Abstract
Lawrence Weed, MD, is renowned for being the father of the Problem-Oriented Medical Record (POMR), the medical care standard for collecting, managing, and contextualizing patient data in medical records. What have been consistently overlooked are his teachings on knowledge coupling, which refers to matching patient data with associated medical knowledge. Together, the POMR standard and knowledge coupling are meant to form the basis of a systems approach that enables individualized evidence-based decision making within the context of multimorbidity and patient complexity.
The POMR and knowledge coupling tools operationalize a problem-oriented model that reflects a sophisticated general systems theoretical approach to knowledge. This paradigm transcends reductionist approaches to knowledge by depicting how the meaning of specific entities (eg, disease constructs) and their associated probabilities can only be understood within their respective spatiotemporal and biopsychosocial relational contexts. Rigorous POMRs therefore require knowledge inputs from a network of interconnections among specific entities, which Dr Weed enabled through development of the Knowledge Net standard. The Knowledge Net’s relational structure determines the applicability of knowledge within specific patient contexts. To enable the linkage of unique combinations of data in individual patient POMRs with existing medical knowledge structured in Knowledge Nets, Dr Weed developed the Knowledge Coupling standard.
Dr Weed’s standards for record keeping and knowledge coupling form the basis of a combinatorial approach to evidence-based medicine that fulfills Stange’s call for a science of connectedness. Ensuing individualized processes of care become the dynamo powering a learning health care system that enables a co-construction of health premised on empowerment and intelligent human decision making, rather than promoting the artificial intelligence of tools. If the value of Engel’s biopsychosocial model indeed relates to “guiding the parsimonious application of medical knowledge to the needs of each patient,” Dr Weed’s approach warrants serious consideration.
OPERATIONALIZING A SYSTEMS APPROACH TO PATIENT COMPLEXITY
The problem of providing evidence-based patient-centered care within the context of multimorbidity and complexity is not new. In a 1968 New England Journal of Medicine article entitled “Medical records that guide and teach,”1 Lawrence Weed, MD, presented a “workable philosophy of multiple problems,” articulated by a “clear approach and practical techniques for coping with the infinite multiplicity of interrelated and continuously changing problems that patients inevitably present.” His sophisticated approach was underpinned by a simple solution: orienting and contextualizing data around the reality of patient problems through the use of the Problem-Oriented Medical Record (POMR).1,2 However, he quickly concluded that the POMR was incomplete because it depended on idiosyncratic, uncontrolled inputs from the unaided minds of physicians.3 That led him to develop the Knowledge Coupling and Knowledge Net tools to enable the linkage of unique combinations of data in individual patient POMRs with existing medical knowledge.4,5
Unlike contemporary probabilistic or algorithmic approaches to evidence-based medicine, Weed’s concepts are premised on a general systems theoretical approach to knowledge, positing that relationships between scientific entities are fundamentally more important than the entities in and of themselves.4 Dr Weed recognized that different combinations of findings on a patient may point in very different directions, and that specific relationships may be relevant in relation to different (otherwise unrelated) problems.4 Like Valderas, Starfield, et al, he recognized that the meaning of specific entities (eg, disease constructs) and their associated probabilities can only be understood within their respective spatiotemporal and biopsychosocial relational contexts.6 Within this paradigm, knowledge is conceived as a network of interconnections for specific entities, which determine their applicability within different clinical situations (ie, a patient’s unique multimorbidity and complexity profile).4
Ingeniously, the POMR and knowledge coupling tools operationalize a problem-oriented epidemiologic model that structures the unique combinations of individual patient variables in ways that enable the creation of a Knowledge Net database of knowledge (consisting of and manifesting the aforementioned networks of interconnections).1,4,7 Dr Weed envisioned that processes of patient care (ie, structured by systematic use of the POMR) would ultimately become an object of clinical research and a source of new medical knowledge. New knowledge would be integrated with existing knowledge from the medical literature in the Knowledge Net repository. He defined the Knowledge Net as “an organized collection of the entities (objects) of medical knowledge and the relationships among them, with commentary on the relationships.”8
