Abstract
Backgrounds
The association of dietary vitamin C (vit C) on periodontitis requires more valid evidence from large representative samples to enable sufficient adjustments. This study aimed to evaluate the association between dietary vit C intake and periodontitis after controlling for various confounders in the representative Korean adult population
Method
A total of 10,930 Korean adults (≥19 years) from the fourth Korean National Health and Nutrition Examination Survey data set were included in this cross-sectional study. Periodontitis was defined as community periodontal index score of 3 or 4. Dietary vit C intake was estimated from a 24-hour dietary record, and categorized into adequate and inadequate according to the Korean Estimated Average Requirement value. Potential confounders included age, sex, income, frequency of tooth brushing, use of floss, dental visit, drinking, smoking, diabetes, hypercholesterolemia, hypertension, and obesity. A multivariable logistic regression analysis and stratified analysis were applied.
Results
Those with inadequate dietary vit C intake were more likely by 1.16 times to have periodontitis than those with adequate dietary vit C intake (adjusted odds ratio [aOR] = 1.16, 95% confidence interval = 1.04–1.29). Lowest and middle-low quartile of dietary vit C intake, compared to highest quartile of dietary vit C intake, showed significant association (aOR = 1.28 and 1.22 respectively), which was in a biological-gradient relationship (trend-p <0.05).
Conclusions
Our data showed that inadequate dietary vit C intake was independently associated with periodontitis among Korean adults. Hence, adequate intake of dietary vitamin C could be substantially important on the promotion of periodontal health among Korean adults.
Introduction
Periodontitis is a specific inflammatory response to periodontal microorganisms which result in the destruction of the periodontal ligament and bone [1]. Periodontitis is a multifactorial disease and the risk factors for periodontitis include age, sex, socioeconomic status [2], and smoking [3]. Moreover, recent Korean data showed that cardiovascular diseases and metabolic syndrome were also related to periodontitis [4–6]. Periodontitis is prevalent among Korean adults, showing the prevalence range of 10.2% to 55.7% across different age groups [7].
The excessive production of reactive oxygen species (ROS) or reduced antioxidant levels has been associated with periodontitis [8,9]. For the scavenging of excessive ROS, many kinds of antioxidants are needed in our body and vitamin C (vit C) is one of important dietary antioxidants which has been associated with periodontal health [10]. Java prospective study showed controversial results: non-fasting serum vit C increased the incidence of periodontitis for three-year follow-up (2002–2005) [11]. However, fasting serum vit C did not increased the incidence of periodontitis for six-year intervention (2005–2011) [12]. Some used serum vit c [13,14,16–19] and some used dietary vit c [15, 20]. Although Clark et al. [21] who reported no association of dietary vit C with periodontitis from a longitudinal study among pregnant women suggested some more longitudinal epidemiological researches, few study could be found.
Moreover, most of studies had limitations such as small sample size [11–14] or lack of adjustment for systemic health-related confounders [16]. Hence, studies with large representative sample and adjustment for potential confounders are needed. Moreover, no study has addressed the association between vit C intake and periodontitis with enough adjustment for potential confounders among Korean adults.
The fourth Korean National Health and Nutrition Examination Survey (KNHANES Ⅳ) has provided information about dietary vit C intake, periodontitis and systemic factors. This study using KNHANES Ⅳ data set aimed to evaluate the association between dietary vit C intake and periodontitis after controlling for age, sex, income, frequency of tooth brushing, use of dental floss, dental visit, alcohol drinking, smoking, diabetes, hypercholesterolemia, hypertension, and obesity in a representative Korean adult population
Materials and methods
Study design and participants
KNHANES is representative of the Korean civilian, non-institutionalized population. KNHANES Ⅳ was a cross-sectional survey conducted by the Korea Center for Disease Control and Prevention (KCDCP) from 2007 to 2009. All participants provided a written informed consent for voluntary participation. The three-stage, stratified, clustered sampling method were used and unequal weight, of which the sum was 100%, was given to each individual. The total participants for KNHANES IV were 24,871. The inclusion criteria of this study were: 1) adult aged over 19 years, 2) those with valid periodontal examination data without edentulous status, 3) participants without missing variables. Among a total of 18,406 participants who were aged 19 years or more, 16,279 participants took periodontal examination and were not edentulous, and 14,227 participants had valid nutrition data. Finally, 10,930 participants who had no missing variable joined in the final analysis.
Assessment of periodontitis
The periodontal status was evaluated by community periodontal index (CPI) developed by World Health Organization (WHO) [22]. Ten index teeth, which are two molars in each posterior sextant, and the upper right and lower left central incisors, were measured for periodontal pocket depth by using a CPI probe (Osung MND, Seoul, Korea) at six sites per tooth (mesio-buccal, mid-buccal, disto-buccal, mesio-lingual, mid-lingual, disto-lingual). Probing was conducted by dentists who had received calibration training. Five CPI scores were recorded: normal gingiva (CPI 0), bleeding on probing (CPI 1), presence of gingival calculus (CPI 2), shallow periodontal pocket of 3.5–5.5mm (CPI 3) and deep periodontal pocket of 5.5 mm or more (CPI 4). Periodontitis was defined as CPI scores of 3 or 4 and participants were classified into two groups: non-periodontitis and periodontitis. The inter-examiner means of the Kappa value for CPI were 0.72 (0.69~0.77) in 2007, and 0.89 (0.55~1.00) in 2008 and 0.75 (0.53~0.94) in 2009 [23].
Assessment of vitamin C intake
Dietary food intake information was estimated by using a 24-hour dietary record (24-hDR) of the day before examination with interview using questionnaires [24,25]. The daily food intake was calculated and converted into an estimate of daily vit C intake using the standard food nutrient composition database and calculation formula guideline of Korean Nutrition Society (KNS) [26]. The Estimated Average Requirement (EAR), one of the Dietary Reference Intakes (DRI), is defined as the nutrient values estimated to meet the nutrient requirements in 50% of the healthy individuals in certain life stage and sex group, while the other remaining 50% are in inadequate state [27, 28]. The cut-off value of vit C by EAR is 75 mg/day for Korean adults [26]. Whereas, the Recommended Nutrient Intake (RNI) is the daily intake level of nutrients to meet the requirement of nearly all (97–98%) individuals. The cut-off value of vit C by RNI is 100 mg/day for Korean adults [26]. The amount of dietary vit C intake was categorized into adequate and inadequate according to EAR value and quartile value. For the quartile values, dietary vit C intake was classified into the four category; Highest (≥132.22 mg/day), Middle high (80.18 to <132.22 mg/day), Middle low (47.34 to <80.18 mg/day) and Lowest (<47.34 mg/day) in the overall sample.
