Abstract
Objective
Hispanic parents in the US are disproportionately affected by low health literacy and limited English proficiency (LEP). We examined associations between health literacy, LEP, and liquid medication dosing errors in Hispanic parents.
Methods
Cross-sectional analysis of data from a multisite randomized controlled experiment to identify best practices for the labeling/dosing of pediatric liquid medications (SAFE Rx for Kids study); 3 urban pediatric clinics. Analyses were limited to Hispanic parents of children <8 years, with health literacy and LEP data (n=1126). Parents were randomized to 5 groups that varied by pairing of units of measurement on the label/dosing tool. Each parent measured 9 doses [3 amounts (2.5,5,7.5 mL) using 3 tools (2 syringes (0.2,0.5 mL increment), 1 cup)] in random order. Dependent variable: Dosing error=>20% dose deviation. Predictor variables: health literacy (Newest Vital Sign) [limited=0–3; adequate=4–6], LEP (speaks English less than “very well”).
Results
83.1% made dosing errors (mean(SD) errors/parent=2.2(1.9)). Parents with limited health literacy and LEP had the greatest odds of making a dosing error compared to parents with adequate health literacy who were English proficient (% trials with errors/parent=28.8 vs. 12.9%; AOR=2.2[1.7–2.8]). Parents with limited health literacy who were English proficient were also more likely to make errors (% trials with errors/parent=18.8%; AOR=1.4[1.1–1.9]).
Conclusion
Dosing errors are common among Hispanic parents; those with both LEP and limited health literacy are at particular risk. Further study is needed to examine how the redesign of medication labels and dosing tools could reduce literacy and language-associated disparities in dosing errors.
Keywords: patient safety, medication administration errors, health literacy, limited English proficiency
INTRODUCTION
In the United States (US), parents frequently make errors in dosing medications for their children;1–3 studies have documented that more than half of parents make errors when dosing liquid medication for their children.4,5 Factors which contribute to the complexity of the task of dosing include: units of measurement (e.g. mL, teaspoon), dosing tools (e.g. dosing cups, syringes, droppers), and the wide range of recommended dose amounts.1,6
One group thought to be at risk for dosing errors are Hispanics. More than 50 million adults in the US identify as Hispanic or Latino, and this population is growing rapidly.7 Results of limited studies involving Hispanics have shown that medication errors and poor adherence are common with adult medication regimens;8,9 few studies have focused on dosing errors by Hispanic parents and the underlying factors involved.1,2,10 Two likely contributors are limited low health literacy and limited English proficiency (LEP).
In the US, approximately one in three parents have low health literacy,11 limiting their ability to obtain, process, and understand the information necessary to make appropriate health-related decisions.12 Hispanic parents have twice the odds of having low health literacy compared to White parents.11 Prior studies have documented that limited health literacy is associated with poorer understanding of medication labels,13 dosing errors,1 and non-adherence,14 but have not focused on Hispanics. LEP affects nearly one in ten adults in the US, with over two-thirds being Spanish-speakers.7
LEP has been associated with misunderstanding of medication labels,10,15 higher prevalence of dosing errors10 and adverse drug events.16 To date, the few studies of LEP and parent dosing of liquid medications have found that those with LEP are at risk for error; these existing studies have involved single sites, and did not look at the combined effects of LEP and health literacy.10,17
In this study, we sought to examine associations between health literacy and English proficiency and liquid medication dosing errors among Hispanic parents, looking at these risk factors independently and in combination.
METHODS
Participants and Setting
This was a cross-sectional analysis of data collected as part of a randomized controlled experiment focused on identifying specific attributes of medication labels/dosing tools that can be optimized to reduce parent dosing errors (SAFE Rx for Kids Study). Subjects were enrolled from three university-affiliated pediatric outpatient clinics which serve largely low income populations (New York University, Stanford, Emory). Northwestern University served as the data management site and enrolled no participants.
Study enrollment was conducted by research assistants (RAs) who approached consecutive adults with children with clinic appointments, to determine eligibility. Parents were told that the study was focused on learning the best way to help parents understand instructions for children’s medicines. They were told that they would be asked to look at instructions like those they might see on a prescription label and show how they would measure out medicines. Inclusion criteria included: parent/legal guardian <18 years of age of a child ≤8 years of age, English- or Spanish-speaking, usually gives medications to child, and no previous participation in a dosing study. Caregivers were excluded if they had visual acuity worse than 20/50 (Rosenbaum Pocket Screener), uncorrectable hearing impairment, or if the child was presenting for emergency care. At the Emory site, only English-speakers were enrolled as this site predominantly serves African-American families; few Spanish-speaking families are seen. Caregivers provided informed consent. For this cross-sectional analysis of data, we only included caregivers who self-identified as “Hispanic or Latino” and completed the dosing and health literacy assessments. We focused on Hispanic parents, as in our study,18 these families had a 1.5 times increased odds of error compared to non-Hispanic parents, and we were interested in examining the individual and combined effects of health literacy and English proficiency in this at-risk group. For the remainder of this paper, parents who identified as either “Hispanic or Latino” are referred to as Hispanic. A $20 gift card was given to parents as an incentive upon completion of the study measurements. Institutional review board approval was obtained from each site.
