SUMMARY
Although the existence of national data on BBIs provides much-needed information on the epidemiology of these serious injuries, there are no prospective studies available to guide management decisions. As a result, treatment recommendations are primarily based on expert opinion from related clinical experience. The single-center experience of the serious esophageal BBI cases presented in this article is the largest published outside of the compiled national data and offers important lessons for the management of future cases. Additional study is needed to better define the role of acid blockade, endoscopy, and MRI in the postremoval management of these cases and determine optimal timing for initiation of enteral feeding. Advocacy efforts are ongoing and vital in order to minimize the occurrence of these potentially fatal injuries.
Keywords: Button battery ingestion, Aortoesophageal fistula, Gastrointestinal hemorrhage, Pediatric, Foreign body ingestion, Caustic ingestion, Esophageal stricture, MRI
INTRODUCTION
Management of foreign body ingestion (FBI) can be one of the most challenging issues in pediatric endoscopy. The myriad variations in size, type, and timing of foreign object ingested, compounded by patient factors, such as age, underlying medical issues, and clinical presentation, make each case inherently unique. Button battery (BB) ingestions (BBIs) epitomize the challenge of pediatric FBI, as the outcome can range from harmless to death. As the authors’ center has personally experienced, when death occurs as a consequence of BBIs in an otherwise healthy child, it is one of the most tragic occurrences that a physician may encounter in a career.
US surveillance data have demonstrated a clear increase in morbidity and mortality due to BBI in the last 2 decades,1,2 fueling public health and advocacy efforts to broadcast the danger of BBs for small children. The urgency to endoscopically remove esophageal batteries is now well appreciated, but further consensus on management has been difficult to develop.3–5 From the clinical standpoint, there are 2 specific areas of management where there is considerable controversy and/or ambiguity. First is the postremoval management of children with moderate/severe esophageal injury. Clinicians must first appreciate the spectrum of esophageal and para-esophageal complications associated with BBI in children and the specific management dilemmas encountered. The risk for delayed occurrence of aortoenteric fistula (AEF) days or weeks following BB removal3 further challenges our decision making, specifically around patient disposition after battery removal.
The second controversial area in the management of BBI surrounds the management of asymptomatic patients with batteries beyond the esophagus (eg, intragastric, duodenal, and so forth). Recent expert opinion-based guidelines from the Endoscopy Committee of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) recommended consideration of endoscopic assessment and removal in certain cases of BBI whereby the battery lies beyond the esophagus.5 This recommendation contradicts previous guidelines from the National Battery Ingestion Hotline (NBIH) and the National Capital Poison Center, which had suggested only conservative initial management in asymptomatic children with postesophageal BB.1,6 In this article, the authors review their single-center experience with BBI with the primary aim of presenting data that may help better inform and support management decisions.
BACKGROUND
Ingestion of batteries has long been recognized as a potential health hazard for children.7,8 Voluntary reporting data, as collected through the NBIH and National Poison Data System since the 1980s, has revealed several important trends in the epidemiology of BBI.9 Although the rate of battery ingestion (per million population) has remained stable in children over the past 30 years,1 data from the National Electronic Injury Surveillance System has shown the absolute number of emergency department (ED) visits for battery-related injury has more than doubled from 1990 to 2009.2
More concerning, the rate of significant complications and death resulting from BBI has increased almost 7-fold.1 This emergence of greater BBI-associated morbidity and mortality appeared in the mid 1990s and temporally corresponds to a change in battery production toward larger-diameter, higher-voltage lithium cells. The composition of swallowed batteries has subsequently trended toward larger-diameter lithium batteries, as these are now ubiquitous in the household environment.
More than 90% of serious outcomes from BBI in children between 2000 and 2009 were due to greater than 20-mm diameter lithium cells.1 Because of its size, the 20-to 25-mm diameter lithium BB is more likely to become impacted in the pediatric esophagus compared with the traditional, previously standard, less than 15-mm alkaline BB. Serious outcomes are most common in small children less than 5 years of age.9 Small children are more likely to mouth objects in the environment, and the smaller diameter of the esophagus in young children predisposes to foreign body impaction. More than 50% of serious outcomes due to BBI occur after unwitnessed ingestions, in which case there is likely a delay in recognition and diagnosis.9
Lithium cells are typically 3.0 V, as compared with the 1.5 V of traditional alkaline BBs. The increased voltage is a major factor in the type and degree of injury transmitted by these newer-age batteries as, per Ohm’s law, higher voltage drives an increase in current.
Animal studies have been helpful in understanding the pathophysiology of BBI-caused injury10 to be caustic rather than thermal. When a BB becomes entrapped in the digestive tract, mucosa bridges the positive and negative terminals of the battery, thus completing a circuit and allowing current to flow. Electrical current from the battery results in generation of hydroxide radicals in the esophageal tissue. The presence of hydroxide radicals rapidly raises the pH of the tissue leading to caustic injury and associated coagulative necrosis. Depending on the site of battery impaction, necrosis weakens the esophageal wall over a short period of time and may extend through to adjacent tissue, such as the trachea or great vessels. The process of coagulative necrosis has been demonstrated to start within 15 minutes of contact.10 Even with batteries that have been ingested after use (and presumably without significant residual capacitance), significant injury may still be possible.6 This reality provides further evidence of the power of the newer lithium cells, which have a much longer storage life than traditional alkaline cells.
Most deaths reported due to BBI involve the development of AEF with resulting catastrophic hemorrhage. Data from the National Capital Poison Center indicate that among the 41 reported fatalities, 19 (46.3%) were confirmed to be due to AEF, with another 12 (29.2%) reported as either merely “aortovascular” or unknown.11 Most concerning have been reports of this catastrophic lesion occurring more than 2 weeks after BB removal.3 AEF secondary to BBI has proven to be extremely difficult to manage even when properly recognized. Short- and long-term fatality rates in adult AEF have been reported at 46.8% and 70.3%, respectively.12 There have been a few reported cases of survival in children after AEF from other causes,13,14 but only one after AEF associated with BBI.15 These reports, however, stress the importance of prompt recognition and intervention to maximize the potential for patient survival after BBI.
With the recognition of the increased risk associated with newer-age lithium BBs, public education and advocacy efforts have been launched, resulting in much greater awareness within the medical and parental communities.16,17 Partnerships with industry have led to increased resources to deal with these hazards and, it is hoped, will result in decreased incidence of severe events (BatteryControlled.com). Furthermore, toy manufacturers have largely answered the call to secure the battery compartments in their products, and battery manufacturers have changed packaging to make the batteries more childproof. Most recently, new technology is being developed that would potentially make batteries incapable of transmitting a charge unless firmly seated within a battery compartment, rendering them safe within the human digestive tract.18 For those who work in the clinical setting, however, the increased awareness has resulted in a parallel increase in calls and referrals following BBI. Given the complexity and potential severity each of these cases represents, pediatric departments and EDs have been challenged to develop appropriate clinical care pathways to rapidly assess and manage them.
CASE DESCRIPTIONS
The following 13 cases describe the most significant and severe esophageal BBIs that have occurred in the authors’ institution over a 6-year period, from 2009 to 2015. With each case there have been important lessons to be learned that have subsequently impacted the authors’ institutional approach to managing these patients in the future. These points are highlighted after each vignette, and the impact on clinical care is summarized in the discussion section. Additional data on the timing of BB removal in relationship to the distance from the authors’ institution are presented in Table 1.
