Abstract
Objective
Develop a novel theatre-based program and test its feasibility, tolerability, and preliminary efficacy for improving empathy/compassion and well-being among older adults.
Method
Thirteen older adults were randomized to a 6-week Drama Workshop (DW) program or time-equivalent Backstage Pass (BP) control condition. Pre- and post-treatment measures included empathy, compassion, and mood scales. Additional post-treatment measures included self-rated change in empathy/compassion, confidence, and affect. Participants also rated their mood/affect after each session.
Results
The program was successfully completed and well-liked. No pre-to-post-treatment changes in empathy/compassion or mood symptoms were found in either group. Compared to BP, DW weekly ratings indicated higher levels of anxiety and lower happiness; however, the DW program had higher self-ratings of positive change in self-esteem, confidence, and happiness post-treatment.
Discussion
While the DW may not promote empathy/compassion and was personally challenging during the program, engagement in dramatic exercises and rehearsing and performing a dramatic piece was seen by participants as a positive growth experience, as indicated by the post-treatment ratings of enhanced self-esteem, confidence and happiness. Thus, such a program might be useful for counteracting some of the potential negative aspects of aging, including reduced self-efficacy due to physical limitations and negative affect due to losses.
Keywords: successful aging, drama instruction, positive psychological traits, randomized controlled trial, community engagement
Introduction
The United States population is aging at a rapid rate due to advances in immunizations, medical care, and an increased focus on healthy living (e.g., better diet; decreased smoking rates) (Office, 2011; Ortman, Velkoff, & Hogan, 2014; van Meijgaard & Fielding, 2012). The U.S. Census Bureau estimates that by 2050, the number of individuals aged 65 and over will double from 43.1 million in 2012 to 83.7 million (Ortman et al., 2014). While living longer is associated with increased risk for debilitating diseases, such as dementia and cancer, current prevalence estimates predict the majority of the aging population will not experience such conditions (Hugo & Ganguli, 2014). Rather, the most frequent issues faced by individuals aged 65 and over are non-pathological age-related changes, including normal age-related declines in cognition, increasing physical limitations, and loss of partners and peers (Depp, Vahia, & Jeste, 2010). Facilitating the maintenance of good quality of life and factors that improve well-being in late life, despite these age-related changes, is imperative (Jeste & Palmer, 2013; Moore, Eyler, et al., 2015; Polyakova et al., 2014; Steffens, Fisher, Langa, Potter, & Plassman, 2009).
In recent years, research has highlighted the positive impact of social support in the aging population (Holt-Lunstad, Smith, & Layton, 2010). Increased social support has been show to predict better cognitive performance (Seeman, Lusignolo, Albert, & Berkman, 2001), greater life satisfaction (Siedlecki, Salthouse, Oishi, & Jeswani, 2014), improved health-related quality of life (Prevention, 2009), and reduction in risk for age-related disabilities (Mendes de Leon, Gold, Glass, Kaplan, & George, 2001). A lack of social support is associated with increased loneliness, which is a known predictor of increased risk for morbidity and mortality (Perissinotto, Stijacic Cenzer, & Covinsky, 2012). Therefore, studies focused on increasing social connectedness among older adults are likely to have a positive impact on quality of life and well-being.
Empathy and compassion are constructs that have been identified as contributing to the development and maintenance of healthy interpersonal relationships (Crocker & Canevello, 2008; Lim, Condon, & DeSteno, 2015; Trobst, Collins, & Embree, 1994). Empathy can be defined as an individual’s ability to feel with another or to put one’s self in another’s shoes (Reynolds & Scott, 1999; Zaki, Bolger, & Ochsner, 2008), whereas compassion can be conceptualized as a sympathetic concern of another’s suffering together with an active desire to relieve that suffering; in other words, compassion is considered an outward behavioral expression of empathy (Halifax, 2012). While a growing body of literature has evaluated the neurobiological and demographic factors contributing to empathy and compassion in late life (Moore, Dev, Jeste, Dziobek, & Eyler, 2015; Moore, Martin, et al., 2015), no research has yet assessed whether these constructs can be directly modified among older adults. Our previous work identified a link between experiencing a negative life event within the past year and greater compassion in late life, which helped shape the goals of the present study (Moore, Martin, et al., 2015).
This study, termed the Empatheatre Project, examined the preliminary efficacy of a theatre-based program for altering levels of empathy, compassion and well-being in an older adult community sample by exercising the neural systems that are used to put oneself in another’s shoes (Moore, Dev, et al., 2015; Singer & Lamm, 2009). Fundamentally, embodying a role as an actor involves temporarily adopting the physical and mental attributes of another in order to create a believable scenario for the observer. In correlational studies examining the relationship between empathy and acting, research has been mixed. In one study, group differences in empathy were found among actors compared to nonactors (Nettle, 2006), whereas another study found no differences between actors and nonactors on self-reported levels of empathy (Goldstein, Wu, & Winner, 2009). More recently, researchers have begun to examine the causal impact of acting on various outcomes. In one study, four-weeks of dramatic instruction was shown to significantly improve well-being and cognitive functioning (word reading and problem solving) among an older adult sample in comparison to individuals in a no-treatment control condition (Noice, Noice, & Staines, 2004). Another longitudinal study specifically evaluated the effectiveness of utilizing theatre-based programs in order to increase levels of empathy among elementary and high school students (Goldstein & Winner, 2012). Participants in this study received ten months of either acting or other arts training (music, visual arts) in an open-label, nonrandomized trial, and in both age groups participants in the acting group demonstrated post-treatment increases in empathy. Despite such findings, as of yet, no studies have evaluated the effectiveness of acting training programs for increasing empathy and compassion among older adults. As a first-step in testing the hypothesis that drama instruction would increase empathy and compassion in late life, we developed a theatre-based program and tested the feasibility (i.e., is this program capable of being done?), tolerability (i.e., is this program acceptable to the participants?) and preliminary efficacy of this program among a community sample of older adults. The study was performed in three Phases: Phase I – Focus Group; Phase II – Open-Label, Nonrandomized Treatment Trial, in which the participants chose to either participate in a drama-instruction program (treatment condition) or a theatre-learning program (control condition); and Phase III – Pilot Randomized Controlled Trial (RCT) comparing the drama-instruction program to the theatre-learning program.
