Abstract
Craniofacial trauma is common in the pediatric population, with most cases limited to soft tissue and dentoalveolar injury. Although facial fractures are relatively rare in children compared with adults, they are often associated with severe injury and cause significant morbidity and disability. Initial evaluation of a child with facial trauma generally involves stabilizing the patient and identifying any severe concomitant injuries before diagnosing and managing facial injuries. The management of pediatric facial fractures is relatively more conservative than that of adults, and nonsurgical management is preferred when possible to prevent the disruption of future growth and development. Outcomes depend on the site of the injury, management plan, and subsequent growth, so children must be followed longitudinally for monitoring and the identification of any complications.
Keywords: pediatric facial trauma, facial fractures, reconstructive surgery
Epidemiology
Trauma is the leading cause of morbidity and mortality in children in the United States. According to the National Trauma Databank, the head is the body part most commonly involved in pediatric trauma cases, whereas the face is the fourth most commonly affected region. In 2016, case fatality rates for pediatric head and face trauma were reported as 3.74% and 3.07%, respectively.1 2 3 Although most cases of craniofacial trauma are due to unintentional injury, child abuse must also be considered, as 2.3% of child maltreatment cases involve facial fractures.4 5
Most cases of craniofacial trauma in children are limited to soft tissue and dentoalveolar injury, and facial fractures are relatively rare in children compared with adults.2 Although only 15% of facial fractures occur in children, pediatric facial fractures are associated with severe morbidity and disability, as well as significant hospital costs.6 7
Pediatric facial fractures most commonly occur outdoors during the summer months, and the most frequently associated injuries are neurologic in nature.4 Statistics on the most commonly fractured facial structures vary based on the population studied, and isolated nasal and dentoalveolar fractures are likely underreported.8 9 In teenagers, the mandible is the most commonly fractured structure, whereas children aged 0 to 11 years most commonly present with orbital fractures.7 10 The pediatric facial fracture pattern is unusual, with most cases demonstrating oblique fracture patterns rather than LeFort fractures, which are more common in adults. Greenstick fractures are also more common in children (Fig. 1).11
Fig. 1.
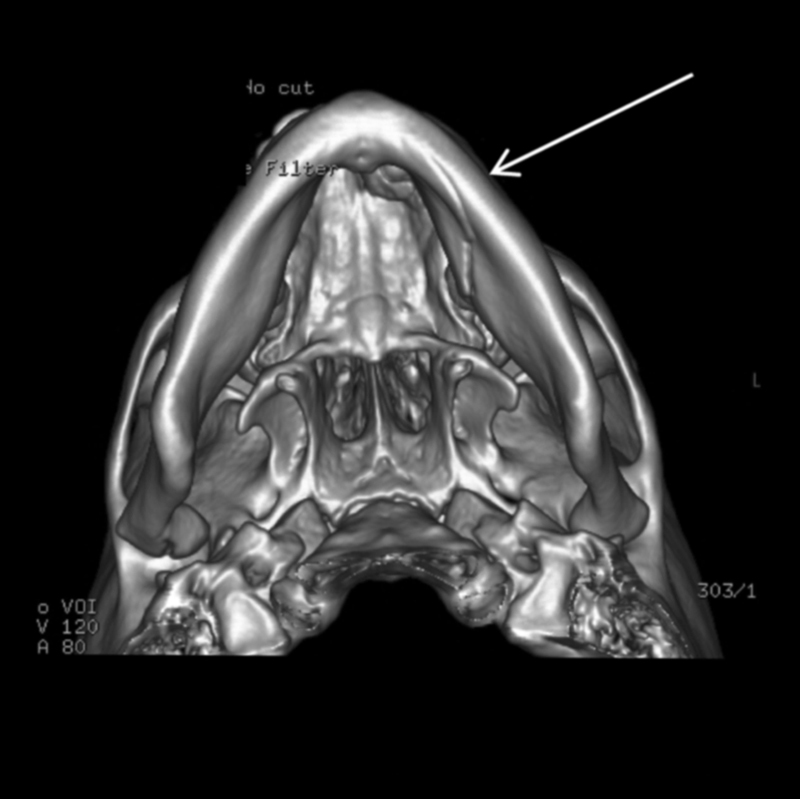
A greenstick mandibular fracture.
