Abstract
Objective
Young adulthood represents a critical time to address elevated obesity rates and the risk of early mortality, particularly among people with serious mental illness. Few studies have assessed the benefits of lifestyle interventions targeting weight loss among these young adults. This study examined the impact of the 12-month In SHAPE lifestyle intervention on weight loss and fitness among overweight and obese young adults with serious mental illness (ages 21–30) compared with participants over age 30.
Methods
Data were combined from three trials of the 12-month In SHAPE program delivered through community mental health centers. In SHAPE includes weekly fitness trainer meetings, a gym membership, and nutrition education. Primary outcomes were weight loss and change in fitness at 12 months.
Results
Participants (N=194) had a schizophrenia spectrum disorder (53%) or a mood disorder (47%). The overall sample achieved significant weight loss and improved fitness; differences between young adults (N=29) and participants over age 30 (N=165) were not significant. An important finding was that 42% of young adults achieved clinically significant reductions in cardiovascular risk, defined as ≥5% weight loss or improved fitness (>50-m increase on the 6-Minute Walk Test), compared with 54% of adults over age 30 (a non-significant difference between age groups).
Conclusions
Among persons enrolled in a lifestyle intervention, overweight and obese young adults experienced benefits comparable with those of adults over age 30. Young adults with serious mental illness face high risk of gaining weight, but a meaningful proportion of these individuals can achieve clinically significant cardiovascular risk reduction, thus highlighting the need to promote lifestyle intervention participation in this group.
Obesity prevalence is nearly double among people with serious mental illness compared with the general population (1,2). Obesity is also a major contributor to cardiovascular disease and the resulting significantly reduced life expectancy for individuals with serious mental illness (3). Among people with serious mental illnesses, achieving meaningful reduction in cardiovascular risk requires not only significant and sustained changes to modifiable risk factors such as poor diet and sedentary behaviors but also overcoming challenges such as poverty, metabolic effects of psychoactive medications, and the impact of symptoms on motivation (4). Young adulthood represents a critical time to address this early mortality disparity because even though young adults are at greatest risk of gaining weight (5), they are also poised to experience lasting benefits through participation in lifestyle interventions by learning and adopting positive habits that they can carry forward across the lifespan.
Young people with serious mental illness are at risk of substantial weight gain as a result of mental illness onset and its consequences on life functioning and motivation, as well as the initiation of some antipsychotic treatments (6). Recent reports have documented the high prevalence of cardiometabolic risk factors among young people with first-episode schizophrenia spectrum disorders (7) as well as the elevated risk of cardiovascular disease among young people with bipolar disorder and major depressive disorder (8). A review found that young people with serious mental illness were more likely than young people in the general population to engage in poor lifestyle habits such as eating more high-fat foods and getting less exercise, resulting in elevated risk for long-term general medical problems, including cardiovascular disease and diabetes (9). However, there is limited research on the effect of lifestyle interventions targeting weight loss among overweight and obese adults age 30 and under who have a serious mental illness, such as a schizophrenia spectrum disorder or a mood disorder.
For young adults in the general population, recent systematic reviews of lifestyle interventions targeting weight loss have found that the effectiveness of these efforts has been variable (10,11). For example, prior studies have been limited by small sample sizes, short intervention periods, homogeneous samples, and elevated participant attrition (12). Research findings also suggest that these mixed findings are partly attributable to challenges with engaging this age group in services, as well as to the predominant focus in prior research on childhood obesity or on developing interventions for middle-aged adults that may not appeal to the interests and unique lifestyles of young adults (12).
Among adults with serious mental illness, there is increasing evidence to support the effectiveness of behavioral interventions promoting fitness and healthy eating for weight loss (13). A series of randomized controlled trials of different lifestyle interventions has demonstrated the effectiveness of these programs for achieving clinically significant weight loss—5% or greater—or reducing cardiovascular risk for as many as half of participants with serious mental illness (14–17). However, across these recent studies, the impact of lifestyle intervention on outcomes among young adults has not been specifically examined and therefore remains unclear. Prior studies have also demonstrated that behavioral interventions can lessen antipsychotic-induced weight gain during illness onset among young adults with serious mental illness who are initiating treatment (18–20). Less clear, however, is whether overweight or obese young adults with serious mental illness who are receiving stable pharmacological treatment can achieve meaningful health benefits, including weight loss, improved fitness, and reduction in cardiovascular risk through participation in a lifestyle intervention.
This study examined the impact of the 12-month In SHAPE lifestyle intervention on weight loss and fitness among overweight and obese young adults with serious mental illness who were ages 21 to 30 compared with adults over age 30. Secondary outcomes, including change in body mass index (BMI), waist circumference, physical activity, blood pressure, and lipid levels and program adherence, were also compared between the two age groups. The primary aim was to determine whether young adult participants with serious mental illness would lose weight, improve fitness, and achieve reduced cardiovascular risk at levels comparable with those of participants over age 30.
