Abstract
Objective
To describe the prevalence and predictors of breastfeeding intent and outcomes in women with histories of childhood maltreatment trauma (CMT), including those with post-traumatic stress disorder (PTSD).
Design
Secondary analysis of a prospective observational cohort study of the effects of PTSD on perinatal outcomes.
Setting
Prenatal clinics in three health systems in the Midwestern United States.
Participants
Women older than 18 expecting their first infants, comprising three groups: women who experienced CMT but did not have PTSD (CMT-resilient), women with a history of CMT and PTSD (CMT-PTSD), and women with no history of CMT (CMT-nonexposed).
Results
Intent to breastfeed was similar among the three groups. Women in the CMT-resilient group were twice as likely to breastfeed exclusively at six weeks (60.5%) as women in the CMT-PTSD group (31.1%). Compared to women in the CMT-nonexposed group, women in the CMT-resilient were more likely to exclusively breastfeed. Four factors were associated with increased likelihood of any breastfeeding at six weeks: prenatal intent to breastfeed, childbirth education, partnered, and a history of CMT. Four factors were associated with decreased odds of breastfeeding: African American race, PTSD, major depression, and low level of education (high school or less).
Conclusion
Post-traumatic stress disorder is more important than childhood maltreatment trauma history in determining likelihood of breastfeeding success. Further research on the promotion of breastfeeding among PTSD-affected women who have experienced CMT is indicated.
Keywords: Breastfeeding, post-traumatic stress disorder, PTSD, childhood abuse, childhood maltreatment trauma, CMT
Breastfeeding is known to have health benefits for mother and infant and is universally recommended with very few exceptions for at least one to two years (United States Department of Health and Human Services [USDHHS], 2010). Breastfeeding reduces maternal risk of breast and ovarian cancer (Chowdhury et al., 2015) and infant risk of diarrheal illness and death (Victora et al., 2016). Other benefits may include a lowered risk of postpartum depression and Type II diabetes (maternal), and decreased risk of allergy, respiratory illness, obesity, and type I and II diabetes (infant; Godfrey & Lawrence, 2010; Kramer & Kakuma, 2012). Possibly the most compelling benefit of breastfeeding is reduced risk of infant mortality. Bartick and Reinhold (2010) estimated that 900 infants die in the United States annually because they are not breastfed, and Victora and colleagues (2016) estimated that more than 800,000 deaths worldwide could be prevented with breastfeeding. However, despite the well-researched and widely-known benefits of breastfeeding, U.S. breastfeeding rates are significantly lower than national goals (Centers for Disease Control and Prevention [CDC], 2015).
Because breastfeeding is a complex relational act as well as a health behavior, it is important to consider life events or stressors that may contribute to reduced odds of breastfeeding. Recently, researchers have begun to consider the effects of childhood maltreatment trauma (CMT), defined as abuse or neglect before age 16 and post-traumatic stress disorder (PTSD) on lifetime physical, emotional, and relational health outcomes, including those related to pregnancy, birth, and early parenting (Bosquet Enlow et al., 2011; Enlow et al., 2009). The purpose of our study was to describe the prevalence and predictors of breastfeeding intent and outcomes in women with a history of CMT, including those with PTSD. We considered these effects within the context of socioeconomic status (SES) and other modifiable and non-modifiable factors known to affect the likelihood of breastfeeding exclusively or not in the immediate postpartum period.
Breastfeeding Decisions
The reasons why a woman may or may not breastfeed are complicated and include emotional, social, psychological, personal, cultural, and physical factors. Because breastfeeding is an active relationship between the mother and infant and takes place in a complex matrix, many disparate factors potentially affect breastfeeding rates. Race, educational status, geographic location, parity, previous experience of breastfeeding, and partner and peer support all appear to affect breastfeeding outcomes, and many of these factors are closely interrelated (Bai, Wunderlich, & Fly, 2010; CDC, 2013; Li, 2004). These effects may be positive, as with increased education and higher parity, or negative, as with lack of partner/peer support (Bai, Wunderlich, & Fly, 2010; Li, Fein, Chen, & Grummer-Strawn, 2008).
Recently, researchers found that breastfeeding is negatively affected by maternal mental health issues, including depression (Stuebe, Grewen, Pedersen, Propper, & Meltzer-Brody, 2012; Watkins, Meltzer-Brody, Zolnoun, & Stuebe, 2011; Zanardo et al., 2011; Figueirido, Canario, & Field, 2014) and that a history of CMT may affect the decision to breastfeed and/or the success of breastfeeding (Coles, 2009; Prentice, Lu, Lange, & Halfon, 2002). This earlier work suggested reduced odds of breastfeeding for women with a history of CMT, but more recent investigators have challenged those findings (Coles, 2015). The relationship between CMT and breastfeeding outcomes is, therefore, somewhat unclear at this time.
Post-traumatic Stress Disorder (PTSD) and Childhood Maltreatment Trauma (CMT)
Childhood maltreatment trauma is a common experience in the United States, affecting approximately one woman in five (Shi, 2013), and globally. A 2010 analysis of World Health Organization (WHO) data showed a similar proportion of childhood maltreatment and family violence (Kessler et al., 2010). Childhood maltreatment trauma is associated with emotional and neuroendocrine dysregulation, including increased interpersonal sensitivity (Shonkoff et al., 2011), increased risk of depression (American College of Obstetricians and Gynecologists, 2001; Norman et al, 2012), and dysfunctional stress-response systems (Schore, 2001). These sequelae can potentially affect breastfeeding by changing how the woman perceives her infant, how competent she believes herself to be, whether she has comorbid conditions such as depression, and whether she is able to tolerate the physical aspects of breastfeeding.
Some women with histories of CMT will develop PTSD, a psychological disorder with physical manifestations that include re-experiencing phenomena (American Psychiatric Association, 2013). The lifetime prevalence of PTSD in women is 12.3% (Kilpatrick et al., 2013), and the prevalence during the childbearing year is estimated at 8% (Seng, Low, Sperlich, Ronis, & Liberzon, 2009) or 320,000 women annually in the United States. PTSD is twice as prevalent in childbearing women as pre-eclampsia (3.9%; Ananth, Keyes, & Wapner, 2013) and almost as common as gestational diabetes (9.2%; DeSisto, Kim, & Sharma, 2014). PTSD is associated with increased tobacco use (Lopez, Konrath, & Seng, 2011), lower mean birth weight (Seng, Low, Sperlich, Ronis, & Liberzon, 2011), and shorter gestation (Seng et al., 2011; Shaw et al., 2014).
The underlying mechanisms for these PTSD-specific adverse outcomes are posited to be related to neuroendocrine changes that occur with traumatic stress sequelae (Seng, 2010; Seng et al., 2011) and/or changes in behaviors such as smoking to cope with stress and to self-medicate for symptoms or reduced utilization of prenatal care (Bell & Seng, 2013; Lopez et al., 2011; Lopez & Seng, 2014). Like breastfeeding, smoking is a complex health behavior with long-term implications and well-known potential sequelae, and therefore the research on the relationships between PTSD and smoking may provide guidance for considering the relationships between CMT/PTSD and breastfeeding behaviors.
Previous researchers associated a history of trauma (specifically childhood sexual abuse) with an increased likelihood of breastfeeding initiation (Prentice et al., 2002), while other researchers found no difference in breastfeeding duration with and without a history of childhood sexual abuse (Coles, Anderson, & Loxton, 2015). However, these researchers did not consider the specific characteristics of PTSD, which may mediate between trauma history and breastfeeding intent and/or continuation (Seng, 2002). These characteristics can include intrusive memories, dissociation, and physiologic hyperarousal, all of which may have adverse effects on the breastfeeding relationship.