When children with facial fractures are divided into age cohorts based on developmental stages, different patterns of injury are revealed. For all children aged 0 to 18 years, facial fractures are more common in males than in females, and the frequency of pediatric fractures increases with age.6 Children aged 0 to 5 years have the lowest incidence of facial fractures, likely due to more time spent in supervised environments. Fractures in this age group occur mostly from activities of daily living. Children aged 6 to 11 years have the second highest incidence of facial fractures, and their injuries are most often caused by motor-vehicle accidents, play, and bike riding. Pediatric facial fractures most commonly occur at 12 to 18 years of age, when adolescents gain more independence, start to drive, and engage in contact sports. Fractures in this age group are most commonly caused by violence, followed by sports-related injuries.10
Anatomy of Pediatric Facial Trauma
Many of the age-related trends in pediatric facial trauma are explained by the growth and development of the skull. Babies are generally more susceptible to craniofacial injury due to their large cranial mass relative to their body.12 In early childhood, the midface is shielded by a prominent forehead and mandible. Fractures to the middle-third of the face are thus rare in early childhood, whereas fronto-orbital fractures are relatively more common.13 14 The ratio of skull-to-face increases from 8:1 at birth to 2.5:1 in adulthood. Thus, facial fractures become more common as the child grows and the face becomes more prominent.10 15
Children also have fewer displaced facial fractures due to added cushioning from fat pads, more compliant sutures, and increased skeletal flexibility. The facial skeleton is also more stable given decreased pneumatization of the sinuses and a stronger maxilla and mandible from nonerupted permanent dentition.12
A knowledge of sinus development is helpful when diagnosing and managing facial injuries. The ethmoid sinuses are partially pneumatized at birth and have almost reached adult size by age 12 years.16 The maxillary sinuses achieve most growth by 9 years, and continue pneumatization into early adulthood. Meanwhile, the sphenoid sinuses start to pneumatize at age 2 years and reach adult size by age 14 years. The frontal sinuses are the last to form, with pneumatization beginning at or after 2 years and growth continuing until after puberty.17
Additional factors to consider when treating facial fractures in children are their potential for future growth and development, a faster rate of healing, and differences in remodeling. Potential growth disturbances must be considered with nasal septum and mandibular condyle injuries.4 In addition, because there are several protective factors that prevent facial fractures from occurring in children, one must consider that a child presenting with facial fractures likely sustained a severe injury. The initial assessment, therefore, must consider severe or high-velocity trauma as the cause of injury and a higher likelihood of associated injuries or combined fractures.11
Initial Evaluation
Stabilization
Any pediatric patient presenting with facial trauma should first be stabilized. Patients are assessed in accordance with the Advanced Trauma Life Support protocol. Life-threatening injuries should be recognized and treated as soon as possible. There are several differences that must be considered in pediatric trauma assessment and management, including a potentially more precarious airway due to the airway's smaller caliber, relatively larger and more flaccid oral and pharyngeal soft tissues, a more cephalad larynx, and a narrower epiglottis. These differences make intubation and ventilation more difficult in children.5
Children presenting with trauma have additional risks due to their higher surface-to-volume ratio, metabolic rate, oxygen demand, and cardiac output. Their low blood volume also makes them especially vulnerable to hemodynamic instability. Together, these factors make pediatric patients more susceptible to hypotension, hypoxia, and hypothermia after a traumatic injury.8 18 19
Examination
Because pediatric facial fractures often occur after severe trauma, a physical examination should assess globally for associated injuries such as intracranial/cervical spine injuries, skull fractures, soft tissue lacerations or abrasions, and injuries to the trunk and extremities. Mandible and midface fractures have the highest rate of associated injuries, with neurocranial injuries seen most frequently.19 Although children are less likely than adults to experience concomitant cervical spine injuries in the setting of craniofacial injury, an examination is nevertheless necessary.20 It should also be noted that the practitioner should look out for signs of child abuse during the physical exam. These signs include repeat injuries, multiple injury sites, a delay between injury and seeking care, inappropriate parental responses, and questionable circumstances of injury.4 5
Due to the prominence of the forehead in children, orbital fractures are common, and a thorough orbital exam is important to assess for ocular injury.15 Most orbital fractures in children warrant an evaluation by ophthalmology. The exam should assess visual acuity, pupil size and response, integrity of the globe, and extraocular muscle movement.4 5 Signs of periorbital fractures include subconjunctival hemorrhage, chemosis, and bony step-offs upon palpation of the orbital margins. However, these step deformities can be difficult to feel in children.8 Enophthalmos or inferior displacement of the globe may occur due to orbital floor disruption, although this is unlikely unless the defect is greater than half the size of the orbital floor (> 1 cm2).18