Measures
Trained RAs conducted study measures in person on the day of the clinic visit, before or after the child’s appointment. There was one senior research coordinator per site who oversaw the activities of all RAs at their site (~2–3/site). Senior coordinators at each site were individually trained by the head project coordinator (JJ) and PI at the lead (NYU) site. Randomization groups were assigned by the project coordinator (JJ) using a random number generator blocked by site, in sets of 100; RAs were blinded to group until after participant enrollment. All assessments were performed in English or Spanish, based on parent preference. The primary outcome of interest was medication dosing error. Primary predictor variables included parent health literacy and English proficiency.
Study Procedures
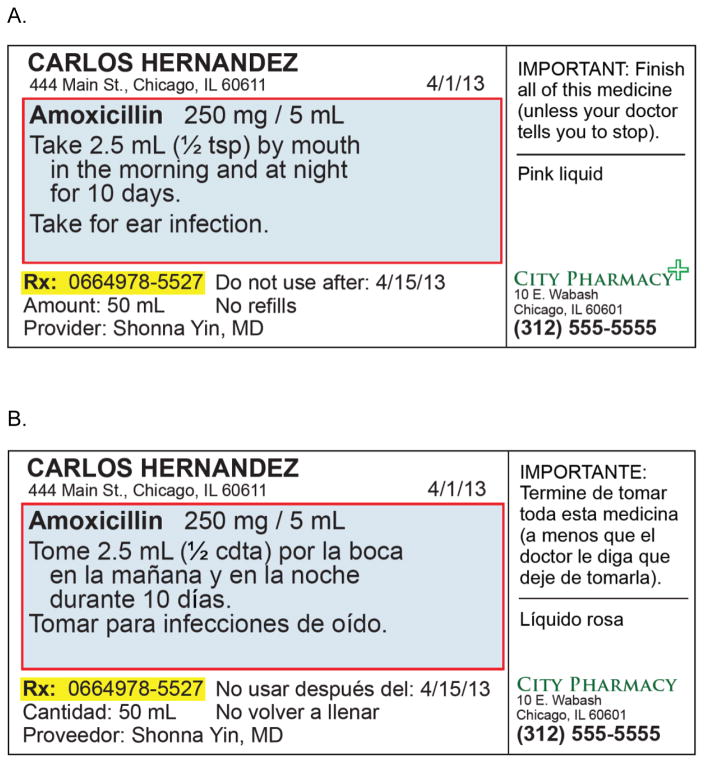
Eligible parents were randomly assigned to one of five groups which differed by the unit of measurement shown on the medication bottle label and dosing tool [Label-Dosing tool: mL-mL (mL-only) (Group 1), mL/tsp-mL/tsp (Group 2), mL/teaspoon-mL/tsp (Group 3), mL/ml-tsp (Group 4), tsp-mL/tsp (Group 5)].18 Labels were written in English or Spanish (e.g. “teaspoon” translated as “cucharadita”; “tsp” as “cdta”); parents were given labels in their language of preference. Translation of the label involved a team-based group consensus review; pilot testing was also conducted. Dosing tools were marked in English only, as is standard practice in the US.
Parents in each group were each asked to measure a total of 9 times [three dose amounts (2.5, 5, 7.5 mL) using three tool types]; order was randomized using a random number generator, blocked by site, in sets of 100. The three dosing tools were: 1)oral syringe (10 mL capacity, 0.2 mL increment markings), 2)oral syringe (10 mL capacity, 0.5 mL increment markings), and 3)dosing cup (1 ounce capacity, 2.5 mL or ½ tsp increment markings). Parents looked at labels in their language of preference (English or Spanish) to determine how much medicine to measure (Figure 1). Dosing assessments were conducted first, followed by a survey to assess sociodemographic characteristics and health literacy.
FIGURE 1.
Example of medication label in English (A) and Spanish (B) for Group 2
Primary Outcome Variable: Medication Dosing Error
Dosing error was defined as having more than a 20% deviation above or below the tested dose. Prior studies have used a 20% deviation to represent a clinically meaningful error.1,2 We determined the measured dose weight by subtracting the weight of the pre-assessment empty dosing tool weight from the weight of the tool containing the parent-measured dose. Percent deviation was calculated by comparing the parent-measured dose weight to a reference dose weight. The reference dose weight for a 5 mL dose was obtained by averaging the measured dose weight of a 5 mL dose for 10 pediatricians using an oral syringe; reference weights were then calculated for the 2.5 and 7.5 mL doses.
Predictor Variables: Health Literacy and Limited English Proficiency
Health literacy was assessed using the Newest Vital Sign (NVS).19 The NVS was selected as it is validated in English and Spanish and tests quantitative, document and prose literacy skills, which are helpful for interpreting medication instructions; other measures of health literacy, such as the Short Test of Functional Health Literacy in Adults and Short Assessment of Health Literacy for Spanish Adults are validated in Spanish but do not focus on quantitative skills.20,21 Participants were categorized into 2 groups, as having adequate (score 4–6), or limited health literacy (score 0–3).1,
Parents were asked “How well do you speak English?” to determine their English proficiency level; this question was asked in the parents’ language of preference. A response of “very well” was considered English proficient. Responses of “well”, “not well”, or “not at all” were considered limited English proficient.22,23 Parents were then categorized into one of four groups based on their health literacy and English proficiency levels: 1) limited health literacy and LEP, 2) limited health literacy and English proficient, 3) adequate health literacy and LEP, and 4) adequate health literacy and English proficient.
