Abstract
Background
The aim of this study was to identify whether iliac vein compression syndrome (IVCS) is a risk factor for left-sided deep venous thrombosis (DVT) in hip fracture patients and the influence IVCS may have on the treatment of DVT.
Material/Methods
A retrospective study was carried out among 424 hip fracture patients admitted to our hospital from 2011 to 2016. Clinical data were analyzed, and all patients were classified into the DVT group and the non-DVT group based on plasmin D-Dimer concentration and results of Doppler ultrasound of the left lower limb. Also, a 50% intraluminal constriction of the left iliac vein in the venography image was considered as IVCS. Comparison of IVCS prevalence was made between the DVT group and the non-DVT group. Patients in the DVT group were further divided into the DVT+/IVCS+ group and the DVT+/IVCS− group to evaluate the influence IVCS may have on the treatment of DVT.
Results
There were 204 patients in the DVT group and 220 patients in the non-DVT group. No statistically significant differences were found regarding the mean age, sex distribution, fracture type, and accompanying risk factors between the two groups. A total of 70 patients (34.3%) were diagnosed with IVCS in the DVT group, while confirmed IVCS was found in 52 patients (23.6%) in the non-DVT group (P=0.02). Postoperatively, the incidence of symptomatic DVT in the DVT+/IVCS+ group and the DVT+/IVCS− group was 30.0% and 11.9%, respectively (P=0.002).
Conclusions
IVCS is an under-recognized risk factor for left-sided DVT in hip fracture patients. What’s more, anticoagulation alone is insufficient for the treatment of DVT when it is complicated with IVCS. More aggressive measures have to be taken to achieve a favorable outcome.
MeSH Keywords: Hip Fractures, Iliac Vein, May-Thurner Syndrome, Risk Factors, Venous Thrombosis
Background
Iliac vein compression syndrome (IVCS), also called May-Thurner syndrome or Cockett syndrome, commonly refers to the anatomic variant resulting in compression of the left common iliac vein by the overriding iliac artery [1]. In 1851, Virchow first described this anatomic variant when he observed a left-sided predominance of iliofemoral deep venous thrombosis (DVT) [2]. Later, several studies showed that this anatomic variant was observed in 22–32% of cadavers [3]. It was not until 1958 that May and Thurner established a detailed description of this syndrome by postulating that repetitive compression leads to the formation of “spurs” inside the affected iliac vein due to the proliferation of vascular endothelium [4]. Compromised venous flow caused by both extraluminal compression and intraluminal obstruction made the patient increasingly predisposed to form DVT in the left lower extremity.
Then in 1965, Cockett and Thomas further explored the field and described an acute phase of swelling and left-sided iliofemoral thrombosis as well as a chronic phase that results in chronic venous insufficiency in IVCS patients [5]. Despite its relatively high prevalence, most IVCS patients could remain asymptomatic for their entire lifetime partly due to the formation of venous collaterals in the pelvis [5]. However, prompt diagnosis of IVCS is still imperative to reduce inappropriate treatment and achieve a favorable outcome.
Like in the setting of IVCS, DVT formation is also a known complication in hip fracture patients, and it can bring about serious clinical problems, with pulmonary embolism (PE) as its life-threatening complication in the acute phase and post-thrombotic syndrome in the chronic phase [5]. Recently, some authors reported extensive left-sided DVT formation in orthopedic surgery patients with concomitant IVCS [6,7], but the exact influence of IVCS on DVT formation in hip fracture patients is not well established.
The aim of this study was to investigate whether IVCS is a risk factor for DVT in hip fracture patients and the influence IVCS may have on the treatment of DVT.
Material and Methods
The study protocol and amendments were approved by the institutional review board. This study was conducted on a consecutive series of old patients (>60 years) admitted to our hospital from January 2011 to March 2016 with hip fractures (fractures of femoral neck or trochanteric) who underwent hemiarthroplasty or closed reduction and intramedullary fixation. All patients signed the informed consent for the venographies (preoperative and postoperative) and participation in this research.
Since IVCS showed a remarkable left-sided predominance, we focused our study only on the left lower extremity. All patients with hip fracture in this study underwent lower limb contrast venography. Contrast venography is the benchmark for diagnosing DVT. The diagnosis is established based on the presence of a constant intraluminal filling defect on at least two projections. Exclusion criteria were as follow: pathologic fractures, patients who were contraindicated for contrast venography, patients who received contrast venography in the right leg only, and incomplete clinical data. DVT that has no symptoms, but is found only by screening, is labeled asymptomatic or incidental. DVT that has symptoms, such as pain and swelling, is labeled symptomatic DVT.
