons become more sensitized through religious activities to possible punitive actions from a higher power. Illness might then be perceived as a punishment for sin (Ellison and Levin 1998; Holt, Clark, and Roth 2014). Alternatively, physical or mental health problems might positively affect religious involvement by prompting affected persons to seek “consolation,” or relief from their difficulties through increased religious activities or strengthened religious beliefs (Ferraro and Kelley-Moore 2000; Oates 2013). There are multiple possible mechanisms, therefore, that might result in observed associations between religious involvement and health-related variables.
Much of the research on the connections between religious involvement and health outcomes has been limited by cross-sectional designs or prospective analyses of subsequent mortality only. Information on temporal lead-lag relationships is therefore usually not available in such studies. Cross-sectional designs do not allow investigators to control for previous or baseline measures of health or religious involvement, or to detect meaningful changes over time on those constructs. Longitudinal designs with repeated measurements offer all of these advantages, which can then begin to inform temporal relationships and strengthen casual interpretations (Ellison and Taylor 1996; Levin and Taylor 1998; Son and Wilson 2011).
It is particularly important to better clarify the associations between religious involvement and health over time for African Americans, who tend to have higher rates of numerous chronic health conditions and higher mortality rates in comparison to Whites (Williams 2012), and higher levels of religious involvement than other race or ethnic subgroups (Levin, Taylor, and Chatters 1994; Taylor et al. 1996). African Americans also often show more pronounced religious involvement-health associations (Ferraro and Kim 2014; Levin, Chatters, and Taylor 2005). For African Americans, religious organizations may be important vehicles for social support and for receiving information on healthy lifestyles and preventive care (Campbell et al. 2007; Ellison et al. 2010).
The purpose of the present study was to evaluate concurrently (1) the impact of religious involvement on changes in health over time, and (2) the impact of health on changes in religious involvement over time in a national sample of African American adults. Cross-lagged panel analyses were conducted on longitudinal data collected over a 2.5-year period from 290 participants in the Religion and Health in African Americans (RHIAA) study (Holt et al. 2015; Holt et al. 2014). Evidence for changes in health over time as a function of baseline religious involvement would support previous theories and research suggesting that religious involvement plays a causal role in health-related outcomes. Conversely, evidence of baseline health affecting changes in religious involvement might support “consolation” interpretations or other mechanisms of reverse causality.
Methods
Participants
All participants in the RHIAA study are African American adults who reside in the United States and were 21 or more years of age at the time of the baseline telephone interview. Eligible participants were those who spoke English, self-identified as being African American, and were 21 years of age or older. The study sample was assembled by an external subcontractor (OpinionAmerica). Telephone calls were attempted without any previous notification about the study, and 19% of those contacted agreed to participate. Most of those who refused did so before the study was explained and eligibility was determined. Of those who were determined to be eligible, 94% agreed to participate in the study. Participants provided verbal assent after being read an informed consent script, and they received a $25 gift card by mail after completing each interview.
The RHIAA study consists of two separate subsamples, and the SF-12v2 measure of health-related quality of life was administered to only the second subsample. Both subsamples are population-based samples of community-dwelling African American adults living in the United States. Of the 803 participants in the second subsample who completed the baseline interview, 314 (39%) were re-contacted 2.5 years later and agreed to complete the 2nd longitudinal assessment. The sampling, recruitment, and retention methods used in the RHIAA study are described in more detail elsewhere (Holt, Clark, and Roth 2014; Holt et al. 2015; Holt et al. 2014). Previous analyses of retention in the RHIAA study found that the retained participants were slightly but significantly older, more educated, more likely to be female, and less likely to report “poor” self-rated health status than those who were not retained from wave 1 to wave 2 (Holt et al. 2015).
Of the 314 participants who completed both telephone interviews, 24 (7.6%) had missing data on either the religious involvement or SF-12v2 measures from either the baseline (wave 1) or follow-up (wave 2) interviews, leaving 290 participants (123 men, 167 women) with complete data for the present analyses.
Measures
Religious involvement
Religious involvement was assessed using an instrument that has been previously validated for use with African Americans (Lukwago et al. 2001; Roth et al. 2012). This 9-item instrument assesses two components: religious beliefs (e.g., “I feel the presence of God in my life.”; “I have a close personal relationship with God.”; Cronbach’s α = .90 in present sample) and religious behaviors (e.g., church service attendance; involvement in other church activities; talking openly about faith with others; Cronbach’s α = .73 in present sample). Seven items use a 5-point Likert-type format, and two monthly service attendance items use a 3-point response format. Scores can range from 4–20 for religious beliefs and 5–21 for religious behaviors, with higher scores indicating higher religious involvement.