Breastfeeding, Mental Health, and Relational Health
Problematic breastfeeding relationships may have effects beyond whether or not a woman chooses to or is able to breastfeed. Women who stopped breastfeeding before the intended weaning age or who had negative breastfeeding experiences had significantly increased rates of depression (Watkins et al., 2011; Ystrom, 2012). These findings suggest an interactive relationship between the emotional and relational aspects of breastfeeding and that whether depression and maternal-infant dysregulation precede or follow breastfeeding outcomes, they are linked. In particular, a disrupted breastfeeding relationship may negatively affect how the woman views her infant as a child and herself as a mother. This kind of negative framing of the infant or the maternal-infant relationship has been associated with changes in maternal-infant relationships (Muzik et al., 2013). Because of the potential significance of breastfeeding disruption and because of the particular vulnerability to poor perinatal outcomes for women who have experienced abuse, research on the effects of the mother’s history of early relational trauma (i.e., CMT) and PTSD on breastfeeding outcomes is warranted.
Methods
Design and Parent Study
We conducted a secondary analysis of an existing dataset in which first-time mothers were well-characterized on trauma history, PTSD, depression, feeding plans, feeding outcomes, and several other factors salient to odds of breastfeeding success. The parent study, known as the Stress, Trauma, and Anxiety in the Childbearing Year (STACY) Project (NIH NR008767, PI Seng) was a prospective three-cohort study of perinatal outcomes in women with PTSD. The data for this secondary analysis were collected at all three time points of the parent study: the initial enrollment interview prior to 28 weeks gestation, the third-trimester interview at approximately 35 weeks gestation, and the final interview six weeks postpartum. Data were also abstracted medical records from the entire pregnancy. Recruitment, survey procedures, and instruments used were extensively described in previous publications (Lopez & Seng, 2014; Seng et al., 2011; 2013) and are reviewed briefly here.
Recruitment and Interview Procedures for Parent Study
Eligible women (age 18 or older, pregnant with a first infant, able to speak English without an interpreter, and in the first or second trimester of pregnancy) were recruited from maternity clinics in three health systems in the Midwestern United States. Clinic nurses identified eligible women and invited them to participate in a survey about stressful things that happen to women, emotions, and pregnancy. Those who accepted the invitation were given written information about the study and provided their contact information. Interviews took place between August 2005 and October 2007 via a professional survey research organization (DataStat, Ann Arbor, Michigan). The surveyors verified eligibility and obtained verbal informed consent, which included an explanation of the confidentiality certificate provisions. This study was approved by the Institutional Review Boards of all three health systems. University human subjects institutional review board approval for this secondary analysis was obtained before analysis of data. The interviews used a computer-assisted telephone interview (CATI) program to conduct a validated diagnostic interview, and a computerized algorithm applied DSM-IV PTSD symptom diagnostic criteria to assign the participants to one of three cohorts: lifetime PTSD-diagnosed (n=319); trauma-exposed PTSD-resilient controls (n=380); and nonexposed controls (n=350). Women who did not fit one of these three cohorts (n=532) were dismissed from follow-up, and were excluded from this study. The size of the sample (n=1581) was determined from power estimates and allowed for attrition to study low-frequency perinatal outcomes, such as hyperemesis gravidarum.
Organizing Framework
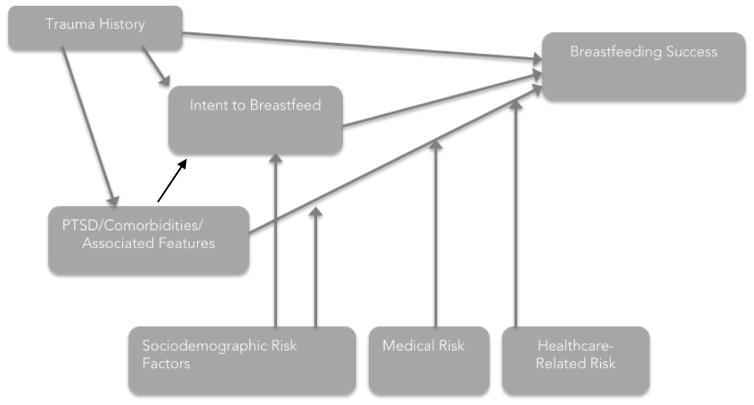
The underlying framework for the statistical modeling in this secondary analysis was an adaptation of the framework previously used to study general relationships between perinatal outcomes and PTSD (Seng, 2002; Figure 1). For this analysis, the framework removed physical injury as a potential sequela of abuse, as such injury is rarely directly the cause of breastfeeding challenges, and made the model outcomes breastfeeding-specific. These adaptations streamlined the application of the model but did not significantly change the theoretical relationships between CMT and perinatal outcomes. In this regression model, we posited that reduced likelihood of breastfeeding for women who have experienced trauma is mediated by PTSD, rather than predicted by the history of trauma itself, and further modified by a number of other factors, including socioeconomic status, partner status, education, prenatal education, and pregnancy-related risk factors like cesarean birth and NICU admission (Figure 1).
Figure 1.
Theoretical framework for relationship between childhood maltreatment (CMT) and breastfeeding outcomes. Adapted from Seng, J. S. (2002). A conceptual framework for research on lifetime violence, posttraumatic stress, and childbearing. Journal of Midwifery & Women’s Health, 47(5), 337–346. Used with permission from American College of Nurse-Midwives.
Measures
The parent study emphasized the use of established instruments when possible. The two key variables for establishment of the comparison groups, trauma history and PTSD symptoms, were measured using well-validated instruments (Table 1). The Life Stressor Checklist (LSC; Wolfe & Kimerling, 1997) assessed 29 traumatic events as dichotomous variables (i.e., occurred/did not occur). The LSC is specifically intended to assess trauma in women and was the most sensitive measure available at that time (Cusack, Falsetti, & de Arellano, 2002). PTSD symptoms (both lifetime and current) were assessed using the National Women’s Study PTSD module (Resnick, et al., 1993), which has high sensitivity and specificity for identifying PTSD when compared to the standard diagnostic interview (Structured Clinical Interview for DSM Disorders, Kilpatrick et al., 1994). Demographic information was collected using questions from the CDC Prenatal Risk Assessment and Monitoring System (PRAMS) survey. Depression and dissociation were measured using standard measures (Composite International Diagnostic Interview-Short Form; UM-CIDI [Wittchen et al., 1994] and Dissociative Experiences Scale-Taxon (DES-T [Bernstein & Putnam, 1986; Waller, Putnam, & Carlson, 1996]). Provider alliance was assessed using a new instrument, the Healthcare Alliance Questionnaire (Roosevelt, Holland, Hiser, & Seng, 2015), while other variables (intent to breastfeeding, attendance at childbirth education) were assessed using direct survey questions.
Table 1.
Validity testing for variable measures
| Measure | Validity testing (original) | Alpha coefficient (this sample) |
|---|---|---|
| National Women’s Study PTSD | 0.99 (sensitivity) | NA |
| Module (NWS-PTSD) | 0.79 (specificity) | |
| Composite International Depression Interview-Short Form (UM-CIDI) | Kappa 0.97 (depression only) | NA |
| Dissociative Experiences Scale- Taxon (DES-T) | test-retest coefficient: 0.86 split-half reliability coefficients: 0.71–0.96 | 0.68 |
| Health Care Alliance Questionnaire (HCAQ) | 0.93 | 0.93 |
| Parenting Sense of Competence (PSOC) | NA – modified significantly from original instrument | NA |
Data Reduction and Group Classification
The sample for the study included all women who participated in all three waves of data collection, and for whom medical records data were available (n=520). One woman stated that she was “not sure” how she was feeding her baby at the six-week interview and was dropped from analysis (final n=519). This sample was chosen in order to incorporate as many variables as possible that had previously been shown to be significant in the literature or were of interest for this analysis. For example, data from Wave 1 included the intended method of infant feeding (Donath, 2003), as well as prenatal/prepregnancy history of major depression (Figueiredo, Canario, & Field, 2014). Because variables were collected at different time points, and because the analysis included factors from each time point, only women with complete data were included in the final analysis. Given standard estimates of adequate sample size (Hulley, et al., 2013), the final sample size was adequately powered for this analysis.