Trapdoor fractures, also known as white-eye blowout fractures, occur almost exclusively in children. They may be difficult to diagnose because they can present with a “white eye” and a lack of typical symptoms. Trapdoor fractures may or may not lead to tissue entrapment, which manifests as restriction of extraocular muscle movement causing diplopia. Entrapment may also present as nausea, vomiting, and bradycardia in pediatric patients.19 21
Midface exam should assess for nasal or naso-orbito-ethmoid (NOE) fractures. Pediatric nasal fractures are suspected to be the most common facial fracture, though their occurrence is likely underreported in the literature.9 To look for nasal fractures, which can be obscured by swelling, the physician should assess the symmetry of the nose and the support of the nasal dorsum. Also, an intranasal exam is needed to check for a septal fracture or septal hematoma. Septal hematomas should be drained immediately to prevent complications.8 Although NOE fractures are rare in children, only accounting for 1 to 8% of all pediatric craniofacial fractures, they can potentially lead to cosmetic or functional sequelae if not identified and managed.7 Naso-orbito-ethmoid fractures present with telecanthus, shortened width of palpebral fissures, and a saddle nose deformity.22
Oral exam should assess for dental trauma as well as signs of fractures of the maxilla or mandible. When assessing the maxilla for fractures, evaluate for trismus, malocclusion, cheek flattening, and lateral canthal dystopia. In mandible fractures, also check for trismus and malocclusion, as well as decreased maximal incisive opening and visible dental step-off.8
Imaging
Maxillofacial computed tomography (CT) scans are commonly used to assess for facial fractures, with routine CT follow-up to assess growth disturbance. However, to reduce the child's exposure to radiation, some authors suggest the restricted use of CT for follow-up, only to be done when the physical exam is abnormal.8
Although ultrasound decreases exposure to radiation, this modality has not been definitively shown to be effective in the diagnosis of facial fractures in the pediatric population.5 Plain films are also unreliable due to children's propensity for greenstick fractures, underdeveloped sinuses, and a lack of ossification in some areas.8
Pediatric Facial Fractures
Overview
Many fractures that require surgical management in adults may be managed conservatively in children. When open reduction and internal fixation (ORIF) is required to treat a pediatric facial fracture, the surgeon must consider growth that will occur afterwards and try to preserve growth centers whenever possible.23 Because healing in children occurs faster than in adults, repair must also be performed sooner. Ideally, especially in younger children, mandibular fractures should be treated within 48 hours of injury, and surgical reduction and fixation should occur within 7 days. Periorbital fractures without extraocular muscle entrapment can wait for edema resolution before surgical management.18
The use of resorbable plates in facial fracture management is still under debate and has not been shown to be superior to conventional titanium plates.24 Although resorbable plates have the inherent advantage of resorbing over time, thereby eliminating the need for plate removal,25 disadvantages include potentially lower stability in high-stress load-bearing areas, and more difficult application with a steeper learning curve. Titanium plates, on the other hand, may require removal at a later stage, although associated growth interference and plate migration remain controversial.18 26
Frontal Bone Fractures
The goals of management of frontal bone fractures are to restore the contour of the forehead and to manage any cerebrospinal leak. Nondisplaced frontal bone fractures do not require surgical intervention. If the fracture is displaced more than the width of the bone, or if there is suspicion of nasofrontal duct injury, surgical intervention and reduction is performed.4 8 After 5 years of age when the frontal sinus begins pneumatizing, frontal bone fractures can potentially involve the sinus. The management of frontal sinus fractures depends on the classification of the fracture and is similar to that of adults.
Orbit Fractures
The treatment of orbital fractures is generally more conservative in pediatric patients than in their adult counterparts. Although orbit fractures can be difficult to diagnose in children without CT scans, the indications for surgical management are mostly based on clinical findings rather than CT findings (Fig. 2). Indications for surgery include extraocular muscle (EOM) entrapment, traumatic optic neuropathy, and large floor defects (> 1 cm2).4 In the case of traumatic optic neuropathy, aggressive steroid treatment is often given before surgical treatment. Cases with EOM entrapment should be treated within 48 hours in children to prevent muscle fibrosis and resultant diplopia.19 Transconjunctival incisions with or without a lateral canthotomy provide the best exposure of the orbital floor. When an implant is needed during reconstruction of the orbital floor, options include bone grafts, titanium mesh, high-density porous polyethylene implants, and other resorbable sheets.4 9
Fig. 2.