Table 1.
Single-center case series of serious BBIs
| Case | Times: Ingestion to Diagnosis, Center to Intervention, Total BB Exposure | Anatomic Location | Distance to Removal Center | Timing to Significant Outcome | CHCO Hospital Duration |
|---|---|---|---|---|---|
| 1 | 2 h, 2.5 h, 6 h | Proximal esophagus | 20 miles | Contained esophageal perforation at 2 d | 6 d |
| 2 | 2 h, 9 h, 15 h | Stomach | 20 miles | Death by exsanguination ~15 h after ingestion | 9 h |
| 3 | 3 h, 3 h, 8 h | Distal esophagus | 25 miles | Readmission at 18 d with death by exsanguination | 5 d; 15 h |
| 4 | 2 h, 1 h, 2.5 h | Proximal esophagus | 20 miles | Ulceration visualized 6 h after ingestion | 15 d |
| 5 | 1 h, 1 h, 2.5 h | Proximal esophagus | 20 miles | Contained esophageal perforation at 4 d | 12 d |
| 6 | Unknown, 4 h, unknown | Unknown; ? esophagus | 10 miles | Death by exsanguination ~6 h after admission | 6 h |
| 7 | 2 d, 1.5 h, 2 d | Proximal esophagus | 175 miles | Ulceration visualized 2 d after ingestion | 8 d |
| 8 | 1 h, 1.5 h, 2.5 h | Distal esophagus | 10 miles | Ulceration visualized at 2.5 h after ingestion | 5 d |
| 9 | 24 h, <2.5 h, 27 h | Proximal esophagus | 30 miles | Contained esophageal perforation at 4 d | 24 d |
| 10 | >2 d, 2 h, >2 d | Midesophagus | 70 miles | Ulceration; esophageal stricture at 4 wk | 7 d |
| 11 | 3 h, <3 h, 6 h | Proximal esophagus | 15 miles | Sinus tract in proximity to R carotid artery at 2 d | 15 d |
| 12 | 3 d, unknown, 3 d | Proximal esophagus | 10 miles | Ulceration; esophageal stricture at 12 wk | 7 d |
| 13 | 3 h, unknown, 7.5 h | Proximal esophagus | 190 miles | Tracheoesophageal fistula at 7 d | 29 d |
Abbreviations: CHCO, Children’s Hospital Colorado; R, right.
BUTTON BATTERY INGESTION CASE SERIES
Case 1
A 2-year-old previously healthy boy presented to the ED after a witnessed BBI. He had one episode of emesis after the ingestion and was drooling on arrival to the ED. Approximately 2 hours after ingestion, a radiologic foreign body series confirmed a retained BB at the proximal esophagus; he was transferred 20 miles to Children’s Hospital Colorado (CHCO). Endoscopic removal was attempted in the procedure center by the gastroenterology team approximately 2.5 hours after arrival. Attempts at removal with flexible endoscopy were unsuccessful because of the dense adhesion of the battery to the esophageal mucosa, despite a total BB exposure time of only 6 hours. The BB was successfully removed by pediatric surgery using rigid esophagoscopy, but a nasogastric tube was unable to be placed because of esophageal edema. The patient was extubated after the procedure and transferred to the inpatient medical floor, where he remained ordered to take nothing by mouth. At 48 hours after removal, a Gastrografin esophagram demonstrated focal perforation of the upper esophagus into the retropharyngeal soft tissues at the level of C4. At 72 hours after removal, a nasogastric tube was placed by interventional radiology and he received enteral nutrition. He was discharged home on hospital day 6 with nasogastric tube feedings. Repeat esophagram 16 days after initial ingestion showed overall improvement but persistence of the esophageal perforation, which ultimately resolved on repeat esophagram 23 days after ingestion. Two days later, the nasogastric tube was removed; he tolerated a regular diet well without further complications. He was subsequently lost to follow-up 1 month after the ingestion, and it is unknown if he ever developed an esophageal stricture.
Lessons Learned
A BB can fuse to the mucosa rapidly, leading to difficult removal that may require rigid esophagoscopy.
Case 2
A 16-month-old previously healthy girl presented to her local ED with 1 day of irritability and approximately 2 ounces of bright red hematemesis. Within 2 hours of initial presentation, an abdominal radiograph was obtained that showed a round, radiopaque foreign body in the abdomen, possibly the transverse colon, suspicious for a BB. She was transferred 20 miles to CHCO ED, where a repeat abdominal radiograph showed an intra-abdominal foreign body consistent with a disc battery; but it was still unclear if it was located in the stomach or colon.
A computed tomography (CT) abdomen without contrast was then used to further delineate the location of the foreign body, which was shown to be in the central portion of the gastric body with a moderate amount of surrounding ingested material. The patient’s vital signs were stable, and she was well appearing without any further hematemesis. In line with the guidelines for gastric BBs, she was scheduled to go to the operating room (OR) for foreign body removal the following morning, which was 7 hours later.
While in the OR preoperative area of the authors’ referral center, within 9 hours of initial presentation to the outside hospital, the patient developed further hematemesis and was taken to the OR for resuscitation because of rapid clinical decompensation. She was intubated and resuscitated with albumin and blood infusions. She suffered 3 episodes of cardiac arrest. During resuscitation, the patient was noted to have many hemorrhages from her mouth and nose despite a large nasogastric tube in place. The procedure was converted to open laparotomy, which revealed a markedly distended stomach with a large clot encasing a 20-mm BB in the fundus. Compression of the abdominal aorta was attempted without achieving control of bleeding; after ongoing resuscitation attempts, she remained asystolic and was pronounced dead in the OR just 15 hours after the initial presentation to our facility.
Autopsy revealed 2 linear midesophageal mucosal erosions, focal collection of blood in the paraesophageal soft tissue adjacent to the erosions, as well as accumulation of blood within the adventitia of the aorta and in the soft tissue of the distal trachea. There were no erosions or ulcerations within the stomach. Cause of death was identified as hypovolemic shock due to ulceration of the midesophagus and hemorrhage from large arterial source due to battery ingestion.
Lessons Learned
Identification of a gastric foreign body does not preclude esophageal injury, especially in unwitnessed ingestions when the total time of BB exposure is unknown. BBs can transiently lodge in the esophagus and cause severe erosion and ongoing injury. Even after passage of the battery to the stomach, necrosis of the esophagus and surrounding tissues is an ongoing process that can lead to fistulization and associated severe outcomes.
Case 3
A 2-year-old previously healthy girl presented to the ED with chest pain, coughing, and vomiting. A chest radiograph 3 hours after presentation showed a round radiopaque 25-mm foreign body in the distal esophagus concerning for BBI, and she was transferred 25 miles to the CHCO ED for further management. Flexible endoscopy was successful in removal of the BB from the distal esophagus, where the underlying tissue was ulcerated and friable (Fig. 1). She was extubated to room air, and repeat complete blood count and chest radiograph in the postanesthesia care unit revealed stable blood counts and no evidence of pneumomediastinum. She was admitted to the inpatient medical floor, where she remained ordered to take nothing by mouth. One day after admission, the esophagram revealed mucosal irregularity and mild narrowing of the distal esophagus in the region of removed BB but no evidence of esophageal perforation/leak. At 48 hours after removal, she was started on a clear-liquid diet, was advanced to a mechanical soft diet at hospital day 4, and was discharged home on hospital day 5.
