The term “resistant hypertension” has been used since the early 1960's to identify patients with difficult-to-treat hypertension, meaning mostly, resistance to pharmacologic therapy.1 In the five decades since the term was seemingly first applied, resistant hypertension has been consistently defined as failure to control high blood pressure despite of use of 3 or more antihypertensive agents of different classes, including a diuretic.2-5 The 2008 American Heart Association Scientific Statement on resistant hypertension included in its definition patients whose blood pressure had been uncontrolled with 3 medications, but controlled with 4 or more medications.4 While the number of medications required to satisfy the definition is arbitrary, the purpose of creating a category of resistant hypertension is to identify patients who, because of the difficulty in controlling their blood pressure, may benefit from special diagnostic and therapeutic considerations, including referral to a hypertension specialist. Having an agreed upon definition that can be reliably applied to different cohorts has also facilitated research for this subgroup of patients, including identification of risk factors and underlying mechanisms, assessing outcomes and developing targeted treatments.
The term “refractory hypertension” has often been used interchangeably with “resistant hypertension” to also refer to patients with difficult-to-treat hypertension.1-3, 5 However, based on the number of respective PubMed citations resistant hypertension has been used much more often than refractory hypertension to indicate patients with hypertension resistant to pharmacologic treatment.
Recently, the term “refractory hypertension” has been applied to a very small group of patients who are truly refractory to treatment, that is, patients who fail to achieve target blood pressure on maximal antihypertensive therapy.6 Determining whether such patients simply represent extreme cases of resistant hypertension or a novel phenotype in terms of risk and etiology has been the focus of initial attempts to define and characterize the phenotype and potentially identify mechanisms of antihypertensive treatment failure. In this brief review, we discuss the emerging data pertaining to this novel phenotype of antihypertensive treatment failure and how it compares and contrasts with resistant hypertension in terms of definition, prevalence, patient characteristics, risk factors, and possible underlying etiologies. We hope that an early discussion of the 2 phenotypes will serve to distinguish refractory from resistant hypertension and engender further research testing the clinical significance of that distinction.
Definition
Resistant Hypertension
Although arbitrary in the number of medications required, resistant hypertension has been largely defined as hypertension that is uncontrolled despite use of 3 or more antihypertensive medications, including, if tolerated, a diuretic.4, 5 The AHA Scientific Statement extended the definition to include patients whose blood pressure was uncontrolled with 3 medications, but was subsequently controlled with use of 4 or more medications, that is, “controlled resistant hypertension”.4
Refractory Hypertension
The definition of refractory hypertension has evolved during the short time that the phenotype has been used to specifically reference patients who fail maximal antihypertensive treatment. The phenotype of refractory hypertension was first proposed in a retrospective analysis of patients referred to the University of Alabama at Birmingham (UAB) Hypertension Clinic whose blood pressure could not be controlled on any antihypertensive regimen.6 The analysis included 304 consecutive patients referred for uncontrolled resistant hypertension, of whom 29 were identified as having refractory hypertension. Refractory hypertension was defined as failure to achieve blood pressure control with treatment prescribed by hypertension experts at minimum of 3 follow-up visits during at least 6 months of care. The 29 patients classified as refractory were receiving an average of 6 different antihypertensive medications (range of 5-8) at the end of the analysis period. All but 1 of the patients with refractory hypertension were being treated with a diuretic and 80% were receiving spironolactone.6
The most recent study to evaluate refractory hypertension as a phenotype of treatment failure was a prospective assessment of over 550 consecutive patients also referred to the UAB Hypertension Clinic for uncontrolled resistant hypertension.7 Of these, 15 were subsequently diagnosed with refractory hypertension. In this study, refractory hypertension was defined as uncontrolled hypertension despite of use of 5 or more different classes of antihypertensive agents, including a long-acting thiazide or thiazide-like diuretic (i.e., chlorthalidone) and a mineralocorticoid receptor antagonist (MRA) (i.e., spironolactone or eplerenone).
In a cross-sectional analysis of patients referred to the Resistant Hypertension Clinic at the University of Campinas, Campinas, Brazil, Modolo et al. compared 36 patients with refractory hypertension to 80 patients with resistant hypertension.8 Refractory hypertension was defined as uncontrolled hypertension in spite of use of at least 5 different classes of antihypertensive agents. Diuretic usage was not specified, but all of the refractory patients were receiving a diuretic and slightly more than 70% were receiving spironolactone.
The Reasons for Geographic And Racial Differences in Stroke (REGARDS) Study is a large population-based cohort study of over 30,000 participants, of whom, 14,854 are being treated for hypertension.9 In a cross-sectional analysis of this cohort, Calhoun et al. identified 78 participants as having refractory hypertension based on having uncontrolled hypertension in spite of being prescribed 5 or more antihypertensive agents.10 All of the participants identified has having refractory hypertension were receiving a diuretic, but less than 20% were prescribed a MRA such as spironolactone.
