Abstract
Mandible fractures account for a significant portion of maxillofacial injuries and the evaluation, diagnosis, and management of these fractures remain challenging despite improved imaging technology and fixation techniques. Understanding appropriate surgical management can prevent complications such as malocclusion, pain, and revision procedures. Depending on the type and location of the fractures, various open and closed surgical reduction techniques can be utilized. In this article, the authors review the diagnostic evaluation, treatment options, and common complications of mandible fractures. Special considerations are described for pediatric and atrophic mandibles.
Keywords: mandibular fracture, occlusion, facial trauma, open reduction, maxillomandibular fixation
Mandible fractures are regularly encountered by plastic surgeons and account for a significant portion of maxillofacial injuries. The majority of adult mandible fractures in the United States are related to interpersonal violence, most frequently in men aged 18 to 24 years old.1 A review1 of 13,142 patients noted that men have a fourfold higher incidence of mandibular fractures with nearly 50% arising from assault. In contrast, women sustain mandible fractures more commonly from motor vehicle accidents (MVAs) and falls.1 2 3 It is reported that ∼25% of mandible fractures in women are secondary to falls,1 although domestic violence should be ruled out if the mechanism and fracture location are inconsistent with accidental trauma.
In recent years the injury pattern and epidemiology of facial fractures has changed with improved safety technology in passenger vehicles.4 Recent reports5 6 suggest that the combination of a seatbelt and airbags decreases the likelihood of sustaining a facial fracture during a MVA by over 50%.
Evaluation
Initial Assessment
Patients should be assessed in accordance with the Advanced Trauma Life Support protocol. Life-threatening injuries should be recognized and treated accordingly. Verifying the mechanism of injury can prove valuable as the type of trauma is often related to fracture patterns. Physical altercations tend to result in a higher incidence of angle fractures due to a lateral blow to the mandible, whereas MVAs are more commonly associated with parasymphyseal, symphyseal, body, and condylar fractures.1 7 8 Concomitant injuries must be ruled out during primary and secondary trauma surveys, especially after MVAs; a careful evaluation of the C-spine is required before proceeding with any operative management. Most studies report an incidence of C-spine injuries between 2 to 10%9 10 11 12 13 14 in patients presenting with facial fractures, although this may be as high as 20% in patients with panfacial injuries.15 Combined facial fracture patterns, involving two or more facial thirds, and unilateral mandible injuries account for the greatest number of C-spine injuries.16 17
Examination
A critical factor in the diagnostic workup of mandible fractures is the evaluation of the patient's occlusion. Asking patients if their “bite feels normal” is a very effective and highly sensitive test in the acute setting. A subjective report of malocclusion by the patient should be taken seriously, documented, and compared with the preinjury occlusion. If the patient is intubated, sedated, or unable to communicate this information, prior dental records can be helpful in addition to an examination of the wear facets. Most patient's preinjury occlusion is imperfect, and the surgeon should not attempt to place the patient into a “normal occlusion” if the wear facets indicate a different preinjury skeletal relationship.
On exam, the physician should bimanually palpate the fracture site to check for fragment mobility. A lack of mobility indicates a stable fracture that may be amenable to conservative management, provided the occlusion has not been altered. Intraoral lacerations, injuries of the soft tissues, and hematomas at the fracture site are also important to note as these may lead to an increased risk of infection. Ecchymosis of the floor of the mouth is classically pathognomonic for mandibular fractures.
The dental status of the patient should also be evaluated. Loose teeth are extremely common following facial trauma and should be noted during the initial assessment. Exceedingly carious or damaged teeth, particularly at the fracture site, should prompt consideration of extraction. Tooth extraction is recommended if the tooth is (1) luxated from its socket and/or interfering with fracture reduction, (2) fractured, (3) has advanced dental caries carrying a significant risk of abscess, (4) has advanced periodontal disease with mobility that would not contribute to establishing stable occlusion, or (5) has existing pathology such as cyst formation and pericoronitis.18 There are certain situations in which teeth in the fracture line can be left in place as they can provide a larger repositioning surface. They can also be used for the application of tension bands in certain cases19 and do not cause delayed healing when treated with a closed reduction.20
Sensation in the lower lip should also be tested and recorded. Damage to the inferior alveolar nerve (IAN) as it courses through the body of the mandible is not uncommon with mandible fractures, and failure to note this preoperatively may be mistaken as a postoperative complication. We have noted mandibular angle fractures to have significantly higher rates of hypoesthesia. Tay et al21 found that IAN injury was 4 times more likely in IAN-bearing posterior mandibular fractures (56.2%) than in non-IAN-bearing anterior mandibular fractures (12.6%).
Imaging
Radiographic assessment is integral in the workup of patients with significant facial trauma. Most patients with mandible fractures, particularly in the setting of polytrauma, present to an emergency room and undergo initial computed tomographic (CT) imaging to evaluate for cervical spine (C-spine) and other concomitant injuries. Although panoramic tomography used to be the gold standard, is cost-effective, and useful in the assessment of dental trauma,22 certain fracture patterns may be missed, particularly in the posterior mandible. Therefore, with helical CT imaging 100% sensitivity in diagnosing mandible fractures compared with 86% sensitivity of panoramic tomography imaging,22 together with the advent of three-dimensional reconstruction, CT is the current diagnostic tool of choice for the radiographic evaluation and diagnosis of mandible fractures.23
Management
The ultimate goal of treatment is to re-establish the patient's preinjury dental occlusion. Fractures that are nondisplaced and exhibit no occlusal changes may be amenable to nonsurgical management, but the majority of mandible fractures will require stabilization for satisfactory healing and to restore pretraumatic maxillomandibular orientation. Various treatment strategies have been described and vary widely depending on the fracture location and surgeon's preference. The patient's demographics, comorbidities, dentition, and fracture characterization will all influence the choice of fixation by the treating surgeon.