Assessment of confounders
Since vitamin C is associated with various confounders including age, sex, education, smoking, alcohol consumption, obesity and physical activity [29], selected potential confounders included socio-demographic factors such as age, sex and income, oral health behaviors such as tooth brushing, use of floss, and dental visit, behavioral factors such as alcohol drinking and lifetime smoking and systemic factors such as diabetes mellitus, hypercholesterolemia, hypertension and obesity. The socio-demographic, oral health behaviors and behavioral factors were surveyed with questionnaires in an interview. The general health-related factors were assessed not only by questionnaires but clinical examination and laboratory procedures.
Age was classified into seven groups: 19 to 29, 30 to 39, 40 to 49, 50 to 59, 60 to 69 and 70 years or more. The monthly house hold income which is adjusted for the family number classified into quartiles groups according to monthly household income: the lowest, middle-low, middle-high, and the highest. Frequency of tooth brushing was classified into three categories: once or no per day, two times per day, and over three times per day. Use of floss was grouped into yes or no. Dental visit were classified into four categories: until the last 6 months, over 6 months to two years, over two years, and unknown. Alcohol drinking frequency in the last one year was categorized into 4 groups: 0–1time per month, 2–4 times per month, 2–3 times per week, 4 or more times per week. Lifetime smoking was categorized into three groups: No, below 5 packs (<100 cigarettes) and 5 packs or more (≥100 cigarettes). Diabetes was classified into three groups: diabetes for fasting blood sugar (FBS) ≥126 mg/dl or diagnosed or medicated for diabetes, pre-diabetes for 100≤FBS<126mg/dl and normal for FBS<100mg/dl. Hypercholesterolemia was classified into two groups: hypercholesterolemia for Total Cholesterol ≥240 mg/dl or on lipid-lowering medication and normal for Total Cholesterol <240 mg/dl. Hypertension was classified into three groups: hypertension for systolic blood pressure (SBP) ≥140mmHg or diastolic blood pressure (DBP) ≥90mmHg or on anti-hypertensive medication, pre-hypertensive for 120≤SBP<140mmHg or 80≤DBP<90mmHg, and normal for SBP<120mmHg and DBP<80mmHg. Obesity was classified into three statuses according to body mass index (BMI): normal for 18.5kg/m2 ≤ BMI <25kg/m2, underweight for BMI<18.5kg/m2, and obese for BMI ≥ 25kg/m2.
Statistical analysis
For the characteristics of the participants by periodontitis status, Chi-square test of complex sample analysis with weight application was performed to estimate the weighted proportions (95% confidence interval [CI]) of the total population sample. Crude associations between independent categorical variables and periodontitis were calculated by un-weighted chi-square test.
Multiple logistic regression analysis of complex sample analysis with applying weight was performed to evaluate the adjusted association between dietary vit C intake (EAR-defined, quartile) and periodontitis. Model 1 was analyzed by EAR value, whereas Model 2 was analyzed by quartile value of dietary vit C intake to confirm whether dietary vit C intake has biological-gradient relationship for periodontitis. Stratified analysis according to age group and sex was performed to reduce the positive bias due to the big sample with over 10,000 participants.
To evaluate the risk groups according to confounding variables, the subsequent stratified analysis among adults aged 30–49 years was performed. In the subsequent stratified analysis, we combined categories (pre-diabetes and diabetes for diabetes stratum, low and low middle for income stratum) to ensure adequate sample size. Moreover, we added the analysis of the association between RNI defined vit C intake and periodontitis among adults aged 30–49 years for more sensitive analysis. We used SPSS package (version 21, IBM, SPSS Inc., Chicago IL.USA) for data analysis.
Results
Characteristics of the participants
The prevalence of periodontitis in adults was 32.0% in our data. Periodontitis was more prevalent among elders, males, those with less vit C intake, lower income, frequent alcohol drinkers, heavy smokers, less tooth brushing, non-use of floss, diabetes, hypercholesterolemia, hypertension and obesity (Table 1).
Table 1. Characteristics of the participants by periodontitis status (N = 10,930).
| Variables | Category | N | Periodontitis* | P value† | |||
|---|---|---|---|---|---|---|---|
| No | Yes | ||||||
| N | % (95% CI) † | N | % (95% CI) † | ||||
| Total | 10930 | 7118 | 68.0 (66.5–69.6) | 3812 | 32.0 (30.4–33.5) | ||
| Age groups (years) | 19–29 | 1515 | 1403 | 92.7 (90.8–94.2) | 112 | 7.3 (5.8–9.2) | <0.001 |
| 30–39, | 2529 | 2047 | 79.5 (77.0–81.8) | 482 | 20.5 (18.2–23.0) | ||
| 40–49 | 2378 | 1497 | 59.8 (57.1–62.5) | 881 | 40.2 (37.5–42.9) | ||
| 50–59 | 1875 | 945 | 48.7 (45.6–51.9) | 930 | 51.3 (48.1–54.4) | ||
| 60–69 | 1614 | 754 | 43.8 (40.3–47.5) | 860 | 56.2 (52.5–59.7) | ||
| ≥70 | 1019 | 472 | 44.1 (39.9–48.3) | 547 | 55.9 (51.7–60.1) | ||
| Sex | Male | 4864 | 2736 | 62.0 (60.0–64.0) | 2128 | 38.0 (36.0–40.0) | <0.001 |
| Female | 6066 | 4382 | 75.1 (73.4–76.7) | 1684 | 24.9 (23.3–26.6) | ||