METHODS
This study used combined data for 194 participants with serious mental illness who received the In SHAPE lifestyle intervention and who completed baseline and follow-up assessments across three separate clinical trials. The trials included a randomized trial of 133 persons with serious mental illness who participated in the In SHAPE program or who had a gym membership from April 2007 to November 2011 in Concord, New Hampshire (14); a randomized trial that compared 210 persons with serious mental illness who participated in In SHAPE or who had a gym membership from April 2008 to May 2013 in Boston (15); and a trial with 122 persons with serious mental illness who participated in In SHAPE implemented in two community mental health centers or who received usual care in two additional centers from December 2009 to March 2013 in rural and urban settings in New Hampshire. Forty participants who completed baseline but not 12-month assessments were not included in this analysis. These individuals did not differ on any baseline characteristics from participants (N=194) who completed the study.
All participants had a serious mental illness, defined by an axis I diagnosis of schizophrenia, schizoaffective disorder, major depressive disorder, or bipolar disorder, and persistent impairment in multiple areas of functioning (such as work, school, or self-care); were age 21 or older; had a BMI greater than 25, indicating excess weight; were on stable pharmacological treatment, defined as receiving the same psychiatric medications over the prior two months; and provided informed consent for participation. Study procedures were approved by Committees for the Protection of Human Subjects at Dartmouth College and specific to each site.
In SHAPE Program
The 12-month In SHAPE lifestyle intervention consists of a gym membership, weekly individual meetings with a certified fitness trainer, and instruction on healthy eating and nutrition. The fitness trainers are trained in tailoring individual wellness plans to the needs of people with serious mental illness and complete a one-week In SHAPE training course consisting of instruction in motivational interviewing, fitness goal setting, nutrition, tracking eating and exercise, and strategies for health behavior change, such as addressing mental health symptoms that interfere with exercise and healthy eating. Participants obtained medical clearance from their primary care provider to enroll in the In SHAPE program. At the start of the program, the fitness trainers conducted lifestyle and fitness evaluations to develop personalized fitness plans for each participant and to use shared goal setting. The fitness trainers delivered the In SHAPE program according to a standardized protocol. For the program duration, fitness trainers met with participants individually each week for 60 minutes at a local gym (YMCA). Each weekly session consisted primarily of fitness coaching, support, and reinforcement for exercise, followed by individualized nutrition education for at least 15 minutes, which emphasized a balanced diet, portion control, and healthy eating on a budget. To ensure fidelity to the In SHAPE program, the fitness trainers received weekly supervision from a health psychologist, a personal fitness trainer, and a registered dietitian.
Measures
Trained research interviewers collected several outcome measures at baseline and 12 months.
Weight
Change in body weight was measured in pounds. The proportion of participants who achieved clinically significant weight loss of ≥5% and ≥10% was calculated because modest weight loss, in this range, contributes to reduction in cardiovascular risk among overweight and obese individuals (21,22).
Fitness
Change in fitness was assessed with the 6-Minute Walk Test (6-MWT), which measures the distance that an individual can walk in six minutes and is a reliable and valid measure of fitness (23). The proportion of participants who achieved clinically significant improvement in fitness, defined as an increase in distance of >50 m (about 164 feet) on the 6-MWT, was also calculated because this improvement is associated with reduced cardiovascular risk (24).
Secondary obesity measures
Change in BMI, calculated as weight (kg)/height(m)2, and change in waist circumference, measured in inches, were reported.
Physical activity
Change in total physical activity was measured with the short-form International Physical Activity Questionnaire, which is a reliable and valid measure of physical activity among people with serious mental illness (25).
Blood pressure and lipid levels
Blood pressure was measured after participants completed the 6-MWT. Lipid levels were measured with the CardioChek PA Analyzer, a portable testing system that produces reliable values for total cholesterol, low-density lipoprotein, high-density lipoprotein, and triglycerides (26).
Program adherence and retention
Adherence was measured as the number of sessions with the fitness trainer, out of 50 planned visits, over the 12-month intervention period. Study retention was defined as completion of the 12-month assessment.
Psychiatric medications
Participants’ medication use was assessed because different antipsychotic agents are associated with varying degrees of weight gain (27,28) and are known to affect ability to lose weight (2). Participants’ antipsychotic medications were classified as having a high (including olanzapine and clozapine), medium (risperidone), or low (ziprasidone) propensity for associated weight gain. Change in psychiatric medication use and the medication’s weight gain propensity was also examined because medication changes can interfere with ability to lose weight (6).