Health-related quality of life
The Medical Outcomes Survey 12-item Short Form (SF-12v2) was used to assess general health functioning (Ware et al. 2002). Most items use a 5-point Likert-type response format to assess how much health problems interfere with daily functioning. The physical component summary (PCS) and mental component summary (MCS) scores were extracted using standard norm-based algorithms (Ware et al. 2002). The resulting PCS and MCS scores have population means of 50, population standard deviations of 10, and a population correlation coefficient of 0. That is, the summary scores for physical and mental health are derived such that they are mostly independent or uncorrelated with each other. Higher scores on the PCS and the MCS indicate better functioning and fewer health-related difficulties with quality of life.
Demographics
Standard interview questions were used to assess demographic characteristics. Covariates included in the present analyses were participant gender, age at the baseline interview, educational attainment, and household income.
Analytic Strategy
Paired t-tests were used to determine whether religious involvement or the SF-12v2 variables changed significantly from wave 1 to wave 2. Structural equation modeling (SEM) was then used to conduct cross-lagged panel analyses across time that examined whether religious involvement and health variables at wave 1 predicted changes in religious involvement and health variables at time 2. The SEM analyses were conducted using version 7 of Mplus (Muthén and Muthén 2013). Maximum likelihood estimation was used and standardized regression coefficients (STDYX in Mplus, reported as β in the present paper) were tested for statistical significance. These standardized regression coefficients indicate the difference, in standard deviation units, on the outcome variable per one standard deviation difference on the predictor variable after accounting for the other predictors of that outcome variable. A β of .20, for example, indicates that a 1.0 standard deviation difference on the predictor is associated with a difference of one-fifth of a standard deviation on the outcome.
A saturated model was examined first such that each variable at wave 2 (religious beliefs, religious behaviors, SF-12 PCS, and SF-12 MCS) was regressed on all four of these variables from the wave 1 interviews and on the four demographic covariates (gender, age, education, and income). Thus, when PCS and MCS at wave 2 were examined as outcome variables, their respective wave 1 scores were included as predictors along with wave 1 measures of religious beliefs and religious behaviors. The standardized regression coefficients for religious beliefs and religious behaviors, therefore, tested whether those religious involvement constructs predicted changes in physical or mental health over time from wave 1 to wave 2. Similarly, for religious beliefs and religious behaviors as outcomes at wave 2, predictors included the respective wave 1 observations of each variable, the four demographic covariates, and the PCS and MCS measures from the SF-12 at wave 1. The standardized regression coefficients for PCS and MCS tested whether those health variables at wave 1 predicted changes in religious involvement from wave 1 to wave 2. After the saturated model was fit, all non-significant predictive paths from religious beliefs, religious behaviors, PCS, or MCS from wave 1 to wave 2 were removed to achieve a more parsimonious or “trimmed” model that still provided excellent fit to the observed data. In addition, because religious beliefs and religious behaviors were moderately correlated at wave 1 (r = .58, p < .0001), these religious involvement predictors of the SF-12 scores at wave 2 were further examined in separate models in order to delineate possible redundant predictive effects or suppression effects.
Results
Descriptive Statistics
Table 1 displays the means and standard deviations for the study variables. Neither measure of religious involvement showed significant change over the 2.5-year interval with only slight and non-significant increases reported. No significant change was also noted for the MCS, but the PCS score showed a significant decrease over time (t(289) = −2.15, p = .03). This finding indicates a general aging effect over the 2.5-year interval on physical health functioning.
Table 1.