Fracture Fixation Principles
Fracture fixation can be divided into two basic categories: load-bearing and load-sharing. Load-bearing osteosynthesis denotes a construct that is capable of bearing 100% of the functional load generated by the mandible such that the bone at the fracture site bears none,18 24 effectively sheltering the bone from masticatory forces as it heals. This is frequently accomplished with locking reconstruction plates. Clinical uses of load-bearing fixation include defect fractures, comminuted fractures, and fractures in severely atrophic mandibles. By comparison, load-sharing osteosynthesis denotes a fixation arrangement whereby the functional load is distributed between the hardware and the bony ends at the fracture site.18 24 Understandably, this requires sufficient bony buttressing at the fracture site and cannot be used for fractures with poor bone-to-bone contact, comminuted, or defect fractures. Examples of load-sharing fixation include a single miniplate along the oblique ridge for angle fractures, a single miniplate and an arch bar for body or symphyseal fractures, and lag screw fixation.
Maxillomandibular fixation can be performed with the use of Erich arch bars, hybrid arch bars, intermaxillary fixation screws, circummandibular and piriform wiring, and orthodontic brackets with hooks.
Surgical Treatment by Fracture Site
Body
Nondisplaced and minimally displaced fractures of the mandibular body can often be managed closed with a period of maxillomandibular fixation (MMF), particularly when the fracture is isolated and reducible and the dentition is sufficient. However, this practice results in prolonged immobility and challenges with intraoral hygiene. As such, open reduction, internal fixation (ORIF) may be preferable for some patients, particularly the elderly, to avoid the discomfort and hindrance of dental wiring. Indeed, more displaced fractures of the mandibular body will generally require ORIF for optimal anatomical reduction. Exposure is obtained via a lateral gingivobuccal sulcus incision, although an extraoral submandibular (Risdon) approach can be utilized if necessary.25 Fixation is commonly achieved by using a single large plate along the inferior border or by two smaller plates, one on the inferior border and another placed just above, sparing the tooth roots, the latter functioning as a tension band. Ellis reviewed26 682 patients treated with ORIF of body and/or symphyseal fractures and found that the use of two miniplates was associated with more postoperative complications than the use of one stronger plate, such as noninfectious wound dehiscence and the need for hardware removal due to exposure.
Symphysis/Parasymphysis
Fractures of the anterior mandible are often secondary to a posteriorly directed force, frequently in the context of MVAs. Given the strength of bone in this region of the mandible, one should always look for concomitant mandibular fractures as well as C-spine injuries from neck hyperextension.
Open reduction, internal fixation is generally the treatment of choice for symphyseal and parasymphyseal fractures, although closed treatment is still an accepted alternative for select patients with simple nondisplaced fractures. Exposure of the fracture is obtained with a lower gingivobuccal sulcus incision and dissection to the inferior border of the mandible. Two miniplates are sufficient in most situations and result in similar outcomes, but with more postoperative complications, as mentioned above.26 27 One larger plate, with or without an arch bar, is the accepted alternative to the two miniplate approach. In the parasymphyseal region, the surgeon should employ careful dissection around the mental nerve to allow placement of the inferior plate below the mental foramen. Two lag screws that span the fracture line provide rigid fixation with relatively low treatment costs. However, these long screws are difficult to apply correctly and can result in shearing of the fracture fragments and subsequent malocclusion if good bone-to-bone contact is not present. As such, some feel that this procedure is very technique sensitive and thus requires more skill and expertise (Fig. 1).27
Fig. 1.
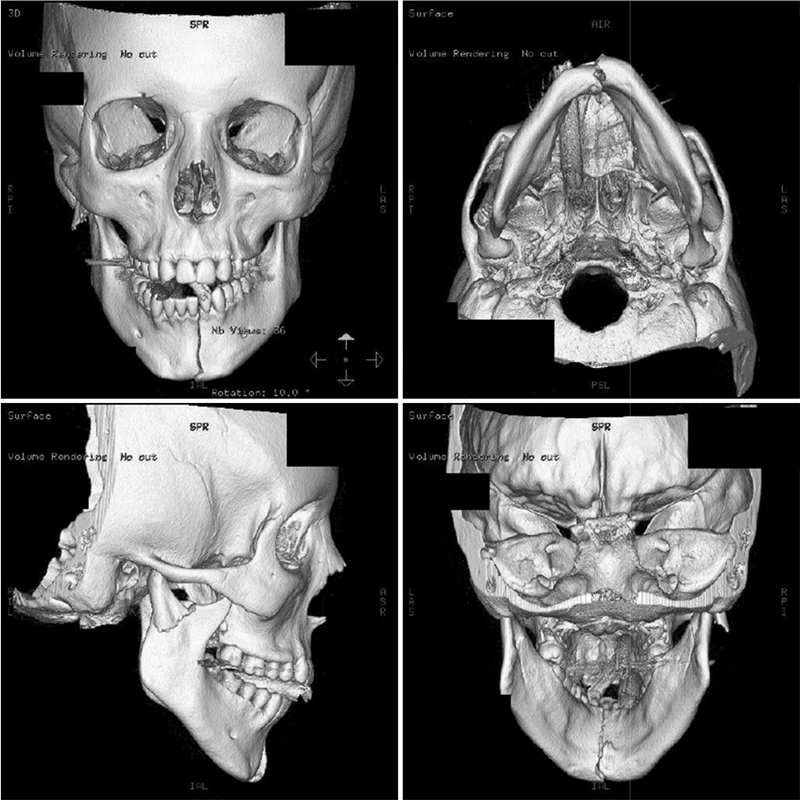
Displaced symphyseal and right subcondylar fractures.
Angle
The angle is the most frequently involved site in patients with isolated mandibular fractures, which typically result from personal assault.28 The thinner cross-sectional area of this region of the mandible29 and the presence of impacted third molars30 are thought to primarily contribute to the high incidence of angle fractures. Mandibular angle fractures are some of the most technically demanding and are associated with the highest complication rate of all mandibular fractures.31 32 33
Disagreement exists in the literature regarding the precise definition of a mandibular “angle” fracture,34 contributing to the various management approaches. The anatomical region contains several powerful muscles capable of generating significant forces in multiple directions that must be accounted for.35 Champy showed that by accounting for the forces of these muscles absolute rigid fixation is not necessary.36 Nondisplaced or minimally displaced fractures in patients with normal occlusion may be treated with observation and a soft diet or a short course of MMF with close follow-up. However, most angle fractures are treated with some form of ORIF due to the tendency of proximal segment displacement. Common strategies to stabilize these fractures have included a single plate along the oblique ridge, two lateral border plates, or a matrix-type miniplate on the lateral border (Fig. 2). An intraoral approach using a vestibular incision is used for the majority of simple angle fractures. In comminuted or more complex fractures, a transbuccal trocar can be employed to improve access.
