Highlights
-
•
The ideal reconstruction method for pancreaticoduodenectomy following a gastrectomy with Billroth II or Roux-en-Y is proposed.
-
•
Half patients in whom the past afferent limb was used for the reconstruction of the pancreaticojejunostomy and hepaticojejunostomy experienced afferent loop syndrome.
-
•
The Roux-en-Y method, using the distal intestine of previous gastrojejunostomy or jejunojejunostomy as a new jejunal limb for pancreaticojejunostomy and hepaticojejunostomy, may be a better reconstruction method to avoid afferent loop syndrome.
Keywords: Pancreaticoduodenectomy following gastrectomy, Roux-en-Y, Billroth II, Afferent loop syndrome
Abstract
Introduction
The ideal reconstruction method for pancreaticoduodenectomy following a gastrectomy with Billroth II or Roux-en-Y reconstruction is unclear. Methods: We reviewed a series of seven pancreaticoduodenectomies performed after gastrectomy with the Billroth II or Roux-en-Y method. Results: While preserving the existing gastrojejunostomy or esophagojejunostomy, pancreaticojejunostomy and hepaticojejunostomy were performed by the Roux-en-Y method using a new Roux limb in all cases. Four patients experienced postoperative complications, although the specific complications varied.
Discussion
A review of the literature revealed 13 cases of pancreaticoduodenectomy following gastrectomy with Billroth II or Roux-en-Y reconstruction. Three patients out of six (50%) in whom the past afferent limb was used for the reconstruction of the pancreaticojejunostomy and hepaticojejunostomy experienced afferent loop syndrome, while 14 previous and current patients in whom a new jejeunal limb was used did not experience this complication.
Conclusion
The Roux-en-Y method, using the distal intestine of previous gastrojejunostomy or jejunojejunostomy as a new jejunal limb for pancreaticojejunostomy and hepaticojejunostomy, may be a better reconstruction method to avoid the complication of afferent loop syndrome after previous gastrectomy with Billroth II or Roux-en-Y reconstruction if the afferent limb is less than 40 cm.
1. Introduction
The present work has been reported in line with the PROCESS criteria [1].
Although the frequency of gastric resection for gastric or duodenal ulcers and gastric cancer is decreasing [2], surgery is an important treatment option for severe ulcer diseases and all stages of gastric cancer. The frequency of pancreaticoduodenectomy (PD) is increasing, along with the rising number of pancreatic or periampullary tumors [2] and the improvement of surgical techniques. Therefore, the likelihood of performing PD in patients who previously underwent gastrectomy will continue to increase. However, PD following gastrectomy is a difficult task, because of adhesions and the varying anatomical structures of the remaining organs. Reconstruction of PD following gastrectomy reconstructed with the Billroth I (B-I) method can be performed similarly to a classical PD, except for the smaller remnant stomach [3], [4]. However, reconstruction of PD after Billroth II (B-II) or Roux-en-Y (R-Y) gastrectomy reconstruction needs special consideration regarding the bloodstream and length of the remnant intestine. This study retrospectively reviews our experience with PD following gastrectomy reconstructed with B-II or R-Y method, as well as perioperative complications.
2. Methods
We retrospectively reviewed all patients who had undergone PD between 2005 and 2015 at Kurashiki Central Hospital, in Okayama, Japan. Among 306 patients, 16 patients (5.2%) underwent gastrectomy before PD and seven of these (six males and one female) had their gastrectomy reconstructed with the B-II or R-Y method. We examined PD reconstruction and perioperative complications in this set of patients.
