Abstract
Introduction
Spice is a synthetic cannabinoid that is readily available for purchase in smoke shops at relatively low cost. Spice is not detectable upon routine drug screening, making it an increasingly popular new street drug.
Case Report
A 21-year-old man presented with new-onset seizures. During the next 2 days, he developed uncontrollable hypertension, agitation, respiratory failure requiring intubation, pulmonary hypertension, and acute kidney injury (AKI) with a maximum blood urea nitrogen/creatinine level of 54/7.90 mg/dL. A complete renal workup was negative, but his urine sediment revealed granular casts. A discussion with family and friends revealed that this patient had smoked Spice during the last month. His renal function started to improve with supportive therapy, and his AKI resolved by the time of discharge without renal replacement therapy.
Discussion
Spice differs from marijuana because it is a cannabinoid receptor type 1 and 2 agonist. The pathologic mechanism of AKI remains unclear, but the condition likely is attributable to acute tubular necrosis or acute interstitial nephritis, as proven by biopsies performed in previous case series. It is important to raise awareness that a new Spice strain that may be circulating in the Southern California Inland Empire can endanger young users who may develop seizures, respiratory failure, and AKI.
INTRODUCTION
Spice, a synthetic cannabinoid, is an increasingly popular new street drug1 that often is perceived as harmless by young adults because it is easily accessible and sold in smoke shops, convenience stores, and online as an “herbal blend,” “incense,” or “air freshener.”2 Spice also is a popular drug because it is not detectable on conventional urine drug screens. A 2012 study revealed that 11% of high school seniors admitted to Spice use during the previous 12 months.1 The first case of acute kidney injury (AKI) related to synthetic cannabinoid use was described in 2012 even though synthetic cannabinoids have been on the market since the 2000s.3 A new Spice metabolite, likely introduced in 2012, is associated with AKI.3
CASE REPORT
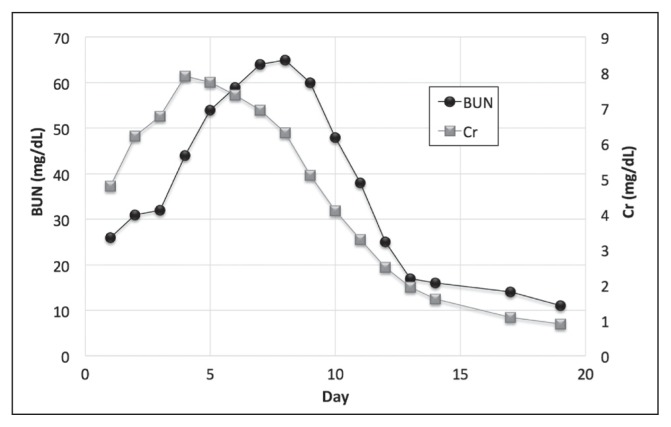
A 21-year-old man with an uneventful medical history with the exception of childhood asthma presented with new-onset seizures. His initial physical examination findings were unremarkable. His laboratory studies revealed acute renal failure and blood urea nitrogen/creatinine levels of 26/4.79 mg/dL (Reference range: ≤ 18 mg/dL/≤ 1.30 mg/dL). His lactic acid level was within defined limits, his fractional excretion of sodium level was 3.2%, and his fractional excretion of urea was 74.3%. His urine drug screen was positive for benzodiazepines (which he received for seizure control in the ambulance after his first seizure) and tetrahydrocannabinol. Amphetamines, cocaine, and phencyclidine screenings were negative, and head computed tomography scan and chest x-ray findings were unremarkable. The patient admitted to daily recreational marijuana use. During the next 2 days, he developed uncontrolled hypertension and agitation and his renal function continued to worsen. By the third hospital day, he was intubated for respiratory failure. His acute renal failure worsened, reaching peak blood urea nitrogen and serum creatinine levels of 54 mg/dL and 7.90 mg/dL, respectively, on the fifth hospital day. Figure 1 depicts blood urea nitrogen/creatinine levels throughout his hospital stay. His urine output, which was between 750 mL and 1645 mL during the first 7 days (Reference range: > 500mL/24h), continued to increase in tandem with his serum creatinine level until he reached a maximum daily urine output of 6000 mL at the end of his hospital stay. A renal workup that included testing for antineutrophil cytoplasmic antibodies, antinuclear antibodies, double-stranded DNA, anti-Smith antibodies, antiglomerular basement membrane antibodies, human immunodeficiency virus, and hepatitis and a renal ultrasound revealed negative findings. His creatinine kinase level was elevated with a maximum value of 1163 U/L (reference range: ≤ 398 U/L). His urine sediment revealed granular casts; however, urine eosinophils were absent.