Fig. 2.
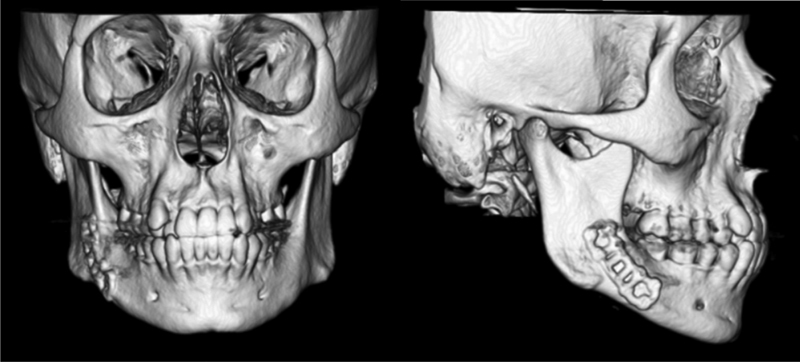
Postoperative angle fracture repaired with a ladder miniplate.
A landmark study in 2010 by Ellis looked at a series of 185 patients with angle fractures over a 12-year period treated in one of three ways: (1) 5 to 6 weeks of MMF, (2) ORIF using a single miniplate, and (3) ORIF using two miniplates. Only the third technique produced rigid fixation, but the single miniplate approach along the external oblique ridge was associated with the lowest number of complications, the shortest operating room time, and was the easiest to perform.32
The risk of postoperative complications was reduced when the single miniplate was placed on the lateral surface of the mandible (transbuccal) compared with placement on the external oblique ridge. The use of geometric miniplates was also found to decrease the risk of postoperative complications compared with the use of conventional miniplates.37 In the rare setting of bilateral mandibular angle fractures, the combination of transoral rigid and nonrigid fixation with 2.0-mm miniplates has been described.38
Condyle
Mandibular condyle fractures account for 25 to 35% of all mandibular fractures.3 39 40 41 These patients will typically present with preauricular pain, malocclusion, or a chin deviation with mandibular opening and closing. In patients with bilateral condylar fractures, premature contact of the posterior teeth leads to the classic anterior open-bite deformity. History of a traumatic force directed at the symphyseal region may also be present, and these fractures are frequently found in association with fractures of the symphysis/parasymphysis.
The management of mandibular condyle fractures is very controversial among maxillofacial surgeons.42 The lack of robust data and standardized definitions regarding fracture classification contribute to the ongoing debate about proper treatment. However, there is general agreement that patients with condylar fractures benefit from early active range-of-motion (ROM) to rehabilitate the temporomandibular articulation.
It is important to distinguish between fractures of the condyle itself (intracapsular) and fractures of the condylar neck (extracapsular). Fractures of the head of the condyle are generally treated closed because the fracture fragments are typically insufficient for fixation and the location within the temporomandibular joint (TMJ) places the patient at risk for ankylosis. Patients with no malocclusion can usually forgo MMF and be placed on a soft diet with close follow-up. If malocclusion is present, MMF is necessary, and occlusion is controlled with elastics.
Fractures of the condylar neck and subcondylar region can result in more serious occlusal disturbances. Management options include closed or open treatment, by either a direct approach or endoscopically. Previous studies have supported a more conservative approach because conservative treatment produced similar occlusal and functional outcomes to those treated with ORIF,43 44 and there is an alleged risk of devascularization of the fractured segment in addition to the visibility of external scars with the open approach.45 46 47 Facial nerve injury is also a purported risk of ORIF, but cases seem to be largely temporary with total recovery in less than 6 months.45
Advocates for ORIF report improved pain control, occlusion, and the restoration of posterior ramus height with the open approach.48 49 50 Additionally, long-term complications such as pain, arthritis, malocclusion, TMJ dysfunction, facial asymmetry, and ankylosis are reported in patients with condylar injuries treated in a closed fashion.51 52 53 A meta-analysis by Al-Moraissi and Ellis51 in 2015 found that ORIF provided superior functional clinical outcomes, such as MIO, protrusion, and a lack of chin deviation, compared with a closed treatment. The authors also found improvements in postoperative pain reduction and occlusion in those treated in an open manner.51 Although objective outcome measures do appear to vary with treatment selection, some authorities42 feel that the management of these fractures should ultimately depend on the skill and comfort level of the surgeon, and whether they feel they can achieve the goals of treatment better with open versus closed treatment.
Bilateral subcondylar fractures represent a unique challenge and have higher rates of complications,40 54 including malocclusion rates of up to 5%.55 Rehabilitating these patients using conservative treatment is more difficult due to the deficiency in structural support from the lack of craniomandibular articulations.51 Although there are reports of these fractures being managed conservatively with low malocclusion and pain rates,56 treating at least one of the fractures with ORIF to re-establish posterior facial height may be the best form of treatment.57 Other indications for ORIF are open fractures, the presence of a foreign body at the fracture site, and the displacement of a fractured fragment into the middle cranial fossa.