| Monthly household Income | Lowest | 1940 | 1030 | 58.3 (54.9–61.6) | 910 | 41.7 (38.4–45.1) | <0.001 |
| Middle low | 2674 | 1664 | 65.5 (63.0–68.0) | 1010 | 34.5 (32.0–37.0) | ||
| Middle high | 3093 | 2085 | 68.3 (66.1–70.5) | 1008 | 31.7 (29.5–33.9) | ||
| Highest | 3223 | 2339 | 73.7 (71.3–75.9) | 884 | 26.3 (24.1–28.7) | ||
| Frequency of tooth brushing | Once or no | 1365 | 756 | 58.3 (54.9–61.6) | 609 | 41.7 (38.4–45.1) | <0.001 |
| Twice | 4590 | 2846 | 64.9 (62.8–66.9) | 1744 | 35.1 (33.1–37.2) | ||
| Over 3 times | 4975 | 3516 | 73.0(71.2–74.7) | 1459 | 27.0 (25.3–28.8) | ||
| Use of floss | No | 9532 | 6000 | 66.2 (64.5–67.8) | 3532 | 33.8 (32.2–35.5) | <0.001 |
| Yes | 1398 | 1118 | 80.1 (77.4–82.6) | 280 | 19.9 (17.4–22.6) | ||
| Dental visit | No | 342 | 229 | 71.1 (64.9–76.7) | 113 | 28.9 (23.3–35.1) | <0.001 |
| 6 months | 2999 | 1929 | 66.8 (64.5–68.9) | 1070 | 33.2 (31.1–35.5) | ||
| 6 m to 2 years | 3867 | 2592 | 70.1 (68.0–72.1) | 1275 | 29.9 (27.9–32.0) | ||
| Over 2 years | 3705 | 2355 | 66.7 (64.4–68.9) | 1350 | 33.3 (31.1–35.6) | ||
| Unknown | 17 | 13 | 74.4 (43.4–91.7) | 4 | 25.6 (8.3–56.6) | ||
| Alcohol Drinking (time) | 0–1/month | 5591 | 3741 | 70.1 (68.2–71.9) | 1850 | 29.9 (28.1–31.8) | <0.001 |
| 2–4/month | 2713 | 1881 | 72.3 (69.9–74.5) | 832 | 27.7 (25.5–30.1) | ||
| 2–3/week | 1717 | 1068 | 64.9 (62,0–67.6) | 649 | 35.1 (32.4–38.0) | ||
| ≥4/week | 909 | 428 | 48.2 (43.9–52.4) | 481 | 51.8 (47.6–56.1) | ||
| Lifetime smoking | No | 6159 | 4424 | 75.4 (73.6–77.0) | 1735 | 24.6 (23.0–26.4) | <0.001 |
| <5pack | 309 | 232 | 80.3 (74.6–85.0) | 77 | 19.7 (15.0–25.4) | ||
| ≥5packs | 4462 | 2462 | 59.5 (57.4–61.6) | 2000 | 40.5 (38.4–42.6) | ||
| Diabetes‡ | Normal | 7981 | 5598 | 72.9 (71.3–74.4) | 2383 | 27.1 (25.6–28.7) | <0.001 |
| Pre-diabetes | 1999 | 1081 | 56.1 (53.0–59.1) | 918 | 43.9 (40.9–47.0) | ||
| Diabetes | 950 | 439 | 45.5 (41.4–49.7) | 511 | 54.5 (50.3–58.6) | ||
| Hypercholesterolemia§ | No | 9818 | 6501 | 69.2 (67.6–70.7) | 3317 | 30.8 (29.3–32.4) | <0.001 |
| Yes | 1112 | 617 | 56.6 (52.9–60.3) | 495 | 43.4 (39.7–47.1) | ||
| Hypertension║ | Normal | 5341 | 3948 | 75.7 (73.9–77.3) | 1393 | 24.3 (22.7–26.1) | <0.001 |
| Prehypertension | 2684 | 1665 | 66.1 (63.4–68.6) | 1019 | 33.9 (31.4–36.6) | ||
| Hypertension | 2905 | 1505 | 53.1 (50.4–55.9) | 1400 | 46.9 (44.1–49.6) | ||
| Obesity¶ | Normal | 7031 | 4701 | 70.1 (68.4–71.8) | 2330 | 29.9 (28.2–31.6) | <0.001 |
| Underweight | 512 | 386 | 78.0 (73.7–81.8) | 126 | 22.0 (18.2–26.3) | ||
| Obese | 3387 | 2031 | 62.3 (59.9–64.6) | 1356 | 37.7 (35.4–40.1) | ||
| Dietary vitamin C (EAR)# | Adequate | 5869 | 3895 | 68.5 (66.7–70.4) | 1974 | 31.5 (29.6–33.3) | <0.05 |
| Inadequate | 5061 | 3223 | 67.4 (65.5–69.3) | 1838 | 32.6 (30.7–34.5) | ||
| Quartile diet vitamin C** | Highest | 2732 | 1847 | 70.2 (67.8–72.4) | 885 | 29.8 (27.6–32.2) | <0.05 |
| Middle high | 2733 | 1792 | 67.6 (65.2–70.0) | 941 | 32.4 (30.0–34.8) | ||
| Middle low | 2733 | 1763 | 66.8 (64.4–69.1) | 970 | 33.2 (30.9–35.6) | ||
| Lowest | 2732 | 1716 | 67.5 (65.1–69.8) | 1016 | 32.5 (30.2–34.9) | ||
*Periodontitis was defined as community periodontal index 3–4.
†Weighted percent, 95% Confidence Interval (CI), and p-value obtained by Chi-square test.
‡Diabetes: Normal; (FBS) <100mg/dl, pre-diabetes; 100≤FBS≤125mg/dl, Diabetes; (FBS) ≥126mg/dl or on anti-diabetic medicine or insulin injection or on diagnose by doctor.
§Hypercholesterolemia: Fasting Total Cholesterol (FTC) ≥ 240 mg/dl or anti-cholesterol drug.
║Hypertension: Normal; systolic blood pressure (SBP) <120mmHg and diastolic blood pressure (DBP) <80mmHg, Pre-hypertension; 120≤ SBP <140mmHg or: 80≤ DBP <90mmHg, Hypertension; SBP ≥140mmHg, or DBP ≥90mmHg or anti-hypertensive medicine.
¶Obesity; Normal; Body Mass Index (BMI) 18.5 to <25, Underweight: BMI <18.5, and Obesity: BMI ≥25.0 kg/m2.
#Dietary vitamin C; Adequate: ≥75mg/day and Inadequate: <75mg/day by estimated average requirement (EAR).
**Quartile diet vit C; Highest (≥132.22 mg/day), middle high (80.18 to <132.22 mg/day), middle low (47.34 to <80.18 mg/day) and Lowest (<47.34 mg/day).
Association between dietary vit C intake and periodontitis in overall sample
EAR-defined dietary vit C intake was significantly associated with periodontitis after controlling for all the possible confounders (Table 2). Those with inadequate intake of dietary vit C were more likely to have periodontitis by 1.16 times than those with adequate intake of dietary vit C. Especially, quartile dietary vit C intake was also associated with periodontitis. Lowest and middle-low quartile of dietary vit C intake, compared to highest quartile of dietary vit C intake, showed significant association of 1.28 times and 1.22 times respectively, which was in a biological-gradient relationship (trend-p <0.05). Our data showed that age, sex and income, use of floss, and dental visit, alcohol drinking and lifetime smoking and diabetes mellitus were also significantly associated with periodontitis. Generally, Koreans visit dental office for dental treatment rather than regular check-up. Especially, those who visit the dental office were more likely to have periodontitis by 1.4–1.5 times than those who did not visit the dental office.