Descriptive Statistics and Changes over 2.5 Years for 290 African Americans
| Wave 1 | Wave 2 | p | |
|---|---|---|---|
| Religious beliefs: M (SD) | 18.00 (2.70) |
18.04 (2.62) |
.76 |
| Religious behaviors: M (SD) | 16.19 (3.38) |
16.47 (3.32) |
.12 |
| SF-12 PCS: M (SD) | 44.72 (11.54) |
43.36 (11.22) |
.03 |
| SF-12 MCS: M (SD) | 52.72 (9.40) |
52.26 (9.95) |
.45 |
| Age: M (SD) | 58.91 (12.70) |
-- | -- |
| Female: N (%) | 167 (57.59) |
-- | -- |
| Education: < High school: N (%) | 24 (8.28) |
-- | -- |
| High school or GED only: N (%) | 96 (33.10) |
-- | -- |
| Some college: N (%) | 73 (25.17) |
-- | -- |
| College graduate or beyond: N (%) | 97 (33.45) |
-- | -- |
| Income: ≤$20,000: N (%) | 78 (26.90) |
-- | -- |
| $20,000 – $40,000: N (%) | 62 (21.38) |
-- | -- |
| >$40,000: N (%) | 103 (35.52) |
-- | -- |
| Missing, refused to provide: N (%) | 47 (16.21) |
-- | -- |
Predictive Effects in Longitudinal Analyses
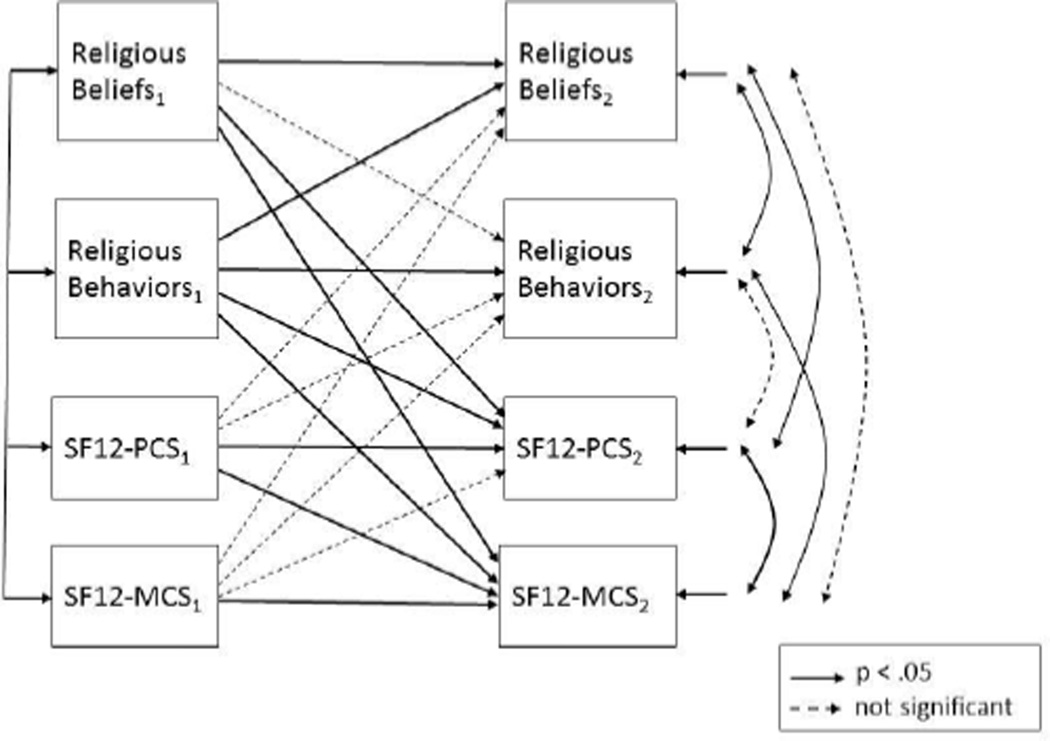
The results of the cross-lagged panel analyses are summarized in Figure 1. Paths that were tested as part of the saturated model but not found to be statistically significant are illustrated in dashed lines, whereas effects that were statistically significant in both the saturated and trimmed models are depicted as solid lines. All effects were tested after adjusting for age, gender, education, and income. Only those effects from the final trimmed model are summarized here unless otherwise noted.
Figure 1.
Cross-Lagged Panel Analysis of Religious Involvement and Health over a 2.5-Year Period in a National Sample of African Americans (N = 290)
For each of the four outcome variables at wave 2, the same variable at wave 1 showed a highly significant “autoregressive” effect (all β > .40, all p < .001). After adjusting for these autoregressive effects and for the demographic covariates, PCS scores at wave 2 were further predicted in a positive direction by wave 1 levels of religious beliefs (β = .20, p = .001) and in a negative direction by wave 1 levels of religious behaviors (β = −.12, p = .04). Subsequent models that examined the two religious involvement predictors from wave 1 separately indicated a significant effect for religious beliefs (β = .11, p = .01) but not for religious behaviors (β = −.01, p = .78) on wave 2 PCS. Thus, the negative effect for religious behaviors in the saturated and final trimmed models indicates a suppression effect due the strong correlation between religious behaviors and religious beliefs at wave 1 (r = .58). Similarly, MCS scores at wave 2 were further predicted in a positive direction by wave 1 religious beliefs (β = .20, p = .001), but in a negative direction by wave 1 religious behaviors (β = −.14, p = .03). When religious involvement factors from wave 1 were analyzed separately, the findings were similar to what was observed for PCS, with a significant effect for wave 1 religious beliefs (β = .13, p = .01), but not for wave 1 religious behaviors (β = −.03, p = .62). In addition, wave 2 MCS scores were also predicted by wave 1 PCS scores (β = .20, p < .001).