We included 424 patients in this study. The clinical data of the patients were reviewed, including clinical manifestations (especially lower extremity pain, swelling, and varicose veins), plasmin D-Dimer concentration, and Doppler ultrasound results. All patients in this study underwent contrast venography for confirmation of DVT and IVCS. Meanwhile, the state of the left iliac vein was obtained from venography imaging, and patients with a 50% intraluminal constriction were diagnosed with IVCS (Figure 1). Usually, multiple left-to-right pelvic collaterals represent the chronic stage of IVC (Figure 2). According to plasmin D-Dimer concentration and Doppler ultrasound results, all patients were classified into two groups: the DVT group (suspicious positive result) and the non-DVT group (confirmed negative result). Then, we further divided the patients in the DVT group into two subgroups: the DVT+/IVCS+ group and the DVT+/IVCS− group by contrast venography results.
Figure 1.
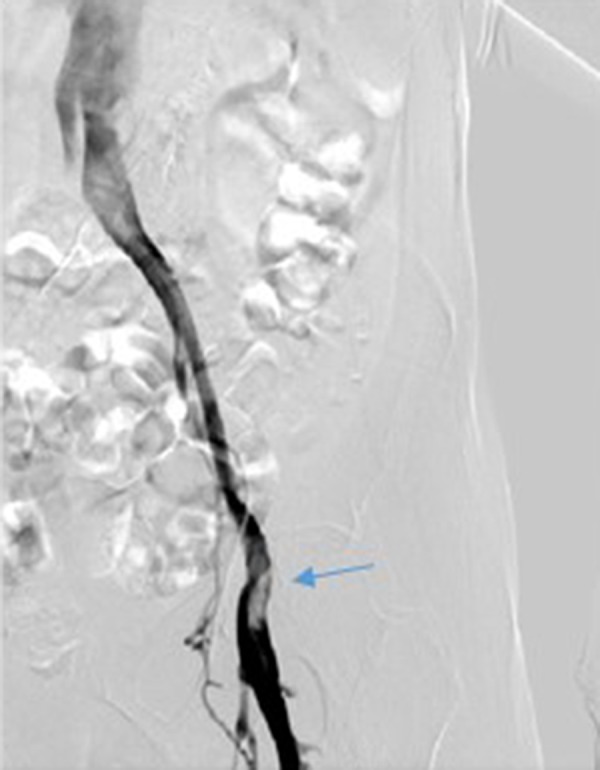
Venography demonstrates compression of the left iliac vein (arrowhead).
Figure 2.

Multiple left-to-right pelvic collaterals are presented, representing the chronic stage of iliac vein compression syndrome (IVCS).
All patients received low molecular weight heparin (LMWH) in a dose of 2500 U of dalteparin subcutaneously the morning after surgery and then 5000 U for 9 more days. All DVT patients were reexamined with contrast venography 7–10 days after surgery. Anticoagulation therapy was continued with rivaroxaban in patients with DVT at discharge.
Chi-square test was used for the analysis of categorical data, while the t-test was used for parametric data. For all tests, P<0.05 was considered statistically significant. All analyses were performed using SPSS for Windows, version 21.0 (SPSS, Chicago, Illinois, USA).
Results
There were 204 patients in the DVT group and 220 patients in the non-DVT group. As shown in Table 1, female patients in the two groups numbered 144 and 152, respectively (P=0.429). The mean age was 82.6 years (range, 75–93 years) for the DVT group and 81.1 years (range, 72–94 years) for the non-DVT group (P=0.642). There were 84 femoral neck fractures and 120 trochanteric fractures in the DVT group, while the corresponding data in the non-DVT group were 86 and 134 (P=0.374). A total of 180 patients in the DVT group had risk factors for developing DVT in addition to IVCS, including cardiovascular disease, smoking, immobilization (average time of hospitalization after injury), previous history of DVT, or malignancy; while in the non-DVT group, 191 patients had the above-mentioned risk factors (P=0.597). Hence, there were no statistically significant differences regarding the mean age, sex distribution, fracture type, and accompanying risk factors between the two groups (P>0.05).
Table 1.
Basic demographic data of patients.
| Variable | DVT group | Non-DVT group | P-value |
|---|---|---|---|
| No. of patients | 204 | 220 | – |
| Age (mean) | 82.6 | 81.1 | 0.642 |
| Sex (Male: Female) | 60: 144 | 68: 152 | 0.429 |
| Type of fractures (Neck: Trochanter) | 80: 120 | 86: 134 | 0.374 |
| Risk fators rate | 180/204 | 191/220 | 0.597 |
DVT – deep venous thrombosis.
According to contrast venography, 70 patients (34.3%) were diagnosed with IVCS in the DVT group, while confirmed IVCS was found in 52 patients (23.6%) in the non-DVT group (P=0.02) (Table 2). In addition, based on the contrast venography 7–10 days after surgery, the incidence of symptomatic DVT in the DVT+/IVCS+ group and the DVT+/IVCS− group was 30.0% and 11.9%, respectively (P=0.002) (Table 3).