Method
Participants
Twenty-six older adults were enrolled across three separate phases of the study (described below). Participants were eligible to co-enroll in Phases I and II; however, participation in Phases I or II excluded participation in Phase III. Phase III participants (mean age = 77) were primarily female, reported an average of 15.6 years of education and 92% of the sample self-identified as Caucasian (see Table 2). We partnered with Jewish Family Service Aging and Wellness Program’s College Avenue Center (hereafter referred to as the Center) to conduct this study, and most study-related activities were completed at the Center (with the exception of some of the assessment visits, which were conducted at UCSD or in the participants’ homes due to space constraints at the Center). Inclusion criteria included the following: (a) 65 years of age or older; (b) no current diagnosis or treatment for a serious mental illness or post-traumatic stress disorder; (c) no clinically-significant levels of depression on the Geriatric Depression Scale (GDS; Pocklington, Gilbody, Manea, & McMillan, 2016); (d) ability to read and write English at an 8th grade level, measured by the Wide Range Achievement Test-4 (WRAT-4; Wilkinson, 1993); and (e) unimpaired cognition, measured by the Montreal Cognitive Assessment screening test (MOCA; Nasreddine et al., 2005). Participants were not excluded if they were receiving psychotherapy or pharmacotherapy for depression or anxiety that was being effectively managed, as evidenced by a negative depression screen. All participants were recruited from the Center via presentations, advertisements in the Center’s newsletter, and flyers. Participants received the following compensation: (a) Phase I: $20; (b) Phase II: $45 at post-treatment assessment visit; (c) Phase III: $45 at pre-treatment assessment visit and $55 at post-treatment assessment visit.
Table 2.
Demographic and Baseline Characteristics.
| Drama Workshop (n=7) | Backstage Pass (n=6) | t-value | Cohen’s d | |
|---|---|---|---|---|
|
| ||||
| Age | 78.0 (8.1) | 75.2 (6.9) | 0.68 | 0.41 |
|
| ||||
| Gender (% female) | 71.4% | 83.3% | 0.47 | 0.28 |
|
| ||||
| Race/Ethnicity (%Caucasian) | 85.7% | 100% | -- | |
|
| ||||
| Education (years) | 15.3 (3.1) | 15.8 (1.6) | 0.39 | 0.24 |
|
| ||||
| Employment Status | 1.72 | 1.04 | ||
| % Retired | 100% | 66.7% | ||
| % Employed Part-Time | 0% | 33.3% | ||
|
| ||||
| Living Situation | 1.11 | 0.67 | ||
| % Live Alone | 28.6% | 66.7% | ||
| % Live with 1+ Other Person(s) | 71.4% | 33.3% | ||
|
| ||||
| Primary Outcome Measures - Baseline | ||||
|
| ||||
| TEQ | 52.3 (2.9) | 54.8 (4.6) | 1.21 | 0.73 |
|
| ||||
| SCBCS | 5.8 (1.3) | 6.2 (0.8) | 0.72 | 0.43 |
|
| ||||
| MET | ||||
| Cognitive Empathy | 20.57 (0.98) | 21.50 (1.38) | 1.42 | 0.86 |
| Affective Empathy | 7.49 (1.30) | 6.82 (1.66) | 0.82 | 0.49 |
|
| ||||
| GDS | 0.7 (1.1) | 0.7 (1.6) | 0.06 | 0.04 |
|
| ||||
| BAI | 8.0 (6.9) | 5.0 (6.1) | 0.73 | 0.44 |
Note.
p<0.05;
p<0.01;
Values are Mean (SD), unless otherwise noted. CES-D = Center for Epidemiologic Studies-Depression scale, Happiness subscale; TEQ = Toronto Empathy Questionnaire; SCBCS = Santa Clara Brief Compassion Scale; MET = Multifaceted Empathy Test; GDS = Geriatric Depression Scale; BAI = Beck Anxiety Inventory
Eighteen individuals were assessed for eligibility to participate in Phase III of the study. Of those evaluated, five were excluded for the following reasons: not meeting inclusion criteria (n = 1), declining to participate (n = 2), personal scheduling conflicts (n = 2). The remaining 13 participants were randomized into either the Drama Workshop treatment group (n = 7) or the Backstage Pass control group (n = 6). All 13 of the participants completed the study, including post-treatment assessments.
Procedure
The study protocol was approved by the UCSD Institutional Review Board. All participants provided written, informed consent. Phase I consisted of a two-hour long focus group comprised of five participants. The focus group was led by the first and senior authors (R.C.M. and L.T.E.), both of whom are licensed clinical psychologists. Feedback from the focus group was used to guide the refinement of treatment components, including the design of the control condition and logistics for Phases II and III. In Phase II, the drama-instruction program (Drama Workshop) and theatre-learning control (Backstage Pass) conditions were tested in an open-label, non-randomized dry-run trial. Participants were able to choose whether to participate in the Drama Workshop (DW) or Backstage Pass (BP) condition, and research staff were aware of the condition of the individual participants. The purpose of this dry-run was to perfect the aspects of each condition before embarking on the RCT phase. Six participants were enrolled in each group. Participants in both conditions received six weekly classes lasting approximately 1.5 hours. Following the six classes, participants in both conditions completed a satisfaction survey. After Phase II, we refined the syllabus for each group, specifically by eliminating more active components of the BP condition.
The final phase of the study, Phase III, was a pilot RCT comparing the effects of the DW and BP conditions on empathy, compassion, and other factors related to general well-being. Two trained Master’s level research assistants completed the pre- and post-treatment assessments. These research assistants were kept blind to randomization condition. Participants were compensated for each completed assessment but were not compensated for group participation. Seven participants were enrolled in the DW group and six participants were enrolled in the BP group. A presentation of study results was offered to all study participants at the completion of Phase III; 14 participants spanning all three Phases of the study attended this presentation.
Program Contents – DW and BP Conditions
Both conditions were facilitated by a professional actor, director, playwright, and associate theatre director (S.S.). The DW entailed participants serving as an audience for a dramatic reading by professional actors, engaging in drama exercises and self-exploration, and executing a final performance of sections of a play as a group. The play, An Accident by Lydia Stryk, was chosen for its emotionally laden content. Briefly, An Accident is a two person play in which a female victim of a car accident is visited at her bedside by the man who hit her. As the female character works toward recovery, the male character struggles with his guilt and responsibility. The DW was designed to introduce the participants to the process of preparing and delivering a dramatic reading and to engage them in activities that would facilitate self-reflection and engagement in the physical and emotional world of the play’s characters. Exercises included body work (e.g., breathing and movement), autobiographical exploration in a dramatic fashion (e.g., singing one’s life story), guided imagination, and learning how to impart intention, opinion, and imagery into a speech (e.g., saying I love you three different times while expressing three different opinions). Interleaved with these exercises was the preparation of the dramatic reading of the play, which followed a typical sequence used with trained actors, including an initial read-through (table work) and then scene work that involved reflecting on the characters’ emotions, practicing reading the lines with intention, opinion, and imagery, and thinking about the larger world inhabited by the characters. In addition, the reading of the play was rehearsed with feedback from the facilitator and finally performed within the group.