Dr Weed recognized that the validity of Knowledge Nets is contingent on whether processes of care are evidence-based. In other words, medical decisions should be premised on the systematic linkage of individual patient data with medical knowledge. Because the human mind cannot make this linkage with the necessary reliability and speed, Dr Weed developed scientific standards and corresponding tools (Knowledge Couplers) to perform the linkage function. Knowledge Couplers, in turn, are constructed from the Knowledge Net. The output from using Knowledge Couplers is exported to the patient’s POMR.4,7,8
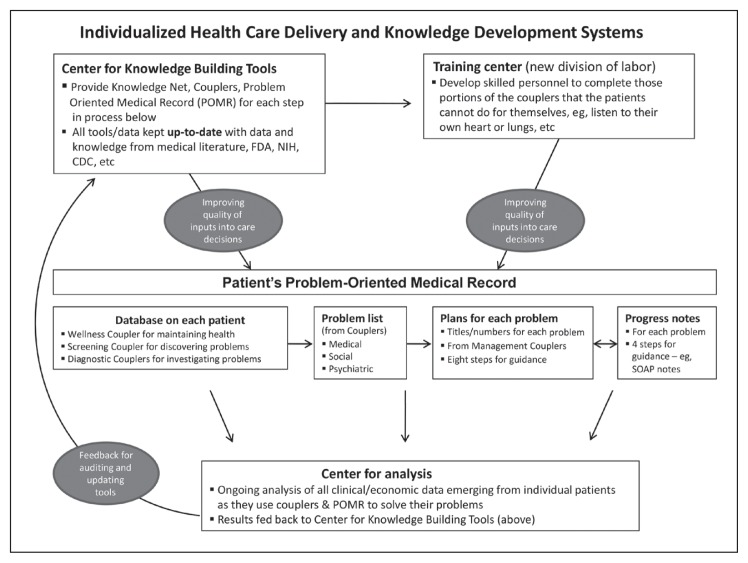
Together, the POMR standard, Knowledge Net, and Knowledge Coupling tools form the basis of Dr Weed’s vision of a learning health system that coherently integrates patient care, research, and medical education (Figure 1).4,8
Figure 1.
Lawrence Weed, MD’s learning health care system. Reprinted with kind permission from Lawrence Weed, MD: Weed LL, Weed L. Medicine in denial. Seattle, WA: CreateSpace; 2011.
CDC = Centers for Disease Control and Prevention; FDA = Food and Drug Administration; NIH = National Institutes of Health; SOAP = Symptomatic findings, other findings, assessment, and plan.4p168
THE KNOWLEDGE NET: PHILOSOPHY, STRUCTURE, AND FUNCTION
Because medical records are not generally maintained in a rigorous manner conforming to POMR standards, the Knowledge Net was primarily constructed using medical knowledge derived from the array of published scientific sources available (eg, population-based studies, pathophysiologic knowledge, consensus reports, clinical guidelines, etc).4,7,9 Regardless of its data source, the structure of the Knowledge Net operationalizes Dewey’s relational philosophy of knowledge, which posits that relationships between entities are fundamentally more important than entities in and of themselves.4,10
Dr Weed explained that “complexity is derived not from an infinite number of chemical and biological entities, but rather from an extremely large number of relationships among the entities. Relationships may be of different types (eg, cause, treatment, risk factor relationships, etc). They can be said to have a sense, or direction, and thus the entities and the links between them can be discussed in terms of ‘predecessors’ and ‘successors.’”7
The skeletal structure of a Knowledge Net is therefore comprised of relationships between entities characterized as predecessors and successors (a particular entity can be both).7 Entity relationships are described using factual descriptors that are linked to scientific references. An important function of the structure of the Knowledge Net is the enablement of a systems perspective, as users become aware how specific relationships relate to particular problems, and how they may also be relevant in relation to other, otherwise unrelated problems.7
The Knowledge Net hence operationalizes Dewey’s conception of knowledge as “a perception of those connections of an object which determine its applicability in a given situation … We respond to [an event’s] connections and not simply to the immediate occurrence … An ideally perfect knowledge would represent such a network of interconnections that any past experience would offer a point of advantage from which to get at the problem presented in a new experience.”4
A Knowledge Network was constructed by a team who continuously reviewed the literature to identify medical knowledge relevant to solving medical problems for which Knowledge Couplers are built. That knowledge is analyzed to determine: 1) what diagnostic or treatment possibilities should be considered for a given medical problem; 2) for each possibility, what initial data points (findings) should be collected (from the patient history, physical exam, and lab tests) to determine whether that possibility is worth considering in a particular patient; and 3) additional information relevant to assessing the possibilities and findings.4
Knowledge from scientific research can be used to continually update the content of the Knowledge Net. Indeed, its structure provides a useful means for updating, organizing, and accessing new information, and can enable meaningful and effective crossdisciplinary and interprofessional research.7
THE PROBLEM-ORIENTED MEDICAL RECORD AND THE KNOWLEDGE NET
As long as the primary information source for building the Knowledge Net remains the contemporary published literature, the process will remain extremely human resource intensive, and subject to serious issues related to the availability and validity of data sources (and perceptions thereof), and inter- and intrarater reliability. These problems can potentially be addressed only when POMR standards are rigorously enforced in patient care, for sufficiently large populations.