Special Considerations
Atrophic Mandible Fractures
The atrophic mandible is more vulnerable to fracture because of decreased bone volume as a result of the resorption of alveolar bone due to tooth loss.58 Fractures occur most commonly in the mandibular body where atrophy appears critical. Atrophic fractures most often occur in the geriatric population, but are infrequent injuries in clinical practice. These patients are also at particularly high risk for nonhealing secondary to the tenuous blood supply and poor bone stock of the atrophic mandible.59 Complication rates, including nonunion, have been reported between 4 to 20%.60 61 62 63 64 65 66
The lack of teeth in these patients and the associated small-cross sectional area of the jaw preclude some traditional methods of fracture immobilization, especially MMF.58 Because many of these patients are medically debilitated, considering no treatment for these fractures is acceptable.67 68 For patients undergoing intervention, closed and open treatments have been described. Bruce and Ellis61 published a series of 104 consecutive edentulous fractures and found higher rates of delayed or fibrous union in closed treatment versus ORIF (25% vs. 12.6%). There was also increased morbidity and disability time, worse jaw function, and poorer aesthetics in those who underwent closed treatment.61 In patients who are medically stable to undergo general anesthesia, ORIF with immediate bone grafting can yield good outcomes.58 Given the poor blood supply of the atrophic mandible, bone grafting allows for facilitating osseous union, providing stability to the fracture, and adding bulk to prevent pathologic fracture and enhance the possibilities for prosthetic reconstruction through augmenting the alveolus.58
Pediatric Fractures
Mandible fractures represent up to 40% of pediatric facial fractures, most frequently as a result of MVAs and falls. Sports-related injuries and assault are common causes in teenagers.69 70 71 72 Mandible fractures also differ between sexes, with a male to female ratio of 4:1.73
In comparison to adult fractures, pediatric fractures are approached differently due to the stage of mixed dentition, the elasticity of the craniofacial skeleton, and the potential for remodeling of the bone and fracture site with growth.74 75 The high elasticity of the cortical bone accounts for why most pediatric mandible fractures are unicortical and minimally displaced.76
A key aspect that distinguishes the pediatric mandible fracture is the dentition, requiring the surgeon to consider the developmental status of the child in the context of their injury. Until the mixed dentition phase is complete, the parasymphysis and body of the mandible are occupied by developing tooth buds. The location of unerupted permanent tooth follicles is an important consideration in terms of where plate-and-screw fixation can be placed during the operative repair of pediatric mandible fractures.77
The most common mandible fractures in children involve the condyle (40–70%),77 78 which is considered a primary growth center of the jaw. Direct trauma to the anterior mandible can result in proximal transmission of force, leading to injury of the mandibular condyle. Forces transmitted to this region often result in intra-articular fractures. Such fractures are associated with a risk for growth disturbance of the mandible, resulting in facial asymmetry due to ipsilateral chin deviation.79 80 81 The risk of growth disruption appears to be highest in cases of comminuted intra-articular fractures.82 The clinical presentation of these children can be very misleading, as they may present to the emergency room with simply a chin laceration and jaw pain.
Similar to the adult literature, the management of pediatric condylar fractures is a contentious topic. Three main treatment modalities have been described, including mandibular physical therapy consisting of ranging exercises without MMF, a short period of MMF followed by mandibular physical therapy, and ORIF. In general, these injuries rarely require operative management as children usually have good ROM and occlusion. Long-term favorable facial growth outcomes have been described with the closed treatment of condylar fractures.83 84
When an intra-articular condylar fracture is diagnosed, attention must be focused on early mobilization and ROM exercises. The condyle is a very vascular structure in children and can fragment under traumatic compression, leading to hemarthrosis and ankylosis. Temporomandibular joint ankylosis is very difficult to treat successfully, and in a child can result in profound deformities, as the injured side fails to grow appropriately (Fig. 3).
Fig. 3.
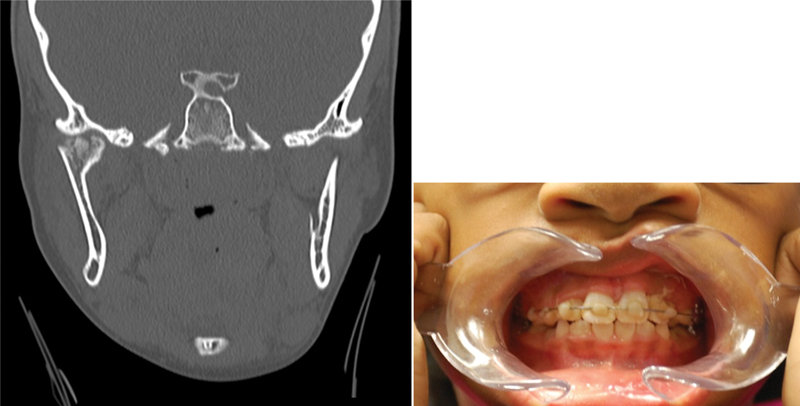
Child with condylar fracture successfully treated with short-course maxillomandibular fixation and contralateral elastics.
In condylar neck or subcondylar injuries, there is a greater chance for more significant occlusal changes. Very young children have exceptional fracture remodeling ability, and the developing dentition can frequently self-correct some degree of malocclusion. A short period of MMF (7–14 days) can be considered for older children or for those patients with more significant malocclusions. Standard Erich arch bars can be a challenge in the mixed dentition stage, but can still be used with no reported periodontal defects, tooth avulsions, or disturbances to permanent dentition.85
In fractures of the angle, body, or symphysis/parasymphysis, ORIF is frequently required. In general, 2.0-mm miniplates with monocortical screws or wires along the inferior border are the preferred methods of fixation.77 A preoperative panoramic radiograph is useful in evaluating the position of the developing tooth buds. The surgeon should exercise caution when plating the inferior-most aspect of the anterior mandibular border to avoid injury to unerupted tooth follicles and the low-lying AIN in the pediatric patient.77 Radiographs should also be taken postoperatively to ensure that none of the screws are transfixing a tooth bud. If this is seen, the plate should be removed once the fracture has sufficiently healed.
Complications
Mandible fracture complication rates range from 7 to 29% and have been correlated to fracture severity, injury site, and the number of involved sites.28 The most common complications include infection, hardware failure, osteomyelitis, nonunion, malunion, and wound dehiscence.86 87 88 Higher complication rates are seen among smokers, patients with systemic illnesses, and those patients with substance use or abuse. Antibiotic usage and delay in surgical repair do not seem to affect the incidence of these complications. Complications are less prevalent in children, which are mostly related to infection.89
In multiple studies, nonunion was most common in the mandibular body and was associated with inadequate stabilization or reduction and multiple fractures, and the presence of medical or social risk factors.90 91
Malocclusion remains the most functionally significant postoperative complication and is most often due to technical error in the placement of the fixation. This should be recognized at the end of the case when MMF is released, and the final occlusion is assessed. If noted postoperatively, most patients should be returned to the operating room as this complication cannot be reliably treated with nonsurgical modalities.