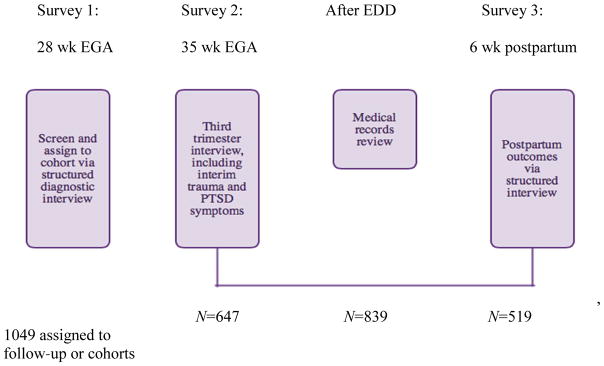
In the parent study, any of the 29 LSC trauma history exposures could have been the index trauma. However, for this analysis, where CMT is the salient trauma history, we formed different groupings from those in the parent study. The CMT-resilient group included women who experienced CMT, but did not have PTSD (n=38). The CMT-PTSD group included women who both experienced CMT and met diagnostic criteria for lifetime PTSD (n=61). The CMT-nonexposed control group had neither (n=420; Figure 2). The final sample size was 519.
Figure 2.
Sample derivation for secondary analysis from Stress, Trauma, and Anxiety in the Childbearing Year (STACY), N=1581. EGA = ; EDD =; PTST = posttraumatic stress disorder.
Contrary to previous analyses of these data (Bell & Seng, 2013; Seng et al., 2011; 2013), we retained individual demographic risk factors rather than using a sum of PTSD risk factors (race, poverty, high crime, low education, and age <21). This was done because each of the risk factors except residence in a high-crime area was previously associated with lower rates of breastfeeding, and our intent was to clarify these relationships as much as possible. Because African American women are significantly less likely to breastfeed than are other women (Centers for Disease Control and Prevention [CDC], 2013; Li, 2004), race was classified as African American or not African American. Poverty was defined as household income <$15,000, and low education as high school or less.
Intent to breastfeed and infant feeding outcome were measured by categorical responses to a direct question. The response options were Bottle, Breast, and Both bottle and breast. Because amount of breastfeeding intended when a woman responded Both breast and bottle could not be determined, the two categories were collapsed into one category, Any breastfeeding, for the purposes of the regression analysis. This meant that the analysis did not distinguish between women who primarily formula-fed (with some breastfeeding) and those who primarily breastfed (with some formula). However, it also meant that all breastfeeding was captured, regardless of amount, for both prenatal intent and postpartum experiences.
Analysis Plan
The participants in the sample were compared by group (CMT-resilient, CMT-PTSD, and CMT-nonexposed) on demographic risk factors, prior and current major depressive disorder, attendance at childbirth education, intent to breastfeed, partner status, and infant feeding method at six weeks postpartum using chi-square tests for categorical variables, and one-way ANOVA for interval-level variables. Logistic regression modeling with variables entered in steps consistent with the conceptual framework (see Figure 1 and Table 5) was used to answer the primary research questions: 1) to what extent do CMT and PTSD status predict infant feeding outcomes in the early postpartum period, and 2) is this moderated by known risk factors for non-initiation/early discontinuation of breastfeeding?
Table 5.
Effects of variables on breastfeeding outcomes at 6 weeks postpartum
| Odds ratio (OR) | p-value | ||
|---|---|---|---|
| Step 1: Intent Intent to breastfeed |
R2=.242, p<.001 | 44.815 | <.001 |
| Step 2: Trauma Adds childhood maltreatment trauma |
R2=.243, R2 =.001, p=.001 | ||
| Intent to breastfeed | 44.586 | <.001 | |
| Hx CMT | 1.219 | .481 | |
| Step 3: PTSD Adds PTSD (lifetime diagnosis) |
R2=.267, R2 =.024, p=.001 | ||
| Intent to breastfeed | 44.286 | <.001 | |
| Hx CMT | 1.808 | .061 | |
| Hx PTSD | .426 | .001 | |
| Step 4: Mental health Adds prenatal dx of major depression |
R2=.288, R2 =.021, p=.003 | ||
| Intent to breastfeed | 43.434 | <.001 | |
| Hx CMT | 1.891 | .050 | |
| Hx PTSD | .549 | .034 | |
| Hx MDD | .363 | .003 | |
| Step 5: Health system Adds medical risk factors and CBE |
R2=.466, R2 =.118, p<.001 | ||
| Intent to breastfeed | 24.145 | <.001 | |
| Hx CMT | 2.522 | .011 | |
| Hx PTSD | .524 | .044 | |
| Hx MDD | .343 | .005 | |
| Attended CBE | 9.016 | <.001 | |
| Cesarean birth | .763 | .307 | |
| NICU admission | .762 | .400 | |
| Step 6: Parenting Adds perceived parenting competence at 6 weeks postpartum |
R2=.471, R2 =.005, p<.001 | ||
| Intent to breastfeed | 22.229 | <.001 | |
| Hx CMT | 2.465 | .014 | |
| Hx PTSD | .503 | .033 | |
| Hx MDD | .345 | .006 | |
| Attended CBE | 8.676 | <.001 | |
| Cesarean birth | .753 | .286 | |
| NICU admission | .673 | .305 | |
| PSOC | .933 | .143 | |
| Step 7: PRAMS Adds demographic risk factors |
R2=.606, R2 =.135, p<.001 | ||
| Intent to breastfeed | 14.958 | <.001 | |
| Hx CMT | 3.176 | .006 | |
| Hx PTSD | .492 | .049 | |
| Hx MDD | .402 | .039 | |
| Attended CBE | 2.557 | .005 | |
| Cesarean birth | .653 | .175 | |
| NICU admission | .519 | .139 | |
| PSOC | .986 | .773 | |
| Poverty (<$15K) | 1.416 3.039 | .376 | |
| Partnered | .659 | .004 | |
| Teen (18–20 yo) | .439 | .328 | |
| Education (HS or less) | .305 | .038 | |
| African American | .001 |
Note: Hx = history of; CMT = childhood maltreatment trauma; PTSD = posttraumatic stress disorder; MDD = major depressive disorder; CBE = childbirth education; NICU = neonatal intensive care unit; PSOC = parenting sense of competence.
Results
Sample
This sample represented a diverse group of women. Fifteen percent (n=78) had household incomes less than $15,000 annually, and 31.8% (n=165) had a high school education or less. Nearly a third of women (29.9%, n=155) identified as African American, 28.5% (n=148) described themselves as single, and 15.8% (n=82) were 18–20 years old at the first interview (Table 2).
Table 2.