3. Results
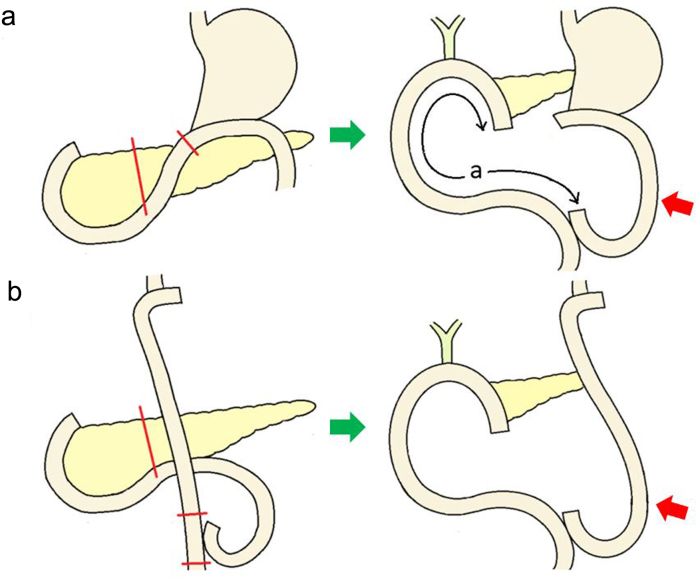
Patient characteristics, diagnoses for the preceding gastrectomy, indications for PD, and perioperative results are summarized in Table 1. Methods of reconstruction after PD are illustrated in Fig. 1. The median age of the patients in this case series was 75 years (range 65–82 years). The median BMI was 19.0 (range 16.1–23.4).
Table 1.
List of patients who underwent pancreaticoduodenectomy following gastrectomy with Billroth II or Roux-en-Y reconstruction.
| case | age | sex | BMI | gastrectomy |
pancreaticoduodenectomy |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| diagnosis | surgery | reconstruction | interval(yr) | diagnosis | operation time | blood loss | length* | postoperative hospital stay (days) |
complication | prognosis (months) |
||||
| 1 | 74 | M | 23.3 | gastric ulcer | distal | B-II | 36 | ca. of duodenal papilla | 367 | 974 | 50 | 116 | pancreatic fistula | 87/alive |
| 2 | 75 | M | 23.4 | gastric cancer | distal | B-II | 15 | IPMN | 267 | 349 | 50 | 29 | wound dehiscence | 63/alive |
| 3 | 77 | M | 22 | duodenal ulcer | distal | B-II | 27 | pancreatic cancer | 267 | 656 | 50 | 71 | ileus | 17/dead |
| 4 | 79 | M | 18.7 | gastric ulcer | distal | B-II | 45 | IPMN | 409 | 701 | 50 | 40 | pancreatic fistula | 13/alive |
| 5 | 65 | M | 16.1 | gastric cancer | total | R-Y | 2 | cholangiocancer | 359 | 1028 | 50 | 17 | none | 26/alive |
| 6 | 82 | F | 19 | gastric cancer | total** | R-Y | 4 | pancreatic cancer | 301 | 850 | 50 | 14 | none | 12/dead |
| 7 | 75 | M | 18.6 | gastric cancer | total | R-Y | 11 | pancreatic cancer | 324 | 1005 | 60 | 11 | none | 2/alive |
M: male, F: female, distal: distal gastrectomy, total: total gastrectomy, B-II: Billroth II reconstruction, R-Y: Roux-en-Y reconstruction.
IPMN: intraductal papillary mucinous neoplasm.
*The length of jejunum from pancreaticojejunostomy to jejunojejunostomy.
**Total gastrectomy with splenectomy.
All patients were reconstructed with modified Child method shown in Fig. 1.
Fig. 1.
Reconstruction of pancreaticoduodenectomy following gastrectomy with a Billroth II or a Roux-en-Y. While preserving the existing gastrojejunostomy or esophagojejunostomy, we used a new Roux limb for pancreaticojejunostomy and cholangiojejunostomy.(For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Red arrow: previous Roux limb.
The primary indication for gastrectomy was gastric cancer in four, gastric ulcer in two, and duodenal ulcer in one patient. Distal gastrectomy was performed in four patients and all were reconstructed with the B-II method. Three patients underwent total gastrectomy, reconstructed with the R-Y method.