References
- 1.Afrooz P N, Bykowski M R, James I B, Daniali L N, Clavijo-Alvarez J A. The epidemiology of mandibular fractures in the United States, part 1: a review of 13,142 cases from the US National Trauma Data Bank. J Oral Maxillofac Surg. 2015;73(12):2361–2366. doi: 10.1016/j.joms.2015.04.032. [DOI] [PubMed] [Google Scholar]
- 2.Erdmann D, Follmar K E, Debruijn M. et al. A retrospective analysis of facial fracture etiologies. Ann Plast Surg. 2008;60(4):398–403. doi: 10.1097/SAP.0b013e318133a87b. [DOI] [PubMed] [Google Scholar]
- 3.Ellis E III, Moos K F, el-Attar A. Ten years of mandibular fractures: an analysis of 2,137 cases. Oral Surg Oral Med Oral Pathol. 1985;59(2):120–129. doi: 10.1016/0030-4220(85)90002-7. [DOI] [PubMed] [Google Scholar]
- 4.Murphy R X Jr, Birmingham K L, Okunski W J, Wasser T. The influence of airbag and restraining devices on the patterns of facial trauma in motor vehicle collisions. Plast Reconstr Surg. 2000;105(2):516–520. doi: 10.1097/00006534-200002000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Hitosugi M, Mizuno K, Nagai T, Tokudome S. Analysis of maxillofacial injuries of vehicle passengers involved in frontal collisions. J Oral Maxillofac Surg. 2011;69(4):1146–1151. doi: 10.1016/j.joms.2010.05.030. [DOI] [PubMed] [Google Scholar]
- 6.Hyman D A, Saha S, Nayar H S, Doyle J F, Agarwal S K, Chaiet S R. Patterns of facial fractures and protective device use in motor vehicle collisions from 2007 to 2012. JAMA Facial Plast Surg. 2016;18(6):455–461. doi: 10.1001/jamafacial.2016.0733. [DOI] [PubMed] [Google Scholar]
- 7.Lamphier J Ziccardi V Ruvo A Janel M Complications of mandibular fractures in an urban teaching center J Oral Maxillofac Surg 2003617745–749., discussion 749–750 [DOI] [PubMed] [Google Scholar]
- 8.Olson R A, Fonseca R J, Zeitler D L, Osbon D B. Fractures of the mandible: a review of 580 cases. J Oral Maxillofac Surg. 1982;40(1):23–28. doi: 10.1016/s0278-2391(82)80011-6. [DOI] [PubMed] [Google Scholar]
- 9.Beirne J C Butler P E Brady F A Cervical spine injuries in patients with facial fractures: a 1-year prospective study Int J Oral Maxillofac Surg 199524(1 Pt 1):26–29. [DOI] [PubMed] [Google Scholar]
- 10.Sinclair D, Schwartz M, Gruss J, McLellan B. A retrospective review of the relationship between facial fractures, head injuries, and cervical spine injuries. J Emerg Med. 1988;6(2):109–112. doi: 10.1016/0736-4679(88)90148-5. [DOI] [PubMed] [Google Scholar]
- 11.Haug R H, Wible R T, Likavec M J, Conforti P J. Cervical spine fractures and maxillofacial trauma. J Oral Maxillofac Surg. 1991;49(7):725–729. doi: 10.1016/s0278-2391(10)80236-8. [DOI] [PubMed] [Google Scholar]
- 12.Luce E A, Tubb T D, Moore A M. Review of 1,000 major facial fractures and associated injuries. Plast Reconstr Surg. 1979;63(1):26–30. doi: 10.1097/00006534-197901000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Baker A B, Mackenzie W. Facial and cervical injuries. Med J Aust. 1976;1(8):236–237. doi: 10.5694/j.1326-5377.1976.tb140555.x. [DOI] [PubMed] [Google Scholar]
- 14.Mulligan R P, Friedman J A, Mahabir R C. A nationwide review of the associations among cervical spine injuries, head injuries, and facial fractures. J Trauma. 2010;68(3):587–592. doi: 10.1097/TA.0b013e3181b16bc5. [DOI] [PubMed] [Google Scholar]
- 15.Stacey D H, Doyle J F, Gutowski K A. Safety device use affects the incidence patterns of facial trauma in motor vehicle collisions: an analysis of the National Trauma Database from 2000 to 2004. Plast Reconstr Surg. 2008;121(6):2057–2064. doi: 10.1097/PRS.0b013e31817071fb. [DOI] [PubMed] [Google Scholar]
- 16.Elahi M M, Brar M S, Ahmed N, Howley D B, Nishtar S, Mahoney J L. Cervical spine injury in association with craniomaxillofacial fractures. Plast Reconstr Surg. 2008;121(1):201–208. doi: 10.1097/01.prs.0000293763.82790.aa. [DOI] [PubMed] [Google Scholar]
- 17.Mithani S K, St-Hilaire H, Brooke B S, Smith I M, Bluebond-Langner R, Rodriguez E D. Predictable patterns of intracranial and cervical spine injury in craniomaxillofacial trauma: analysis of 4786 patients. Plast Reconstr Surg. 2009;123(4):1293–1301. doi: 10.1097/PRS.0b013e31819e26f2. [DOI] [PubMed] [Google Scholar]
- 18.AO Foundation. AO Surgery reference. Available at: https://www2.aofoundation.org/. Accessed December 20, 2016
- 19.Shetty V, Freymiller E. Teeth in the line of fracture: a review. J Oral Maxillofac Surg. 1989;47(12):1303–1306. doi: 10.1016/0278-2391(89)90729-5. [DOI] [PubMed] [Google Scholar]
- 20.Baykul T, Erdem E, Dolanmaz D, Alkan A. Impacted tooth in mandibular fracture line: treatment with closed reduction. J Oral Maxillofac Surg. 2004;62(3):289–291. doi: 10.1016/j.joms.2003.06.007. [DOI] [PubMed] [Google Scholar]
- 21.Tay A B, Lai J B, Lye K W. et al. Inferior alveolar nerve injury in trauma-induced mandible fractures. J Oral Maxillofac Surg. 2015;73(7):1328–1340. doi: 10.1016/j.joms.2015.02.003. [DOI] [PubMed] [Google Scholar]
- 22.Wilson I F, Lokeh A, Benjamin C I. et al. Prospective comparison of panoramic tomography (zonography) and helical computed tomography in the diagnosis and operative management of mandibular fractures. Plast Reconstr Surg. 2001;107(6):1369–1375. doi: 10.1097/00006534-200105000-00008. [DOI] [PubMed] [Google Scholar]