Sample characteristics
| Variable | n (%) |
|---|---|
| History of childhood maltreatment trauma | 99 (19.1) |
| Lifetime history of posttraumatic stress disorder | 138 (26.6) |
| Poverty (<$15,000 annual household income) | 78 (15.0) |
| Single (not married or partnered) | 148 (28.5) |
| Teen (18–20 years old) | 82 (15.8) |
| High school education or less | 165 (31.8) |
| African American | 155 (29.9) |
| Provider (n=511) | |
| Physician | 396 (76.3) |
| Midwife | 115 (22.2) |
Infant Feeding Classification
Prenatal intent to breastfeed
Overall, 60.5% of women (n=314) intended to exclusively breastfeed, while 9.1% (n=47) intended to exclusively formula-feed. The remainder of women intended to mix bottle and breastfeeding, and nine out of ten intended for their infants to receive at least some breastmilk. Prenatal intent to breastfeed differed significantly across the cohorts when comparing intended exclusive and mixed feeding (χ2=10.523, df=6, p=.020). Intent to exclusively breastfeed was highest for the CMT-resilient group (84.2%, n=32), and lowest for the CMT-PTSD group (57.4%, n=35), while intent to exclusively formula-feed varied from a low of 5.3% for the CMT-resilient group (n=2) to 9.5% (n=40) for the CMT-nonexposed group (Table 3).
Table 3.
Intended feeding method at 28 weeks of pregnancy and feeding method at 6 weeks postpartum
| Group | Exclusive breast n (%) | Mixed feeding n (%) | Exclusive formula n (%) | Don’t know | Chi-squared n (%) |
|---|---|---|---|---|---|
| Intended feeding method | |||||
| CMT-resilient | 32 (84.2) | 3 (7.9) | 2 (5.3) | 1 (2.6) | χ2=10.523, df=6, p=.020 |
| CMT-PTSD | 35 (57.4) | 19 (31.1) | 5 (8.2) | 2 (3.3) | |
| Non-CMT | 247 (58.8) | 115 (27.4) | 40 (9.5) | 18 (4.3) | |
| Overall | 314 (60.5) | 137 (26.4) | 47 (9.1) | 21 (4.0) | |
| Actual feeding method | |||||
| CMT-resilient | 23 (60.5) | 6 (15.8) | 9 (23.7) | NA | χ2=14.817, df=4, p=.005 |
| CMT-PTSD | 19 (31.1) | 21 (34.4) | 21 (34.4) | ||
| Non-CMT | 206 (49.0) | 136 (32.4) | 78 (18.6) | ||
| Overall | 246 (47.8) | 163 (31.4) | 110 (21.2) | ||
Note. CMT: childhood maltreatment trauma; PTSD: posttraumatic stress disorder
Infant feeding method at postpartum survey
Overall, just under half of all women surveyed were breastfeeding exclusively at six weeks postpartum (χ2=14.817, df=4, p=.005). As with prenatal intent to breastfeed, women in the CMT-resilient group were most likely to be exclusively breastfeeding postpartum (60.5%, n=23), while women in the CMT-PTSD group were least likely (31.1%, n=19). Unlike prenatal intent to breastfeed, women in the CMT-resilient group fell in between the other two groups in exclusive formula use (23.7%, n=9, compared to 34.4%[n=21] for the CMT-PTSD group and 18.6% [n=78] for the CMT-nonexposed group) (Table 3).
Mental Health and Trauma History
Of the 519 participants, 99 (19.1%) had a history of CMT, and 138 (26.6%) had a lifetime history of PTSD. There were no differences in breastfeeding rates at six weeks postpartum when comparing women with a history of CMT with those without (χ2=.970, p=.325). Women with a history of PTSD were 24% less likely to be breastfeeding at all at six weeks than were women without PTSD (58.7% [n=81], χ2=8.549, df=2, p=.003), compared to 77.2% [n=371], χ2=14.817, df=4, p=.005). One woman in nine (12.3%, n=64) reported a lifetime history of major depressive disorder (MDD), and fewer than half of these were breastfeeding at the postpartum survey (45.3%, n=29,χ2=18.367, df=2, p<.001) (Table 3).
Health-related Factors
The rate of Cesarean birth in the sample was 31.6% (n=164) and one infant in eight was admitted to the neonatal intensive care unit (12.5%, n=63). An overwhelming majority (79.8%) of women had at least one antepartum complication such as hypertension, threatened preterm labor, substance use, or smoking (n=414), and 88.4% (n=459) had at least one intrapartum complication/intervention, including infection, Pitocin, or epidural use. Postpartum complications such as hemorrhage were much less frequent, affecting 3.5% (n=18) of women in the sample. Of health-related factors (Cesarean birth, NICU admission, and/or ante/intra/postpartum complications), only NICU admission (χ2=5.107, p=.024) and postpartum complications (χ2=7.637, p=.006) were associated with a decreased frequency of breastfeeding. (Table 4)
Table 4.
Breastfeeding rates at 6 weeks postpartum by variable
| Variable | Sample total n (%) | Breastfeeding n (%) | Not breastfeeding n (%) | Test statistic | p- value |
|---|---|---|---|---|---|
| African American | 155 (29.9) | 41(26.5) | 114 (73.5) | χ2=82.189 | <.001 |
| Pregnant as a teen (18–20) | 82 (15.8) | 21 (25.6) | 61 (74.4) | χ2=83.523 | <.001 |
| High school education or less | 165 (31.8) | 48 (29.1) | 117 (70.9) | χ2=175.225 | <.001 |
| Poverty (<$15K/year) | 78 (15.0) | 28 (35.9) | 50 (64.1) | χ2=45.552 | <.001 |
| Single | 148 (28.5) | 42 (28.4) | 106 (71.6) | χ2=155.428 | <.001 |
| CMT+ | 99 (19.1) | 72 (72.7) | 27 (27.2) | χ2=.970 | .325 |
| PTSD+ | 138 (26.6) | 81 (58.7) | 57 (41.3) | χ2=8.549 | .003 |
| Intended to breastfeed | 451 (90.6) | 342 (75.8) | 109 (24.2) | χ2=96.454 | <.001 |
| Major depression | 64 (12.3) | 29 (45.3) | 35 (54.7) | χ2=18.367 | <.001 |
| Dissociation mean (SD) | .37 (1.254) | .38 (1.306) | .36 (1.137) | F=.030 | .862 |
| Cesarean birth | 164 (31.6) | 108 (65.9) | 56 (34.1) | χ2=.835 | .361 |
| NICU admission | 63 (12.5) | 35 (55.6) | 28 (44.4) | χ2=5.107 | .024 |
| AP complications | 414 (79.8) | 276 (66.7) | 138 (33.3) | χ2=3.526 | .060 |
| IP complications | 459 (88.4) | 310 (67.5) | 149 (32.5) | χ2=2.053 | .152 |
| PP complications | 18 (3.5) | 7 (38.9) | 11 (61.1) | χ2=7.637 | .006 |
| BMI, mean (SD) (n=403) | 24.92 (6.665) | 24.23 (5.699) | 27.41 (8.968) | F=16.280 | <.001 |
| Attended CBE | 282 (54.3) | 253 (89.7) | 29 (10.3) | χ2=127.900 | <.001 |
| Provider alliance, mean (SD) | 67.66 (9.548) | 68.20 (9.722) | 66.46 (9.049) | F=3.742 | .054 |
| Parenting sense of competence, mean (SD) (n=453) | 52.66 (3.162) | 52.29 (3.338) | 53.55 (2.491) | F=15.639 | <.001 |
| Impaired postpartum bonding | 118 (22.7) | 100 (84.7) | 18 (15.3) | χ2=18.496 | <.001 |
| Discomfort with IAP, mean (SD) | 13.91 (3.260) | 14.28 (2.680) | 13.104 (4.157) | F=14.820 | <.001 |
Note: CMT = childhood maltreatment trauma; PTSD = posttraumatic stress disorder; NICU = neonatal intensive care unit; AP = antepartum; IP = intrapartum; PP = postpartum; BMI = body mass index; CBE = childbirth education; IAP = intimate aspects of parenting (e.g., diaper changes).