Table 2.
Factor affecting the occurence of thrombosis.
| Variable | DVT group | Non-DVT group | OR 95% CI | P-value |
|---|---|---|---|---|
| IVCS+ | 70 | 52 | 1.69 (1.10–2.58) | 0.02 |
| IVCS− | 134 | 168 |
DVT – deep venous thrombosis; IVCS – iliac vein compression syndrome.
Table 3.
Symptomatic DVT rate after surgery in DVT group patients.
| Variable | DVT+/IVCS+ group | DVT+/IVCS− group | OR 95% CI | P-value |
|---|---|---|---|---|
| Symptomatic DVT+ | 21 | 16 | 3.16 (1.52–5.56) | 0.002 |
| Symptomatic DVT− | 49 | 118 |
DVT – deep venous thrombosis; IVCS – iliac vein compression syndrome.
Discussion
The current study clearly showed that IVCS serves as a risk factor for left-sided DVT in hip fracture patients (P=0.02, OR=1.69). This result was as previously estimated because IVCS and hip fracture share a common mechanism of thrombus formation, which is known as the classic triad of Virchow [8]: hypercoagulability, endothelial injury, and venous stasis. Concomitant IVCS put hip fracture patients at an even higher risk to develop DVT compared to hip fracture alone. Consequently, we recommend that greater attention should be paid to the status of the left iliac vein in hip fracture patients. In particular, acute formation of extensive iliofemoral thrombus in the left lower limb strongly suggests the existence of IVCS, making further diagnostic modalities necessary.
Overall, IVCS usually occurs in the second or third decade of life and is particularly prevalent in women [9]. The main risk factors for IVCS include prolonged immobilization, dehydration, abdomen lesions or surgery, contraceptive usage, or febrile illness [9]. Once symptoms occur, the patient can present either acutely or chronically; acute presentation of IVCS includes sudden onset of left lower extremity pain, swelling, and thrombus formation, while the chronic presentation of IVCS is varicose veins, skin pigmentation changes, ulcerations, chronic venous insufficiency, and venous claudication [10]. Once the patient is suspected to have IVCS, further examination should be implemented to reach a diagnosis.
Contrast venography remains the gold standard in diagnosing IVCS despite its various disadvantages [9]. To date, diagnostic imaging criteria for IVCS are not well established, but a few indicators of IVCS can be ascertained, including a compression greater than 50% in the luminal diameter, the presence of venous collaterals, intraluminal spurs formation, and greater than 2 mm Hg changes in hemodynamic flow across the stenotic region [11–13]. Contrast venography demonstrates the degree of iliac vein stenosis and can visualize pelvic venous collaterals. Venography also offers hemodynamic information about IVCS [9]. Other diagnostic techniques for IVCS include computed tomography (CT), magnetic resonance venography (MRV), and intravascular ultrasound (IVUS) [10].
In the current study, the postoperative symptomatic DVT rate in the DVT+/IVCS+ group was significantly higher than that in the DVT+/IVCS− group (P=0.002, OR=3.16), indicating that IVCS patients don’t respond well to anticoagulation therapy alone. A study showed that anticoagulation alone or removal of the thrombus with successive anticoagulation yielded a 73% recurrence of thrombosis in IVCS patients with venous spur formation [14,15]. Due to the mechanical nature of the obstruction in IVCS, anticoagulation or removal of the clot does not deal with the underlying cause of this disease (external compression and intraluminal constriction). Recently, endovascular management has been regarded as the first-line treatment for IVCS [16,17]. Thrombolysis with/without prophylactic retrievable inferior vena cava filter placement followed by angioplasty/stenting of the afflicted iliac vein appears to be the best option in IVCS patients with extensive DVT [9]. Anticoagulation with warfarin is recommended after the procedure.
Overall, the current study demonstrated that for left-sided DVT in hip fracture patients, IVCS is a risk factor that needs more attention and education. Further studies concerning the relationship between IVCS and right-sided or bilateral DVT are needed in the future. This study also showed the limitations of anticoagulation therapy alone in the treatment of DVT in IVCS patients. The optimal treatment of IVCS still needs to be further elucidated by future studies with patients who have a different clinical status. Thus, an interdisciplinary study should be carried out to achieve a better clinical outcome in the future. The effect of anticoagulant therapy in IVCS-positive DVT patients seems not good, so early detection of IVCS and preventive anticoagulation are necessary for the orthopedic surgeon.