- 23.Roth F S, Kokoska M S, Awwad E E. et al. The identification of mandible fractures by helical computed tomography and Panorex tomography. J Craniofac Surg. 2005;16(3):394–399. doi: 10.1097/01.scs.0000171964.01616.a8. [DOI] [PubMed] [Google Scholar]
- 24.Ellis E III, Miles B A. Fractures of the mandible: a technical perspective. Plast Reconstr Surg. 2007;120(7) 02:76S–89S. doi: 10.1097/01.prs.0000260721.74357.e7. [DOI] [PubMed] [Google Scholar]
- 25.Nishioka G J, Van Sickels J E. Transoral plating of mandibular angle fractures: a technique. Oral Surg Oral Med Oral Pathol. 1988;66(5):531–535. doi: 10.1016/0030-4220(88)90370-2. [DOI] [PubMed] [Google Scholar]
- 26.Ellis E III. A study of 2 bone plating methods for fractures of the mandibular symphysis/body. J Oral Maxillofac Surg. 2011;69(7):1978–1987. doi: 10.1016/j.joms.2011.01.032. [DOI] [PubMed] [Google Scholar]
- 27.Agnihotri A, Prabhu S, Thomas S. A comparative analysis of the efficacy of cortical screws as lag screws and miniplates for internal fixation of mandibular symphyseal region fractures: a randomized prospective study. Int J Oral Maxillofac Surg. 2014;43(1):22–28. doi: 10.1016/j.ijom.2013.07.001. [DOI] [PubMed] [Google Scholar]
- 28.Gutta R, Tracy K, Johnson C, James L E, Krishnan D G, Marciani R D. Outcomes of mandible fracture treatment at an academic tertiary hospital: a 5-year analysis. J Oral Maxillofac Surg. 2014;72(3):550–558. doi: 10.1016/j.joms.2013.09.005. [DOI] [PubMed] [Google Scholar]
- 29.Schubert W Kobienia B J Pollock R A Cross-sectional area of the mandible J Oral Maxillofac Surg 1997557689–692., discussion 693 [DOI] [PubMed] [Google Scholar]
- 30.Dodson T B Third molars may double the risk of an angle fracture of the mandible Evid Based Dent 20045378. Doi: 10.1038/sj.ebd.6400263 [DOI] [PubMed] [Google Scholar]
- 31.James R B, Fredrickson C, Kent J N. Prospective study of mandibular fractures. J Oral Surg. 1981;39(4):275–281. [PubMed] [Google Scholar]
- 32.Ellis E III. A prospective study of 3 treatment methods for isolated fractures of the mandibular angle. J Oral Maxillofac Surg. 2010;68(11):2743–2754. doi: 10.1016/j.joms.2010.05.080. [DOI] [PubMed] [Google Scholar]
- 33.Chuong R, Donoff R B, Guralnick W C. A retrospective analysis of 327 mandibular fractures. J Oral Maxillofac Surg. 1983;41(5):305–309. doi: 10.1016/0278-2391(83)90297-5. [DOI] [PubMed] [Google Scholar]
- 34.Ellis E III. Management of fractures through the angle of the mandible. Oral Maxillofac Surg Clin North Am. 2009;21(2):163–174. doi: 10.1016/j.coms.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 35.Tate G S, Ellis E III, Throckmorton G. Bite forces in patients treated for mandibular angle fractures: implications for fixation recommendations. J Oral Maxillofac Surg. 1994;52(7):734–736. doi: 10.1016/0278-2391(94)90489-8. [DOI] [PubMed] [Google Scholar]
- 36.Champy M, Lodde J P. [Osteosynthesis of the external orbital cavity using screwed plates. Therapeutic indications and results] Rev Otoneuroophtalmol. 1976;48(4):243–248. [PubMed] [Google Scholar]
- 37.Al-Moraissi E A, Ellis E III. What method for management of unilateral mandibular angle fractures has the lowest rate of postoperative complications? A systematic review and meta-analysis. J Oral Maxillofac Surg. 2014;72(11):2197–2211. doi: 10.1016/j.joms.2014.05.023. [DOI] [PubMed] [Google Scholar]
- 38.Cillo J E Jr, Ellis E III. Management of bilateral mandibular angle fractures with combined rigid and nonrigid fixation. J Oral Maxillofac Surg. 2014;72(1):106–111. doi: 10.1016/j.joms.2013.07.008. [DOI] [PubMed] [Google Scholar]
- 39.Booth P W, Schendel S A, Hausamen J E II, editors. Vol. 1. Philadelphia, PA: Churchill Livingstone Elsevier; 2007. Maxillofacial surgery. [Google Scholar]
- 40.Zachariades N, Mezitis M, Mourouzis C, Papadakis D, Spanou A. Fractures of the mandibular condyle: a review of 466 cases. Literature review, reflections on treatment and proposals. J Craniomaxillofac Surg. 2006;34(7):421–432. doi: 10.1016/j.jcms.2006.07.854. [DOI] [PubMed] [Google Scholar]
- 41.Zide M F, Kent J N. Indications for open reduction of mandibular condyle fractures. J Oral Maxillofac Surg. 1983;41(2):89–98. doi: 10.1016/0278-2391(83)90214-8. [DOI] [PubMed] [Google Scholar]
- 42.Ellis E III. Discussion: which factors are associated with open reduction of adult mandibular condylar injuries? Plast Reconstr Surg. 2016;137(6):1822–1823. doi: 10.1097/PRS.0000000000002154. [DOI] [PubMed] [Google Scholar]
- 43.Marker P, Nielsen A, Bastian H L. Fractures of the mandibular condyle. Part 1: patterns of distribution of types and causes of fractures in 348 patients. Br J Oral Maxillofac Surg. 2000;38(5):417–421. doi: 10.1054/bjom.2000.0317. [DOI] [PubMed] [Google Scholar]
- 44.Santler G Kärcher H Ruda C Köle E Fractures of the condylar process: surgical versus nonsurgical treatment J Oral Maxillofac Surg 1999574392–397., discussion 397–398 [DOI] [PubMed] [Google Scholar]