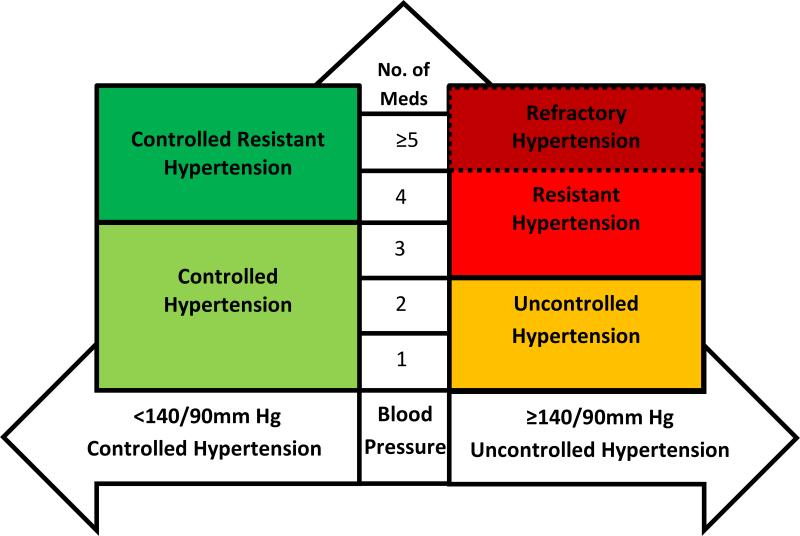
Among the 4 published studies of refractory hypertension, the phenotype was defined variably as either failing treatment after at least 3 months of care by a hypertension specialist; failing to control blood pressure with use of 5 or more different classes of antihypertensive agents; or, most rigorously, failing treatment comprised of 5 or more different classes of antihypertensive agents, including chlorthalidone and spironolactone. The latter more rigorous definition is what we believe the most appropriate. Given the well-established superiority of the thiazide-type diuretic chlorthalidone over hydrochlorothiazide (HCTZ) to reduce blood pressure and the preferential benefit of MRAs for treating resistant hypertension, any treatment regimen should not be considered truly maximal unless it incorporates intensive diuretic therapy based on the combined use of both of these agents.11-14 A schematic of different hypertensive categories, including refractory hypertension, based on blood control and the number of prescribed antihypertensive medications is shown in Figure 1.
Figure 1.
Hypertension classification based on blood pressure control and number of antihypertensive medications (No. of Meds). Reprinted with permission.
Prevalence
Resistant Hypertension
The prevalence of resistant hypertension has been consistently reported as 10-20% of all persons with hypertension.4, 15-17 These estimates have generally been based on the number of medications prescribed according to the AHA definition (uncontrolled blood pressure on 3 or more antihypertensive agents or controlled blood pressure on 4 or more agents).4 In one of the largest assessments, Sim et al. analyzed data from individuals enrolled in the Kaiser Permanente Southern California healthcare system.17 The analysis included over 470,000 individuals with hypertension, of whom over 60,000 met the criteria for resistant hypertension. Overall, 12.8% of all hypertensive individuals and 15.3% of those taking antihypertensive medications had resistant hypertension in this analysis. The majority of these individuals had uncontrolled blood pressure while taking 3 or more antihypertensive agents; the remainder had controlled resistant hypertension, i.e., blood pressure <140/90 mmHg with use of 4 or more medications.
European studies have reported similar prevalence rates of resistant hypertension in large cohorts. For example, de la Sierra et al. evaluated the prevalence of resistant hypertension in over 60,000 hypertensive individuals participating in the Spanish Ambulatory Blood Pressure Monitoring (ABPM) Registry.15 Over 10,000, or 14.8% of participants were identified as having resistant hypertension based on an elevated office blood pressure (>140/90 mmHg) despite use of 3 antihypertensive agents or treatment with 4 or more agents regardless of the level of office blood pressure. Most (12.2%) of the participants with resistant hypertension had uncontrolled blood pressure levels; only a small proportion (2.6%) had controlled resistant hypertension.
The prevalence of resistant hypertension is higher in persons of African origin, who are overweight or obese, who are older, and especially, in those with chronic kidney disease (CKD). In a recent cross-sectional analysis of the 3,367 hypertensive participants in the Chronic Renal Insufficiency Cohort, 40.4% were identified as having resistant hypertension according to the AHA definition (including both controlled and uncontrolled resistant hypertension).18 In contrast to the Kaiser Permanente and Spanish ABPM Registry cohorts, in which blood pressure was uncontrolled in most participants with resistant hypertension, resistant hypertension in the CRIC cohort was almost evenly divided between individuals with uncontrolled and controlled resistant hypertension (52.5 vs. 47.5%, respectively). As in many other studies, African American race, higher body mass index (BMI), and older age were all independent predictors of having resistant hypertension.18
Refractory Hypertension
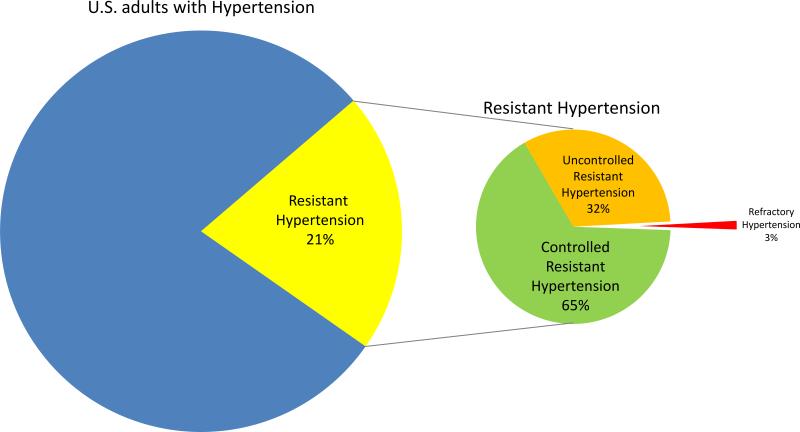
Estimates of prevalence of the phenotype of refractory hypertension are limited to 4 published studies.6-8, 10 The studies are consistent in indicating that refractory hypertension is uncommon, especially if the more rigorous definition that requires patients to fail intensive antihypertensive diuretic treatment that includes chlorthalidone and spironolactone is applied. In the retrospective analysis by Acelajado et al., of the 304 consecutive patients with resistant hypertension included in the analysis, only 29 or 9.5% never achieved blood pressure control when being treated in a hypertension specialty clinic.6 In the follow-up prospective analysis from the same clinic, only 3% of the 559 patients originally referred for uncontrolled resistant hypertension were diagnosed with refractory hypertension.7 An important distinction between these 2 studies that likely explains the lower prevalence of refractory hypertension in the prospective analysis is that the later study specifically required use of chlorthalidone 25 mg and spironolactone 25 mg daily before defining a patient as being refractory to treatment, while the earlier, retrospective analysis had no such requirement. Many of the patients in the earlier retrospective study received hydrochlorothiazide rather than chlorthalidone, and only 80% received spironolactone.6 In contrast, by definition, all of the participants in the prospective study received both agents.7 As suggested by the authors, underutilization of chlorthalidone and spironolactone likely contributed importantly to lower control rates, and thereby, the higher prevalence of refractory hypertension in the earlier study.7