Sociodemographic Data and Child Health Status
Parents completed a questionnaire following the dosing assessment which included questions on parent characteristics (age, gender, relationship to child, race/ethnicity, education, household income) and child characteristics (age, gender). Child chronic disease status was assessed using questions adapted from the CSHCN survey.24
Statistical Analyses
Data were analyzed using SAS software version 9.4 (SAS Institute, Inc., Cary, NC). Differences in parent characteristics across levels of health literacy and English proficiency were assessed using chi-square tests for categorical variables and Kruskal-Wallis tests for continuous measures. The likelihood of making a dosing error by health literacy and English proficiency levels was estimated using multiple logistic regression with generalized estimating equations (GEE) to account for repeated dosing trial measurements per parent. Models were adjusted for factors chosen a priori (randomization group, dosing tool type, dose amount, trial order) and identified confounders (parent age, education, household income; study site).
Spearman correlations were used to look at the relationship between LEP and country of birth (US born vs. non-US born) as well as LEP and language (language interview conducted in; English or Spanish). As LEP and non-US country of birth, and LEP and Spanish-speaking were highly correlated, country of birth and language were not included in the main model, although alternate regression models were run replacing LEP status with country of birth, and LEP status with language.
For analyses, a 2-tailed P <0.05 was considered statistically significant.
RESULTS
Of 2110 parents enrolled in the SAFE Rx for Kids study between August 26, 2013 and December 18, 2014, 1141 (54.1%) self-identified as Hispanic. Findings of the main study are reported elsewhere;18 this analysis focuses only on Hispanic parents. Of the Hispanic parents enrolled, 15 were excluded because they did not complete a dosing (n=1) or health literacy (n=14) assessment. Thus, 1126 parents were included in analyses (Table 1). Nearly 70% of parents had LEP (69.2%). 82.7% had limited health literacy (42.1% low, 40.6% marginal health literacy). Of parents who had LEP, 88.8% had limited and 11.2% adequate health literacy; of parents who were English proficient, 68.9% had limited and 31.1% adequate health literacy (p<0.001).
TABLE 1.
Study Subject Characteristics (n=1126)
| Mean (SD) or n (%) | |
|---|---|
| Child age, mean (SD) yrs | 2.2 (2.2) |
| Parent age, mean (SD), yrs | 29.8 (6.6) |
| Relationship to child – Mother, n (%) | 1063 (94.4%) |
| Born in the US, n (%) | 315 (28.0%) |
| Parent language, n (%) | |
| English | 406 (36.1%) |
| Spanish | 720 (63.9%) |
| English proficiency, n (%) | |
| English proficient | 347 (30.8%) |
| LEP | 779 (69.2%) |
| Parent educationa – | |
| Less than HS graduate, n (%) | 487 (43.4%) |
| Household income, n (%) | |
| <$10,000 | 199 (17.7%) |
| $10–19,999 | 320 (28.4%) |
| $20–39,999 | 364 (32.3%) |
| >=$40,000 | 111 (9.9%) |
| Unknown | 132 (11.7%) |
| Health literacy levelb, n (%) | |
| Limited | 931 (82.7%) |
| Adequate | 195 (17.3%) |
| Child with chronic disease, n (%) | 223 (20.7%) |
| Site, n (%) | |
| Site 1 | 562 (49.9%) |
| Site 2 | 535 (47.5%) |
| Site 3 | 29 (2.6%) |
Missing for 3 subjects
Health literacy measured using the Newest Vital Sign (NVS). Mean(SD) NVS score was 2.0(1.5).
Overall, 83.1% of parents made a dosing error at least one out of the nine dosing trials. Parents made an average of 2 errors each [mean(SD)=2.2(1.9)].