Statistical Analysis
Young adult participants (ages 21–30 years) were compared with participants over age 30 at baseline on demographic characteristics, obesity measures, fitness, blood pressure, lipid levels, and use of antipsychotic medications and on their psychiatric medications’ propensity to lead to weight gain. Chi-square tests were used for categorical variables, and t tests were used for continuous variables. Linear regression models were used to compare young adult participants and participants over age 30 at 12 months on continuous outcome variables, including primary outcomes of weight loss and fitness and secondary measures of obesity, physical activity, blood pressure, and lipid levels. Logistic regression models were used to compare the age groups on binary outcomes of whether the participant lost weight compared with baseline weight, achieved ≥5% weight loss, achieved ≥10% weight loss, showed improved fitness (>50-m increase on the 6-MWT), or achieved reduced cardiovascular risk (≥5% weight loss or >50-m increase on the 6-MWT) at 12 months. All regression models controlled for study (trial 1, 2, or 3), gender, diagnosis, race-ethnicity, and level of program adherence. A value of p≤.05 was considered significant. All statistical analyses were performed in 2015 with Stata 14.0 software.
RESULTS
Participants’ baseline characteristics are listed in Table 1. Greater proportions of young adult participants compared with participants over age 30 were living in supervised or supportive housing and were either never married or were currently married. Young adults also had higher levels of fitness at baseline. Other demographic characteristics, physical activity, smoking status, obesity measures, blood pressure and lipid levels, and use of antipsychotic medications did not differ between age groups at baseline.
TABLE 1.
Baseline characteristics of In SHAPE participants overall and by age groupa
| Characteristic | Total sample (N=194)
|
21–30 years (N=29)
|
>30 years (N=165)
|
p | |||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | ||
| Demographic | |||||||
| Age (M±SD) | 44.0±11.1 | 26.0±3.2 | 47.2±8.7 | <.001 | |||
| Sex | .712 | ||||||
| Male | 93 | 48 | 13 | 45 | 80 | 49 | |
| Female | 101 | 52 | 16 | 55 | 85 | 52 | |
| Race-ethnicity | .205 | ||||||
| Black | 33 | 17 | 8 | 28 | 25 | 15 | |
| Hispanic | 17 | 9 | 4 | 14 | 13 | 8 | |
| Non-Hispanic white | 132 | 68 | 15 | 52 | 117 | 71 | |
| Other | 12 | 6 | 2 | 7 | 10 | 6 | |
| Completed high school | 162 | 84 | 23 | 79 | 139 | 84 | .509 |
| Current smoker | 80 | 41 | 12 | 41 | 68 | 41 | .987 |
| Living situation | .011 | ||||||
| Living independently | 133 | 69 | 14 | 48 | 119 | 72 | |
| In supervised or supportive housing | 61 | 31 | 15 | 52 | 46 | 28 | |
| Married | .001 | ||||||
| Never married | 127 | 66 | 25 | 86 | 102 | 62 | |
| Currently married | 13 | 7 | 4 | 14 | 9 | 6 | |
| Previously married | 54 | 28 | 0 | — | 54 | 33 | |
| Diagnosis | .808 | ||||||
| Schizophrenia spectrum disorder | 103 | 53 | 16 | 55 | 87 | 53 | |
| Mood disorder | 91 | 47 | 13 | 45 | 78 | 47 | |
| Obesity measures | |||||||
| Body mass index (M±SD)b | 37.1±8.0 | 36.9±7.0 | 37.2±8.2 | .847 | |||
| Weight (M±SD pounds) | 235.2±56.0 | 235.0±59.5 | 235.2±55.6 | .984 | |||
| Waist circumference (M±SD inches) | 47.0±6.9 | 46.4±6.9 | 47.2±7.0 | .593 | |||
| Fitness (M±SD)c | 1,388.3±313.0 | 1,498.3±233.5 | 1,369.3±321.6 | .044 | |||
| Total physical activity (M±SD)d | 2,108.8±2,554.2 | 2,449.6±3,055.1 | 2,048.6±2,554.2 | .118 | |||
| Blood pressure (M±SD mmHg) | |||||||
| Systolic | 126.4±18.5 | 123.6±13.6 | 126.9±19.3 | .378 | |||
| Diastolic | 81.9±12.3 | 80.8±10.4 | 82.1±12.6 | .616 | |||
| Total cholesterol (M±SD mg/dl) | 182.4±44.7 | 177.6±40.7 | 183.4±45.5 | .531 | |||
| Low-density lipoprotein | 109.6±37.3 | 118.4±38.6 | 108.1±37.1 | .244 | |||
| High-density lipoprotein | 41.9±15.6 | 40.5±10.8 | 42.2±16.3 | .589 | |||
| Triglycerides | 178.0±115.4 | 150.5±106.7 | 183.3±116.6 | .170 | |||
| Elevated risk of hypertensione | 64 | 34 | 8 | 29 | 56 | 35 | .522 |
| Medications | |||||||
| Number of psychotropic medications (M±SD) | 2.1±1.1 | 2.0±1.1 | 2.1±1.1 | .467 | |||
| Weight gain propensity | .530 | ||||||
| Highf | 69 | 38 | 8 | 31 | 61 | 39 | |
| Mediumg | 71 | 39 | 9 | 35 | 62 | 40 | |
| Lowh | 32 | 18 | 7 | 27 | 25 | 16 | |
| None | 11 | 6 | 2 | 8 | 9 | 6 | |
The age groups were compared by using chi-square tests for categorical variables and t tests for continuous variables.