Fig. 1.
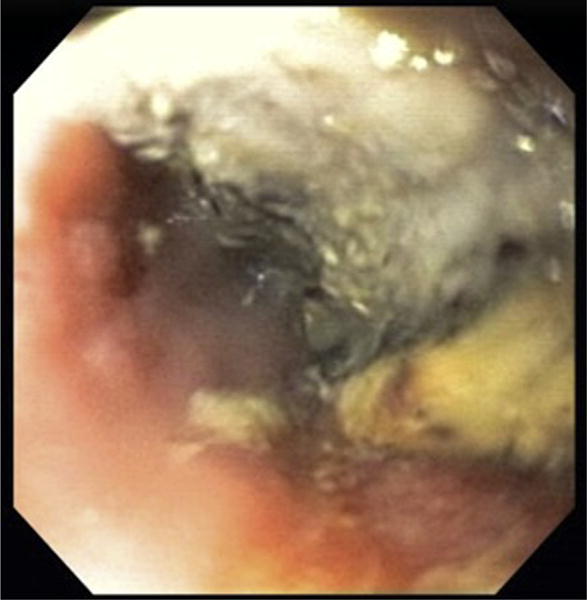
Severe esophageal injury at site of BB removal, with necrosis and eschar.
Thirteen days after discharge (18 days following BB removal), the patient presented to the ED with a history of abdominal pain and diarrhea for 5 days as well as new-onset hematemesis and hematochezia and was admitted to the ICU. Repeat esophagram revealed mucosal irregularity of the distal esophagus without clear stricture or evidence of perforation. In the ICU, she developed hematemesis and shock. Emergent bedside endoscopy revealed an intact lower esophageal ulceration and copious blood and a large clot in the gastric fundus. Endoscopic attempts at hemostasis, including Blakemore tube inflation and epinephrine injections, were unsuccessful; despite 4 hours of aggressive attempts at stabilization and resuscitation, cardiorespiratory support was withdrawn.
Lessons Learned
Despite a reassuring esophagram and clinical stability 5 days after ingestion, devastating hemorrhage from esophageal erosion secondary to BBI can unexpectedly occur weeks out from the initial ingestion. Because of the high arterial pressure from AEF, Blakemore tubes may not be able to control or stabilize bleeding.
Case 4
A 6-year-old previously healthy girl presented to the ED after witnessed BBI. She complained of throat pain and intermittent nonbloody emesis; 2 hours after arrival to the ED, a chest radiograph revealed a BB at the proximal esophagus. She was transferred 20 miles to the CHCO ED, where emergent endoscopic removal of a 20-mm BB by the surgery team was performed. There was extensive proximal esophageal erosion and ulceration despite just 6 total hours of BB exposure. She was extubated after the procedure and transferred to the pediatric ICU (PICU) where she remained ordered to take nothing by mouth on total parenteral nutrition (TPN). Five days after ingestion, MRI of the chest with magnetic resonance angiography showed significant inflammation of the anterior esophageal wall, sparing the posterior wall, without disruption of surrounding vasculature. This study was thought to be reassuring, as no immediate major vessels seemed to be threatened by the location of necrotic injury. On hospital day 7, an esophagram showed mucosal ulceration and probable edema or stricture without visible fistula or evidence of perforation. With these imaging studies, the patient was determined to be at a decreased risk of hemorrhage and perforation. In turn, she was advanced to an oral soft diet and was discharged home on hospital day 15. It was unknown if there were further complications, such as stricture, as she was subsequently lost to follow-up.
Lessons Learned
As mucosal injury occurs with even short exposure to BBs, every effort should be made to expedite removal when possible. MRI is a useful tool for post–battery-ingestion evaluation of the extension of injury beyond the esophagus and may help guide treatment decisions.
Case 5
A 6-year-old boy with a history of repaired tracheoesophageal fistula presented to the ED after witnessed BBI. He was clinically stable, and a chest radiograph demonstrated the BB to be retained in the proximal esophagus. Shortly after presentation (within 1–2 hours), the patient developed hematemesis and vomited up the BB, which was noted to be corroded, and had an adherent blood clot; he was immediately transferred 20 miles to the CHCO ED. Within 1 hour of transfer, endoscopy was performed in the CHCO OR with findings of noncircumferential proximal esophageal ulceration and eschar formation, without bleeding. The BB exposure time at endoscopy was estimated to be 2.5 hours. The patient was extubated and admitted to the general medical floor and was advanced to a soft diet 1 day after admission. Four days later, he developed dysphagia and pain with eating; MRI of the chest revealed a focal fluid collection with a beak directed to the esophagus concerning for contained esophageal perforation. He was made to take nothing by mouth on TPN and placed on intravenous (IV) antibiotics. Seven days later, a repeat MRI showed a persistent esophageal fluid collection with improvement of the proximal esophageal mucosal inflammation. An esophagram demonstrated no extravasation of fluid. On hospital day 8, he was advanced to a soft diet and was discharged home on hospital day 12. A repeat esophagram 1 month after discharge did not demonstrate a leak or stricture; on the follow-up visit 2 years after the initial ingestion, he was tolerating a regular diet without any dysphagia or complications.
Lessons Learned
A total BB exposure time of just 2.5 hours was associated with contained esophageal perforation, giving credence to the growing concern for potential morbidity associated with any BB exposure to the esophageal mucosa. As with other type of esophageal foreign bodies, children with a history of tracheo-esophageal fistula (TEF) have an increased risk of impaction.
Case 6
An 18-month-old previously healthy girl presented to the ED after 24 hours of hematemesis and mild abdominal pain. She was noted on vital signs to be hypotensive and tachycardic, and her laboratory test results revealed normocytic anemia. The patient received IV fluid resuscitation with subsequent normalization of vital signs and was transferred to the PICU for monitoring. In addition, chest and abdominal radiographs were obtained and read as normal, without a visualized foreign body. A nasogastric tube was placed, which showed a small amount of bright red blood in the tube. Consultation with the gastrointestinal (GI) service led to a plan for endoscopy after stabilization and transfusion of packed red blood cells.
Approximately 4 hours after admission to the ICU, the patient developed gasping respirations and clinical decompensation requiring intubation and was noted to have substantial esophageal bleeding. Gastroenterology and surgery coordinated an emergent bedside endoscopy with active resuscitation including chest compressions. On endoscopic intubation of the esophagus, a moderate amount of red blood was flushed away and the visualized esophageal mucosa was not determined to show lesions. The stomach was noted to have a large clot present that could not be suctioned or flushed, without signs of active bleeding. After 2 hours of aggressive resuscitation attempts and just 6 hours after initial presentation, the patient was pronounced dead. Autopsy revealed erosions in the midesophagus extending into the aorta, consistent with injury from a BB, though no battery was identified at any site.
Lessons Learned
Although this case could not be completely confirmed to be secondary to BBI, the opinion of the pathologist and the clinicians involved support this as the most likely underlying cause of death. This case again highlights that the absence of a battery within the esophagus at the time of presentation does not preclude significant injury at some point prior. In otherwise healthy toddlers with acute onset of severe hematemesis, a high index of suspicion for battery ingestion should be maintained.