The BP condition involved listening to and asking questions of theatre experts. In this condition, different local theatre experts presented each week. This condition was designed to control for the time spent in the program, general social interaction, general theater-related content, and to be attractive enough so that potential participants would be willing to be randomized into this group. A summary of the content of each session is provided in Table 1.
Table 1.
Session Order and Content of the Drama Workshop and Backstage Pass Classes.
| Session No. | Drama Workshop: Session Details | Backstage Pass: Session Topic |
|---|---|---|
| 1 |
|
Scene design |
| 2 |
|
Voice and dialect coaching |
| 3 |
|
Sound design |
| 4 |
|
Playwriting and screenwriting |
| 5 |
|
Artistic direction |
| 6 |
|
Program review and wrap-up |
RCT Measures
Demographic information – pre-treatment
Demographic characteristics assessed included age, sex, race/ethnicity, level of formal education, and monthly household income.
Empathy and compassion scales
Participants completed the Toronto Empathy Questionnaire (TEQ) both pre- and post- treatment. The TEQ is a 16-item self-report questionnaire in which participants rate how frequently they feel or act in the manner described (e.g., I can tell when others are sad even when they do not say anything) on a 5-point scale from 0=Never to 4=Always. Scores on the TEQ are summed to derive a total score, with higher scores indicating greater empathy. Reliability and validity of the TEQ have been previously reported (Spreng, McKinnon, Mar, & Levine, 2009) and the internal consistency within our own sample was established with a Cronbach’s alpha of 0.87 at baseline.
The Santa Clara Brief Compassion Scale (SCBCS) was also administered both pre- and post-treatment. The SCBCS is a 5-item self-report questionnaire asking about feelings towards strangers (e.g., When I hear about someone (a stranger) going through a difficult time, I feel a great deal of compassion for him or her). Items are scored on a 7-point scale ranging from 1=Not at all true of me to 7=Very true of me, and responses are averaged to generate a total empathy/compassion score ranging from 1 to 7. Reliability and validity of the SCBCS have been previously reported (Hwang, Plante, & Lackey, 2008) and the internal consistency within our own sample was established with a Cronbach’s alpha of 0.89 at baseline.
Participants also completed the computerized Multifaceted Empathy Test (MET) at both assessment periods. The MET is an objective measure used to assess both cognitive and affective empathy. Cognitive empathy is defined as one’s ability to accurately interpret the emotions of others, whereas affective empathy is the capacity to have an emotional response to others’ distress (Shamay-Tsoory, Aharon-Peretz, & Perry, 2009). During this task, participants view a series of photographs, which mostly show people in emotionally laden contexts. To assess cognitive empathy, participants are asked to identify the emotional state of the person in the photo by choosing one of four offered emotions. Immediate feedback about the correct answer is provided. To assess affective empathy, participants are asked to rate their emotional reactions in response to the photos (e.g., How calm/aroused does this picture make you feel?) on a scale from 1=Calm/no concern to 9=Highly aroused/highly concerned. Our previous work has found distinct neural correlates of cognitive and affective empathy, assessed via the MET, in a small sample of older adults (Moore, Dev, et al., 2015). Reliability and validity of the MET have been previously reported (Dziobek et al., 2008) and the internal consistency within our own sample was established with a Cronbach’s alpha of 0.89 at baseline.
Mood questionnaires
Participants completed the Geriatric Depression Scale-Short Form (GDS) at both pre and post-treatment. This measure is designed to assess for symptoms of depression in older adults. Reliability and validity (Yesavage & Sheikh, 1986) as well as diagnostic sensitivity and specificity (Pocklington et al., 2016) of the GDS have been previously reported.
Symptoms of anxiety were also assess both pre- and post-treatment with the Beck Anxiety Inventory (BAI). Reliability and validity of the BAI has been previously reported (Creamer, Foran, & Bell, 1995).
Engagement and emotion ratings
Immediately upon completion of each weekly class, participants in both conditions completed a brief rating form that assessed their feelings about the day’s class on a scale from 1=Not at all to 9=Extremely in the following domains: engaged, challenged, interested, anxious, happy, satisfied, upset, and calm/aroused.
Program evaluation and subjective change
Participants completed a satisfaction survey at their post-treatment visit. Phase II participants were also asked to complete a satisfaction survey developed by the study team to assess the likeability and feasibility of the protocol to prepare for Phase III. Participants were asked questions including if they had fun participating, would recommend the program to others, found the material engaging and would be interested in participating in a similar program again. All questions were rated on a Likert scale from 1 to 5.
In addition to satisfaction ratings regarding the program, this survey included items on subjective change. Specifically, participants were asked to think back to how they were prior to starting the program compared to how they are today and rate their degree of change on several factors, including energy, kindness, sadness, happiness, stress, relaxed, forgetfulness, clarity of thinking, degree to which in tune with other peoples’ feelings, degree to which in tune with own feelings, confidence, and self-esteem, on a scale from −4=Less to +4=More (with 0=Same as was 6 weeks ago).
Evaluation tasks – post-treatment
Lastly, we developed and tested two tasks to assess participants’ willingness to engage in empathic/compassionate behaviors when they were unaware they were being assessed: a Charity Task and a Volunteer Task. The Charity Task aimed to test participants’ willingness to make monetary donations and their choices about distributions of any such donations. Participants were given $12 in single dollar bills and told that there was unexpected money left over in the study budget and the researchers decided to award it to the participants as bonus compensation. This bonus money was in addition to the compensation received for study participation. Participants were told they were welcome to keep all of the bonus money for themselves as a reward. They were also told that if they would like, they could elect to donate some or all of the bonus money to one of three charitable organizations by placing money in one of three envelopes. The envelopes had brief descriptions of real charity organizations in the San Diego community on them. The examiner presented the money and the envelopes and then turned away to pack-up testing supplies so the participant could have some privacy to decide whether to donate any of the bonus money. The amount and distribution of any donations were recorded after the participant left, and all donations were given to the respective charities at the completion of the study.