There were no statistically significant effects in the saturated model for either PCS or MCS at wave 1 when examined as predictors of changes in religious beliefs or religious behaviors at wave 2 (all β < .09, p > .12). Consequently, these paths were removed (i.e., their effects forced to be 0) in the final trimmed model displayed in Figure 1. In addition, the religious behaviors measure at wave 1 was found to be a significant predictor of religious beliefs at wave 2 (β = .15, p = .009). The final trimmed model was found to provide an excellent fit to the observed data, with no significant difference between the observed covariances among the variables and the covariances that could be accounted for by the model (χ2 (df = 8) = 13.00, p = .11, root mean square error of approximation = .046).
Discussion
The results of these analyses support contentions from numerous previous studies that religious involvement can have a positive impact on both physical and mental health. The present findings provide new information on the temporal nature of these relationships through the use of a longitudinal cross-lagged panel analysis design, and they further clarify the nature of these effects for African Americans by indicating that their health is improved or maintained more by their more personal religious beliefs than by their more public religious behaviors. It is also apparent that high religious beliefs appear to provide health benefits for African Americans that are quite general, across both physical and mental health domains. The similar pattern of predictive effects for religious beliefs and religious behaviors across both physical and mental health indicators was found even though the PCS and MCS are scaled so that they are largely independent and uncorrelated with each other. It is also compelling that these strikingly similar patterns of change were observed over a relatively brief 2.5-year time period between the wave 1 and wave 2 assessments.
Although religious beliefs at wave 1 had positive effects on both physical and mental health 2.5 years later, religious behaviors showed a more complicated pattern of effects on health. No significant effects were found for religious behaviors on changes in health when religious behaviors were examined alone. These findings are consistent with those of Levin and Taylor (1998), who found no longitudinal effects for religious behaviors on measures of subsequent well-being in panel analyses that controlled for baseline well-being. Our findings extend beyond those of Levin and Taylor by uncovering small but statistically significant, negative suppression effects for religious behaviors on subsequent health which were examined in conjunction with the predictive effects of religious beliefs. Furthermore, religious behaviors at wave 1 predicted increases in religious beliefs at wave 2. Taken together, our findings suggest that religious behaviors (e.g., church attendance) do not positively impact changes in health directly, but may do so indirectly by strengthening one’s religious beliefs over time.
The present findings did not reveal any evidence to indicate that health at wave 1 affected changes in either religious beliefs or religious behaviors at time 2. Previous authors have suggested that individuals might increase their religious involvement in search of “consolation” or comfort when confronted with illnesses or serious health problems (Ferraro and Kelley-Moore 2000), but our findings are consistent with other recent reports that illness-induced consolation is not a common occurrence among African Americans (Oates 2013). Although “consolation” responses may still occur in specific cases, such as for those experiencing a health crisis, such experiences do not appear to be common or to occur often enough to be registered as a significant finding in a population-based sample. Likewise, the complementary hypothesis – that health problems might interfere with religious activities – may also occur in some individual cases, but was not supported as a general pattern due to the lack of a longitudinal PCS-religious behaviors relationship in the present analyses.
The present findings may have implications for clinical service providers who are treating African Americans with physical or mental health problems. Historically, the Church has been a major coping resource for African Americans (Lincoln and Mamiya 1990), and many African American churches and clergy are comfortable linking health topics and health behaviors with faith-related matters (Lumpkins et al. 2013). Our findings suggest that health providers should consider assessing the religious beliefs of their African American patients and utilizing those beliefs as a possible mechanism for improving health. We emphasize that religious beliefs appear to provide the potential pathway to improved health, more so than just encouraging more church attendance and other forms of religious behaviors.