The resulting accumulation of POMR records are referred to here as a POMR database. Also needed are initiatives such as the Transition and TRANSFoRm projects, which collect International Classification of Primary Care (ICPC) coded electronic medical record data, which could potentially be adapted (as they are currently used for probabilistic approaches) and leveraged for the development of Knowledge Nets.11–13
Dr Weed recognized that the development of robust POMR databases is contingent on an ability to systematically link individual patient records with medical knowledge, through the use of Knowledge Couplers, as described below.7–9
LINKING PATIENT DATA WITH MEDICAL KNOWLEDGE: KNOWLEDGE COUPLING
Knowledge Couplers are simply tools yielding diagnostic or management possibilities for specific problems. They are constructed using knowledge components derived from the Knowledge Net in the form of relationships between combinations of possible findings, and possible diagnoses or options for management.7,9,14 The construction and use of Knowledge Couplers are further described, below.
The Knowledge Net is used to identify possibilities for consideration, along with the data health care providers need to collect to investigate each possibility. This forms the basis of an electronic questionnaire (the Knowledge Coupler) for each presenting problem. The patient and provider use the questionnaire as guidance to determine what data to collect. They enter the collected data into the Coupler as findings (positive or negative or uncertain).
The Coupler output consists of the possibilities for which at least one positive finding was made, plus a list of positive and negative findings for each possibility, plus additional detail useful for assessing the possibilities and the findings. This process filters out possibilities that can safely be ignored. As to the possibilities that should not be ignored, the Coupler output organizes detailed information (data and knowledge) in a maximally usable form.
This output should be entered in electronic, problem-oriented records. If such records are rigorously maintained for large populations, it will then become possible to analyze those records for feedback on existing knowledge and development of new knowledge, which ultimately would be incorporated into the Knowledge Net.4,5
Knowledge Couplers therefore enable patients (and their families and caregivers) and health care providers to jointly discern and decide upon relationships between possible findings and possible diagnoses or options for management.4,9,14 In other words, Knowledge Couplers present possible diagnostic and management options for specific problems, which are subsequently matched to the unique biopsychosocial profile of the patient by purposively and systematically eliciting relevant qualitative and quantitative findings from both patients (eg, history, symptoms) and their health care providers (eg, signs, physical status).4,7 Through a series of systematic questions and prompts, possibilities are either eliminated or further investigated.
Couplers therefore enable patients and health care providers to jointly process the initial undercoded abductions of possibilities using combinatorial approaches, thereby enabling sound hypotheticodeductive reasoning and individualized care.7,15 The combinatorial approach’s iterative processes of abductive and deductive thought enables desired health care behaviors associated with meaningful communication, problem recognition, and joint decision making.4,14 More importantly, it is an empathetic scientific approach that starts and ends with an awareness of the uniqueness of each and every patient, as human beings.
The key aim of the knowledge coupling process is to enable the contextualization of patient problems, thereby rendering them more meaningful. An important derivative of this care process is the recognition and transparent disclosure of important gaps in medical knowledge, specifically in relation to the actual needs of patients.16
The combinatorial matching process therefore actively engages patients, families, and health care providers, and provides comparisons of the number of positive findings relative to the total number of potential findings that define specific diagnostic and management options.9 These ratios are not probability estimates; they simply show how well the patient matches with the array of options that may warrant consideration.9 For each option, the Knowledge Coupler provides more detailed information, including links to scientific references and probabilities derived from population-based statistics.7
THE ROLE AND USE OF STATISTICS
This alternative approach to evidence-based medicine is premised on the assumption that probabilities derived from population statistics should only be leveraged once the medical knowledge base related to the specific context of the patient’s unique combination of variables has been exhausted.4,9 The combinatorial approach is therefore not mutually exclusive, but complementary to probabilistic techniques, and potentially strengthens their validity.17
Dr Weed highlights that commencing with, or solely using, probabilistic logic may cause clinicians to miss rare possibilities, whereas algorithmic logic forces either-or decisions (when there may be two simultaneous choices).4,9 However, reconciling and synthesizing the combinatorial and probabilistic approaches is both desirable and necessary, because possibility and probability are mutually constitutive domains that are essential for the enablement of the science of medicine. The aforementioned ICPC-related projects have already demonstrated how POMR-derived databases could become powerful enough to generate statistically significant feedback on existing knowledge.12,13
THE PROBLEM-ORIENTED MEDICAL RECORD AS A DYNAMIC STANDARD: ENABLING A LEARNING HEALTH SYSTEM