Figure 1.
Graphic depiction of the patient’s BUN and Cr values during his hospital stay. Note his maximum BUN of 65 mg/dL on day 8, and maximum Cr of 7.9 mg/dL on day 4. At his 1-month follow-up appointment his BUN was 6 mg/dL and his Cr was 0.84 mg/dL.
BUN = blood urea nitrogen; Cr = creatinine.
Further interviewing of family and friends revealed that this patient had smoked Spice during the previous month and on the day of admission. We obtained this information on hospital day 5, and his urine was sent for a synthetic cannabinoid panel; an XLR-11 level was ordered on hospital day 7. Both tests revealed negative findings. After the fifth hospital day, the patient’s renal function began to improve with supportive therapy and his AKI resolved by the time of discharge. The patient remained intubated until his tenth hospital day. Because he became tachycardic and hemodynamically unstable whenever he was moved; he was too unstable to undergo renal biopsy. By the time of extubation on hospital day 10, his renal function was recovering well and risks associated with renal biopsy at this juncture outweighed potential benefits. At no point was he oliguric, and he did not require renal replacement therapy.
DISCUSSION
Synthetic cannabis initially was invented in an effort to research the pharmacology of cannabinoid receptors.2 Its pharmacology differs from traditional marijuana in that traditional marijuana’s Δ9-tetrahydrocannabinol is a partial agonist of cannabinoid receptors, whereas Spice is a cannabinoid receptor types 1 and 2 full agonist in both cellular assays and animal studies.4 Because Spice does not have the same chemical makeup as marijuana, people who use it will have a negative urine tetrahydrocannabinol drug screen finding, making it an attractive drug for anyone subject to drug testing. These drugs initially were distributed in 2009,5 but the first AKI cases were not reported until 2012.3
There are several theories behind the pathologic mechanism of AKI via Spice consumption. Our patient was a young healthy man with adequate oral intake who appeared euvolemic upon examination, so prerenal causes were unlikely. Upon admission, his fractional excretion of sodium was 3.2% and his fractional excretion of urea was 74.3%, which is in accordance with intrinsic renal failure. There were no urine eosinophils and this patient was not taking any medications, making acute interstitial nephritis unlikely. His creatinine kinase levels were too low at 1163 U/L to cause AKI from rhabdomyolysis. Renal ultrasound findings were negative for postrenal obstruction; however, his urine sediment revealed granular casts, making acute tubular necrosis a possible mechanism leading to Spice-induced AKI. It is possible that an unidentified byproduct in new Spice batches can cause acute tubular necrosis. Similar mechanisms were hypothesized in previous case reports.6 Table 1 summarizes previously reported cases and their respective urine microscopy and renal biopsy findings and the suspected mechanism of injury. Acute tubular necrosis is the most commonly observed mechanism of injury; however, acute interstitial nephritis also has been observed.3,6–10 One case involved hyperemesis induced by Spice that led to rhabdomyolysis. In this case, rhabdomyolysis was the suspected cause of AKI.11 Interestingly, some patients had calcium oxalate crystals upon renal biopsy. Calcium oxalate can be a Spice byproduct or it may be a nonspecific finding.6 Only 2 renal biopsies have revealed calcium oxalate crystals thus far.6
Table 1.