In contrast to the above studies of patients referred to a hypertension specialty clinic specifically for resistant hypertension, the REGARDS cohort includes a large, general hypertensive population.9 In the cross-sectional analysis of this cohort, the prevalence of refractory hypertension (uncontrolled blood pressure on 5 or more agents) was only 0.5% of all hypertensive participants and 3.6% of participants with resistant hypertension.10 This is likely an underestimate, as there was a large proportion of patients who were uncontrolled on 2 and 3 medications, such that after appropriate titration, a percentage would have remained uncontrolled on 5 agents and thus identified as having refractory hypertension. On the other hand, chlorthalidone and spironolactone were rarely used in this cohort, and with broader use, control rates would no doubt have been better. Overall, the findings of these studies indicate that in the general hypertensive population and with the intensive care provided by hypertension specialists, including use of chlorthalidone and spironolactone, true antihypertensive treatment failure is rare (Figure 2).
Figure 2.
Prevalence of resistant and refractory hypertension
“Apparent” versus “True”
Resistant Hypertension
The term “apparent” as opposed to “true resistant hypertension” has been used by investigators to refer to patients with resistant hypertension based on the number of prescribed medications, without accounting for common causes of pseudoresistance, i.e., inaccurate blood pressure measurements, non-adherence, under-treatment, or white coat effects. Such causes of pseudoresistance are common such that up to 50% of patients with apparent resistant hypertension may not be truly resistant to treatment.19
Estimates of the prevalence of the different causes of pseudoresistance have been largely done considering one factor at a time in different cohorts. Analysis of the Spanish Ambulatory Blood Pressure Monitoring Registry estimated that the prevalence of white coat resistant hypertension, that is, uncontrolled office but controlled ambulatory blood pressure levels, to be 37.5% of participants otherwise fulfilling the criteria for having resistant hypertension.15 In a cross-sectional evaluation of almost 500 patients with resistant hypertension who had undergone ambulatory blood pressure monitoring, Muxfeldt et al. reported very similar results, with 37.0% of patients having white coat resistant hypertension.20
Poor adherence to antihypertensive drug treatment is a common cause of pseudoresistance among patients with apparent resistant hypertension. Jung et al. evaluated patients referred to a university-based nephrology clinic for resistant hypertension.21 After exclusion of secondary causes of hypertension and white coat resistant hypertension, adherence was quantified by testing for prescribed antihypertensive medications or their metabolites by liquid chromatography-mass spectrometry analysis of urine samples.21 Of the 76 patients assessed, 53% were identified as being non-adherent: 30% were taking none of their prescribed medications, with the remainder being only partially adherent. In a prospective assessment of 339 patients undergoing evaluation for resistant hypertension while either hospitalized or as an outpatient, Štrauch et al. determined adherence by measuring serum antihypertensive medication concentrations by liquid chromatography-mass spectrometry.22 Overall 47% of patients were considered non-adherent, with roughly half taking none of their medications.
Most studies have quantified single causes of pseudoresistance in their respective cohorts. In contrast, a study by Grigoryan et al. simultaneously determined the prevalence of poor adherence, white coat resistant hypertension, and under-treatment as causes of pseudo-resistant hypertension in the same cohort.19 This study was a retrospective analysis of primary care patients with resistant hypertension who were participants in a study of determinants of blood pressure control that included electronic pill monitoring and ambulatory blood pressure measurement. Of the 69 patients analyzed, 22% had white coat resistant hypertension and 29% were non-adherent with their medications based on taking <80% of the prescribed doses.19 Accordingly, only half of the patients could be classified has having true resistant hypertension based on being adequately adherent with their prescribed medications and having elevated ambulatory blood pressure levels. Further, none of these patients were optimally treated in that only a small number of them were receiving a maximum recommended dose of an angiotensin converting enzyme inhibitor, angiotensin receptor blocker, or calcium channel blocker, and none were receiving chlorthalidone or spironolactone. Combined, these studies clearly demonstrate that pseudo-resistant hypertension represents a large proportion of patients with apparent resistant hypertension, since more than 50% of patients in these cohorts were not adequately compliant with their prescribed medications, had white coat resistant hypertension, or were undertreated.