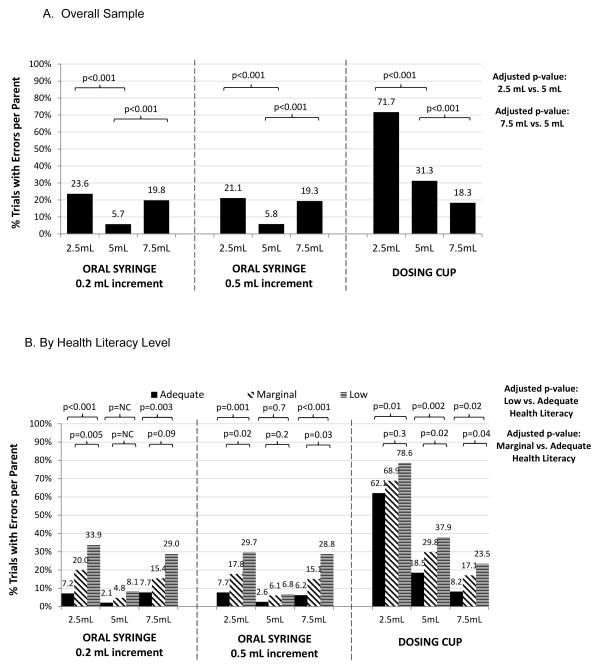
The frequency and magnitude of dosing error rates varied by dose amount and tool type. There was no difference in error rates between the two syringe types tested (p=0.1). More parents made errors with cups than syringes (cup vs. 0.5 mL increment syringe: 40.4% vs. 15.4%, p<0.001; AOR=4.6[95%CI:4.1–5.2]). For oral syringes, more errors were observed for 2.5 mL and 7.5 mL doses compared to the 5 mL dose (2.5 vs. 5 mL amount: 22.3% vs. 5.7%, p<0.001; AOR= 5.3[4.2–6.7]; 7.5 vs. 5 mL amount: 19.5% vs. 5.7%, p<0.001; AOR=4.4[3.5–5.6]) (Figure 2A). For cups, more errors were seen with 2.5 mL and 5 mL doses (2.5 vs. 5 mL amount: 71.7% vs. 31.3%, p<0.001; AOR=6.2[5.2–7.4]; 7.5 vs 5 mL amount: 18.3% vs. 31.3%, p<0.001; AOR=0.5[0.4–0.6]).
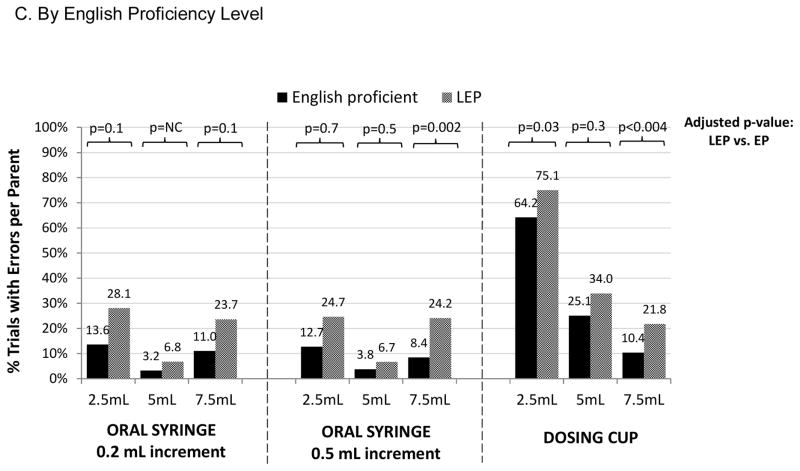
FIGURE 2.
Hispanic Parent Dosing Errors Stratified By Dosing Tool and Dose Amounta
NC=model does not converge
aMultiple logistic regression with Generalized Estimating Equations; model adjusted for randomization group, dosing tool type, dose amount, trial order, parent age, education, household income, study site.
Parent Dosing Errors by Health Literacy and English Proficiency Level
Overall, across the dose amounts and dosing tools tested, parents with limited health literacy and parents with LEP made the most errors (Figures 2B and 2C). There were few errors seen with the 5 mL dose with syringes; no significant differences were found in errors by health literacy or English proficiency when looking at 5 mL dose amounts using syringes, with 3 models not converging due to the small number of errors in these cases.
In adjusted models accounting for repeated measures across doses and dosing tool types, parents with low health literacy and LEP had a higher odds of making a dosing error (low vs. adequate health literacy: AOR=2.0[1.6–2.4]; marginal vs. adequate health literacy: AOR=1.5[1.2–1.8]; LEP vs. English proficient: AOR=1.4[1.2–1.6]) (Table 2). Those with both limited health literacy and LEP had over twice the odds of making an error compared to parents with adequate health literacy and English proficiency (AOR=2.2[1.7–2.8]).
TABLE 2.
Health Literacy, Limited English Proficiency, and Dosing Errors by Hispanic Parents: Adjusted Analyses
| n | % trials with errors/parent | AOR (95% CI)a | p value | ||
|---|---|---|---|---|---|
| Model Looking at Health Literacy and English Proficiency Status Separately | |||||
| Health Literacy Level | Low | 472 | 30.7 | 2.0 (1.6–2.4) | <0.001 |
| Marginal | 456 | 21.7 | 1.5 (1.2–1.8) | 0.0002 | |
| Adequate | 195 | 13.6 | 1.0 | Ref | |
| English Proficiency Level | Limited English Proficiency | 777 | 27.2 | 1.4 (1.2–1.6) | 0.0001 |
| English Proficiency | 346 | 16.9 | 1.0 | Ref | |
| Model with Adequate Health Literacy and English Proficient Parents as Referent Group | |||||
| Limited Health Literacy | Limited English Proficiency | 690 | 28.8 | 2.2 (1.7–2.8) | <0.001 |
| Limited Health Literacy | English Proficiency | 238 | 18.8 | 1.4 (1.1–1.9) | 0.01 |
| Adequate Health Literacy | Limited English Proficiency | 87 | 14.4 | 1.2 (0.9–1.6) | 0.3 |
| Adequate Health Literacy | English Proficiency | 108 | 12.9 | 1.0 | Ref |
| Model with Limited Health Literacy and Parents with LEP as Referent Group | |||||
| Limited Health Literacy | Limited English Proficiency | 690 | 28.8 | 1.0 | Ref |
| Limited Health Literacy | English Proficiency | 238 | 18.8 | 0.7 (0.5–0.8) | <0.001 |
| Adequate Health Literacy | Limited English Proficiency | 87 | 14.4 | 0.5 (0.4–0.7) | <0.001 |
| Adequate Health Literacy | English Proficiency | 108 | 12.9 | 0.5 (0.4–0.6) | <0.001 |
Multiple logistic regression with Generalized Estimating Equations; model adjusted for randomization group, dosing tool type, dose amount, trial order, parent age, education, household income, study site.