Case 7
A 2-year-old previously healthy boy presented to his pediatrician’s office with 1 day of fever, sore throat, and nonbloody emesis. He was initially treated with azithromycin; but after he developed food refusal the following day, a chest radiograph was obtained that showed a BB in the proximal esophagus. The patient was transferred 175 miles to the CHCO ED and had endoscopic removal in the OR 1.5 hours after transfer. Before removal, surgery and cardiothoracic surgery were called and placed on standby as an additional precautionary measure because of the prolonged time of BB exposure. Flexible esophagosocopy by gastroenterology and rigid esophagoscopy by otolaryngology were initially unsuccessful in removal. Otolaryngology then used a Miller laryngoscope and alligator forceps and successfully removed the battery. Subsequently, there was concern for circumferential necrotic ulceration where the BB had been impacted, and a nasogastric tube was placed. The patient was extubated to room air and transferred to the medical inpatient floor where he remained ordered to take nothing by mouth.
The following day, a CT angiogram of the neck showed no evidence of soft tissue or vessel injury, and an esophagram showed no evidence of perforation. The patient’s diet was advanced to clears by mouth and nasogastric feeds on hospital day 2. A repeat esophagram on hospital day 7 showed extensive mucosal irregularity in the proximal esophagus, extending 3.5 cm, which represented mucosal ulceration. On hospital day 8, repeat CT angiogram again did not show evidence of injury to large vessels. The patient was discharged home on hospital day 8 on a combination of nasogastric feeds and a limited amount of a soft mechanical diet. He was quickly weaned from nasogastric tube feeds; at the follow-up visit 4 months after discharge, he had no difficulties with oral intake.
Lessons Learned
Coordination between gastroenterology and otolaryngology and precautionary measures with surgery and cardiothoracic surgery on standby allowed for a well-controlled environment with prompt removal of the BB in this clinical scenario that was at high risk for morbidity/mortality because of 48 hours of esophageal BB exposure. In this case, neither flexible nor rigid esophagoscopy was able to remove the battery; but a laryngoscope with alligator forceps was effective.
Case 8
A 4-year-old previously healthy boy presented to a local urgent care with abdominal pain and chest pain and a self-report of swallowing a magnet. Within 1 hour of ingestion, chest and abdominal radiographs confirmed a retained BB in the distal esophagus; he was transferred 10 miles to a CHCO satellite campus where he vomited up a 19-mm BB. Endoscopy approximately 2.5 hours after the initial diagnosis demonstrated 2 small linear erosions of the distal esophagus with surrounding dusky mucosa concerning for necrosis. He was transferred to the CHCO main campus PICU for monitoring. One day after removal, a CT angiogram of the neck showed no large vessel injury; on hospital day 4, an MRI of the chest showed no evidence of aortoesophageal fistula. He was started on an oral soft mechanical diet, which he tolerated well, and discharged home on hospital day 5. Three weeks later, a follow-up esophagoscopy showed healing ulcers without stricture formation. The patient was lost to follow-up after this procedure.
Lessons Learned
CT angiography and MRI can be used concurrently to help estimate the risk of injury beyond the esophagus and to guide treatment decisions, including discharge planning from the ICU as well as when to initiate feeding.
Case 9
An 11-month-old previously healthy boy presented to his pediatrician with 24 hours of cough, increased oral secretions, refusal to eat, and fever. A chest radiograph showed a retained proximal esophageal BB, and he was transferred 30 miles to a local ED for further management. Removal of the BB with esophagoscopy by otolaryngology in the local ED within 3 hours after initial diagnosis was difficult but successful. After battery removal, laryngoscopy was noted to reveal circumferential ulceration in the proximal esophagus.
The patient was then transferred to the CHCO PICU and ordered to take nothing by mouth on IV fluids. On hospital day 2, an esophagram showed significant esophageal wall irregularity and deep mucosal ulceration along the posterior lateral wall, without evidence of perforation or fistulous tract formation. On hospital day 3, endoscopy demonstrated severe edema, exudates, and necrosis of the proximal esophagus. A nasojejunal tube was placed. Rigid bronchoscopy and laryngoscopy showed vocal cord paralysis but with normal trachea.
An MRI of the chest with angiogram on hospital day 4 showed extensive periesophageal inflammatory changes tracking between the esophagus and trachea, with a localized perforation along the left cervical esophagus, as well as loculated pockets of fluid extending into the mediastinum between the proximal right innominate artery and the left common carotid artery without disruption of the vessels. On hospital day 5, nasojejunal feedings were started and tolerated well. Repeat endoscopy 2 days before discharge showed healing ulcers without stricture formation. However, because of the anticipated prolonged duration of tube feedings due to aspiration from vocal cord paralysis, a gastrostomy tube was placed simultaneously.
Repeat esophagram was normal before discharge, and he went home on hospital day 24 with gastrostomy tube feeds and an oral pureed diet. In the follow-up visit 3 months after discharge, he continued on oral purees and gastrostomy tube feeds because of persistent aspiration from vocal cord paralysis, without evidence of stricture formation on repeat esophagram.
Lessons Learned
Morbidity and mortality associated with BBI is not strictly limited to vascular injury and bleeding events but also includes vocal cord paralysis and perforation.
Case 10
A 15-month-old previously healthy girl presented to the pediatrician’s office with a barking cough for 1 week and 2 days of decreased oral intake and fever. She had progressive coughing and sputtering with eating, and the follow-up visit with a chest radiograph showed a midesophageal BB. She was transferred 70 miles to the CHCO ED, where she was taken to the hybrid OR within the cardiac catheterization laboratory, with endoscopic removal by gastroenterology performed within 2 hours of transfer in the presence of interventional cardiology and cardiothoracic surgery. Because of the high risk and concern for AEF formation because of the long duration of battery impaction in this case, arteriogram of the aorta was performed before removal and showed the BB to be approximately 3 to 4 mm from the aortic arch. This distance was thought to be reasonably safe to allow endoscopic removal without surgical intervention. On endoscopic removal of the BB, there were 2 large ulcerations of the midesophagus with friability and edema.
The patient was extubated after the procedure and transferred to the PICU, where she was made to take nothing by mouth and started on TPN. Her hospital course was complicated by left leg hypoperfusion secondary to focal occlusive thrombus in the proximal left superficial femoral artery from the cardiac catheterization, which was treated with continuous heparin for 4 days and then stopped because of the risk of esophageal ulceration bleed. On hospital day 3, an MRI of the chest with angiogram showed circumferential periesophageal wall thickening extending 6.8 cm and separated by 4 mm from the descending thoracic aorta at the level of the aortic arch, with the esophageal lumen separated from the proximal descending thoracic aorta by 1 cm. The lack of progression of injury on MRI was assessed to be reassuring; on hospital day 4, she was started on a soft mechanical diet, which she tolerated well up to discharge on hospital day 7.
Approximately 4 weeks after ingestion, an esophagram showed a focal stricture of the patient’s upper esophagus, requiring esophageal dilation and localized injection of steroid at the stricture site. She has not been reevaluated since her procedure and is now considered lost to follow-up.