Refractory Hypertension
The prevalence of contributors to pseudoresistance, i.e., poor medication adherence, white coat effects, and under-treatment, has not yet been quantified in patients with refractory hypertension. In the comparison of patients with refractory versus resistant hypertension by Modolo et al., a significant white coat effect was reported as being much more common in the refractory group, but the actual prevalence of white coat refractory hypertension was not indicated.8 Dudenbostel et al. reported that ambulatory blood pressure levels were significantly higher in patients with refractory hypertension compared to those with controlled resistant hypertension, but did not quantify the prevalence of white coat refractory hypertension.7 None of the studies of refractory hypertension has reported adherence based on measurement of drug or drug metabolite levels in serum or urine. Application of the strictest definition of refractory hypertension, i.e., use of 5 or medications including chlorthalidone and spironolactone (or pharmacologic equivalents), excludes under-treatment as a cause of antihypertensive treatment failure. Further, the contribution of inaccurate blood pressure measurement to apparent lack of blood pressure control has not been specifically quantified for either resistant or refractory hypertension.
Risk Factors and Comorbidities
Resistant Hypertension
Large, cross-sectional analyses consistently identify older age, increased body mass index (BMI), African American race, and male gender as strong, independent risk factors for having resistant hypertension, with African American race being the patient characteristic most commonly associated with treatment resistance.15-17, 23 These studies also show that chronic kidney disease (CKD), diabetes, heart disease, and left ventricular hypertrophy are common comorbidities associated with resistant hypertension, with CKD being especially common.
Refractory Hypertension
Important similarities and differences in risk factors have been identified in persons with refractory hypertension compared to the larger population of patients with resistant hypertension. Both refractory and resistant hypertension are more common among patients of African ancestry compared to those of European descent.7, 8, 10 In contrast, patients with refractory hypertension tend to be younger but of similar weight compared to the larger cohort of patients with resistant hypertension, indicating that increasing age and higher BMI are not risk factors for having refractory hypertension compared to resistant hypertension.6-8, 10 There is evidence of gender differences between refractory versus resistant hypertension cohorts. While not observed in the retrospective or cross-sectional analyses, the prospective study of refractory hypertension that utilized the most rigorous definition of the phenotype, i.e., requiring failure of 5 or more drug regimen including chlorthalidone and spironolactone, refractory hypertension was more common in women, such that African American women were the race-gender subgroup most affected.7
While it seems intuitive that patients with refractory hypertension, given their history of severe blood pressure elevation, should have more comorbidities, particularly cardiovascular disease, than patients with resistant hypertension, the published literature has not consistently supported this conclusion. In the cross-sectional analysis of the REGARDS cohort, refractory hypertension was more commonly associated with CKD (i.e., albuminuria) and diabetes than was resistant hypertension, and patients with refractory patients were more likely to have a history of stroke or heart disease compared to all hypertensive individuals.10 In the retrospective analysis of patients referred to the UAB Hypertension Clinic, patients with refractory, compared to controlled resistant hypertension, were more likely to have a history of prior stroke or congestive heart failure (CHF), but not diabetes or CKD.6 Similarly, in the prospective assessment done by the same investigators, diabetes, CKD, and prior stroke were not more common in refractory patients compared to those with controlled resistant hypertension, but refractory patients were more likely to have been hospitalized for CHF.7 The retrospective analysis by Modolo et al. did not find differences in comorbidities between patients with refractory versus resistant hypertension except that refractory patients were more likely to have left ventricular hypertrophy (LVH) based on echocardiography.8
The lack of consistency in the reported associations between refractory hypertension and various comorbidities is likely attributable, at least in part, to differences in study design, especially in how refractory hypertension was defined. For example, both the retrospective and prospective studies carried out in the UAB Hypertension Clinic and the cross-sectional analysis done at the Resistant Hypertension Clinic at the University of Campinas specifically excluded patients with Stage 4 and 5 CKD, thereby precluding identification of any association between refractory hypertension and advanced CKD.6-8
Prognosis
Resistant Hypertension
Longitudinal studies indicate that patients with resistant hypertension, especially if uncontrolled, have a worse prognosis than general hypertensive cohorts, both in terms of cardiovascular events and total mortality.16, 23-27 For example, in a secondary analysis of data from over 14,000 hypertensive participants in the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT), the incidence of coronary heart disease (CHD), stroke, CHF, peripheral arterial disease (PAD), and end-stage renal disease (ESRD) were all increased among those with controlled or uncontrolled resistant hypertension compared to those without resistant hypertension.16
In an analysis of the ongoing REGARDS Study, Irvin et al. found that the incidence of stroke, CHD, and all-cause mortality was increased in participants with controlled or uncontrolled resistant hypertension compared to those without resistant hypertension during a median follow-up of 5.9, 4,4 and 6.0 years for stroke, CHD, and total mortality, respectively.23 After full multivariable adjustment, the increased hazard ratio for CHD and all-cause mortality remained statistically significant, whereas the association of stroke and resistant hypertension did not. After initial adjustment, individuals with controlled resistant hypertension had an increased risk of all-cause mortality compared to participants without resistant hypertension; however, the risk was attenuated after full multivariable analysis. The hazard ratios for stroke and heart disease were not increased among individuals with controlled resistant hypertension compared to participants without resistant hypertension.23
Prognosis is particularly unfavorable in patients with resistant hypertension and CKD. In a recent analysis of hypertensive individuals with CKD participating the CRIC study, the incidence of stroke, CHF, renal events, and all-cause mortality as well as the combined outcomes of stroke, myocardial infarction, and PAD, were increased in individuals with resistant hypertension (controlled or uncontrolled) compared to those without resistant hypertension. The higher risk for each event, except for stroke, remained statistically significant after full multivariable adjustment.