Body mass index was measured as kg/m2, with >25 kg/m2 indicating excess weight.
Fitness was measured with the 6-Minute Walk Test (6-MWT), which measures the distance (feet) that a participant walks in six minutes. Higher values indicate better fitness.
Physical activity was measured with the short-form International Physical Activity Questionnaire, which measures respondent’s total self-reported activity in minutes and converts this value to a weighted estimate of metabolic equivalent expenditure (MET-min) per week. Higher values indicate greater participation in physical activity.
Systolic blood pressure >140 mmHg or diastolic blood pressure >90 mmHg
Olanzapine and clozapine
Haloperidol, risperidone, quetiapine, thioridazine, chlorpromazine, paroxetine, amitriptyline, divalproex, valproate, doxepin, lithium, carbamazepine, imipramine, and gabapentin
Ziprasidone, perphenazine, fluphenazine, fluoxetine, bupropion, venlafaxine, molindone, lamotrigine, duloxetine, aripiprazole, fluvoxamine, trazodone, desipramine, loxapine, sertraline, escitalopram, clomipramine, nortriptyline, citalopram, paliperidone, topiramate, mirtazapine, and lurasidone
At 12 months, the overall sample showed significant mean±SD weight loss of 4.37±19.20 pounds (p=.002 for pre-post change) and significant improvement in fitness, as reflected by an increase on the 6-MWT of 59.89±228.98 feet (p=.002 for pre-post change). As highlighted in Table 2, there were no significant differences in outcomes between age groups. Although these results were not statistically significant, average weight loss and average BMI reduction were greater for participants over age 30 compared with young adults.
TABLE 2.
Change in weight and fitness outcomes among adults with serious mental illness from baseline to 12 months, by age group
| Variable | N | Overall (N=194)
|
21–30 years (N=29)
|
>30 years (N=165)
|
pa | |||
|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | |||
| Change in primary outcomes | ||||||||
| Weight (pounds) | 185 | −4.37 | 19.20 | 1.61 | 24.09 | −5.44 | 18.08 | .084 |
| Fitness (6-MWT)b | 165 | 59.89 | 228.98 | 12.77 | 205.26 | 68.70 | 232.77 | .406 |
| Change in secondary measures | ||||||||
| Obesity | ||||||||
| BMIc | 185 | −.72 | 3.03 | .31 | 3.79 | −.90 | 2.85 | .060 |
| Waist circumference (inches) | 185 | −1.42 | 3.32 | −1.43 | 4.15 | −1.42 | 3.17 | .864 |
| Total physical activityd | 192 | 309.33 | 2,822.80 | 263.36 | 4,579.90 | 317.52 | 2,401.82 | .833 |
| Blood pressure (mmHg) | ||||||||
| Systolic | 173 | 2.32 | 18.37 | 6.15 | 14.77 | 1.64 | 18.90 | .320 |
| Diastolic | 173 | −.21 | 12.15 | .92 | 8.63 | −.42 | 12.69 | .703 |
| Total cholesterol (mg/dl) | 149 | −3.08 | 40.43 | 3.50 | 39.20 | −4.22 | 40.68 | .598 |
| Low-density lipoprotein | 105 | −3.46 | 36.44 | 8.75 | 23.37 | −5.03 | 37.60 | .421 |
| High-density lipoprotein | 149 | 3.22 | 16.51 | 7.14 | 18.66 | 2.54 | 16.09 | .261 |
| Triglycerides | 149 | −8.42 | 114.15 | 11.73 | 123.53 | −11.91 | 112.60 | .354 |
p values from linear regression models adjusted for study (trial 1, 2, or 3), gender, diagnosis, race-ethnicity, and level of program adherence.
Measured with the 6-Minute Walk Test (6-MWT), which measures the distance (feet) that a participant walks in six minutes. Higher values indicate better fitness.
Body mass index, measured as kg/m2, with >25 kg/m2 indicating excess weight
Measured with the short-form International Physical Activity Questionnaire, which converts respondent’s total self-reported activity in minutes to a weighted estimate of metabolic equivalent expenditure (MET-min) per week. Higher values indicate greater participation in physical activity.