Joint decisions by patients and health care providers related to diagnostic and management options should indeed be systematically incorporated into the respective patient’s POMR, which is transformed into a dynamic tool that educates patients and families, and enables them to actively play a central role in the management of their own health.4,7 Furthermore, systematic and rigorous utilization of the POMR yields structured databases that provide ongoing insight of the individual’s health status and enable the review and analysis of the logic of care decisions, thereby serving as the underpinning dynamo of a learning health care system by enabling meaningful feedback on existing knowledge, and the development of new knowledge (see Figure 1).4,7,8
The aforementioned combinatorial approach to evidence-based medicine therefore has important implications for the design and conduct of medical education, described by Dr Weed:
“Conceiving knowledge in these terms could lead to a new form of education, where students would be judged on their personal effectiveness in using network connections to solve real problems rather than their personal displays of disconnected knowledge.”4 “Flexner’s vision led to the Sisyphean ordeal that all medical students undergo—loading their minds with massive amounts of medical knowledge, and using their minds to apply all this knowledge to detailed patient data … . What Flexner missed was that medical students need to learn a core of behavior, the intellectual behaviors essential to modern science. First identified by Francis Bacon four centuries ago, these behaviors include the habitual use of external tools and techniques and standards to produce and manipulate complex information.”10
AN OVERLOOKED ALTERNATIVE PARADIGM FOR EVIDENCE-BASED MEDICINE
Some of the basic practicalities of implementing the problem-oriented combinatorial approach have been described in detail by Bartholomew18; however, fundamental questions pertaining to the theoretical and philosophical underpinnings of Dr Weed’s approach, and its impact on care processes and outcomes remain largely unaddressed.18,19 The fact that most health services researchers remain largely unaware of Dr Weed’s important contributions to medicine—specifically in relation to the creation of problem-oriented standards for medical records and combinatorial knowledge coupling—is troublesome in light of the ongoing problems facing contemporary evidence-based medicine.3,20
CONTEMPORARY APPROACHES TOWARD CONTEXTUALIZATION AND INDIVIDUALIZATION
It is well understood how and why (ontologically and epistemologically) contemporary evidence-based medicine fails to contextualize and individualize care within the context of patient complexity.17,21 The negative consequences of “standardized care” and so-called “best practices” on patient and provider experiences (particularly in relation to processes of care delivery and receipt), iatrogenicity, and health outcomes are well documented, and have given rise to the concept of quaternary prevention.22 Evidence-based medicine has attempted to address the issue of contextuality and the problems associated with patient complexity using various means, notably: isomorphic mimicry, aggregation, precision medicine, and normative calls for humanism.21,23–25
Isomorphic mimicry is a phrase derived from studies of “evidence-based policy,” and relates to pretense, emphasizing form over function.23 This is common in contemporary performance assessment, which often measures and reports person-centered attributes for nonperson-centered care approaches (eg, inappropriately applying Starfield’s performance attributes of comprehensiveness, longitudinality, first contact care, and coordination to disease management).26 Aggregation relates to contemporary approaches to multiple disease management within the context of multimorbidity on the basis of the flawed assumption that the whole is equal to the sum of the parts.25,27 Precision medicine’s increasing precision is inversely proportional to its accuracy, from the perspective of a person’s overall health outcomes (accuracy decreases caused by increasingly complex interactions within and between micro to macro holons of human biopsychosocial systems).24,28 Normative calls for humanism were addressed by Engel, who remarked that “given the opportunity, the younger generation is very ready to accept the importance of learning more about the psychosocial dimensions of illness and health care and the need for such education to be soundly based on scientific principles. Once exposed to such an approach, most recognize how ephemeral and insubstantial are appeals to humanism and compassion when not based on rational principles.”29
PHILOSOPHICAL AND OPERATIONAL DIFFERENCES BETWEEN COMBINATORIAL AND PROBABILISTIC PARADIGMS TO EVIDENCE-BASED MEDICINE
New paradigms to evidence-based medicine are urgently needed; paradigms that operationalize clear, coherent, and scientific approaches to “cope with the infinite multiplicity of interrelated and continuously changing problems that patients inevitably present,”1 something Dr Weed has attempted to address for close to half a century.30 The problem-oriented combinatorial approach presents an alternative paradigm to evidence-based medicine: rather than standardizing care, it individualizes care through the systematic application of scientific standards. The fundamental difference between the two approaches is that Dr Weed leverages standards to understand the meaning of specific constructs (eg, disease entities) within the context of individual patients, rather than imputing and imposing constructs (regardless of their sophistication) onto a person.17
Simply put, Dr Weed recognizes that constructs are simply tools, and are therefore means toward ends, and not ends themselves. This becomes clear when it is understood that the desired end is human problem recognition and awareness. He heeded Thoreau’s lament, that “Lo! Men have become the tools of their tools.”31 Contrary to contemporary nihilistic reductionist approaches, the combinatorial approach enables intelligent human decision making through the appropriate use of tools, rather than through promoting the artificial intelligence of tools.