Refractory Hypertension
No study assessing the prognosis of patients with refractory hypertension has yet been reported. While it seems intuitive that patients whose blood pressure cannot be controlled will fare more poorly than those whose blood pressure is controlled, even if it requires use of multiple medications, evidence of such increased risk is currently unavailable.
Mechanisms: Role of Excess Fluid Retention vs. Heightened Sympathetic Tone
Resistant Hypertension
While resistant hypertension is multifactorial in etiology, a large body of literature implicates excess fluid retention as an important cause. A pathogenic role of fluid retention is suggested by studies demonstrating that successful control of resistant hypertension often requires intensification of diuretic therapy.12, 14, 28-30 Such a role is further supported by studies linking indices of increased volume expansion to resistant hypertension and reduction in fluid retention to overcoming treatment resistance. For example, Taler et al. reported that resistant hypertension was characterized by increased thoracic fluid content as measured by thoracic impedance.31 Awareness of this increased fluid retention on an individual patient basis allowed treating clinicians to tailor prescribed antihypertensive regimens to achieve better blood pressure control rates, primarily through broader use of diuretic therapy. Gaddam et al. also reported that patients with resistant hypertension have persistent fluid retention in spite of use of a standard thiazide diuretic (HCTZ) that could be overcome by intensifying diuretic therapy by combining chlorthalidone with spironolactone.32, 33 Well recognized causes of the excess volume that characterizes resistant hypertension include increased salt sensitivity attributable to African American race, CKD, older age, and obesity; high rates of hyperaldosteronism, and high dietary sodium intake.34, 35
Refractory Hypertension
Findings from published studies provide evidence that refractory hypertension may be less volume dependent than resistant hypertension. This is suggested by its definition in that patients with refractory hypertension are identified only after failing intensive diuretic treatment, including the combination of chlorthalidone and spironolactone. Further, indirect indices of volume status suggest similar or even reduced fluid retention in patients with refractory versus controlled resistant hypertension. For example, in their prospective analysis of patients with refractory hypertension, prior to the standardization of the diuretic regimen with use of chlorthalidone and spironolactone, Dudenbostel and colleagues found that plasma renin activity, brain natriuretic peptide levels, and 24-hr urine aldosterone excretion were similar in the two groups, while dietary sodium ingestion (as indexed by 24-hr urinary sodium excretion) was significantly lower in the patients with refractory hypertension.7 In addition, thoracic fluid content measured by thoracic impedance was not different in the two groups. These findings are important in terms of excluding excess fluid retention, aldosterone production, and dietary sodium intake of greater magnitude as causes of antihypertensive treatment failure than that seen in the general population of patients with resistant hypertension.
Stimulated by the observation of higher clinic heart rates in the earlier retrospective analysis of patients with refractory hypertension, the study of Dudenbostel et al. was designed to prospectively explore other indices of sympathetic tone.6, 7 Patients with refractory hypertension were found to have higher resting heart rates compared to patients with controlled resistant hypertension both in the clinic and by ambulatory monitoring.7 The difference was most pronounced at night, with nighttime ambulatory heart rates of 72.7±9.0 vs. 65.6±9.0 beats/min in patients with refractory vs. controlled resistant hypertension, respectively. Further evidence of increased sympathetic tone included increased 24-hr urinary excretion of normetanephrines, increased vascular resistance as indexed by pulse wave analysis and velocity, and reduced heart rate variability.7 If heightened sympathetic tone is confirmed by prospective assessments of these parameters in larger cohorts or by direct measurement of sympathetic outflow, the finding would suggest an important mechanistic distinction between refractory compared to resistant hypertension, that is, refractory hypertension may be more neurogenic in etiology whereas resistant hypertension tends to be more volume dependent. Further, this observation may have important therapeutic implications in that control of refractory hypertension may require application of effective sympatholytic strategies either with pharmacologic agents or device-based approaches as opposed to continued intensification of diuretic therapy.
The finding of heightened sympathetic tone in patients with refractory hypertension is potentially critical in identifying an important mechanistic cause of antihypertensive treatment failure. However, the findings to date are not definitive and have not been consistently observed across studies. For example, higher heart rates were not observed in the cross-sectional analyses of participants in the REGARDS study nor in the cross-sectional analysis of by Modolo et al. of patients with refractory hypertension in their university-based clinic.6-8, 10 Further, increases in sympathetic tone may represent a secondary phenomenon rather than an underlying cause of refractory hypertension. Possible secondary causes of increased heart rates and sympathetic tone in patients with refractory hypertension include more severe CKD, underlying CHF, over diuresis, obstructive sleep apnea, and/or greater use of vasodilators, all of which are known to promote increased sympathetic output. Design of future studies to further explore this proposed phenotype should take these competing possibilities into consideration.