Reported cases of Spice-induced acute kidney failure (urine microscopy findings, renal biopsy findings, suspected mechanism of injury, and need for renal replacement therapy)
| Author, year | Age | Sex | Peak creatinine level (mg/dL) | Urine microscopy | Renal biopsy | Suspected mechanism of AKI | Need for RRT |
|---|---|---|---|---|---|---|---|
| Present case | 21 | M | 7.9 | Granular casts | — | ATN | No |
| Srisung et al, 20151 | 31 | M | 3.0 | — | — | Intrinsic AKI | No |
| 32 | M | 5.7 | — | — | ATN | Yes | |
| 31 | M | 3.5 | — | — | AIN with eosinophiluria and ATN | No | |
| Bhanushali et al, 20132 | 20 | M | 13.7 | 3+ protein; trace glucose; 6/10 WBC/HPF; occasional muddy brown casts | ATN (tubular dilation, tubular epithelial cell vacuolization, sloughing, and apical blebbing); rare calcium oxalate crystals | ATN | No |
| 23 | M | 15.2 | 2+ protein; 25 RBC/HPF; occasional granular casts | Mild ATN; few calcium oxalate crystals | ATN | No | |
| 26 | M | 13.3 | 3+ protein; 26–50 WBC/HPF; > 25 RBC/HPF; 3+ leukocyte esterase | ATN | ATN | No | |
| 30 | M | 3.2 | Normal | — | ATN suspected | No | |
| Buser et al, 20143 | 17 | M | 10.2 | WBCs; RBCs; trace protein; 1+ eosinophils | ATN with mild interstitial nephritis | ATN and AIN | No |
| 15 | M | 7.8 | Trace protein | ATN (vacuolization of proximal tubular epithelial cells) with medullary peritubular capillaritis | ATN | Yes | |
| Kazory & Aiyer, 20134 | 22 | M | 9.3 | Proteinuria; WBCs; RBCs; trace ketones; trace hemoglobin | ATN (focal tubular atrophy and flattened epithelium, loss of brush border, casts, vacuolization, and mitosis) | ATN | No |
| Thornton et al, 20135 | 26 | M | 7.7 | 1+ protein; trace blood | — | — | No |
| Ergül et al, 20156 | 27 | M | 5.6 | — | — | — | Yes |
| 24 | M | 4.4 | — | — | — | Yes | |
| 21 | M | 2.9 | — | — | — | No | |
| Gudsoorkar & Perez, 20157 | 26 | M | 8.1 | 200 RBC/HPF initially; 5 RBC/HPF the next day; 1+ proteinuria; no WBCs | — | Intrinsic AKI | Yes |
| Argamany et al, 20168 | 27 | M | 13.9 | 2+ protein; 3+ blood | — | Rhabdomyolysis attributable to hyperemesis | No |
| Sherpa et al, 20159 | 45 | M | 3.1 | — | — | — | No |
| Sinangail et al, 201610 | 42 | M | 4.3 | + glucose; otherwise normal | Diffuse inflammatory infiltrates with lymphocytic predominance affecting the cortex of the renal tubules and the interstitium with associated tubulitis | ATN and acute tubulointerstitial nephritis | |
| Centers for Disease Control and Prevention, 201211 | 19 | M | 5.2 | WBCs; RBCs; RBC/granular casts | 8 biopsies performed; 6 revealed ATN and 3 revealed AIN | — | 5 of 16 patients required RRT |
| 15 | M | 6.8 | WBCs; RBCs; RBC/granular casts; eosinophils | — | |||
| 21 | M | 6.3 | WBCs; RBCs; epithelial casts; granular casts | — | |||
| 18 | M | 4.1 | Hyaline casts; WBCs | — | |||
| 25 | M | 21.0 | RBCs; proteinuria; eosinophils | — | |||
| 30 | M | 9.0 | WBCs; RBCs; RBC/hyaline casts | — | |||
| 18 | M | 6.6 | WBCs; protein 30 | — | |||
| 33 | M | 3.3 | — | — | |||
| 27 | M | 4.7 | Small blood; protein 30 | — | |||
| 15 | M | 9.1 | Protein trace | — | |||
| 26 | M | 7.7 | Normal | — | |||
| 17 | M | 10.6 | WBCs; RBCs; protein 2+; eosinophils 1+ | — | |||
| 18 | M | 9.6 | Protein 2+; blood 3+; no RBCs | — | |||
| 18 | M | 5.5 | Protein 1+ | — | |||
| 15 | M | 11.5 | WBCs; RBCs | — | |||
| 15 | M | 6.2 | WBCs; protein 1+ | — |
— = Not reported; AIN = acute interstitial nephritis; AKI = acute kidney injury; ATN = acute tubular necrosis; HPF = high-power field; M = male; RBC = red blood cell; RRT = renal replacement therapy; WBC = white blood cell.