Role of Country of Origin and Language
LEP and non-US country of origin were highly correlated (Spearman rho= 0.68 (p<0.0001)). Among those with LEP, 92.5% were non-US born; among those who were English proficient, 74.0% were US-born. In models where LEP was replaced with country of origin, non-US born parents had 1.3 times the odds of an error compared to non-US parents (AOR=1.3[1.1–1.6]).
LEP and Spanish language were also highly correlated (Spearman rho=0.77, p<0.0001). Among those with LEP, 88.6% opted to conduct the assessment in Spanish; among those who were English proficient, 91.3% did assessments in English. In models where LEP was replaced with language, Spanish-speaking parents had 1.6 times the odds of an error compared to English-speaking parents (AOR=1.6[1.3–1.9]).
DISCUSSION
This study is the first to specifically examine medication dosing errors made by Hispanic parents and the independent and combined roles of parent health literacy and English proficiency. We found that liquid medication dosing errors by Hispanic parents are common, with over 80% of parents making at least one error, and that errors were more common among those with limited health literacy and LEP. These findings demonstrate the importance of addressing health literacy and LEP as part of efforts to reduce pediatric medication errors.
The high rate of liquid medication dosing errors among Hispanic parents that we found is consistent with prior studies;1,2,10 one prior study found that nearly 80% of Spanish-speaking parents made a dosing error, compared to 50% of English-speaking parents.10 While few studies have looked specifically at disparities in rates of dosing errors for pediatric patients, prior studies have revealed racial/ethnic disparities in misunderstanding and adherence with adult medications.25 Factors underlying these disparities are multifold, although limited health literacy and LEP likely play a role.16,26 When looking at error rates in the SAFE Rx study, while Hispanics had ~1.5 times increased odds of error compared to non-Hispanics, this effect was no longer significant once factors like health literacy and LEP were included in models (analyses not shown).
Similar to prior studies of low health literacy and suboptimal medication use,1,6,17 our investigation found that parents with limited health literacy made more dosing errors compared to parents with adequate health literacy; a prior study by our team also found a nearly 2-fold increased odds of error for those with low health literacy compared to those with adequate health literacy, with error rates differing by dosing tool used (e.g. for one of the cups, 55% of low literacy parents made a dosing error compared to 31% parents with adequate literacy).6 Just as imparting health literacy best practices for the labeling of adult prescriptions has been recommended, our findings suggest that the design of medication labels and dosing tools in the context of pediatric liquid medications should also factor in health literacy principles.
In the US, Spanish speakers, along with other non-English speakers, must frequently manage medications using English language instructions and materials, as pharmacy translation services are often limited or even non-existent.27 Efforts to improve access to language-concordant medication labeling are ongoing and are an important step in reducing disparities that result from LEP.28 Misunderstanding of medical instructions can place LEP families at disproportionate risk for poor outcomes; one prior study of adverse events found that those with LEP were more likely to experience significant harm compared to English-speaking patients, and that adverse events experienced by those with LEP were more likely to be due to communication errors.29 In our study, we found that Hispanic parents with LEP made more dosing errors than their English proficient counterparts, even when they receive medication labels in their language of preference. It is likely that simply providing translated materials is not enough to overcome communication barriers related to medication instructions. Notably, the dosing tools we provided had English markings only, as this is standard practice in the US. Thus, Spanish speakers randomized to the groups who received labels with teaspoon units saw the Spanish abbreviation for teaspoon (“cdta”) on medication labels, but had dosing tools with “tsp” units. It is also possible that acculturation may have played a role in medication dosing. LEP is sometimes used as a proxy for limited acculturation,30 and LEP parents are often recent immigrants to the US from Latin American nations, where there are wide variations in the availability and format of prescription medication labels.31 Further study is needed to better understand our study findings, including identifying strategies beyond language concordance that can be used to reduce errors in LEP populations.
Although limited health literacy and LEP have been individually recognized as barriers to communication and understanding of health information, and often coexist in a population, little work has been done to explore these issues together, 32 particularly as they relate to pediatric medication dosing errors. We found that parents who had both limited health literacy and LEP were at particular risk for making dosing errors. This finding highlights that it is especially important to consider the communication needs of this vulnerable population in the design and implementation of strategies to reduce medication errors.