Table 2. Adjusted association between dietary vitamin C and periodontitis (N = 10,930).
| Variable | Subgroups | N | Odds ratio* (95% Confidence Interval) | |
|---|---|---|---|---|
| Model 1 | Model 2 | |||
| Dietary vitamin C† | Adequate | 5869 | 1 | |
| Inadequate | 5061 | 1.161 (1.042–1.294) | ||
| Quartile values‡ | Highest | 2732 | 1 | |
| Middle high | 2733 | 1.120 (0.973–1.289) | ||
| Middle low | 2733 | 1.225 (1.054–1.423) | ||
| Lowest | 2732 | 1.282 (1.099–1.497) | ||
| (Trend-p = 0.012) | ||||
| Age groups | 19–29 | 1515 | 1 | 1 |
| 30–39 | 2529 | 3.321 (2.518–4.379) | 3.325 (2.520–4.388) | |
| 40–49 | 2378 | 8.519 (6.546–11.088) | 8.539 (6.561–11.114) | |
| 50–59 | 1875 | 12.581 (9.466–16.720) | 12.615 (9.491–16.767) | |
| 60–69 | 1614 | 13.329 (9.825–18.081) | 13.334 (9.822–18.101) | |
| 70 | 1019 | 12.216 (8.869–16.827) | 12.163 (8.818–16.776) | |
| Sex | Male | 4864 | 1 | 1 |
| Female | 6066 | 0.754 (0.644–0.884) | 0.750 (0.640–0.880) | |
| Monthly house Income | Low | 1940 | 1 | 1 |
| Middle-low | 2674 | 0.989 (0.832–1.177) | 0.991 (0.833–1.179) | |
| Middle-high | 3093 | 0.954 (0.795–1.145) | 0.958 (0.799–1.149) | |
| High | 3223 | 0.713 (0.584–0.871) | 0.717 (0.587–0.876) | |
| Tooth brushing | Once or no/day | 1365 | 1 | 1 |
| Twice /day | 4590 | 1.015 (0.863–1.194) | 1.017 (0.864–1.196) | |
| Over 3 times/day | 4975 | 0.908 (0.767–1.074) | 0.910 (0.769–1.076) | |
| Use of floss | No | 9532 | 1 | 1 |
| Yes | 1398 | 0.694 (0.583–0.827) | 0.696 (0.584–0.830) | |
| Dental visit | No visit | 342 | 1 | 1 |
| Last 6 months | 2999 | 1.517 (1.101–2.091) | 1.522 (1.105–2.097) | |
| Last 6 months to 2 years | 3867 | 1.408 (1.022–1.940) | 1.413 (1.025–1.947) | |
| Over last 2 years | 3705 | 1.485 (1.068–2.066) | 1.489 (1.071–2.071) | |
| Unknown | 17 | 1.607 (0.295–8.742) | 1.606 (0.294–8.778) | |
| Alcohol drinking | 0–1/month | 5591 | 1 | 1 |
| 2–4/month | 2713 | 1.024 (0.894–1.172) | 1.022 (0.893–1.171) | |
| 2–3/week | 1717 | 1.015 (0.866–1.189) | 1.007 (0.859–1.181) | |
| ≥4/week | 909 | 1.264 (1.033–1.548) | 1.262 (1.032–1.544) | |
| Lifetime Smoking | No | 6159 | 1 | 1 |
| <5packs | 309 | 0.899 (0.613–1.318) | 0.896 (0.611–1.312) | |
| ≥5packs | 4462 | 1.643 (1.400–1.928) | 1.639 (1.396–1.924) | |
| Diabetes | Normal | 7981 | 1 | 1 |
| Pre-diabetes | 1999 | 1.183 (1.037–1.350) | 1.184 (1.039–1.351) | |
| Diabetes | 950 | 1.359 (1.126–1.639) | 1.359 (1.126–1.639) | |
| Hypercholesterolemia | No | 9818 | 1 | 1 |
| Yes | 1112 | 1.044 (0.893–1.220) | 1.045 (0.895–1.221) | |
| Hypertension | Normal | 5341 | 1 | 1 |
| Prehypertension | 2684 | 1.047 (0.903–1.214) | 1.047 (0.903–1.214) | |
| Hypertension | 2905 | 1.036 (0.887–1.210) | 1.037 (0.888–1.211) | |
| Obesity | Normal | 7031 | 1 | 1 |
| Underweight | 512 | 1.159 (0.886–1.516) | 1.153 (0.881–1.508) | |
| Obese | 3387 | 1.096 (0.969–1.240) | 1.097 (0.970–1.241) | |
Periodontitis was defined as community periodontal index 3–4.
*Odds ratios in Model 1 and 2 are adjusted for age, sex, income, tooth brushing, use of floss, dental visit, alcohol drinking, smoking, diabetes, hypercholesterolemia, hypertension, and obesity.
† Dietary vitamin C; Adequate: ≥75mg/day and Inadequate: <75mg/day by Estimated Average Requirement value.
‡Quartile value; Highest (≥132.22 mg/day), middle high (80.18 to <132.22 mg/day), middle low (47.34 to <80.18 mg/day) and Lowest (<47.34 mg/day).
Bold denotes statistical significance at p〈0.05
Age and sex stratified association between EAR-defined dietary vit C and periodontitis
In the age stratified analysis, the association of inadequate intake of vit-C was highlighted among those aged 30–39 years (adjusted Odds Ratio [aOR] = 1.26, 95% confidence interval [CI] = 1.004–1.58) and 40–49 years (aOR = 1.36, 95% CI = 1.10–1.67), while those in other age groups were not statistically significant (Table 3). In terms of sex, the association was highlighted in females (aOR = 1.30, 95% CI = 1.12–1.51). In terms of age groups and sex, the link was highlighted among males aged 40–49 year group and females aged 30–39 and 40–49 years groups (Table 3). Of them, the link was the highest among females aged 30–39 years group (aOR = 1.62, 95% CI = 1.15–2.25).