The simplicity of Dr Weed’s approach is underpinned by immense intellectual sophistication, for it applies Dewey’s humanistic philosophy of knowledge to clinical medicine (ie, knowledge as “arising from an active adaptation of the human organism to its environment”),32 and operationalizes Frankl’s conceptualization of meaning to scientific constructs (ie, becoming aware of a possibility against the background of reality).33 It applies humanistic scientific principles to fulfill Donabedian’s call for the “affirmation and celebration of the uniqueness of every individual.”34
A transparent systems approach to evidence-based medicine is made possible, leveraging validated knowledge through combinatorial approaches to enable an individualized perspective that begins and ends with an awareness of each patient’s uniqueness.4,17 This approach eases medicine’s quandary of operating a “reduction ad unum of a plurality,” enabling health care providers to gradually bring Numbers Needed to Treat (eg, NNT) values closer to one.15 The complex transition processes that characterize and define diagnosis and treatment (as described by Baerheim)15 no longer remain obscure, and the art of medicine would manifest—rather than negate—scientific integrity.4 Furthermore, its problem-orientation aligns to the contemporary definition of value “as the health outcomes achieved that matter to patients.”35
A CALL FOR SERIOUS SCIENTIFIC CONSIDERATION AND INQUIRY
Health services research has called for a renaissance of evidence-based medicine that is real in relation to our humanity.21 For such a paradigm shift to happen, it needs to give serious consideration to thinkers who challenge their own status quo. Dr Weed’s combinatorial approach has been around for decades (with roots in the 1970s, when he led the Problem-Oriented Medical Information System laboratory at the Medical Center Hospital of Vermont), yet there have been extremely few meaningful independent scientific studies of the philosophical or theoretical underpinnings of his approach, or of the evaluations of implementation and impact on processes of care and outcomes of care.9 Furthermore, performance-related studies took the form of two randomized control trials, which are antithetical to the combinatorial approach, by design.4,36 Appropriate and meaningful evaluations operationalizing the theoretical principles of general systems theory are required. Moreover, apart from Dr Weed’s Problem Knowledge Coupling tools, it is unclear whether there exist meaningful alternative operationalizations of the generic concept of Knowledge Coupling.14,18
Without serious scientific research, it is impossible to validly ascertain the problem-oriented combinatorial approach’s impact on processes and outcomes of care from the perspective of diverse professional groups, care settings, and patient subpopulations. It is also important to note that combinatorial approaches such as the Johns Hopkins Adjusted Clinical Groups System, developed by Starfield,37 have shown significant power and accuracy in relation to the characterization of population health outcomes and are actively in use.
THE POLITICAL ECONOMY OF MEDICINE’S “DENIAL”: SOME INITIAL PROPOSITIONS WARRANTING FURTHER INVESTIGATION
The question of why medicine and health services research has ignored (or remains unaware of) Dr Weed’s approach is beyond the scope of this article. Note, however, that Dr Weed, in a series of articles and supplements in the British Medical Journal,38 along with his book Medicine in Denial,4 clearly described how his approach could overturn traditional Flexnerian medical education, training, and practice; transform the credentialing, professional roles, and functions of physicians (and other practitioners); and activate patients and their families.4,10,16,38 He openly stated the transformational threat he poses to those invested in contemporary health care systems.4,16,38–43
Clinicians have also shown significant reluctance toward seriously considering Dr Weed’s proposals. Critiques generally manifest fundamental misunderstandings of his approach, along with a tendency to conflate his paradigm with contemporary reductionist big data approaches to evidence-based medicine. Many of their basic concerns,39–40 related to physician autonomy, the role and empowerment of patients (and their families and caregivers), empathy, and the art of medicine, have been addressed by Dr Weed, himself a physician, in Medicine in Denial.4
Although his particular operationalization of knowledge coupling tools (the Problem Knowledge Coupling system) was commercialized at the conclusion of the PROMIS (Patient-Reported Outcomes Measurements Information System) project, Dr Weed has repeatedly expressed that his software is “just a particular implementation of the generic concept of [knowledge coupling], and that others are free to build and disseminate their own implementations of the concept.”3 Now at age 93 years, he continues to attempt to persuade the medical field and senior health care administrators to try his approach.18,42,43 Dr Weed believes that the National Library of Medicine should develop Knowledge Couplers and the Knowledge Net tools, and make Couplers available to both clinicians and patients. He views such development as a logical extension of the National Library of Medicine’s electronic repository.