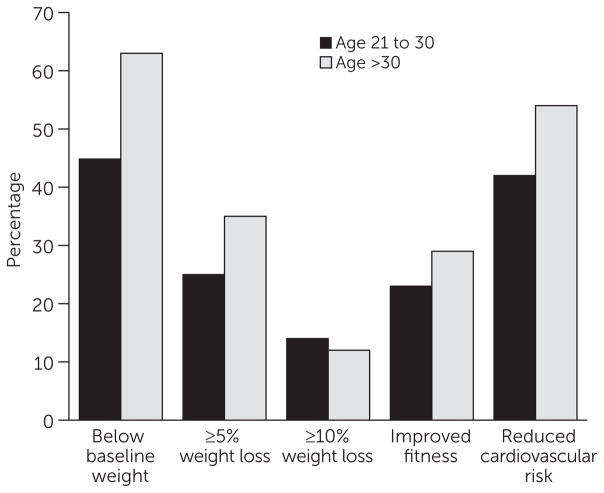
Figure 1 illustrates the proportions of participants in both age groups who lost weight or who achieved clinically significant weight loss, improved fitness, or cardiovascular risk reduction. At 12 months, a greater proportion of participants over age 30 compared with young adults were below their baseline weight, achieved ≥5% weight loss, and showed improved fitness and cardiovascular risk reduction; however, none of these differences were statistically significant. Nearly half (45%) of young adult participants were below their baseline weight, 25% achieved ≥5% weight loss, 14% achieved ≥10% weight loss, and 23% showed clinically significant improved fitness based on a >50-m increase on the 6-MWT. Overall, 42% of young adult participants (compared with 54% of participants over age 30) showed clinically significant cardiovascular risk reduction, defined as either clinically significant weight loss or improved fitness (the difference was not statistically significant).
FIGURE 1. Proportion of participants achieving weight loss, fitness, and improved cardiovascular outcomes at 12 months, by age groupa.
aThere were no significant differences between age groups at 12 months in the proportion of participants who were below baseline weight; achieved ≥5% or ≥10% weight loss; showed improved fitness, measured as >50-m increase on the 6-Minute Walk Test; or achieved reduced cardiovascular risk, defined as ≥5% weight loss or >50-m increase on the 6-Minute Walk Test.
Study attrition did not differ between young adults (17%) and participants over age 30 (17%). Adherence to the In SHAPE intervention, measured as session attendance with the fitness trainer out of a possible 50 sessions over the 12-month study period, was comparable between age groups. On average, young adults attended 27.0±14.4 sessions compared with 29.2±13.5 sessions for participants over age 30. There were no differences in medication changes between the groups.
DISCUSSION
This study showed that overweight and obese young adults with serious mental illness were able to achieve clinically significant benefits through participation in the In SHAPE lifestyle intervention. At 12 months, 42% of young adult participants achieved reduction in cardiovascular risk, defined as ≥5% weight loss or >50-m increase on the 6-MWT. Although average weight loss and average BMI reduction were greater among participants over age 30 than among young adults, these differences were not statistically significant. These findings expand on existing efforts to prevent weight gain among young adults with serious mental illness (18,19) and show promise for offering behavioral weight loss interventions to overweight and obese young adults in community mental health settings.
Another important finding was that neither attrition nor program adherence differed between age groups. This finding suggests that when young adults with serious mental illness enroll in a lifestyle intervention, they are as motivated as participants over age 30 to continue participating throughout the 12-month program. This finding is in contrast to findings of many prior studies of standard behavioral weight loss treatment consisting of education and didactic instruction in the general population, in which young adults seemed reluctant to participate or sustain involvement in programs over time (11).
Benefits of the In SHAPE lifestyle intervention among young adults with serious mental illness may be due to the emphasis on physical activity through the use of personalized health coaching sessions with a fitness trainer at a fitness facility located outside of the mental health center, which is consistent with research from the general population showing that young adults prefer physical activity over other methods for losing weight (29). In addition, research has shown that young adults respond well to emotional support for weight loss (29). The personal connection and support provided by the fitness trainers, who were mostly young adults themselves, in the In SHAPE program may have been especially motivating for young adult participants with serious mental illness. For example, during weekly meetings with participants, the fitness trainers helped participants to develop individualized fitness plans, supported personal goal setting, and suggested strategies for overcoming mental health symptoms that interfered with healthy eating or exercise, which may have promoted engagement with the program (30).