Interestingly, with oral syringes, the pattern of increased rates of error for those with low health literacy and LEP was seen across dose amounts tested, with the fewest errors seen overall with the 5 mL dose. This is not surprising, as the 5 mL dose involved a simpler, whole number amount, compared to the 2.5 and 7.5 mL doses, which involved amounts with decimals. There were so few errors with the 5 mL dose that 3 models we looked at in subanalyses did not converge (0.2 mL increment syringe with 5 mL dose by health literacy and English proficiency level). In the other models involving 5 mL doses and oral syringes, there were no statistically significant differences by health literacy or English proficiency. These findings suggest that in addition to improving the design of labels/dosing tools, changes in prescriber practices, such that whole number doses are prescribed, should be further studied as a potentially promising strategy to reduce errors for parents across health literacy and English proficiency levels.
This study has several limitations. It is a cross-sectional analysis, which limits our ability to draw conclusions regarding causation. Errors were examined using a hypothetical dosing assessment which may not accurately reflect how parents dose medicines at home. We examined error rates at one point in time, and not actual behaviors over time, so we were not able to examine parent ability to learn the skill of dosing over time, although notably, we did not find any association between child chronic disease status and dosing error. Parents did not receive verbal medication counseling, as they might receive from their child’s doctor, nurse, or pharmacist, and thus our study looks only at parent understanding of written medication instructions. While there has been limited study of the content and depth of health care provider medication counseling, prior studies have documented that counseling from physicians and pharmacists is often suboptimal;29,33 in 2 studies, ~50% of patients reported not receiving any counseling by the pharmacist.33 This leaves the medication bottle label as an important source of information that should be designed to be easily understood. In addition, it is well-recognized that patients often forget a large percentage of the information verbally presented to them by their health care provider;34 the bottle label thus serves as an important piece of written information that the patient can refer to prior to administering a medication at home.35 We tested dosing with a limited set of dosing tools, which had markings written in English, as is standard for dosing tools available in the US, but this may have been a source of confusion for Spanish-speakers. Additionally, Spanish-speaking parents were given medication label instructions in their language of preference, so our results likely underestimate the impact of LEP on medication dosing errors in the real world where English language materials are common. We assessed health literacy using the NVS, which has been validated in Spanish, however prior studies have found that Spanish-speakers consistently score lower on the NVS than English-speakers. Although there were three sites, one site contributed only a small amount of data; overall findings however, were not different whether or not the site was excluded or included in analyses (data not shown). In addition, we excluded parents of children who were being seen for emergency care, which may have led to selection bias towards enrolling healthy children, however, about 1 in 5 children in our sample were identified as having a chronic disease. Finally, we conducted this study with English- and Spanish-speaking families seeking care for their children at urban hospital-affiliated pediatric clinics, and our results may therefore not be generalizable to other populations.
Still, this study highlights the importance of addressing both limited health literacy and LEP when considering new strategies to reduce liquid medication dosing errors by Hispanic parents, especially when both risk factors are present. Efforts to revise existing standards or to redesign pediatric medication labels and dosing tools should be specifically tailored to meet the needs of limited literacy and LEP individuals. Further research is needed to better understand the intersection between health literacy and language barriers in order to effectively promote the safe use of pediatric liquid medications.
WHAT’S NEW.
Limited health literacy and limited English proficiency (LEP) are independently associated with more medication dosing errors in Hispanic parents. Hispanic parents with both low health literacy and LEP are at greatest risk.
Acknowledgments
We thank our research staff, and the staff of the pediatric outpatient clinics at Bellevue Hospital Center, Gardner Packard Children's Health Care Center, and Children’s Hospital of Atlanta at Hughes Spaulding, for their support.
This research was supported with funding from the National Institutes of Health (NIH) / National Institute of Child Health and Human Development (NICHD) (R01 HD070864; Principal investigator H. Shonna Yin); authors funded as part of this grant include Drs Yin, Mendelsohn, Bailey, Sanders, Wolf, Parker, and Kim, and Ms. Patel, Jimenez, Jacobson, Smith. Dr. Yin was also supported by HRSA Grant 12-191-1077- Academic Administrative Units in Primary Care. Dr. Sanders is also supported by FDA CERSI grant (UCSF-Stanford CERSI Award #13). Dr. Harris was supported by the New York Academy of Medicine Margaret E. Mahoney Fellowship and the Arnold P. Gold Foundation Student Summer Research Fellowship. Study sponsors were not involved in the design of the study, the collection, analysis or interpretation of the data, the writing of the manuscript, or the decision to submit the manuscript for publication.
Footnotes
Conflict of Interest: The authors have no conflicts of interest to disclose.
Previous Presentation: Preliminary data from this study were presented at the 2015 Pediatric Academic Societies meeting; April 25, 2015; San Diego, CA.
Clinical Trial Registration: ClinicalTrials.gov Identifier: NCT01854151
Preliminary data from this study were presented at the 2015 Pediatric Academic Societies meeting; April 25, 2015; San Diego, CA.
CONTRIBUTOR STATEMENT
Leslie M. Harris: Dr. Harris conceptualized and designed the study, analyzed and interpreted the data, drafted the initial manuscript, critically revised the manuscript for important intellectual content, and approved the final manuscript as submitted. No honorarium, grant, or other form of payment was received to produce the manuscript.