The Volunteer Task aimed to measure the participants’ willingness to volunteer their own time to a community service project. A real volunteer project at the Center was described to the participants and they were asked if they would like to participate or not. The tasks involved little skill or physical activity to include those with physical limitations, but were boring/repetitive enough to make participation somewhat of a sacrifice. Potential volunteering tasks included helping with tasks at the Center, including, serving lunch, helping with activities like Bingo, and working at the snack stand. Participants who were interested in volunteering their time were instructed to complete a form indicating their name, best way to reach them, how many hours they would be willing to volunteer, and what days and times are generally most convenient for them. Participants were provided with an envelope and a blank form, and instructed to place the form in the envelope when they were finished, regardless of whether or not they decided to volunteer. The form indicated how many people are needed at each slot and showed the number that have already signed up for each slot, but did not contain names of other participants (i.e., a clean sign-up sheet was used for each participant). As with the Charity Task, the examiner turned away and continued packing the testing supplies.
Data Analyses
Data was analyzed using SPSS version 23 (IBM Corp., 2013). Group differences for variables measured only at baseline or only at follow-up were examined with Chi-square tests for discrete variables and Student’s t-tests for continuous variables. Weekly post-class ratings were averaged across the 6 weeks for each item, and compared between groups with Student’s t-tests. For measures that were administered pre- and post-treatment, the effect of the program was tested by examining the group (DW vs. BP) by time (pre- vs. post-) interaction within a repeated-measures ANOVA with group, time, and the interaction as predictors. Given the preliminary nature of this study, no corrections for multiple comparisons were made. The effect size (Cohen’s d) is presented for each comparison, and moderate to large effects (d ≥ .45) are interpreted.
Results
Sample
All participants in Phase II completed the post-treatment satisfaction survey and all participants in Phase III 3 completed the post-treatment assessment visit.
Phase I
From the focus group, the investigators gained important insight about what types of activities would be comfortable for participants (e.g., a dramatic reading, but not a memorized part; a small within-group performance, but not in front of the whole Center) and how to maximize attendance (e.g., provide snacks at each class, have time slot not conflict with other popular classes at the Center). Four of the five Phase I participants volunteered for the Phase II open-label, nonrandomized dry run trial.
Phase II
We were successful in implementing the DW and BP groups in the dry-run, open label trial. Satisfaction levels (rated from 1 to 5) were high and generally equivalent for both groups in Phase II. Across both groups, participants reported that they had fun participating (mean DW = 5; mean BP = 5), would recommend this program to others (mean DW = 5; mean BP = 5), found the lessons interesting and well-presented (mean DW = 5.8; mean BP = 5; t = 1.00, p = 0.63), thought the program was interesting and well-presented (mean DW = 4.8; mean BP = 5; t = 1.00, p = 0.63), felt comfortable asking questions and expressing self in class (mean DW = 5; mean BP = 5), and would participate in a program like this again (mean DW = 4.3; mean BP = 5.0; t = 1.00, p = 0.63). Interestingly, self-reported positive changes in empathy were greater in the BP compared to DW group (t = 3.08, df = 10, p = 0.01, d = 1.95). Since we did not randomize participants and did not conduct pre- and post-treatment assessments in this Phase, we do not know if there were systematic differences in empathy at baseline. Based on our observations and on comments from participants, we attributed the potency of the BP group to the personalities of the particular experts who were interviewed, the personal nature of the discussions, the modeling of empathy by important and busy local theater professionals who volunteered their time to spend with the participants, and inclusion of powerful self-discovery exercises as part of one of the presentations. For Phase III, the self-discovery exercises were moved to the DW group and discussions in the BP group were steered away from more personal topics and towards professional activities.
Phase III
Participants
As seen in Table 3, participants in both conditions did not significantly differ on any demographic or baseline variables, suggesting that randomization was effective in minimizing pre-treatment differences between the groups.
Table 3.
Phase III Post-Class Ratings and Subjective Change
| Drama Workshop (n=7) | Backstage Pass (n=6) | t-value | Cohen’s d | |
|---|---|---|---|---|
| Post-Class Ratings: I was…. | ||||
| Engaged | 8.53 (0.45) | 8.49 (0.76) | 0.13 | 0.08 |
| Challenged | 8.15 (0.51) | 6.52 (2.90) | 1.47 | 0.89 |
| Interested | 8.44 (0.77) | 8.64 (0.50) | 0.59 | 0.36 |
| Anxious | 6.23 (1.55) | 2.25 (1.34) | 4.94** | 2.98 |
| Happy | 5.94 (1.13) | 7.79 (0.71) | 3.46** | 2.09 |
| Satisfied | 7.57 (1.21) | 8.30 (0.82) | 1.24 | 0.75 |
| Upset | 3.62 (2.43) | 1.70 (1.09) | 1.78 | 1.07 |
| Calm/Aroused | 6.91 (1.44) | 6.72 (1.63) | 0.23 | 0.14 |
| Subjective Change: Since participating in this program, I’ve seen the following changes in my… | ||||
| Energy | 1.67 (1.86) | 0.00 (0.00) | 2.19 | 1.39 |
| Kindness | 1.83 (1.60) | 0.67 (1.63) | 1.25 | 0.79 |
| Sadness | −0.67 (2.50) | 0.50 (1.23) | 1.03 | 0.65 |
| Happiness | 1.83 (1.72) | −0.50 (1.23) | 2.70* | 1.71 |
| Stress | −0.86 (1.46) | 0.33 (0.82) | 1.76 | 1.06 |
| Relaxed | 1.43 (1.51) | 0.50 (1.23) | 0.26 | 0.16 |
| Forgetfulness | 0.71 (1.25) | 0.67 (1.63) | 0.06 | 0.04 |
| Clarity of Thinking | 1.86 (1.57) | 0.67 (1.63) | 1.34 | 0.81 |
| Degree to Which I’m in Tune with Other Peoples’ Feelings | 2.14 (1.46) | 0.67 (1.63) | 1.72 | 1.04 |
| Degree to Which I’m in Tune with My Own Feelings | 2.00 (1.41) | 0.67 (1.63) | 1.58 | 0.95 |
| Confidence | 2.29 (1.50) | 0.00 (0.00) | 3.72* | 2.24 |
| Self-Esteem | 2.14 (1.35) | 0.33 (0.82) | 2.86* | 1.72 |
Note.
p<0.05;
p<0.01
Feasibility
We were successfully able to partner with a community-based organization and engage with the theatre community to develop and implement the Empatheatre program. As a result of this program, our relationship with our community partner was strengthened. Results of the study demonstrated excellent adherence to the study protocol, with no participants dropping out or lost to follow-up.