The findings are promising in that 45% of young adult participants in the In SHAPE program were below their baseline weight at 12 months given the substantial risk of weight gain observed in this group. This result suggests that a lifestyle intervention delivered through community mental health settings may benefit both younger and older groups of adults. These findings could also inform continued efforts needed to target the young adult participants who were not successful at losing weight. Approaches that appeal specifically to the unique interests, perspectives, and attitudes of young adults with serious mental illness and that focus on sensitive issues for young people, such as self-esteem and body image (31), may afford added impact. For example, lifestyle interventions for young adults with serious mental illness could promote the benefits of adopting a healthy lifestyle to look and feel good while offering opportunities to socialize and have fun (12,29). Interventions targeting this group could also include brief education about the role of psychiatric medications and weight gain and provide training on how to talk to mental health providers about weight gain from psychotropic medications (4,6).
Emerging mobile and online technologies may also offer advantages for promoting and supporting weight loss and fitness among young adults with serious mental illness (4). Popular social media and smartphone technologies are increasingly becoming part of the daily lives of young people with serious mental illness (32) and may afford new opportunities for delivering scalable interventions capable of reaching and engaging these individuals at their own convenience (33). In the general population, Facebook has been successfully used to support weight loss among college students (34), and hybrid approaches using Facebook, text messaging, and smartphone applications appear promising for promoting engagement and retention in behavioral weight loss efforts for young adults (35). Recent preliminary pilot studies have highlighted the feasibility, acceptability, and potential effectiveness of supporting lifestyle interventions for people with serious mental illness by using Facebook, smartphone technologies, and wearable activity tracking devices (36,37). However, use of these technologies for specifically targeting and supporting behavioral weight loss among young adults with serious mental illness has not yet been explored.
Several limitations warrant consideration. First, all participants were receiving services at community mental health centers, indicating that these findings may not be generalizable to individuals with serious mental illness not receiving treatment. Second, nearly 70% of the sample was non-Hispanic white, which may limit generalizability across diverse racial or ethnic groups. Third, fewer young adult participants received the In SHAPE lifestyle intervention compared with participants over age 30. This may have increased the risk of type II statistical error (that is, failure to detect an effect that was present).
CONCLUSIONS
As young people with mental illness grow older, they often experience a decline in physical function and risk developing serious medical conditions resulting from the cumulative impact of obesity, poor health behaviors, low socioeconomic status, and effects of living with mental illness on motivation and personal well-being (9). Efforts are urgently needed to alter this trajectory and to support young adults with serious mental illness as they develop behavioral patterns and habits and learn to balance their mental health symptoms with life demands and pursuits. Drawing from the findings presented here, future lifestyle interventions must specifically target weight loss and fitness among overweight and obese young adults with serious mental illness, so that these individuals can build confidence, learn necessary skills, and adopt healthy behaviors that may decrease the significant early mortality gap affecting this high-risk group.
Acknowledgments
This study was supported by grants from the U.S. Centers for Disease Control and Prevention (CDC U48DP001935-0) and the National Institute of Mental Health (R01 MH078052 and R01 MH089811-01). Additional support was received from the Health Promotion Research Center at Dartmouth (Cooperative Agreement U48 DP005018). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
The authors report no financial relationships with commercial interests.
Contributor Information
Mr. John A. Naslund, Dartmouth Institute for Health Policy and Clinical Practice, Dartmouth College, Lebanon, New Hampshire
Dr. Kelly A. Aschbrenner, Department of Psychiatry, Geisel School of Medicine at Dartmouth, Lebanon, New Hampshire
Dr. Emily A. Scherer, Department of Biomedical Data Science, Geisel School of Medicine at Dartmouth, Lebanon, New Hampshire
Dr. Sarah I. Pratt, Department of Psychiatry, Geisel School of Medicine at Dartmouth, Lebanon, New Hampshire