- 45.Kyzas P A, Saeed A, Tabbenor O. The treatment of mandibular condyle fractures: a meta-analysis. J Craniomaxillofac Surg. 2012;40(8):e438–e452. doi: 10.1016/j.jcms.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 46.Haug R H Assael L A Outcomes of open versus closed treatment of mandibular subcondylar fractures J Oral Maxillofac Surg 2001594370–375., discussion 375–376 [DOI] [PubMed] [Google Scholar]
- 47.Walker R V. Condylar fractures: nonsurgical management. J Oral Maxillofac Surg. 1994;52(11):1185–1188. doi: 10.1016/0278-2391(94)90542-8. [DOI] [PubMed] [Google Scholar]
- 48.Ellis E III, Simon P, Throckmorton G S. Occlusal results after open or closed treatment of fractures of the mandibular condylar process. J Oral Maxillofac Surg. 2000;58(3):260–268. doi: 10.1016/s0278-2391(00)90047-8. [DOI] [PubMed] [Google Scholar]
- 49.Ellis E III Throckmorton G Facial symmetry after closed and open treatment of fractures of the mandibular condylar process J Oral Maxillofac Surg 2000587719–728., discussion 729–730 [DOI] [PubMed] [Google Scholar]
- 50.Schneider M, Erasmus F, Gerlach K L. et al. Open reduction and internal fixation versus closed treatment and mandibulomaxillary fixation of fractures of the mandibular condylar process: a randomized, prospective, multicenter study with special evaluation of fracture level. J Oral Maxillofac Surg. 2008;66(12):2537–2544. doi: 10.1016/j.joms.2008.06.107. [DOI] [PubMed] [Google Scholar]
- 51.Al-Moraissi E A, Ellis E III. Surgical treatment of adult mandibular condylar fractures provides better outcomes than closed treatment: a systematic review and meta-analysis. J Oral Maxillofac Surg. 2015;73(3):482–493. doi: 10.1016/j.joms.2014.09.027. [DOI] [PubMed] [Google Scholar]
- 52.Suzuki T, Kawamura H, Kasahara T, Nagasaka H. Resorbable poly-L-lactide plates and screws for the treatment of mandibular condylar process fractures: a clinical and radiologic follow-up study. J Oral Maxillofac Surg. 2004;62(8):919–924. doi: 10.1016/j.joms.2004.01.016. [DOI] [PubMed] [Google Scholar]
- 53.Singh V, Bhagol A, Goel M, Kumar I, Verma A. Outcomes of open versus closed treatment of mandibular subcondylar fractures: a prospective randomized study. J Oral Maxillofac Surg. 2010;68(6):1304–1309. doi: 10.1016/j.joms.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 54.Gupta M, Iyer N, Das D, Nagaraj J. Analysis of different treatment protocols for fractures of condylar process of mandible. J Oral Maxillofac Surg. 2012;70(1):83–91. doi: 10.1016/j.joms.2011.02.009. [DOI] [PubMed] [Google Scholar]
- 55.Marker P, Nielsen A, Bastian H L. Fractures of the mandibular condyle. Part 2: results of treatment of 348 patients. Br J Oral Maxillofac Surg. 2000;38(5):422–426. doi: 10.1054/bjom.2000.0457. [DOI] [PubMed] [Google Scholar]
- 56.Forouzanfar T, Lobbezoo F, Overgaauw M. et al. Long-term results and complications after treatment of bilateral fractures of the mandibular condyle. Br J Oral Maxillofac Surg. 2013;51(7):634–638. doi: 10.1016/j.bjoms.2012.12.005. [DOI] [PubMed] [Google Scholar]
- 57.Ellis E III, Kellman R M, Vural E. Subcondylar fractures. Facial Plast Surg Clin North Am. 2012;20(3):365–382. doi: 10.1016/j.fsc.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 58.Ellis E III, Price C. Treatment protocol for fractures of the atrophic mandible. J Oral Maxillofac Surg. 2008;66(3):421–435. doi: 10.1016/j.joms.2007.08.042. [DOI] [PubMed] [Google Scholar]
- 59.Bradley J C. Age changes in the vascular supply of the mandible. Br Dent J. 1972;132(4):142–144. doi: 10.1038/sj.bdj.4802812. [DOI] [PubMed] [Google Scholar]
- 60.Bruce R A, Strachan D S. Fractures of the edentulous mandible: the Chalmer J. Lyons Academy study. J Oral Surg. 1976;34(11):973–979. [PubMed] [Google Scholar]
- 61.Bruce R A, Ellis E III. The second Chalmers J. Lyons Academy study of fractures of the edentulous mandible. J Oral Maxillofac Surg. 1993;51(8):904–911. doi: 10.1016/s0278-2391(10)80113-2. [DOI] [PubMed] [Google Scholar]
- 62.Buchbinder D. Treatment of fractures of the edentulous mandible, 1943 to 1993: a review of the literature. J Oral Maxillofac Surg. 1993;51(11):1174–1180. doi: 10.1016/s0278-2391(10)80285-x. [DOI] [PubMed] [Google Scholar]
- 63.Luhr H G Reidick T Merten H A Results of treatment of fractures of the atrophic edentulous mandible by compression plating: a retrospective evaluation of 84 consecutive cases J Oral Maxillofac Surg 1996543250–254., discussion 254–255 [DOI] [PubMed] [Google Scholar]
- 64.Eyrich G K Grätz K W Sailer H F Surgical treatment of fractures of the edentulous mandible J Oral Maxillofac Surg 199755101081–1087., discussion 1087–1088 [DOI] [PubMed] [Google Scholar]
- 65.Iatrou I, Samaras C, Theologie-Lygidakis N. Miniplate osteosynthesis for fractures of the edentulous mandible: a clinical study 1989-96. J Craniomaxillofac Surg. 1998;26(6):400–404. doi: 10.1016/s1010-5182(98)80075-9. [DOI] [PubMed] [Google Scholar]
- 66.Kunz C Hammer B Prein J [Fractures of the edentulous atrophic mandible. Fracture management and complications]. [in German] Mund Kiefer Gesichtschir 200154227–232. [DOI] [PubMed] [Google Scholar]
- 67.Allard R H, Lekkas C. Unusual healing of a fracture of an atrophic mandible. Report of a case. Oral Surg Oral Med Oral Pathol. 1983;55(6):560–563. doi: 10.1016/0030-4220(83)90370-5. [DOI] [PubMed] [Google Scholar]