Table 3. Age and sex stratified association of dietary vitamin C intake (inadequate against adequate) with periodontitis (N = 10,930).
| Stratum | Subgroup | N | Odds ratio* (95% confidence interval) |
|---|---|---|---|
| Age | 19–29 years | 1515 | 1.091 (0.681–1.749) |
| 30–39 years | 2529 | 1.260 (1.004–1.581) | |
| 40–49 years | 2378 | 1.361 (1.105–1.675) | |
| 50–59 years | 1875 | 1.048 (0.825–1.331) | |
| 60–69 years | 1614 | 1.034 (0.797–1.342) | |
| ≥70 years | 1019 | 0.922 (0.668–1.272) | |
| Sex | Male | 4864 | 1.054 (0.909–1.222) |
| Female | 6066 | 1.305 (1.123–1.516) | |
| Age and sex | |||
| Male | 19–29 years | 641 | 0.995 (0.514–1.925) |
| 30–39 years | 969 | 1.078 (0.784–1.483) | |
| 40–49 years | 998 | 1.408 (1.049–1.888) | |
| 50–59 years | 856 | 0.872 (0.626–1.216) | |
| 60–69 years | 835 | 0.921 (0.648–1.309) | |
| ≥70 years | 565 | 0.938 (0.607–1.449) | |
| Female | 19–29 years | 874 | 1.265 (0.689–2.323) |
| 30–39 years | 1560 | 1.615 (1.158–2.253) | |
| 40–49 years | 1380 | 1.303 (1.001–1.694) | |
| 50–59 years | 1019 | 1.271 (0.931–1.735) | |
| 60–69 years | 779 | 1.174 (0.827–1.666) | |
| ≥70 years | 454 | 0.964 (0.593–1.568) |
Periodontitis was defined as community periodontal index 3–4.
* Odds ratio of dietary vitamin C defined by EAR (Inadequate: [< 75mg/day] against the reference, Adequate: [≥75mg/day]) was adjusted for age, sex, income, frequency of tooth brushing, use of floss, dental visit, alcohol drinking, smoking, diabetes, hypercholesterolemia, hypertension, and obesity except for stratum
Bold denotes statistical significance at p〈0.05
Sensitivity of the link between dietary vit C and periodontitis among Korean adults aged 30 to 49 years
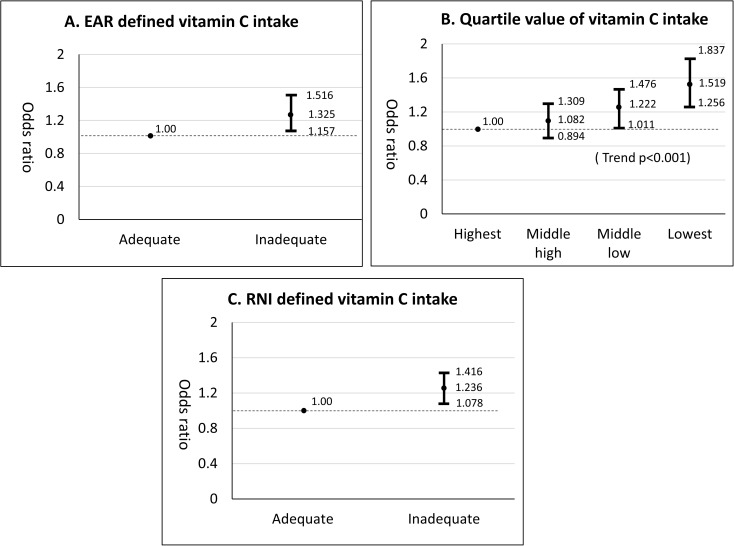
EAR-defined dietary vit C intake was associated with periodontitis among Korean adults aged 30 to 49 years (aOR = 1.33, 95% CI = 1.16–1.52) (Fig 1), which was confirmed by two other analyses, quartile dietary vit C intake and RNI-defined dietary vit C intake analyses. The association between quartile dietary vit C intake and periodontitis also showed a biological-gradient relationship (trend-p <0.05). Moreover, RNI-defined dietary vit C intake also showed a significant association with periodontitis (aOR = 1.24, 95% CI = 1.08–1.42).
Fig 1. Sensitivity of association between dietary vitamin C intake and periodontitis among Korean adults aged 30 to 49 years (N = 4907).
A. EAR defined vit C intake; B. Quartile vit C intake C.RNI defined vit C intake. Odds ratios were adjusted for age, sex, income, frequency of tooth brushing, use of floss, dental visit, drinking, smoking, diabetes, hypercholesterolemia, hypertension, and obesity. Dots indicate odds ratios, bars indicate 95% confidence intervals and the horizontal dotted line is the reference (odds ratio = 1).
Socio-behavioral-systemic factors stratified association between dietary vitamin C intake (inadequate against adequate) and periodontitis among Korean adults aged 30 to 49 years
Among adults aged 30–49 years, the link between EAR defined vit C intake (inadequate against adequate) and periodontitis was highlighted among those with middle or low income, drinking frequency of two to four times per month, no smoking, prediabetes or diabetes, prehypertension or hypertension (Table 4). Of them, the link was the highest among those with pre-diabetes or diabetes (aOR = 1.68, 95% CI = 1.26–2.23).
Table 4. Socio-behavioral-systemic factors stratified association between dietary vitamin C intake (inadequate against adequate) and periodontitis among adults aged 30–49 years (n = 4907).
| Subgroup | N | Odds ratio* (95% confidence interval) |
|---|---|---|
| Monthly house Income | ||
| <50% | 1381 | 1.339 (1.054–1.701) |
| 50–75% | 1744 | 1.376 (1.094–1.731) |
| >75% | 1782 | 1.293 (1.020–1.640) |
| Drinking (times/week or month) | ||
| 0–1/month | 2382 | 1.311 (1.069–1.608) |
| 2–4/month | 1364 | 1.458 (1.133–1.876) |
| ≥2/week | 1161 | 1.223 (0.941–1.589) |
| Lifetime cigarette smoking | ||
| No | 2893 | 1.376 (1.141–1.658) |
| Yes | 2014 | 1.255 (1.030–1.529) |
| Prediabetes or diabetes† | ||
| No | 3914 | 1.228 (1.053–1.433) |
| Yes | 993 | 1.677 (1.264–2.227) |
| Prehypertension or hypertension‡ | ||
| No | 2986 | 1.279 (1.069–1.530) |
| Yes | 1921 | 1.377 (1.120–1.693) |
| Obesity§ | ||
| No | 3484 | 1.300 (1.103–1.533) |
| Yes | 1423 | 1.322 (1.041–1.679) |
Periodontitis was defined as community periodontal index 3–4.
*Odds Ratio of dietary vitamin C defined by EAR (Inadequate [<75mg/day] against the reference, adequate [≥75mg/day]) was adjusted for age, sex, income, tooth brushing, use of floss, dental visit, alcohol drinking, smoking, diabetes, hypercholesterolemia, hypertension, and obesity except the subgroup.