In terms of feasibility challenges, approximately 90% of Center members are female, which made the recruitment of male participants difficult. There were also challenges with locating assessment space in the busy Center, and many participants were tested in their homes or at UCSD. Lastly, consistency with attendance was challenging: during the RCT, three people missed one class each of the DW group and two people missed one class each, with one person missing two classes, of the BP group. Reasons for missing class were medical illness or doctor’s appointment (n=5), other plans (n=1), and extenuating circumstances (n=1; car would not start).
Tolerability of the Program
On weekly post-class ratings, participants reported mostly high positive feelings and low negative feelings and the groups did not differ (see Table 4). Significant group differences were found, however, for ratings of happiness and anxiousness. On average, the BP group reported significantly higher happiness and lower anxiety than the DW immediately after each class over the course of the program. Despite this, as mentioned above, all participants in both groups completed the study protocol.
Efficacy – Change in Empathy and Compassion
Contrary to our hypotheses, no significant treatment effect (group by time interaction) was found in regard to self-report or objective measures of empathy/compassion (TEQ: F = 1.5, p = 0.24, d = 0.90; SCBCS: F = 0.04, p = 0.84, d = 0.02; MET Cognitive Empathy: F = 1.83, p = 0.20, d = 1.10; MET Affective Empathy: F = 0.02; p = 0.89, d = 0.01). Further, no significant treatment effects were observed for depression (GDS: F = 0.53, p = 0.48, d = 0.03) or anxiety scores (BAI: F = 0.06, p = 0.82, d = 0.04). For all variables, the main effect of time was also not significant and effect sizes were low (all p’s > 0.05, all Cohen’s d’s < 0.45), suggesting no change from pre- to post- assessment for either BP or DW.
When examining group differences on the Charity and Volunteer Tasks, the Backstage Pass group donated significantly more of their bonus money to charity (DW = $4.3 ± $5.50, BP = $10.0 ± $3.3; t = 2.22, df = 11, p = 0.09). No group differences were found for amount of time participants were willing to volunteer to a future event (DW = 0.4 ± 0.5, BP = 0.2 ± 0.4; t = 0.98, df = 11, p = 0.35).
Efficacy – Subjective Change
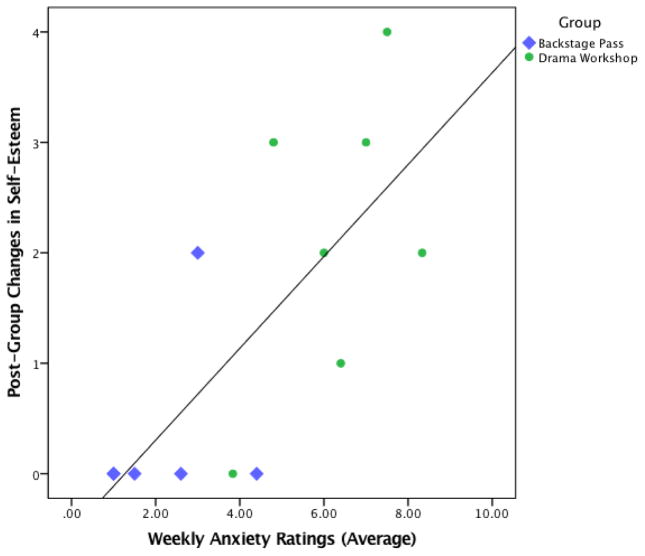
We also examined post-treatment self-rated change in emotional and psychological factors, and found that the DW group reported more positive change in happiness, confidence, and self-esteem than the BP group (Table 4). Follow-up analyses within the DW group indicated greater anxiety and less happiness after each class were related to increases in self-esteem (anxiety: r = 0.83, p = 0.04; happiness: r = −0.94, p < 0.01; see Figure 1 for a visual representation of group differences regarding the relationship between post-class anxiety and post-treatment self-esteem); less happiness after each class was also related to post-treatment increases in confidence (r = −0.94, p < 0.01). Neither post-class anxiety nor happiness was related to overall changes in happiness, and post-class anxiety was unrelated to overall changes in confidence (p’s > 0.5).
Figure 1.
Greater post-class anxiety and less happiness in the Drama Workshop related to post-treatment increase in self-esteem.
Program Evaluation Results
Program evaluations were collected from all participants in Phase III. Participants in the DW group (mean ± SD = 4.6 ± 0.8) and BP group (mean ± SD = 4.5 ± 0.3) did not significantly differ in terms of satisfaction with the program (t = 0.16, df = 11, p =0.88, d = 0.10), likelihood of recommending this program (DW = 4.9 ± 0.38, BP = 4.3 ± 0.8; t = 1.53, df = 11, p = 0.16, d = 0.92), feeling the lessons were interesting and well-presented (DW = 5.0 ± 0, BP = 5.0 ± 0; t = N/A), feeling the program was well-organized and easy to understand (DW = 4.7 ± 0.76, BP = 4.8 ± 0.41; t = 0.34, df = 11, p = 0.74, d = 0.21), comfort asking questions and expressing themselves in class (DW = 5.0 ± 0, BP = 5.0 ± 0; t = N/A), or interest in participating in a program like this again (DW = 4.8 ± 0.41, BP = 4.2 ± 0.98; t = 1.53, df = 10, p = 0.16, d = 0.97). One participant in the DW group and two participants in the BP group expressed that they wished they had been randomized to the other class.
Discussion
The Empatheatre Project pilot study examined the efficacy of drama instruction compared to passive exposure to theater personnel to alter levels of empathy, compassion and well-being in a small sample of community dwelling older adults. In the DW group, older adults learned to embody a role (i.e., temporarily adopting physical and mental attributes of a character) by engaging in drama exercises and performing sections of a play. In the BP control group, older adults attended a series of discussion sessions involving local theatre experts. After conducting a focus group and a dry-run of both the BP and DW condition in order to tailor treatment components, a randomized controlled trial was conducted in Phase III, and pre-and post-treatment assessments of positive psychological traits and mood symptoms were collected from all participants. This pilot study demonstrated excellent adherence to the study protocol, a perfect retention rate, and high participant satisfaction, indicating that this program is both feasible and well-tolerated by this population.