Other Factors
Approximately half of all women attended childbirth education classes (54.3%, n=282); of these women, 89.7% (n=253) were breastfeeding at six weeks postpartum (χ2=127.900, p<.001). Women who were breastfeeding at six weeks had a decreased parenting sense of competence (μ=52.29, SD=3.338, f=15.639, p<.001) compared both to women who were not breastfeeding at six weeks (μ=53.55, SD=2.491) and to the sample overall (μ=52.66, SD=3.162); however, it is unclear whether these represent clinically-significant differences or what their clinical implications may be (Table 4).
Regression Models
A stepwise logistic regression model (Table 5) was used to explore the factors that increased the risk of not breastfeeding at six weeks postpartum, and to identify the relationships between those factors. The model was based on the modified PTSD/perinatal outcomes framework described above and shown in Figure 1, and considered 1) prenatal intent to breastfeed, 2) history of CMT (abuse or neglect prior to the age of 16), 3) lifetime history of PTSD, 4) lifetime history of major depression, 5) medical risk factors and attendance at CBE, 6) parenting sense of competence, and 7) demographic factors associated in the literature with not breastfeeding. Factors included in the models were derived from factors known in the literature to affect breastfeeding, and those consistent with the theoretical framework. Overall, the regression model predicted 60.1% of variance.
Consistent with previous research (Chezem, 2003; Donath, et al., 2003), prenatal (<28 weeks) intent to breastfeed was by far the strongest predictor of breastfeeding, and was associated with a nearly 15-fold increase in breastfeeding likelihood at six weeks postpartum(OR 14.958, p<.001). Seven other factors (history of CMT, lifetime history of PTSD, lifetime history of major depression, attendance at CBE, partner status, education, and race) were significant in the final step of the model. The Hosmer-Lemeshow goodness-of-fit statistic for the logistic regression models was above the discriminant of .05 at .797, indicating an acceptable model fit (Archer, Lemeshow, & Hosmer, 2007). The significant factors remaining in the final step of the model included both positive factors (increased the likelihood of breastfeeding) and negative factors (decreased the likelihood of breastfeeding) (Table 5). Each of these factors had a unique contribution to predicting breastfeeding odds, which are described below.
Positive Factors
Four factors, prenatal intent to breastfeed, history of CMT, attendance at CBE, and having a partner relationship, predicted an increased likelihood of breastfeeding at the six-week interview. As noted above, intent to breastfeeding was associated with a 15-fold increase in odds of breastfeeding. Both a history of CMT and having a partner relationship were associated with an approximately threefold increase in breastfeeding (CMT OR 3.176, p=.006; partner relationship OR 3.039, p=.004). Women who attended CBE were two and a half times more likely to breastfeed than were women who did not (OR 2.557, p=.005). (Table 5)
Negative Factors
Four factors, lifetime history of CMT-mediated PTSD, lifetime history of major depression, high school education or less, and African American race, were associated with lower rates of breastfeeding in the final step of the model. Women with a lifetime history of CMT-mediated PTSD were half as likely to breastfeed as were women without that history (OR .492, p=.049), and women with a lifetime history of major depression were 60% less likely to breastfeed than were women without that history (OR .402, p=.039). Of the demographic factors considered, women with a high school education or less were half as likely to breastfeed as were women who had attended postsecondary education (OR .439, p=.038), and African American women were 70% less likely to breastfeed than were other women (OR .305, p=.001) (Table 5).
Nonsignificant Factors
Several factors that were significant in previous research were not significant in this model. Neither Cesarean birth nor NICU admission were significant in the final step of the model. Neither teen pregnancy nor poverty, both previously associated with decreased odds of breastfeeding, were significant. Parenting sense of competence was likewise not significant in the final model (Table 5).
Discussion
Previous analyses have shown that PTSD is associated with negative perinatal outcomes, including shorter gestation (Seng et al., 2011), lower birth weight (Seng et al., 2011), more substance use (Lopez et al., 2011; Rogal et al., 2007), and greater risk of postpartum depression (Grote et al., 2012). In this analysis, we confirmed that PTSD is also implicated in lower breastfeeding rates, which has long-term health implications for both mother and infant. This association held when controlling for history of maltreatment, pre-existing depression, and socioeconomic risk factors, all of which had previously been associated with lower odds of breastfeeding. Thus, in this analysis it was the PTSD sequelae rather than maltreatment history itself that was the key risk factor for not breastfeeding. This underscores the importance of assessing for, and distinguishing between, resilient and PTSD-affected women with a history of CMT.
CMT and PTSD Effects on Breastfeeding
Women who have experienced CMT intended to breastfeed at rates similar to those of their non-exposed peers, and those without PTSD were 15% more likely to plan breastfeeding than are those with PTSD. More strikingly, women who were CMT-resilient were twice as likely to be breastfeeding exclusively at six weeks when compared to their PTSD-affected peers. While the intent was similar for all three groups, PTSD-mediated differences created divergent outcomes. This may be due to increased PTSD symptoms or “triggering” related to pregnancy, birth, or breastfeeding itself, or may be due to underlying changes in physiology related to previous abuse, such as alterations in cortisol-oxytocin regulation (Schore, 2001). It is possible that PTSD-affected mothers are less able to tolerate the intimate physical aspects of breastfeeding, or that reactivation of PTSD symptoms from pregnancy and/or birth is problematic, rather than breastfeeding itself.
The strongest predictor of breastfeeding outcome in our analysis remained prenatal intent to breastfeed. Of the non-intent predictors of breastfeeding, PTSD decreased the odds of breastfeeding by half. Given the three-fold higher breastfeeding odds conferred by a history of CMT, this 50% decrease represented a more clinically-significant loss than it initially seemed.
That CMT increased the odds of breastfeeding threefold is an interesting finding, and at first glance is counterintuitive: why, after all, would a negative life experience increase the odds of intent to perform a health behavior? However, this is congruent with previous qualitative findings that suggested a history of abuse may increase the motivation of the woman to breastfeed (e.g., Coles, 2009), possibly as a way to parent “correctly”. Thus, in breastfeeding as in other health outcomes, PTSD is a better predictor of outcomes than history of CMT alone.
Limitations
While the findings of our study are important to understanding the effects of PTSD on infant feeding, there were limitations. As a secondary analysis, the information about breastfeeding was limited to a single prenatal intent question and information about infant feeding status at the six-week postpartum visit. Previous researchers found that breastfeeding rates continue to fall throughout the postpartum year (CDC, 2015; Li, Fein, Chen, & Grummer-Strawn, 2008), and we did not have data on whether that was the case for this sample. Each of the intent and outcome variables relied on self-report, which may be subject to the perceived social desirability of breastfeeding given the emphasis on universal breastfeeding, and intent may vary throughout pregnancy and birth. (Importantly, there was no way to quantify the amount of breastfeeding for an infant who was receiving mixed breast/bottle feeding.) Previous research has also shown that prior experience with infant feeding is predictive of future infant feeding (DiGirolamo, Thompson, Martorell, Fein, & Grummer-Strawn, 2005), but our sample included only women expecting a first infant. Finally, while the available data are rich when considering the number of available variables, the size and composition of the sample, and the study design strength, they were collected almost 10 years ago, and may differ from the present situation.