Benard Dreyer and Alan Mendelsohn: Drs. Dreyer and Mendelsohn helped conceptualize and design the study, were involved in the analysis and interpretation of data, critically revised the manuscript for important intellectual content, provided study supervision, and approved the final manuscript as submitted.
Stacy Bailey, Lee M. Sanders, Michael S. Wolf, Ruth M. Parker: Drs. Bailey, Sanders, Wolf, and Parker helped conceptualize and design the study, were involved in the analysis and interpretation of the data, critically revised the manuscript for important intellectual content, provided study supervision, and approved the final manuscript as submitted.
Deesha Patel and Kwang-Youn Kim: Ms. Patel and Dr. Kim helped conceptualize and design the study, analyzed and interpreted the data, critically revised the manuscript for important intellectual content, and approved the final manuscript as submitted.
Jessica Jimenez, Kara Jacobson, and Michelle Smith: Ms. Jimenez, Ms. Jacobson, and Ms. Smith participated in the conceptualization and design of the study, assisted in acquisition of data used in the study, analysis and interpretation of the data, drafting of the manuscript, and approved the final manuscript as submitted.
H. Shonna Yin: Dr. Yin helped conceptualize and design the study, analyzed and interpreted the data, critically revised the manuscript for important intellectual content, provided study supervision, and approved the final manuscript as submitted.
Financial Disclosure: Drs. Bailey, Parker, and Wolf, and Ms. Jacobson, have served as consultants to, and received grant funding, from Merck, Sharp and Dohme for work unrelated to this study.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Yin HS, Dreyer BP, Ugboaja DC, et al. Unit of measurement used and parent medication dosing errors. Pediatrics. 2014;134(2):e354–e361. doi: 10.1542/peds.2014-0395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yin HS, Dreyer BP, van Schaick L, Foltin GL, Dinglas C, Mendelsohn AL. Randomized controlled trial of a pictogram-based intervention to reduce liquid medication dosing errors and improve adherence among caregivers of young children. Arch Pediatr Adol Med. 2008;162(9):814–822. doi: 10.1001/archpedi.162.9.814. [DOI] [PubMed] [Google Scholar]
- 3.Madlon-Kay DJ, Mosch FS. Liquid medication dosing errors. J Fam Practice. 2000;49(8):741–744. [PubMed] [Google Scholar]
- 4.Li SF, Lacher B, Crain EF. Acetaminophen and ibuprofen dosing by parents. Pediatr Emerg Care. 2000;16(6):394–397. doi: 10.1097/00006565-200012000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Simon HK, Weinkle DA. Over-the-counter medications: do parents give what they intend to give? Arch Pediatr Adol Med. 1997;151(7):654–656. doi: 10.1001/archpedi.1997.02170440016003. [DOI] [PubMed] [Google Scholar]
- 6.Yin HS, Mendelsohn AL, Wolf MS, et al. Parents' medication administration errors: role of dosing instruments and health literacy. Arch Pediatr Adol Med. 2010;164(2):181–186. doi: 10.1001/archpediatrics.2009.269. [DOI] [PubMed] [Google Scholar]
- 7.U.S. Census Bureau. Ennis SR, Rios-Vargas M, Albert NG. The Hispanic Population: 2010. 2010 Census Briefs. 2011:1–16. [Google Scholar]
- 8.Kaplan RC, Bhalodkar NC, Brown EJ, Jr, White J, Brown DL. Race, ethnicity, and sociocultural characteristics predict noncompliance with lipid-lowering medications. Prev Med. 2004;39:1249–1255. doi: 10.1016/j.ypmed.2004.04.041. [DOI] [PubMed] [Google Scholar]
- 9.Mohan AV, Riley MB, Boyington DR, Kripalani S. Illustrated medication instructions as a strategy to improve medication management among Latinos: a qualitative analysis. J Health Psychol. 2012;18(2):187–197. doi: 10.1177/1359105312440300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Levya M, Sharif I, Ozuah PO. Health literacy among Spanish-speaking Latino parents with limited English proficiency. Ambul Pediatr. 2005;5(1):56–59. doi: 10.1367/A04-093R.1. [DOI] [PubMed] [Google Scholar]
- 11.Yin HS, Johnson M, Mendelsohn AL, Abrams MA, Sanders LM, Dreyer BP. The health literacy of parents in the United States: a nationally representative study. Pediatrics. 2009;124(Suppl 3):S289–298. doi: 10.1542/peds.2009-1162E. [DOI] [PubMed] [Google Scholar]
- 12.Institute of Medicine. Health Literacy: A Prescription to End Confusion. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- 13.Bailey SC, Pandit AU, Yin S, et al. Predictors of misunderstanding pediatric liquid medication instructions. Fam Med. 2009;41(10):715–721. [PubMed] [Google Scholar]
- 14.Zhang NJ, Terry A, McHorney CA. Impact of health literacy on medication adherence: a systematic review and meta-analysis. Ann Pharmacother. 2014;48(6):741–751. doi: 10.1177/1060028014526562. [DOI] [PubMed] [Google Scholar]