Conclusions
IVCS is an under-recognized risk factor for left-sided DVT in hip fracture patients. What’s more, anticoagulation alone is insufficient for the treatment of DVT when it is complicated with IVCS. More aggressive measures have to be taken to achieve a favorable outcome.
Footnotes
Conflicts of interest
The authors declare no competing financial interests.
Source of support: This project is supported by the National Science Foundation of China (grant no. 81371950)
References
- 1.Mousa AY, AbuRahma AF. May-Thurner syndrome: Update and review. Ann Vasc Surg. 2013;27(7):984–95. doi: 10.1016/j.avsg.2013.05.001. [DOI] [PubMed] [Google Scholar]
- 2.Virchow R. Uber die Erweiterung kleiner Gefasse. Arch Path Anat. 1851;3(3):427–62. [in German] [Google Scholar]
- 3.Kibbe MR, Ujiki M, Goodwin AL, et al. Iliac vein compression in an asymptomatic patient population. J Vasc Surg. 2004;39(5):937–43. doi: 10.1016/j.jvs.2003.12.032. [DOI] [PubMed] [Google Scholar]
- 4.May R, Thurner J. The cause of the predominantly sinistral occurrence of thrombosis of the pelvic veins. Angiology. 1957;8(5):419–27. doi: 10.1177/000331975700800505. [DOI] [PubMed] [Google Scholar]
- 5.Cockett FB, Thomas ML. The iliac compression syndrome. Br J Surg. 1965;52(10):816–21. doi: 10.1002/bjs.1800521028. [DOI] [PubMed] [Google Scholar]
- 6.Reddy D, Mikhael MM, Shapiro GS, et al. Extensive deep venous thrombosis resulting from anterior lumbar spine surgery in a patient with iliac vein compression syndrome: A case report and literature review. Global Spine J. 2015;5(4):e22–e27. doi: 10.1055/s-0034-1396431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Foit NA, Chen QM, Cook B, et al. Iliofemoral deep vein thrombosis after tibial plateau fracture fixation related to undiagnosed May-Thurner syndrome: A case report. Patient Saf Surg. 2013;7(1):12. doi: 10.1186/1754-9493-7-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Virchow R. Neuer fall von todlicher emboli der kungerarteries. Arch Path Anat. 1856;10:225. [in German] [Google Scholar]
- 9.Donatella N, Marcello BU, Gaetano V, et al. What the young physician should know about May-Thurner syndrome. Transl Med UniSa. 2015;12:19–28. [PubMed] [Google Scholar]
- 10.Brinegar KN, Sheth RA, Khademhosseini A, et al. Iliac vein compression syndrome: Clinical, imaging and pathologic findings. World J Radiol. 2015;7(11):375–81. doi: 10.4329/wjr.v7.i11.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu Z, Gao N, Shen L, et al. Endovascular treatment for symptomatic iliac vein compression syndrome: A prospective consecutive series of 48 patients. Ann Vasc Surg. 2014;28(3):695–704. doi: 10.1016/j.avsg.2013.05.019. [DOI] [PubMed] [Google Scholar]
- 12.McDermott S, Oliveira G, Ergul E, et al. May-Thurner syndrome: Can it be diagnosed by a single MR venography study? Diagn Interv Radiol. 2013;19(1):44–48. doi: 10.4261/1305-3825.DIR.5939-12.1. [DOI] [PubMed] [Google Scholar]
- 13.O’Sullivan GJ, Semba CP, Bittner CA, et al. Endovascular management of iliac vein compression (May-Thurner) syndrome. J Vasc Interv Radiol. 2000;11(7):823–36. doi: 10.1016/s1051-0443(07)61796-5. [DOI] [PubMed] [Google Scholar]
- 14.Burroughs KE. New considerations in the diagnosis and therapy of deep vein thrombosis. South Med J. 1999;92(5):517–20. doi: 10.1097/00007611-199905000-00014. [DOI] [PubMed] [Google Scholar]
- 15.Rastogi N, Kabutey NK, Kim D. Incapacitating pelvic congestion syndrome in a patient with a history of May-Thurner syndrome and left ovarian vein embolization. Ann Vasc Surg. 2012;26(5):732–37. doi: 10.1016/j.avsg.2011.08.029. [DOI] [PubMed] [Google Scholar]
- 16.Hager ES, Yuo T, Tahara R, et al. Outcomes of endovascular intervention for May-Thurner syndrome. J Vasc Surg Venous Lymphat Disord. 2013;1(3):270–75. doi: 10.1016/j.jvsv.2012.11.002. [DOI] [PubMed] [Google Scholar]
- 17.Cil BE, Akpinar E, Karcaaltincaba M, et al. Case 76: May-Thurner syndrome. Radiology. 2004;233(2):361–65. doi: 10.1148/radiol.2332030152. [DOI] [PubMed] [Google Scholar]