Strengths
There were numerous strengths to this study as well. The sample included a diverse group of women from both public-access and private health clinics, which increased the generalizability of the results. Data were collected prospectively to minimize recall bias, particularly for subjective measures like infant feeding intent, and gold-standard instruments were used to identify women with CMT history and adverse lifetime mental health history, including PTSD and depression. The theoretical model used was a modification of one that had previously performed well in studies of perinatal outcomes in women with PTSD, and incorporated known risk and protective factors for infant feeding outcomes. This was the first study exploring the effects of PTSD on breastfeeding outcomes, and as such represented an important step to understanding the relationships between maternal mental health and infant outcomes. Finally, the regression model predicted a high proportion of the overall variance, suggesting this model was a valid basis for future research to support development of effective interventions.
Future Research Directions
Future research should include questions about both concerns and motivations for intent and initiation of breastfeeding among women with and without PTSD. In particular, there is a lack of information from women who experienced non-sexual abuse as children, and the potential effects of this early relational trauma on their breastfeeding relationships. Multiple time points for data collection on intent and continuation of breastfeeding would allow researchers to identify particularly high-risk points when interventions might be most effective. Questions about support for and constraints on breastfeeding, as well as types and sources of information about breastfeeding, will be helpful in designing trauma-informed breastfeeding interventions that may be applicable for all women. Additionally, research is needed to establish a woman-centered measure of breastfeeding success that reflects the complex nature of the breastfeeding relationship as well as the public-health recommendations for infant feeding.
Relevance to Clinical Practice
Our findings are informative for perinatal professionals, particularly nurses and midwives. CMT-related PTSD was a risk factor for reduced success at breastfeeding despite similar intent to breastfeed. This suggests that screening to identify the one in five women with CMT, and and to identify those with PTSD, during prenatal care are important for breastfeeding outcomes as well as maternal mental health, perinatal, and parenting outcomes. We should not assume that positive intention will translate to success, and we should stand by to support women with CMT history, especially those with PTSD, with trauma-informed care and trauma-specific interventions. These latter remain to be developed, but simple changes in practice that are consistent with trauma-informed care (e.g., asking permission to touch, individualizing care, awareness of language choices, and awareness of the prevalence of abuse) are within the scope of all providers, and are part of many nurses’ practices already (Jennings, 2004).
Given the relatively brief window of opportunity to establish a successful breastfeeding relationship, the prenatal period represents an opportunity to focus on making a plan if breastfeeding does not go as intended, as well as for the mother to clarify what she considers “successful breastfeeding”. This study also lends support to the need to individualize care, including consideration of a particular woman’s history and needs, when providing care in the immediate postpartum period. With the rapid increase in facilities participating in the Baby-Friendly Hospital Initiative (BFHI), policies need to take into consideration the effects of BFHI policies and norms on individual clients. While breastfeeding is the preferred method of infant feeding, it may not be desirable for all women, and support for these women needs to continue even as we shift our practices and norms to those of the BFHI.
Since we know that one in five women have a history of sexual abuse prior to age 18 (Shi, 2013), it is essential to move from thinking of this group of women as having an unusual (e.g., low-prevalence and idiosyncratic) problem to considering them a significant subpopulation whose physiology and psychology we must consider in care planning. Because PTSD is so common, and because breastfeeding has the potential for being both healing and/or re-traumatizing, there is a clear need for a trauma-informed model of the breastfeeding relationship.
We encourage the development of trauma-informed policies and care practices, as recommended by the Substance Abuse and Mental Health Services Administration (SAMHSA). “Trauma-informed” approaches or systems consider existing or proposed systems/theories within the context of what is known about the effects of violence and allows services to be delivered in a way that does not re-traumatize survivors of violence (Jennings, 2004).
While this is care that includes an understanding of how trauma may affect patients and health outcomes, it is appropriate for all patients, including those without a history of trauma exposure (SAMHSA, n.d.). As noted above, such care practices include simple changes like asking permission to touch the patient, informed consent, and awareness of language that may be difficult for some survivors. Given that one woman in five experiences CMT, that many may not disclose this history to their providers, and that trauma-informed care guidelines are consistent with ethical and respectful patient care, such care is appropriate in all clinical settings, for all patients.
Conclusion
Breastfeeding is a complex health behavior that encompasses biological, psychological, social, emotional, historical, and personal circumstances of both the breastfeeding woman and the infant. Likewise, PTSD has neuroendocrine, social, emotional, and personal effects for the trauma-exposed person. Efforts at increasing breastfeeding rates in the population have focused primarily on the cognitive and social aspects of breastfeeding behavior, but these findings suggest that maltreatment and mental health histories play a significant role in breastfeeding outcomes. While some of the factors affecting breastfeeding rates are non-modifiable or difficult to address (e.g., race, previous trauma history, partner status), health care systems can potentially address issues like access to and quality of CBE, and identify and treat mental health disorders including PTSD and depression. Given that women are likely to access health care in pregnancy, the perinatal period represents a time of opportunity for trauma-informed care to support women regardless of disclosure status, and for trauma-specific interventions to maximize not only breastfeeding rates, but potentially to reduce the lifetime burden of PTSD symptoms.
Callouts
Childhood abuse and post-traumatic stress disorder are growing topics of interest in perinatal research, but little is known about their effects on breastfeeding.
Women with a history of childhood maltreatment and post-traumatic stress disorder are half as likely to breastfeed at six weeks postpartum.
Using trauma-informed care may prevent re-traumatization and can be universal in perinatal care.
Footnotes
Disclosure
The authors report no conflict of interest or relevant financial relationships.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Meghan Eagen-Torkko, Assistant professor in the School of Nursing and Health Studies, University of Washington Bothell and a certified nurse-midwife in the Family Planning Program, Seattle, WA.
Lisa Kane Low, Associate Dean for Practice and Professional Graduate Studies and an associate professor in the School of Nursing, University of Michigan, Ann Arbor, MI.
Ruth Zielinski, Clinical associate professor in the School of Nursing, University of Michigan, Ann Arbor, MI.
Julia S. Seng, Professor in the School of Nursing, University of Michigan, Ann Arbor, MI.
References
- American College of Obstetricians and Gynecologists. ACOG (American College of Obstetricians and Gynecologists) educational bulletin. Adult manifestation of childhood sexual abuse, number 259, July 2000. Clinical management guidelines for obstetrician473 gynecologists. International Journal of Gynaecology and Obstetrics. 2001;74(3):311–320. doi: 10.1016/s0020-7292(01)00491-x. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Arlington, VA: American Psychiatric Publishing; 2013. pp. 271–280. [Google Scholar]
- Ananth CV, Keyes KM, Wapner RJ. Pre-eclampsia rates in the United States, 1980–2010: Age-period-cohort analysis. British Medical Journal. 2013;347:f6564–f6564. doi: 10.1136/bmj.f6564. http://doi.org/10.1136/bmj.f6564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Archer KJ, Lemeshow S, Hosmer DW. Goodness-of-fit tests for logistic regression models when data are collected using a complex sampling design. Computational Statistics & Data Analysis. 2007;51(9):4450–4464. doi: 10.1016/j.csda.2006.07.006. [DOI] [Google Scholar]
- Bai Y, Wunderlich SM, Fly AD. Predicting intentions to continue exclusive breastfeeding for 6 months: a comparison among racial/ethnic groups. Maternal and Child Health Journal. 2010;15(8):1257–1264. doi: 10.1007/s10995-010-0703-7. http://doi.org/10.1007/s10995-010-0703-7. [DOI] [PubMed] [Google Scholar]
- Bartick M, Reinhold A. The burden of suboptimal breastfeeding in the United States: A pediatric cost analysis. Pediatrics. 2010;125(5):e1048–e1056. doi: 10.1542/peds.2009-1616. http://doi.org/10.1542/peds.2009-1616. [DOI] [PubMed] [Google Scholar]
- Bell SA, Seng J. Childhood maltreatment history, posttraumatic relational sequelae, and prenatal care utilization. Journal of Obstetric, Gynecologic, & Neonatal Nursing. 2013;42(4):404–415. doi: 10.1111/1552-6909.12223. http://doi.org/10.1111/1552-6909.12223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein EM, Putnam FW. Development, reliability, and validity of a dissociation scale. Journal of Nervous and Mental Disease. 1986;174(12):727–735. doi: 10.1097/00005053-198612000-00004. [DOI] [PubMed] [Google Scholar]
- Bosquet Enlow M, Kitts RL, Blood E, Bizarro A, Hofmeister M, Wright RJ. Maternal posttraumatic stress symptoms and infant emotional reactivity and emotion regulation. Infant Behavior and Development. 2011;34(4):487–503. doi: 10.1016/j.infbeh.2011.07.007. http://doi.org/10.1016/j.infbeh.2011.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Progress in increasing breastfeeding and reducing racial/ethnic differences - United States, 2000–2008 births. Morbidity and Mortality Weekly Report. 2013;62(5):77–80. [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Breastfeeding report card –– United States, 2014. 2015 Retrieved from https://www.cdc.gov/breastfeeding/pdf/2014breastfeedingreportcard.pdf.