- 15.Masland MC, Kang SH, Ma Y. Association between limited English proficiency and understanding prescription labels among five ethnic groups in California. Ethn Health. 2011;16(2):125–144. doi: 10.1080/13557858.2010.543950. [DOI] [PubMed] [Google Scholar]
- 16.Wilson E, Chen AH, Grumbach K, Wang F, Fernandez A. Effects of limited English proficiency and physician language on health care comprehension. J Gen Intern Med. 2005;20(9):800–806. doi: 10.1111/j.1525-1497.2005.0174.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yin HS, Mendelsohn AL, Fierman A, van Schaick L, Bazan IS, Dreyer BP. Use of a pictographic diagram to decrease parent dosing errors with infant acetaminophen: a health literacy perspective. Academic pediatrics. 2011;11(1):50–57. doi: 10.1016/j.acap.2010.12.007. [DOI] [PubMed] [Google Scholar]
- 18.Yin HS, Parker RM, Sanders LM, et al. Liquid Medication Errors and Dosing Tools: A Randomized Controlled Experiment. Pediatrics. 2016;138(4):e20160357. doi: 10.1542/peds.2016-0357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Weiss BD, Mays MZ, Martz W, et al. Quick assessment of literacy in primary care: the Newest Vital Sign. Ann Fam Med. 2005;3(6):514–522. doi: 10.1370/afm.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38(1):33–42. doi: 10.1016/s0738-3991(98)00116-5. [DOI] [PubMed] [Google Scholar]
- 21.Lee SYD, Bender DE, Ruiz RE, Cho YI. Development of an easy-to-use Spanish health literacy test. Health Services Research. 2006;41(4p1):1392–1412. doi: 10.1111/j.1475-6773.2006.00532.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Institute of Medicine. Race, Ethnicity, and Language Data: Standardization for Health Care Quality Improvement. National Academies Press; 2009. [PubMed] [Google Scholar]
- 23.Karliner LS, Napoles-Springer AM, Schillinger D, Bibbins-Domingo K, Perez-Stable EJ. Identification of limited English proficient patients in clinical care. J Gen Intern Med. 2008;23(10):1555–1560. doi: 10.1007/s11606-008-0693-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bethell CD, Read D, Stein REK, Blumberg SJ, Wells N, Newacheck PW. Identifying children with special health care needs: development and evaluation of a short screening instrument. Ambul Pediatr. 2002;2(1):38–48. doi: 10.1367/1539-4409(2002)002<0038:icwshc>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 25.Mixon AS, Myers AP, Leak CL, et al. Characteristics associated with post-discharge medication errors. Mayo Clin Proc. 2014;89(8):1042–1051. doi: 10.1016/j.mayocp.2014.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Williams MV, Davis T, Parker RM, Weiss BD. The role of health literacy in patient-physician communication. Fam Med. 2002;34(5):383–389. [PubMed] [Google Scholar]
- 27.Bailey SC, Pandit AU, Curtis LM, Wolf MS. Availability of Spanish prescription labels: a multi-state pharmacy survey. Med Care. 2009;47(6):707–710. doi: 10.1097/MLR.0b013e318195fd02. [DOI] [PubMed] [Google Scholar]
- 28.U.S. Pharmacopeial Convention. Prescription container labeling. USP 36 - NF 31. 2012 USP 36(General Chapter 17) [Google Scholar]
- 29.Tarn DM, Heritage J, Paterniti DA, Hays RD, Kravitz RL, Wenger NS. Physician communication when prescribing new medications. Archives of Internal Medicine. 2006;166(17):1855–1862. doi: 10.1001/archinte.166.17.1855. [DOI] [PubMed] [Google Scholar]
- 30.Lara M, Gamboa C, Kahramanian MI, Morales LS, Hayes Bautista DE. Acculturation and Latino health in the United States: a review of the literature and its sociopolitical context. Annu Rev Public Health. 2005;26:367–397. doi: 10.1146/annurev.publhealth.26.021304.144615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Reggi V, Balocco-Mattavelli R, Bonati M, et al. Prescribing information in 26 countries: a comparative study. Eur J Clin Pharmacol. 2003;59:263–270. doi: 10.1007/s00228-003-0607-1. [DOI] [PubMed] [Google Scholar]
- 32.Flores G, Abreu M, Tomany-Korman SC. Limited English proficiency, primary language at home, and disparities in children's health care: how language barriers are measured matters. Public Health Rep. 2005;120(4):418–430. doi: 10.1177/003335490512000409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yin HS, Dreyer BP, Moreira HA, et al. Liquid medication dosing errors in children: role of provider counseling strategies. Academic pediatrics. 2014;14(3):262–270. doi: 10.1016/j.acap.2014.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pusic MV, Ching K, Yin HS, Kessler D. Seven practical principles for improving patient education: Evidence-based ideas from cognition science. Paediatrics & child health. 2014;19(3):119. doi: 10.1093/pch/19.3.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shrank WH, Avorn J. Educating patients about their medications: the potential and limitations of written drug information. Health Affairs. 2007;26(3):731–740. doi: 10.1377/hlthaff.26.3.731. [DOI] [PubMed] [Google Scholar]