Limitations of the current work include the sole reliance on self-report data and the partial follow-up data that were obtained. It is not known, for example, if different findings would have been observed for those participants who were not retained for the longitudinal follow-up interviews, and individuals with poor health status at wave 1 were somewhat less likely to be retained. The present results also apply only to African Americans, and most of the sample consisted of Protestant Christians. Future research would be needed to determine if similar findings are observed in other race, ethnic, and religious denomination groups.
In addition to conducting research with other ethnic and religious populations, future work should also include more longitudinal waves of data that will allow more sophisticated causal models to be examined. Ongoing analyses in the RHIAA study are further examining possible longitudinal mechanisms for the health benefits of religious involvement. Using mediation modeling, we are determining if religious beliefs or behaviors influence health outcomes through their effects on promoting healthier lifestyles (e.g., better diet, less smoking) or more positive self-perceptions. Such hypotheses have been supported from cross-sectional analyses of the wave 1 data (Holt, Clark, and Roth 2014; Holt et al. 2014), but additional longitudinal waves of data are necessary to subject such causal models to a more rigorous evaluation of hypothesized temporal relationships.
In summary, the present results suggest that, for African Americans, religious involvement has stronger predictive effects on preserving health over time than health status has on altering levels of religious involvement. Strengthening the personal religious beliefs of African Americans appears to be one potential tool for improving their health, and potentially, for reducing some race disparities in health functioning. Our results suggest that simply attending religious services will not, by itself, achieve health benefits, but if greater religious involvement leads to increases in social support (Shor and Roelfs 2013) or healthier attitudes and personal beliefs, then health benefits might be expected accrue over time.
Acknowledgments
This work was supported by grants from the National Cancer Institute (R01 CA 105202; R01 CA154419) and a grant from the Duke University Center for Spirituality, Theology, and Health, through the John Templeton Foundation (#11993).
Footnotes
Note: The data used in these analyses were collected as part of the Religion and Health in African Americans (RHIAA) study directed by Cheryl Holt. Information on how to apply for a data use agreement to receive a copy of the de-identified data for replication purposes may be obtained from Dr. Holt upon written request.
Contributor Information
David L. Roth, Center on Aging and Health, Johns Hopkins University
Therri Usher, Center on Aging and Health, Johns Hopkins University.
Eddie M. Clark, Department of Psychology, Saint Louis University
Cheryl L. Holt, Department of Behavioral and Community Health, University of Maryland
References
- Campbell Marci K, Hudson Marlyn A, Resnicow Ken, Blakeney Natasha, Paxton Amy, Baskin Monica. Church-based health promotion interventions: Evidence and lessons learned. Annual Review of Public Health. 2007;28(33):213–234. doi: 10.1146/annurev.publhealth.28.021406.144016. [DOI] [PubMed] [Google Scholar]
- Ellison Christopher G, Hummer Robert A, Burdette Amy M, Benjamins Maureen R. Race, religious involvement, and health: The case of African Americans. In: Ellison Christopher G, Hummer Robert A., editors. Religion, families and health: Population-based research in the United States. New Brunswick, NJ: Rutgers University Press; 2010. pp. 321–348. [Google Scholar]
- Ellison Christopher G, Levin Jeffrey S. The religion-health connection: Evidence, theory, and future directions. Health Education and Behavior. 1998;25(6):700–720. doi: 10.1177/109019819802500603. [DOI] [PubMed] [Google Scholar]
- Ellison Christopher G, Taylor Robert J. Turning to prayer: Social and situational antecedents of religious coping among African Americans. Review of Religious Research. 1996;38(2):111–131. [Google Scholar]
- Ferraro Kenneth E, Kelley-Moore Jessica A. Religious consolation among men and women: Do health problems spur seeing. Journal for the Scientific Study of Religion. 2000;39(2):220–234. [Google Scholar]
- Ferraro Kenneth F, Kim Seoyoun. Health benefits of religion among black and white older adults? Race, religiosity, and C-reactive protein. Social Science and Medicine. 2014;120(1):92–99. doi: 10.1016/j.socscimed.2014.08.030. [DOI] [PubMed] [Google Scholar]