CONCLUSION
Dr Weed is already renowned for being the father of the POMR, the ubiquitous medical care standard for collecting and managing patient data. What has been consistently overlooked was the reason this titan of medicine developed the problem-oriented approach in the first place. If the value of Engel’s biopsychosocial model indeed relates to “guiding the parsimonious application of medical knowledge to the needs of each patient,”44 Dr Weed’s problem-oriented approach warrants serious scientific consideration and study.
Acknowledgments
The author acknowledges and thanks Kees van Boven, MD, PhD; Jean Karl Soler, MD, PhD; Niek Klazinga, MD, PhD; and Dionne Kringos, PhD, for kindly reviewing and providing useful feedback in relation to the structure and content of an earlier draft of this article. The author thanks Lawrence Weed, MD (Emeritus Professor, University of Vermont College of Medicine), and Lincoln Weed, JD (retired lawyer and consultant) for answering questions about Dr Weed’s work. The author notes that the content of the article does not necessarily reflect the views or perspectives of those acknowledged or thanked.
Footnotes
Disclosure Statement
The author(s) have no conflicts of interest to disclose.
References
- 1.Weed LL. Medical records that guide and teach. N Engl J Med. 1968 Mar 21;278(12):652–7. doi: 10.1056/NEJM196803212781204. DOI: https://doi.org/10.1056/nejm196803212781204. [DOI] [PubMed] [Google Scholar]
- 2.VisualDx. Larry Weed’s 1971 internal medicine grand rounds [Internet]q. San Bruno, CA: YouTube; 2012. Jun 22, [cited 2016 Aug 7]. Available from: www.youtube.com/watch?v=qMsPXSMTpFI. [Google Scholar]
- 3.Jacobs L. Interview with Lawrence Weed, MD—the father of the problem-oriented medical record looks ahead. Perm J. 2009 Summer;13(3):84–9. doi: 10.7812/tpp/09-068. DOI: https://doi.org/10.7812/TPP/09-068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weed LL, Weed L. Medicine in denial. Seattle, WA: CreateSpace; 2011. [Google Scholar]
- 5.Weed L, Abbey LM, Bartholomew KA, et al. Knowledge Coupling: New premises and new tools for medical care and education. 1st ed. New York: Springer-Verlag; 1991. [Google Scholar]
- 6.Valderas JM, Starfield B, Sibbald B, Salisbury C, Roland M. Defining comorbidity: Implications for understanding health and health services. Ann Fam Med. 2009 Jul-Aug;7(4):357–63. doi: 10.1370/afm.983. DOI: https://doi.org/10.1370/afm.983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weed LL, Hertzberg RY. The use and construction of problem-knowledge couplers, the knowledge coupler editor, knowledge networks, and the problem-oriented medical record for the microcomputer. Proceedings of the Seventh Annual Symposium on Computer Applications in Medical Care. 1983 Oct;26:831–6. DOI: https://doi.org/10.1109/scamc.1983.764783. [Google Scholar]
- 8.Weed LL, Weed L. Building a reliable and affordable system of medical care. In: Weaver CA, Ball MJ, Kim GR, Kiel JM, editors. Healthcare information management systems: Cases, strategies, and solutions. 4th ed. Cham, Switzerland: Springer International Publishing; 2015. [Google Scholar]
- 9.Weed LL, Zimny NJ. The problem-oriented system, problem-knowledge coupling, and clinical decision making. Phys Ther. 1989 Jul;69(7):565–8. doi: 10.1093/ptj/69.7.565. [DOI] [PubMed] [Google Scholar]
- 10.Weed LL, Weed L. Diagnosing diagnostic failure. Diagnosis. 2014 Jan;1(1):13–7. doi: 10.1515/dx-2013-0020. DOI: https://doi.org/10.1515/dx-2013-0020. [DOI] [PubMed] [Google Scholar]
- 11.Soler JK, Corrigan D, Kazienko P, et al. Evidence-based rules from family practice to inform family practice; the learning healthcare system case study on urinary tract infections. BMC Fam Pract. 2015 May 16;16:63. doi: 10.1186/s12875-015-0271-4. DOI: https://doi.org/10.1186/s12875-015-0271-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Danger R, Corrigan D, Soler JK, et al. A methodology for mining clinical data: Experiences from TRANSFoRm project. Stud Health Technol Inform. 2015;210:85–9. DOI: https://doi.org/10.3233/978-1-61499-512-8-85. [PubMed] [Google Scholar]