Lessons Learned
Endoscopic removal in the cardiac catheterization laboratory OR with fluoroscopic guidance and arteriogram of the aorta allowed direct visualization of the BB and proximity to the aorta, which improved preparedness for potential complications to the multidisciplinary team involved in the procedure. The use of arteriography, however, does carry the risk of thrombus formation, which must be weighed against the benefit of identifying proximity of injury to the aorta.
Case 11
A 4-year-old previously healthy girl presented to a local ED with drooling and self-reported, unwitnessed FBI. Chest radiograph 3 hours after presentation confirmed a proximal esophageal BB; she was taken to the OR for removal by otolaryngology approximately 6 hours after presentation to the ED, with mild edema and irritation of the proximal esophagus on removal of the battery. The patient was subsequently transferred to the CHCO medical inpatient floor, where she remained ordered to take nothing by mouth. One day after admission, an esophagram demonstrated mild cervical esophageal edema/irregularity without stricture; she was started on a clear-liquid diet. Because of pain and difficulty swallowing on hospital day 3, she had a repeat endoscopy that showed severe ulceration of the proximal esophagus and had an MRI of the chest with angiogram that demonstrated formation of a sinus tract from the right lateral wall of the esophagus, in close proximity to her right carotid artery. She was immediately made to take nothing by mouth, transferred to the PICU, and started on TPN.
A repeat esophagram on hospital day 7 showed no perforation, and a repeat MRI of the chest with angiogram on hospital day 9 showed no evidence of arterial or venous irregularity at the site of prior sinus tract formation. She was started on a soft mechanical diet on hospital day 11, which was tolerated well without complication; she was discharged home on a regular diet on hospital day 15. One month after discharge, the patient was assessed to be doing well without dysphagia, with no stricture noted on repeat esophagram.
Lessons Learned
Despite minimal findings of edema and ulceration on initial esophagoscopy at removal of the BB, esophageal necrosis and surrounding inflammation progresses despite no further exposure, making timing of associated morbidity from BB exposure somewhat unpredictable. Although there was no clinical vascular complication in this case, MRI helped to evaluate the risk and take appropriate precautionary measures until subsequent imaging showed resolution of potential danger to vascular structures.
Case 12
A previously healthy 20-month-old girl presented to her local ED with 2 days of drooling, congestion, fever, vomiting, retching, and dysphagia. In the ED, she had labored breathing and refusal to move her neck; a CT of her neck showed a retained proximal esophageal BB. A 25-mm BB was removed in the OR by otolaryngology; surrounding mucosa showed erythema, ulceration, and necrosis. A nasogastric tube was placed, and the patient was transferred to the CHCO PICU. On hospital day 2, an MRI of the chest showed inflammatory changes, with wall thickening noted to be most extensive in the posterior esophageal wall, with no evidence of approximation between the esophagus and large vessels. On hospital day 3, the patient underwent a repeat esophagoscopy that demonstrated severe ulceration without evidence of stricture or fistula; she started a limited clear-liquid diet and nasogastric tube feedings. She was discharged home on hospital day 7 on a regular diet. The patient subsequently complained of dysphagia and blood tinged spit-up at the follow-up 1 month later, and endoscopy showed a mild esophageal stricture that was dilated. She has had no further dysphagia since esophageal dilation and remains clinically well 10 months after discharge.
Lessons Learned
Stricturing of the esophagus can be a common complication after BB exposure but does not often present before 4 weeks after initial ingestion.
Case 13
A 20-month-old boy developed drooling, watery eyes, neck pain, and neck extension and was taken to a local ED because of suspected FBI. A chest radiograph 3 hours after the onset of symptoms demonstrated a retained proximal esophageal BB, and he was transferred 187 miles to CHCO for removal. Endoscopic removal of the battery was performed 7.5 hours after diagnosis and demonstrated circumferential necrosis. A nasogastric tube was placed, and the patient was transferred from the OR to the CHCO PICU with continued mechanical ventilation via endotracheal intubation for further management. MRI of the neck/chest with angiography on hospital day 1 showed esophageal wall thickening and paraesophageal inflammation most pronounced at the level of the aortic arch, with a paraesophageal fluid collection just above the aortic arch without compromise of the surrounding vasculature. An esophagram showed no evidence of perforation, and he was extubated after repeat endoscopy showed healing ulceration on hospital day 5. Four days later, he developed biphasic stridor and fever and was urgently intubated. Subsequently he was found to have vocal cord paralysis, with bronchoscopy demonstrating an 11-mm tracheal erosion with communication to the mediastinum and the tip of the endotracheal tube terminating in the esophagus. Because of persistent fevers and concern for mediastinitis that was unresponsive to intravenous antibiotics, the patient underwent diversion of the proximal esophagus to a spit fistula and temporary closure of the distal esophagus as well as gastrostomy tube placement for nutritional support.
During the patient’s prolonged hospitalization, he underwent microlaryngoscopy with bronchoscopy 5 times, with the final bronchoscopy before discharge showing persistent tracheoesophageal fistula and left vocal cord paralysis. The patient was discharged home on hospital day 29 with gastrostomy tube feeds and a pureed oral diet. One month after discharge, he was readmitted for 24 hours because of a spit fistula stricture that was dilated.
The patient was scheduled for repeat endoscopy approximately 3 months after initial ingestion that showed marked improvement and a well-healed tracheoesophageal fistula. In turn, he underwent a takedown of cervical esophagostomy with cervical esophageal anastomosis followed by a 14-day hospitalization for recovery. Repeat esophagram has demonstrated anastomotic cervical esophageal leak; but because of financial stressors, the patient has not returned for recommended evaluation, including repeat esophagram, esophagoscopy with possible dilation, bronchoscopy for vocal cord assessment, and swallow evaluation.
Lessons Learned
Respiratory symptoms after battery removal should prompt emergent evaluation for vocal cord and tracheal complications, including tracheoesophageal fistula.
Summary Data
Although these data do not encompass the numerous calls the authors’ institution receives on a regular basis regarding more benign cases of BBI (beyond the esophagus and estimated to be at low risk for esophageal injury), it does illustrate the spectrum of severe morbidity and mortality that occur when there is significant esophageal injury. In this series of 13 severe cases, 4 (30.8%) resulted in esophageal perforation, 3 (23.1%) developed an esophageal stricture, and 2 (15.4%) required gastrostomy placement. Mortality in this series of patients with severe esophageal injury from BBI was 23.1%. For survivors, the average hospital stay was 12.1 days.
DISCUSSION
Initial Presentation and Assessment
Successful management of BBIs demands a multidisciplinary approach and coordinated care across the ED, anesthesia, pediatric gastroenterology, pediatric surgery, otolaryngology, cardiothoracic surgery, and radiology physicians. First contact may occur by phone from a referring institution or from direct presentation in the ED. In general, any child presenting to the ED with symptoms consistent with a foreign body should have both anteroposterior and lateral films of the chest and airway to help differentiate the ubiquitous coin ingestions from BB.19 Careful examination of these films for the halo sign, as well as the step-off between the positive and negative nodes of BBs, should be performed. If a BB is found, orientation of the slightly smaller negative pole (anode) should be noted, as this is the direction of most serious injury.