Indications for PD included pancreatic cancer in three, intraductal papillary mucinous neoplasm (IPMN) in two, carcinoma of the duodenal papilla in one, and cholangiocarcinoma in one patient. The interval between the two operations ranged from 2 to 45 years (median 15 years).
Median surgical time for PD was 324 min (range 267–409 min) and intra-operative blood loss was 850 ml (range 349–1028 ml). The Modified Child method was chosen while preserving the existing GJ or EJ, and the R-Y method using a new Roux limb for pancreaticojejunostomy (PJ) and hepaticojejunostomy (HJ) was utilized in all cases. The length of jejunum from PJ to jejunojejunostomy (JJ) (Fig. 1a) was 50 cm in six cases and 60 cm in one case. Postoperative complications greater than Clavien–Dindo classification grade 3 occurred in four patients. Pancreatic fistulas greater than International Study Group of Postoperative Pancreatic Fistula grade B occurred in two patients, wound dehiscence in one patient, and ileus in one patient. Patients with pancreatic fistula were treated with antibiotics and percutaneous drainage. The patient with wound dehiscence needed the resuture at the bed side. The patient with ileus was treated with nasogastric and nasoenteric tubes. They all recovered without relaparotomy and surgical intervention. All patients were discharged and the median length of hospital stay after PD was 29 days (range 11–116 days). Two patients were dead during the follow up time because of the recurrence of the cancer.
4. Discussion
Performing PD in a patient with a history of gastrectomy, especially with the B-II or R-Y method, is a challenging task because of adhesions, varying anatomical structures, atypical vascular patterns, and length of the remnant intestine. We performed seven PD surgeries under these conditions. Surgical times and estimated blood loss volumes were acceptable in all cases. An average hospital stay of 29 days was also acceptable in Japan because under the Japanese insurance system, patients are generally allowed to stay in the hospital until they can live in their homes without professional support.
In the reconstruction of PD, we utilized the R-Y method using the distal intestine of the past GJ or JJ as a new jejunal limb, avoiding the use of the remnant afferent jejunum. When making a new jejunal limb, ischemia of the jejunum distal to the previous EJ or GJ (Fig. 1, red arrows) must be taken into consideration. Therefore, it is important to preserve at least one jejunal artery to this limb and check the bloodstream by clamping the marginal arteries before resection of the mesentery. Four complications greater than Clavien–Dindo grade 3 occurred, but none of them were related to ischemia of the preserved jejunum.
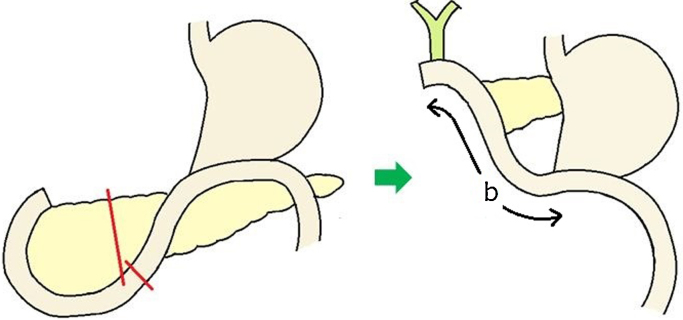
A PubMed search on May 2016 with the key words “pancreaticoduodenectomy” and “gastrectomy” revealed seven English-language reports [4], [5], [6], [7], [8], [9], [10] describing 13 cases of PD following gastrectomy reconstructed with the B-II or R-Y method. These cases are summarized in Table 2. In seven cases, the reconstruction of PD was similar to ours, preserving the existing GJ or EJ and performing PJ and HJ by the R-Y type method making a new jejunal limb. In the other six cases, the previous afferent limb was used for pancreatic and biliary reconstruction (Fig. 2). Interestingly, three patients out of six (50%) using the past afferent limb for the reconstruction of PD experienced afferent loop syndrome (ALS) while another 14 patients, including our patients, did not experience this complication. Afferent loop syndrome mostly develops after B-II reconstruction with gastrectomy [11], but also develops after PD [12]. The etiology of ALS is multifactorial, involving such factors as radiation enteropathy, markedly angulated or fixed afferent limb placement resulting in luminal obstruction, surgical technique, adhesions, and intestinal ischemia [12]. A short afferent limb and obstruction distal to the JJ caused by adhesions have been suggested to cause ALS [4] after PD following gastrectomy reconstructed with the B-II or R-Y method. Although the length of the afferent limb (Fig. 2, b) is not mentioned in all previously reported cases, two out of three ALS cases had only quite short afferent limbs. By using the remaining part of the afferent loop for PJ and HJ, we can reduce the number of intestinal anastomoses. However, when the afferent limb is short, torsion or kinking as a result of adhesion could occur, resulting in a luminal obstruction that can cause ALS. The determination the most appropriate length of afferent limb for PJ and HJ is difficult, but at least 50 cm is necessary, and we should not use the remnant afferent jejunum for the PJ and HJ if it is less than 50 cm, in order to avoid ALS.
