DYT1 early-onset primary dystonia (DYT1) is a well-described dystonia caused by an in-frame GAG nucleotide deletion in the TOR1A gene, c.907_909delGAG.1 The only phenotype linked to TOR1A is dystonia.2 Homozygous GAG deletions or compound heterozygosity for mutations in TOR1A have never been reported in humans.
Arthrogryposis, defined as multiple congenital contractures, affects 1 in 3,000–5,000 births.3 The underlying etiology for arthrogryposis is broad, and includes neurologic disease, maternal illness, myopathic processes, among many others.3 The number of genetic factors causing arthrogryposis is vast, with over 150 genes currently identified.3
We report an infant with a severe congenital phenotype characterized by arthrogryposis, respiratory failure, and feeding difficulties found to have biallelic mutations in TOR1A identified by whole-exome sequencing (WES).
Case.
The proband was born at 37 weeks to his 24-year-old G2P1001 mother via cesarean section. He weighed 2,150 g (2%), he was 44 cm long (2%), his head circumference was 32 cm (12%), and he had APGAR scores of 5 and 7 at 1 and 5 minutes, respectively. The pregnancy was complicated by intrauterine growth restriction, reduced fetal movements, and arthrogryposis. Invasive prenatal genetic testing was declined, and no teratogenic exposures or maternal illnesses were reported. Following delivery, examination was notable for contractures in all extremities and skeletal anomalies, including bilateral hip dislocations, bilateral clubfeet, 11 sets of ribs, and scoliosis (figure). He developed restrictive lung disease requiring tracheostomy with ventilator support, and a G-tube was placed for swallowing discoordination. Brain MRI at 3 weeks of age was unremarkable (figure). He is currently 7 months old and has no spontaneous or involuntary movements, although he responds to voices and makes eye contact.
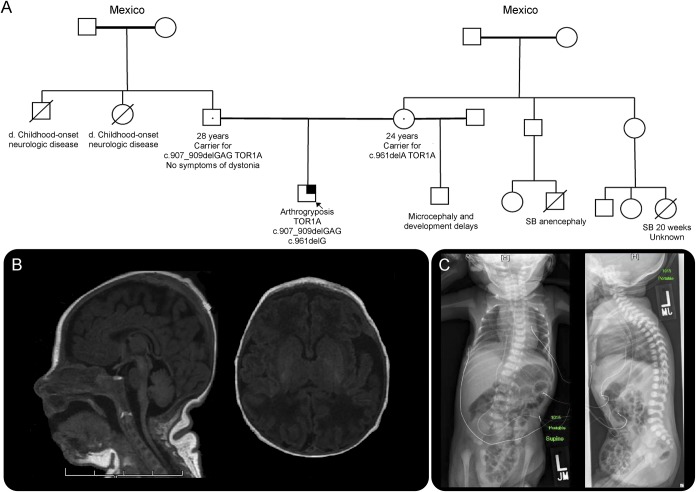
Figure. Family history and clinical imaging of the proband.
(A) Pedigree—the proband is the first child born to his parents and is designated by the arrow. The family history is unremarkable for symptoms of arthrogryposis or DYT1 dystonia; however, there is a paternal aunt and uncle who died of an unknown childhood onset neurologic disease. (B) Brain MRI was performed at 3 weeks of age. Sagittal view of the cerebellum and axial view of the caudate are unremarkable for the proband's age. (C) Chest and abdomen X-rays taken at birth show multiple skeletal anomalies including 11 pairs of ribs, bilateral hip dislocations, and scoliosis.
There is no extended family history of arthrogryposis or dystonia; however, a paternal aunt and uncle died during childhood from a nonspecific neurologic condition (figure). He has a maternal half-sibling with microcephaly and developmental delays who has no contractures. The family has declined genetic evaluation for this sibling.
Genetic workup included karyotype and chromosomal microarray, testing for congenital myasthenia gravis, distal arthrogryposis, spinal muscular atrophy, and spinal muscular atrophy with respiratory disease—all unremarkable. WES, using the proband and his parents, was reported negative for characterized genetic etiologies relating to known genes and phenotypes. However, 2 TOR1A variations—the known c.907_909delGAG (p.E303del) mutation (paternally inherited) and a c.961delA (p.T321Rfs*6) variant (maternally inherited)—were listed as suspected candidates for a potential novel genetic etiology. These findings refer to a gene-disease relationship and/or mechanism not previously proposed or with limited evidence.
Discussion.