Dr. Stephen J. Bartels, Department of Psychiatry, Geisel School of Medicine at Dartmouth, Lebanon, New Hampshire
References
- 1.Dickerson FB, Brown CH, Kreyenbuhl JA, et al. Obesity among individuals with serious mental illness. Acta Psychiatrica Scandinavica. 2006;113:306–313. doi: 10.1111/j.1600-0447.2005.00637.x. [DOI] [PubMed] [Google Scholar]
- 2.Allison DB, Newcomer JW, Dunn AL, et al. Obesity among those with mental disorders: a National Institute of Mental Health meeting report. American Journal of Preventive Medicine. 2009;36:341–350. doi: 10.1016/j.amepre.2008.11.020. [DOI] [PubMed] [Google Scholar]
- 3.Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry. 2015;72:334–341. doi: 10.1001/jamapsychiatry.2014.2502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gates J, Killackey E, Phillips L, et al. Mental health starts with physical health: current status and future directions of non-pharmacological interventions to improve physical health in first-episode psychosis. Lancet Psychiatry. 2015;2:726–742. doi: 10.1016/S2215-0366(15)00213-8. [DOI] [PubMed] [Google Scholar]
- 5.Williamson DF, Kahn HS, Remington PL, et al. The 10-year incidence of overweight and major weight gain in US adults. Archives of Internal Medicine. 1990;150:665–672. [PubMed] [Google Scholar]
- 6.Alvarez-Jiménez M, González-Blanch C, Crespo-Facorro B, et al. Antipsychotic-induced weight gain in chronic and first-episode psychotic disorders: a systematic critical reappraisal. CNS Drugs. 2008;22:547–562. doi: 10.2165/00023210-200822070-00002. [DOI] [PubMed] [Google Scholar]
- 7.Correll CU, Robinson DG, Schooler NR, et al. Cardiometabolic risk in patients with first-episode schizophrenia spectrum disorders: baseline results from the RAISE-ETP study. JAMA Psychiatry. 2014;71:1350–1363. doi: 10.1001/jamapsychiatry.2014.1314. [DOI] [PubMed] [Google Scholar]
- 8.Goldstein BI, Carnethon MR, Matthews KA, et al. Major Depressive Disorder and Bipolar Disorder Predispose Youth to Accelerated Atherosclerosis and Early Cardiovascular Disease: a scientific statement from the American Heart Association. Circulation. 2015;132:965–986. doi: 10.1161/CIR.0000000000000229. [DOI] [PubMed] [Google Scholar]
- 9.McCloughen A, Foster K, Huws-Thomas M, et al. Physical health and wellbeing of emerging and young adults with mental illness: an integrative review of international literature. International Journal of Mental Health Nursing. 2012;21:274–288. doi: 10.1111/j.1447-0349.2011.00796.x. [DOI] [PubMed] [Google Scholar]
- 10.Hebden L, Chey T, Allman-Farinelli M. Lifestyle intervention for preventing weight gain in young adults: a systematic review and meta-analysis of RCTs. Obesity Reviews. 2012;13:692–710. doi: 10.1111/j.1467-789X.2012.00990.x. [DOI] [PubMed] [Google Scholar]
- 11.Partridge SR, Juan SJ, McGeechan K, et al. Poor quality of external validity reporting limits generalizability of overweight and/or obesity lifestyle prevention interventions in young adults: a systematic review. Obesity Reviews. 2015;16:13–31. doi: 10.1111/obr.12233. [DOI] [PubMed] [Google Scholar]
- 12.Poobalan AS, Aucott LS, Precious E, et al. Weight loss interventions in young people (18 to 25 year olds): a systematic review. Obesity Reviews. 2010;11:580–592. doi: 10.1111/j.1467-789X.2009.00673.x. [DOI] [PubMed] [Google Scholar]
- 13.McGinty EE, Baller J, Azrin ST, et al. Interventions to address medical conditions and health-risk behaviors among persons with serious mental illness: a comprehensive review. Schizophrenia Bulletin. 2016;42:96–124. doi: 10.1093/schbul/sbv101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bartels SJ, Pratt SI, Aschbrenner KA, et al. Clinically significant improved fitness and weight loss among overweight persons with serious mental illness. Psychiatric Services. 2013;64:729–736. doi: 10.1176/appi.ps.003622012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bartels SJ, Pratt SI, Aschbrenner KA, et al. Pragmatic replication trial of health promotion coaching for obesity in serious mental illness and maintenance of outcomes. American Journal of Psychiatry. 2015;172:344–352. doi: 10.1176/appi.ajp.2014.14030357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Daumit GL, Dickerson FB, Wang N-Y, et al. A behavioral weight-loss intervention in persons with serious mental illness. New England Journal of Medicine. 2013;368:1594–1602. doi: 10.1056/NEJMoa1214530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Green CA, Yarborough BJH, Leo MC, et al. The STRIDE weight loss and lifestyle intervention for individuals taking antipsychotic medications: a randomized trial. American Journal of Psychiatry. 2015;172:71–81. doi: 10.1176/appi.ajp.2014.14020173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alvarez-Jiménez M, González-Blanch C, Vázquez-Barquero JL, et al. Attenuation of antipsychotic-induced weight gain with early behavioral intervention in drug-naive first-episode psychosis patients: a randomized controlled trial. Journal of Clinical Psychiatry. 2006;67:1253–1260. doi: 10.4088/jcp.v67n0812. [DOI] [PubMed] [Google Scholar]