Conclusion
A novel phenotype of antihypertensive treatment failure is proposed based on the inability to control high blood pressure with use of 5 or more different classes of antihypertensive agents, including a long-acting thiazide-type diuretic, such as chlorthalidone, and a MRA, such as spironolactone. Findings from a small number of recent studies suggest the phenotype is rare, with a prevalence of less than 5% of patients referred to hypertension centers for uncontrolled resistant hypertension. The degree to which pseudo-causes of treatment failure, such as poor adherence and white coat effects, contribute to the apparent prevalence the phenotype is unknown.
Studies characterizing patients with refractory hypertension indicate that, similar to resistant hypertension in general, being of African ancestry and having CKD increases risk of never achieving blood pressure control. However, patients with refractory hypertension tend to be younger and more likely female than their counterparts with controlled resistant hypertension (Table). Not surprisingly, patients with refractory hypertension are at greatly increased cardiovascular risk, especially related to LVH and CHF.
Table.
Characteristics of patients with refractory and controlled resistant hypertension.
| Characteristics | Refractory hypertension | Controlled resistant hypertension |
|---|---|---|
| Patient characteristics | ||
| Age | Younger | Older |
| Gender | More female | Both |
| African descent | Higher | |
| BMI | No difference | |
| Comorbidities | ||
| Type 2 diabetes | No difference | |
| Chronic kidney disease | ? | |
| Heart disease | No difference | |
| Stroke | No difference | |
| Heart failure | Higher | |
| Biochemical parameters | ||
| eGFR | ? | |
| Plasma aldosterone | No difference | |
| Plasma renin activity | No difference | |
| 24h urinary aldosterone | No difference | |
| 24h urinary sodium | Higher | |
| 24h urinary normetanephrines | Higher | |
| Hemodynamic parameters | ||
| Clinic heart rate | Higher | |
| Clinic systolic BP | Higher | |
| Clinic diastolic BP | Higher | |
| Aortic stiffness | Higher | |
| Heart Rate Variability | Higher | |
| Central aortic BP | Higher | |
| 24h heart rate | Higher | |
| 24h mean BP | Higher | |
BMI, body mass index; BP, blood pressure, eGFR, estimated glomerular filtration rate.
Underlying mechanisms of refractory hypertension clearly lack full elucidation, but available findings do not support greater degrees of fluid retention and/or aldosterone excess as contributing causes. Findings of increased heart rate and catecholamine excretion suggest a possible role of increased sympathetic tone as an important mediator.
Acknowledgments
Source of Funding
Work on this paper was by supported by the National Institutes of Health (NIH R01 HL113004).
Footnotes
Disclosures
Dr. Calhoun has received travel support/consulting fees from Valencia Technologies.
References
- 1.Van Dyne JR. Iproniazid in the treatment of resistant hypertension. A preliminary report on twenty intractable cases. J Am Geriatr Soc. 1960;8:454–462. doi: 10.1111/j.1532-5415.1960.tb00410.x. [DOI] [PubMed] [Google Scholar]
- 2.Gifford RW., Jr. Resistant hypertension. Introduction and definitions. Hypertension. 1988;11:II65–66. doi: 10.1161/01.hyp.11.3_pt_2.ii65. [DOI] [PubMed] [Google Scholar]
- 3.Gifford RW, Jr., Tarazi RC. Resistant hypertension: diagnosis and management. Ann Intern Med. 1978;88:661–665. doi: 10.7326/0003-4819-88-5-661. [DOI] [PubMed] [Google Scholar]
- 4.Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, White A, Cushman WC, White W, Sica D, Ferdinand K, Giles TD, Falkner B, Carey RM. Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension. 2008;51:1403–1419. doi: 10.1161/HYPERTENSIONAHA.108.189141. [DOI] [PubMed] [Google Scholar]
- 5.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr., Jones DW, Materson BJ, Oparil S, Wright JT, Jr., Roccella EJ, National Heart L. Blood Institute Joint National Committee on Prevention DE. Treatment of High Blood P and National High Blood Pressure Education Program Coordinating C The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 6.Acelajado MC, Pisoni R, Dudenbostel T, Dell'Italia LJ, Cartmill F, Zhang B, Cofield SS, Oparil S, Calhoun DA. Refractory hypertension: definition, prevalence, and patient characteristics. J Clin Hypertens. 2012;14:7–12. doi: 10.1111/j.1751-7176.2011.00556.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dudenbostel T, Acelajado MC, Pisoni R, Li P, Oparil S, Calhoun DA. Refractory Hypertension: Evidence of Heightened Sympathetic Activity as a Cause of Antihypertensive Treatment Failure. Hypertension. 2015;66:126–133. doi: 10.1161/HYPERTENSIONAHA.115.05449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Modolo R, de Faria AP, Sabbatini AR, Barbaro NR, Ritter AM, Moreno H. Refractory and resistant hypertension: characteristics and differences observed in a specialized clinic. J Am Soc Hypertens. 2015;9:397–402. doi: 10.1016/j.jash.2015.03.005. [DOI] [PubMed] [Google Scholar]