Contrary to our hypothesis, the DW program did not have a significant effect on measures of empathy and compassion in this preliminary sample. One possible explanation for this non-significant finding may be that the participants did not receive a strong enough dose of acting. Work by Goldstein and Winner (2012) showed increases in empathy among elementary school and high school students after participating in ten months of acting training (90 minutes/week for elementary school students and 5–9 hours per week for high school students). Thus, perhaps a longer and more intense acting dose of Empatheatre would result in changes in empathy and compassion among older adults. That a larger dose might be more effective in enhancing empathy is suggested by the large, though non-significant, effect size for the subjective rating of positive change in the degree to which I’m in tune with other people’s feelings. Similarly, older adults in the DW group did not report a reduced number of depression or anxiety symptoms after completion, though this is perhaps unsurprising given the exclusion of mental illness in the sample and the low baseline scores of depression and anxiety. Interestingly, older adults in the BP control group made larger monetary donations during the post-treatment Charity task compared to those in the DW program group. This could be because those in the BP group were exposed to many stories about the need for monetary support for the arts, or could be because the DW participants felt more entitled to keep bonus money after working hard on the program for six weeks. It is also possible, however, that the DW participants later donated the bonus money to friends or family rather than to the three charities we selected.
Importantly, although the DW group was more anxious and less happy after weekly meetings, they reported subjective increases in happiness, confidence and self-esteem compared to the BP group post-treatment. We further found that individuals reporting greater anxiety and less happiness following weekly sessions of the DW group indicated more positive changes in self-esteem and confidence post-treatment, suggesting that stepping out of one’s comfort zone may lead to greater empowerment in the future. We did not specifically measure which aspects of the DW condition were seen as anxiety provoking or led to lukewarm ratings of happiness after the class. However, we speculate that the sometimes distressing content of the play, the personally revealing and extroverted nature of the exercises, and the pressure to perform well during rehearsals and the final reading may have led to discomfort that led to slightly more negative post-class ratings in the DW compared to BP group. The finding that those participants who were least comfortable on a weekly basis were the same ones who said that they changed the most for the better in terms of self-esteem and confidence is analogous to the known phenomenon in physical exercise of needing to use a muscle past the point of comfort in order to gain strength. In addition, discomfort is also sometimes required for positive change within the context of psychotherapy (e.g., exposure therapy for anxiety disorders; Simmons, Norman, Spadoni, & Strigo, 2013), and more generally, mastery is unlikely to result if activities are insufficiently challenging (Roediger & Karpicke, 2006). Similarly, our previous work has demonstrated that both resilience and recent negative life events, independently, facilitate a desire to help others (Moore, Martin, et al., 2015) in a sample of older adults. Thus, it is possible that the experience of negative emotions may lead to positive growth in normal aging older adults. On the other hand, it is possible that cognitive dissonance drove the observed relationship between post-class ratings and post-treatment change ratings – those who were most uncomfortable may have been biased to report more growth in order to justify having endured this discomfort. Future longitudinal study designs are required to replicate and clarify interpretation of these findings. If they prove replicable, however, it would suggest that some of the negative effects of aging, such as decreases in positive affect due to loneliness or loss and reduced self-efficacy due to societal stigma around aging and increasing physical limitations, might be addressed with a program like the DW. The findings also suggest that treatments should not be designed to avoid negative affect or personal challenge at all times, since it appears that some struggle during the treatment was associated with greater feelings of improvement after the treatment was complete.
Limitations
There are several limitations to this study. First, as this was a pilot study, our sample size was small and each 6-week group was only conducted one time, which may have limited our ability to detect effects in our primary outcome measures. Additionally, we did not have the resources to conduct long-term follow-up assessments, which would allow us to examine any lasting effects of the DW group on improving confidence and self-esteem. A future larger trial with an additional focus on maintenance of effects is needed to truly test the efficacy of this treatment. Second, our design used an active control condition in which participants engaged with a different local theatre expert each week. While having an active control group allowed us to control for the effects of theatre professionals and peer contact, it may have limited our ability to detect efficacy. Although BP participants were not learning how to step into another’s shoes, they may have empathized with the stories of the starving artists of the theatre community, which in turn may have impacted study outcomes, including their desire to donate some of their bonus money. Furthermore, although we attempted to go beyond self-report measures of empathy and compassion, the real world tests of these constructs that we designed had several potential limitations to their validity. Behavior on the Charity task could have been influenced by an individual’s financial status, their dislike of the charities we chose, or attitudes about giving to charities versus family, friends, or religious groups. Behavior on the Volunteering task could have been influenced by transportation limitations, having just participated in a time-consuming voluntary activity, or the somewhat vague nature of the described activities. Additionally, all participants were recruited from the Center, which consists of a select community of older adults and limits generalizability of our findings. A majority of the participants were women and were Caucasian, which was representative of the Center’s demographic composition yet limited our ability to examine gender or racial/ethnic differences among the participants. Moreover, many of the participants knew each other prior to enrollment in the study, and some participants expressed that they had a friend in the other group. Therefore, despite encouragement from the research team to not disclose the content of the sessions to other Center members when engaged in the program, some treatment contamination effects likely occurred.
Conclusions
Notwithstanding these limitations, our preliminary evidence demonstrates the potential of the Drama Workshop program to improve well-being in late life. While we are unable to speculate on the long-term sustainability of the program’s effects, in the short-term it appears as though putting oneself in a novel, anxiety-provoking situation (in this case, by imagining the mental states of others and feeling their emotions, participating in self-discovery exercises, and receiving evaluative feedback in front of one’s peers) leads to empowerment. Findings from this study provide preliminary support for the notion that drama instruction in late-life may improve well-being; if future work can replicate these findings and provide evidence for their sustainability, there are positive implications for health and longevity.
Supplementary Material
Highlights.
Programs are needed to improve well-being in late life
We developed a novel theatre-based program focused on improving well-being
13 older adults participated in a Drama Workshop (DW) or control condition
Drama instruction may foster happiness, confidence, and self-esteem in late life
Acknowledgments
The authors would like to acknowledge Elissa Landsman and the Jewish Family Service of San Diego for their partnership in conducting this research, along with the staff of the College Avenue Center for help with set-up and logistics. We would also like to acknowledge UCSD staff and students who assisted with this project: Rebecca Daly, Elizabeth Farro, Savannah Raye Jones, Sidonie Kilpatrick, Nana Kori, and Cheyenne Minstry, as well as members of the San Diego theater community who gave generously of their time: Jacob Bruce, Charlotte Devaux, Barry Edelstein, David Ellenstein, Jan Gist, Joe Huppert, Stephen Metcalfe, Michael Murphy, Erika Philips, Delicia Turner-Sonnenberg, Greg Watanabe, Roberta Wells-Famula, and David Weiner.