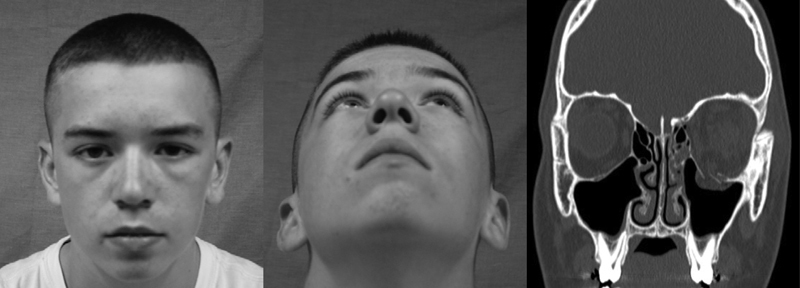
A patient with a large orbital floor defect and no clinical signs of enophthalmos or entrapment, therefore, managed conservatively.
Midface and Zygomaticomaxillary Complex
Treatment of pediatric zygomaticomaxillary complex (ZMC) fractures is similar to that of adults. Goals of treatment include restoring facial height, contour, dental occlusion, and any visual deficits.8 Minimally displaced or greenstick fractures without resultant functional deficits are managed conservatively; significantly displaced or comminuted fractures require ORIF.27 When maxillomandibular fixation is needed, creativity can be employed in the use of arch bars, orthodontic brackets (Fig. 3), circummandibular and circumpiriform wiring, and home-made IMF hooks.
Fig. 3.
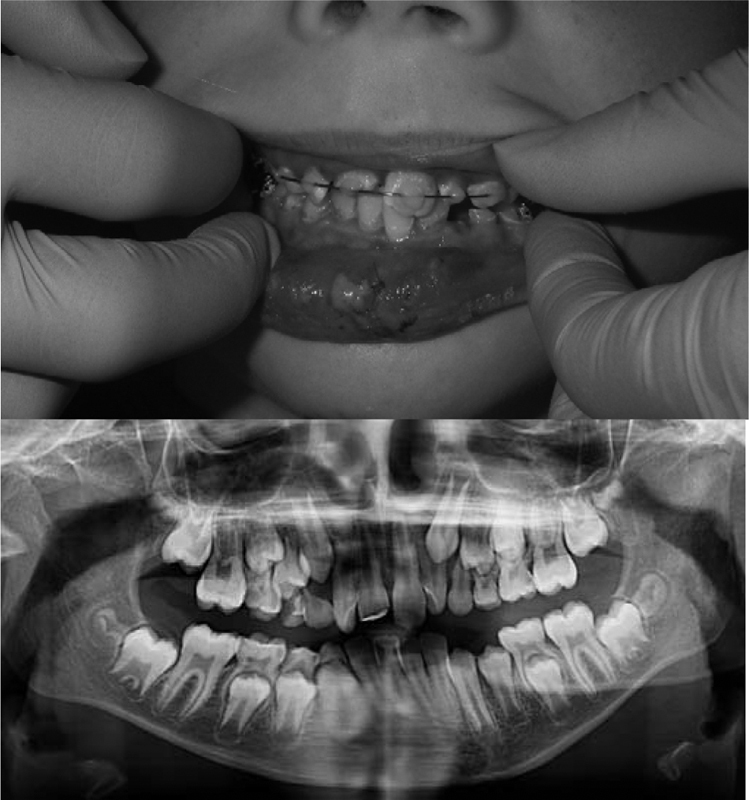
The use of orthodontic brackets for maxillomandibular fixation on a patient in mixed dentition, performed without the need for general anesthesia and no risk of injuring tooth roots/buds.