†Prediabetes or diabetes: fasting blood sugar ≥ 100 mg/dl or on anti-diabetic medicine or insulin injection or on diagnosis by doctor.
‡Prehypertension or hypertension: systolic blood pressure (SBP) ≥120 mmHg, diastolic blood pressure (DBP) ≥80mmHg or anti-hypertensive medicine.
§Obesity: Body Mass Index (BMI) ≥25 m2/kg.
Bold denotes highlighted association with odds ratio more than 1.325 (non-stratified odds ratio in 30–49 years).
Discussion
Our data showed that the EAR-defined vit C intake was associated with periodontitis after controlling for potential confounders among Korean adults. Our data supports previous studies which found an inverse association between dietary vit C intake and periodontitis [15, 20]. It was speculated that our data also supported other serum or plasma vit c studies which showed a significant inverse association with periodontitis indirectly [11, 14, 16, 17, 19, 30]. Though some clinical studies failed to show effects of oral administration of additional vit C on reducing periodontitis [31–33], they demonstrated that excessive vit C does not have therapeutic benefit for periodontitis while inadequate intake of vit C could be harmful for periodontitis. To the best of our knowledge, this study is the first evidence that applied EAR as daily intake guideline for evaluating the association between dietary vit C intake and periodontitis.
The major strengths of this study are three-fold. Firstly, our data is a representative national data with a large sample size and information of various potential confounders, enabling multivariable analysis and stratified analysis. Secondly, the individual weighted factors were applied by using complex sample analysis. In multistage sampling design, when certain subgroups of the population are oversampled, the estimated association may be biased, and application of weight by complex sample analysis is recommended to attenuate this problem [34]. Finally, we applied the EAR to define dietary vit C intake. Moreover, we additionally applied quartile values and RNI for dietary vit C intake to evaluate a biological-gradient relationship and provide sensitive analysis of the link.
Our data showed that the association between dietary vit C intake and periodontitis was statistically significant among adults aged 30 to 49 years. Periodontitis is a chronic inflammatory disease with multiple risk factors. In young adults aged below 30 years, the prevalence of periodontitis is low, possibly due to the insufficient duration of time exposed to develop periodontitis. In contrast, older adults aged over 50 could have had more chance of multiple tooth extraction due to periodontitis than younger adults. Hence, the effect of inadequate dietary vit C intake on periodontitis could be masked and highlighted only among those aged 30 to 49 years. Further studies are needed to validate our finding that the link between dietary vit C intake and periodontitis is highlighted in those aged 30 to 49 years.
Our data did not show an association between dietary vit C intake and periodontitis among elders, which is different from a Japanese study conducted among elders [16]. It should be considered that the Japanese study was not fully adjusted for systemic factors. Our data showed that the link between vit C and periodontitis was highlighted in females which are in accordance with Dutch study [13]. Males generally have more periodontitis than females [35]. Hence, it is speculated that the effect of vit C on periodontitis could be masked in males due to other risk factors for periodontitis.
Hyperglycemia in diabetics can lead to development of oxidative stress [36]. Since periodontitis is also associated with oxidative stress [9], the scavenging of ROS by antioxidants such as ascorbic acid may be important for the prevention of periodontitis in diabetics and hence, vit C in diabetic adults could mean interdependent effect on developing periodontitis.
In the stratified analysis, the link between vit C and periodontitis was highlighted among those with low income, less 4 times drinking frequency per month, non-smokers, diabetes including pre-diabetes, hypertension including pre-hypertension, and obese individuals. It was reported that the proportion of Korean adults who does not had proper dental treatment was 24.5% for the highest income while those of the lowest, middle-low, middle-high were 34.3, 30.3 and 31.4% [37]. Since alcohol drinking [38,39], smoking [40] and hypertension [41] could be risk factors to periodontitis, the link between vit C deficiency and periodontitis could be masked among heavy drinkers, smokers and hypertensive. On the other hand, the link between vit-C and periodontitis was highlighted among diabetic individuals. Obesity and diabetes mellitus are associated with modulation of immune activity which results in higher susceptibility to infectious diseases such as periodontitis [42,43]. Hence, when there is inadequate intake of vit C, those with diabetes would be more sensitive to oxidative stress for developing periodontitis.
Some biological mechanisms have been suggested to explain how vit C could influence periodontitis. First, vit C is an intracellular antioxidant which scavenges free radicals and protect cells from oxidative stress [8]. Second, vit C functions as an essential co-factor for the hydroxylation of proline and lysine which is vital to collagen biosynthesis in connective tissue [25]. Last but not least, an in vitro study showed that vit C induced the osteogenic differentiation of periodontal ligament progenitor cells through ERK/MARK pathway [44]. Therefore, vit C could possibly stimulate stem cells to differentiate and enhance skeletomuscular development.
Our data has some limitations. Firstly, the cross-sectional study design could not infer the causal relationship between vit C and periodontitis. Thus our data require a longitudinal study for the incidence of periodontitis to infer the causality. Secondly, applying CPI for evaluating periodontitis might underestimate the periodontal prevalence by 50% or more due to partial mouth recordings protocols so there might be misclassification of periodontitis [45]. Thus, full mouth periodontal examination using CPI or clinical attachment loss (CAL) could have provided a more valid periodontitis classification. Thirdly, vit C intake by 24-hour recall method could be different from the actual dietary intake. In order to adjust for day-to-day variations, researchers are encouraged to average multiple 24-hour recall or use statistical approaching method [46,47]. Finally, this investigation did not consider seasonal variation in food intake, nutritional supplement, and number of teeth, respectively. Notwithstanding these limitations, our data is valid enough to address the association between vit C and periodontitis among Korean adults.
Conclusions
Our data showed that dietary vit C intake was independently associated with periodontitis among Korean adults. The link was in a biological-gradient relationship and highlighted in adults aged 30 to 49 years. Hence, adequate intake of dietary vitamin C could be substantially important on the promotion of periodontal health among Korean adults.
Supporting information
(DOC)
Acknowledgments
The authors declare no conflicts of interest. We acknowledge the Korea Centers for Disease Control and Prevention (KCDCP) which provided data of the Fourth Korea National Health and Nutrition Examination Survey (KNHANES Ⅳ) from 2007–2009 to be used in this study.
This work was supported by a grant from the National Research Foundation of Korea through the Oromaxillofacial Dysfunction Research Center for the Elderly (No. 2015–048003) at Seoul National University, Korea.