Funding
This work was supported by the University of California, San Diego Frontiers of Innovation Scholars Program (FISP) [application number #P3041]; the National Institutes of Health (R.C.M., salary support, grant number K23 MH107260), and the Stein Institute for Research on Aging.
Footnotes
Declaration of Conflicting Interests
No conflicts of interest were declared.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Centers for Disease Control and Prevention. Healthy Aging: Improving health and quality of life among older Americans. 2009 Retrieved from http://www.cdc.gov/nccdphp/publications/aag/pdf/healthy_aging.pdf.
- Centers for Disease Control and Prevention. Healthy people 2010: Final review. 2011 Retrieved from http://www.cdc.gov/nchs/data/hpdata2010/hp2010_final_review.pdf.
- Creamer M, Foran J, Bell R. The Beck Anxiety Inventory in a non-clinical sample. Behavior Research and Therapy. 1995;33(4):477–485. doi: 10.1016/0005-7967(94)00082-u. Retrieved from http://www.sciencedirect.com/science/article/pii/000579679400082U. [DOI] [PubMed] [Google Scholar]
- Crocker J, Canevello A. Creating and undermining social support in communal relationships: The role of compassionate and self-image goals. Journal of Personality and Social Psychology. 2008;95(3):555–575. doi: 10.1037/0022-3514.95.3.555. http://dx.doi.org/10.1037/0022-3514.95.3.555. [DOI] [PubMed] [Google Scholar]
- Depp C, Vahia IV, Jeste D. Successful aging: Focus on cognitive and emotional health. Annual Reviews in Clinical Psychology. 2010;6:527–550. doi: 10.1146/annurev.clinpsy.121208.131449. http://dx.doi.org/10.1146/annurev.clinpsy.121208.131449. [DOI] [PubMed] [Google Scholar]
- Dziobek I, Rogers K, Fleck S, Bahnemann M, Heekeren HR, Wolf OT, Convit A. Dissociation of cognitive and emotional empathy in adults with Asperger syndrome using the Multifaceted Empathy Test (MET) Journal of Autism and Developmental Disorders. 2008;38(3):464–473. doi: 10.1007/s10803-007-0486-x. http://dx.doi.org/10.1007/s10803-007-0486-x. [DOI] [PubMed] [Google Scholar]
- Goldstein TR, Winner E. Enhancing empathy and theory of mind. Journal of Cognition and Development. 2012;13(1):19–37. http://dx.doi.org/10.1080/15248372.2011.573514. [Google Scholar]
- Goldstein TR, Wu K, Winner E. Actors are skilled in theory of mind but not empathy. Imagination, Cognition and Personality. 2009;29(2):115–133. http://dx.doi.org/10.2190/IC.29.2.c. [Google Scholar]
- Halifax J. A heuristic model of enactive compassion. Current Opinions in Supportive and Palliative Care. 2012;6(2):228–235. doi: 10.1097/SPC.0b013e3283530fbe. http://dx.doi.org/10.1097/SPC.0b013e3283530fbe. [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: A meta-analytic review. PLOS Medicine. 2010;7(7) doi: 10.1371/journal.pmed.1000316. http://dx.doi.org/10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hugo J, Ganguli M. Dementia and cognitive impairment: Epidemiology, diagnosis, and treatment. Clinics in Geriatric Medicine. 2014;30(3):421–442. doi: 10.1016/j.cger.2014.04.001. http://dx.doi.org/10.1016/j.cger.2014.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang JY, Plante T, Lackey K. The development of the Santa Clara Brief Compassion Scale: An abbreviation of Sprecher and Fehr’s Compassionate Love Scale. Pastoral Psychology. 2008;56:421–428. http://dx.doi.org/10.1007/s11089-008-0117-2. [Google Scholar]
- IBM Corp. IBM SPSS Statistics for Macintosh, Version 23.0. Armonk, NY: IBM Corp; Released 2013. [Google Scholar]
- Jeste DV, Palmer BW. A call for a new positive psychiatry of ageing. British Journal of Psychiatry. 2013;202:81–83. doi: 10.1192/bjp.bp.112.110643. http://dx.doi.org/10.1192/bjp.bp.112.110643. [DOI] [PubMed] [Google Scholar]
- Lim D, Condon P, DeSteno D. Mindfulness and compassion: An examination of mechanism and scalability. PLoS One. 2015;10(2):e0118221. doi: 10.1371/journal.pone.0118221. http://dx.doi.org/10.1371/journal.pone.0118221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendes de Leon CF, Gold DT, Glass TA, Kaplan L, George LK. Disability as a function of social networks and support in elderly African Americans and Whites: The Duke EPESE 1986–1992. Journal of Gerontology Series B: Psychological Sciences and Social Sciences. 2001;56(3):S179–190. doi: 10.1093/geronb/56.3.s179. Retrieved from http://psychsocgerontology.oxfordjournals.org/content/56/3/S179.long. [DOI] [PubMed] [Google Scholar]
- Moore RC, Dev SI, Jeste DV, Dziobek I, Eyler LT. Distinct neural correlates of emotional and cognitive empathy in older adults. Psychiatry Research. 2015;232(1):42–50. doi: 10.1016/j.pscychresns.2014.10.016. http://dx.doi.org/10.1016/j.pscychresns.2014.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore RC, Eyler LT, Mausbach BT, Zlatar ZZ, Thompson WK, Peavy G, … Jeste DV. Complex interplay between health and successful aging: Role of perceived stress, resilience, and social support. American Journal of Geriatric Psychiatry. 2015;23(6):622–632. doi: 10.1016/j.jagp.2014.08.004. http://dx.doi.org/10.1016/j.jagp.2014.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore RC, Martin AS, Kaup AR, Thompson WK, Peters ME, Jeste DV, … Eyler LT. From suffering to caring: A model of differences among older adults in levels of compassion. International Journal of Geriatric Psychiatry. 2015;30(2):185–191. doi: 10.1002/gps.4123. http://dx.doi.org/10.1002/gps.4123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nasreddine ZS, Phillips NA, Bedirian V, Charbonneau S, Whitehead V, Collin I, … Chertkow H. The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. Journal of the American Geriatric Society. 2005;53(4):695–699. doi: 10.1111/j.1532-5415.2005.53221.x. http://dx.doi.org/10.1111/j.1532-5415.2005.53221.x. [DOI] [PubMed] [Google Scholar]
- Nettle D. Psychological profiles of professional actors. Personality and Individual Differences. 2006;40:375–383. http://dx.doi.org/10.1016/j.paid.2005.07.008. [Google Scholar]
- Noice H, Noice T, Staines G. A short-term intervention to enhance cognitive and affective functioning in older adults. Journal of Aging and Health. 2004;16(4):562–585. doi: 10.1177/0898264304265819. http://dx.doi.org/10.1177/0898264304265819. [DOI] [PubMed] [Google Scholar]
- Ortman JM, Velkoff VA, Hogan H. An aging nation: The older population in the United States. Current Population Reports. 2014 Retrieved from https://www.census.gov/prod/2014pubs/p25-1140.pdf.