Once the diagnosis of an esophageal BBI is confirmed, rapid assessment of the risk level must be performed in order to mobilize the appropriate resources. This initial assessment should minimally include the age of the patient, size of the battery, timing of ingestion, and current location of the battery, whenever possible. These factors encompass the most important risk factors for predicting severe injury. As illustrated in the cases discussed earlier and from the national data,11 esophageal impaction at the level of the aortic arch, age less than 5 years, battery size of 20 mm or greater, and prolonged time of impaction are all factors that should prompt the greatest level of concern. Similarly, a child who has recently undergone endoscopic removal of a battery and then presents with any degree of hematemesis or coffee-ground emesis should be considered as an impending AEF and treated accordingly.
Recommended indications for endoscopic intervention in cases of BBI beyond the esophagus in asymptomatic patients are variable across published guildelines.1,5,6 Based on most of the national data, which shows postesophageal batteries have not been associated with significant morbidity and mortality, guidelines from the NBIH1 and the Button Battery Taskforce6 currently advocate abdominal radiographs and observation in asymptomatic patients. In higher-risk patients (<6 years of age and BB 15 mm), the radiograph is in 4 days and 10 to 14 days in low-risk patients. These guidelines do advocate for endoscopic removal in high-risk asymptomatic patients if the battery is still in the stomach after 4 days.
However, more recent recommendations5 by the Endoscopy Committee of the NASPGHAN call for consideration of endoscopic intervention even in cases of asymptomatic postesophageal BBI in high-risk patients (aged <5 years, BB ≥ 20 mm). The rationale for this more conservative guideline is not primarily due to concerns regarding the risk of gastric injury, though this has been reported.20 It is instead based on concerns for unrecognized esophageal injury before passage into the stomach, as noted in 2 of the fatalities cited earlier (case 2 and case 6). The role of endoscopy is, therefore, primarily diagnostic, rather than the therapeutic removal of the battery itself. In this fashion, one may consider radiographic studies (CT, esophagram) as alternative methods to assess for unrecognized esophageal injury. Nevertheless, these have the disadvantage of not allowing for removal of the battery and may be less sensitive than endoscopy. (MRI is contraindicated with a metallic foreign body present.)
In addition to mobilizing all the necessary personnel, critical management decisions include whether endoscopic intervention is needed as well as what is the most appropriate site for the procedure. Location of endoscopic intervention may vary by case and by institution, depending on what resources are available and the timing of presentation. At the authors’ institution, with the highest-risk cases, they have found that the cardiac catheterization laboratory (case 10) has offered the best combination of imaging capability and ability to convert to an open surgical case. In cases whereby there is less suspicion for direct aortic involvement but still concerns about hemorrhage or the ability to remove the battery with a flexible endoscope, the general OR may be the most appropriate choice. In lower-risk cases, whereby the battery has already passed into the stomach or beyond, but the endoscopic assessment of any subsequent esophageal injury is desired, a well-equipped endoscopic procedure unit may be used.
In addition to determining the appropriate venue for endoscopic removal, timing of removal and a corresponding anesthesia/sedation plan are needed. In the case of an esophageal BBI, there is an obvious premium on removal as urgently as possible. With the potential for long-term injury in as short as 15 minutes after impaction,10 the sooner removal is achieved the better. In the authors’ institution, triage guidelines for surgical and endoscopic procedures have been created that characterize BB removal at the highest priority level. With this designation, the authors’ institutional goal is to have patients in the OR within 60 minutes of entry into the facility.
Achieving this level of response requires rapid and efficient communication between all of the medical and surgical subspecialists appropriate for the case. Principal among these is anesthesiology. With the emphasis on rapid preparation for surgical/endoscopic intervention, usual nothing-by-mouth guidelines are circumvented, by definition. As with all FBI cases, the airway must be secured and protected, especially with the potential for a full stomach. Therefore, rapid sequence intubation will likely be needed.
ENDOSCOPIC REMOVAL
After the decision of where to perform the removal and the assembly of the appropriate personnel for the procedure, the specifics of the removal itself should be determined. As illustrated in case 10, in high-risk cases whereby esophageal impaction has been prolonged and injury to vascular structures is suspected, localization of the battery in relation to the aorta and other large vessels through angiography may be performed immediately before endoscopic removal. Although this may further delay actual removal by up to 30 minutes, in cases whereby there has already been prolonged exposure of the tissue, this additional delay may be negligible compared with the value of determining proximity to the aorta.
In terms of actual endoscopic removal, use of the smallest gastroscope available that still has a 2.8-mm biopsy channel is advised to allow the use of the full complement of foreign body retrieval devices. In the authors’ institution, this is the Olympus GIF-160 (Olympus America, Center Valley, PA, USA), with an outer diameter of 8.6 mm. Although newer endoscopes have better optics and field of view, the narrower diameter may provide some additional measure of safety in preventing perforation, as most of these patients with BBI are younger than 4 years of age. In larger patients, the additional 0.5 to 1.0 mm in diameter may be negligible in terms of increased risk.
Once the battery is visualized within the esophageal lumen, the depth (in centimeters) and orientation of the impaction should be noted as best as possible. Examination of the surrounding tissue for eschar formation and fusion to the surface of the battery may help indicate how difficult removal will be. Although gastric batteries may be effectively removed with nets, these may be difficult to pass between the battery and esophageal mucosa and are typically not helpful when the battery is adherent to the esophagus. Within the esophagus, grasping devices are usually most successful. In the authors’ institution, the use of the Raptor forceps (BX00711177, US Endoscopy, Mentor, OH, USA) has been effective in most cases. The combination of alligator and rat tooth jaws helps provide a firm grip in the crevice between the positive and negative poles of the battery. Nevertheless, the authors’ experience has also dictated that, in some instances, as in case 1, the battery is so densely adherent to the mucosa that flexible endoscopy tools are not able to generate enough traction for removal necessitating the use of rigid esophagoscopy.
Alternatively, a case report has been published on the use of a modified magnet endoscope to capture esophageal BBs that were not retrievable with conventional devices.21 In this report, a magnet head tube (Cook Co, Bloomfield, IL, USA) was attached to an infant endoscope, with a 0.5-cm step-off between the tip of the endoscope and the end of the magnet tube. With a battery firmly fused to the mucosa, however, the authors suspect it would still be unlikely that a magnet would provide sufficient traction.
POSTREMOVAL EVALUATION
After battery removal, the scope should be reinserted into the esophagus and another careful examination of the mucosa performed to better assess the severity and location of any injury as well as to determine the most likely complications (Fig. 2). Trauma to the anterior aspect of the esophagus prompts greater concern for vascular and tracheal injury, whereas posteriorly oriented inflammation has been associated with the development of spondylodiscitis.22 Anterior injury in the proximal esophagus should prompt concern for thyroid artery involvement or tracheoesophageal fistula as well as vocal cord injury (case 9). Location in the midesophagus should evoke the greatest concern for AEF. Although injury in the distal esophagus is perhaps reassuring against atrioesophageal complications, one of the 3 fatalities in this series (case 3) did show erosion at this level; caustic burns anywhere in the esophagus have the potential to result in perforation and stricture formation. Circumferential involvement in particular should increase concerns about long-term complications of stricture or stenosis, as seen in cases 10, 12, and 13.
Fig. 2.