- 19.Curtis J, Watkins A, Rosenbaum S, et al. Evaluating an individualized lifestyle and life skills intervention to prevent antipsychotic-induced weight gain in first-episode psychosis. Early Intervention in Psychiatry. 2016;10:267–276. doi: 10.1111/eip.12230. [DOI] [PubMed] [Google Scholar]
- 20.Lovell K, Wearden A, Bradshaw T, et al. An exploratory randomized controlled study of a healthy living intervention in early intervention services for psychosis: the INTERvention to encourage ACTivity, improve diet, and reduce weight gain (INTERACT) study. Journal of Clinical Psychiatry. 2014;75:498–505. doi: 10.4088/JCP.13m08503. [DOI] [PubMed] [Google Scholar]
- 21.Wing RR, Lang W, Wadden TA, et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care. 2011;34:1481–1486. doi: 10.2337/dc10-2415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Van Gaal LF, Wauters MA, De Leeuw IH. The beneficial effects of modest weight loss on cardiovascular risk factors. International Journal of Obesity and Related Metabolic Disorders. 1997;21(suppl 1):S5–S9. [PubMed] [Google Scholar]
- 23.Beriault K, Carpentier AC, Gagnon C, et al. Reproducibility of the 6-Minute Walk Test in obese adults. International Journal of Sports Medicine. 2009;30:725–727. doi: 10.1055/s-0029-1231043. [DOI] [PubMed] [Google Scholar]
- 24.Rasekaba T, Lee AL, Naughton MT, et al. The Six-Minute Walk Test: a useful metric for the cardiopulmonary patient. Internal Medicine Journal. 2009;39:495–501. doi: 10.1111/j.1445-5994.2008.01880.x. [DOI] [PubMed] [Google Scholar]
- 25.Faulkner G, Cohn T, Remington G. Validation of a physical activity assessment tool for individuals with schizophrenia. Schizophrenia Research. 2006;82:225–231. doi: 10.1016/j.schres.2005.10.020. [DOI] [PubMed] [Google Scholar]
- 26.Springer L, Murphy R, Enright M, et al. CardioChek PA Technical Bulletin: Clinical Performance Verification of the CardioChek PA Test System. Indianapolis: Polymer Technology Systems; 2010. [Google Scholar]
- 27.Allison DB, Mentore JL, Heo M, et al. Antipsychotic-induced weight gain: a comprehensive research synthesis. American Journal of Psychiatry. 1999;156:1686–1696. doi: 10.1176/ajp.156.11.1686. [DOI] [PubMed] [Google Scholar]
- 28.Taylor DM, McAskill R. Atypical antipsychotics and weight gain—a systematic review. Acta Psychiatrica Scandinavica. 2000;101:416–432. doi: 10.1034/j.1600-0447.2000.101006416.x. [DOI] [PubMed] [Google Scholar]
- 29.LaRose JG, Leahey TM, Hill JO, et al. Differences in motivations and weight loss behaviors in young adults and older adults in the National Weight Control Registry. Obesity. 2013;21:449–453. doi: 10.1002/oby.20053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shiner B, Whitley R, Van Citters AD, et al. Learning what matters for patients: qualitative evaluation of a health promotion program for those with serious mental illness. Health Promotion International. 2008;23:275–282. doi: 10.1093/heapro/dan018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sim K, Mahendran R, Chong SA. Health-related quality of life and psychiatric comorbidity in first episode psychosis. Comprehensive Psychiatry. 2005;46:278–283. doi: 10.1016/j.comppsych.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 32.Birnbaum ML, Rizvi AF, Correll CU, et al. Role of social media and the Internet in pathways to care for adolescents and young adults with psychotic disorders and non-psychotic mood disorders. Early Intervention in Psychiatry. doi: 10.1111/eip.12237. Epub ahead of print, March 23, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Naslund JA, Aschbrenner KA, Marsch LA, et al. The future of mental health care: peer-to-peer support and social media. Epidemiology and Psychiatric Sciences. 2016;25:113–122. doi: 10.1017/S2045796015001067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Napolitano MA, Hayes S, Bennett GG, et al. Using Facebook and text messaging to deliver a weight loss program to college students. Obesity. 2013;21:25–31. doi: 10.1002/oby.20232. [DOI] [PubMed] [Google Scholar]
- 35.Gupta A, Calfas KJ, Marshall SJ, et al. Clinical trial management of participant recruitment, enrollment, engagement, and retention in the SMART study using a Marketing and Information Technology (MARKIT) model. Contemporary Clinical Trials. 2015;42:185–195. doi: 10.1016/j.cct.2015.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Aschbrenner KA, Naslund JA, Shevenell M, et al. Feasibility of behavioral weight loss treatment enhanced with peer support and mobile health technology for individuals with serious mental illness. Psychiatric Quarterly. 2015;87:401–415. doi: 10.1007/s11126-015-9395-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Aschbrenner KA, Naslund JA, Shevenell M, et al. A pilot study of a peer-group lifestyle intervention enhanced with mHealth technology and social media for adults with serious mental illness. Journal of Nervous and Mental Disease. 2016;204:483–486. doi: 10.1097/NMD.0000000000000530. [DOI] [PMC free article] [PubMed] [Google Scholar]