- Chezem J. Breastfeeding knowledge, breastfeeding confidence, and infant feeding plans: Effects on actual feeding practices. Journal of Obstetric, Gynecologic, & Neonatal Nursing. 2003;32(1):40–47. doi: 10.1177/0884217502239799. http://doi.org/10.1177/0884217502239799. [DOI] [PubMed] [Google Scholar]
- Coles J. Qualitative study of breastfeeding after childhood sexual assault. Journal of Human Lactation. 2009;25(3):317–324. doi: 10.1177/0890334409334926. http://doi.org/10.1177/0890334409334926. [DOI] [PubMed] [Google Scholar]
- Coles J, Anderson A, Loxton D. Breastfeeding duration after childhood sexual abuse: an Australian cohort study. Journal of Human Lactation. 2015;32(3):NP28–NP35. doi: 10.1177/0890334415590782. http://doi.org/10.1177/0890334415590782. [DOI] [PubMed] [Google Scholar]
- Cusack K, Falsetti S, de Arellano M. Gender considerations in the psychometric assessment of PTSD. In: Kimerling R, Ouimette P, Wolfe J, editors. Gender and PTSD. New York: Guilford Press; 2002. [Google Scholar]
- DeSisto CL, Kim SY, Sharma AJ. Prevalence estimates of gestational diabetes mellitus in the United States, Pregnancy Risk Assessment Monitoring System (PRAMS), 2007–2010. Preventing Chronic Disease. 2014;11:E104. doi: 10.5888/pcd11.130415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiGirolamo A, Thompson N, Martorell R, Fein S, Grummer-Strawn L. Intention or experience? Predictors of continued breastfeeding. Health Education & Behavior. 2005;32(2):208–226. doi: 10.1177/1090198104271971. http://doi.org/10.1177/1090198104271971. [DOI] [PubMed] [Google Scholar]
- Donath SM, Amir LH ALSPAC Study Team. Relationship between prenatal infant feeding intention and initiation and duration of breastfeeding: A cohort study. Acta Paediatrica. 2003;92(3):352–356. [PubMed] [Google Scholar]
- Enlow MB, Kullowatz A, Staudenmayer J, Spasojevic J, Ritz T, Wright RJ. Associations of maternal lifetime trauma and perinatal traumatic stress symptoms with infant cardiorespiratory reactivity to psychological challenge. Psychosomatic Medicine. 2009;71(6):607–614. doi: 10.1097/PSY.0b013e3181ad1c8b. http://doi.org/10.1097/PSY.0b013e3181ad1c8b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Figueiredo B, Canário C, Field T. Breastfeeding is negatively affected by prenatal depression and reduces postpartum depression. Psychological Medicine. 2014;44(5):927–936. doi: 10.1017/S0033291713001530. [DOI] [PubMed] [Google Scholar]
- Godfrey JR, Lawrence RA. Toward optimal health: the maternal benefits of breastfeeding. Journal of Women’s Health. 2010;19(9):1597–1602. doi: 10.1089/jwh.2010.2290. http://doi.org/10.1089/jwh.2010.2290. [DOI] [PubMed] [Google Scholar]
- Grote NK, Spieker SJ, Lohr MJ, Geibel SL, Swartz HA, Frank E, et al. Impact of childhood trauma on the outcomes of a perinatal depression trial. Depression and Anxiety. 2012;29(7):563–573. doi: 10.1002/da.21929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hulley SB, Cummings SR, Browner WS, Grady D, Newman TB. Designing clinical research : An epidemiologic approach. 4. Philadelphia, PA: Lippincott Williams & Wilkins; 2013. [Google Scholar]
- Ip S, Chung M, Raman G, Chew P, Magula N, DeVine D, Trikalinos T, Lau J. Breastfeeding and maternal and infant health outcomes in developed countries. Rockville, MD: Agency for Healthcare Research and Quality; 2007. AHRQ Publication No. 07-E007. [PMC free article] [PubMed] [Google Scholar]
- Jennings A. Models for developing trauma-informed behavioral health systems and trauma-specific services. Alexandria, VA: National Association of State Mental Health Program Directors, National Technical Assistance Center for State Mental Health Planning; 2004. [Google Scholar]
- Kessler RC, McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, … Williams DR. Childhood adversities and adult psychopathology in the WHO World Mental Health Surveys. British Journal of Psychiatry. 2010;197(5):378–385. doi: 10.1192/bjp.bp.110.080499. http://doi.org/10.1192/bjp.bp.110.080499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, Friedman MJ. National estimates of exposure to traumatic events and PTSD prevalence using DSM-IVand DSM-5 criteria. Journal of Traumatic Stress. 2013;26(5):537–547. doi: 10.1002/jts.21848. http://doi.org/10.1002/jts.21848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer MS, Kakuma R. Optimal duration of exclusive breastfeeding. Cochrane Database of Systematic Review. 2012;8:CD003517. doi: 10.1002/14651858.CD003517.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li R. Breastfeeding rates in the United States by characteristics of the child, mother, or family: The 2002 National Immunization Survey. Pediatrics. 2004;115(1) doi: 10.1542/peds.2004-0481. http://doi.org/10.1542/peds.2004-0481. [DOI] [PubMed] [Google Scholar]
- Li R, Fein SB, Chen J, Grummer-Strawn LM. Why mothers stop breastfeeding: mothers’ self-reported reasons for stopping during the first year. Pediatrics. 2008;122(Supplement 2):S69–76. doi: 10.1542/peds.2008-1315i. http://doi.org/10.1542/peds.2008-1315i. [DOI] [PubMed] [Google Scholar]
- Lopez WD, Seng JS. Posttraumatic stress disorder, smoking, and cortisol in a community sample of pregnant women. Addictive Behaviors. 2014;39(10):1408–1413. doi: 10.1016/j.addbeh.2014.04.027. http://doi.org/10.1016/j.addbeh.2014.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez WD, Konrath SH, Seng JS. Abuse-related post-traumatic stress, coping, and tobacco use in pregnancy. Journal of Obstetric, Gynecologic, & Neonatal Nursing. 2011;40(4):422–431. doi: 10.1111/j.1552-6909.2011.01261.x. http://doi.org/10.1111/j.1552-6909.2011.01261.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muzik M, Bocknek EL, Broderick A, Richardson P, Rosenblum KL, Thelen K, Seng JS. Mother-infant bonding impairment across the first 6 months postpartum: the primacy of psychopathology in women with childhood abuse and neglect histories. Archives of Women’s Mental Health. 2013;16(1):29–38. doi: 10.1007/s00737-012-0312-0. http://doi.org/10.1007/s00737-012-0312-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman RE, Byambaa M, De R, Butchart A, Scott J, Vos T. The long-term health consequences of child physical abuse, emotional abuse, and neglect: a systematic review and meta-analysis. PLoS Med. 2012;9(11):e1001349. doi: 10.1371/journal.pmed.1001349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prentice JC, Lu MC, Lange L, Halfon N. The association between reported childhood sexual abuse and breastfeeding initiation. Journal of Human Lactation. 2002;18(3):219–226. doi: 10.1177/089033440201800303. http://doi.org/10.1177/089033440201800303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, Best CL. Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. Journal of Consulting and Clinical Psychology. 1993;61(6):984–991. doi: 10.1037//0022-006x.61.6.984. [DOI] [PubMed] [Google Scholar]