- 9.Howard VJ, Cushman M, Pulley L, Gomez CR, Go RC, Prineas RJ, Graham A, Moy CS, Howard G. The reasons for geographic and racial differences in stroke study: objectives and design. Neuroepidemiology. 2005;25:135–143. doi: 10.1159/000086678. [DOI] [PubMed] [Google Scholar]
- 10.Calhoun DA, Booth JN, 3rd, Oparil S, Irvin MR, Shimbo D, Lackland DT, Howard G, Safford MM, Muntner P. Refractory hypertension: determination of prevalence, risk factors, and comorbidities in a large, population-based cohort. Hypertension. 2014;63:451–458. doi: 10.1161/HYPERTENSIONAHA.113.02026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ernst ME, Carter BL, Goerdt CJ, Steffensmeier JJ, Phillips BB, Zimmerman MB, Bergus GR. Comparative antihypertensive effects of hydrochlorothiazide and chlorthalidone on ambulatory and office blood pressure. Hypertension. 2006;47:352–358. doi: 10.1161/01.HYP.0000203309.07140.d3. [DOI] [PubMed] [Google Scholar]
- 12.Khosla N, Chua DY, Elliott WJ, Bakris GL. Are chlorthalidone and hydrochlorothiazide equivalent blood-pressure-lowering medications? J Clin Hypertens. 2005;7:354–356. doi: 10.1111/j.1524-6175.2005.04451.x. [DOI] [PubMed] [Google Scholar]
- 13.Nishizaka MK, Zaman MA, Calhoun DA. Efficacy of low-dose spironolactone in subjects with resistant hypertension. Am J Hypertens. 2003;16:925–930. doi: 10.1016/s0895-7061(03)01032-x. [DOI] [PubMed] [Google Scholar]
- 14.Williams B, MacDonald TM, Morant S, Webb DJ, Sever P, McInnes G, Ford I, Cruickshank JK, Caulfield MJ, Salsbury J, Mackenzie I, Padmanabhan S, Brown MJ, British Hypertension Society's PSG Spironolactone versus placebo, bisoprolol, and doxazosin to determine the optimal treatment for drug-resistant hypertension (PATHWAY-2): a randomised, double-blind, crossover trial. Lancet. 2015;386:2059–2068. doi: 10.1016/S0140-6736(15)00257-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.de la Sierra A, Segura J, Banegas JR, Gorostidi M, de la Cruz JJ, Armario P, Oliveras A, Ruilope LM. Clinical features of 8295 patients with resistant hypertension classified on the basis of ambulatory blood pressure monitoring. Hypertension. 2011;57:898–902. doi: 10.1161/HYPERTENSIONAHA.110.168948. [DOI] [PubMed] [Google Scholar]
- 16.Muntner P, Davis BR, Cushman WC, Bangalore S, Calhoun DA, Pressel SL, Black HR, Kostis JB, Probstfield JL, Whelton PK, Rahman M, Group ACR Treatment-resistant hypertension and the incidence of cardiovascular disease and end-stage renal disease: results from the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Hypertension. 2014;64:1012–1021. doi: 10.1161/HYPERTENSIONAHA.114.03850. [DOI] [PubMed] [Google Scholar]
- 17.Sim JJ, Bhandari SK, Shi J, Liu IL, Calhoun DA, McGlynn EA, Kalantar-Zadeh K, Jacobsen SJ. Characteristics of resistant hypertension in a large, ethnically diverse hypertension population of an integrated health system. Mayo Clin Proc. 2013;88:1099–1107. doi: 10.1016/j.mayocp.2013.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thomas G, Xie D, Chen HY, Anderson AH, Appel LJ, Bodana S, Brecklin CS, Drawz P, Flack JM, Miller ER, 3rd, Steigerwalt SP, Townsend RR, Weir MR, Wright JT, Jr., Rahman M, Investigators CS Prevalence and Prognostic Significance of Apparent Treatment Resistant Hypertension in Chronic Kidney Disease: Report From the Chronic Renal Insufficiency Cohort Study. Hypertension. 2016;67:387–396. doi: 10.1161/HYPERTENSIONAHA.115.06487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grigoryan L, Pavlik VN, Hyman DJ. Characteristics, drug combinations and dosages of primary care patients with uncontrolled ambulatory blood pressure and high medication adherence. J Am Soc Hypertens. 2013;7:471–476. doi: 10.1016/j.jash.2013.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Muxfeldt ES, Bloch KV, Nogueira Ada R, Salles GF. True resistant hypertension: is it possible to be recognized in the office? Am J Hypertens. 2005;18:1534–1540. doi: 10.1016/j.amjhyper.2005.06.013. [DOI] [PubMed] [Google Scholar]
- 21.Jung O, Gechter JL, Wunder C, Paulke A, Bartel C, Geiger H, Toennes SW. Resistant hypertension? Assessment of adherence by toxicological urine analysis. J Hypertens. 2013;31:766–774. doi: 10.1097/HJH.0b013e32835e2286. [DOI] [PubMed] [Google Scholar]
- 22.Strauch B, Petrak O, Zelinka T, Rosa J, Somloova Z, Indra T, Chytil L, Maresova V, Kurcova I, Holaj R, Wichterle D, Widimsky J., Jr Precise assessment of noncompliance with the antihypertensive therapy in patients with resistant hypertension using toxicological serum analysis. J Hypertens. 2013;31:2455–2461. doi: 10.1097/HJH.0b013e3283652c61. [DOI] [PubMed] [Google Scholar]