Table 2.
List of reported patients who underwent pancreaticoduodenectomy following gastrectomy with Billroth II or Roux-en-Y reconstruction.
 |
Shaded cases indicate reconstruction using the previous afferent jejunal limb for pancreaticoduodenectomy and cholangiojejunostomy.
M: male, F: female, B-II: Billroth II reconstruction, R-Y: Roux-en-Y reconstruction, ALS: afferent loop syndrome, N/A: not available.
*Length of the new afferent limb (Fig. 2b) in shaded cases and jejunum from pancreaticojejunostomy to jejunojejunostomy in nonshaded cases (Fig. 1a).
**Pancreaticojejunostomy using the past afferent limb and cholangiojejunostomy using a new jejunal limb.
Fig. 2.
An example of reconstruction of pancreaticoduodenectomy using the past afferent limb for pancreatic and biliary reconstruction.
a: the length of the afferent limb.
5. Conclusion
To the best of our knowledge, there have been no previous English reports concerning the reconstruction following PD in patients who have previously undergone distal gastrectomy with Billroth II or Roux-en-Y reconstruction. The Roux-en-Y method, using the distal intestine of previous gastrojejunostomy or jejunojejunostomy as a new jejunal limb for pancreaticojejunostomy and hepaticojejunostomy, may be a better reconstruction method to avoid the complication of afferent loop syndrome for those patients if the afferent limb is less than 50 cm. However, the number of cases is small. Sufficient size study is necessary to establish a standard reconstruction procedure for these conditions.
Conflict of interest statement
The authors have no conflicts of interest.
Consent
Written informed consent was obtained from the patient for publication of this case series.
Authors contributions
Yusuke Kawamoto, Yusuke Ome, Taebum Park, and Kazuyuki Kawamoto performed the operation. Yusuke Kawamoto wrote the manuscript, Yusuke Koda and Kennichi Saga collected the data, while Yusuke Ome and Kazuyuki Kawamoto critically revised it.
Funding
None.
Ethical approval
Ethical approval not required.
Registration of research studies
2065
Guarantor
Yusuke Kawamoto.
Contributor Information
Yusuke Kawamoto, Email: y1q8roqdf14@gmail.com.
Yusuke Ome, Email: yo14408@kchnet.or.jp.
Yusuke Kouda, Email: yuusuke-k@n.vodafone.ne.jp.
Kennichi Saga, Email: ks13108@kchnet.or.jp.
Taebum Park, Email: tp8713@kchnet.or.jp.
Kazuyuki Kawamoto, Email: kk7159@kchnet.or.jp.