Abbreviations
- vit C
vitamin C
- EAR
estimated average requirement
- RNI
Recommended Nutrient Intake
Data Availability
Data are available from the Korea National Health and Nutrition Examination Survey database (https://knhanes.cdc.go.kr/knhanes/eng/index.do) for researchers who meet the criteria for access to confidential data.
Funding Statement
This work was supported by a grant from the National Research Foundation of Korea through the Oromaxillofacial Dysfunction Research Center for the Elderly (No. 2015-048003) at Seoul National University, Korea. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Bartold PM, Cantley MD, Haynes DR (2010) Mechanisms and control of pathologic bone loss in periodontitis. Periodontol 2000 53: 55–69. [DOI] [PubMed] [Google Scholar]
- 2.Genco RJ, Borgnakke WS (2013) Risk factors for periodontal disease. Periodontol 2000 62: 59–94. [DOI] [PubMed] [Google Scholar]
- 3.Gelskey SC (1999) Cigarette smoking and periodontitis: methodology to assess the strength of evidence in support of a causal association. Community Dent Oral Epidemiol 27: 16–24. [DOI] [PubMed] [Google Scholar]
- 4.Kim HD, Sim SJ, Moon JY, Hong YC, Han DH (2010) Association between periodontitis and hemorrhagic stroke among Koreans: a case-control study. J Periodontol 81: 658–665. doi: 10.1902/jop.2010.090614 [DOI] [PubMed] [Google Scholar]
- 5.Sim SJ, Kim HD, Moon JY, Zavras AI, Zdanowicz J, Jang S, et al. (2008) Periodontitis and the risk for non-fatal stroke in Korean adults. J Periodontol 79: 1652–1658. doi: 10.1902/jop.2008.080015 [DOI] [PubMed] [Google Scholar]
- 6.Han DH, Lim S, Paek D, Kim HD (2012) Periodontitis could be related factors on metabolic syndrome among Koreans: a case-control study. J Clin Periodontol 39: 30–37. doi: 10.1111/j.1600-051X.2011.01806.x [DOI] [PubMed] [Google Scholar]
- 7.Kim DW, Park JC, Rim TT, Jung UW, Kim CS, Donos N, et al. (2014) Socioeconomic disparities of periodontitis in Koreans based on the KNHANES IV. Oral Dis 20: 551–559. doi: 10.1111/odi.12168 [DOI] [PubMed] [Google Scholar]
- 8.Chapple IL, Matthews JB (2007) The role of reactive oxygen and antioxidant species in periodontal tissue destruction. Periodontol 2000 43: 160–232. [DOI] [PubMed] [Google Scholar]
- 9.Han DH, Kim MS, Shin HS, Park KP, Kim HD (2013) Association between periodontitis and salivary nitric oxide metabolites among community elderly Koreans. J Periodontol 84: 776–784. doi: 10.1902/jop.2012.120237 [DOI] [PubMed] [Google Scholar]
- 10.Van der Velden U, Kuzmanova D, Chapple IL (2011) Micronutritional approaches to periodontal therapy. J Clin Periodontol 38 Suppl 11: 142–158. [DOI] [PubMed] [Google Scholar]
- 11.Amaliya, Timmerman MF, Abbas F, Loos BG, Van der Weijden GA, Van Winkelhoff AJ, et al. (2007) Java project on periodontal diseases: the relationship between vitamin C and the severity of periodontitis. J Clin Periodontol 34: 299–304. doi: 10.1111/j.1600-051X.2007.01053.x [DOI] [PubMed] [Google Scholar]
- 12.Amaliya A (2014) Java project on periodontal disease. Periodontal condition in relation to vitamin C, systemic conditions and tooth loss.
- 13.Kuzmanova D, Jansen ID, Schoenmaker T, Nazmi K, Teeuw WJ, Bizzarro S, et al. (2012) Vitamin C in plasma and leucocytes in relation to periodontitis. J Clin Periodontol 39: 905–912. doi: 10.1111/j.1600-051X.2012.01927.x [DOI] [PubMed] [Google Scholar]
- 14.Chapple IL, Milward MR, Dietrich T (2007) The prevalence of inflammatory periodontitis is negatively associated with serum antioxidant concentrations. J Nutr 137: 657–664. [DOI] [PubMed] [Google Scholar]
- 15.Nishida M, Grossi SG, Dunford RG, Ho AW, Trevisan M, Genco RJ (2000) Dietary vitamin C and the risk for periodontal disease. J Periodontol 71: 1215–1223. doi: 10.1902/jop.2000.71.8.1215 [DOI] [PubMed] [Google Scholar]
- 16.Amarasena N, Ogawa H, Yoshihara A, Hanada N, Miyazaki H (2005) Serum vitamin C-periodontal relationship in community-dwelling elderly Japanese. J Clin Periodontol 32: 93–97. doi: 10.1111/j.1600-051X.2004.00643.x [DOI] [PubMed] [Google Scholar]
- 17.Merchant AT (2008) Plasma Vitamin C is Inversely Associated with Periodontitis. Journal of evidence based dental practice 8: 103–104. doi: 10.1016/j.jebdp.2008.03.005 [DOI] [PubMed] [Google Scholar]
- 18.Rai B, Anand S (2008) Serum and Salivary Vitamin C in Periodontal Disease. Adv in Med Dent Sci 2: 26–27. [Google Scholar]
- 19.Pussinen PJ, Laatikainen T, Alfthan G, Asikainen S, Jousilahti P (2003) Periodontitis is associated with a low concentration of vitamin C in plasma. Clin Diagn Lab Immunol 10: 897–902. doi: 10.1128/CDLI.10.5.897-902.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ismail AI, Burt BA, Eklund SA (1983) Relation between Ascorbic Acid Intake and Periodontal Disease in the United States. The Journal of the American Dental Association 107: 927–931. [DOI] [PubMed] [Google Scholar]
- 21.Clark DE, Navia JM, Manson-Hing LR, Duncan HE (1990) Evaluation of alveolar bone in relation to nutritional status during pregnancy. J Dent Res 69: 890–895. doi: 10.1177/00220345900690031201 [DOI] [PubMed] [Google Scholar]
- 22.Ainamo J, Barmes D, Beagrie G, Cutress T, Martin J, Sardo-Infirri J (1982) Development of the World Health Organization (WHO) community periodontal index of treatment needs (CPITN). Int Dent J 32: 281–291. [PubMed] [Google Scholar]
- 23.Korea Center for Disease Control and Prevention (2010) Korean National Health and Nutrition Examination Survey: the 4th surveys.