Srisung W, Jamal F, Prabhakar S. Synthetic cannabinoids and acute kidney injury. Proc (Bayl Univ Med Cent) 2015 Oct;28(4):475–7.
Bhanushali GK, Jain G, Fatima H, Leisch LJ, Thornley-Brown D. AKI associated with synthetic cannabinoids: A case series. Clin J Am Soc Nephrol 2013 Apr;8(4):523–6. DOI: https://doi.org/10.2215/cjn.05690612.
Buser GL, Gerona RR, Horowitz BZ, et al. Acute kidney injury associated with smoking synthetic cannabinoid. Clin Toxicol (Phila) 2014 Aug;52(7):664–73. DOI: https://doi.org/10.3109/15563650.2014.932365.
Kazory A, Aiyer R. Synthetic marijuana and acute kidney injury: An unforeseen association. Clin Kidney J 2013 Jun;6(3):330–3. DOI: https://doi.org/10.1093/ckj/sft047.
Thornton SL, Wood C, Friesen MW, Gerona RR. Synthetic cannabinoid use associated with acute kidney injury. Clin Toxicol (Phila) 2013 Mar;51(3):189–90. DOI: https://doi.org/10.3109/15563650.2013.770870.
Ergül DF, Ekemen S, Yelken BB. Synthetic cannabinoid ‘bonzai’ intoxication: Six case series. Turk J Anaesthesiol Reanim 2015 Oct;43(5):347–51. DOI: https://doi.org/10.5152/tjar.2015.05668.
Gudsoorkar VS, Perez JA Jr. A new differential diagnosis: Synthetic cannabinoids-associated acute renal failure. Methodist Debakey Cardiovasc J 2015 Jul–Sep;11(3):189–91. DOI: https://doi.org/10.14797/mdcj-11-3-189.
Argamany JR, Reveles KR, Duhon B. Synthetic cannabinoid hyperemesis resulting in rhabdomyolysis and acute renal failure. Am J Emerg Med 2016 Apr;34(4):765.e1–2. DOI: https://doi.org/10.1016/j.ajem.2015.08.051.
Sherpa D, Paudel BM, Subedi BH, Chow RD. Synthetic cannabinoids: The multi-organ failure and metabolic derangements associated with getting high. J Community Hosp Intern Med Perspect 2015 SEP 1;5(4):27540. DOI: https://doi.org/10.3402/jchimp.v5.27540.
Sinangail A, Celik V, Kockar A, Ecder T. Synthetic cannabinoid induced acute tubulointerstitial nephritis and uveitis syndrome: A case report and review of literature. J Clin Diagn Res 2016 May;10(5):OD31–2. DOI: https://doi.org/10.7860/jcdr/2016/18762.7826.