Zygomatic fractures that affect only the arch can be observed while the patient adheres to a soft diet. Minimally displaced zygomatic fractures are accessed via an intraoral approach, whereas comminuted zygomatic fractures require ORIF. Maxillary fractures are treated with maxillomandibular fixation and elastic traction if teeth have erupted adequately; if not, ORIF is needed. During fixation, screws should be placed far away from the dentition to avoid disrupting developing tooth follicles.8
Nasal Fractures and NOE Fractures
The management of fractures of the nose and the NOE are also similar to that of adults, with goals of therapy being the restoration of normal appearance and the correction of telecanthus when present.8 As mentioned previously, nasal septal hematomas should be drained immediately. There is no indication for imaging for a suspected isolated nasal fracture because treatment is indicated only if a deformity is present. Displaced nasal fractures can be reduced upon presentation or within a few days after edema has resolved. Closed reduction with external fixation is preferred in children to prevent distortion with growth.28 Most cases need anatomical realignment, hemostasis, and fixation under general anesthesia. However, some cases can be reduced under sedation.18 Naso-orbito-ethmoid fractures are usually repaired via ORIF, with transnasal wiring used for stabilization when bony fragments are too small for screw fixation.29
Mandible Fractures
The goal of therapy after a mandibular fracture is to restore occlusion. Minor malocclusion is often tolerated well in children due to their potential for future growth and remodeling. When there is no displacement or malocclusion, pediatric mandibular fractures can be observed. Analgesics, soft diet, and rest should be prescribed. Unstable displaced or comminuted fractures are treated with rigid fixation, which must take into account mandibular tooth buds. Fixation should not last more than 7 to 10 days, as this can lead to severe ankylosis of temporomandibular joints in children.30 Open reduction and internal fixation may be necessary for injuries that cannot be reduced via closed reduction, or for those associated with condylar fractures. A single miniplate, or wire with monocortical screws placed at the inferior border of the mandible, is usually sufficient to maintain stabilization in children.8
For the management of displaced subcondylar fractures, conservative therapy is often used with arch bars and contralateral elastics, given this region's ability to remodel without surgical reduction. Early range-of-motion and rehabilitation is also suggested to improve outcomes. Patients younger than 8 or 9 years with malocclusion may require 2 to 3 weeks of intermaxillary fixation.4 18
Outcomes and Complications
The outcomes of pediatric facial trauma depend on the location and severity of the fracture and the treatment type. The outcomes also evolve as the child grows and develops, so children should be followed longitudinally. Complications after facial fracture repair are less common in children than adults. These include infection, malunion, and nonunion, and associated malocclusion and growth restrictions. A classification scheme of all adverse outcomes after facial trauma repair was developed by Rottgers et al. In this system, type 1 outcomes are those that are related to the fracture itself, such as immediate blindness in orbital fracture. Type 2 outcomes are adverse outcomes that are related to treatment, such as a failure of hardware. Type 3 outcomes are related to altered future development, such as late mandibular hypoplasia. When possible, nonoperative management is preferred to reduce type 2 and type 3 adverse outcomes.23
Severe pediatric midface trauma is more likely to result in compromised bone growth and permanent facial differences if the child is younger at the time of injury, has more severe injuries, and requires more extensive surgery.31 Central facial fractures can result in maxillary hypoplasia, periorbital complications, and telecanthus. Intracapsular condylar fractures are more likely to result in complications in cases of bilateral fractures, young age (2–5 years), delayed treatment, and prolonged mandibulomaxillary fixation. These complications include mandibular asymmetry, hemarthrosis, and ankylosis. Malocclusion is rare after mandibular and maxillary fractures, as eruption of primary teeth and dental compensation usually are adequate to restore normal occlusion.18 23
A rare complication of orbital roof fractures in children is a growing skull fracture, which occurs when there is an underlying dural tear that allows brain growth and normal brain pulsations to transmit pressure into the orbit. A growing skull fracture can present with exophthalmos and is diagnosed during follow-up visits via clinical exam and CT scan.11
Because outcomes depend on the growth and development of the child, we suggest routine follow-up with CT scans to assess any disturbances in growth. Future investigation is needed on the long-term outcomes of pediatric facial trauma, and we encourage all hospitals to start facial trauma databases to collect follow-up and epidemiological data on these patients.