- Holt Cheryl L, Clark Eddie M, Roth David L. Positive and negative religious beliefs explaining the religion–health connection among African Americans. International Journal for the Psychology of Religion. 2014;24(4):311–331. doi: 10.1080/10508619.2013.828993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt Cheryl L, Le Daisy, Calvanelli Joe, Huang Jin, Clark Eddie M, Roth David L, Williams Beverly, Schulz Emily. Participant retention in a longitudinal national telephone survey of African-American men and women. Ethnicity and Disease. 2015;25(1):187–192. [PMC free article] [PubMed] [Google Scholar]
- Holt Cheryl L, Roth David L, Clark Eddie M, Debnam Katrina. Positive self-perceptions as a mediator of religious involvement and health behaviors in a national sample of African Americans. Journal of Behavioral Medicine. 2014;37(1):102–112. doi: 10.1007/s10865-012-9472-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koenig Harold G, McCullough Michael E, Larson David B. Handbook of religion and health. New York: Oxford University Press; 2001. [Google Scholar]
- Levin Jeffrey S. God, faith, and health: Exploring the spirituality-healing connection. Hoboken, NJ: Wiley and Sons; 2001. [Google Scholar]
- Levin Jeffrey S, Chatters Linda M, Taylor Robert J. Religion, health and medicine in African Americans: Implications for physicians. Journal of the National Medical Association. 2005;97(2):237–249. [PMC free article] [PubMed] [Google Scholar]
- Levin Jeffrey S, Taylor Robert J. Panel analyses of religious involvement and well-being in African Americans: Contemporaneous vs. longitudinal effects. Journal for the Scientific Study of Religion. 1998;37(4):695–706. [Google Scholar]
- Levin Jeffrey S, Chatters Linda M. Race and gender differences in religiosity among older adults: Findings from four national surveys. Journal of Gerontology: Social Sciences. 1994;49(3):S137–S145. doi: 10.1093/geronj/49.3.s137. [DOI] [PubMed] [Google Scholar]
- Lincoln C Eric, Mamiya Lawrence H. The black church in the African American experience. Durham, NC: Duke University Press; 1990. [Google Scholar]
- Lukwago Susan N, Kreuter Matthew W, Bucholtz Dawn C, Holt Cheryl L, Clark Eddie M. Development and validation of brief scales to measure collectivism, religiosity, racial pride, and time orientation in urban African American women. Family and Community Health. 2001;24(3):63–71. doi: 10.1097/00003727-200110000-00008. [DOI] [PubMed] [Google Scholar]
- Lumpkins Crystal Y, Allen Greiner K, Daley Christine, Mabachi Natabhona M, Neuhaus Kris. Promoting healthy behavior from the pulpit: Clergy share their perspectives on effective health communication in the African American church. Journal of Religion and Health. 2013;52(4):1093–1107. doi: 10.1007/s10943-011-9533-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maselko Joanna, Hayward R David, Hanlon Alexandra, Buka Stephen, Meador Keith. Religious service attendance and major depression: A case of reverse causality? American Journal of Epidemiology. 2012;175(6):576–583. doi: 10.1093/aje/kwr349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén Linda K, Muthén Bengt O. Mplus user’s guide. 7th. Los Angeles: Muthén and Muthén; 2013. [Google Scholar]
- Oates Gary L. Enhanced religiosity following illness? Assessing evidence of religious consolation among black and white Americans. Review of Religious Research. 2013;55(4):997–1003. doi: 10.1007/s13644-013-0118-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth David L, Mwase Isaac, Holt Cheryl L, Clark Eddie M, Lukwago Susan N, Kreuter Matthew W. Religious involvement measurement model in a national sample of African Americans. Journal of Religion and Health. 2012;51(2):567–578. doi: 10.1007/s10943-011-9475-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shor Eran, Roelfs David J. The longevity effects of religious and nonreligious participation: A meta-analysis and meta-regression. Journal for the Scientific Study of Religion. 2013;52(1):120–145. [Google Scholar]
- Son Joonmo, Wilson John. Religiosity, psychological resources, and physical health. Journal for the Scientific Study of Religion. 2011;50(3):588–603. doi: 10.1111/j.1468-5906.2011.01588.x. [DOI] [PubMed] [Google Scholar]
- Taylor Robert J, Chatters Linda M, Jayakody Rukmalie, Levin Jeffrey S. Black and white differences in religious participation: A multisample comparison. Journal for the Scientific Study of Religion. 1996;35(4):403–410. [Google Scholar]
- Ware John E, Kosinski Mark, Turner-Bowker Diane M, Gandek Barbara. User’s manual for the SF-12v2® health survey. Lincoln, RI: QualityMetric Inc.; 2002. [Google Scholar]
- Williams David R. Miles to go before we sleep: Racial inequities in health. Journal of Health and Social Behavior. 2012;53(3):279–295. doi: 10.1177/0022146512455804. [DOI] [PMC free article] [PubMed] [Google Scholar]