References
- 1.Agha R.A., Fowler A.J., Rammohan S., Barai I. Orgill DP and the PROCESS group. the PROCESS statement: preferred reporting of case series in surgery. Int. J. Surg. 2016;36(Pt A):319–323. doi: 10.1016/j.ijsu.2016.10.025. [DOI] [PubMed] [Google Scholar]
- 2.Katanoda K., Hori M., Matsuda T., Shibata A., Nishino Y., Hattori M., Soda M., Ioka A., Sobue T., Nishimoto H. An updated report on the trends in cancer incidence and mortality in Japan, 1958–2013. Jpn. J. Clin. Oncol. 2015;45:390–401. doi: 10.1093/jjco/hyv002. [DOI] [PubMed] [Google Scholar]
- 3.Oida T., Mimatsu K., Kawasaki A., Kano H., Kuboi Y., Amano S. Reconstruction following pancreaticoduodenectomy for patients who have previously undergone partial gastrectomy. Hepatogastroenterology. 2010;57:149–154. [PubMed] [Google Scholar]
- 4.Doi R., Fujimoto K., Imamura M. Effects of preceding gastrectomy on the outcome of pancreatoduodenectomy. J. Gastrointest. Surg. 2004;8(5):575–579. doi: 10.1016/j.gassur.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 5.Noguchi K., Okada K., Kawamura H., Ishizu H., Homma S., Kataoka A. Operative procedure for pancreatoduodenectomy in a patient who had previously undergone total gastrectomy, distal pancreatectomy, and splenectomy. Am. Surg. 2012;78(2):103–105. [PubMed] [Google Scholar]
- 6.Oida T., Kano H., Mimatsu K., Kawasaki A., Kuboi Y., Fukino N., Kida K., Amano S. Jejunal scarf-covering method in pancreaticojejunostomy after total gastrectomy. Case Rep. Gastroenterol. 2012;6:472–477. doi: 10.1159/000341520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yokoyama S., Sekioka A., Ueno K., Higashide Y., Okishio Y., Kawaguchi N., Hagihara T., Yamada H., Kamimura R., Kuwahara M., Ichimiya M., Utsunomiya H., Uyama S., Kato H. Pancreaticoduodenectomy following total gastrectomy: a case report and literature review. World J. Gastroenterol. 2014;20(10):2721–2724. doi: 10.3748/wjg.v20.i10.2721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mizuno S., Isaji S., Ohsawa I., Kishiwada M., Hamada T., Usui M., Sakurai H., Tabata M. Pancreaticoduodenectomy with resection of the splenic artery and splenectomy for pancreatic double cancers after total gastrectomy. Preservation of the pancreatic function via the blood supply from the posterior epiploic artery: report of a case. Surg. Today. 2012;42:482–488. doi: 10.1007/s00595-011-0018-3. [DOI] [PubMed] [Google Scholar]
- 9.Paolo B., Lorenzo D. Reconstructive strategy after pancreaticoduodenectomy in partially gastrectomized patients. J. Pancreas. 2015;16(2):198–200. doi: 10.6092/1590-8577/2956. [DOI] [PubMed] [Google Scholar]
- 10.Yun S., Choi D. Pancreaticoduodenectomy in patients with a history of total gastrectomy for stomach cancers. Int. Surg. 2014;99:71–76. doi: 10.9738/INTSURG-D-13-00071.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bolton J.S., Conway W.C., 2nd Postgastrectomy syndromes. Surg. Clin. North Am. 2011;91:1105. doi: 10.1016/j.suc.2011.07.001. [DOI] [PubMed] [Google Scholar]
- 12.Pannala R., Brandabur J., Gan S., Gluck M., Irani S., Patterson D.J., Ross A.S., Dorer R., Traverso L.W., Picozzi V.J., Kozarek R.A. Afferent limb syndrome and delayed GI problems after pancreaticoduodenectomy for pancreatic cancer: single-center, 14-year experience. Gastrointest. Endoscopy. 2011;74(2):295–302. doi: 10.1016/j.gie.2011.04.029. [DOI] [PubMed] [Google Scholar]