- 24.Salvador Castell G, Serra-Majem L, Ribas-Barba L (2015) What and how much do we eat? 24-hour dietary recall method. Nutr Hosp 31 Suppl 3: 46–48. [DOI] [PubMed] [Google Scholar]
- 25.Kaye EK (2012) Nutrition, dietary guidelines and optimal periodontal health. Periodontol 2000 58: 93–111. [DOI] [PubMed] [Google Scholar]
- 26.The Korean Nutrition Society (2010) Dietary Reference Intakes for Koreans 2010, 1st revised. Seoul
- 27.Murphy SP, Poos MI (2002) Dietary Reference Intakes: summary of applications in dietary assessment. Public Health Nutr 5: 843–849. doi: 10.1079/PHN2002389 [DOI] [PubMed] [Google Scholar]
- 28.Standing Committee on the Scientific Evaluation of Dietary Refence Intakes of the Food and Nutrition Board IOM, National Academy of Sciences, (1997) Dietary reference intakes. Nutr Rev 55: 319–326. 9329268 [Google Scholar]
- 29.Pfeiffer CM, Sternberg MR, Schleicher RL, Rybak ME (2013) Dietary supplement use and smoking are important correlates of biomarkers of water-soluble vitamin status after adjusting for sociodemographic and lifestyle variables in a representative sample of U.S. adults. J Nutr 143: 957S–965S. doi: 10.3945/jn.112.173021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Iwasaki M, Manz MC, Taylor GW, Yoshihara A, Miyazaki H (2012) Relations of Serum Ascorbic Acid and α-tocopherol to Periodontal Disease. Journal of Dental Research 91: 167–172. doi: 10.1177/0022034511431702 [DOI] [PubMed] [Google Scholar]
- 31.Abou Sulaiman AE, Shehadeh RM (2010) Assessment of total antioxidant capacity and the use of vitamin C in the treatment of non-smokers with chronic periodontitis. J Periodontol 81: 1547–1554. doi: 10.1902/jop.2010.100173 [DOI] [PubMed] [Google Scholar]
- 32.Leggott PJ, Robertson PB, Jacob RA, Zambon JJ, Walsh M, Armitage GC (1991) Effects of ascorbic acid depletion and supplementation on periodontal health and subgingival microflora in humans. J Dent Res 70: 1531–1536. doi: 10.1177/00220345910700121101 [DOI] [PubMed] [Google Scholar]
- 33.Vogel RI, Lamster IB, Wechsler SA, Macedo B, Hartley LJ, Macedo JA (1986) The effects of megadoses of ascorbic acid on PMN chemotaxis and experimental gingivitis. J Periodontol 57: 472–479. doi: 10.1902/jop.1986.57.8.472 [DOI] [PubMed] [Google Scholar]
- 34.Ciol MA, Hoffman JM, Dudgeon BJ, Shumway-Cook A, Yorkston KM, Chan L (2006) Understanding the use of weights in the analysis of data from multistage surveys. Arch Phys Med Rehabil 87: 299–303. doi: 10.1016/j.apmr.2005.09.021 [DOI] [PubMed] [Google Scholar]
- 35.Haytac MC, Ozcelik O, Mariotti A (2013) Periodontal disease in men. Periodontol 2000 61: 252–265. [DOI] [PubMed] [Google Scholar]
- 36.Johansen JS, Harris AK, Rychly DJ, Ergul A (2005) Oxidative stress and the use of antioxidants in diabetes: linking basic science to clinical practice. Cardiovasc Diabetol 4: 5 doi: 10.1186/1475-2840-4-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Korea Center for Disease Control & prevention (2014) Korea health statistics 2013: korea national health and nutrition examination survey (VI-I)
- 38.Petersen PE, Ogawa H (2005) Strengthening the prevention of periodontal disease: the WHO approach. Journal of periodontology 76: 2187–2193. doi: 10.1902/jop.2005.76.12.2187 [DOI] [PubMed] [Google Scholar]
- 39.Park JB, Han K, Park YG, Ko Y (2014) Association between alcohol consumption and periodontal disease: the 2008 to 2010 Korea National Health and Nutrition Examination Survey. J Periodontol 85: 1521–1528. doi: 10.1902/jop.2014.130782 [DOI] [PubMed] [Google Scholar]
- 40.Jang AY, Lee JK, Shin JY, Lee HY (2016) Association between Smoking and Periodontal Disease in Korean Adults: The Fifth Korea National Health and Nutrition Examination Survey (2010 and 2012). Korean J Fam Med 37: 117–122. doi: 10.4082/kjfm.2016.37.2.117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ahn YB, Shin MS, Byun JS, Kim HD (2015) The association of hypertension with periodontitis is highlighted in female adults: results from the Fourth Korea National Health and Nutrition Examination Survey. J Clin Periodontol 42: 998–1005. doi: 10.1111/jcpe.12471 [DOI] [PubMed] [Google Scholar]
- 42.Falagas ME, Kompoti M (2006) Obesity and infection. Lancet Infect Dis 6: 438–446. doi: 10.1016/S1473-3099(06)70523-0 [DOI] [PubMed] [Google Scholar]
- 43.Llambes F, Arias-Herrera S, Caffesse R (2015) Relationship between diabetes and periodontal infection. World J Diabetes 6: 927–935. doi: 10.4239/wjd.v6.i7.927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yan Y, Zeng W, Song S, Zhang F, He W, Liang W, et al. (2013) Vitamin C induces periodontal ligament progenitor cell differentiation via activation of ERK pathway mediated by PELP1. Protein Cell 4: 620–627. doi: 10.1007/s13238-013-3030-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Eke PI, Thornton-Evans GO, Wei L, Borgnakke WS, Dye BA (2010) Accuracy of NHANES Periodontal Examination Protocols. Journal of Dental Research 89: 1208–1213. doi: 10.1177/0022034510377793 [DOI] [PubMed] [Google Scholar]
- 46.Dwyer J, Picciano MF, Raiten DJ (2003) Estimation of usual intakes: What We Eat in America-NHANES. J Nutr 133: 609S–623S. [DOI] [PubMed] [Google Scholar]
- 47.Dodd KW, Guenther PM, Freedman LS, Subar AF, Kipnis V, Midthune D, et al. (2006) Statistical methods for estimating usual intake of nutrients and foods: a review of the theory. J Am Diet Assoc 106: 1640–1650. doi: 10.1016/j.jada.2006.07.011 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
Data Availability Statement
Data are available from the Korea National Health and Nutrition Examination Survey database (https://knhanes.cdc.go.kr/knhanes/eng/index.do) for researchers who meet the criteria for access to confidential data.