- Rogal SS, Poschman K, Belanger K, Howell HB, Smith MV, Medina J, Yonkers KA. Effects of posttraumatic stress disorder on pregnancy outcomes. Journal of Affective Disorders. 2007;102(1–3):137–143. doi: 10.1016/j.jad.2007.01.003. http://doi.org/10.1016/j.jad.2007.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roosevelt LK, Holland KJ, Hiser J, Seng JS. Psychometric assessment of the Health Care Alliance Questionnaire with women in prenatal care. Journal of Health Psychology. 2015;20(7):1013–1024. doi: 10.1177/1359105313506027. http://doi.org/10.1177/1359105313506027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schore AN. The effects of early relational trauma on right brain development, affect regulation, and infant mental health. Infant Mental Health Journal. 2001;22(1–2):201–269. [Google Scholar]
- Seng JS. A conceptual framework for research on lifetime violence, posttraumatic stress, and childbearing. Journal of Midwifery & Women’s Health. 2002;47(5):337–346. doi: 10.1016/s1526-9523(02)00275-1. [DOI] [PubMed] [Google Scholar]
- Seng JS. Posttraumatic oxytocin dysregulation: Is it a link among posttraumatic self disorders, posttraumatic stress disorder, and pelvic visceral dysregulation conditions in women? Journal of Trauma & Dissociation. 2010;11(4):387–406. doi: 10.1080/15299732.2010.496075. http://doi.org/10.1080/15299732.2010.496075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seng JS, Low LK, Sperlich M, Ronis DL, Liberzon I. Prevalence, trauma history, and risk for posttraumatic stress disorder among nulliparous women in maternity care. Obstetrics & Gynecology. 2009;114(4):839–847. doi: 10.1097/AOG.0b013e3181b8f8a2. http://doi.org/10.1097/AOG.0b013e3181b8f8a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seng JS, Low LK, Sperlich M, Ronis DL, Liberzon I. Post-traumatic stress disorder, child abuse history, birthweight and gestational age: a prospective cohort study. British Journal of Obstetrics and Gynaecology. 2011;118(11):1329–1339. doi: 10.1111/j.1471-0528.2011.03071.x. http://doi.org/10.1111/j.1471-0528.2011.03071.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seng JS, Sperlich M, Low LK, Ronis DL, Muzik M, Liberzon I. Childhood abuse history, posttraumatic stress disorder, postpartum mental health, and bonding: a prospective cohort study. Journal of Midwifery & Women’s Health. 2013;58(1):57–68. doi: 10.1111/j.1542-2011.2012.00237.x. http://doi.org/10.1111/j.1542-2011.2012.00237.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw JG, Asch SM, Kimerling R, Frayne SM, Shaw KA, Phibbs CS. Posttraumatic stress disorder and risk of spontaneous preterm birth. Obstetrics & Gynecology. 2014;124(6):1111–1119. doi: 10.1097/AOG.0000000000000542. http://doi.org/10.1097/AOG.0000000000000542. [DOI] [PubMed] [Google Scholar]
- Shi L. Childhood abuse and neglect in an outpatient clinical sample: Prevalence and impact. The American Journal of Family Therapy. 2013;41(3):198–211. http://doi.org/10.1080/01926187.2012.677662. [Google Scholar]
- Shonkoff JP, Garner AS, Siegel BS, Dobbins MI, Earls MF, Garner AS, et al. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2011;129(1):e232–e246. doi: 10.1542/peds.2011-2663. http://doi.org/10.1542/peds.2011-2663. [DOI] [PubMed] [Google Scholar]
- Stuebe AM, Grewen K, Pedersen CA, Propper C, Meltzer-Brody S. Failed lactation and perinatal depression: Common problems with shared neuroendocrine mechanisms? Journal of Women’s Health. 2012;21(3):264–272. doi: 10.1089/jwh.2011.3083. http://doi.org/10.1089/jwh.2011.3083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Administration (SAMHSA) Trauma-informed approach and trauma-specific interventions. n.d Retrieved from http://www.samhsa.gov/nctic/trauma-interventions.
- US Department of Health and Human Services, & Office of Disease Prevention and Health Promotion. Healthy People 2020. 2010 Retrieved from https://www.healthypeople.gov/2020/topics-objectives/topic/maternal-infant-and-child625health/objectives.
- Victora CG, Bahl R, Barros AJ, França GV, Horton S, Krasevec J … Group TLBS. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. The Lancet. 2016;387(10017):475–490. doi: 10.1016/S0140-6736(15)01024-7. [DOI] [PubMed] [Google Scholar]
- Waller N, Putnam FW, Carlson EB. Types of dissociation and dissociative types: A taxometric analysis of dissociative experiences. Psychological Methods. 1996;1(3):300–321. doi: 10.1037/1082-989X.1.3.300. [DOI] [Google Scholar]
- Watkins S, Meltzer-Brody S, Zolnoun D, Stuebe A. Early breastfeeding experiences and postpartum depression. Obstetrics & Gynecology. 2011;118(2 Pt 1):214–221. doi: 10.1097/AOG.0b013e3182260a2d. http://doi.org/10.1097/AOG.0b013e3182260a2d. [DOI] [PubMed] [Google Scholar]
- Wittchen HU. Reliability and validity studies of the WHO-Composite International Diagnostic Interview (CIDI): a critical review. Journal of Psychiatric Research. 1994;28(1):57–84. doi: 10.1016/0022-3956(94)90036-1. [DOI] [PubMed] [Google Scholar]
- Wolfe J, Kimerling R. Gender issues in the assessment of posttraumatic stress disorder. In: Wilson JP, Keane TM, editors. Assessing Psychological Trauma and PTSD. New York: Guilford Press; 1997. [Google Scholar]
- World Health Organization. Global strategy for infant and young child feeding. WHO; Geneva: 2003. pp. 1–30. Retrieved from http://www.who.int/nutrition/publications/gs_infant_feeding_text_eng.pdf. [Google Scholar]
- Ystrom E. Breastfeeding cessation and symptoms of anxiety and depression: a longitudinal cohort study. BMC Pregnancy and Childbirth. 2012;12(1):36. doi: 10.1186/1471-2393-12-36. http://doi.org/10.1186/1471-2393-12-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanardo V, Gambina I, Begley C, Litta P, Cosmi E, Giustardi A, Trevisanuto D. Psychological distress and early lactation performance in mothers of late preterm infants. Early Human Development. 2011;87(4):321–323. doi: 10.1016/j.earlhumdev.2011.01.035. http://doi.org/10.1016/j.earlhumdev.2011.01.035. [DOI] [PubMed] [Google Scholar]