References
- 1.Department of Health and Human Services, Centers for Disease Control and Prevention. CDC Childhood Injury Report: Patterns of Unintentional Injuries among 0–19 year olds in the United States, 2000–2016. 2008. Available at: https://www.cdc.gov/safechild/pdf/cdc-childhoodinjury.pdf. Accessed February 8, 2017
- 2.Gassner R, Tuli T, Hächl O, Moreira R, Ulmer H. Craniomaxillofacial trauma in children: a review of 3,385 cases with 6,060 injuries in 10 years. J Oral Maxillofac Surg. 2004;62(4):399–407. doi: 10.1016/j.joms.2003.05.013. [DOI] [PubMed] [Google Scholar]
- 3.American College of Surgeons. The National Trauma Databank 2016. Pediatric Annual Report. Available at: https://www.facs.org/∼/media/files/quality%20programs/trauma/ntdb/ntdb%20pediatric%20annual%20report%202016.ashx. Accessed February 8, 2017
- 4.Hatef D A, Cole P D, Hollier L H Jr. Contemporary management of pediatric facial trauma. Curr Opin Otolaryngol Head Neck Surg. 2009;17(4):308–314. doi: 10.1097/MOO.0b013e32832d95a0. [DOI] [PubMed] [Google Scholar]
- 5.Ryan M L, Thorson C M, Otero C A. et al. Pediatric facial trauma: a review of guidelines for assessment, evaluation, and management in the emergency department. J Craniofac Surg. 2011;22(4):1183–1189. doi: 10.1097/SCS.0b013e31821c0d52. [DOI] [PubMed] [Google Scholar]
- 6.Vyas R M Dickinson B P Wasson K L Roostaeian J Bradley J P Pediatric facial fractures: current national incidence, distribution, and health care resource use J Craniofac Surg 2008192339–349., discussion 350 [DOI] [PubMed] [Google Scholar]
- 7.Imahara S D, Hopper R A, Wang J, Rivara F P, Klein M B. Patterns and outcomes of pediatric facial fractures in the United States: a survey of the National Trauma Data Bank. J Am Coll Surg. 2008;207(5):710–716. doi: 10.1016/j.jamcollsurg.2008.06.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Holland AJ A, Broome C, Steinberg A, Cass D T. Facial fractures in children. Pediatr Emerg Care. 2001;17(3):157–160. doi: 10.1097/00006565-200106000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Wright R J, Murakami C S, Ambro B T. Pediatric nasal injuries and management. Facial Plast Surg. 2011;27(5):483–490. doi: 10.1055/s-0031-1288931. [DOI] [PubMed] [Google Scholar]
- 10.Grunwaldt L, Smith D M, Zuckerbraun N S. et al. Pediatric facial fractures: demographics, injury patterns, and associated injuries in 772 consecutive patients. Plast Reconstr Surg. 2011;128(6):1263–1271. doi: 10.1097/PRS.0b013e318230c8cf. [DOI] [PubMed] [Google Scholar]
- 11.Naran S, MacIsaac Z, Katzel E. et al. Pediatric craniofacial fractures: trajectories and ramifications. J Craniofac Surg. 2016;27(6):1535–1538. doi: 10.1097/SCS.0000000000002837. [DOI] [PubMed] [Google Scholar]
- 12.Totonchi A, Sweeney W M, Gosain A K. Distinguishing anatomic features of pediatric facial trauma. J Craniofac Surg. 2012;23(3):793–798. doi: 10.1097/SCS.0b013e31821c0cc7. [DOI] [PubMed] [Google Scholar]
- 13.Iizuka T, Thorén H, Annino D J Jr, Hallikainen D, Lindqvist C. Midfacial fractures in pediatric patients. Frequency, characteristics, and causes. Arch Otolaryngol Head Neck Surg. 1995;121(12):1366–1371. doi: 10.1001/archotol.1995.01890120026005. [DOI] [PubMed] [Google Scholar]
- 14.McGraw B L, Cole R R. Pediatric maxillofacial trauma. Age-related variations in injury. Arch Otolaryngol Head Neck Surg. 1990;116(1):41–45. doi: 10.1001/archotol.1990.01870010045014. [DOI] [PubMed] [Google Scholar]
- 15.Ferreira P C, Amarante J M, Silva P N. et al. Retrospective study of 1251 maxillofacial fractures in children and adolescents. Plast Reconstr Surg. 2005;115(6):1500–1508. doi: 10.1097/01.prs.0000160268.20294.fd. [DOI] [PubMed] [Google Scholar]