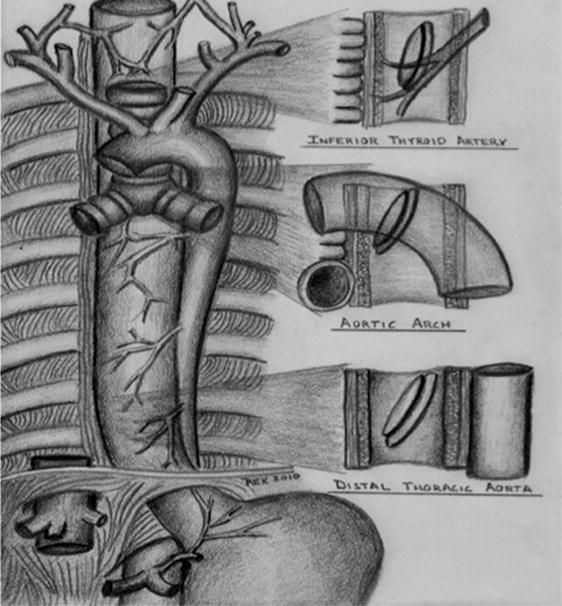
Sites of esophageal button battery impaction and related risk of injury.
After reexamination of the esophagus, passage of the endoscope into the stomach and proximal duodenum to exclude additional foreign bodies is prudent, presuming that this is not hampered by esophageal trauma and/or edema.
POSTREMOVAL MANAGEMENT
Postendoscopy management is perhaps the most difficult and controversial aspect of the care of these patients. The level of care necessary depends highly on the location, duration, and difficulty of removal of the BBI. In more than half of the cases (63.6%) in the authors’ institution when removal was performed, patients were admitted to the PICU for monitoring, with a trend toward a lower threshold in more recent years. Patients are generally taking nothing by mouth for a variable amount of time (range 1–29 days), depending on the degree of injury and the risk of complications. As in 5 of the cases described earlier, a nasogastric tube may be placed to initiate enteral nutrition.
The role of repeat endoscopy in the management of these patients is also ripe for debate. Although others have cited the value of a second-look endoscopy 2 to 4 days after ingestion to help determine the timing of feeding introduction,23 based on what we now appreciate to be the pathophysiology of injury in these cases, such timing for a second look may lead to false reassurance about continued risks for complications. In the authors’ series, a repeat endoscopy was performed before patient discharge in 5 patients (38.5%).
Over time, the authors’ center has come to favor MRI for evaluation after removal in order to assess the proximity of submucosal and extraesophageal injury to the aorta and other important structures (Fig. 3). In cases whereby the extent of injury has been beyond 3 mm from the aorta, it has been thought to be safe to reinitiate feeds (case 10). Although most of these patients will still require anesthesia to perform MRI, the value of this modality over endoscopy is the less invasive nature as well as the ability to follow the evolution of unseen injury over time and determine when inflammation is receding away from the vascular structures. The authors have found this information to be invaluable in making management decisions, such as when to start oral feeds, transfer from the PICU, and discharge home. With the potential for catastrophic complications several weeks after removal, this modality seems the most promising for stratifying risk.
Fig. 3.

T1 MRI with contrast 5 days after BB removal showing persistent inflammation anterior to esophagus (black arrow) above aortic arch (white arrow).
Esophagram is another useful noninvasive study for assessing injury, primarily for the purpose of detecting perforation and/or stricture formation. It is obviously prudent to use water-soluble contrast in these cases whereby the perforation risk is relatively high. In the authors’ institution, an initial esophagram is typically performed 1 to 7 days after battery removal, with a repeat study 7 to 14 days later.
Discharge criteria for patients with injury after BBI have generally been either tolerance of oral feeds or stable tube feeds (nasogastric or via gastrostomy), along with reassuring indications that their injury is not involving any vascular structures. However, even with these criteria met, there may be fatality (as in the authors’ case 3), which can occur many days after discharge and more than 2 weeks after successful battery removal. The details of case 3 highlight the danger of ongoing injury and the importance of continued vigilance necessary to manage these patients. Factors such as the reliability of the family to return for follow-up visits as well as the distance patients live from the responsible medical providers need to be carefully considered before discharge. Exhaustive discharge instructions need to be provided that outline the signs and symptoms of upper GI bleeding. Use of acid blockade to minimize the impact of acid reflux on the esophageal injury has not been studied but would seem well justified. Minor sentinel bleeding has been noted in the authors’ patients (cases 2, 3, and 6) and others before impending AEF hemorrhage and should prompt immediate referral and emergent activation of the cardiothoracic team. At some point during patient care, cases should be reported to the National Battery Ingestion Hotline (US phone number: [202] 625–3333).
Follow-up care for patients after BBI is essential to assess for midterm complications (ie, bleeding) and long-term sequelae (ie, stricture formation). In most cases of significant esophageal injury (and especially those with circumferential injury), a repeat esophagram 4 weeks after removal is prudent to assess for stricture. If this is normal and patients are asymptomatic, no additional surveillance is necessary unless feeding issues develop. In the event of a stricture, endoscopic dilation should be considered promptly (as illustrated by case 10), as 4 weeks should represent sufficient healing time to minimize perforation risk. Respiratory issues should prompt evaluation for tracheal erosion/injury. See Fig. 4 for an algorithm summarizing the suggested management of BBI in children.
Fig. 4.
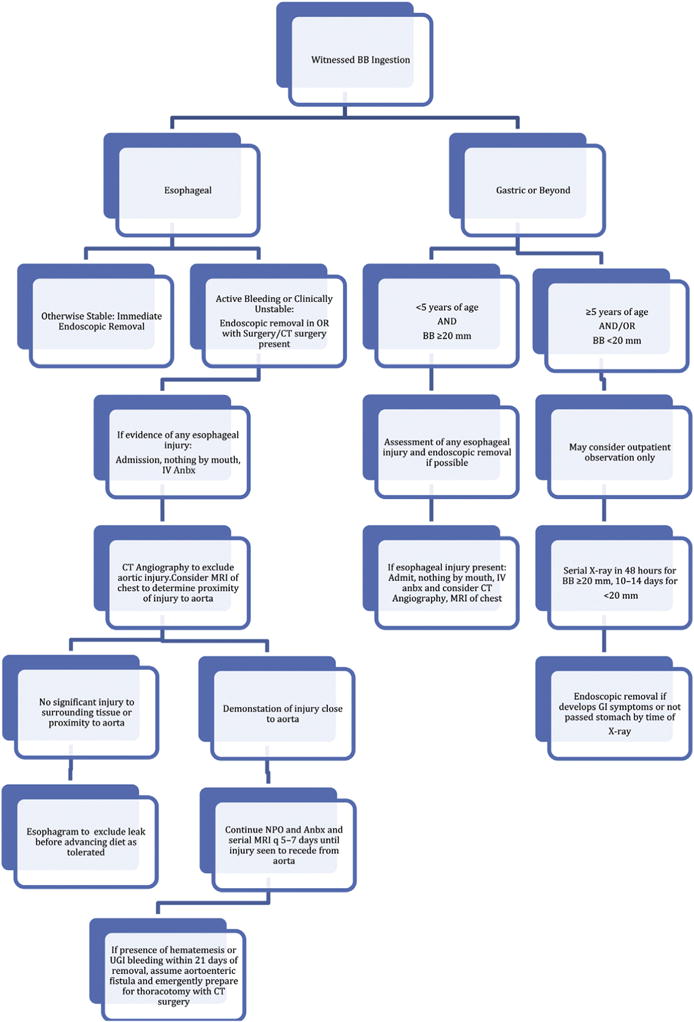
Suggested algorithm for management of BBIs in children. Anbx, antibiotics; UGI, upper gastrointestinal. (Adapted from Kramer RE, Lerner DG, Lin T, et al. Management of ingested foreign bodies in children: a clinical report of the NASPGHAN Endoscopy Committee. J Pediatr Gastroenterol Nutr 2015;60(4):564; with permission.)