- 68.Zachariades N, Papavassiliou D, Triantafyllou D. et al. Fractures of the facial skeleton in the edentulous patient. J Maxillofac Surg. 1984;12(6):262–266. doi: 10.1016/s0301-0503(84)80256-8. [DOI] [PubMed] [Google Scholar]
- 69.Rowe N L. Fractures of the jaws in children. J Oral Surg. 1969;27(7):497–507. [PubMed] [Google Scholar]
- 70.Kaban L B, Mulliken J B, Murray J E. Facial fractures in children: an analysis of 122 fractures in 109 patients. Plast Reconstr Surg. 1977;59(1):15–20. doi: 10.1097/00006534-197701000-00002. [DOI] [PubMed] [Google Scholar]
- 71.Sherick D G Buchman S R Patel P P Pediatric facial fractures: a demographic analysis outside an urban environment Ann Plast Surg 1997386578–584., discussion 584–585 [PubMed] [Google Scholar]
- 72.Smith D M, Bykowski M R, Cray J J. et al. 215 mandible fractures in 120 children: demographics, treatment, outcomes, and early growth data. Plast Reconstr Surg. 2013;131(6):1348–1358. doi: 10.1097/PRS.0b013e31828bd503. [DOI] [PubMed] [Google Scholar]
- 73.Owusu J A, Bellile E, Moyer J S, Sidman J D. Patterns of pediatric mandible fractures in the United States. JAMA Facial Plast Surg. 2016;18(1):37–41. doi: 10.1001/jamafacial.2015.1456. [DOI] [PubMed] [Google Scholar]
- 74.Kaban L B. Diagnosis and treatment of fractures of the facial bones in children 1943-1993. J Oral Maxillofac Surg. 1993;51(7):722–729. doi: 10.1016/s0278-2391(10)80409-4. [DOI] [PubMed] [Google Scholar]
- 75.Siy R W, Brown R H, Koshy J C, Stal S, Hollier L H Jr. General management considerations in pediatric facial fractures. J Craniofac Surg. 2011;22(4):1190–1195. doi: 10.1097/SCS.0b013e31821c0cf9. [DOI] [PubMed] [Google Scholar]
- 76.James D R. In: Rowe N L, Williams J L, editors. New York: Churchill Livingstone; 1985. Maxillofacial injuries in children; Maxillofacial Injuries; pp. 538–558. [Google Scholar]
- 77.Wolfswinkel E M, Weathers W M, Wirthlin J O, Monson L A, Hollier L H Jr, Khechoyan D Y. Management of pediatric mandible fractures. Otolaryngol Clin North Am. 2013;46(5):791–806. doi: 10.1016/j.otc.2013.06.007. [DOI] [PubMed] [Google Scholar]
- 78.MacLennan W D. Consideration of 180 cases of typical fractures of the mandibular condylar process. Br J Plast Surg. 1952;5(2):122–128. doi: 10.1016/s0007-1226(49)80020-8. [DOI] [PubMed] [Google Scholar]
- 79.Ferreira P C, Amarante J M, Silva P N. et al. Retrospective study of 1251 maxillofacial fractures in children and adolescents. Plast Reconstr Surg. 2005;115(6):1500–1508. doi: 10.1097/01.prs.0000160268.20294.fd. [DOI] [PubMed] [Google Scholar]
- 80.Demianczuk A N, Verchere C, Phillips J H. The effect on facial growth of pediatric mandibular fractures. J Craniofac Surg. 1999;10(4):323–328. doi: 10.1097/00001665-199907000-00007. [DOI] [PubMed] [Google Scholar]
- 81.Schweinfurth J M, Koltai P J. Pediatric mandibular fractures. Facial Plast Surg. 1998;14(1):31–44. doi: 10.1055/s-0028-1085300. [DOI] [PubMed] [Google Scholar]
- 82.Lund K. Mandibular growth and remodelling processes after condylar fracture. A longitudinal roentgencephalometric study. Acta Odontol Scand Suppl. 1974;32(64):3–117. [PubMed] [Google Scholar]
- 83.Ghasemzadeh A, Mundinger G S, Swanson E W, Utria A F, Dorafshar A H. Treatment of pediatric condylar fractures: a 20-year experience. Plast Reconstr Surg. 2015;136(6):1279–1288. doi: 10.1097/PRS.0000000000001811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Rémi M, Christine M C, Gael P, Soizick P, Joseph-André J. Mandibular fractures in children: long term results. Int J Pediatr Otorhinolaryngol. 2003;67(1):25–30. doi: 10.1016/s0165-5876(02)00288-4. [DOI] [PubMed] [Google Scholar]
- 85.Naran S, Keating J, Natali M. et al. The safe and efficacious use of arch bars in patients during primary and mixed dentition: a challenge to conventional teaching. Plast Reconstr Surg. 2014;133(2):364–366. doi: 10.1097/01.prs.0000436842.07871.b6. [DOI] [PubMed] [Google Scholar]
- 86.Iizuka T Lindqvist C Rigid internal fixation of fractures in the angular region of the mandible: an analysis of factors contributing to different complications Plast Reconstr Surg 1993912265–271., discussion 272–273 [PubMed] [Google Scholar]
- 87.Anderson T Alpert B Experience with rigid fixation of mandibular fractures and immediate function J Oral Maxillofac Surg 1992506555–560., discussion 560–561 [DOI] [PubMed] [Google Scholar]
- 88.Iizuka T, Lindqvist C, Hallikainen D, Paukku P. Infection after rigid internal fixation of mandibular fractures: a clinical and radiologic study. J Oral Maxillofac Surg. 1991;49(6):585–593. doi: 10.1016/0278-2391(91)90340-r. [DOI] [PubMed] [Google Scholar]
- 89.Odom E B, Snyder-Warwick A K. Mandible fracture complications and infection: the influence of demographics and modifiable factors. Plast Reconstr Surg. 2016;138(2):282e–289e. doi: 10.1097/PRS.0000000000002385. [DOI] [PubMed] [Google Scholar]
- 90.Haug R H, Schwimmer A. Fibrous union of the mandible: a review of 27 patients. J Oral Maxillofac Surg. 1994;52(8):832–839. doi: 10.1016/0278-2391(94)90230-5. [DOI] [PubMed] [Google Scholar]
- 91.Mathog R H Toma V Clayman L Wolf S Nonunion of the mandible: an analysis of contributing factors J Oral Maxillofac Surg 2000587746–752., discussion 752–753 [DOI] [PubMed] [Google Scholar]