- Perissinotto CM, Stijacic Cenzer I, Covinsky KE. Loneliness in older persons: A predictor of functional decline and death. Archives of Internal Medicine. 2012;172(14):1078–1083. doi: 10.1001/archinternmed.2012.1993. http://dx.doi.org/10.1001/archinternmed.2012.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pocklington C, Gilbody S, Manea L, McMillan D. The diagnostic accuracy of brief versions of the Geriatric Depression Scale: A systematic review and meta-analysis. International Journal of Geriatric Psychiatry. 2016;31(8):837–857. doi: 10.1002/gps.4407. http://dx.doi.org/10.1002/gps.4407. [DOI] [PubMed] [Google Scholar]
- Polyakova M, Sonnabend N, Sander C, Mergl R, Schroeter ML, Schroeder J, Schonknecht P. Prevalence of minor depression in elderly persons with and without mild cognitive impairment: A systematic review. Journal of Affective Disorders. 2014;152–154:28–38. doi: 10.1016/j.jad.2013.09.016. http://dx.doi.org/10.1016/j.jad.2013.09.016. [DOI] [PubMed] [Google Scholar]
- Reynolds WJ, Scott B. Empathy: A crucial component of the helping relationship. Journal of Psychiatric Mental Health Nurses. 1999;6(5):363–370. doi: 10.1046/j.1365-2850.1999.00228.x. Retrieved from http://onlinelibrary.wiley.com/doi/10.1046/j.1365-2850.1999.00228.x/abstract;jsessionid=7AC78A48D26FB3D7193FAF1B293431DB.f03t03. [DOI] [PubMed] [Google Scholar]
- Roediger HL, Karpicke JD. Test-enhanced learning: Taking memory tests improves long-term retention. Psychological Science. 2006;17:249–255. doi: 10.1111/j.1467-9280.2006.01693.x. http://dx.doi.org/10.1111/j.1467-9280.2006.01693.x. [DOI] [PubMed] [Google Scholar]
- Seeman TE, Lusignolo TM, Albert M, Berkman L. Social relationships, social support, and patterns of cognitive aging in healthy, high-functioning older adults: MacArthur studies of successful aging. Health Psychology. 2001;20(4):243–255. doi: 10.1037//0278-6133.20.4.243. Retrieved from http://psycnet.apa.org/journals/hea/20/4/243/ [DOI] [PubMed] [Google Scholar]
- Shamay-Tsoory SG, Aharon-Peretz J, Perry D. Two systems for empathy: A double dissociation between emotional and cognitive empathy in inferior frontal gyrus versus ventromedial prefrontal lesions. Brain. 2009;132(Pt 3):617–627. doi: 10.1093/brain/awn279. http://dx.doi.org/10.1093/brain/awn279. [DOI] [PubMed] [Google Scholar]
- Siedlecki KL, Salthouse TA, Oishi S, Jeswani S. The relationship between social support and subjective well-being across age. Social Indicators Research. 2014;117(2):561–576. doi: 10.1007/s11205-013-0361-4. http://dx.doi.org/10.1007/s11205-013-0361-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simmons AN, Norman SB, Spadoni AD, Strigo IA. Neurosubstrates of remission following prolonged exposure therapy in veterans with posttraumatic stress disorder. Psychotherapy and Psychosomatics. 2013;82(6):382–389. doi: 10.1159/000348867. http://dx.doi.org/10.1159/000348867. [DOI] [PubMed] [Google Scholar]
- Singer T, Lamm C. The social neuroscience of empathy. Annals of the New York Academy of Sciences. 2009;1156:81–96. doi: 10.1111/j.1749-6632.2009.04418.x. http://dx.doi.org/10.1111/j.1749-6632.2009.04418.x. [DOI] [PubMed] [Google Scholar]
- Spreng RN, McKinnon MC, Mar RA, Levine B. The Toronto Empathy Questionnaire: Scale development and initial validation of a factor-analytic solution to multiple empathy measures. Journal of Personality Assessment. 2009;91(1):62–71. doi: 10.1080/00223890802484381. http://dx.doi.org/10.1080/00223890802484381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steffens DC, Fisher GG, Langa KM, Potter GG, Plassman BL. Prevalence of depression among older Americans: The Aging, Demographics and Memory Study. International Psychogeriatrics. 2009;21(5):879–888. doi: 10.1017/S1041610209990044. http://dx.doi.org/10.1017/S1041610209990044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trobst KK, Collins RL, Embree JM. The role of emotion in social support provision: Gender, empathy and expressions of distress. Journal of Social and Personal Relationships. 1994;11(1):45–62. Retrieved from http://spr.sagepub.com/content/11/1/45.abstract. [Google Scholar]
- van Meijgaard J, Fielding JE. Estimating benefits of past, current, and future reductions in smoking rates using a comprehensive model with competing causes of death. Preventing Chronic Disease. 2012;9:E122. doi: 10.5888/pcd9.110295. http://dx.doi.org/10.5888/pcd9.110295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson GS. Wide-Range Achievement Test 3: Administration Manual. Wilmington: Del Wide Range; 1993. [Google Scholar]
- Yesavage JA, Sheikh JI. 9/Geriatric Depression Scale (GDS) Clinical Gerontologist. 1986;5(1–2):165–173. http://dx.doi.org/10.1300/J018v05n01_09. [Google Scholar]
- Zaki J, Bolger N, Ochsner K. It takes two: The interpersonal nature of empathic accuracy. Psychological Science. 2008;19(4):399–404. doi: 10.1111/j.1467-9280.2008.02099.x. http://dx.doi.org/10.1111/j.1467-9280.2008.02099.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.