In DYT1, one-third of carriers of the common mutation develop dystonia during childhood or adolescence with previously normal development.2 The factors that determine penetrance remain largely unknown. In affected individuals, brain imaging studies are normal.
The protein coded by TOR1A, torsinA, contains 332 amino acids and is widely expressed in the endoplasmic reticulum and is thought to function as an adenosine triphosphate–regulated chaperone in the secretory pathway and the nuclear envelope.1 Overall, published research supports that DYT1 is caused by the loss of torsinA function, likely due to a dominant negative effect of the mutant torsinA over the wild-type protein.4 Animal models of DYT1 have been developed and demonstrate that torsinA is essential for postnatal life, as TOR1A−/−, homozygous TOR1AΔGAG/ΔGAG, and TOR1A−/ΔGAG mice die within 48 hours of birth.5 Of interest, the animal models described above appear normal at birth except for a smaller size than their littermates, however, do not feed or generate sounds, suggesting oropharyngeal dysfunction. Gross neuroanatomy is normal, but they have ultrastructural defects in neurons. Mice with restricted conditional deletion of torsinA exhibit longer survival.6
Our proband exhibits several features seen in animal models, including oropharyngeal dysfunction and delayed growth with no gross neuroanatomical defects appreciated by MRI. The c.907_909delGAG mutation is causative of DYT1. The c.961delA variant has not been previously associated with disease, but is expected to result in a translational frameshift at the 3′ terminus, deleting the last 12 amino acids of the typical protein. This would abolish a highly conserved essential domain, the sensor-II domain, likely resulting in a protein with reduced function.7 To demonstrate pathogenicity, identification of more patients or robust biological evidence is required. Nevertheless, given our current knowledge, it is reasonable to speculate that these compound heterozygous deleterious mutations result in the severe congenital phenotype observed.
This represents a rare case of TOR1A compound heterozygous mutations in a patient with congenital arthrogryposis. This information is valuable for researchers investigating biological bases of DYT1. Moreover, TOR1A mutations should be considered as a potential genetic cause in the evaluation of arthrogryposis.
Footnotes
Author contributions: Ms. Reichert contributed to report concept, acquisition of data, analysis and interpretation, and critical revision of the manuscript for important intellectual content. Dr. Gonzelez-Alegre contributed to analysis and interpretation and critical revision of the manuscript for important intellectual content. Dr. Scharer contributed to acquisition of data, analysis and interpretation, and critical revision of the manuscript for important intellectual content.
Study funding: No targeted funding reported.
Disclosure: Ms. Reichert reports no disclosures. Dr. Gonzalez-Alegre has received compensation from TEVA for participation in the Huntington's Disease Advisory Board. Dr. Scharer reports no disclosures. Go to Neurology.org/ng for full disclosure forms. The Article Processing Charge was funded by the authors.
References
- 1.Ozelius LJ, Hewett JW, Page CE, et al. The early-onset torsion dystonia gene (DYT1) encodes an ATP-binding protein. Nat Genet 1997;17:40–48. [DOI] [PubMed] [Google Scholar]
- 2.Bressman SB, Sabatti C, Raymond D, et al. The DYT1 phenotype and guidelines for diagnostic testing. Neurology 2000;54:1746–1752. [DOI] [PubMed] [Google Scholar]
- 3.Hall JG. Arthrogryposis (multiple congenital contractures): diagnostic approach to etiology, classification, genetics, and general principles. Eur J Med Genet 2014;57:464–472. [DOI] [PubMed] [Google Scholar]
- 4.Torres GE, Sweeney AL, Beaulieu JM, Shashidharan P, Caron MG. Effect of torsinA on membrane proteins reveals a loss of function and a dominant-negative phenotype of the dystonia-associated DeltaE-torsinA mutant. Proc Natl Acad Sci USA 2004;101:15650–15655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goodchild RE, Kim CE, Dauer WT. Loss of the dystonia-associated protein torsinA selectively disrupts the neuronal nuclear envelope. Neuron 2005;48:923–932. [DOI] [PubMed] [Google Scholar]
- 6.Liang CC, Tanabe LM, Jou S, Chi F, Dauer WT. TorsinA hypofunction causes abnormal twisting movements and sensorimotor circuit neurodegeneration. J Clin Invest 2014;124:3080–3092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhu L, Wrabl JO, Hayashi AP, Rose LS, Thomas PJ. The torsin-family AAA+ protein OOC-5 contains a critical disulfide adjacent to Sensor-II that couples redox state to nucleotide binding. Mol Biol Cel 2008;19:3599–3612. [DOI] [PMC free article] [PubMed] [Google Scholar]