Centers for Disease Control and Prevention (CDC). Acute kidney injury associated with synthetic cannabinoid use—multiple states, 2012. MMWR Morb Mortal Wkly Rep 2013 Feb 15;62(6):93–8.
Among the 35 case reports available, 10 patients required renal replacement therapy, and renal function recovered for all patients. Only one case report included commentary on the timeline of Spice ingestion and development of renal failure. In these cases, admission for renal failure occurred within 12 to 48 hours after last Spice use, as was the case with our patient.8 No cases were followed for long enough to assess the development of chronic kidney disease years after AKI recovery.
Metabolites composing Spice are constantly changing. The present case indicates that the most recent batches of Spice are likely more toxic than previous batches. To date, the synthetic cannabinoid metabolites XLR-11, AM-2201, and UR-144 have been isolated in patients with Spice-induced AKI. Distributors assign appealing names to different batches of Spice such as “Phantom Wicked Dreams,” “Mr Happy,” “Clown Loyal,” “Lava,” and “Flame 2.0.”3 It is unclear whether these metabolites have a nephrotoxic effect. One proposed mechanism is that these metabolites are directly nephrotoxic because they bind cannabinoid 2 receptors in the kidneys.7 Few autopsy reports have been published on fatal incidences of Spice abuse. A case series on 4 fatal cases, in which one patient had a history of AKI 12 hours before death, isolated the metabolite 5F-PB-22.12 However, testing of these metabolites is difficult. It took our local laboratory several days to identify a laboratory that could test our patient’s urine for XLR-11 and previously identified metabolites. On hospital day 7, we were able to send the patient’s urine for a synthetic cannabis panel and results were negative. This result likely was attributable to the 7-day delay in collecting and sending out the specimen and the frequently changing metabolites that are created to make Spice, which are not part of the previously created panels. A full history was not available because of our patient’s altered mental status and tests were unavailable, so we could not detect the AKI cause sooner.
Clinicians need to know that a new strain of Spice may be circulating in the Southern California Inland Empire; this strain can cause young users to develop seizures, respiratory failure, and AKI. In 2016, several news reports on the Los Angeles Skid Row homeless population highlighted the need for hospitalization for this population, which is experiencing seizures and acute loss of consciousness as a result of using new, strong Spice batches. Medical reports on these incidences that include more information about these patients’ health status and renal function have not been released, however.13–15 Spice abuse is an ongoing issue that has affected many people in the US, especially in Southern California. As a result, it is important to educate physicians about Spice’s side effects and popularity so they may include the drug in their differential when examining otherwise healthy patients who are experiencing acute renal or respiratory failure and/or new-onset seizures.
Acknowledgment
Brenda Moss Feinberg, ELS, provided editorial assistance.
Footnotes
Disclosure Statement
The author(s) have no conflicts of interest to disclose.