- 13.Soler JK, Okkes I, Oskam S, et al. An international comparative family medicine study of the Transition Project data from the Netherlands, Malta, Japan and Serbia. An analysis of diagnostic odds ratios aggregated across age bands, years of observation and individual practices. Fam Pract. 2012 Jun;29(3):315–31. doi: 10.1093/fampra/cmr100. DOI: https://doi.org/10.1093/fampra/cmr100. [DOI] [PubMed] [Google Scholar]
- 14.Burger C. The use of problem-knowledge couplers in a primary care practice. Perm J. 2010 Spring;14(1):47–50. doi: 10.7812/tpp/09-115. DOI: https://doi.org/10.7812/TPP/09-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baerheim A. The diagnostic process in general practice: Has it a two-phase structure? Fam Pract. 2001 Jun;18(3):243–5. doi: 10.1093/fampra/18.3.243. DOI: https://doi.org/10.1093/fampra/18.3.243. [DOI] [PubMed] [Google Scholar]
- 16.Weed LL. New connections between medical knowledge and patient care. BMJ. 1997 Jul 26;315(7102):231–5. doi: 10.1136/bmj.315.7102.231. DOI: https://doi.org/10.1136/bmj.315.7102.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weaver RR. Reconciling evidence-based medicine and patient-centred care: Defining evidence-based inputs to patient-centred decisions. J Eval Clin Pract. 2015 Dec;21(6):1076–80. doi: 10.1111/jep.12465. DOI: https://doi.org/10.1111/jep.12465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bartholomew KA. Knowledge Coupling: New premises and new tools for medical care and education. New York: Springer-Verlag; 1991. Chapter 13 The Perspective of a Practitioner; pp. 235–77. [Google Scholar]
- 19.Thomas B. The problem-knowledge coupler principle: A conversation with Dr. Charles Burger [Internet] Seattle, WA: ChangingAging; 2012. Jan 10, [cited 2016 Nov 23]. Available from: http://changingaging.org/blogstream/the-problem-knowledge-coupler-principle-a-conversation-with-dr-charles-burger/ [Google Scholar]
- 20.Wright A, Sittig DF, McGowan J, Ash JS, Weed LL. Bringing science to medicine: An interview with Larry Weed, inventor of the problem-oriented medical record. J Am Med Inform Assoc. 2014 Nov-Dec;21(6):964–8. doi: 10.1136/amiajnl-2014-002776. DOI: https://doi.org/10.1136/amiajnl-2014-002776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Greenhalgh T, Howick J, Maskrey N Evidence Based Medicine Renaissance Group. Evidence based medicine: A movement in crisis? BMJ. 2014 Jun 13;348:g3725. doi: 10.1136/bmj.g3725. DOI: https://doi.org/10.1136/bmj.g3725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jamoulle M. Quaternary prevention, an answer of family doctors to overmedicalization. Int J Health Policy Manag. 2015 Feb 4;4(2):61–4. doi: 10.15171/ijhpm.2015.24. DOI: https://doi.org/10.15171/ijhpm.2015.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Andrews M, Pritchett L, Woolcock M. Escaping capability traps through problem-driven iterative adaptation (PDIA)—working paper 299 [Internet] Washington, DC: Center for Global Development; 2012. Jun 22, [cited 2016 Nov 23]. Available from: www.cgdev.org/publication/escaping-capability-traps-through-problem-driven-iterative-adaptation-pdia-working-paper. [Google Scholar]
- 24.Interlandi J. The paradox of precision medicine [Internet] New York, NY: Scientific American; 2016. Apr 1, [cited 2016 Nov 23]. Available from: www.scientificamerican.com/article/the-paradox-of-precision-medicine/ [DOI] [PubMed] [Google Scholar]
- 25.Shaneyfelt TM, Centor RM. Reassessment of clinical practice guidelines: Go gently into that good night. JAMA. 2009 Feb 25;301(8):868–9. doi: 10.1001/jama.2009.225. DOI: https://doi.org/10.1001/jama.2009.225. [DOI] [PubMed] [Google Scholar]