- 23.Irvin MR, Booth JN, 3rd, Shimbo D, Lackland DT, Oparil S, Howard G, Safford MM, Muntner P, Calhoun DA. Apparent treatment-resistant hypertension and risk for stroke, coronary heart disease, and all-cause mortality. J Am Soc Hypertens. 2014;8:405–413. doi: 10.1016/j.jash.2014.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kumbhani DJ, Steg PG, Cannon CP, Eagle KA, Smith SC, Jr., Crowley K, Goto S, Ohman EM, Bakris GL, Perlstein TS, Kinlay S, Bhatt DL, Investigators RR Resistant hypertension: a frequent and ominous finding among hypertensive patients with atherothrombosis. Eur Heart J. 2013;34:1204–1214. doi: 10.1093/eurheartj/ehs368. [DOI] [PubMed] [Google Scholar]
- 25.Pepine CJ, Handberg EM, Cooper-DeHoff RM, Marks RG, Kowey P, Messerli FH, Mancia G, Cangiano JL, Garcia-Barreto D, Keltai M, Erdine S, Bristol HA, Kolb HR, Bakris GL, Cohen JD, Parmley WW, Investigators I A calcium antagonist versus a non-calcium antagonist hypertension treatment strategy for patients with coronary artery disease. The International Verapamil-Trandolapril Study (INVEST): a randomized controlled trial. JAMA. 2003;290:2805–2816. doi: 10.1001/jama.290.21.2805. [DOI] [PubMed] [Google Scholar]
- 26.Smith SM, Gong Y, Handberg E, Messerli FH, Bakris GL, Ahmed A, Bavry AA, Pepine CJ, Cooper-Dehoff RM. Predictors and outcomes of resistant hypertension among patients with coronary artery disease and hypertension. J Hypertens. 2014;32:635–643. doi: 10.1097/HJH.0000000000000051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Smith SM, Huo T, Delia Johnson B, Bittner V, Kelsey SF, Vido Thompson D, Noel Bairey Merz C, Pepine CJ, Cooper-Dehoff RM. Cardiovascular and mortality risk of apparent resistant hypertension in women with suspected myocardial ischemia: a report from the NHLBI-sponsored WISE Study. J Am Heart Assoc. 2014;3:e000660. doi: 10.1161/JAHA.113.000660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Garg JP, Elliott WJ, Folker A, Izhar M, Black HR, Service RUH Resistant hypertension revisited: a comparison of two university-based cohorts. Am J Hypertens. 2005;18:619–626. doi: 10.1016/j.amjhyper.2004.11.021. [DOI] [PubMed] [Google Scholar]
- 29.Ouzan J, Perault C, Lincoff AM, Carre E, Mertes M. The role of spironolactone in the treatment of patients with refractory hypertension. Am J Hypertens. 2002;15:333–339. doi: 10.1016/s0895-7061(01)02342-1. [DOI] [PubMed] [Google Scholar]
- 30.Vlase HL, Panagopoulos G, Michelis MF. Effectiveness of furosemide in uncontrolled hypertension in the elderly: role of renin profiling. Am J Hypertens. 2003;16:187–193. doi: 10.1016/s0895-7061(02)03260-0. [DOI] [PubMed] [Google Scholar]
- 31.Taler SJ, Textor SC, Augustine JE. Resistant hypertension: comparing hemodynamic management to specialist care. Hypertension. 2002;39:982–988. doi: 10.1161/01.hyp.0000016176.16042.2f. [DOI] [PubMed] [Google Scholar]
- 32.Gaddam K, Corros C, Pimenta E, Ahmed M, Denney T, Aban I, Inusah S, Gupta H, Lloyd SG, Oparil S, Husain A, Dell'Italia LJ, Calhoun DA. Rapid reversal of left ventricular hypertrophy and intracardiac volume overload in patients with resistant hypertension and hyperaldosteronism: a prospective clinical study. Hypertension. 2010;55:1137–1142. doi: 10.1161/HYPERTENSIONAHA.109.141531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gaddam KK, Nishizaka MK, Pratt-Ubunama MN, Pimenta E, Aban I, Oparil S, Calhoun DA. Characterization of resistant hypertension: association between resistant hypertension, aldosterone, and persistent intravascular volume expansion. Arch Intern Med. 2008;168:1159–1164. doi: 10.1001/archinte.168.11.1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Calhoun DA, Nishizaka MK, Zaman MA, Thakkar RB, Weissmann P. Hyperaldosteronism among black and white subjects with resistant hypertension. Hypertension. 2002;40:892–896. doi: 10.1161/01.hyp.0000040261.30455.b6. [DOI] [PubMed] [Google Scholar]
- 35.Pimenta E, Gaddam KK, Oparil S, Aban I, Husain S, Dell'Italia LJ, Calhoun DA. Effects of dietary sodium reduction on blood pressure in subjects with resistant hypertension: results from a randomized trial. Hypertension. 2009;54:475–481. doi: 10.1161/HYPERTENSIONAHA.109.131235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Siddiqui M, Dudenbostel T, Calhoun DA. Resistant and Refractory Hypertension: Antihypertensive Treatment Resistance vs Treatment Failure. Can J Cardiol. 2015 Jul 8; doi: 10.1016/j.cjca.2015.06.033. doi:10.1016/j.cjca.2015.06.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Roberie DR, Elliott WJ. What is the prevalence of resistant hypertension in the United States? Curr Opin Cardiol. 2012;27:386–391. doi: 10.1097/HCO.0b013e328353ad6e. [DOI] [PubMed] [Google Scholar]