References
- 1.Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. 2012 overview: Key findings on adolescent drug use. Ann Arbor, MI: Institute for Social Reseach, The University of Michigan; 2013. Monitoring the future: National survey results on drug use 1975–2012. [Google Scholar]
- 2.Seely KA, Lapoint J, Moran JH, Fattore L. Spice drugs are more than harmless herbal blends: A review of the pharmacology and toxicology of synthetic cannabinoids. Prog Neuropsychopharmacol Biol Psychiatry. 2012 Dec 3;39(2):234–43. doi: 10.1016/j.pnpbp.2012.04.017. DOI: https://doi.org/10.1016/j.pnpbp.2012.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention (CDC) Acute kidney injury associated with synthetic cannabinoid use—multiple states, 2012. MMWR Morb Mortal Wkly Rep. 2013 Feb 15;62(6):93–8. [PMC free article] [PubMed] [Google Scholar]
- 4.Fantegrossi WE, Moran JH, Radominska-Pandya A, Prather PL. Distinct pharmacology and metabolism of K2 synthetic cannabinoids compared to Δ(9)-THC: Mechanism underlying greater toxicity? Life Sci. 2014 Feb 27;97(1):45–54. doi: 10.1016/j.lfs.2013.09.017. DOI: https://doi.org/10.1016/j.lfs.2013.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.US Department of Justice, Drug Enforcement Administration, Office of Diversion Control. Special report: Synthetic cannabinoids and synthetic cathinones reported in NFLIS, 2009–2010. Springfield, VA: US Drug Enforcement Administration, National Forensic Laboratory Information System; 2011. [Google Scholar]
- 6.Bhanushali GK, Jain G, Fatima H, Leisch LJ, Thornley-Brown D. AKI associated with synthetic cannabinoids: A case series. Clin J Am Soc Nephrol. 2013 Apr;8(4):523–6. doi: 10.2215/CJN.05690612. DOI: https://doi.org/10.2215/cjn.05690612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Buser GL, Gerona RR, Horowitz BZ, et al. Acute kidney injury associated with smoking synthetic cannabinoid. Clin Toxicol (Phila) 2014 Aug;52(7):664–73. doi: 10.3109/15563650.2014.932365. DOI: https://doi.org/10.3109/15563650.2014.932365. [DOI] [PubMed] [Google Scholar]
- 8.Srisung W, Jamal F, Prabhakar S. Synthetic cannabinoids and acute kidney injury. Proc (Bayl Univ Med Cent) 2015 Oct;28(4):475–7. doi: 10.1080/08998280.2015.11929313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kazory A, Aiyer R. Synthetic marijuana and acute kidney injury: An unforeseen association. Clin Kidney J. 2013 Jun;6(3):330–3. doi: 10.1093/ckj/sft047. DOI: https://doi.org/10.1093/ckj/sft047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sinangail A, Celik V, Kockar A, Ecder T. Synthetic cannabinoid induced acute tubulointerstitial nephritis and uveitis syndrome: A case report and review of literature. J Clin Diagn Res. 2016 May;10(5):OD31–2. doi: 10.7860/JCDR/2016/18762.7826. DOI: https://doi.org/10.7860/jcdr/2016/18762.7826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Argamany JR, Reveles KR, Duhon B. Synthetic cannabinoid hyperemesis resulting in rhabdomyolysis and acute renal failure. Am J Emerg Med. 2016 Apr;34(4):765.e1–2. doi: 10.1016/j.ajem.2015.08.051. DOI: https://doi.org/10.1016/j.ajem.2015.08.051. [DOI] [PubMed] [Google Scholar]
- 12.Behonick G, Shanks KG, Firchau DJ, et al. Four postmortem case reports with quantitative detection of the synthetic cannabinoid, 5F-PB-22. J Anal Toxicol. 2014 Oct;38(8):559–62. doi: 10.1093/jat/bku048. DOI: https://doi.org/10.1093/jat/bku048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mohney G. Synthetic marijuana suspected in mass LA overdose [Internet] New York, NY: ABC News Network; 2016. Aug 23, [cited 2016 Dec 4]. Available from: http://abcnews.go.com/Health/synthetic-marijuana-suspected-mass-la-overdose/story?id=41589561. [Google Scholar]
- 14.Pamer M. Synthetic marijuana creating ‘public health crisis’ in skid row: LAFD medical director [Internet] Los Angeles, CA: KTLA5; 2016. Aug 22, [cited 2016 Dec 4]. Available from: http://ktla.com/2016/08/22/lafd-again-responds-to-skid-row-for-multipatient-incident-likely-involving-illicit-substance/ [Google Scholar]
- 15.Karlamangla S. ‘The cheapest buzz you can get on skid row’: Officials try to stop homeless from smoking Spice after dozens sickened [Internet] Los Angeles, CA: Los Angeles Times; 2016. Aug 25, [cited 2016 Dec 5]. Available from: www.latimes.com/local/lanow/la-me-spice-skid-row-20160824-snap-story.html. [Google Scholar]