- 26.Starfield B. Is patient-centered care the same as person-focused care? Perm J. 2011 Spring;15(2):63–9. doi: 10.7812/tpp/10-148. DOI: https://doi.org/10.7812/TPP/10-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Friedman DJ, Hunter EL, Parrish RG III, editors. Health statistics: Shaping policy and practice to improve the population’s health. New York, NY: Oxford University Press Inc; 2005. [Google Scholar]
- 28.Stange KC.A science of connectedness Ann Fam Med 2009September-October75387–95. DOI: https://doi.org/10.1370/afm.990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Engel GL. The need for a new medical model: A challenge for biomedicine. Science. 1977 Apr 8;196(4286):129–36. doi: 10.1126/science.847460. DOI: https://doi.org/10.3109/13561828909043606. [DOI] [PubMed] [Google Scholar]
- 30.Weed LL. Medical records, patient care, and medical education. Ir J Med Sci. 1964 Jun;462:271–82. doi: 10.1007/BF02945791. DOI: https://doi.org/10.1007/bf02945791. [DOI] [PubMed] [Google Scholar]
- 31.Thoreau HD. Walden. Scotts Valley, CA: CreateSpace Independent Publishing Platform; 2014. [Google Scholar]
- 32.Pernecky T. Epistemology and metaphysics for qualitative research. Thousand Oaks, CA: SAGE; 2016. [Google Scholar]
- 33.Frankl VE. Man’s search for meaning. Boston, MA: Beacon Press; 2000. [Google Scholar]
- 34.Donabedian A. The quality of care. How can it be assessed? JAMA. 1988 Sep 23;260(12):1743–8. doi: 10.1001/jama.260.12.1743. DOI: https://doi.org/10.1001/jama.1988.03410120089033. [DOI] [PubMed] [Google Scholar]
- 35.Porter ME. What is value in health care? N Engl J Med. 2010 Dec 23;363(26):2477–81. doi: 10.1056/NEJMp1011024. DOI: https://doi.org/10.1056/nejmp1011024. [DOI] [PubMed] [Google Scholar]
- 36.Apkon M, Mattera JA, Lin Z, et al. A randomized outpatient trial of a decision-support information technology tool. Arch Intern Med. 2005 Nov 14;165(20):2388–94. doi: 10.1001/archinte.165.20.2388. DOI: https://doi.org/10.1001/archinte.165.20.2388. [DOI] [PubMed] [Google Scholar]
- 37.Starfield B, Kinder K. Multimorbidity and its measurement. Health Policy. 2011 Nov;103(1):3–8. doi: 10.1016/j.healthpol.2011.09.004. DOI: https://doi.org/10.1016/j.healthpol.2011.09.004. [DOI] [PubMed] [Google Scholar]
- 38.Weed LL, Weed L. Opening the black box of clinical judgment—an overview. BMJ. 1999 Nov 13;319(7220):1279. doi: 10.1136/bmj.319.7220.1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kernick DP. New connections between medical knowledge and patient care. Intervention of health professionals acts as an inductance, not as a resistor. BMJ. 1997 Nov 15;315(7118):1310. DOI: https://doi.org/10.1136/bmj.315.7118.1309b. [PMC free article] [PubMed] [Google Scholar]
- 40.Carty AT. New connections between medical knowledge and patient care. Human condition is full of decisions that aren’t simple yes/no decisions. BMJ. 1997 Nov 15;315(7118):1309–10. doi: 10.1136/bmj.315.7118.1309b. DOI: https://doi.org/10.1136/bmj.315.7118.1309b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hutchon DJ. New connections between medical knowledge and patient care. Information technology has much to offer certain aspects of health care. BMJ. 1997 Nov 15;315(7118):1310. DOI: https://doi.org/10.1136/bmj.315.7118.1309b. [PMC free article] [PubMed] [Google Scholar]
- 42.Weed L, Szecket N. Episode 19: Medicine in denial? An introduction to Dr Larry Weed. Sep 5, 2016. [Internet].[cited 2017 Jan 30]. Available from: http://imreasoning.com/episode-19-medicine-denial-introduction-dr-larry-weed/
- 43.Weed L, Szecket N. Episode 20: Medicine in Denial—Part 2—An interview with Larry Weed. Sep 23, 2016. [Internet].[cited 2017 Jan 30]. Available from: http://imreasoning.com/episode-20-medicine-denial-part-2-interview-larry-weed/
- 44.Borrell-Carrió F, Suchman AL, Epstein RM. The biopsychosocial model 25 years later: Principles, practice, and scientific inquiry. Ann Fam Med. 2004 Nov-Dec;2(6):576–82. doi: 10.1370/afm.245. DOI: https://doi.org/10.1370/afm.245. [DOI] [PMC free article] [PubMed] [Google Scholar]