- 16.Shah R K, Dhingra J K, Carter B L, Rebeiz E E. Paranasal sinus development: a radiographic study. Laryngoscope. 2003;113(2):205–209. doi: 10.1097/00005537-200302000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Scuderi A J, Harnsberger H R, Boyer R S. Pneumatization of the paranasal sinuses: normal features of importance to the accurate interpretation of CT scans and MR images. AJR Am J Roentgenol. 1993;160(5):1101–1104. doi: 10.2214/ajr.160.5.8470585. [DOI] [PubMed] [Google Scholar]
- 18.Siy R W, Brown R H, Koshy J C, Stal S, Hollier L H Jr. General management considerations in pediatric facial fractures. J Craniofac Surg. 2011;22(4):1190–1195. doi: 10.1097/SCS.0b013e31821c0cf9. [DOI] [PubMed] [Google Scholar]
- 19.Criden M R, Ellis F J. Linear nondisplaced orbital fractures with muscle entrapment. J AAPOS. 2007;11(2):142–147. doi: 10.1016/j.jaapos.2006.08.022. [DOI] [PubMed] [Google Scholar]
- 20.Thorén H, Schaller B, Suominen A L, Lindqvist C. Occurrence and severity of concomitant injuries in other areas than the face in children with mandibular and midfacial fractures. J Oral Maxillofac Surg. 2012;70(1):92–96. doi: 10.1016/j.joms.2011.06.227. [DOI] [PubMed] [Google Scholar]
- 21.Cohen S M, Garrett C G. Pediatric orbital floor fractures: nausea/vomiting as signs of entrapment. Otolaryngol Head Neck Surg. 2003;129(1):43–47. doi: 10.1016/S0194-59980300487-X. [DOI] [PubMed] [Google Scholar]
- 22.Liau J Y, Woodlief J, van Aalst J A. Pediatric nasoorbitoethmoid fractures. J Craniofac Surg. 2011;22(5):1834–1838. doi: 10.1097/SCS.0b013e31822ea9ef. [DOI] [PubMed] [Google Scholar]
- 23.Rottgers S A, Decesare G, Chao M. et al. Outcomes in pediatric facial fractures: early follow-up in 177 children and classification scheme. J Craniofac Surg. 2011;22(4):1260–1265. doi: 10.1097/SCS.0b013e31821c6ab7. [DOI] [PubMed] [Google Scholar]
- 24.Dorri M, Nasser M, Oliver R. Resorbable versus titanium plates for facial fractures. Cochrane Database Syst Rev. 2009;1(1):CD007158. doi: 10.1002/14651858.CD007158.pub2. [DOI] [PubMed] [Google Scholar]
- 25.Eppley B L. Use of resorbable plates and screws in pediatric facial fractures. J Oral Maxillofac Surg. 2005;63(3):385–391. doi: 10.1016/j.joms.2004.11.011. [DOI] [PubMed] [Google Scholar]
- 26.Imola M J, Hamlar D D, Shao W, Chowdhury K, Tatum S. Resorbable plate fixation in pediatric craniofacial surgery: long-term outcome. Arch Facial Plast Surg. 2001;3(2):79–90. doi: 10.1001/archfaci.3.2.79. [DOI] [PubMed] [Google Scholar]
- 27.Wheeler J, Phillips J. Pediatric facial fractures and potential long-term growth disturbances. Craniomaxillofac Trauma Reconstr. 2011;4(1):43–52. doi: 10.1055/s-0031-1272901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rohrich R J, Adams W P Jr. Nasal fracture management: minimizing secondary nasal deformities. Plast Reconstr Surg. 2000;106(2):266–273. doi: 10.1097/00006534-200008000-00003. [DOI] [PubMed] [Google Scholar]
- 29.Nguyen M, Koshy J C, Hollier L H Jr. Pearls of nasoorbitoethmoid trauma management. Semin Plast Surg. 2010;24(4):383–388. doi: 10.1055/s-0030-1269767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Goth S, Sawatari Y, Peleg M. Management of pediatric mandible fractures. J Craniofac Surg. 2012;23(1):47–56. doi: 10.1097/SCS.0b013e318240c8ab. [DOI] [PubMed] [Google Scholar]
- 31.Davidson E H, Schuster L, Rottgers S A. et al. Severe pediatric midface trauma: a prospective study of growth and development. J Craniofac Surg. 2015;26(5):1523–1528. doi: 10.1097/SCS.0000000000001818. [DOI] [PubMed] [Google Scholar]