KEY POINTS.
Button battery ingestions are the most dangerous form of foreign body ingestion commonly encountered in pediatrics.
A multidisciplinary approach is needed to most effectively manage these patients, including emergency medicine, anesthesia, pediatric gastroenterology, pediatric surgery/cardiothoracic surgery, otolaryngology, interventional cardiology, and radiology.
Even after removal of the battery from the esophagus, there may be ongoing evolution of the injury for up to several weeks thereafter, placing patients at risk for a catastrophic aortoesophageal fistula or other severe sequelae.
Endoscopic intervention for asymptomatic gastric button batteries remains controversial but may be considered in high-risk patients in order to evaluate for esophageal injury.
Surveillance of esophageal injury with MRI may be used to stratify the risk of severe hemorrhage and guide management decisions.
Footnotes
Disclosure: The authors have no significant financial relationships to disclose related to the content of this article.
References
- 1.Litovitz T, Whitaker N, Clark L, et al. Emerging battery-ingestion hazard: clinical implications. Pediatrics. 2010;125(6):1168–77. doi: 10.1542/peds.2009-3037. [DOI] [PubMed] [Google Scholar]
- 2.Sharpe SJ, Rochette LM, Smith GA. Pediatric battery-related emergency department visits in the United States, 1990–2009. Pediatrics. 2012;129(6):1111–7. doi: 10.1542/peds.2011-0012. [DOI] [PubMed] [Google Scholar]
- 3.Brumbaugh DE, Colson SB, Sandoval JA, et al. Management of button battery-induced hemorrhage in children. J Pediatr Gastroenterol Nutr. 2011;52(5):585–9. doi: 10.1097/MPG.0b013e3181f98916. [DOI] [PubMed] [Google Scholar]
- 4.Russell RT, Griffin RL, Weinstein E, et al. Esophageal button battery ingestions: decreasing time to operative intervention by level I trauma activation. J Pediatr Surg. 2014;49(9):1360–2. doi: 10.1016/j.jpedsurg.2014.01.050. [DOI] [PubMed] [Google Scholar]
- 5.Kramer RE, Lerner DG, Lin T, et al. Management of ingested foreign bodies in children: a clinical report of the NASPGHAN Endoscopy Committee. J Pediatr Gastroenterol Nutr. 2015;60(4):562–74. doi: 10.1097/MPG.0000000000000729. [DOI] [PubMed] [Google Scholar]
- 6.Jatana KR, Litovitz T, Reilly JS, et al. Pediatric button battery injuries: 2013 task force update. Int J Pediatr Otorhinolaryngol. 2013;77(9):1392–9. doi: 10.1016/j.ijporl.2013.06.006. [DOI] [PubMed] [Google Scholar]
- 7.Dinary G, Rosenbach Y, Zahavi I, et al. Hazards of button battery ingestion by children. Harefuah. 1983;105(11):361–2. [in Hebrew] [PubMed] [Google Scholar]
- 8.Litovitz TL. Button battery ingestions. A review of 56 cases JAMA. 1983;249(18):2495–500. [PubMed] [Google Scholar]
- 9.Litovitz T, Whitaker N, Clark L. Preventing battery ingestions: an analysis of 8648 cases. Pediatrics. 2010;125(6):1178–83. doi: 10.1542/peds.2009-3038. [DOI] [PubMed] [Google Scholar]
- 10.Tanaka J, Yamashita M, Kajigaya H. Esophageal electrochemical burns due to button type lithium batteries in dogs. Vet Hum Toxicol. 1998;40(4):193–6. [PubMed] [Google Scholar]
- 11.Center NCP. Fatal button battery ingestions: 41 reported cases. Case data on BBI fatalities to date. 2015 Available at: http://www.poison.org. Accessed June 15, 2015.
- 12.Akashi H, Kawamoto S, Saiki Y, et al. Therapeutic strategy for treating aortoesophageal fistulas. Gen Thorac Cardiovasc Surg. 2014;62(10):573–80. doi: 10.1007/s11748-014-0452-4. [DOI] [PubMed] [Google Scholar]
- 13.Hill SJ, Zarroug AE, Ricketts RR, et al. Bedside placement of an aortic occlusion balloon to control a ruptured aorto-esophageal fistula in a small child. Ann Vasc Surg. 2010;24(6):822.e8–9. doi: 10.1016/j.avsg.2009.12.016. [DOI] [PubMed] [Google Scholar]
- 14.Sigalet DL, Laberge JM, DiLorenzo M, et al. Aortoesophageal fistula: congenital and acquired causes. J Pediatr Surg. 1994;29(9):1212–4. doi: 10.1016/0022-3468(94)90803-6. [DOI] [PubMed] [Google Scholar]
- 15.Spiers A, Jamil S, Whan E, et al. Survival of patient after aorto-oesophageal fistula following button battery ingestion. ANZ J Surg. 2012;82(3):186–7. doi: 10.1111/j.1445-2197.2011.05984.x. [DOI] [PubMed] [Google Scholar]
- 16.Button Battery Task Force: the hazards of button batteries. Available at: http://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/Pages/Button-Battery.aspx. Accessed June 15, 2015.
- 17.Coin lithium battery safety. Available at: http://www.energizer.com/responsibility/coin-lithium-battery-safety. Accessed June 15, 2015.
- 18.Laulicht B, Traverso G, Deshpande V, et al. Simple battery armor to protect against gastrointestinal injury from accidental ingestion. Proc Natl Acad Sci U S A. 2014;111(46):16490–5. doi: 10.1073/pnas.1418423111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thabet MH, Basha WM, Askar S. Button battery foreign bodies in children: hazards, management, and recommendations. Biomed Res Int. 2013;2013:846091. doi: 10.1155/2013/846091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Honda S, Shinkai M, Usui Y, et al. Severe gastric damage caused by button battery ingestion in a 3-month-old infant. J Pediatr Surg. 2010;45(9):e23–6. doi: 10.1016/j.jpedsurg.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 21.Soong WJ, Yuh YS. Ingested button battery retrieved by a modified magnet endoscope. J Chin Med Assoc. 2007;70(3):132–5. doi: 10.1016/S1726-4901(09)70344-2. [DOI] [PubMed] [Google Scholar]
- 22.Tan A, Wolfram S, Birmingham M, et al. Neck pain and stiffness in a toddler with history of button battery ingestion. J Emerg Med. 2011;41(2):157–60. doi: 10.1016/j.jemermed.2010.02.027. [DOI] [PubMed] [Google Scholar]
- 23.Ruhl DS, Cable BB, Rieth KK. Emergent treatment of button batteries in the esophagus: evolution of management and need for close second-look esophagoscopy. Ann Otol Rhinol Laryngol. 2014;123(3):206–13. doi: 10.1177/0003489414522969. [DOI] [PubMed] [Google Scholar]


